Abstract
In June and July 2010, we conducted a national internet-based survey of 64 city, state, and territorial immunization program managers (IPMs) to assess their experiences in managing the 2009-10 H1N1 influenza vaccination campaign. Fifty-four (84%) of the managers or individuals responsible for an immunization program responded to the survey. To manage the campaign, 76% indicated their health department activated an incident command system (ICS) and 49% used an emergency operations center (EOC). Forty percent indicated they shared the leadership of the campaign with their state-level emergency preparedness program. The managers' perceptions of the helpfulness of the emergency preparedness staff was higher when they had collaborated with the emergency preparedness program on actual or simulated mass vaccination events within the previous 2 years. Fifty-seven percent found their pandemic influenza plan helpful, and those programs that mandated that vaccine providers enter data into their jurisdiction's immunization information system (IIS) were more likely than those who did not mandate data entry to rate their IIS as valuable for facilitating registration of nontraditional providers (42% vs. 25%, p<0.05) and tracking recalled influenza vaccine (50% vs. 38%, p<0.05). Results suggest that ICS and EOC structures, pandemic influenza plans, collaborations with emergency preparedness partners during nonemergencies, and expanded use of IIS can enhance immunization programs' ability to successfully manage a large-scale vaccination campaign. Maintaining the close working relationships developed between state-level immunization and emergency preparedness programs during the H1N1 influenza vaccination campaign will be especially important as states prepare for budget cuts in the coming years.
The authors conducted a study of state and local immunization program managers to assess their experiences in managing the 2009-10 H1N1 influenza vaccination campaign. Results suggest that incident command and emergency operations center structures, pandemic influenza plans, collaborations with emergency preparedness partners during nonemergencies, and expanded use of immunization information systems are important in successfully managing a large-scale vaccination campaign.
The 2009-10 H1N1 influenza vaccination campaign was conducted in response to a major public health event that required state-level1 immunization programs to activate plans to expand their vaccine management and distribution capabilities. Determining how to rapidly disseminate H1N1 influenza vaccine to thousands of new and existing vaccine providers and the public was a major challenge for state and local health departments because of the changing estimates of when the vaccine would be available, uncertainties in distribution, and prioritization strategies.* To rapidly deliver the vaccine, many state-level immunization programs worked closely and in unique ways with their state-level emergency preparedness (EP) programs. Under the National Incident Management System, the federal government encourages all levels of government, including state health departments, to use incident command structures (ICS) and emergency operations centers (EOC) to help efficiently and consistently manage response activities and personnel. Previous studies and after-action reports from other incidents have highlighted the benefits of using ICS and EOC to help organize personnel, responsibilities, and resources.2–4 Understanding how immunization programs collaborated with emergency preparedness programs and how they used ICS and EOC during the H1N1 vaccination campaign can inform future preparedness and response initiatives. Similarly, learning how immunization information systems (IISs), or vaccine registries, helped immunization programs manage H1N1 vaccine inventory and track vaccine administration is key to improving the usefulness of these systems during future vaccine-related events.
Capturing lessons learned to enhance systems that work becomes especially important in light of cuts to federal and state budgets, expiration of American Recovery and Reinvestment Act funds to immunization programs, and potential reorganization of CDC's immunization grant program.5–7 To explore how state-level immunization and emergency preparedness programs worked together and how IISs assisted the relationships and systems implemented during the H1N1 vaccination campaign, we conducted a survey of city, state, and territorial immunization program managers in July 2010.
Methods
We conducted an electronic survey of the 64 immunization program managers (IPMs) representing the city, state, and territory grantee jurisdictions supported by the Centers for Disease Control's (CDC) National Center for Immunization and Respiratory Diseases (NCIRD).8 These CDC grantee jurisdictions include the 50 states, American Samoa, Guam, the Republic of Marshall Islands, Micronesia, the Northern Marianas Islands, Palau, Puerto Rico, the Virgin Islands, Chicago, the District of Columbia, Houston, New York City, Philadelphia, and San Antonio. We conducted the survey in collaboration with the Association of Immunization Managers (AIM), the national professional organization that represents IPMs from all 64 grantee jurisdictions. The survey was open between June 30, 2010, and July 28, 2010. It was initially distributed by email; follow-up with nonrespondents began 2 weeks after initial survey dissemination and included reminders posted in AIM's weekly report to IPMs and follow-up phone calls to nonrespondents.
The 35-question survey asked immunization program managers about their health department's management structure during the H1N1 vaccination campaign, including whether or not the department had used an incident command system (ICS), the role of their incident commander, and whether they opened an emergency operations center (EOC). The survey also gathered perceptions of the helpfulness of existing pandemic influenza plans. The extent of collaboration with state-level emergency preparedness programs was assessed through questions regarding the degree of collaboration with those programs prior to the pandemic, as well as delineation of tasks between the 2 programs during the H1N1 vaccination campaign. Using a 5-point scale with values of “very effective,” “effective,” “neither effective nor ineffective,” “ineffective,” or “very ineffective,” with an additional “not applicable” response option, respondents were asked to describe their perceptions of the effectiveness of the emergency preparedness staff in regards to specific activities related to facilitating their state's overall mass vaccination campaign, supplementing immunization staff, and developing risk communication materials for the public and vaccine providers.
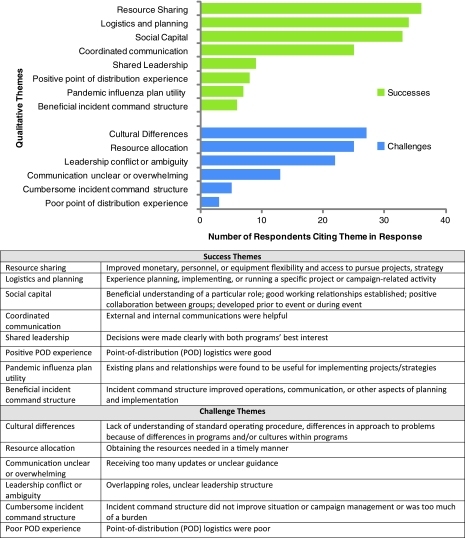
We asked immunization program managers about successes and challenges in working with emergency preparedness programs. Free text responses to these qualitative questions were analyzed for themes by 2 coders with agreement of 90%. A code book was developed a priori and included the themes and codes described below.
Qualitative Codes
Successful Experiences with Emergency Preparedness Programs
Social Capital described comments that implied a beneficial understanding of a particular role, establishment of good working relationships, or positive collaboration between groups developed prior to the H1N1 vaccination campaign or during the campaign event. Resource Sharing described improved monetary, personnel, or equipment management; flexibility; and ability to pursue projects or strategies. Logistics was used to describe positive experiences during planning, implementing, or running a specific project or campaign-related activity. Shared Leadership indicated that decisions were made clearly and jointly with both programs' best interests in mind. Communication was used to code any positive mention of external or internal health department communications. Plan Utility was used when existing plans, particularly pandemic influenza plans, and relationships were found to be useful for implementing projects and strategies. Beneficial ICS indicated that the use of incident command systems improved operations, communications, or other aspects of planning and campaign implementation. Positive POD Experience indicated a positive perception of logistics for points-of-distribution (PODs).
Challenging Experiences with Emergency Preparedness Programs
To describe challenges, Cultural Differences indicated a perceived lack of understanding of standard operating procedures or differences in approach to problems because of differences in programs and/or cultures within programs. Resource Allocation indicated difficulties in obtaining the resources needed in a timely manner (eg, Public Health Emergency Response [PHER] money, personnel, supplies, location, and space issues). Communication was used when respondents indicated receiving too many updates or unclear guidance. Leadership Conflict or Ambiguity indicated that respondents described overlapping roles or unclear leadership structures that had a detrimental effect. Poor ICS indicated that the use of incident command structures or emergency operating centers did not improve the situation or campaign management or became too much of a burden. Poor POD Experience indicated that point-of-distribution site logistics were challenging.
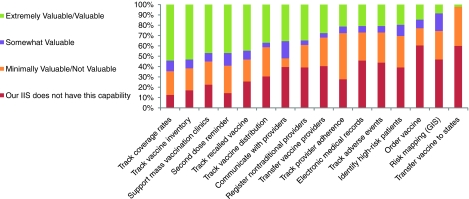
Regarding use of IIS during the mass vaccination campaign, we asked immunization program managers whether providers were required to participate in their state or territory's vaccine registry, and we asked about provider compliance with entering data into the IIS. Perceptions of the value of specific IIS functionalities—including tracking coverage rates, supporting mass immunization clinics, tracking provider adherence to priority group recommendations, pushing vaccine-related communications out to providers, and facilitating the registration of nontraditional providers like OB/GYNs and pharmacies—were assessed using a 5-point Likert-like scale with values of “extremely valuable,” “valuable,” “somewhat valuable,” “minimally valuable,” or “not valuable.” Additionally, the response option “Our IIS does not have this capability” was also available. Immunization program managers were also asked to share any additional functional capabilities they wished their jurisdiction's IIS had that would have aided their ability to manage the vaccination campaign.
At the end of the survey, immunization program managers were offered a free DVD copy of “Master the Disaster,” an interactive, customizable tabletop exercise builder tool designed by the CDC-supported Emory Center for Public Health Preparedness in 2007 to help public health agencies plan, design, conduct, and evaluate disaster preparedness exercises.9
The Emory University institutional review board (IRB) approved the survey as an exempt study. SAS version 9.2 statistical software (SAS Institute, Cary, NC) was used for data analysis, including frequency calculations and proportion comparisons with chi-square and Fisher's exact tests. Associations with a p-value of 0.05 or less were considered statistically significant. Feedback Server version 4.4 (Data Illusion, Geneva, Switzerland) was used to administer the survey. Some respondents did not answer all survey questions, so we analyzed each question with only the number of responses received for that question.
Results
Fifty-four of the 64 (84%) city, state, and territorial immunization program managers or individuals responsible for the immunization program responded to the survey. Forty-six responding managers represented states, 6 represented large U.S. cities, and 2 represented U.S. territories. Respondents to this survey represented programs covering approximately 93% of the estimated 2010 U.S. population.10
Use of ICS, EOCs, and Pandemic Influenza Plans
Seventy-six percent (41/54) of immunization program managers indicated their health department used an ICS to manage the H1N1 vaccination campaign. Of those, 39% said their incident commander was the state public health officer, 32% said the public health preparedness coordinator, 7% the state medical officer, and 5% the immunization program manager. The remaining 17% indicated “other,” followed by open-ended responses largely consisting of nonspecific responses.
Forty-nine percent (26/53) of immunization program managers indicated their health department opened an EOC to manage the influenza vaccine campaign. Of these, 50% (13/26) opened an in-person EOC, 42% (11/26) opened both an in-person and virtual EOC (ie, a web-based EOC), and 4% (1/26) opened only a virtual EOC.
Fifty-seven percent (30/53) found their existing pandemic plan helpful, with 29 respondents specifically citing the plan's role in providing an established framework for response and forging collaborations among stakeholder partners as particularly helpful. Among the 8 respondents who perceived their pandemic influenza plan as unhelpful, the primary reasons cited were the inappropriateness of the plan for the specific characteristics of this pandemic (6 respondents) and the plan's being outdated or inadequate in scope (2 respondents).
Collaborations with Emergency Preparedness Programs
Forty percent (21/53) of responding immunization program managers shared the programmatic lead for the 2009-10 H1N1 influenza vaccination campaign with their emergency preparedness program. Of the remaining 32 managers, 15 (28%) indicated that their immunization program was the programmatic lead, 15 (28%) indicated that the emergency preparedness program was the lead, and 2 (4%) indicated other leadership arrangements.
When stratified by programmatic lead, there were no meaningful differences regarding which program performed the majority of the work related to specific H1N1 mass vaccination activities, except for the activity of establishing point-of-distribution (POD) centers. Among the 15 immunization program managers who indicated that the immunization program was their programmatic lead for the H1N1 influenza vaccination campaign, responses varied regarding which entity performed the majority of the work related to establishing PODs. Five (33%) of these managers indicated that regional or local health departments performed the majority of the POD-related work, 4 (27%) indicated that the immunization program performed the majority of the work, 4 (27%) indicated that the work was jointly shared between the immunization program and the emergency preparedness program, and 2 (13%) indicated that POD establishment was the responsibility of the emergency preparedness program. In contrast, 47% (7/15) of immunization program managers from jurisdictions whose emergency preparedness program was the lead for the vaccination campaign indicated that POD establishment was the responsibility of the emergency preparedness program, and 50% (10/20) of immunization program managers from jurisdictions whose immunization and emergency preparedness programs shared programmatic leadership of the campaign indicated that establishing PODs was also a joint effort between the immunization and emergency preparedness programs.
Seventy percent (38/54) of immunization program managers indicated that their immunization program had coordinated with their emergency preparedness within the previous 2 years to conduct an actual and/or simulated mass vaccination. While the majority of immunization program managers perceived their emergency preparedness staff as effective in facilitating their state's overall H1N1 influenza vaccination response (69%) and supplementing the immunization program staff (56%), managers who had coordinated with their emergency preparedness program on actual and/or simulated mass vaccination events in the 2 years prior to the H1N1 influenza vaccination campaign were more likely to perceive their emergency preparedness staff as effective in specific H1N1-related activities than those who had not coordinated with their emergency preparedness program (Table 1). These activities included allocating scarce vaccine inventory to providers (p=0.03), facilitating decisions about who should receive scarce vaccine among subpriority groups (p=0.05), developing risk communications materials for providers about the H1N1 influenza vaccine (p=0.02), and developing risk communications materials for the public about H1N1 influenza vaccine (p=0.04). The trend was similar for both of the other activities we asked about, supplementing immunization program staff and facilitating the overall H1N1 influenza vaccination campaign, but not significantly so (both p=0.30).
Table 1.
Association of Collaboration with Emergency Preparedness Staff on Mass Vaccination Event in 2 Years Prior to 2009-10 H1N1 Influenza Vaccination Campaign with Immunization Program Managers' Perceived Effectiveness of Emergency Preparedness Staff
| |
Number of Immunization Programs That Had Collaborated with EP Program |
Number of Immunization Programs That Had Not Collaborated with EP Program |
|
||||
|---|---|---|---|---|---|---|---|
| Effective/ very effective | Ineffective/very ineffective/neither effective nor ineffective | Total | Effective/ very effective | Ineffective/very ineffective/neither effective nor ineffective | Total | p-value* | |
| How effective was your EP staff in: | |||||||
| Allocating scarce vaccine inventory to providers (n=37) | 79% | 21% | 24 | 38% | 62% | 13 | 0.03 |
| Facilitating decisions about who should receive scarce vaccine (n=43) | 69% | 31% | 29 | 36% | 64% | 14 | 0.05 |
| Developing risk communications materials about H1N1 influenza vaccine: | |||||||
| For providers (n=44) | 66% | 34% | 32 | 25% | 75% | 12 | 0.02 |
| For the public (n=45) | 69% | 31% | 32 | 31% | 69% | 13 | 0.04 |
| Supplementing immunization program staff (n=45) | 72% | 28% | 32 | 54% | 46% | 13 | 0.30 |
| Facilitating your jurisdiction's overall H1N1 influenza vaccination campaign (n=51) | 78% | 22% | 36 | 60% | 40% | 15 | 0.30 |
p-values ≤0.05 statistically significant
The top 3 successes cited by immunization program managers in regards to working with their emergency preparedness programs during the H1N1 influenza campaign were resource sharing, logistics, and social capital (Figure 1). The top 3 challenges cited were cultural differences between the programs, resource allocation, and leadership conflict or ambiguity. Communication was the theme most commonly indicated as both a success and a challenge.
Figure 1.
Themes Cited by Immunization Program Managers Regarding Successes and Challenges in Collaborating with Emergency Preparedness Programs During the H1N1 Vaccination Campaign. Color images available online at www.liebertonline.com/bsp
Use of Immunization Information Systems
Among the 51 respondents who indicated their jurisdiction has an IIS, 61% (31/51) indicated that provider registration in their IIS was a precondition for receipt of H1N1 influenza vaccine. Fifty-one percent (26/51) indicated that data entry into their IIS was mandatory for H1N1 influenza vaccine providers. Forty-four percent (20/45) and 51% (23/45) indicated that providers were “compliant” or “somewhat compliant,” respectively, with entering data into their IIS. Compared to immunization program managers from jurisdictions that did not mandate providers enter data into their IIS, managers from jurisdictions that did mandate IIS data entry were more likely to rate their IIS as valuable for facilitating registration of nontraditional vaccine providers like obstetricians and pharmacists (42% vs. 25%, p<0.05) and tracking recalled influenza vaccine (50% vs. 38%, p<0.05).
Immunization program managers rated IIS as most valuable for supporting H1N1 influenza vaccination clinics, facilitating reminder/recall for children needing a second dose of vaccine, and tracking vaccine coverage rates (Figure 2). Fifty-seven percent (16/28) of immunization program managers who indicated their IIS has the capability to “facilitate the registration of nontraditional vaccine providers” and 59% (17/29) who indicated their IIS has the capability to “push communications out to providers” rated those functionalities as valuable or extremely valuable to the campaign, while nearly 40% of immunization program managers indicated that their IIS did not have those functionalities. Among 35 respondents who provided comments regarding what capabilities or functionalities they “wished” their IIS had, the most frequent response was more provider participation in their IIS (26%). Other frequently cited responses included better vaccine ordering capabilities (14%), better inventory management (14%), and improved linkage with electronic medical records (14%).
Figure 2.
Perceived Value of IIS Capabilities During 2009-10 H1N1 Vaccination Campaign. Color images available online at www.liebertonline.com/bsp
Discussion
During the 2009-10 H1N1 vaccination campaign, state-level immunization programs employed a variety of strategies to expand their programmatic and technological capacity to distribute H1N1 influenza vaccine in an efficient and timely manner. More than three-quarters of immunization program managers indicated their health department activated an ICS, nearly half indicated their health department opened an EOC to manage the vaccine campaign, and 40% indicated having shared the role of programmatic lead for the campaign with their state-level emergency preparedness program. Immunization program managers' perception of the helpfulness of their department's emergency preparedness staff was also perceived to be higher if they had previously collaborated with the emergency preparedness program for simulation or other emergency preparedness activities. More than half of immunization program managers working in jurisdictions with IISs required providers to enter data into their system, and more than one-third of managers indicated using their IIS as a way to push important communications out to providers. Each of these strategies used during the H1N1 vaccination campaign illustrates the value of the perspective of immunization program managers to collaborating with their emergency preparedness program partners. In addition, immunization program managers also shared input on the importance of IIS to the management of vaccine-related public health emergencies.
The extent to which ICS/EOC structures were used for this vaccination campaign was substantial, given that these management structures were largely foreign to public health agencies prior to the 2003 adoption of the national incident management system (NIMS) that uses ICS for emergency response.11 Since the hierarchical nature of the ICS is not typically used to manage state and local health departments, implementation of the relatively unfamiliar ICS was initially met with some reticence by public health agencies.12 Results from our survey suggest that while some immunization program managers indicated resistance and frustration with the culture of ICS, more felt that using ICS helped them to work effectively and efficiently with collaborators, especially their emergency preparedness partners. Additionally, use of existing pandemic influenza plans was high; many immunization program managers asserted their value in having provided a structured basis for planning and operations as well as in enacting previously established partnerships with entities like hospitals and federally qualified health centers that proved integral to the coordination of the campaign.
In addition to the roles ICS/EOC systems and pandemic influenza preparedness plans played in managing the H1N1 vaccination campaign, shared programmatic leadership and degree of prior collaboration among immunization and emergency preparedness programs also had an impact on program managers' perceptions of their emergency preparedness counterparts during the campaign.
These 2 programs have very different histories in state health departments; immunization programs have existed for nearly 50 years with funding provided by the Vaccination Assistance Act (Section 317 of the Public Health Service Act) and the Vaccines for Children (VFC) program, a federally funded entitlement program that provides childhood vaccines free to children who might otherwise be unable to afford vaccines.13,14 Public health emergency preparedness programs were largely created following the enactment of the Public Health Security and Bioterrorism Preparedness and Response Act of 2002, and they receive the majority of their funding through grants from the CDC and the Health Resources Services Administration (HRSA).15 Since both programs operate largely on discretionary funding that varies from year to year and has either remained constant or declined in recent years, it may be mutually beneficial for these 2 programs to share resources and personnel.
This survey found that among jurisdictions in which the responsibility of campaign management was shared between the immunization program and the emergency preparedness program, the majority of the work needed to establish PODs was also shared. Immunization program managers' perception of the helpfulness of their emergency preparedness colleagues was also affected by their degree of prior collaboration with the emergency preparedness program. While results suggest that immunization program managers' perceptions of their emergency preparedness programs' general helpfulness in facilitating their jurisdiction's mass vaccination response was not significantly associated with exercise collaborations in the previous 2 years, perceptions of the emergency preparedness program's helpfulness on more specific, targeted activities was significantly associated with prior collaborations. Taken together, these findings underscore the importance of interprogram preevent planning and highlight benefits to structuring exercises and responding to actual events in ways that familiarize staff from each program with the specific needs and nuances of the other. Many of the successes and challenges cited by immunization program managers in working with the emergency preparedness program can be achieved or addressed through preevent planning. Developing a mutual understanding of each other's programs and assigning leadership structures that are both flexible and clear when the 2 programs unite are 2 examples. Methods for streamlining and targeting communications as well as determining resource allocation plans can contribute greatly to the success of programmatic collaborations.
In addition to the importance of strong personnel management, the use of IIS technology was also emphasized during the H1N1 influenza vaccination campaign. Mandating provider participation in IIS was an approach some states took to improve the ability to track vaccine, with states more frequently reporting problems tracking vaccine administration if their state did not require mandatory reporting through their state registries.16 Lack of provider compliance with entering data into a registry system limits the benefits these systems can have for activities like inventory management, reminder/recall, and strategic planning on behalf of health departments. While our results suggest that such a requirement did not have a sweeping impact on immunization program managers' perceived value of all IIS's functionalities, it may have assisted the program managers' ability to use their IIS for the registration of nontraditional vaccine providers and tracking recalled vaccine. These functionalities, as well as the ability to use IIS to push communications out to vaccine providers, are especially important in an emergency situation when mass quantities of vaccine need to be distributed and monitored across a diverse population. While many immunization program managers realized the value of having an IIS with these capabilities during the H1N1 vaccination campaign, more than 40% indicated their IIS could not facilitate the registration of nontraditional vaccine providers or push communications out to providers. Enabling more IISs to include these types of functionalities would benefit management of future vaccine-related emergencies. For those programs that did require providers to participate in their IIS for the H1N1 influenza vaccine campaign, it will be important to assess how this affects their willingness to participate in the system over the long term. Moreover, with the push toward adoption of electronic medical records, it remains to be seen how IIS will interface with these systems. As this transition occurs, more research is needed to determine the most effective ways to either merge IIS into electronic health records or enable the 2 systems to exchange information efficiently.
This survey has several limitations. It was not conducted in parallel among state directors of emergency preparedness, so complementary data from their perspectives are currently unavailable. Results from this survey have been shared and discussed with directors of emergency preparedness, and obtaining their responses to similar questions would be particularly useful to comprehensive planning for future public health emergencies. Further, respondent self-report may be biased due to an inability to precisely recall events from the prior year. Another limitation is that the beliefs of immunization program managers regarding collaborations with emergency preparedness programs, use of ICS/EOCs, characteristics of IIS reporting requirements, and other issues were not correlated with outcome measures such as immunization coverage in their respective jurisdictions. Despite this limitation, the results clearly show differences in perceptions of immunization program managers regarding effectiveness of a variety of measures and point the way forward to improved collaborations and preparedness.
Strong partnerships among staff within immunization and emergency preparedness programs are integral to preparedness against future vaccine-related emergencies. Considering the importance of collaboration among immunization programs and emergency preparedness programs, as well as the most effective ways to use information systems like IIS, are especially appropriate in light of the current public health funding landscape. Reductions to Health and Human Services budgets, as well as to state health department budgets, are likely to result in corresponding reductions in state and local public health programs and staff. Fostering alignment of immunization and emergency preparedness programs at a national level could help diffuse the consequences of tighter budgets. Given that the federal governance structure in the U.S. provides autonomy to the states regarding budgetary decisions, encouraging discussions of programmatic collaborations at the level of professional organization might be most practical. Despite such budgetary constraints, maintaining and improving the capacity of public health to respond to health threats remains more important than ever due to the increasing threat of catastrophic illness or injury resulting from natural or man-made disasters.17,18 Understanding which aspects of collaboration worked well and which did not work well during the 2009-10 H1N1 influenza vaccination campaign is important to sustaining these programmatic partnerships over time and across a variety of emergency and nonemergency events.
Conclusion
The 2009-10 pandemic influenza H1N1 vaccination campaign holds useful lessons regarding preparation for and implementation of future mass vaccination programs. Close collaborations among state-level immunization programs and emergency preparedness programs, as well as use of existing pandemic influenza plans, incident command systems, and emergency operation centers, were important in many jurisdictions across the U.S. Coupling these programmatic collaborations with new approaches to use of immunization information systems, such as mandatory provider participation, can assist jurisdictions' responses to future vaccine-related public health threats. Actively maintaining the interprogram relationships and expanded use of IIS that were cultivated during the H1N1 vaccination campaign experience are always important, and especially so as public health budgets fluctuate.
Footnotes
For the purposes of this article, the term state-level is used to describe the immunization programs and emergency preparedness programs operating at the state and territorial levels, as well as those in the 6 major metropolitan areas directly funded by the Centers for Disease Control's (CDC) National Center for Immunization and Respiratory Diseases. Unless otherwise indicated, this does not include immunization programs or emergency preparedness programs that may exist in regional, county, city, or other local levels of government.
Acknowledgments
We thank the American Immunization Registry Association for contributing to the development of this survey and the immunization program managers for participating and responding to this survey. We also thank our graduate research assistants, Koo Chung, Jennifer Richards, and Joshua Van Otterloo, for their assistance in administering, cleaning, and analyzing data related to this survey. This study was supported by a grant from the Centers for Disease Control and Prevention (CDC), grant # 5P01TP000300, to the Emory Preparedness and Emergency Response Research Center, Emory University, Atlanta, GA. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the CDC.
References
- 1.Rambhia KJ. Watson M. Sell TK. Waldhorn R. Toner E. Mass vaccination for the 2009 H1N1 pandemic: approaches, challenges, and recommendations. Biosecur Bioterror Dec. 2010;8(4):321–330. doi: 10.1089/bsp.2010.0043. [DOI] [PubMed] [Google Scholar]
- 2.Porter D. Hall M. Hartl B, et al. Local health department 2009 H1N1 influenza vaccination clinics—CDC staffing model comparison and other best practices. J Public Health Manag Pract. 2011;17(6):530–533. doi: 10.1097/PHH.0b013e31822146eb. [DOI] [PubMed] [Google Scholar]
- 3.Adams EH. Scanlon E. Callahan JJ., 3rd Carney MT. Utilization of an incident command system for a public health threat: West Nile virus in Nassau County, New York, 2008. J Public Health Manag Pract. 2010;16(4):309–315. doi: 10.1097/PHH.0b013e3181bb8392. [DOI] [PubMed] [Google Scholar]
- 4.Mignone AT., Jr Davidson R. Public health response actions and the use of emergency operations centers. Prehosp Disaster Med. 2003;18(3):217–219. doi: 10.1017/s1049023x00001084. [DOI] [PubMed] [Google Scholar]
- 5.Association of Immunization Managers. National ARRA Funds for Immunization. Mar, 2011. http://www.immunizationmanagers.org/immunization/data/ARRA_Fact_Sheet_National.pdf. [Feb 15;2012 ]. http://www.immunizationmanagers.org/immunization/data/ARRA_Fact_Sheet_National.pdf
- 6.U.S. Department of Health and Human Services. Justification of Estimates for Appropriation Committees. 2011. http://www.cdc.gov/fmo/topic/Budget%20Information/appropriations_budget_form_pdf/FY2011_ATSDR_CJ_Final.pdf. [Feb 15;2012 ]. http://www.cdc.gov/fmo/topic/Budget%20Information/appropriations_budget_form_pdf/FY2011_ATSDR_CJ_Final.pdf Fiscal Year.
- 7.Centers for Disease Control and Prevention. Recovery Act Funds for Section 317 Program. 2009. http://www.hhs.gov/recovery/programs/cdc/immunizationgrant.html. [Jan 4;2012 ]. http://www.hhs.gov/recovery/programs/cdc/immunizationgrant.html
- 8.Centers for Disease Control and Prevention. Grantee Immunization Websites. http://www.cdc.gov/vaccines/spec-grps/prog-mgrs/grantee-imz-websites.htm. [Feb 15;2012 ]. http://www.cdc.gov/vaccines/spec-grps/prog-mgrs/grantee-imz-websites.htm
- 9.Emory Center for Public Health Preparedness. Rollins School of Public Health EU. Master the Disaster! 2007. [CD-ROM]
- 10.Mackun P. Wilson S. Population Distribution and Change: 2000 to 2010 (C2010BR-01) Census Briefs. 2010. Mar, 2011.
- 11.Homeland Security Presidential Directive 5. Management of Domestic Incidents. Feb 28, 2003. http://www.dhs.gov/xabout/laws/gc_1214592333605.shtm. [Jan 4;2012 ]. http://www.dhs.gov/xabout/laws/gc_1214592333605.shtm Issued.
- 12.Sergienko E. Public health and the incident command system. American College of Emergency Physicians Newsletter. 2006:15. [Google Scholar]
- 13.Rein DB. Honeycutt AA. Rojas-Smith L. Hersey JC. Impact of the CDC's Section 317 immunization grants program funding on childhood vaccination coverage. Am J Public Health. 2006;96(9):1548–1553. doi: 10.2105/AJPH.2005.078451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hinman AR. Orenstein WA. Rodewald L. Financing immunizations in the United States. Clin Infect Dis. 2004;38(10):1440–1446. doi: 10.1086/420748. [DOI] [PubMed] [Google Scholar]
- 15.Buehler J. Holtgrave D. Who gets how much: funding formulas in federal public health programs. J Public Health Manag Pract. 2007;13(2):151–155. doi: 10.1097/00124784-200703000-00010. [DOI] [PubMed] [Google Scholar]
- 16.Elliott PI. Assessing policy barriers to effective public health response in the H1N1 influenza pandemic. Association of State and Territorial Health Officials Project Report. Jun, 2010.
- 17.Andrus JK. Aguilera X. Oliva O. Aldighieri S. Global health security and the International Health Regulations. BMC Public Health. 2010;10(Suppl 1):S2. doi: 10.1186/1471-2458-10-S1-S2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Johns MC. Blazes DL. International Health Regulations (2005) and the U.S. Department of Defense: building core capacities on a foundation of partnership and trust. BMC Public Health. 2010;10(Suppl 1):S4. doi: 10.1186/1471-2458-10-S1-S4. [DOI] [PMC free article] [PubMed] [Google Scholar]