Abstract
Although several epidemiological and intervention studies suggest that polyphenols (PPs) and PP-rich foods may improve memory and cognition in animals and humans, PPs’ mode of action is only poorly understood. To help distinguish between the different modes of action that have been proposed for PPs, it is obviously important to know how much PPs can accumulate in the brain, if any at all. However, reliable data on PP uptake into the brain of animals are limited as many studies failed to report important control procedures during data acquisition. In this paper, we summarize published data on the penetration of PPs into animal brain and review some hypotheses to explain the biological basis of potentially health-beneficial effects of PPs to the brain. Finally, we highlight promising new approaches, especially those of a hormetic dose-response and gut microbiota-brain interaction, which may allow a better understanding of PPs’ mode of action in animals and humans.
Keywords: Antioxidants, Effective brain concentration, Gut microbiota, Hormesis, Metabolic signalling, Polyphenols, Plasma concentration, Residual blood, Vitamin C
Introduction
Several epidemiological studies suggest that diets rich in polyphenols (PPs) beneficially affect human brain function (Commenges et al. 2000; Letenneur et al. 2007). Similarly, supplementing rodents and humans with isolated PPs (Macready et al. 2009; Maher et al. 2006) or PP-rich foods and plant extracts (e.g. tea, blueberries or pine bark extract) (Andres-Lacueva et al. 2005; Francis et al. 2006; Macready et al. 2009; Nurk et al. 2009; Ryan et al. 2008) may improve memory and cognition. Numerous mechanisms, such as free radical scavenging, metal chelation and the modulation of enzyme activities, have been proposed for explaining a positive impact of PPs on the brain (Schaffer et al. 2006; Spencer 2008, 2009). However, the existence of direct antioxidant or other significant systemic effects of PPs, especially in the brain, are often met with scepticism, mainly due to the relatively poor intestinal uptake of PPs, their substantial biotransformation (so that blood and tissue concentrations of unaltered PPs are very low) and rapid excretion (Halliwell et al. 2005; Halliwell 2007a, b; Hollman et al. 2011; Hu 2007; Lotito and Frei 2006; Zini et al. 2006).
From first principles, PPs might alter brain function at three locations: (1) outside the CNS (for instance by improving cerebral blood flow or by modulating signalling pathways from peripheral organs to the brain), (2) at the blood–brain barrier (BBB, e.g. by altering multi-drug-resistant protein-dependent influx and efflux mechanisms of various biomolecules) and (3) inside the CNS (e.g. by directly modifying the activity of neurons and glial cells) (Ghosh and Scheepens 2009; Spencer 2007; Youdim et al. 2004). To help distinguish between these different modes of action, it is obviously important to know how much PPs can accumulate in the brain, if any at all. However, as many studies failed to report important control procedures, reliable data on PP uptake into the brain of animals are limited. For obtaining meaningful information on this question, data ideally need to be collected either in exsanguinated and perfused animals (or tissues) or, alternatively, corrected for residual blood in the brain (Youdim et al. 2004). The importance of accurate in vivo measurements of brain drug exposure is highlighted in a recent study conducted in rats by Friden et al. (2010) who developed a mathematical model correcting drug brain concentrations for residual blood. After applying their model, the authors noted that concentrations of the drugs indomethacin and moxalactam in rat brain were significantly influenced by the amount of drug present in the residual blood.
In this paper, we first discuss published data on the penetration of PPs into animal brain. In cases where the PP-supplemented animals have neither been perfused nor residual blood in the brain has been corrected for as potential confounder, a correction of the reported PP brain concentrations has been attempted based on the mathematical model published by Friden et al. (2010). The second part of the current article summarizes some of the prevailing hypotheses for explaining the biological basis of potentially health-beneficial effects of PPs to the brain. Finally, we highlight promising new approaches that may allow for better understanding PPs’ mode of action in animals and humans.
Concentration of polyphenols in brain and the effect of mathematical correction
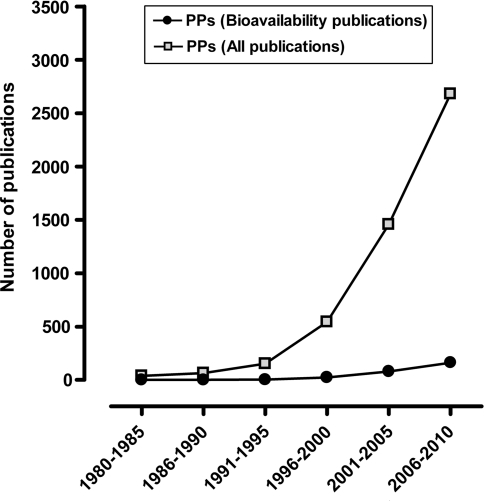
Since the mid-1990s, the number of articles published on PPs has increased exponentially. However, despite the tremendous interest in PP research, only a small fraction of all studies addressed the important question of PP uptake and bioavailability (Fig. 1). Unsurprisingly, our knowledge regarding PP absorption, metabolism, tissue distribution, intracellular accumulation and excretion is insufficient.
Fig. 1.
Number of hits found for the search term ‘polyphenols’ or ‘polyphenols AND bioavailability’ in PubMed. The search field tag was limited to ‘Title/Abstract’
So far, PP brain bioavailability has mainly been studied in rodents although at least one study was conducted in higher organisms, i.e. pigs (Tables 1 and 2). Exsanguinated and perfused animals are the gold standard for determining the amount of nutrient or drug that penetrated into the brain. Data from studies following this approach indicate that PPs usually accumulate at levels below 1 nmol/g tissue (Section 1 of Table 2). Similar findings result from studies where the brain PP concentration has been corrected for residual blood (Section 2 of Table 2). Furthermore, Janle et al. (2010) used accelerator mass spectrometry for detecting small amounts of labelled PPs in brain of perfused rats. Apart from this, a substantial number of articles reported brain PP uptake and concentrations without considering residual blood as a potential confounder (Chang et al. 2000; Datla et al. 2001; Huebbe et al. 2010; Pan et al. 1999; Peng et al. 1998; Purkayastha et al. 2009).
Table 1.
Methodological parameters of studies assessing PPs concentrations in animal brain (inclusion criteria were either the usage of exsanguinated and perfused animals or the correction for residual blood by other means)
| No. | PPs | Species | Route | Dosage | Duration | Sampling | Anaesthesia | Killing and tissue collection | References |
|---|---|---|---|---|---|---|---|---|---|
| Section I: studies in exsanguinated and perfused animals | |||||||||
| 1 | Epicatechin | Rat | Oral | 100 mg/kg BW | 1 day | 2 h after PP intake | Phenobarbitone | Plasma: Decapitation Brain: Perfusion |
Abd El Mohsen et al. (2002) |
| 2 | Pelargonidin | Rat | Oral | 50 mg/kg BW | 1 day | 2 h and 18 h after PP intake | Pentobarbitone | Perfusion | El Mohsen et al. (2006) |
| 3 | Grape seed extract | Rat | Oral | 300 mg/kg BW (twice daily) | 3 days | 4 h after last PP intake | Isoflurane | Cervical dislocation and heart puncture followed by perfusion | Prasain et al. (2009) |
| 4 | Grape seed extract | Rat | Oral | Dose-escalating design | 10 days | 8 h after last administration | – | Plasma: Collected from jugular vein (catheter) Brain: Perfusion |
Ferruzzi et al. (2009) |
| Days 1–2: 50 mg/kg BW | |||||||||
| Days 3–4: 100 mg/kg BW | |||||||||
| Days 5–10: 150 mg/kg BW | |||||||||
| 5 | Blackberry extract | Rat | Oral | 15 g/kg diet (with 14.8 mmol anthocyanins/kg diet) | 15 days | 3 h after last meal | Pentobarbital | Blood: All blood drawn from abdominal aorta Brain: removed from bloodless animals |
Talavera et al. (2005) |
| 6 | Epigallo catechin-3-gallate | Rat | Oral | 500 mg/kg BW | 1 day | 1 h after administration | Ether | Blood: Collected from abdominal artery Brain: Perfusion |
Nakagawa and Miyazawa (1997) |
| 7 | Quercetin | Rat | Oral | 1% w/w | 1 month | No details given | Pentobarbital | Blood: – Brain: Perfusion |
Ishisaka et al. (2011) |
| Section II: studies correcting for residual blood | |||||||||
| 8 | Quercetin | Rat | Oral | 0.1% in diet | 11 weeks | Morning w/out overnight fasting | Isoflurane | Full bleeding from aorta | de Boer et al. (2005) |
| 9 | Quercetin | Pig | Oral | 500 mg/kg BW | 3 days | Fasting for 8 h | No details given | No details given | |
BW body weight
Table 2.
PPs concentrations in plasma and animal brain obtained from studies using either exsanguinated and perfused animals or correcting for residual blood by other means
| No. | PP measured | Plasma conc. | Correction achieved by | Brain conc. corrected | References |
|---|---|---|---|---|---|
| Section I: studies in exsanguinated and perfused animals | |||||
| 1 | Epicatechin metabolites (total) | 66 uM | Perfusion | 0.4 nmol/g tissue (estimated) | Abd El Mohsen et al. (2002) |
| 2 | Pelargonidin metabolites (total) | 2 h: ~1.5 uM | Perfusion | 2 h: 0.16 nmol/g tissue [43 ng/g] | El Mohsen et al. (2006) |
| 18 h: ~0.65 uM | 18 h: <LOD | ||||
| 3 | (+)-Catechin | <LOD | Perfusion | 53 ng/g tissue | Prasain et al. (2009) |
| 4 | Catechin | 1.98 ug/ml | Perfusion | 0.57 ng/g tissue | Ferruzzi et al. (2009) |
| Epicatechin | 3.86 ug/ml | 0.29 ng/g tissue | |||
| 5 | Cyanidin-3-glucoside | 0.15 uM | Blood-less animals used; no explicit information on brain perfusion | 0.21 nmol/g tissue | Talavera et al. (2005) |
| 6 | Epigallocatechin-3-gallate | 12.3 uM | Perfusion | 0.5 nmol/g tissue | Nakagawa and Miyazawa (1997) |
| 7 | Quercetin | No details given | Perfusion | 40.1 pmol/g tissue | Ishisaka et al. (2011) |
| Section II: studies correcting for residual blood | |||||
| 8 | Quercetin | 7.7 umol/l | Hb method | <LOD | de Boer et al. (2005) |
| Isorhamnetin | 15.7 umol/l | 0.19 nmol/g tissue | |||
| Tamarixetin | <LOD | 0.14 nmol/g tissue | |||
| 9 | Quercetin | 1.1 umol/l | Hb methods | 0.22 nmol/g tissue | |
| Isorhamnetin | 0.15 umol/l | <LOD | |||
| Tamarixetin | <LOD | <LOD | |||
LOD limit of detection
In order to assess the magnitude of residual blood as a confounder in the quantification of brain PP concentrations, we applied a recently published mathematical correction model to one study, as an example (Friden et al. 2010). The limitation of this approach, however, is that studies only qualify for re-analysis when the mode of animal anaesthesia and killing ideally follow those published by Friden et al. (Table 3). In this case, the model can also be applied to other rodents, for example, mice (M. Friden, personal communication). The latter proposition is supported by a previous study reporting similar residual blood content (in per cent) for various rat and mouse organs (Schumann et al. 2007). Unfortunately, none of the studies on brain PP penetration available to us for evaluation strictly adhered to the above-mentioned criteria for re-analysis due to differences in the method of euthanasia and tissue sampling. However, as also mentioned by Friden et al. (2010), exsanguination by severing the heart seemed to result in less residual blood in rat brain compared to brain obtained from decapitated animals. Based on this notion, applying the correction model to studies where more residual blood in the brain samples will likely occur (as a result of the sampling procedure) can be considered conservative and will in most cases presumably still overestimate the amount of PP in the brain sample. Despite the above-mentioned limitations, we suggest that our approach highlights the often underappreciated problem of confounded levels of PPs in brain tissue reported in the scientific literature.
Table 3.
Anaesthesia and tissue collection procedure prior analysis of brain drug concentrations and their mathematical correction as published in Friden et al. (2010)
| Step | Procedure |
|---|---|
| 1 | Anaesthesia with isoflurane |
| 2 | Collection of blood sample from abdominal aorta (2 mL) for analysis |
| 3 | Exsanguination by severing the heart |
| 4 | Removal of brain, taking of coronal section for analysis |
In the study selected for re-assessment, female mice (6–7 weeks old) were fed a PP-poor, semi-synthetic diet supplemented with quercetin (2 g/kg diet) for 6 weeks (Huebbe et al. 2010). The brain concentrations of quercetin and its metabolite, isorhamnetin, at baseline and at the end of the intervention for both control and supplemented animals are depicted in Fig. 2. The results of the mathematical correction model indicate that the actual amounts of brain quercetin and isorhamnetin in supplemented mice are about 8 and 27% lower, respectively, whereas values for control animals remained unchanged. Although only of moderate magnitude, the corrected values for brain PPs, especially of isorhamnetin, suggest that residual blood might confound supplementation studies aiming to quantify the enrichment of PPs in brain beyond baseline data. Somewhat surprising are the high baseline levels of quercetin in the brain of control animals despite the low quercetin concentrations (0.12 μM) in blood. The authors provided two possible explanations for this observation: (1) the transfer of quercetin from the mothers to their offspring during the intrauterine development and (2) the uptake of quercetin (and its subsequent accumulation in the brain) from a standard feed (Huebbe et al. 2010). Although it is still difficult to say from current data whether some PPs not only accumulate but also persist (as the quercetin data for the control animals suggest) in specific target organs for longer periods of time, data published for other bioactive compounds, in particular the naturally occurring amino acid ergothioneine, are consistent with this notion (Cheah and Halliwell 2011).
Fig. 2.
Effect of mathematical correction for residual blood on the published concentrations of quercetin (OU) and isorhamnetin (IsoR) in the brain of quercetin-supplemented mice (Huebbe et al. 2010). For details see text
Nonetheless, results from the aforementioned mouse study (Huebbe et al. 2010) in combination with those reports listed in Table 2 provide reasonable evidence that PPs do enter the brain at measurable levels. An additional important parameter affecting the correction for residual blood and subsequently the uptake of drug into brain is protein binding (Friden et al. 2010). For example, Diniz et al. (2008) observed significant, structure-dependent differences in the binding behaviours of PPs to plasma proteins, ranging from more than 90% human serum albumin (HSA) binding affinity for PPs such as apigenin and quercetin to below 10% as, e.g., in the case of epicatechin. Noteworthy, plasma fatty acids allosterically inhibit PP binding to HSA (Bolli et al. 2010), suggesting that dietary factors might modulate PP plasma, and subsequently, tissue distribution. The accuracy of PP quantification in brain, of course, also significantly depends on other parameters, such as PP extraction efficiency from the tissue as well as on the applied analytical method (Wilkinson et al. 2002).
Does it matter that polyphenols can enter the brain?
Classically, PPs are considered as potent antioxidants due to their ability to directly scavenge free radicals and other reactive species (RS, for details see Halliwell 2006) in vitro (Pannala et al. 1997; Russo et al. 2000; Visioli et al. 1998) and perhaps sometimes also in vivo. Given the brain’s vulnerability to oxidative and nitrosative stress, the sufficient supply of the CNS with antioxidants is of prime importance (Halliwell 2006; Reiter 1995).
In the following, we compare the ability of PPs to act as brain antioxidants with ascorbic acid (AA, vitamin C) one of the most abundant low-molecular-mass antioxidants in the mammalian brain (Rice 2000). AA levels of about 2,000 nmol/g tissue have been measured, for instance, in the brain of perfused, male Wistar rats (Sun et al. 1999). Some caution has to be taken when conducting vitamin C studies in rats and mice (both rodent species not only possess a much higher neuron density per mm3 than humans—and consequently greater AA content per g brain tissue—but are also able to synthesize their own vitamin C, unlike humans who depend on a dietary AA supply). Nevertheless, rat brain AA levels are in a similar range to those reported for guinea pigs, which need vitamin C from the diet (about 1,500 nmol/g tissue; perfused animals Lykkesfeldt et al. 2007), but are (as expected) higher than in humans (about 600–900 nmol/g tissue) (Rice 2000; Terpstra et al. 2011). Compared to PPs (for details see Table 2), AA brain concentrations of perfused laboratory rodents are thus about 3,000–4,000 times higher, making it rather unlikely that PPs, even when considering their several fold higher in vitro antioxidant activity (Rice-Evans et al. 1995; Schaffer et al. 2004), exert appreciable direct RS-scavenging effects in the mammalian brain, unless they act in different compartments, e.g. lipids, depending on their solubility in lipophilic and hydrophilic environments.
Furthermore, the question of whether compounds such as AA and PPs are active within the CNS also depends on their compartmentalization between the cerebrospinal fluid (CSF), extracellular fluid (ECF) and the different types of brain cells. Concentrations of AA are highest in neurons (~10 mM), followed by glial cells (~1 mM), CSF (~500 μM) and ECF (200–400 μM) (Rice 2000). Our knowledge of PP compartmentalization within the CNS, on the other hand, is rather scarce. Data from in vitro studies, however, might serve as a first approximation. First of all, there is now good evidence from cell culture experiments that PPs are able to enter at least some cell types (Ernst et al. 2010; Watjen et al. 2005), and in a few studies, actual PP uptake has been quantified (Table 4). Assuming an average cell volume of 22 × 10−13 l [=22 picolitres, based on cell volume data for HepG2 cells of 12.1 × 10−13 l, PC12 cells of 20.5 × 10−13 l and cardiac myocytes of 33.4 × 10−13 l (Atkins et al. 1991; Leung et al. 1994; Wehner et al. 2002)], an estimated quercetin uptake of 20 nmol/106 cells would result in an intracellular quercetin concentration of 9 mM. This, however, would require the extracellular presence of PPs at un-physiological concentrations of a few hundred micromolar (Table 4). As there is currently no evidence that CSF and ECF concentrations of PPs exceed 1–5 micromolar (at best), it is thus highly unlikely that intracellular PP concentrations in neurons and glial cells will exceed the very low micromolar to nanomolar range. This, clearly, is not sufficient for exerting any appreciable direct antioxidant effect (compared, e.g., to vitamin C and glutathione)—but might still be high enough to modulate other cellular parameters in the CNS (see below).
Table 4.
Cellular uptake of PPs reported for different cell lines
| PP | Test conc. (μM) | Incubation time | Cell line | Intracellular conc. | Study |
|---|---|---|---|---|---|
| Apigenin | 50 | 2 h | Caco-2 | ~1.2 nmol/mg protein | Yokomizo and Moriwaki (2006)a |
| Kaempferol | ~1.8 nmol/mg protein | ||||
| Luteolin | ~1.3 nmol/mg protein | ||||
| Quercetin | ~0.9 nmol/mg protein | ||||
| Myricetin | ND | ||||
| Myricetrin | ND | ||||
| Rutin | ND | ||||
| Isoquercitrin | ND | ||||
| Quercetin | 500 | 1 h | H4IIE | 33.4 nmol/106 cells | Watjen et al. (2005) |
| Fisetin | 12.67 nmol/106 cells | ||||
| Myricetin | 0.22 nmol/106 cells | ||||
| Morin | 2.35 nmol/106 cells | ||||
| Taxifolin | 0.2 nmol/106 cells | ||||
| Rutin | 0 | ||||
| Catechin | 0 | ||||
| EC | 50 | 1 h | Caco-2 | 0 | Vaidyanathan and Walle (2003)a |
| (+)-Catechin | ~150 pmol/mg protein | ||||
| ECG | ~3,000 pmol/mg protein | ||||
| EGCG | ~2,400 pmol/mg protein | ||||
| Quercetin | 5 | 30 min | HepG2 | ~900 pmol/mg protein | Boulton et al. (1999)a |
ND not detected
PP polyphenols
aData were estimated from graphs
Direct antioxidant effects of PPs are thus not very likely in the brain in vivo, nor are there any literature data we are aware of measuring accurate biomarkers of oxidative damage that show that PPs have direct antioxidant effects in the brain. We ought to consider the absence of evidence as evidence of absence for direct RS-scavenging activities of PPs in animals and humans, especially as PPs levels in vivo are likely too low to matter in the face of endogenous antioxidants (Halliwell and Gutteridge 2007).
How, then, can we explain the several studies reporting positive effects for PPs on brain function? One research field attracting more and more attention is the modulation of monoaminergic and GABA neurotransmission by PPs. The treatment of rats with PP-rich Ginkgo biloba extract for 14 days, for example, resulted in significantly increased extracellular levels of dopamine and noradrenaline (but not of serotonin) in the animals’ prefrontal cortex (Yoshitake et al. 2010). Of the three main Ginkgo biloba extract constituents, the PP (flavonoid) fraction caused a significant (and most pronounced) increase in brain dopamine levels, whereas ginkgolides had only a moderate and bilobalides no effect (Yoshitake et al. 2010). The observed effects appear not to depend on the activity of monoamine oxidases (MAO-A and MAO-B) as these were unchanged in mice chronically treated with the extract (Fehske et al. 2009). The low concentration of PPs in brain (Table 2) compared to the Ki values, for instance, of quercetin for MAO-A of 7.26 μM and for MAO-B of 7.95 μM (Dixon Clarke and Ramsay 2011) suggests that other parameters, such as neurotransmitter re-uptake mechanisms, might be involved in the modulation of monoaminergic neurotransmission by PPs (Fehske et al. 2009; Ofir et al. 2003). Mood and behavioural disorders often arise from a dysfunctional neurotransmission and thus might benefit from drug-induced alterations in the amount of available neurotransmitters within the CNS (Racagni and Popoli 2010). Neurotransmitter re-uptake inhibition in synaptosomal preparations has been reported for some PPs and PP-rich plant extract fractions (e.g. resveratrol, catechin or Ginkgo flavonoids) but not others (e.g. kaempferol) (Muller et al. 1998; Rocha et al. 2007; Yanez et al. 2006). Similarly, a plethora of in vitro data indicates that PPs act as modulators of the GABAA-benzodiazepine receptor. Whereas the Ki values for the affinity of many PPs to the receptor is in the one-digit to two-digit micromolar range, some PPs are effective at lower (and maybe physiologically achievable) concentrations, such as amentoflavone with reported Ki values of 6–56 nM (Jager and Saaby 2011). Much more work, however, needs to be done in order to understand whether the same PP actions on GABAA receptors occur in vivo and, even more challenging, by what mechanism (Hanrahan et al. 2011; Jager and Saaby 2011).
Based on today’s knowledge, other promising explanations of the possible brain effects of PPs are also indirect in nature: (1) the activation of a hormetic dose-response and (2) effects on peripheral systems of the body, which in turn influence CNS functioning.
Hormesis describes a process in which exposure to a low dose of an agent that is toxic at higher doses induces a beneficial effect on the cell or organism (Mattson and Cheng 2006). Whereas most studies describing hormetic effects for PPs have been performed in cell culture or the nematode C. elegans (Ali and Rattan 2006; Gruber et al. 2007; Pietsch et al. 2011; Wagner et al. 2011), recently, the first direct evidence for hormesis induction in vivo has been reported in mammals. Pretreatment of mice with the PP epicatechin significantly reduced the negative impact of stroke induction in wild-type but not Nrf2 knock-out animals (Shah et al. 2010). As the transcription factor Nrf2 is one of the key regulators responsible for the induction of antioxidant and cell protective genes, this study suggests that PPs might indeed operate by hormesis activation. One caveat affecting the evaluation of hormetic phenomena, however, needs to be considered based on ontogenetic studies, i.e. that a subject’s developmental stage might influence the magnitude of an observed hormetic response. For example, the U-shaped effects of acute ethanol exposure on overall social activity of rats are not only influenced by the measuring time post-exposure but are also strongly age-dependent (Spear and Varlinskaya 2005). Similarly, changes in the penetration efficiency of substances due to the disruption of the blood–brain barrier, for example in stroke (Cipolla et al. 2004), might shift the dose-response away from reference values, posing either the risk of unexpected side effects or the possibility for an improved therapeutic outcome. Some authors also noted the lack of a precise definition of hormesis and furthermore pointed out that the evaluation of a hormetic response in terms of possible health effects must be carefully studied as compounds, even at low dose, might exert significant beneficial or detrimental effects on physiological and cellular mechanisms, which are often non-linear and chaotic in nature, such as coronary circulation, neuronal signalling or calcium oscillation (Chirumbolo 2011; Clay and Shrier 1999; Haberichter et al. 2001; Trzeciakowski and Chilian 2008). The perturbing impact of PPs at concentrations as low as 1 μM on cellular signalling pathways and metabolic processes has been demonstrated, for example, for PP-dependent effects on mitochondrial calcium uptake and on the activity of protein kinase C (Kalfon et al. 2007; Montero et al. 2004). Note that there is currently a trend of moving away from studying PP parent compounds and towards the assessment of biological activities exerted by PP metabolites and degradation products. Several extensive reviews regarding the consequences of PPs and their metabolites on cellular mechanisms are available (Lau et al. 2005; Manach et al. 2004; Spencer et al. 2004, 2007; Visioli et al. 2011), although the overall picture remains somewhat diffuse given the impressive number of signalling pathways shown to be affected. Whereas little is known about the in vivo effects of PP metabolites and degradation products on the brain, evidence from some studies indicates that these compounds might also enter the CNS, although usually at a very low level (Abd El Mohsen et al. 2002; Ferruzzi et al. 2009; Huebbe et al. 2010).
However, many activities of PPs have, so far, only been demonstrated in cell culture studies, which are prone to artefacts (Halliwell 2003). Upon exposure to standard cell culture media (e.g. DMEM, MEM or RPMI), many PPs become degraded and, at the same time, initiate the production of hydrogen peroxide in the one-digit to three-digit micromolar range (Long et al. 2010; Schaffer and Halliwell 2011). Common medium supplements (such as pyruvate) or excreted cellular metabolites (for instance α-ketoglutarate) effectively scavenge PP-derived hydrogen peroxide and thus become depleted, which can affect results where pyruvate or α-ketoglutarate are important growth factors to the cells being cultured (Long and Halliwell 2009, 2011). Hence, careful thought is essential when elucidating the in vivo mode of PP action and subsequently their possible areas of preventive or therapeutic application in humans.
Furthermore, the regulation of brain integrity and function must not be seen in isolation but as strongly dependent on feedback information (in the form of hormones, nutrients, metabolites and, of course, sensory neuron signalling) of the body periphery. In addition, mainly physico-mechanical parameters, such as the amount of blood supplied to the brain, are important factors to consider when assessing CNS effects of patho-physiological events and preventive/therapeutic interventions (e.g. drugs and diet). Endothelial dysfunction, for example, is associated with reduced cerebral perfusion and the occurrence of dementia (Ghosh and Scheepens 2009). Reasonable evidence exists that PPs from cocoa (Francis et al. 2006; Heiss et al. 2007; Heiss et al. 2010) and other dietary sources, such as tea (Grassi et al. 2009) and grapes (Lekakis et al. 2005), increase blood flow in humans, thus possibly helping to provide the brain with greater amounts of oxygen and glucose. Negative studies, however, have also been published on this topic (Auclair et al. 2010; van Mierlo et al. 2010). A recurrent observation in many studies assessing the effect of bioactive compounds (PPs, phytochemicals and plant extracts) is the strong impact of age and health status on the study outcome. Several clinical trials indicate that young- to middle-aged healthy human subjects often do not benefit from the intake of bioactive compounds when applied in the form of antioxidant supplements or antioxidant-enriched foods (Boots et al. 2008; Canter and Ernst 2007; Kelly et al. 2008; Lee et al. 2009). Also, older humans suffering from advanced stages of chronic diseases (such as Alzheimer’s disease) reveal negligible or zero therapeutic effects when the patients are treated with PPs or other phytochemicals (Daviglus et al. 2010; Lloret et al. 2009; Quinn et al. 2010). Thus, clearly more work is needed in order to identify the optimal time frame for preventive and therapeutic interventions in humans, probably not too young and not when disease has progressed to an advanced stage.
Another example highlighting the impact that peripheral organs can exert on brain (mal)function is metabolic signalling by the gastro-intestinal tract (GIT). Compared to blood, dietary PPs can be present in high amounts in the GIT and could even exert direct antioxidant effects there, e.g. in the stomach (Halliwell et al. 2000, 2005; Kanner and Lapidot 2001). Some PPs also reach the colon (Jenner et al. 2005; van Duynhoven et al. 2011). In the past 5–10 years, exciting new information regarding health implications of the brain-gut-enteric microbiota axis has emerged (Rhee et al. 2009). Whereas some aspects of this bidirectional interaction are well established, for instance the effect of mucosal inflammation on pain reception, effects of gut microbiota on other CNS-regulated phenomena such as mood changes or anxious behaviour have only recently been described (Forsythe et al. 2010; Rhee et al. 2009). A new study by Heijtz et al. (2011) emphasizes the importance of gut microbiota for brain development and behaviour. When comparing specific pathogen-free with germ-free mice, the authors found significant differences in motor control and anxiety-like behaviour between the two mouse groups, possibly indicating that evolution might have driven the link between gut microbiota and brain development. As PPs strongly affect both composition and metabolism of the intestinal microbiota, it is possible that this interaction might exert effects not only on the GIT but also indirectly on the brain, especially when considering that luminal microorganisms (about 1011 bacterial cells per gram colon content) represent 100 times the total genetic material contained in a human body, thus allowing for a stunning production of a wide range of metabolites (Forsythe et al. 2010; Rhee et al. 2009). Most of the biological activities that these microbial metabolites exert on the human body, and especially the brain, are currently unknown, but they might soon be revolutionizing how we look at human health and disease.
In conclusion, what does the scientific community need to do with respect to PP research? We propose two adjustments: (1) the development of more sophisticated analytical methods to establish levels of PPs and their metabolites to confirm the view that direct effects on brain cells and tissue are likely or unlikely and (2) a significant spike in non-reductionist research efforts for elucidating bi- and even multi-directional inter-organ actions and reactions, especially between peripheral organs and the brain, which are too often studied in isolation. Furthermore, in order to master the likely overwhelming amount of data associated with such complex research agendas, experimental research should ideally go hand-in-hand with systems biology (Assmus et al. 2006; Desiere 2004; Lemberger 2007). Only then, we predict, will the biomedical research community be able to significantly advance our understanding of the effects of PPs as external and internal determinants of human health and disease.
Acknowledgments
BH is most grateful for the financial support provided by the Tan Chin Tuan Centennial Fund, Singapore.
References
- Abd El Mohsen MM, Kuhnle G, Rechner AR, et al. Uptake and metabolism of epicatechin and its access to the brain after oral ingestion. Free Radic Biol Med. 2002;33:1693–1702. doi: 10.1016/s0891-5849(02)01137-1. [DOI] [PubMed] [Google Scholar]
- Ali RE, Rattan SI. Curcumin’s biphasic hormetic response on proteasome activity and heat-shock protein synthesis in human keratinocytes. Ann NY Acad Sci. 2006;1067:394–399. doi: 10.1196/annals.1354.056. [DOI] [PubMed] [Google Scholar]
- Andres-Lacueva C, Shukitt-Hale B, Galli RL, et al. Anthocyanins in aged blueberry-fed rats are found centrally and may enhance memory. Nutr Neurosci. 2005;8:111–120. doi: 10.1080/10284150500078117. [DOI] [PubMed] [Google Scholar]
- Assmus HE, Herwig R, Cho KH, et al. Dynamics of biological systems: role of systems biology in medical research. Expert Rev Mol Diagn. 2006;6:891–902. doi: 10.1586/14737159.6.6.891. [DOI] [PubMed] [Google Scholar]
- Atkins DL, Rosenthal JK, Krumm PA, et al. Application of stereological analysis of cell volume to isolated myocytes in culture with and without adrenergic innervation. Anat Rec. 1991;231:209–217. doi: 10.1002/ar.1092310209. [DOI] [PubMed] [Google Scholar]
- Auclair S, Chironi G, Milenkovic D, et al. The regular consumption of a polyphenol-rich apple does not influence endothelial function: a randomised double-blind trial in hypercholesterolemic adults. Eur J Clin Nutr. 2010;64:1158–1165. doi: 10.1038/ejcn.2010.135. [DOI] [PubMed] [Google Scholar]
- Bolli A, Marino M, Rimbach G, et al. Flavonoid binding to human serum albumin. Biochem Biophys Res Commun. 2010;398:444–449. doi: 10.1016/j.bbrc.2010.06.096. [DOI] [PubMed] [Google Scholar]
- Boots AW, Wilms LC, Swennen EL, et al. In vitro and ex vivo anti-inflammatory activity of quercetin in healthy volunteers. Nutrition. 2008;24:703–710. doi: 10.1016/j.nut.2008.03.023. [DOI] [PubMed] [Google Scholar]
- Boulton DW, Walle UK, Walle T. Fate of the flavonoid quercetin in human cell lines: chemical instability and metabolism. J Pharm Pharmacol. 1999;51:353–359. doi: 10.1211/0022357991772367. [DOI] [PubMed] [Google Scholar]
- Canter PH, Ernst E. Ginkgo biloba is not a smart drug: an updated systematic review of randomised clinical trials testing the nootropic effects of G. biloba extracts in healthy people. Hum Psychopharmacol. 2007;22:265–278. doi: 10.1002/hup.843. [DOI] [PubMed] [Google Scholar]
- Chang HC, Churchwell MI, Delclos KB, et al. Mass spectrometric determination of Genistein tissue distribution in diet-exposed Sprague-Dawley rats. J Nutr. 2000;130:1963–1970. doi: 10.1093/jn/130.8.1963. [DOI] [PubMed] [Google Scholar]
- Cheah IK, Halliwell B (2011) Ergothioneine: antioxidant potential, physiological function and role in disease. Biochim Biophys Acta. doi:10.1016/j.bbadis.2011.09.017 [DOI] [PubMed]
- Chirumbolo S (2011) Hormesis, resveratrol and plant-derived polyphenols: some comments. Hum Exp Toxicol. doi:10.1177/0960327111408153 [DOI] [PubMed]
- Cipolla MJ, Crete R, Vitullo L, et al. Transcellular transport as a mechanism of blood-brain barrier disruption during stroke. Front Biosci. 2004;9:777–785. doi: 10.2741/1282. [DOI] [PubMed] [Google Scholar]
- Clay JR, Shrier A. On the role of subthreshold dynamics in neuronal signaling. J Theor Biol. 1999;197:207–216. doi: 10.1006/jtbi.1998.0867. [DOI] [PubMed] [Google Scholar]
- Commenges D, Scotet V, Renaud S, et al. Intake of flavonoids and risk of dementia. Eur J Epidemiol. 2000;16:357–363. doi: 10.1023/a:1007614613771. [DOI] [PubMed] [Google Scholar]
- Datla KP, Christidou M, Widmer WW, et al. Tissue distribution and neuroprotective effects of citrus flavonoid tangeretin in a rat model of Parkinson’s disease. Neuroreport. 2001;12:3871–3875. doi: 10.1097/00001756-200112040-00053. [DOI] [PubMed] [Google Scholar]
- Daviglus ML, Bell CC, Berrettini W et al (2010) NIH State-of-the-science conference statement: preventing Alzheimer’s disease and cognitive decline. NIH Consens State Sci Statements 27 [PubMed]
- de Boer VC, Dihal AA, van der Woude H, Arts IC, Wolffram S, Alink GM, Rietjens IM, Keijer J, Hollman PC (2005) Tissue distribution of quercetin in rats and pigs. J Nutr 135:1718–1725 [DOI] [PubMed]
- Desiere F. Towards a systems biology understanding of human health: interplay between genotype, environment and nutrition. Biotechnol Annu Rev. 2004;10:51–84. doi: 10.1016/S1387-2656(04)10003-3. [DOI] [PubMed] [Google Scholar]
- Diniz A, Escuder-Gilabert L, Lopes NP, et al. Characterization of interactions between polyphenolic compounds and human serum proteins by capillary electrophoresis. Anal Bioanal Chem. 2008;391:625–632. doi: 10.1007/s00216-008-2046-4. [DOI] [PubMed] [Google Scholar]
- Dixon Clarke SE, Ramsay RR. Dietary inhibitors of monoamine oxidase A. J Neural Transm. 2011;118:1031–1041. doi: 10.1007/s00702-010-0537-x. [DOI] [PubMed] [Google Scholar]
- El Mohsen MA, Marks J, Kuhnle G, et al. Absorption, tissue distribution and excretion of pelargonidin and its metabolites following oral administration to rats. Br J Nutr. 2006;95:51–58. doi: 10.1079/bjn20051596. [DOI] [PubMed] [Google Scholar]
- Ernst IM, Wagner AE, Lipinski S, et al. Cellular uptake, stability, visualization by ‘Naturstoff reagent A’, and multidrug resistance protein 1 gene-regulatory activity of cyanidin in human keratinocytes. Pharmacol Res. 2010;61:253–258. doi: 10.1016/j.phrs.2009.10.006. [DOI] [PubMed] [Google Scholar]
- Fehske CJ, Leuner K, Muller WE. Ginkgo biloba extract (EGb761) influences monoaminergic neurotransmission via inhibition of NE uptake, but not MAO activity after chronic treatment. Pharmacol Res. 2009;60:68–73. doi: 10.1016/j.phrs.2009.02.012. [DOI] [PubMed] [Google Scholar]
- Ferruzzi MG, Lobo JK, Janle EM, et al. Bioavailability of gallic acid and catechins from grape seed polyphenol extract is improved by repeated dosing in rats: implications for treatment in Alzheimer’s disease. J Alzheimers Dis. 2009;18:113–124. doi: 10.3233/JAD-2009-1135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forsythe P, Sudo N, Dinan T, et al. Mood and gut feelings. Brain Behav Immun. 2010;24:9–16. doi: 10.1016/j.bbi.2009.05.058. [DOI] [PubMed] [Google Scholar]
- Francis ST, Head K, Morris PG, et al. The effect of flavanol-rich cocoa on the fMRI response to a cognitive task in healthy young people. J Cardiovasc Pharmacol. 2006;47(Suppl 2):S215-20–S215-S220. doi: 10.1097/00005344-200606001-00018. [DOI] [PubMed] [Google Scholar]
- Friden M, Ljungqvist H, Middleton B, et al. Improved measurement of drug exposure in the brain using drug-specific correction for residual blood. J Cereb Blood Flow Metab. 2010;30:150–161. doi: 10.1038/jcbfm.2009.200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghosh D, Scheepens A. Vascular action of polyphenols. Mol Nutr Food Res. 2009;53:322–331. doi: 10.1002/mnfr.200800182. [DOI] [PubMed] [Google Scholar]
- Grassi D, Mulder TP, Draijer R, et al. Black tea consumption dose-dependently improves flow-mediated dilation in healthy males. J Hypertens. 2009;27:774–781. doi: 10.1097/HJH.0b013e328326066c. [DOI] [PubMed] [Google Scholar]
- Gruber J, Tang SY, Halliwell B. Evidence for a trade-off between survival and fitness caused by resveratrol treatment of Caenorhabditis elegans. Ann NY Acad Sci. 2007;1100:530–542. doi: 10.1196/annals.1395.059. [DOI] [PubMed] [Google Scholar]
- Haberichter T, Marhl M, Heinrich R. Birhythmicity, trirhythmicity and chaos in bursting calcium oscillations. Biophys Chem. 2001;90:17–30. doi: 10.1016/s0301-4622(01)00127-2. [DOI] [PubMed] [Google Scholar]
- Halliwell B. Oxidative stress in cell culture: an under-appreciated problem? FEBS Lett. 2003;540:3–6. doi: 10.1016/s0014-5793(03)00235-7. [DOI] [PubMed] [Google Scholar]
- Halliwell B. Oxidative stress and neurodegeneration: where are we now? J Neurochem. 2006;97:1634–1658. doi: 10.1111/j.1471-4159.2006.03907.x. [DOI] [PubMed] [Google Scholar]
- Halliwell B. Dietary polyphenols: good, bad, or indifferent for your health? Cardiovasc Res. 2007;73:341–347. doi: 10.1016/j.cardiores.2006.10.004. [DOI] [PubMed] [Google Scholar]
- Halliwell B (2007b) Flavonoids: a re-run of the carotenoids story? Novartis Found Symp 282:93–101 (discussion 101-4, 212-8:93–101) [DOI] [PubMed]
- Halliwell B, Gutteridge J. Free radicals in biology and medicine. Oxford: Oxford University Press; 2007. [Google Scholar]
- Halliwell B, Zhao K, Whiteman M. The gastrointestinal tract: a major site of antioxidant action? Free Radic Res. 2000;33:819–830. doi: 10.1080/10715760000301341. [DOI] [PubMed] [Google Scholar]
- Halliwell B, Rafter J, Jenner A. Health promotion by flavonoids, tocopherols, tocotrienols, and other phenols: direct or indirect effects? Antioxidant or not? Am J Clin Nutr. 2005;81:268S–276S. doi: 10.1093/ajcn/81.1.268S. [DOI] [PubMed] [Google Scholar]
- Hanrahan JR, Chebib M, Johnston GA. Flavonoid modulation of GABA(A) receptors. Br J Pharmacol. 2011;163:234–245. doi: 10.1111/j.1476-5381.2011.01228.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heijtz RD, Wang S, Anuar F, et al. Normal gut microbiota modulates brain development and behavior. Proc Natl Acad Sci USA. 2011;108:3047–3052. doi: 10.1073/pnas.1010529108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heiss C, Finis D, Kleinbongard P, et al. Sustained increase in flow-mediated dilation after daily intake of high-flavanol cocoa drink over 1 week. J Cardiovasc Pharmacol. 2007;49:74–80. doi: 10.1097/FJC.0b013e31802d0001. [DOI] [PubMed] [Google Scholar]
- Heiss C, Jahn S, Taylor M, et al. Improvement of endothelial function with dietary flavanols is associated with mobilization of circulating angiogenic cells in patients with coronary artery disease. J Am Coll Cardiol. 2010;56:218–224. doi: 10.1016/j.jacc.2010.03.039. [DOI] [PubMed] [Google Scholar]
- Hollman PC, Cassidy A, Comte B, et al. The biological relevance of direct antioxidant effects of polyphenols for cardiovascular health in humans is not established. J Nutr. 2011;141:989S–1009S. doi: 10.3945/jn.110.131490. [DOI] [PubMed] [Google Scholar]
- Hu M. Commentary: bioavailability of flavonoids and polyphenols: call to arms. Mol Pharm. 2007;4:803–806. doi: 10.1021/mp7001363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huebbe P, Wagner AE, Boesch-Saadatmandi C, et al. Effect of dietary quercetin on brain quercetin levels and the expression of antioxidant and Alzheimer’s disease relevant genes in mice. Pharmacol Res. 2010;61:242–246. doi: 10.1016/j.phrs.2009.08.006. [DOI] [PubMed] [Google Scholar]
- Ishisaka A, Ichikawa S, Sakakibara H et al (2011) Accumulation of orally administered quercetin in brain tissue and its antioxidative effects in rats. Free Radic Biol Med 51:1329–1336 [DOI] [PubMed]
- Jager AK, Saaby L. Flavonoids and the CNS. Molecules. 2011;16:1471–1485. doi: 10.3390/molecules16021471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Janle EM, Lila MA, Grannan M, et al. Pharmacokinetics and tissue distribution of 14C-labeled grape polyphenols in the periphery and the central nervous system following oral administration. J Med Food. 2010;13:926–933. doi: 10.1089/jmf.2009.0157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jenner AM, Rafter J, Halliwell B. Human fecal water content of phenolics: the extent of colonic exposure to aromatic compounds. Free Radic Biol Med. 2005;38:763–772. doi: 10.1016/j.freeradbiomed.2004.11.020. [DOI] [PubMed] [Google Scholar]
- Kalfon L, Youdim MB, Mandel SA. Green tea polyphenol (−)-epigallocatechin-3-gallate promotes the rapid protein kinase C—and proteasome-mediated degradation of Bad: implications for neuroprotection. J Neurochem. 2007;100:992–1002. doi: 10.1111/j.1471-4159.2006.04265.x. [DOI] [PubMed] [Google Scholar]
- Kanner J, Lapidot T. The stomach as a bioreactor: dietary lipid peroxidation in the gastric fluid and the effects of plant-derived antioxidants. Free Radic Biol Med. 2001;31:1388–1395. doi: 10.1016/s0891-5849(01)00718-3. [DOI] [PubMed] [Google Scholar]
- Kelly RP, Poo YK, Isaac HB, et al. Lack of effect of acute oral ingestion of vitamin C on oxidative stress, arterial stiffness or blood pressure in healthy subjects. Free Radic Res. 2008;42:514–522. doi: 10.1080/10715760802087431. [DOI] [PubMed] [Google Scholar]
- Lau FC, Shukitt-Hale B, Joseph JA. The beneficial effects of fruit polyphenols on brain aging. Neurobiol Aging. 2005;26(Suppl 1):128–132. doi: 10.1016/j.neurobiolaging.2005.08.007. [DOI] [PubMed] [Google Scholar]
- Lee CY, Isaac HB, Huang SH, et al. Limited antioxidant effect after consumption of a single dose of tomato sauce by young males, despite a rise in plasma lycopene. Free Radic Res. 2009;43:622–628. doi: 10.1080/10715760902942816. [DOI] [PubMed] [Google Scholar]
- Lekakis J, Rallidis LS, Andreadou I, et al. Polyphenolic compounds from red grapes acutely improve endothelial function in patients with coronary heart disease. Eur J Cardiovasc Prev Rehabil. 2005;12:596–600. doi: 10.1097/00149831-200512000-00013. [DOI] [PubMed] [Google Scholar]
- Lemberger T. Systems biology in human health and disease. Mol Syst Biol. 2007;3:136. doi: 10.1038/msb4100175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Letenneur L, Proust-Lima C, Gouge A, et al. Flavonoid intake and cognitive decline over a 10-year period. Am J Epidemiol. 2007;165:1364–1371. doi: 10.1093/aje/kwm036. [DOI] [PubMed] [Google Scholar]
- Leung S, O’Donnell ME, Martinez A, et al. Regulation by nerve growth factor and protein phosphorylation of Na/K/2Cl cotransport and cell volume in PC12 cells. J Biol Chem. 1994;269:10581–10589. [PubMed] [Google Scholar]
- Lloret A, Badia MC, Mora NJ, et al. Vitamin E paradox in Alzheimer’s disease: it does not prevent loss of cognition and may even be detrimental. J Alzheimers Dis. 2009;17:143–149. doi: 10.3233/JAD-2009-1033. [DOI] [PubMed] [Google Scholar]
- Long LH, Halliwell B. Artefacts in cell culture: pyruvate as a scavenger of hydrogen peroxide generated by ascorbate or epigallocatechin gallate in cell culture media. Biochem Biophys Res Commun. 2009;388:700–704. doi: 10.1016/j.bbrc.2009.08.069. [DOI] [PubMed] [Google Scholar]
- Long LH, Halliwell B. Artefacts in cell culture: alpha-Ketoglutarate can scavenge hydrogen peroxide generated by ascorbate and epigallocatechin gallate in cell culture media. Biochem Biophys Res Commun. 2011;406:20–24. doi: 10.1016/j.bbrc.2011.01.091. [DOI] [PubMed] [Google Scholar]
- Long LH, Hoi A, Halliwell B. Instability of, and generation of hydrogen peroxide by, phenolic compounds in cell culture media. Arch Biochem Biophys. 2010;501:162–169. doi: 10.1016/j.abb.2010.06.012. [DOI] [PubMed] [Google Scholar]
- Lotito SB, Frei B. Consumption of flavonoid-rich foods and increased plasma antioxidant capacity in humans: cause, consequence, or epiphenomenon? Free Radic Biol Med. 2006;41:1727–1746. doi: 10.1016/j.freeradbiomed.2006.04.033. [DOI] [PubMed] [Google Scholar]
- Lykkesfeldt J, Trueba GP, Poulsen HE, et al. Vitamin C deficiency in weanling guinea pigs: differential expression of oxidative stress and DNA repair in liver and brain. Br J Nutr. 2007;98:1116–1119. doi: 10.1017/s0007114507787457. [DOI] [PubMed] [Google Scholar]
- Macready AL, Kennedy OB, Ellis JA, et al. Flavonoids and cognitive function: a review of human randomized controlled trial studies and recommendations for future studies. Genes Nutr. 2009;4:227–242. doi: 10.1007/s12263-009-0135-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maher P, Akaishi T, Abe K. Flavonoid fisetin promotes ERK-dependent long-term potentiation and enhances memory. Proc Natl Acad Sci USA. 2006;103:16568–16573. doi: 10.1073/pnas.0607822103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manach C, Scalbert A, Morand C, et al. Polyphenols: food sources and bioavailability. Am J Clin Nutr. 2004;79:727–747. doi: 10.1093/ajcn/79.5.727. [DOI] [PubMed] [Google Scholar]
- Mattson MP, Cheng A. Neurohormetic phytochemicals: low-dose toxins that induce adaptive neuronal stress responses. Trends Neurosci. 2006;29:632–639. doi: 10.1016/j.tins.2006.09.001. [DOI] [PubMed] [Google Scholar]
- Montero M, Lobaton CD, Hernandez-Sanmiguel E, et al. Direct activation of the mitochondrial calcium uniporter by natural plant flavonoids. Biochem J. 2004;384:19–24. doi: 10.1042/BJ20040990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muller WE, Singer A, Wonnemann M, et al. Hyperforin represents the neurotransmitter reuptake inhibiting constituent of hypericum extract. Pharmacopsychiatry. 1998;31(Suppl 1):16–21. doi: 10.1055/s-2007-979341. [DOI] [PubMed] [Google Scholar]
- Nakagawa K, Miyazawa T. Absorption and distribution of tea catechin, (−)-epigallocatechin-3-gallate, in the rat. J Nutr Sci Vitaminol (Tokyo) 1997;43:679–684. doi: 10.3177/jnsv.43.679. [DOI] [PubMed] [Google Scholar]
- Nurk E, Refsum H, Drevon CA, et al. Intake of flavonoid-rich wine, tea, and chocolate by elderly men and women is associated with better cognitive test performance. J Nutr. 2009;139:120–127. doi: 10.3945/jn.108.095182. [DOI] [PubMed] [Google Scholar]
- Ofir R, Tamir S, Khatib S, et al. Inhibition of serotonin re-uptake by licorice constituents. J Mol Neurosci. 2003;20:135–140. doi: 10.1385/JMN:20:2:135. [DOI] [PubMed] [Google Scholar]
- Pan MH, Huang TM, Lin JK. Biotransformation of curcumin through reduction and glucuronidation in mice. Drug Metab Dispos. 1999;27:486–494. [PubMed] [Google Scholar]
- Pannala AS, Rice-Evans CA, Halliwell B, et al. Inhibition of peroxynitrite-mediated tyrosine nitration by catechin polyphenols. Biochem Biophys Res Commun. 1997;232:164–168. doi: 10.1006/bbrc.1997.6254. [DOI] [PubMed] [Google Scholar]
- Peng HW, Cheng FC, Huang YT, et al. Determination of naringenin and its glucuronide conjugate in rat plasma and brain tissue by high-performance liquid chromatography. J Chromatogr B Biomed Sci Appl. 1998;714:369–374. doi: 10.1016/s0378-4347(98)00204-7. [DOI] [PubMed] [Google Scholar]
- Pietsch K, Saul N, Chakrabarti S, et al. Hormetins, antioxidants and prooxidants: defining quercetin-, caffeic acid- and rosmarinic acid-mediated life extension in C. elegans. Biogerontology. 2011;12:329–347. doi: 10.1007/s10522-011-9334-7. [DOI] [PubMed] [Google Scholar]
- Prasain JK, Peng N, Dai Y, et al. Liquid chromatography tandem mass spectrometry identification of proanthocyanidins in rat plasma after oral administration of grape seed extract. Phytomedicine. 2009;16:233–243. doi: 10.1016/j.phymed.2008.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Purkayastha S, Berliner A, Fernando SS et al (2009) Curcumin blocks brain tumor formation. Brain Res 1266:130–138 [DOI] [PubMed]
- Quinn JF, Raman R, Thomas RG, et al. Docosahexaenoic acid supplementation and cognitive decline in Alzheimer disease: a randomized trial. JAMA. 2010;304:1903–1911. doi: 10.1001/jama.2010.1510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Racagni G, Popoli M. The pharmacological properties of antidepressants. Int Clin Psychopharmacol. 2010;25:117–131. doi: 10.1097/YIC.0b013e3283311acd. [DOI] [PubMed] [Google Scholar]
- Reiter RJ. Oxidative processes and antioxidative defense mechanisms in the aging brain. FASEB J. 1995;9:526–533. [PubMed] [Google Scholar]
- Rhee SH, Pothoulakis C, Mayer EA. Principles and clinical implications of the brain-gut-enteric microbiota axis. Nat Rev Gastroenterol Hepatol. 2009;6:306–314. doi: 10.1038/nrgastro.2009.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rice ME. Ascorbate regulation and its neuroprotective role in the brain. Trends Neurosci. 2000;23:209–216. doi: 10.1016/s0166-2236(99)01543-x. [DOI] [PubMed] [Google Scholar]
- Rice-Evans CA, Miller NJ, Bolwell PG, et al. The relative antioxidant activities of plant-derived polyphenolic flavonoids. Free Radic Res. 1995;22:375–383. doi: 10.3109/10715769509145649. [DOI] [PubMed] [Google Scholar]
- Rocha FF, Lima-Landman MT, Souccar C, et al. Antidepressant-like effect of Cecropia glazioui Sneth and its constituents—in vivo and in vitro characterization of the underlying mechanism. Phytomedicine. 2007;14:396–402. doi: 10.1016/j.phymed.2007.03.011. [DOI] [PubMed] [Google Scholar]
- Russo A, Acquaviva R, Campisi A, et al. Bioflavonoids as antiradicals, antioxidants and DNA cleavage protectors. Cell Biol Toxicol. 2000;16:91–98. doi: 10.1023/a:1007685909018. [DOI] [PubMed] [Google Scholar]
- Ryan J, Croft K, Mori T, et al. An examination of the effects of the antioxidant pycnogenol on cognitive performance, serum lipid profile, endocrinological and oxidative stress biomarkers in an elderly population. J Psychopharmacol. 2008;22:553–562. doi: 10.1177/0269881108091584. [DOI] [PubMed] [Google Scholar]
- Schaffer S, Halliwell B (2011) Comment on ‘Hydroxytyrosol induces proliferation and cytoprotection against oxidative injury in vascular endothelial cells: role of Nrf2 activation and HO-1 induction’. J Agric Food Chem 59:10770–10771 [DOI] [PubMed]
- Schaffer S, Eckert GP, Muller WE, et al. Hypochlorous acid scavenging properties of local Mediterranean plant foods. Lipids. 2004;39:1239–1247. doi: 10.1007/s11745-004-1353-9. [DOI] [PubMed] [Google Scholar]
- Schaffer S, Eckert GP, Schmitt-Schillig S, et al. Plant foods and brain aging: a critical appraisal. Forum Nutr. 2006;59:86–115. doi: 10.1159/000095209. [DOI] [PubMed] [Google Scholar]
- Schumann K, Szegner B, Kohler B, et al. A method to assess 59Fe in residual tissue blood content in mice and its use to correct 59Fe-distribution kinetics accordingly. Toxicology. 2007;241:19–32. doi: 10.1016/j.tox.2007.08.082. [DOI] [PubMed] [Google Scholar]
- Shah ZA, Li RC, Ahmad AS, et al. The flavanol (−)-epicatechin prevents stroke damage through the Nrf2/HO1 pathway. J Cereb Blood Flow Metab. 2010;30:1951–1961. doi: 10.1038/jcbfm.2010.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spear LP, Varlinskaya EI. Low dose effects in psychopharmacology: ontogenetic considerations. Nonlinearity Biol Toxicol Med. 2005;3:97–111. doi: 10.2201/nonlin.003.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spencer JP. The interactions of flavonoids within neuronal signalling pathways. Genes Nutr. 2007;2:257–273. doi: 10.1007/s12263-007-0056-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spencer JP. Flavonoids: modulators of brain function. Br J Nutr. 2008;99(E Suppl 1):ES60–ES77. doi: 10.1017/S0007114508965776. [DOI] [PubMed] [Google Scholar]
- Spencer JP. Flavonoids and brain health: multiple effects underpinned by common mechanisms. Genes Nutr. 2009;4:243–250. doi: 10.1007/s12263-009-0136-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spencer JP, Abd-el-Mohsen MM, Rice-Evans C. Cellular uptake and metabolism of flavonoids and their metabolites: implications for their bioactivity. Arch Biochem Biophys. 2004;423:148–161. doi: 10.1016/j.abb.2003.11.010. [DOI] [PubMed] [Google Scholar]
- Sun F, Iwaguchi K, Shudo R, et al. Change in tissue concentrations of lipid hydroperoxides, vitamin C and vitamin E in rats with streptozotocin-induced diabetes. Clin Sci (Lond) 1999;96:185–190. [PubMed] [Google Scholar]
- Talavera S, Felgines C, Texier O, et al. Anthocyanin metabolism in rats and their distribution to digestive area, kidney, and brain. J Agric Food Chem. 2005;53:3902–3908. doi: 10.1021/jf050145v. [DOI] [PubMed] [Google Scholar]
- Terpstra M, Torkelson C, Emir U, et al. Noninvasive quantification of human brain antioxidant concentrations after an intravenous bolus of vitamin C. NMR Biomed. 2011;24:521–528. doi: 10.1002/nbm.1619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trzeciakowski J, Chilian WM. Chaotic behavior of the coronary circulation. Med Biol Eng Comput. 2008;46:433–442. doi: 10.1007/s11517-008-0329-8. [DOI] [PubMed] [Google Scholar]
- Vaidyanathan JB, Walle T. Cellular uptake and efflux of the tea flavonoid (−)epicatechin-3-gallate in the human intestinal cell line Caco-2. J Pharmacol Exp Ther. 2003;307:745–752. doi: 10.1124/jpet.103.054296. [DOI] [PubMed] [Google Scholar]
- Duynhoven J, Vaughan EE, Jacobs DM, et al. Metabolic fate of polyphenols in the human superorganism. Proc Natl Acad Sci USA. 2011;108(Suppl 1):4531–4538. doi: 10.1073/pnas.1000098107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mierlo LA, Zock PL, Knaap HC, et al. Grape polyphenols do not affect vascular function in healthy men. J Nutr. 2010;140:1769–1773. doi: 10.3945/jn.110.125518. [DOI] [PubMed] [Google Scholar]
- Visioli F, Bellomo G, Galli C. Free radical-scavenging properties of olive oil polyphenols. Biochem Biophys Res Commun. 1998;247:60–64. doi: 10.1006/bbrc.1998.8735. [DOI] [PubMed] [Google Scholar]
- Visioli F, Lastra CA, Andres-Lacueva C, et al. Polyphenols and human health: a prospectus. Crit Rev Food Sci Nutr. 2011;51:524–546. doi: 10.1080/10408391003698677. [DOI] [PubMed] [Google Scholar]
- Wagner AE, Boesch-Saadatmandi C, Breckwoldt D, et al. Ascorbic acid partly antagonizes resveratrol mediated heme oxygenase-1 but not paraoxonase-1 induction in cultured hepatocytes—role of the redox-regulated transcription factor Nrf2. BMC Compl Altern Med. 2011;11:1. doi: 10.1186/1472-6882-11-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watjen W, Michels G, Steffan B, et al. Low concentrations of flavonoids are protective in rat H4IIE cells whereas high concentrations cause DNA damage and apoptosis. J Nutr. 2005;135:525–531. doi: 10.1093/jn/135.3.525. [DOI] [PubMed] [Google Scholar]
- Wehner F, Lawonn P, Tinel H. Ionic mechanisms of regulatory volume increase (RVI) in the human hepatoma cell-line HepG2. Pflugers Arch. 2002;443:779–790. doi: 10.1007/s00424-001-0765-x. [DOI] [PubMed] [Google Scholar]
- Wilkinson AP, Wahala K, Williamson G. Identification and quantification of polyphenol phytoestrogens in foods and human biological fluids. J Chromatogr B Analyt Technol Biomed Life Sci. 2002;777:93–109. doi: 10.1016/s1570-0232(02)00095-8. [DOI] [PubMed] [Google Scholar]
- Yanez M, Fraiz N, Cano E, et al. Inhibitory effects of cis- and trans-resveratrol on noradrenaline and 5-hydroxytryptamine uptake and on monoamine oxidase activity. Biochem Biophys Res Commun. 2006;344:688–695. doi: 10.1016/j.bbrc.2006.03.190. [DOI] [PubMed] [Google Scholar]
- Yokomizo A, Moriwaki M. Effects of uptake of flavonoids on oxidative stress induced by hydrogen peroxide in human intestinal Caco-2 cells. Biosci Biotechnol Biochem. 2006;70:1317–1324. doi: 10.1271/bbb.50604. [DOI] [PubMed] [Google Scholar]
- Yoshitake T, Yoshitake S, Kehr J. The Ginkgo biloba extract EGb 761(R) and its main constituent flavonoids and ginkgolides increase extracellular dopamine levels in the rat prefrontal cortex. Br J Pharmacol. 2010;159:659–668. doi: 10.1111/j.1476-5381.2009.00580.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Youdim KA, Shukitt-Hale B, Joseph JA. Flavonoids and the brain: interactions at the blood-brain barrier and their physiological effects on the central nervous system. Free Radic Biol Med. 2004;37:1683–1693. doi: 10.1016/j.freeradbiomed.2004.08.002. [DOI] [PubMed] [Google Scholar]
- Zini A, Del Rio D, Stewart AJ, et al. Do flavan-3-ols from green tea reach the human brain? Nutr Neurosci. 2006;9:57–61. doi: 10.1080/10284150600637739. [DOI] [PubMed] [Google Scholar]