Abstract
It is estimated that 10–15% of couples are infertile and male factors account for about half of these cases. With the advent of intracytoplasmic sperm injection (ICSI), many infertile men have been able to father offspring. However, teratozoospermia still remains a big challenge to tackle. Septins belong to a family of cytoskeletal proteins with GTPase activity and are involved in various biological processes e.g. morphogenesis, compartmentalization, apoptosis and cytokinesis. SEPTIN12, identified by c-DNA microarray analysis of infertile men, is exclusively expressed in the post meiotic male germ cells. Septin12+/+/Septin12+/− chimeric mice have multiple reproductive defects including the presence of immature sperm in the semen, and sperm with bent neck (defect of the annulus) and nuclear DNA damage. These facts make SEPTIN12 a potential sterile gene in humans. In this study, we sequenced the entire coding region of SEPTIN12 in infertile men (n = 160) and fertile controls (n = 200) and identified ten variants. Among them is the c.474 G>A variant within exon 5 that encodes part of the GTP binding domain. The variant creates a novel splice donor site that causes skipping of a portion of exon 5, resulting in a truncated protein lacking the C-terminal half of SEPTIN12. Most individuals homozygous for the c.474 A allele had teratozoospermia (abnormal sperm <14%) and their sperm showed bent tail and de-condensed nucleus with significant DNA damage. Ex vivo experiment showed truncated SEPT12 inhibits filament formation in a dose-dependent manner. This study provides the first causal link between SEPTIN12 genetic variant and male infertility with distinctive sperm pathology. Our finding also suggests vital roles of SEPT12 in sperm nuclear integrity and tail development.
Introduction
Male infertility
Between 10% and 15% of couples worldwide are affected by reduced fertility, and the defects can be traced to the men in roughly half of the cases [1]. The pathology of male infertility includes anatomic defects, gametogenesis dysfunction, endocrinopathies, immunologic problems, ejaculatory failure, environmental exposures, and gene mutations [2], [3]. During the past two decades, the development of intracytoplasmic sperm injection (ICSI) has changed the treatment of male infertility [4]. Although the ICSI technique is a breakthrough for assisted reproduction, many infertile couples are still unable to achieve paternity through testicular sperm extraction (TESE) and ICSI [5]. Recently, several studies indicated sperm DNA damage is associated with ICSI failure, development arrest of preimplantation embryos and high rates of miscarriage [3], [4], [5].
Septins
Septins belong to a highly conserved family of polymerizing GTP binding proteins [6], [7]. They were initially identified in the budding yeast, Saccharomyces cerevisia. Loss of function for any one of the five septins, Cdc3p, Cdc10p, Cdc11p, Cdc12p, and Shs1p/Sep7p, which are localized to the ring(s) of mother and budding daughter cells, results in multi-nuclear morphology [8], [9]. There are 14 septin genes in mammalian species, and most of them generate multiple splice isoforms [6], [10]. Some septins are expressed ubiquitously, while others are only expressed in well-differentiated cells (e.g. neuron or male germ cells) [6]. In well-differentiated cells, septins are involved in vesicle trafficking and boundary formation [11], [12], [13]. For example, SEPT3 and SEPT5 are solely expressed in neurons, localized in presynaptic terminal and with synaptic vesicles [14], [15]. However, Septin 3− /− and Septin 5−/− mice do not show any overt neurological phenotypes [16], [17]. Besides, growing evidence has suggested mammalian septins interact with diverse molecules to ensure completion of cytokinesis in somatic cells, but the underlying mechanisms still remain elusive [18], [19]. In somatic cells, SEPT2, SEPT6, SEPT7 and SEPT9 have been implicated in the completion of cytokinesis in dividing cells [18], [19], [20], [21]. SEPT7 also interacts with centromere protein E (CENP-E) for stable CENP-E localization to the kinetochore and for achieving chromosome alignment at the equator during cytokinesis [19]. In cell models, knockdown of SEPTIN2, SEPTIN6, SEPTIN7 or SEPTIN9 causes high percentage of cells with two nuclei [18], [22], [23]. However, Septin 6-deficient mice were grossly normal and did not exhibit abnormal phenotypes [24]. Roles of SEPT2, 7 and 9 in the animals are still not demonstrated.
The role of SEPTs in male reproduction
In Drosophila, SEPTs (Pnut, Sep1, and Sep2) are involved in the formation of ring canal structure between the intercellular bridge of male and female germ cells [25]. In the mammalian species, SEPT2, 7 and 9 have been found to co-localize with an intercellular bridge marker of male germ cells, TEX14 (testis-expressed gene14) [26]. Loss of TEX14 in mice cause disruption of intercellular bridge as well as increased apoptosis of germ cells [27]. SEPT4, along with other SEPTs (SEPT1, SETP6, and SEPT7), is located at the annulus, a ring-like structure between the midpiece and the tail region of spermatozoa [12], [13]. Septin 4 null mice were viable but sterile in males; the immotile sperm had defective annulus and showed dis-localization of SEPT1, SEPT6 and SEPT7 from the annulus [12], [13]. Disorganized annulus/septin rings were also found in a subset of human patients with asthenozoospermia [12], [28], [29].
SEPTIN12
We have used microarray analysis to search for genes that are potentially involved in human spermatogenic defects. Of ten novel testis-specific genes thus identified, one was SEPTIN12 (MIM* 611562) [30]. In rat, SEPT12 is found at the annulus of mature spermatozoa [31]. We also found that in humans SEPT12 is expressed in different subcellular compartments of post-meiotic germ cells, including the head and neck of spermatids and the annulus of mature sperm [32]. By knocking out one allele of Septin12 in the mouse, we found that haploinsufficiency of Septin12 results in male sterility [32]. Sperm obtained from Septin12 +/+/Septin12+/− chimeric mice reveals multi-defects including immature sperm, bent- neck with disrupted annulus, and nuclear DNA damage [32], [33]. Considering SEPT12 is exclusively expressed in the testis and its expression level is critical for male germ cell development, SEPTIN12 has emerged as an interesting candidate for male sterile gene.
Filament formation of SEPTs via polymerization
SEPTs usually mediate their cellular function through the formation of macromolecular and hetero-oligomeric filaments both in vivo and in vitro [21], [34]. Biochemical methods have been used to isolate at least three SEPT complexes: SEPT2/6/7 [34], SEPT7/9b/11 [35] and SEPT4/5/8 [36]. The filament-like structure has been observed in many SEPTs [18], [20], [22] and loss of a SEPT subunit may affect the stability of other subunits in the same complex [18], [34], [37]. We previously found that SEPT12 forms long filaments both in vitro (293T cells) and in vivo (round spermatids) [32], [33]. SEPT12 also interacts with SEPT6 and SEPT11 and forms filaments in Hela cells [38], [39]. In the mouse, SEPT1/4/6/7 may be assembled to form a circular-like structure at the annulus of mature sperm [13].
In this study, we sequenced the entire coding sequences of SEPTIN12 in infertile men with abnormal semen parameters and identified ten SNPs. One of them, c.474 G>A, is more prevalent in infertile men than control subjects. This SNP, c.474G>A, located at exon 5 within the GTP binding domain, may create a novel alternative splicing variant by the activation of a cryptic splice donor. The novel transcript leads to the translation of a truncated protein that lacks partial exon 5 and exons 6–10. The truncated SEPT12 may disturb the filament formation of wild-type SEPT12. Infertile men carrying this SNP are presented with distinctive sperm pathology, including de-condensed nucleus with significant DNA damage, bent tail or loss of tail. Our findings provide the first clue about a causal link between SEPTIN12 genetic variant and male infertility with distinctive sperm pathology.
Results
Identification of genetic variants in SEPTIN12
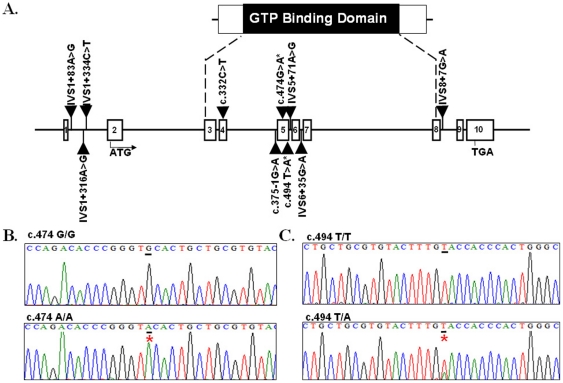
A total of 160 infertile men with abnormal semen parameters and 200 fertile controls were subjected to SEPTIN12 sequence analysis. Ten SNPs identified included seven intronic variants (IVS1+83A>G, IVS1+316A>G, IVS1+334C>T, c.375−1G>A, IVS5+71A>G, IVS6+35G>A and IVS8+7G>A), one synonymous variant (c.474G>A) and two non-synonymous variant (c.332C>A, pThr111Lys; c.494T>A, p.Val165Gln). Their locations are shown in Figure 1A. Six SNPs are located between exon 3 to exon 8, which encode the GTP binding domain critical for the polymerization of SEPT. They are c.332C>A, c.375−1G>A, c.474G>A, c.494T>A, IVS5+71A>G and IVS6+35G>A (Figure 1A). Both allele and genotype frequencies of c.474 A were more prevalent in the infertile men (p = 0.007 and 0.003, respectively) (Figure 1B and Table 1). Another SNP, c.494T>A SNP, was more prevalent in the control subjects (p = 0.032 and 0.013, respectively) (Figure 1B and Table 1).
Figure 1. Identification of novel variants in the SEPTIN12 gene.
Genomic structure of the SEPTIN12 gene and positions of the ten SNPs. Open bars indicate exons. The ATG start site is located at exon 2. Exon 3 to exon 8 encodes the GTP -Binding Domain of SETIN12. (B.–C.) Electropherograms showing DNA sequences. Lower panels show the variant (c.474C→A, Left; c.494T→A, Right) sequences, whereas the upper panels show the wild-type (normal) sequences. Red stars indicate locations of the variants.
Table 1. SEPTIN12 allele frequencies in infertile men and control subjects.
| SNP | Allele frequency | Genotype frequency (%) | ||||||
| Allele | Control (n = 400) (%)) | Spermatogenic failure (n = 320) (%) | p | Genotype | Control (n = 200) (%) | Spermatogenic failure (n = 160) (%) | p | |
| IVS1+ 83A>G | A | 279 (69.8%) | 219 (68.4%) | 0.705 | AA | 93(46.5%) | 80 (50%) | 0.060 |
| G | 121(30.2%) | 101(31.6%) | AG | 93(46.5%) | 59 (37% ) | |||
| GG | 14 (7%) | 21 (13%) | ||||||
| IVS1+ 316A>G | A | 307 (76.8%) | 239 (74.7%) | 0.521 | AA | 117 (58.5%) | 91 (56.9%) | 0.616 |
| G | 93 (23.2%) | 81 (25.3%) | GA | 73(36.5%) | 57 (35.6%) | |||
| GG | 10 (5%) | 12(7.5%) | ||||||
| IVS1+ 334C>T | C | 395 (98.7%) | 315(98.4%) | 0.722 | CC | 195 (97.5%) | 155 (96.9%) | 0.720 |
| T | 5 (1.3%) | 5( 1.6%) | CT | 5(2.5%) | 5 (3.1%) | |||
| TT | 0 (0%) | 0 (0%) | ||||||
| c.332 C>A | C | 394(98.5%) | 318 (99.4%) | 0.266 | CC | 194 (97%) | 158 (98.7%) | 0.263 |
| A | 6(1.5%) | 2 (0.6%) | CA | 6 (3%) | 2 (0.3% ) | |||
| AA | 0(0%) | 0 (0%) | ||||||
| c.375− 1G>A | G | 383 (95.7%) | 297 (92.8%) | 0.087 | GG | 183 (91.5%) | 137 (85.6%) | 0.078 |
| A | 17 (4.3%) | 23 (7.2%) | GA | 17 (8.5%) | 23 (14.4%) | |||
| AA | 0 (0%) | 0 (0%) | ||||||
| c.474 G>A | G | 360(90%) | 266 (83.1%) | 0.007** | GG | 163 (81.5%) | 121(75.6%) | 0.003** |
| A | 40(10%) | 54( 16.9%) | GA | 34(17%) | 24(15.0%) | |||
| AA | 3(1.5%) | 15(9.4%) | ||||||
| c.494 T>A | T | 304 (76%) | 264 (96%) | 0.034* | TT | 104(52%) | 104 (65%) | 0.013* |
| A | 96(24%) | 56(4%) | TA | 96(48%) | 56 (35% ) | |||
| AA | 0(0%) | 0 (0%) | ||||||
| IVS5+ 71A>G | A | 386 (96.5%) | 311 (97.2%) | 0.602 | AA | 187 (93.5%) | 153 (95.6%) | 0.333 |
| G | 14 (3.5%) | 9( 2.8%) | AG | 12 (6%) | 5 (3.1%) | |||
| GG | 1(0.5%) | 2 (1.3%) | ||||||
| IVS6+ 35G>A | G | 385 (96.2%) | 302 (94.4%) | 0.232 | GG | 185 (92.5%) | 146 (91.2%) | 0.074 |
| A | 15 (3.8%) | 18 (5.6%) | GA | 15 (7.5%) | 10 (6.3%) | |||
| AA | 0 (0.0%) | 4 (2.5%) | ||||||
| IVS8+ 7G>A | G | 392(98.0%) | 312 (97.5%) | 0.651 | GG | 192(96.0%) | 152 (95.0%) | 0.647 |
| A | 8 (2.0%) | 8 (2.5%) | GA | 8(4.0%) | 8 (5.0%) | |||
| AA | 0(0.0%) | 0(0.0%) | ||||||
Nucleotide numbering indicates cDNA numbering with 1+ corresponding to the A of the ATG translation initiation codon in the reference cDNA sequence of SEPTIN12 (NM_144605.3).
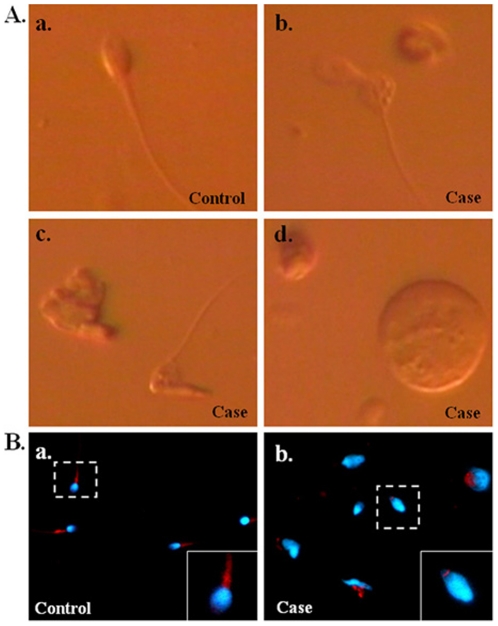
Spermatozoa from patients who carried c.474 A/A showed distinct morphological defects
In this study, 9 of the 15 infertile men with c.474A/A were presented with teratozoospermia (88%–99% of abnormal sperm) (Table 2). To detail the morphological pattern of their spermatozoa, motile sperm organelle morphology examination (MSOME) and immuno-fluorescence assay (IFA) were performed. Most sperm were found to have distinct pathological features, including bent-tail, head with abnormal shape and immature spermatid (Figure 2A and 2B).
Table 2. Clinical features of the 15 men with the c.474 A/A genotype.
| Patient NO. | Age (years) | Sperm count (×106/ml) | Abnormal Sperm (%) | c.474 G/A |
| 1 | 39 | 186.0 | 91 | AA |
| 2 | 33 | 28.4 | 88 | AA |
| 3 | 35 | 20.4 | 99 | AA |
| 4 | 38 | 66.0 | 92 | AA |
| 5 | 38 | 24.0 | 94 | AA |
| 6 | 38 | 91.0 | 92 | AA |
| 7 | 35 | 27.7 | 97 | AA |
| 8 | 43 | 109.0 | 93 | AA |
| 9 | 37 | 1.3 | 97 | AA |
| 10 | 37 | Azoospermia | – | AA |
| 11 | 31 | Azoospermia | – | AA |
| 12 | 30 | Azoospermia | – | AA |
| 13 | 34 | Azoospermia | – | AA |
| 14 | 34 | Azoospermia | – | AA |
| 15 | 25 | NA | NA | AA |
Figure 2. Abnormal morphology of spermatozoa from a case with c.474A/A.
(A.) Motile sperm organelle morphology examination (MSOME) for sperm cells using a high-magnification inverted microscope (magnification was ×8400). (a.) sperm from a fertile control with c.474C/C; (b.–d.) sperm from an infertile man with c.474A/A. Sperm with bent-tail (b.), neck(c.) and round head (d.). (B.) IFA assay for sperm from a fertile control with c.474C/C (a.) and an infertile man with c.474A/A (b.). DAPI: blue; mito-tracker: red. (Magnification: ×400).
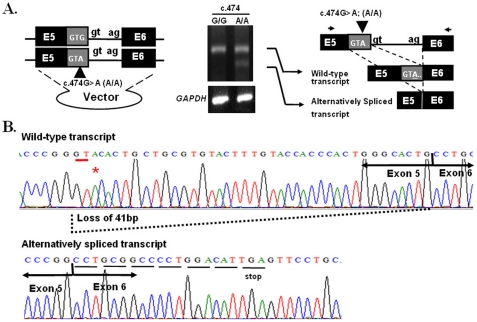
The c.474 G to A transition may activate a cryptic splice donor site
To evaluate the functional effect of c.474G→A, ex vivo assay was preformed in the NTERA-2 d.D1 (NT2D1) cell line, a pluripotent human testicular embryonal carcinoma cells. The cell line was transfected with plasmids containing partial SEPTIN12 (exon 5, intron 5, exon 6, intron 6 and exon 7) with either c.474G/G or A/A. RT-PCR analysis of cells transfected with the c.474 A/A plasmid showed a smaller minor transcript that was absent in cells transfected with the c.474 G/G plasmid (Figure 3A). The ratio between the wild-type and alternatively spliced transcript was about 1.7 to 1. Sequencing analysis showed that the G to A transition created a novel splice donor site and resulted in the skipping of the 3′ portion of exon 5 (loss of 41 bp) and the shift to a new reading frame with a premature stop codon in exon 6 (Figure 3B). The novel transcript therefore encodes a truncated protein lacking the C-terminal half of SEPT12, including part of the GTP binding domain.
Figure 3. Effects of the c.474G→A variant on the splicing process.
(A.) The c.474 G→A SNP induces alternative splicing ex vivo. Left panel: PCR fragments containing exon 5 (E5, back and gray box), intron 5 (within splice donor site “gt” and splice acceptor site “ag”) and exon 6 (E6, black box) with c.474 G or c.474A were constructed into a vector, respectively. Middle panel: products of RT–PCR are shown on an agarose gel. Control: GAPDH Two transcripts (wild-type and alternatively spliced)are produced by the minigene with c.474A. Right panel: schematic depiction of the RT–PCR products. Wild-type transcript: using the original splice donor and acceptor site. Alternatively spliced transcript: using the novel splice donor induced by c.474G→A and the original splice acceptor site. (B.) Sequences of the wild-type (upper panel) and alternatively spliced (lower panel) products from the minigene containing c.474A. The alternatively spliced transcript induces a novel splice donor site, which results in skipping of partial exon 5 (with loss of 41 bp), and also created a premature stop codon in exon 6.
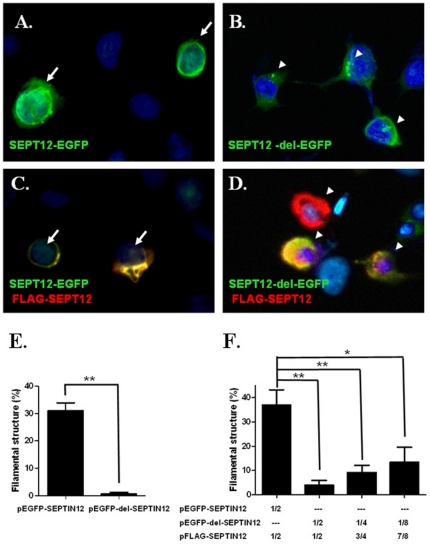
Truncated SPET12 disrupts polymerization of wild-type SEPT12 and nuclear membrane localization
To determine the functional significance of the truncated SEPT12 protein (SEPT12-del-EGFP) generated from the c.474A/A allele, plasmids encoding SEPT12-EGFP and SEPT12-del-EGFP were transfected into NT2D1 cells, respectively. Over-expressed SEPT12-EGFP formed filaments surrounding the nuclear membrane (Figure 4A.). However, over-expressed SEPT12-del-EGFP aggregated to form a dot- like structure that did not surround the nuclear periphery (Figure 4B and 4E). To test the hypothesis that the mutant protein may influence the function of wild-type protein, we co-transfected cells with SEPT12-del-EGFP and FLAG-SEPT12 expression vectors in different ratios, 1∶ 1, 1∶ 3 and 1∶7. Cells co-transfected with FLAG-SEPT12 and SEPT12-EGFP formed well polymerized filaments around the nuclear membrane (Figure 4C). However, SEPT12-del-EGFP disrupted the filament formation of FLAG-SEPT12 in a dose-dependent manner (Figure 4D and 4F). The finding suggests that truncated SEPT12 lacking the C-terminal may disrupt the polymerization (and filament formation) of the wild-type SEPT12.
Figure 4. Effects of truncated - SEPT12 on filament - like formation in NT2D1 cells.
Immuno-fluorescence assay (IFA) shows wild- SEPT12-EGFP (SEPT12-EGFP) (A.) or truncated- SEPT12-EGFP (SEPT12-del-EGFP) (B.) forms filament - like or dot- like structure, respectively. (A.–B.) Merged pictures for staining with anti-EGFP antibody (green) and DAPI (light blue). The results of co-expressed wild- SEPT12-EGFP (SEPT12-EGFP) (C.) or truncated- SEPT12-EGFP (SEPT12-del-EGFP) (D.) with wild- FLAG-SEPT12 (FLAG-SEPT12) in cells are presented in (C.) and (D.), respectively. Signals from EGFP protein (green), anti-FLAG antibody (red) and DAPI (Light blue) signals are merged in (C.) and (D.). (A.–D.) Arrows indicated filament-like structure; Arrow head indicated dot-like structure. Magnification: ×400 in A–D. (E.–F) Quantification of the percentage of filament- like structures in transfected cells. The height of the boxes represents the mean of value obtained from four independent experiments. At least 100 transfected cells were counted in each experiment (**: p<0.01, Student's t test). (F.) Dosage- dependent inhibition of filament-like formation by the truncated SEPT12 protein. Plasmids encoding FLAG-tagged wild-type SEPTIN12 were mixed with various amounts of plasmids encoding EGFP-tagged wild- or truncated SEPTIN12, then the mixtures were transfected into NT2D1 cells (**: p<0.01,*: p<0.05, Student's t test).
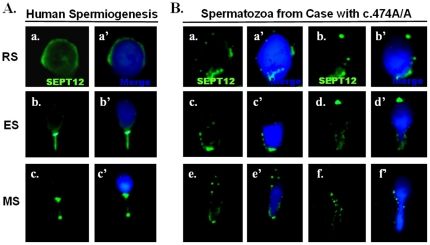
Disruption of SETP12 filament in spermatozoa of infertile men with c.474 A/A
To determine whether del-SEPT12 also affects terminal differentiation of male germ cells in humans, spermatozoa were isolated from the testis biopsies of fertile controls with c.474C/C and infertile men with c.474A/A. IFA showed that in fertile men, SEPT12 is present around the nuclear periphery of round spermatids, at the neck region of elongating spermatids, and at the neck region and annulus of mature spermatozoa (Figure 5A), a finding in accord with our previously report [33]. In germ cells isolated from infertile men who carried c.477A/A, SEPT12 showed a dot-like pattern in differential stages of haploid germ cells (Figure 5B). This finding is in accord with the expression pattern of SEPT12-del-EGFP in NT2D1 cells (Figure 4B and 4D).
Figure 5. Expression patterns of SEPT12 human male germ cells with the c.474G/G (wild) and c.474A/A genotypes.
(A.) Detection of SEPT12 signals during human spermiogenesis. (a.–a′): Round Spermatids (RS), (b.–b′) Elongating Spermatids (ES) and Mature Sperm (MS). Left: SEPT12 signal (green); Right: merge of SEPT12 (green) and DAPI (light blue) signals. (B.) Varied type of spermatozoa isolated from cases with the c.474A/A genotype. Left: SEPT12 signal (green); Right: merge of SEPT12 (green) and DAPI (light blue) signals (Magnification: ×1,000).
De-condensed sperm nucleus and increased DNA damage in infertile men with c.474 A/A
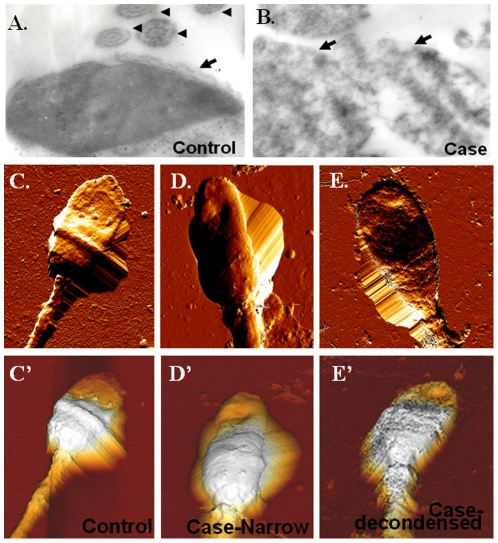
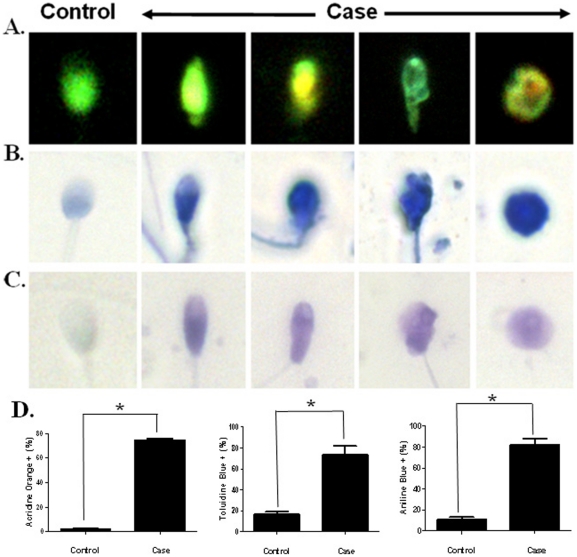
Increased sperm nuclear DNA damage has been observed in abnormal sperm of Septin12+/+/Septin12+/− chimeric mice [33]. In addition, oocytes couldn't develop beyond the morula stages after IVF or ICSI using sperm obtained from the Septin12+/+/Septin12+/− chimeric mice [33]. To evaluate sperm nuclear integrity of infertile men with c.474A/A, transmission electron microscopy (TEM) and atomic force microscopy (AFM) were used. Sperm from c474A/A patients had loose nuclear matrix as examined by TEM (Figure 6A and 6B) and narrow head/de-condensed nuclear matrix as observed under AFM (Figure 6 D and E). These two classical phenotypes have been described in a previous study using AFM to examine human sperm [40]. Further, we found high percentage of sperm with nuclear DNA damage by AO, TB and AB staining (AO: P<0.05; TB: P<0.05; AB: p<0.05; by Mann-Whitney test) (Figure 7 A–D). Taken together, we found SEPT12 dysfunction caused by c.474A/A may disrupt the nuclear integrity, a finding reminiscent of that observed in the Septin12+/+/Septin12+/− chimeric mice.
Figure 6. Spermatozoa from c.474A/A patients with abnormal head shape.
(A.–B.) TEM images of sperm isolated from a fertile control (A.) and an infertile mam with c.474A/A (B). The latter shows de-condensed chromatin. Arrows indicate the nucleus; arrow heads indicate the axonemal 9+2 structures (Magnification: ×10,000). (C.–E.) Top-view AFM images confirm abnormal morphology in sperm head. Sperm of a control subject (C.). Sperm of an infertile man with c.474A/A have a narrow head (D.) or a de-condensed nucleus (E.). Three-dimensional images are displayed in the bottom (C′.–E′.).
Figure 7. Nuclear DNA damage in the spermatozoa of infertile men who carried c.474A/A.
(A.–C.) The spermatozoa were stained with AO (A.), TB (B.) and AB (C.) dyes. (A.) The spermatozoa with normal (green) or abnormal nucleus (yellow). (B.–C.) Spermatozoa with normal (light blue) or abnormal (dark blue) nucleus. (Magnification: ×1,000). (D.) Quantification of the percentage of AO-, AB- or TB- stained spermatozoa. At least 100 spermatozoa cells were counted in each case (*: p<0.05; Mann-Whitney test).
Discussions
In this study, a SEPTIN12 genetic variant (c.474G→A) was found to be significantly associated with male infertility with distinctive sperm pathology. This variant induced alternative splicing by activating a novel splice donor site. The resultant truncated SEPT12 disturbs polymerization of the wild-type SEPT12 in cells. Sperm from cases with this variant were presented with high percentage of abnormal morphology (teratozoospermia) with significant nuclear DNA damage. Our findings indicated a genetic variant of SEPTIN12 is causally linked to male infertility with distinctive sperm pathology.
Truncated SEPT12 disrupts SEPT12-related complex in a dose-dependent manner
SEPT12 forms filament- like structure with SEPT4, SEPT6 or SEPT11 ex vivo [31], [38], [39]. Previous studies also indicated a mutation in the GTP- binding motif (Gly56) of SEPT12 resulted in large aggregates instated of filamentous structure [32], [39]. However, the components of SEPT12-related complex and how SEPT12 interacts with other SEPTs are not known. In this study, we found truncated SEPT12 disrupts the filamentous structure of wild- type SEPT12 in a dose dependent manner. The ratio of truncated SEPT12 to wild-SEPT12 ranged from 1∶ 1 to 1∶6 (Figure 4), a ratio used to mimic the relative abundance of the alternatively spliced form (1∶1.7). We speculate truncated SEPT12 perturbs self-assembly of wide-type SEPT12 or assembly of wild-type SEPT12 with other SEPTs (e.g. SEPT4, SEPT6 or SEPT11) or other structural proteins during the terminal differentiation of male germline [21], [32], [38], [39], [41]. It is intriguing that wide-type SEPT12 forms filamentous structure wrapping around the nuclear membrane (Figure 4 and 5), a finding consistent with a previous study using the Chinese hamster ovary (CHO) cell, a female germ line cell, co-transfected with SEPT12 and SEPT4 [31]. Moreover, SEPT12 signals were dis-located or disrupted around the sperm nucleus in patients' sperm. It has yet to be tested whether dysfunctional SEPT12 interferes with the integrity of the nuclear membrane.
Phenotypic variation of SNPs
Recently, Miyakawa et al., suggested SEPTIN12 as a good candidate gene for male infertility and chose cases with Sertoli- cell-only syndrome (SCOS) [42]. Their study enrolled 140 healthy men and 100 cases with SCOS. They identified eight SNPs (SNP1 to SNP8) in SEPTIN12. Among them, three synonymous variants (SNP3 or 210G>A, SNP4 or 225G>A, and SNP6 or 423G>C) were more prevalent in the SCOS patients, but their functional significance still remains to be explored. Two of the 8 SNPs were also found in our study. One is SNP5 or c.332C→A, pThr111Lys, but the frequency of c.332C→A did not show significant difference between infertile men and fertile controls in both studies. The other is SNP8 or c.474G→A. The frequency of this SNP did not show any significant difference between patients and controls in the previous study (10.7% vs. 12.0%) [42]. However, in our study, both allelic and genotypic frequencies of c.474A/A were significantly higher in infertile men with abnormal semen parameters (sperm number, motility or morphology). The difference may result from different ethnic backgrounds of enrollees or criteria of patients' selection. It is noteworthy that some fertile men were found to carry c.474A/A, suggesting c.474A/A as a predisposing factor of abnormal spermiogenesis. Indeed, a few infertile men who did not carry c.474G→A (A/A) variant were also presented with similar sperm morphological defects. For these cases, other genetic or environmental factors might be implicated [3], [43], [44], [45], [46], [47]. On the other hand, some fertile controls also carried the c.474G→A (A/A) variant, but the incidence was much lower than the study group. We speculate the c.474G→A (A/A) variant is non-penetrat, a phenomenon common to splicing mutations [48], [49]. Genetic variations of splicing process in human population have been shown to be far more complex than previously observed, and many factors may be accountable for the phenotypic expression of splicing mutations [50], [51], [52]. Incomplete penetrance is common to splicing mutations of many genes [53], [54], [55], [56], [57] and both cis- and trans-acting modifiers are involved [58], [59], [60]. For SEPT12, the relative abundance of truncated protein may be too low to perturb filament formation in the “non-penetrant” men. Unfortunately the amount of remaining semen samples was not sufficient for us to test this hypothesis.
SEPT and DNA damage
In our previous study, decreased SEPT12 expression level resulted in significant sperm DNA damage in the mouse [33]. In this study, a SNP of SEPTIN12 (c.474A/A) was causally linked to the disruption of sperm nuclear integrity and DNA damage. How decreased expression level of SEPT12 and dysfunctional SEPT12 cause nuclear DNA damage still remains to be explored. In yeast, all five septins, Cdc3p, Cdc10p, Cdc11p, Cdc12p, and Shs1p/Sep7p, in the SEPT complex interact with the FHA domain of Rad 53, an important DNA damage checkpoint kinase [61]. Shs1, one of these septins, appears to have an important role in the response to DNA replication stress [61]. In addition, Cdc3p also interacts with BUB2, which is important to maintain a mitotic arrest during kinetochore damage [62]. In mammalian cells, the SEPT 2/6/7 complexes regulate actin organization and are links to the DNA damage checkpoint by accumulation of adaptor protein, NCK, in the nucleus [63]. It deserves to be explored whether the SEPT/SCOS7/NCK pathway is well conserved between different species and different organ systems.
SEPTIN pathology
Loss of SEPT functions has been implicated in the pathogenesis of many diseases, including neurodegeneration, male infertility and different type of cancers [64]. SEPT1, 2 and 4 are associated with tau-based helical filaments and contribute to the formation of tangles in Alzheimer's disease [65]. Mutations in SEPTIN9 cause hereditary neuralgic amotrophy in some families [66]. SEPTIN2, 5, 6, 9 and 11 are involved in reciprocal translocations of myeloid/lymphoid or mixed-lineage leukemia (MLL) gene [67], [68], [69], [70], [71], [72]. SEPTIN9 was mapped to a region of loss of heterozygosity (LOH) at chromosome 17q25.3 in some cases of sporadic ovarian and breast cancer [73], [74], [75]. Loss of SEPT4 was observed in sperm of patients with asthenozoospermia [12], [13], [28], [29]. In this study, we identified a common SEPTIN12 variant that may confer susceptibility to defect of spermiogenesis. The characteristic human sperm pathology includes bent tail, abnormal head, immature spermatids, and significant nuclear DNA damage.
Materials and Methods
Human samples
The study was approved by the Institutional Review Board of National Cheng Kung University Hospital and Kuo General Hospital. From January 2005 to July 2007, infertile men with abnormal semen parameters were enrolled into the study. They underwent a comprehensive examination, including a detailed medical history, physical examination, hormone profiles and a molecular test for Y-chromosome micro-deletions, as described previously [76]. Patients with Y-chromosomal microdeletion have been excluded from the study. During the same period, we also recruited fertile men with normal semen parameters as control subjects. They were recruited from husbands of women who received regular prenatal care at the University Hospital. All of them had fathered at least 1 child within 2 years without assisted reproductive technologies. All study and control subjects were Han Taiwanese, the major ethnic group in Taiwan (making up more than 95% of the country's population).
Semen analysis
The ejaculate was obtained by masturbation after a minimum 48 h of sexual abstinence. The assessment of concentration was performed according to the World Health Organization's recommendations using a modified Neubauer chamber and displacement pipettes for proper dilution of the ejaculate [1]. Evaluation of sperm morphology is according to Kruger criteria (normal spermatozoa <14%) and the fourth edition of WHO guidelines for semen analysis [1], [77]. Peroxidase staining was used to detect granulocyte in semen samples and cases with significant leukocytospermia (leukocyte counts >10×105/mL) had been excluded from the study. Abnormal semen parameters included oligozoospermia (sperm count <20×106/mL), asthenozoospermia (percentage of motile sperm <50%), and teratozoospermia (percentage of sperm with normal morphology <14%). The infertile men were recruited if at least one of three major parameters (semen concentration, sperm morphology, and sperm motility) were abnormal.
PCR and Sequencing
Cases with abnormality in at least one of three major parameters (sperm concentration, motility, and morphology) were subjected to analysis of the SEPTIN12 gene. Genomic DNA was extracted from peripheral blood samples using a Gentra Puregene Blood Kit (Catalog #158389, QIAGEN, Hilden, Germany.). The entire coding region and exon–intron boundaries of SEPTIN12 (GenBank accession number NM_144605.3) were analyzed. PCR products were made and visible by using ethidium bromide, followed by sequencing analysis. The oligonucleotide primers are listed in Table S1.
Cloning, Mutagenesis, Transfection, and RT-PCR
Fragments containing exon 5, intron 5, and exon 6 of human SEPTIN12 were PCR amplified from human genomic DNAs and cloned into the pEGFP-N1-CMV2 vector. The constructs were confirmed by DNA sequencing. A SEPTIN12 variant with c.474G→A was prepared using QuickChange Site-directed Mutagenesis Kits (Stratagene, La Jolla, CA) [32]. After transfecting with the plasmids by Lipofectamine 2000 (Invitrogen, Carlsbad, CA), total RNA was extracted from the NTERA-2 d.D1 (NT2D1) cell line, followed by measuring total absorbance at 260 nm for quantification. The RT-PCR conditions and product detection were performed as described in our previous publication [78].
Separation of the testicular germ cell populations and sperm preparation
Separation of spermatogenic cells was carried out by a centrifugal system based on the density of different types of germ cells, as described previously [79]. After de-capsulation and enzyme digestion of testis biopsies from the case treated with testicular sperm extraction (TESE), germ cell suspensions were filtered through 35 µM nylon filters (Falcon; Becton Dickinson, Franklin Lakes, NJ, USA), followed by centrifugation using a Kubota centrifuge 2010. Germ cells at different developmental stages were collected. Mature spermatozoa were collected from the semen of men with spermatogenic cases and controls. Finally, suspensions were centrifuged with maximal force (2580×g, Kubota 2010) for 10 min, spread on a slide, and air-dried. The slides were then subjected to immuno-fluorescence assay (IFA).
Immuno-fluorescence assay (IFA)
The protocol of IFA has been described previously [32]. The slide was treated with 0.1% Triton X-100, washed twice with Tris-buffered-saline (TBS), followed by incubation with the anti-SEPT12 antibody (H00124404-B01, Abnova; Taipei, Taiwan) or anti-FLAG antibody (F1804, Sigma, MI, USA) for 60 minutes at room temperature. Following the washing steps with TBS, sections was incubated with goat anti- mouse Alexa Flou 488 or goat anti- mouse Alexa Flou 568 (Invitrogen) for 60 min at room temperature and washed with TBS. Mito-tracker -conjugated with Alexa Fluor 568 (10 mg/ml) (Invitrogen) was used to locate the mid-piece in spermatozoa. 4,6-diamidino-2-phenylindole (DAPI) was used for nuclear staining.
Motile sperm organelle morphology examination (MSOME) Transmission electron microscopy (TEM) and Atomic force microscopy (AFM)
For bight-field examination, the sperm cells were observed under a high-magnification inverted microscope (Eclipse TE 2000 U; Nikon, Japan) equipped with differential interference contrast microscope (DIC/Nomarski) as described previously [80]. Morphological evaluation was accomplished on a monitor screen and the total calculated magnification was ×8400. Other sperms were air dried on slides after being washed with 1 X phosphate buffered saline (PBS). For TEM studies, spermatozoa were washed in 0.1 M phosphate buffer (pH 7.2), fixed, and further processed according to the protocol described in our previously study [33]. The final sections were counter-stained with lead citrate and uranyl acetate and subjected to observation with a JOEL 1200 TEM (JOEL Institute Inc., Lexington, MA, USA). The AFM examination was performed according to the protocol described previously [40].
Sperm nuclear DNA damage assays using Acridine orange (AO), Toluidine blue (TB) and Aniline blue (AB) staining
Three assays were used to detect sperm nuclear integrity. The assays included AO, TB and AB staining described in the previous publication [33]. At least 100 spermatozoa were counted for each case per assay.
Supporting Information
List of human SEPTIN12 primers for sequencing analysis.
(DOC)
Acknowledgments
We deeply appreciated Dr. Pauline Yen (Institute Biomedical Sciences, Academia Sinica) for criticism of the manuscript.
Footnotes
Competing Interests: The authors have declared that no competing interests exist.
Funding: No current external funding sources for this study.
References
- 1.WHO. 1998. WHO Laboratory Manual for the Examination of Human Semen and Sperm-Cervical Mucus Interaction.
- 2.Matzuk MM, Lamb DJ. Genetic dissection of mammalian fertility pathways. Nat Cell Biol. 2002;4(Suppl):s41–49. doi: 10.1038/ncb-nm-fertilityS41. [DOI] [PubMed] [Google Scholar]
- 3.Matzuk MM, Lamb DJ. The biology of infertility: research advances and clinical challenges. Nat Med. 2008;14:1197–1213. doi: 10.1038/nm.f.1895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Palermo G, Joris H, Devroey P, Van Steirteghem AC. Pregnancies after intracytoplasmic injection of single spermatozoon into an oocyte. Lancet. 1992;340:17–18. doi: 10.1016/0140-6736(92)92425-f. [DOI] [PubMed] [Google Scholar]
- 5.Javed M, Esfandiari N, Casper RF. Failed fertilization after clinical intracytoplasmic sperm injection. Reprod Biomed Online. 2010;20:56–67. doi: 10.1016/j.rbmo.2009.10.010. [DOI] [PubMed] [Google Scholar]
- 6.Hall PA, Jung K, Hillan KJ, Russell SE. Expression profiling the human septin gene family. J Pathol. 2005;206:269–278. doi: 10.1002/path.1789. [DOI] [PubMed] [Google Scholar]
- 7.Peterson EA, Petty EM. Conquering the complex world of human septins: implications for health and disease. Clin Genet. 2010;77:511–524. doi: 10.1111/j.1399-0004.2010.01392.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hartwell LH. Genetic control of the cell division cycle in yeast. IV. Genes controlling bud emergence and cytokinesis. Exp Cell Res. 1971;69:265–276. doi: 10.1016/0014-4827(71)90223-0. [DOI] [PubMed] [Google Scholar]
- 9.Gladfelter AS, Pringle JR, Lew DJ. The septin cortex at the yeast mother-bud neck. Curr Opin Microbiol. 2001;4:681–689. doi: 10.1016/s1369-5274(01)00269-7. [DOI] [PubMed] [Google Scholar]
- 10.Peterson EA, Kalikin LM, Steels JD, Estey MP, Trimble WS, et al. Characterization of a SEPT9 interacting protein, SEPT14, a novel testis-specific septin. Mamm Genome. 2007;18:796–807. doi: 10.1007/s00335-007-9065-x. [DOI] [PubMed] [Google Scholar]
- 11.Kartmann B, Roth D. Novel roles for mammalian septins: from vesicle trafficking to oncogenesis. J Cell Sci. 2001;114:839–844. doi: 10.1242/jcs.114.5.839. [DOI] [PubMed] [Google Scholar]
- 12.Ihara M, Kinoshita A, Yamada S, Tanaka H, Tanigaki A, et al. Cortical organization by the septin cytoskeleton is essential for structural and mechanical integrity of mammalian spermatozoa. Dev Cell. 2005;8:343–352. doi: 10.1016/j.devcel.2004.12.005. [DOI] [PubMed] [Google Scholar]
- 13.Kissel H, Georgescu MM, Larisch S, Manova K, Hunnicutt GR, et al. The Sept4 septin locus is required for sperm terminal differentiation in mice. Dev Cell. 2005;8:353–364. doi: 10.1016/j.devcel.2005.01.021. [DOI] [PubMed] [Google Scholar]
- 14.Xue J, Tsang CW, Gai WP, Malladi CS, Trimble WS, et al. Septin 3 (G-septin) is a developmentally regulated phosphoprotein enriched in presynaptic nerve terminals. J Neurochem. 2004;91:579–590. doi: 10.1111/j.1471-4159.2004.02755.x. [DOI] [PubMed] [Google Scholar]
- 15.Son JH, Kawamata H, Yoo MS, Kim DJ, Lee YK, et al. Neurotoxicity and behavioral deficits associated with Septin 5 accumulation in dopaminergic neurons. J Neurochem. 2005;94:1040–1053. doi: 10.1111/j.1471-4159.2005.03257.x. [DOI] [PubMed] [Google Scholar]
- 16.Dent J, Kato K, Peng XR, Martinez C, Cattaneo M, et al. A prototypic platelet septin and its participation in secretion. Proc Natl Acad Sci U S A. 2002;99:3064–3069. doi: 10.1073/pnas.052715199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tsang CW, Fedchyshyn M, Harrison J, Xie H, Xue J, et al. Superfluous role of mammalian septins 3 and 5 in neuronal development and synaptic transmission. Mol Cell Biol. 2008;28:7012–7029. doi: 10.1128/MCB.00035-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Spiliotis ET, Kinoshita M, Nelson WJ. A mitotic septin scaffold required for Mammalian chromosome congression and segregation. Science. 2005;307:1781–1785. doi: 10.1126/science.1106823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhu M, Wang F, Yan F, Yao PY, Du J, et al. Septin 7 interacts with centromere-associated protein E and is required for its kinetochore localization. J Biol Chem. 2008;283:18916–18925. doi: 10.1074/jbc.M710591200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kinoshita M, Kumar S, Mizoguchi A, Ide C, Kinoshita A, et al. Nedd5, a mammalian septin, is a novel cytoskeletal component interacting with actin-based structures. Genes Dev. 1997;11:1535–1547. doi: 10.1101/gad.11.12.1535. [DOI] [PubMed] [Google Scholar]
- 21.Surka MC, Tsang CW, Trimble WS. The mammalian septin MSF localizes with microtubules and is required for completion of cytokinesis. Mol Biol Cell. 2002;13:3532–3545. doi: 10.1091/mbc.E02-01-0042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nagata K, Kawajiri A, Matsui S, Takagishi M, Shiromizu T, et al. Filament formation of MSF-A, a mammalian septin, in human mammary epithelial cells depends on interactions with microtubules. J Biol Chem. 2003;278:18538–18543. doi: 10.1074/jbc.M205246200. [DOI] [PubMed] [Google Scholar]
- 23.Estey MP, Di Ciano-Oliveira C, Froese CD, Bejide MT, Trimble WS. Distinct roles of septins in cytokinesis: SEPT9 mediates midbody abscission. J Cell Biol. 2010;191:741–749. doi: 10.1083/jcb.201006031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ono R, Ihara M, Nakajima H, Ozaki K, Kataoka-Fujiwara Y, et al. Disruption of Sept6, a fusion partner gene of MLL, does not affect ontogeny, leukemogenesis induced by MLL-SEPT6, or phenotype induced by the loss of Sept4. Mol Cell Biol. 2005;25:10965–10978. doi: 10.1128/MCB.25.24.10965-10978.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hime GR, Brill JA, Fuller MT. Assembly of ring canals in the male germ line from structural components of the contractile ring. J Cell Sci. 1996;109(Pt 12):2779–2788. doi: 10.1242/jcs.109.12.2779. [DOI] [PubMed] [Google Scholar]
- 26.Greenbaum MP, Ma L, Matzuk MM. Conversion of midbodies into germ cell intercellular bridges. Dev Biol. 2007;305:389–396. doi: 10.1016/j.ydbio.2007.02.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Greenbaum MP, Yan W, Wu MH, Lin YN, Agno JE, et al. TEX14 is essential for intercellular bridges and fertility in male mice. Proc Natl Acad Sci U S A. 2006;103:4982–4987. doi: 10.1073/pnas.0505123103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sugino Y, Ichioka K, Soda T, Ihara M, Kinoshita M, et al. Septins as diagnostic markers for a subset of human asthenozoospermia. J Urol. 2008;180:2706–2709. doi: 10.1016/j.juro.2008.08.005. [DOI] [PubMed] [Google Scholar]
- 29.Lhuillier P, Rode B, Escalier D, Lores P, Dirami T, et al. Absence of annulus in human asthenozoospermia: case report. Hum Reprod. 2009;24:1296–1303. doi: 10.1093/humrep/dep020. [DOI] [PubMed] [Google Scholar]
- 30.Lin YH, Lin YM, Teng YN, Hsieh TY, Lin YS, et al. Identification of ten novel genes involved in human spermatogenesis by microarray analysis of testicular tissue. Fertil Steril. 2006;86:1650–1658. doi: 10.1016/j.fertnstert.2006.04.039. [DOI] [PubMed] [Google Scholar]
- 31.Steels JD, Estey MP, Froese CD, Reynaud D, Pace-Asciak C, et al. Sept12 is a component of the mammalian sperm tail annulus. Cell Motil Cytoskeleton. 2007;64:794–807. doi: 10.1002/cm.20224. [DOI] [PubMed] [Google Scholar]
- 32.Lin YH, Lin YM, Wang YY, Yu IS, Lin YW, et al. The expression level of septin12 is critical for spermiogenesis. Am J Pathol. 2009;174:1857–1868. doi: 10.2353/ajpath.2009.080955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lin YH, Chou CK, Hung YC, Yu IS, Pan HA, et al. SEPT12 deficiency causes sperm nucleus damage and developmental arrest of preimplantation embryos. Fertil Steril. 2011;95:363–365. doi: 10.1016/j.fertnstert.2010.07.1064. [DOI] [PubMed] [Google Scholar]
- 34.Kinoshita M, Field CM, Coughlin ML, Straight AF, Mitchison TJ. Self- and actin-templated assembly of Mammalian septins. Dev Cell. 2002;3:791–802. doi: 10.1016/s1534-5807(02)00366-0. [DOI] [PubMed] [Google Scholar]
- 35.Nagata K, Asano T, Nozawa Y, Inagaki M. Biochemical and cell biological analyses of a mammalian septin complex, Sept7/9b/11. J Biol Chem. 2004;279:55895–55904. doi: 10.1074/jbc.M406153200. [DOI] [PubMed] [Google Scholar]
- 36.Martinez C, Sanjuan MA, Dent JA, Karlsson L, Ware J. Human septin-septin interactions as a prerequisite for targeting septin complexes in the cytosol. Biochem J. 2004;382:783–791. doi: 10.1042/BJ20040372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kremer BE, Haystead T, Macara IG. Mammalian septins regulate microtubule stability through interaction with the microtubule-binding protein MAP4. Mol Biol Cell. 2005;16:4648–4659. doi: 10.1091/mbc.E05-03-0267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ding X, Yu W, Liu M, Shen S, Chen F, et al. SEPT12 interacts with SEPT6 and this interaction alters the filament structure of SEPT6 in Hela cells. J Biochem Mol Biol. 2007;40:973–978. doi: 10.5483/bmbrep.2007.40.6.973. [DOI] [PubMed] [Google Scholar]
- 39.Ding X, Yu W, Liu M, Shen S, Chen F, et al. GTP Binding Is Required for SEPT12 to Form Filaments and to Interact with SEPT11. Mol Cells. 2008;25:385–389. [PubMed] [Google Scholar]
- 40.Lee JDt, Allen MJ, Balhorn R. Atomic force microscope analysis of chromatin volumes in human sperm with head-shape abnormalities. Biol Reprod. 1997;56:42–49. doi: 10.1095/biolreprod56.1.42. [DOI] [PubMed] [Google Scholar]
- 41.Joo E, Surka MC, Trimble WS. Mammalian SEPT2 is required for scaffolding nonmuscle myosin II and its kinases. Dev Cell. 2007;13:677–690. doi: 10.1016/j.devcel.2007.09.001. [DOI] [PubMed] [Google Scholar]
- 42.Miyakawa H, Miyamoto T, Koh E, Tsujimura A, Miyagawa Y, et al. Single-Nucleotide Polymorphisms in the SEPTIN12 Gene May Be a Genetic Risk Factor for Japanese Patients with Sertoli Cell-Only Syndrome. J Androl. 2011 doi: 10.2164/jandrol.110.012146. [DOI] [PubMed] [Google Scholar]
- 43.Yan W. Male infertility caused by spermiogenic defects: lessons from gene knockouts. Mol Cell Endocrinol. 2009;306:24–32. doi: 10.1016/j.mce.2009.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Auger J, Eustache F, Andersen AG, Irvine DS, Jorgensen N, et al. Sperm morphological defects related to environment, lifestyle and medical history of 1001 male partners of pregnant women from four European cities. Hum Reprod. 2001;16:2710–2717. doi: 10.1093/humrep/16.12.2710. [DOI] [PubMed] [Google Scholar]
- 45.Baccetti B, Collodel G, Estenoz M, Manca D, Moretti E, et al. Gene deletions in an infertile man with sperm fibrous sheath dysplasia. Hum Reprod. 2005;20:2790–2794. doi: 10.1093/humrep/dei126. [DOI] [PubMed] [Google Scholar]
- 46.Yeung CH, Tuttelmann F, Bergmann M, Nordhoff V, Vorona E, et al. Coiled sperm from infertile patients: characteristics, associated factors and biological implication. Hum Reprod. 2009;24:1288–1295. doi: 10.1093/humrep/dep017. [DOI] [PubMed] [Google Scholar]
- 47.Tarnasky H, Cheng M, Ou Y, Thundathil JC, Oko R, et al. Gene trap mutation of murine outer dense fiber protein-2 gene can result in sperm tail abnormalities in mice with high percentage chimaerism. BMC Dev Biol. 2010;10:67. doi: 10.1186/1471-213X-10-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bonnet C, Krieger S, Vezain M, Rousselin A, Tournier I, et al. Screening BRCA1 and BRCA2 unclassified variants for splicing mutations using reverse transcription PCR on patient RNA and an ex vivo assay based on a splicing reporter minigene. J Med Genet. 2008;45:438–446. doi: 10.1136/jmg.2007.056895. [DOI] [PubMed] [Google Scholar]
- 49.Quaye L, Tyrer J, Ramus SJ, Song H, Wozniak E, et al. Association between common germline genetic variation in 94 candidate genes or regions and risks of invasive epithelial ovarian cancer. PLoS One. 2009;4:e5983. doi: 10.1371/journal.pone.0005983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Graveley BR. The haplo-spliceo-transcriptome: common variations in alternative splicing in the human population. Trends Genet. 2008;24:5–7. doi: 10.1016/j.tig.2007.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kwan T, Benovoy D, Dias C, Gurd S, Provencher C, et al. Genome-wide analysis of transcript isoform variation in humans. Nat Genet. 2008;40:225–231. doi: 10.1038/ng.2007.57. [DOI] [PubMed] [Google Scholar]
- 52.de Souza JE, Ramalho RF, Galante PA, Meyer D, de Souza SJ. Alternative splicing and genetic diversity: silencers are more frequently modified by SNVs associated with alternative exon/intron borders. Nucleic Acids Res. 2011 doi: 10.1093/nar/gkr081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Rave-Harel N, Kerem E, Nissim-Rafinia M, Madjar I, Goshen R, et al. The molecular basis of partial penetrance of splicing mutations in cystic fibrosis. Am J Hum Genet. 1997;60:87–94. [PMC free article] [PubMed] [Google Scholar]
- 54.Moolman JA, Reith S, Uhl K, Bailey S, Gautel M, et al. A newly created splice donor site in exon 25 of the MyBP-C gene is responsible for inherited hypertrophic cardiomyopathy with incomplete disease penetrance. Circulation. 2000;101:1396–1402. doi: 10.1161/01.cir.101.12.1396. [DOI] [PubMed] [Google Scholar]
- 55.Liu HX, Cartegni L, Zhang MQ, Krainer AR. A mechanism for exon skipping caused by nonsense or missense mutations in BRCA1 and other genes. Nat Genet. 2001;27:55–58. doi: 10.1038/83762. [DOI] [PubMed] [Google Scholar]
- 56.Basel-Vanagaite L, Pelet A, Steiner Z, Munnich A, Rozenbach Y, et al. Allele dosage-dependent penetrance of RET proto-oncogene in an Israeli-Arab inbred family segregating Hirschsprung disease. Eur J Hum Genet. 2007;15:242–245. doi: 10.1038/sj.ejhg.5201733. [DOI] [PubMed] [Google Scholar]
- 57.Rio Frio T, McGee TL, Wade NM, Iseli C, Beckmann JS, et al. A single-base substitution within an intronic repetitive element causes dominant retinitis pigmentosa with reduced penetrance. Hum Mutat. 2009;30:1340–1347. doi: 10.1002/humu.21071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Nissim-Rafinia M, Kerem B. Splicing regulation as a potential genetic modifier. Trends Genet. 2002;18:123–127. doi: 10.1016/s0168-9525(01)02619-1. [DOI] [PubMed] [Google Scholar]
- 59.Buratti E, Brindisi A, Pagani F, Baralle FE. Nuclear factor TDP-43 binds to the polymorphic TG repeats in CFTR intron 8 and causes skipping of exon 9: a functional link with disease penetrance. Am J Hum Genet. 2004;74:1322–1325. doi: 10.1086/420978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Rio Frio T, Civic N, Ransijn A, Beckmann JS, Rivolta C. Two trans-acting eQTLs modulate the penetrance of PRPF31 mutations. Hum Mol Genet. 2008;17:3154–3165. doi: 10.1093/hmg/ddn212. [DOI] [PubMed] [Google Scholar]
- 61.Smolka MB, Chen SH, Maddox PS, Enserink JM, Albuquerque CP, et al. An FHA domain-mediated protein interaction network of Rad53 reveals its role in polarized cell growth. J Cell Biol. 2006;175:743–753. doi: 10.1083/jcb.200605081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Krishnan R, Pangilinan F, Lee C, Spencer F. Saccharomyces cerevisiae BUB2 prevents mitotic exit in response to both spindle and kinetochore damage. Genetics. 2000;156:489–500. doi: 10.1093/genetics/156.2.489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Kremer BE, Adang LA, Macara IG. Septins regulate actin organization and cell-cycle arrest through nuclear accumulation of NCK mediated by SOCS7. Cell. 2007;130:837–850. doi: 10.1016/j.cell.2007.06.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Hall PA, Russell SE. The pathobiology of the septin gene family. J Pathol. 2004;204:489–505. doi: 10.1002/path.1654. [DOI] [PubMed] [Google Scholar]
- 65.Kinoshita A, Kinoshita M, Akiyama H, Tomimoto H, Akiguchi I, et al. Identification of septins in neurofibrillary tangles in Alzheimer's disease. Am J Pathol. 1998;153:1551–1560. doi: 10.1016/S0002-9440(10)65743-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Kuhlenbaumer G, Hannibal MC, Nelis E, Schirmacher A, Verpoorten N, et al. Mutations in SEPT9 cause hereditary neuralgic amyotrophy. Nat Genet. 2005;37:1044–1046. doi: 10.1038/ng1649. [DOI] [PubMed] [Google Scholar]
- 67.Megonigal MD, Rappaport EF, Jones DH, Williams TM, Lovett BD, et al. t(11;22)(q23;q11.2) In acute myeloid leukemia of infant twins fuses MLL with hCDCrel, a cell division cycle gene in the genomic region of deletion in DiGeorge and velocardiofacial syndromes. Proc Natl Acad Sci U S A. 1998;95:6413–6418. doi: 10.1073/pnas.95.11.6413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Borkhardt A, Teigler-Schlegel A, Fuchs U, Keller C, Konig M, et al. An ins(X;11)(q24;q23) fuses the MLL and the Septin 6/KIAA0128 gene in an infant with AML-M2. Genes Chromosomes Cancer. 2001;32:82–88. doi: 10.1002/gcc.1169. [DOI] [PubMed] [Google Scholar]
- 69.Ono R, Taki T, Taketani T, Kawaguchi H, Taniwaki M, et al. SEPTIN6, a human homologue to mouse Septin6, is fused to MLL in infant acute myeloid leukemia with complex chromosomal abnormalities involving 11q23 and Xq24. Cancer Res. 2002;62:333–337. [PubMed] [Google Scholar]
- 70.Osaka M, Rowley JD, Zeleznik-Le NJ. MSF (MLL septin-like fusion), a fusion partner gene of MLL, in a therapy-related acute myeloid leukemia with a t(11;17)(q23;q25). Proc Natl Acad Sci U S A. 1999;96:6428–6433. doi: 10.1073/pnas.96.11.6428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Kojima K, Sakai I, Hasegawa A, Niiya H, Azuma T, et al. FLJ10849, a septin family gene, fuses MLL in a novel leukemia cell line CNLBC1 derived from chronic neutrophilic leukemia in transformation with t(4;11)(q21;q23). Leukemia. 2004;18:998–1005. doi: 10.1038/sj.leu.2403334. [DOI] [PubMed] [Google Scholar]
- 72.Cerveira N, Correia C, Bizarro S, Pinto C, Lisboa S, et al. SEPT2 is a new fusion partner of MLL in acute myeloid leukemia with t(2;11)(q37;q23). Oncogene. 2006;25:6147–6152. doi: 10.1038/sj.onc.1209626. [DOI] [PubMed] [Google Scholar]
- 73.Russell SE, McIlhatton MA, Burrows JF, Donaghy PG, Chanduloy S, et al. Isolation and mapping of a human septin gene to a region on chromosome 17q, commonly deleted in sporadic epithelial ovarian tumors. Cancer Res. 2000;60:4729–4734. [PubMed] [Google Scholar]
- 74.Burrows JF, Chanduloy S, McIlhatton MA, Nagar H, Yeates K, et al. Altered expression of the septin gene, SEPT9, in ovarian neoplasia. J Pathol. 2003;201:581–588. doi: 10.1002/path.1484. [DOI] [PubMed] [Google Scholar]
- 75.Gonzalez ME, Peterson EA, Privette LM, Loffreda-Wren JL, Kalikin LM, et al. High SEPT9_v1 expression in human breast cancer cells is associated with oncogenic phenotypes. Cancer Res. 2007;67:8554–8564. doi: 10.1158/0008-5472.CAN-07-1474. [DOI] [PubMed] [Google Scholar]
- 76.Teng YN, Lin YH, Tsai YC, Hsu CC, Kuo PL, et al. A simplified gene-specific screen for Y chromosome deletions in infertile men. Fertil Steril. 2007;87:1291–1300. doi: 10.1016/j.fertnstert.2006.11.050. [DOI] [PubMed] [Google Scholar]
- 77.Kruger TF, Menkveld R, Stander FS, Lombard CJ, Van der Merwe JP, et al. Sperm morphologic features as a prognostic factor in in vitro fertilization. Fertil Steril. 1986;46:1118–1123. doi: 10.1016/s0015-0282(16)49891-2. [DOI] [PubMed] [Google Scholar]
- 78.Lin YH, Lin YM, Kuo YC, Wang YY, Kuo PL. Identification and characterization of a novel Rab GTPase-activating protein in spermatids. Int J Androl. 2010 doi: 10.1111/j.1365-2605.2010.01126.x. [DOI] [PubMed] [Google Scholar]
- 79.Yeh YC, Yang VC, Huang SC, Lo NW. Stage-dependent expression of extra-embryonic tissue-spermatogenesis-homeobox gene 1 (ESX1) protein, a candidate marker for X chromosome-bearing sperm. Reprod Fertil Dev. 2005;17:447–455. doi: 10.1071/rd04077. [DOI] [PubMed] [Google Scholar]
- 80.Oliveira JB, Massaro FC, Mauri AL, Petersen CG, Nicoletti AP, et al. Motile sperm organelle morphology examination is stricter than Tygerberg criteria. Reprod Biomed Online. 2009;18:320–326. doi: 10.1016/s1472-6483(10)60088-0. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
List of human SEPTIN12 primers for sequencing analysis.
(DOC)