Abstract
Objective:
Despite frequent theorizing, prior literature on the association between depressive symptoms and alcohol use in adolescence has been inconsistent. Yet studies have varied widely with respect to age at assessments, time frame of prediction, and controls for comorbid conditions and demographic factors. The current study examined whether the associations between depressive symptoms and alcohol use were similar in valence and magnitude over a 4-year period in early adolescence.
Method:
A sample of 521 young adolescents and their parents were interviewed every year from sixth (Mage = 12.0 years) through ninth grades. At each interview, symptom counts on depressive and conduct disorders were generated from the Diagnostic Interview Schedule for Children. Adolescents also reported on their alcohol use, which was converted to a binary variable. Autoregressive, cross-lagged panel models specifying depressive and conduct disorder symptoms as predictors of alcohol use 1 year later with equality constraints were tested and compared with models allowing path coefficients to vary over time.
Results:
For youth self-report, depressive symptoms were positively associated with alcohol use 1 year later over and above conduct problems and earlier alcohol use throughout early adolescence. By parental report, only very early adolescent depressive symptoms (sixth to seventh grades) were associated with alcohol use. Gender did not moderate findings for analyses with self- or parental-report data.
Conclusions:
These results indicate that, even in the context of conduct disorder symptoms, depressive symptoms are important indicators of risk for use of alcohol across early adolescence.
Adolescence is a crucial period for the development of alcohol use because it represents the time during which the majority of individuals initiate use (Johnston et al., 2001). The age at which an adolescent initiates alcohol use has been found to be a robust predictor of later problems, with early initiation (<14 years of age) being associated with heavier use throughout adolescence and emerging adulthood, more serious long-term substance use problems, and adult substance dependence (DeWit et al., 2000; King and Chassin, 2007; Maggs and Schulenberg, 2006; Sung et al., 2004). Furthermore, prior research has suggested that the developmental trajectory toward adolescent alcohol use disorders most frequently begins with the emergence of childhood mental disorders (Clark, 2004), with conduct and depressive disorders in particular often co-occurring with or preceding substance use (Armstrong and Costello, 2002; Kandel et al., 1999; Wu et al., 2008). Conduct problems and depression may carry different etiological importance in the development of substance use and problem use, but research on the role of depression in early alcohol use remains relatively sparse (Costello, 2007; Hussong et al., 2011).
A negative affect pathway, in which adolescents turn to alcohol or other drugs to alleviate psychological distress, has been frequently hypothesized in theoretical models explaining depression as a risk factor for alcohol use (Hussong et al., 2011; Zucker, 1994), although support has been inconsistent. Using cross-sectional data, Rohde and colleagues (1996) reported a depression prevalence of 47.9% among high school students with alcohol abuse or dependence compared with about 20% in abstainers, experimenters, or social drinkers. Furthermore, early depressive symptomatology increased risk of initiation of alcohol use in adolescence, with major depressive disorder doubling the odds of first-time use of alcohol by age 14 (King et al., 2004). Cognitive biases typically associated with depression (e.g., negative thinking patterns) are also predictive of early drinking onset (Corte and Zucker, 2008). However, other studies have not found adolescent depressive symptoms to be associated with later alcohol problems or to have actually suggested inverse associations (Hussong et al., 1998; Mason et al., 2008).
Our review of longitudinal studies examining the association between depressive symptoms in childhood or adolescence and later alcohol use or problems has identified several factors that may explain these mixed results (McCarty et al., 2011b). First, a large proportion of these studies (14 of 42 studies in our review; 33%) have examined depression as a static variable, using only a single time point in assessing depression. Doing so likely underestimates associations because depression is an episodic phenomenon that typically waxes and wanes over time. Moreover, the relation between depression and early alcohol use may change over the course of adolescent development as the nature and features, such as severity and persistence, of each corresponding disorder emerge. A dramatic increase in prevalence of both disorders occurs in adolescence yet with different normative time courses (Hankin et al., 1998; Washington State Department of Health, 2008).
A second limitation of many of the prior studies is that they did not examine depression in the context of conduct problems (18 of 38; 47%), although the two are highly co-morbid (Angold et al., 1999; Verhulst et al., 1993). There is a strong and robust literature documenting the prospective association between youth conduct problems and alcohol consumption (Costello et al., 1999; Fergusson et al., 2007; King and Chassin, 2008; King et al., 2004; Loeber et al., 1999; Mason and Windle, 2002). Conduct problems in both middle childhood and adolescence are associated with increased risks for longer term alcohol use, abuse, and dependence (Fergusson et al., 2007). Childhood disruptive behavior disorders and later alcohol use disorders appear to have a common diathesis (Cadoret et al., 1995), with deviant behavior playing a central role in theoretical models of alcoholism. Thus, it may be that positive findings may result from conduct disorder that is comorbid with depression, rather than from depression itself. In short, it is essential to examine depressive symptoms in the context of conduct problems, which may account for some of the shared variance between depressive symptoms and alcohol use.
A third limitation is that most of the research in this area has measured this association using self-report of both depression (32 of 42; 76% of the longitudinal studies included in the review) and substance use. It is important to understand the extent to which observed associations are independent of reporting or measurement bias. Youth may be able to give more nuanced reports of their internal states than parents (Braaten et al., 2001). Among those studies including another informant for the assessment of depressive symptoms, most have not observed associations between depressive symptoms and substance use (Hussong et al., 1998; Ingoldsby et al., 2006; King et al., 2004; Mason et al., 2008; Rao et al., 1999). Most commonly, these studies have examined parental report in addition to youth report and have variously examined parental and youth reports separately (Hussong et al., 1998; Maggs et al., 2008), combined both into a latent or composite variable (Ingoldsby et al., 2006; Mason et al., 2008), or used diagnostic “or” algorithms (King et al., 2004; Rao et al., 1999). To control for the bias in the data, the current study examined youth and parental reports separately to test the robustness of associations across informants.
Finally, prior studies have found differential associations between depression and alcohol use for boys and girls (Crum et al., 2008; Fleming et al., 2008; Marmorstein, 2009; Mason et al., 2007; Needham, 2007). Whereas some studies have found that higher levels of early depressed mood were associated with increased risk of use among boys but not girls (Crum et al., 2008; Tapert et al., 2003), others have found a stronger association for girls (Fleming et al., 2008; Marmorstein, 2009; Mason et al., 2007). Moreover, a striking gender difference in the epidemiology of depression only becomes apparent at or after age 13 (Angold et al., 1998; Hankin et al., 1998; McGee et al., 1992; Velez et al., 1989), which could result in a differential magnification or attenuation of risk for alcohol use by gender depending on developmental stage.
The current study was designed to explicate the associations between depressive symptoms and alcohol use in early adolescence while addressing methodological issues not adequately accounted for in prior research. This study had four important objectives. Our first objective was to examine whether there were specific developmental periods when depressive symptoms and conduct problems were particularly salient to the onset or course of alcohol use and problems, or whether associations were consistent across the course of early adolescent development. We hypothesized that stronger positive associations would be found between depression and substance use at younger ages. Second, we examined the effects in the context of conduct disorder symptoms to determine to what extent depressive symptoms are associated with increased risk above and beyond the effects of co-occurring conduct problems. We expected that depressive symptoms would predict alcohol use in early adolescence even when accounting for conduct disorder symptoms. Third, we examined whether youth-reported depressive symptoms would yield differential prediction of alcohol use compared with parent-reported depressive symptoms, with the hypothesis that more robust associations would be found for youth report. Fourth, in the absence of hypotheses, we tested for gender differences in the magnitude of associations on an exploratory basis.
Method
Sample
The Developmental Pathways Project (DPP) is a community-based prospective cohort study designed to examine the antecedents, phenomenology, and outcomes of depression and conduct problems in early adolescence. DPP participants were recruited from four Seattle-area public schools representative of the Seattle public middle school population. These schools are located in four distinct geographic and demographic areas within the city and together have a racial/ethnic distribution that is nearly identical to the total enrolled student population of the school district. Universal emotional health screening was carried out with sixth-grade students at these schools in 4 consecutive years (2001–2004); details of the screening procedure have been described elsewhere (Vander Stoep et al., 2005).
Students eligible for screening included sixth-graders who had a third-grade reading comprehension level or higher. Of the 2,920 eligible students, 2,187 (74.9%) were screened. Each year following screening, a random sample of students—stratified by their scores on the Mood and Feelings Questionnaire for depression (Angold and Costello, 1987) and the Youth Self-Report externalizing scale for conduct problems (Achenbach, 2001)—were identified for participation in the longitudinal study. Students were first assigned to one of four groups based on their screening results: high depression and conduct problem score (comorbid; CM) high depression and low conduct problem score (DP), low depression and high conduct problem score (CD), and low depression and low conduct problem score (neither [NE]). These groups were formed using a cutoff of 0.5 SD above the screening sample mean for the Mood and Feelings Questionnaire and the Youth Self-Report externalizing scales. This distribution-based group assignment has been used in prior studies (Capaldi, 1992; Ingoldsby et al., 2006; Miller-Johnson et al., 1998). Students who had been screened, who had at least one parent who could speak English, and who were still residing in the district were eligible for recruitment into the longitudinal study. A stratified random sample of 807 students was selected for longitudinal follow-up, with students scoring high on depressive and/or conduct problem scores oversampled according to a ratio of 1:1:1:2 from the four psychopathology screening groups (CM, DP, CD, and NE). Because in the general school population the ratio is approximately 1 CM:1 DP:1 CD: 6 NE, this sample selection approach yielded an overrepresentation of children in the CM, DP, and CD groups relative to their distribution in the general population. Oversampling of children in psychopathology risk groups was carried out to increase the likelihood of observing depressive and conduct disorders over the course of the longitudinal study. Of those selected, 521 (64.6%) students and their parents/guardians consented to participate. Demographic information on the sample at baseline is provided in Table 1.
Table 1.
Demographic characteristics of sample at baseline
| Variable | M (range) or frequency % |
| Age, in years | 12.0 (11.0–13.6) |
| Male gender | 51.6% |
| Race/ethnicity | |
| Non-Hispanic White | 39.5% |
| Black | 24.9% |
| Asian/Pacific Islander | 24.1% |
| Hispanic | 10.1% |
| Native American | 1.4% |
| Household income | |
| Low income, <$34,999 | 33.4% |
| Mid income, $35,000–$74,999 | 35.5% |
| High income, ≥$75,000 | 31.1% |
| Single-parent household | 27.3% |
| Lifetime history of any substance use disorder among biological parentsa | 42.0% |
Based on the Family History Screen (Weissman et al., 2000) collected at the eighth-grade interview (n = 457).
In-home interviews were administered to participating students and parents/guardians (76% biological mothers, 15% biological fathers, 9% other relatives) by two trained research interviewers. Consistent with recommendations of the Diagnostic Interview Schedule for Children (DISC) development group, the training protocol involved 16 hours of training before conducting study interviews. Interviewers’ training included didactic information, observation of a trained interviewer, delivery of a mock interview, and live supervision of the first interview. Ongoing quality assurance checks of interviews were also performed. Interviewers were blind to the psychopathology risk group status of the students. Baseline interviews were conducted within 3 months of screening (fall of sixth grade), and in-person follow-up interviews were conducted at 6, 12, 18, 24, and 36 months afterward. Of the participants originally enrolled in DPP, between 86% and 90% were retained in each of the first four follow-up interviews, including more than 80% in each psychopathology risk category. We ran analyses comparing cases with any missing data (n = 209) to those with no missing data whatsoever (n = 312).
Measures
Depressive symptoms and conduct problems.
In the fall of each assessment year (sixth, seventh, eighth, and ninth grades), the DISC was administered (Shaffer et al., 2000). The DISC is designed to make psychiatric diagnoses by applying criteria from the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (American Psychiatric Association, 1994), pertaining to anxiety, mood, disruptive behavior, and other disorders. The DISC has well-established psychometric properties, including strong agreement between clinician-administered DISC diagnoses and diagnoses made from clinical interviews (Schwab-Stone et al., 1996). DPP adolescents completed the self-administered depression and conduct disorder DISC modules while parents also completed the same DISC modules on their child. Depressive and conduct disorder symptoms endorsed as occurring within the past year were summed to form adolescent- and parent-reported depressive and conduct disorder symptom counts. Depressive symptom counts ranged from 0 to 22, whereas conduct disorder symptom counts ranged from 0 to 26.
Alcohol use.
The Customary Drinking and Drug Use Record (Brown et al., 1998) was administered at each visit to assess the level of alcohol and drug use participants engaged in during the prior 6 months. The Customary Drinking and Drug Use Record was originally validated in a community sample of adolescents, demonstrating high test–retest reliability over 1 week (r = .83 for alcohol), strong convergent validity (r = .68 for alcohol), and high interrater reliability (Brown et al., 1998). Given the limited amount and variability of alcohol use in the DPP sample, which is typical of early adolescent samples, a binary variable was created to indicate whether adolescents reported any use of alcohol within the past 6 months. Alcohol use questions specified how a standard drink was defined and required “more than just a sip or taste.”
Analytic plan
This study specified an autoregressive, cross-lagged path model with depressive and conduct disorder symptoms and alcohol use measured yearly from sixth to ninth grades. Analyses were first conducted with adolescent ratings of depressive and conduct disorder symptoms and with parental ratings of symptoms. We began by testing a fully constrained model using the total sample, with autoregressive and cross-lagged paths and within-grade covariances fixed to be equal across all grades. Then, to test whether depressive and conduct disorder symptoms varied over time as unique risk factors for alcohol use, we freed constraints on these paths in a stepwise fashion across grades and assessed whether model fit improved significantly via the chi-square difference test (Satorra and Bentler, 2001). Finally, to test whether prospective associations between depressive and conduct disorder symptoms and alcohol use varied by gender, we specified a multiple group model and tested whether freeing pathways across gender improved the fit of the model.
We estimated the path models using Mplus 6.0 (Muthén and Muthén, 2010) and the weighted least squares with robust means and variances estimator because alcohol use was a binary outcome. All participants contributed at least some data to these analyses; no cases were dropped owing to missing data because full-information maximum likelihood estimates were used. Preliminary analyses indicated that participants missing some data were more likely to be ethnic minorities and lower income, compared with participants missing no data. Thus, these variables were included as covariates. Missingness was not associated with gender, χ2(1) = 0.83, p = .36, but was significantly associated with more depressive symptoms (three of four time points for youth report, one of four time points for parental report), higher conduct problems (four of four time points for youth report, two of four time points for parental report), and more frequent alcohol use (two of four time points). Because these variables were included in our model, the assumption of missing at random is retained. Model fit indices used in this study were chi-square, root mean square error of approximation (RMSEA), and comparative fit index (CFI). A model is considered a good fit for the data when chi-square is nonsignificant (or when χ2/df < 2) or when RMSEA is .06 or less and CFI is .95 or greater (Hu and Bentler, 1999).
Results
Descriptive statistics
Correlations between adolescent and parental report of major depressive symptoms were significant at every time point but were small to modest in magnitude (mean r = .22, range: .16−.26). Correlations between adolescent and parental report of conduct disorder symptoms were also significant at every time point and were higher in magnitude (mean r = .46, range: .41−.51). Table 2 provides descriptive statistics for depressive symptoms, conduct disorder symptoms, and alcohol use for males and females from sixth to ninth grades. Although neither mean number of depressive nor conduct disorder symptoms changed appreciably over the course of early adolescence, the proportion of adolescents using alcohol increased from 3%,–4% in sixth grade to 21%–31% in ninth grade. T tests indicated that adolescent females reported more depressive symptoms than males in eighth and ninth grades but not in sixth and seventh grades. However, parents of males indicated that their sons exhibited more depressive symptoms in sixth grade than did the parents of females. There were no significant gender differences on parent-reported depressive symptoms from seventh to ninth grades. Males and their parents reported that they exhibited significantly more conduct problems at each time point than females. Although there were no gender differences in alcohol use from sixth to eighth grades, chi-square analyses indicated that females were more likely than males to report using alcohol in ninth grade. Inter-correlations among depressive symptoms, conduct disorder symptoms, and alcohol use within and across grades are presented in Table 3.
Table 2.
Descriptive statistics for depressive symptoms, conduct disorder symptoms, and alcohol use
| Variable | Sixth grade1 |
Seventh grade2 |
Eighth grade3 |
Ninth grade4 |
||||
| Males M (SD) or % | Females M (SD) or % | Males M (SD) or % | Females M (SD) or % | Males M (SD) or % | Females M (SD) or % | Males M (SD) or % | Female M (SD) or % | |
| DEP-adol. | 6.88 (4.73) | 6.36 (4.65) | 4.71 (4.19) | 4.79 (4.38) | 3.93 (3.79)a | 5.30(4.71)b | 4.40 (3.65)a | 5.76 (4.52)b |
| DEP-par. | 4.55 (3.44)a | 3.73 (3.57)b | 3.87 (3.23) | 3.37 (3.36) | 3.73 (3.39) | 3.23 (3.32) | 3.80 (3.47) | 3.22 (3.50) |
| CD-adol. | 2.92 (3.67)a | 1.35 (2.20)b | 2.50 (2.74)a | 1.59 (2.72)b | 2.98 (3.85)a | 2.04 (2.96)b | 3.72 (4.02)a | 2.93 (3.47)b |
| CD-par. | 2.00 (2.50)a | 1.36 (2.05)b | 2.00 (2.45)a | 1.43 (2.09)b | 2.43 (3.04)a | 1.57 (2.21)b | 2.71 (3.06)a | 1.65(2.51)b |
| Alcohol use | 4.10% | 3.17% | 3.88% | 7.04% | 7.73% | 12.92% | 21.03%a | 30.92%b |
Notes: Variables with different subscripts for males and females indicate a significant gender effect (p < .05). DEP = depression symptom count from the Diagnostic Interview Schedule for Children (DISC); adol. = adolescent report; par. = parental report on adolescent behavior; CD = conduct disorder symptom count from DISC; alcohol use = adolescent report of whether he or she used alcohol in the past 6 months (yes/no).
Males: n = 269; females: n = 252.
Males: n = 232; females: n = 213.
Males: n = 228; females: n = 215.
Males: n = 214; females: n = 207.
Table 3.
Intercorrelations among depressive (DEP) and conduct disorder (CD) symptoms and alcohol use (ALC) from sixth through ninth grades
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | |
| 1. Gender | – | −.12** | −.14** | −.03 | −.08 | −.12** | .07 | −.07 | −.16** | .09 | −.08 | −.19** | .11* |
| 2. DEP-6th | −.06 | – | .35** | .07 | .64** | .28** | .19** | .57** | .29** | .11** | .55** | .26** | .09 |
| 3. CD-6th | −.25** | .38** | – | .03 | .30** | .74** | .11** | .28* | .74** | .07 | .29** | .63** | .08 |
| 4. ALC-6th | −.03 | .23** | .37** | – | .04 | .04 | .23** | .05 | .10* | –a | .06 | .05 | .06 |
| 5. DEP-7th | .01 | .61** | .26** | .13** | – | .41** | .11* | .66** | .33** | .09 | .65** | .37** | .07 |
| 6. CD-7th | −.16** | .33** | .65** | .22** | .42** | – | .10* | 27** | .69** | .07 | .31** | .62** | .09 |
| 7. ALC-7th | .07 | .19** | .11** | .23** | .19** | .25** | – | .09 | .15** | .35** | .09 | .20** | .24** |
| 8. DEP-8th | .16** | .50** | .14* | .16** | .60** | .31** | .08 | – | .35** | .01 | .69** | .28** | .06 |
| 9. CD-8th | −.14** | .24** | .65** | .12** | .33** | .69** | .17** | .26** | – | .17** | .28** | .75** | .22** |
| 10. ALC-8th | .09 | .14** | .20** | –a | .17** | .17** | .35** | .18** | .34** | – | .08 | .27** | .35** |
| 11.DEP-9th | .16** | .49** | .17** | .17** | .54** | .21** | .02 | .68** | .20** | .17** | – | .40** | .08 |
| 12. CD-9th | −.10* | .27** | .72** | .16** | .27** | .67** | .13** | .26** | .80** | .33** | .34** | – | .15** |
| 13. ALC-9th | .11* | .11* | .23** | .06 | .19** | .19** | .24** | .20** | .36** | .35** | .15** | .38** | – |
Notes: Adolescent-reported depressive and conduct disorder symptoms are shown below the diagonal. Parental ratings of adolescent depressive and conduct disorder symptoms are shown above the diagonal. Sample sizes range from 373 to 512 for adolescent ratings and from 370 to 517 for parental ratings, depending on what grades were correlated. Gender (1 = male, 2 = female); DEP = depression symptom count from the Diagnostic Interview Schedule for Children (DISC); CD = conduct disorder symptom count from DISC; ALC = adolescent-report of whether he or she used alcohol in the past 6 months (yes/no).
Correlation could not be computed because sixth-grade alcohol use was 0 for all respondents available for the correlation.
p < .05;
p < .01.
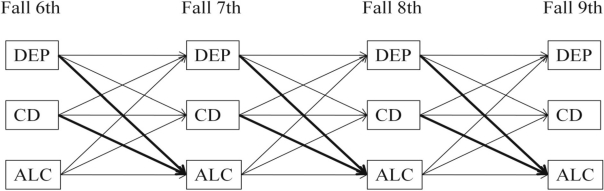
Fully constrained models
The fully constrained, autoregressive, cross-lagged path model tested in this study is shown in Figure 1. This model was built in several steps. First, we imposed an autoregressive structure, such that depressive and conduct disorder symptoms and alcohol use at each grade were predicted by the same behavior at the prior grade, with respective stability paths for depressive and conduct disorder symptoms, and alcohol use constrained to equality over time. Second, we estimated prospective paths between depressive and conduct disorder symptoms and alcohol use, over and above the stability paths. These cross-lagged paths were assumed to be time invariant and thus were constrained to be equal across grades. Third, we also estimated within-time covariances between the residuals of the variables at Grades 7–9 and fixed each specific residual covariance to be equal across grades. Taken together, the fully constrained model adequately fit the adolescent-report data, χ2(51, N = 521) = 102.75, p < .001 (CFI = .95; RMSEA = .04), and the parental-report data, χ2(51, N = 521) = 85.87, p < .01 (CFI = .97; RMSEA = .04).
Figure 1.
Autoregressive, cross-lagged path model examining prospective relations among depressive (DEP) and conduct disorder (CD) symptoms and alcohol use (ALC) in early adolescence. Notes: Bold lines indicate paths of interest. Within-time correlations between depressive symptoms, conduct problems, and alcohol use at Grade 6, as well as within-time correlations between the residuals of the variables at Grades 7–9, were included in the model. They are omitted from figure for sake of parsimony.
Time invariance of effects
Next, we examined whether within-grade covariances and stability coefficients freed in a stepwise, sequential fashion would improve model fit. Model fit did not change significantly when covariances and stability coefficients were freed with adolescent data. However, the path between sixth- and seventh-grade conduct disorder symptoms was smaller than the paths at other time points in the adolescent data, Δχ2(1) = 21.00, p < .001. For parental data, results indicated that the residual covariance between alcohol use and depressive symptoms in eighth grade was weaker relative to the same association at other grades in the parental report data, Δχ2(1) = 4.62, p < .05. Moreover, the path between eighth-and ninth-grade alcohol use was larger relative to the paths, Δχ2(1) = 4.27, p < .05, whereas the path between seventh-and eighth-grade conduct disorder symptoms was smaller, Δχ20) = 5.13, p < .05, than it was at other time points. These results indicated partial invariance in the stability coefficients and residual covariances over time.
In terms of the cross-lagged effects, there was no evidence for non-invariance across time in the adolescent data. This suggested that the strength of prospective associations between depressive or conduct disorder symptoms and alcohol use did not vary across grades according to self-report ratings. Conversely, the prospective path between sixth-grade depressive symptoms and seventh-grade alcohol use was stronger than at other time points in the parental report data, Δχ20) = 6.18, p < .05, suggesting partial invariance in the prospective associations between adolescent depression and alcohol use among the parent ratings.
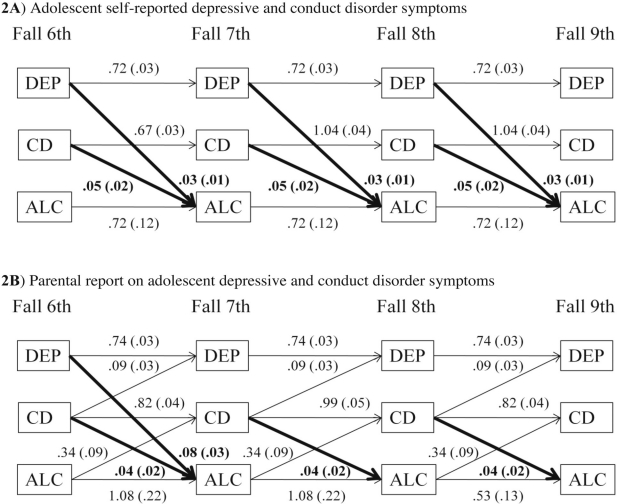
The final models were a good fit with the adolescent data, χ2(50, N= 521) = 81.75, p < .01 (CFI = .97; RMSEA = .04), and parental data, χ2(47, N = 521) = 65.68, p < .05 (CFI = .98; RMSEA = .03). Figures 2A and 2B illustrate models with adolescent and parental data, respectively. Regarding the model with adolescent-report data, both depressive and conduct disorder symptoms were unique and consistent predictors of subsequent alcohol use over and above prior use. The strength of risk did not vary significantly across grades for depressive symptoms (β range: .09-. 13) or conduct disorder symptoms (β range: .09−. 14). (Although paths were fixed over time for both depression and conduct disorder symptoms, standardized betas differ over time. This is because standardized estimates are derived from the standard deviation and exact predictive model for each dependent variable, which often varies from one time point to the next.) Results with parental ratings of adolescent behavior indicated that conduct disorder symptoms consistently increased risk of alcohol use across grades over and above prior use (β range: .06−.09). However, only depressive symptoms observed by parents in sixth grade increased the risk of subsequent (seventh grade) alcohol use over and above prior use (β = .24). Depressive symptoms in seventh and eighth grades did not significantly predict alcohol use in eighth and ninth grades, respectively. Results were replicated using ethnicity (racial minority vs. White) and then total household family income as covariates in the model.
Figure 2.
Path model examining depressive (DEP) and conduct disorder (CD) symptoms as risk factors for alcohol use (ALC) in early adolescence. Notes: Only significant (p < .05) paths shown. Bold lines indicate paths of interest. Unstandardized B coefficients are provided (with standard errors in parentheses).
Gender differences
Using the best-fitting models for adolescent and parental data, we then tested whether the strength of paths between depressive and conduct disorder symptoms and alcohol use varied by adolescent gender using multiple group analyses. Initial tests with paths of interest constrained to be equal across gender indicated that the multiple group model fit the adolescent data adequately, χ2(116, N= 521) = 154.60, p < .01 (CFI = .97; RMSEA = .04), as well as the parental data, χ2(112, N = 521) = 129.54, p = .12 (CFI = .99; RMSEA =.03). When the prospective paths from depressive and conduct disorder symptoms to alcohol use were freed to vary between males and females, model fit did not improve with adolescent or parental data—for adolescent data, Δχ2(2) = 1.74, p = .42; for parental data, Δχ2(1) = 1.20, p = .27. Thus, both self- and parent-report data indicate that risk for alcohol use conferred by depressive and conduct disorder symptoms do not differ between male and female adolescents.
Discussion
The current study was designed to examine the association between adolescent depression and early adolescent alcohol use addressing several methodological limitations in previous studies. Specifically, we assessed effects annually for 4 years during the early adolescent period (∼12–15 years, representing sixth to ninth grades); we controlled for the most common comorbid condition for alcohol use, conduct disorder; we analyzed data from two different informants (adolescent self-report vs. parental report); and we tested moderation by gender. Results suggested that depressive symptoms were associated with increased risk for alcohol use during early adolescence, even while controlling for conduct disorder. However, effects differed depending on informant. For youth self-report, a consistent and positive association between depressive symptoms and alcohol use 1 year later was established throughout our window of assessment. In contrast, according to parental report, only very early adolescent depressive symptoms and alcohol use (sixth to seventh grades, representing ages 12–13) were significantly associated, with other time points indicating no evidence for an association. These effects were found controlling for the presence of conduct disorder and were not moderated by gender.
The broader literature has suggested mixed findings regarding the role of depression as a risk factor for the development of early alcohol use and alcohol problems. It is not unusual to find seemingly discrepant findings as to whether depression is prospectively associated with alcohol use even within study based on measures and time frames used in the analyses (McCarty et al., 2011b). Of particular note, our recent review of this literature has suggested that studies using samples earlier in adolescence, studies measuring substance use within the past year or less (as opposed to measuring lifetime use), studies using community or school-based samples, and studies examining shorter term associations between depression and substance use were more likely to report positive associations (McCarty et al., 2011b). The current study has each of these methodological characteristics and yielded a positive association between depressive symptoms and substance use. Measurement and methodological choices may have greater influence on study findings for depression and alcohol use (in comparison with conduct problems and alcohol use) because associations between depression and alcohol use appear to be generally less robust. In a previous study using the same sample, depressive symptoms were elevated for the earliest substance users (those who had used by the fall of sixth grade) but were not associated with time to onset of alcohol use after sixth grade (McCarty etal., 2011a).
Prospective associations between conduct problems and alcohol use were significant for all time points and for parent and child informants, showing developmental consistency. These results are generally consistent with other studies that suggest conduct problems are a strong predictor of alcohol use, but the findings add to the existing literature by explicitly demonstrating similarity over time in the effects of conduct problems through empirical model comparisons. One previous study has examined the effects of past conduct disorder on substance use disorders at different ages in adolescence, suggesting that the effects are stronger earlier in adolescence (ages 13, 14, and 15) compared with later in adolescence (age 16) (Sung et al., 2004). However, the current study differs in that we tested the proximal effects of conduct disorder (and depression) in the prior year instead of using a static measure of “any past disorder.” We also examined an earlier developmental time frame (corresponding to ages 12, 13, 14, and 15), and thus did not have the opportunity to replicate the previously observed weakening of the association at age 16.
There are several potential explanations for the different findings regarding depressive symptoms across informant. For example, it is possible that parents’ ability to detect depressive symptoms among their children is low because many of the symptoms involve assessment of internal feel, states, and cognitions that may not be readily shared by parent and child, particularly in the absence of behavioral problems (Rockhill et al., 2007). As adolescents age and spend more time away from parents and out-of-the-home context, observation of these symptoms may become even more difficult for parents. Another possibility is that depressive symptoms with an early onset are indicative of a different and more heterogeneous developmental pathway, with more susceptibility to broader behavioral problems like alcohol use. This is in contrast to depressive symptoms that emerge later in development when symptoms are more prevalent but also are more strongly linked to increased risk for recurrent depression in adulthood (Alpert et al., 1999; Harrington, 2001; Weissman et al., 1999). This may be particularly true if depressive symptoms are prominent enough to be noticed by parents.
No gender differences emerged in the associations between depressive symptoms and alcohol use for boys versus girls. Selective studies have found differential effects (Fleming et al., 2008; Marmorstein, 2009; Mason et al., 2007), although these studies have been inconsistent as to whether associations are greater for girls or boys. A number of studies have also tested for but not found gender differences in the association between depressive symptoms and alcohol use (McCarty et al., 201 1b).
The strengths of this study include the prospective, multiwave annual measurement of depressive and conduct disorder symptoms and the use of a large, ethnically diverse community-based sample. Nonetheless, several limitations should be acknowledged. First, much of the data, including substance use, were assessed via self-report. The greater consistency for youth-reported depression and substance use found in the current and previous studies may, to some extent, reflect method variance. There was no external validation of substance use, but other research indicates that individuals’ self-reports of substance use in surveys of this type are reliable and valid (Stone and Latimer, 2005). A second limitation is generalizability in that the study sample comprises youth residing in the metropolitan area of Seattle, and alcohol use patterns likely differ from youth in other parts of the country, as well as from suburban or rural locations (Way et al., 1994). Third, depressive symptoms in the sample did not demonstrate an overall increase over the developmental window examined in this study, which may have been affected by selecting students for the study on the basis of conduct problems and depressive symptoms or by repeated measurement (Angold et al., 2002). Finally, other emotional and behavioral problems, including anxiety and inattention/impulsivity, were not included in models but may be important in providing a more complete understanding of the role of psychopathology in the development of alcohol use in early adolescence.
Despite these limitations, the study offers important implications for alcohol use prevention and research. These results indicate that conduct disorder symptoms and depressive symptoms are both important indicators of risk for early use of alcohol across early adolescence—a time in which use is associated with particularly pernicious consequences—and provide further support toward a possible “internalizing pathway” to alcohol use (Hussong et al., 2011). Youth with elevated conduct problems, whether with or without depressive symptoms, are clearly at risk for the development of alcohol use. Although parental assessment of youth depression is not as reliable an indicator of risk for early alcohol use, there may be some utility in considering parental report of depression for early-onset symptoms. However, youth-reported depressive symptoms are more reliable in their association with later alcohol use. An important design feature of the current study was examining depressive symptoms as a unique predictor over and above conduct disorder symptoms. Our findings suggest that depressive symptoms serve a unique role in predicting early adolescent substance use. Overall, early intervention to reduce both depressive symptoms and conduct problems may be a useful way to interrupt trajectories leading to early adolescent alcohol use. Development and testing of interventions that explicitly address co-occurring depression, conduct problems, and alcohol use or that target common risk factors may help reduce the likelihood that these clinical comorbidities will persist and adversely affect multiple aspects of development.
Footnotes
This research was supported by National Institutes of Health Grants R01 AA018701 (to Carolyn A. McCarty) and R01 MH/DA63711 (to Ann Vander Stoep and Elizabeth McCauley), Seattle Children's Hospital Steering Committee Grant and American Foundation for Suicide Prevention Grant (to Ann Vander Stoep), and University of Washington Provost Bridge Funding (to Ann Vander Stoep and Elizabeth McCauley). Analyses were previously presented at the Society for Research in Child Development, Montreal, Canada (April 2011).
References
- Achenbach TM. Youth Self-Report for ages 11–18. Burlington, VT: University of Vermont; 2001. [Google Scholar]
- Alpert JE, Fava M, Uebelacker LA, Nierenberg AA, Pava JA, Worthington JJ, III, Rosenbaum JF. Patterns of axis I comorbidity in early-onset versus late-onset major depressive disorder. Biological Psychiatry. 1999;46:202–211. doi: 10.1016/s0006-3223(99)00017-7. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington, DC: Author; 1994. [Google Scholar]
- Angold A, Costello EJ. Mood and Feelings Questionnaire (MFQ) Durham, NC: Duke University, Developmental Epidemiology Program; 1987. [Google Scholar]
- Angold A, Costello EJ, Erkanli A. Comorbidity. Journal of Child Psychology and Psychiatry. 1999;40:57–87. [PubMed] [Google Scholar]
- Angold A, Costello EJ, Worthman CM. Puberty and depression: The roles of age, pubertal status and pubertal timing. Psychological Medicine. 1998;28:51–61. doi: 10.1017/s003329179700593x. [DOI] [PubMed] [Google Scholar]
- Angold A, Erkanli A, Silberg J, Eaves L, Costello EJ. Depression scale scores in 8–17-year-olds: Effects of age and gender. Journal of Child Psychology and Psychiatry. 2002;43:1052–1063. doi: 10.1111/1469-7610.00232. [DOI] [PubMed] [Google Scholar]
- Armstrong TD, Costello EJ. Community studies on adolescent substance use, abuse, or dependence and psychiatric comorbidity. Journal of Consulting and Clinical Psychology. 2002;70:1224–1239. doi: 10.1037//0022-006x.70.6.1224. [DOI] [PubMed] [Google Scholar]
- Braaten EB, Biederman J, Dimauro A, Mick E, Monuteaux MC, Muehl K, Faraone SV. Methodological complexities in the diagnosis of major depression in youth: An analysis of mother and youth self-reports. Journal of Child and Adolescent Psychopharmacol-ogy. 2001;11:395–407. doi: 10.1089/104454601317261573. [DOI] [PubMed] [Google Scholar]
- Brown SA, Myers MG, Lippke L, Tapert SF, Stewart DG, Vik PW. Psychometric evaluation of the Customary Drinking and Drug Use Record (CDDR): A measure of adolescent alcohol and drug involvement. Journal of Studies on Alcohol. 1998;59:427–438. doi: 10.15288/jsa.1998.59.427. [DOI] [PubMed] [Google Scholar]
- Cadoret RJ, Yates WR, Troughton E, Woodworth G, Stewart MA. Adoption study demonstrating two genetic pathways to drug abuse. Archives of General Psychiatry. 1995;52:42–52. doi: 10.1001/archpsyc.1995.03950130042005. [DOI] [PubMed] [Google Scholar]
- Capaldi DM. Co-occurrence of conduct problems and depressive symptoms in early adolescent boys: II. A 2-year follow-up at Grade 8. Development and Psychopathology. 1992;4:125–144. doi: 10.1017/s0954579499001959. [DOI] [PubMed] [Google Scholar]
- Clark DB. The natural history of adolescent alcohol use disorders. Addiction, 99, Supplement 2. 2004:5–22. doi: 10.1111/j.1360-0443.2004.00851.x. [DOI] [PubMed] [Google Scholar]
- Corte C, Zucker RA. Self-concept disturbances: Cognitive vulnerability for early drinking and early drunkenness in adolescents at high risk for alcohol problems. Addictive Behaviors. 2008;33:1282–1290. doi: 10.1016/j.addbeh.2008.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costello EJ. Psychiatric predictors of adolescent and young adult drug use and abuse: What have we learned? Drug and Alcohol Dependence, 88, Supplement 1. 2007:S97–S99. doi: 10.1016/j.drugalcdep.2006.12.027. [DOI] [PubMed] [Google Scholar]
- Costello EJ, Erkanli A, Federman E, Angold A. Development of psychiatric comorbidity with substance abuse in adolescents: Effects of timing and sex. Journal of Clinical Child Psychology. 1999;28:298–311. doi: 10.1207/S15374424jccp280302. [DOI] [PubMed] [Google Scholar]
- Crum RM, Storr CL, Ialongo N, Anthony JC. Is depressed mood in childhood associated with an increased risk for initiation of alcohol use during early adolescence? Addictive Behaviors. 2008;33:24–40. doi: 10.1016/j.addbeh.2007.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeWit DJ, Adlaf EM, Offord DR, Ogborne AC. Age at first alcohol use: A risk factor for the development of alcohol disorders. American Journal of Psychiatry. 2000;157:745–750. doi: 10.1176/appi.ajp.157.5.745. [DOI] [PubMed] [Google Scholar]
- Fergusson DM, Horwood LJ, Ridder EM. Conduct and attentional problems in childhood and adolescence and later substance use, abuse and dependence: Results of a 25-year longitudinal study. Drug and Alcohol Dependence, 88, Supplement 1. 2007:S14–S26. doi: 10.1016/j.drugalcdep.2006.12.011. [DOI] [PubMed] [Google Scholar]
- Fleming CB, Mason WA, Mazza JJ, Abbott RD, Catalano RF. Latent growth modeling of the relationship between depressive symptoms and substance use during adolescence. Psychology of Addictive Behaviors. 2008;22:186–197. doi: 10.1037/0893-164X.22.2.186. [DOI] [PubMed] [Google Scholar]
- Hankin BL, Abramson LY, Moffitt TE, Silva PA, McGee R, Angell KE. Development of depression from preadolescence to young adulthood: Emerging gender differences in a 10-year longitudinal study. Journal of Abnormal Psychology. 1998;107:128–140. doi: 10.1037//0021-843x.107.1.128. [DOI] [PubMed] [Google Scholar]
- Harrington R. Adolescent depression: Same or different? Archives of General Psychiatry. 2001;58:21–22. doi: 10.1001/archpsyc.58.1.21. [DOI] [PubMed] [Google Scholar]
- Hu L-T, Bentler PM. Cutoff criteria for fit indexes in covari-ance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal. 1999;6:1–55. [Google Scholar]
- Hussong AM, Curran PJ, Chassin L. Pathways of risk for accelerated heavy alcohol use among adolescent children of alcoholic parents. Journal of Abnormal Child Psychology. 1998;26:453–466. doi: 10.1023/a:1022699701996. [DOI] [PubMed] [Google Scholar]
- Hussong AM, Jones DJ, Stein GL, Baucom DH, Boeding S. An internalizing pathway to alcohol use and disorder. Psychology of Addictive Behaviors. 2011;25:390–404. doi: 10.1037/a0024519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ingoldsby EM, Kohl GO, McMahon RJ, Lengua L the Conduct Problems Prevention Research Group. Conduct problems, depressive symptomatology and their co-occurring presentation in childhood as predictors of adjustment in early adolescence. Journal of Abnormal Child Psychology. 2006;34:603–621. doi: 10.1007/s10802-006-9044-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnston LD, O'Malley PM, Bachman JG. Monitoring the Future national results on adolescent drug use: Overview of key findings, 2000 (NIH Publication No. 01-4923) Bethesda, MD: National Institute on Drug Abuse; 2001. [Google Scholar]
- Kandel DB, Johnson JG, Bird HR, Weissman MM, Goodman SH, Lahey BB, Schwab-Stone ME. Psychiatric comorbidity among adolescents with substance use disorders: Findings from the MECA Study. Journal of the American Academy of Child & Adolescent Psychiatry. 1999;38:693–699. doi: 10.1097/00004583-199906000-00016. [DOI] [PubMed] [Google Scholar]
- King KM, Chassin L. A prospective study of the effects of age of initiation of alcohol and drug use on young adult substance dependence. Journal of Studies on Alcohol and Drugs. 2007;68:256–265. doi: 10.15288/jsad.2007.68.256. [DOI] [PubMed] [Google Scholar]
- King KM, Chassin L. Adolescent stressors, psychopathology, and young adult substance dependence: A prospective study. Journal of Studies on Alcohol and Drugs. 2008;69:629–638. doi: 10.15288/jsad.2008.69.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King SM, Iacono WG, McGue M. Childhood externalizing and internalizing psychopathology in the prediction of early substance use. Addiction. 2004;99:1548–1559. doi: 10.1111/j.1360-0443.2004.00893.x. [DOI] [PubMed] [Google Scholar]
- Loeber R, Stouthamer-Loeber M, White HR. Developmental aspects of delinquency and internalizing problems and their association with persistent juvenile substance use between ages 7 and 18. Journal of Clinical Child Psychology. 1999;28:322–332. doi: 10.1207/S15374424jccp280304. [DOI] [PubMed] [Google Scholar]
- Maggs JL, Patrick ME, Feinstein L. Childhood and adolescent predictors of alcohol use and problems in adolescence and adulthood in the National Child Development Study. Addiction, 103, Supplement 1. 2008:7–22. doi: 10.1111/j.1360-0443.2008.02173.x. [DOI] [PubMed] [Google Scholar]
- Maggs JL, Schulenberg JE. Initiation and course of alcohol consumption among adolescents and young adults. In: Galanter M, editor. Alcohol problems in adolescents and young adults: Epidemiology, neu-robiology, prevention, and treatment. New York, NY: Springer; 2006. [Google Scholar]
- Marmorstein NR. Longitudinal associations between alcohol problems and depressive symptoms: Early adolescence through early adulthood. Alcoholism: Clinical and Experimental Research. 2009;33:49–59. doi: 10.1111/j.1530-0277.2008.00810.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mason WA, Hitchings JE, Spoth RL. Emergence of delinquency and depressed mood throughout adolescence as predictors of late adolescent problem substance use. Psychology of Addictive Behaviors. 2007;21:13–24. doi: 10.1037/0893-164X.21.1.13. [DOI] [PubMed] [Google Scholar]
- Mason WA, Hitchings JE, Spoth RL. The interaction of conduct problems and depressed mood in relation to adolescent substance involvement and peer substance use. Drug and Alcohol De. 2008;96:233–248. doi: 10.1016/j.drugalcdep.2008.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mason WA, Windle M. Reciprocal relations between ado substance use and delinquency: A longitudinal latent variable analysis. Journal ofAbnormal Psychology. 2002;111:63–76. doi: 10.1037//0021-843x.111.1.63. [DOI] [PubMed] [Google Scholar]
- McCarty CA, Rhew IC, Murowchick E, McCauley E, Vander Stoep A. Emotional health predictors of substance use initiation during middle school. Psychology of Addictive Behaviors. 2011a doi: 10.1037/a0025630. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCarty CA, Vander Stoep A, Wymbs BT, McCauley E, Myaing M, Zhou C, et al. Longitudinal studies of adolescent depression and substance use: Some methodological considerations. Manuscript in preparation. 2011b [Google Scholar]
- McGee R, Feehan M, Williams S, Anderson J. DSM-III disorders from age 11 to age 15 years. Journal of the American Academy of Child & Adolescent Psychiatry. 1992;31:50–59. doi: 10.1097/00004583-199201000-00009. [DOI] [PubMed] [Google Scholar]
- Miller-Johnson S, Lochman JE, Coie JD, Terry R, Hyman C. Comorbidity of conduct and depressive problems at sixth grade: Substance use outcomes across adolescence. Journal of Abnormal Child Psychology. 1998;26:221–232. doi: 10.1023/a:1022676302865. [DOI] [PubMed] [Google Scholar]
- Muthén B, Muthén L. Mplus user's guide. 6th ed. Los Angeles, CA: Authors; 2010. [Google Scholar]
- Needham BL. Gender differences in trajectories of depressive symptomatology and substance use during the transition from adolescence to young adulthood. Social Science & Medicine. 2007;65:1166–1179. doi: 10.1016/j.socscimed.2007.04.037. [DOI] [PubMed] [Google Scholar]
- Rao U, Ryan ND, Dahl RE, Birmaher B, Rao R, Williamson DE, Perel JM. Factors associated with the development of substance use disorder in depressed adolescents. Journal of the American Academy of Child & Adolescent Psychiatry. 1999;38:1109–1117. doi: 10.1097/00004583-199909000-00014. [DOI] [PubMed] [Google Scholar]
- Rockhill CM, Russo JE, McCauley E, Katon WJ, Richardson LP, Lozano P. Agreement between parents and children regarding anxiety and depression diagnoses in children with asthma. The Journal of Nervous and Mental Disease. 2007;195:897–904. doi: 10.1097/NMD.0b013e318159289c. [DOI] [PubMed] [Google Scholar]
- Rohde P, Lewinsohn PM, Seeley JR. Psychiatric comorbid with problematic alcohol use in high school students. Journal of the American Academy of Child & Adolescent Psychiatry. 1996;35:101–109. doi: 10.1097/00004583-199601000-00018. [DOI] [PubMed] [Google Scholar]
- Satorra A, Bentler PM. A scaled difference chi-square test statistic for moment structure analysis. Psychometrika. 2001;66:507–514. doi: 10.1007/s11336-009-9135-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwab-Stone ME, Shaffer D, Dulcan MK, Jensen PS, Fisher P, Bird HR, Rae DS. Criterion validity of the NIMH Diagnostic Interview Schedule for Children Version 2.3 (DISC-2.3) Journal of the American Academy of Child & Adolescent Psychiatry. 1996;35:878–888. doi: 10.1097/00004583-199607000-00013. [DOI] [PubMed] [Google Scholar]
- Shaffer D, Fisher P, Lucas CP, Dulcan MK, Schwab-Stone ME. NIMH Diagnostic Interview Schedule for Children Version IV (NIMH DISC-IV): Description, differences from previous versions, and reliability of some common diagnoses. Journal of the American Academy of Child & Adolescent Psychiatry. 2000;39:28–38. doi: 10.1097/00004583-200001000-00014. [DOI] [PubMed] [Google Scholar]
- Stone AL, Latimer WW. Adolescent substance use assessment: Concordance between tools using self-administered and interview formats. Substance Use & Misuse. 2005;40:1865–1874. doi: 10.1080/10826080500260925. [DOI] [PubMed] [Google Scholar]
- Sung M, Erkanli A, Angold A, Costello EJ. Effects of age at first substance use and psychiatric comorbidity on the develop of substance use disorders. Drug and Alcohol Dependence. 2004;75:287–299. doi: 10.1016/j.drugalcdep.2004.03.013. [DOI] [PubMed] [Google Scholar]
- Tapert SF, Colby SM, Barnett NP, Spirito A, Rohsenow DJ, Myers MG, Monti PM. Depressed mood, gender, and problem drinking in youth. Journal of Child & Adolescent Substance Abuse. 2003;12:55–68. [Google Scholar]
- Vander Stoep A, McCauley E, Thompson KA, Herting JR, Kuo ES, Stewart DG, Kushner S. Universal emotional health screening at the middle school transition. Journal of Emotional and Behavioral Disorders. 2005;13:213–223. doi: 10.1177/10634266050130040301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Velez CN, Johnson J, Cohen P. A longitudinal analysis of selected risk factors for childhood psychopathology. Journal of the American Academy of Child & Adolescent Psychiatry. 1989;28:861–864. doi: 10.1097/00004583-198911000-00009. [DOI] [PubMed] [Google Scholar]
- Verhulst FC, Eussen MLJM, Berden GEMG, Sanders-Woudstra J, van der Ende J. Pathways of problem behaviors from childhood to adolescence. Journal of the American Academy of Child & Adolescent Psychiatry. 1993;32:388–396. doi: 10.1097/00004583-199303000-00021. [DOI] [PubMed] [Google Scholar]
- Washington State Department of Health. Healthy Youth Survey. 2008. Retrieved from https://fortress.wa.gov/doh/hys/ASPX/HYSreports.aspx. [Google Scholar]
- Way N, Stauber HY, Nakkula MJ, London P. Depression and substance use in two divergent high school cultures: A quantitative and qualitative analysis. Journal of Youth and Adolescence. 1994;23:331–357. [Google Scholar]
- Weissman MM, Wolk S, Goldstein RB, Moreau D, Adams P, Gre-enwald S, Wickramaratne P. Depressed adolescents grown up. Journal of the American Medical Association. 1999;281:1707–1713. doi: 10.1001/jama.281.18.1707. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Wickramaratne P, Adams P, Wolk S, Verdeli H, Olfson M. Brief screening for family psychiatric history: The family history screen. Archives of General Psychiatry. 2000;57:675–682. doi: 10.1001/archpsyc.57.7.675. [DOI] [PubMed] [Google Scholar]
- Wu P, Hoven CW, Okezie N, Fuller CJ, Cohen P. Alcohol abuse and depression in children and adolescents. Journal of Child & Adolescent Substance Abuse, 17. 2008:51–69. [Google Scholar]
- Zucker RA. Pathways to alcohol problems and alcoholisms: A developmental account of the evidence for multiple alcoholisms and for contextual contributions to risk. In: Zucker RA, Howard J, Boyd GM, editors. The development of alcohol problems: Exploring the biopsychosocial matrix of risk (Vol. 26, pp. 255–290) Rockville, MD: National Institute on Alcohol Abuse and Alcoholism; 1994. [Google Scholar]