Abstract
INTRODUCTION
Skip segment Hirschsprung's is an extremely rare condition, with only 25 reported cases in the English language literature. Diagnosis of skip segment Hirschsprung's may be missed as it is rarely suspected at initial surgery.
PRESENTATION OF CASE
A case report of an infant with total colonic aganglionosis and a skip segment Hirschsprung's in the cecum is presented. A review of literature on current surgical practice is presented along with our suggested modification to the diagnostic and therapeutic algorithm of this rare condition.
DISCUSSION
In our patient the initial leveling colostomy was incorrectly sited at the level of the first detected ganglionated segment. Subsequent recurrent episodes of enterocolitis led to a diagnosis of a long skip segment involving the ascending colon, cecum and terminal ileum. Correct leveling colostomy and a subsequent Duhamel procedure led to a good outcome.
CONCLUSION
Determination of the transition zone in Hirschsprung's may be incorrect if intestinal biopsies are terminated at the first evidence of ganglion cells. Extended segment intestinal biopsies should be included in the algorithm for management of long segment Hirschsprung's disease and will enable the surgeon to correctly detect rare manifestations such as skip segment disease at the initial procedure.
Keywords: Hirschsprung's disease, Skip-segment, Biopsy
1. Introduction
Laparoscopic or laparotomy based intestinal biopsies and single stage pull through procedures are being increasingly offered to patients with classical Hirschsprung's disease that involves the recto sigmoid region of the colon.1 The biopsies help define the location of the ganglionated segment of bowel before mesenteric transection and bowel mobilization. This avoids committing the patient to a trans-anal Soave or Swenson endorectal pull-through procedure which may not necessarily be optimal in the long segment variants of this disease. Biopsy localization of the ganglionated segment also helps in performing the stoma at an appropriate location in patients who may not be suitable candidates for a one-stage pull-through procedure.2 While this is often a straight forward procedure we recently encountered a patient with total colonic aganglionosis (TCA) in whom a skip lesion in the ascending colon complicated surgical decision making. Although skip lesions can occur in the classical recto-sigmoid variant of Hirschsprung's it is more common in the extended long segment and total colonic forms of the disease.3 We suggest a modification to the biopsy technique in these variants of Hirshsprung's disease based on our recent experience. This simple step may prevent many episodes of enterocolitis after pull through which may be due to a retained aganglionic segment.
2. Case report
A two day old full term, male infant with abdominal distension, failure to pass meconium, and feeding intolerance was evaluated by us. Contrast enema suggested Hirschsprung's disease with a transition zone at the level of the splenic flexure and the diagnosis was confirmed on suction rectal biopsies (Fig. 1). The infant did not have any signs of sepsis but had significant bowel distension. The infant was subsequently scheduled for laparoscopic biopsies and one stage pull through or stoma based on the anatomic location of the transition zone. Partial thickness biopsies of the colon were performed at the level of the upper rectum, sigmoid, splenic flexure, mid transverse colon, and hepatic flexure until we found ganglion cells in the ascending colon on frozen section. The biopsies (including sub mucosa) were reviewed by two experienced pathologists after standard hematoxylin and eosin staining. We performed an ascending colostomy 5 cm proximal to the ganglionated biopsy site and frozen and permanent sections from this segment showed normal ganglion cells (Fig. 2). The procedure was completed by performing a subtotal colectomy, appendectomy, and a mucous fistula at the level of the sigmoid colon. The permanent sections from the appendix did not show ganglion cells (Fig. 3). While the infant did well initially he had several re-admissions to the hospital for episodes of enterocolitis. A contrast enema through the stoma performed on one such admission showed a narrow segment of colon and terminal ileum with a large dilated segment of ileum proximal to that. As we were not able to resolve the episodes of enterocolitis with irrigation and antibiotics alone we decided to perform a laparotomy with revision of the stoma. Biopsies performed this time around reconfirmed normal ganglion cells at the level of the stoma but no ganglion cells in the cecum (5 cm proximal to the stoma) and in the terminal ileum (Fig. 4). Normal ganglion cells were identified in the dilated ileum and in the small intestine 10 cm proximal to that (Fig. 5). This segment of bowel was resected and a new ileostomy was created. The revised ileostomy functioned well and the child subsequently underwent a successful Duhamel pull through at four months of age and is doing well nearly a year after the definitive pull through.
Fig. 1.

Contrast enema showing the narrow left colon opening up into a large caliber transverse colon (with diluted contrast). The cecum is significantly distended.
Fig. 2.
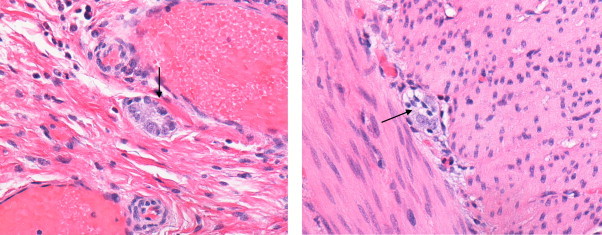
Ascending colon (40×), Meissner's plexus (left) and (40×) Aurebach's plexus (right) (arrow noting ganglion cells) (left).
Fig. 3.
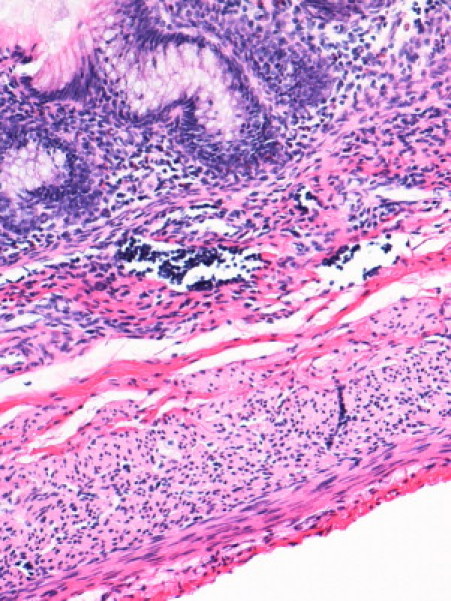
Appendix (20×), no ganglion cells in Meissner's and Auerbach's plexus.
Fig. 4.
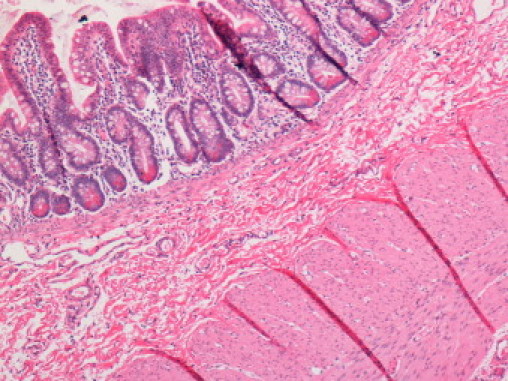
Terminal Ileum showing no ganglion cells in Meissner's and Auerbach's plexus (40×).
Fig. 5.
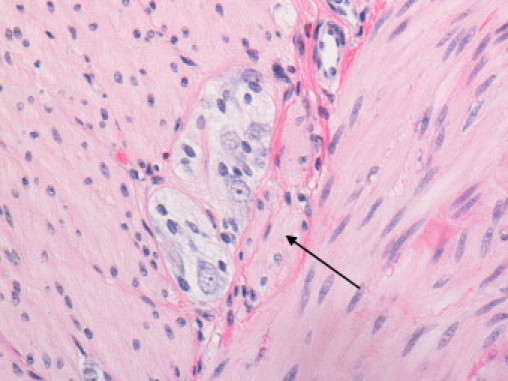
Proximal Ileum showing ganglion cells in Aurebach plexus (40×).
3. Discussion
Skip lesions are very rare with only twenty five cases being discovered in a recent review on this condition.6 Its pathological basis has been difficult to explain and various causative hypotheses have been proposed.9 However its occurrence can confound surgical management of what is a fairly common pediatric surgical problem. In our patient two questions that immediately arise are if we could have avoided the problem by performing full thickness biopsies or by performing additional staining techniques. We have never had any diagnostic difficulty with partial thickness biopsies (performed by either laparoscopic or open techniques) and the ganglion cells of the myenteric plexus which are abundant are easily evaluated with this technique.10 Clearly even a full thickness biopsy would be misleading if performed in a skip area as we noted in our case. Furthermore using immuno-staining methods such as acetylcholinestrase or calretinin routinely would not help in identifying patients with skip lesions who have normal appearing ganglion cells and nerve fibers in the ganglionated segment of skip segment Hirschsprung's.11,12 We do not believe that changing staining techniques will replace an experienced pathologist in identifying this difficult problem. However we have come to realize that biopsy sampling of colonic and ileal walls needs to be more extensive in long segment variants of Hirschsprung's to avoid missing skip segments and particularly should not stop at the first evidence of ganglionated bowel (Fig. 2). This recommendation is different to the current practice of performing the pull through or a colostomy with a segment of intestine a little proximal (approximately 5–10 cm) to the location where ganglion cells were found on biopsies to ensure complete removal of the transition zone of “hypoganglionosis”.5
The proximal extent of the biopsies is roughly guided by the location of the transition zone as detected on the contrast enema or by surgical findings of dilated intestine proximal to the aganglionic segment. However there is often a significant geographical discrepancy between the radiological and pathological transition zones and surgical judgment of pathological transition zones are often inaccurate and hence cannot be relied upon to determine the proximal extent of biopsies.4 To avoid missing this rare lesion we believe frozen section seromuscular intestinal biopsies should be performed at two anatomic locations proximal to the first identified ganglionated bowel to “hop the skip segment”. In our patient this would have involved performing biopsies on the cecum and the terminal ileum and would have been sufficient to identify the problem. This practice should be particularly adopted in patients with extended long segment disease in whom skips are more common.6 Patients who are likely to have extended long segment disease or total colonic aganglionosis (TCA) are those with mutations in the RET proto-oncogene and those who have familial variants of this disease.7
It is currently not known as to what the length of a skip segment exactly is because of the clinical rarity of this condition. While some reports talk of skip lesions a few centimeters long others talk of skip lesions that have a fully ganglionated and functional transverse colon segment.3,6 Such knowledge would enable one to plan intestinal biopsies effectively for surgical decision making. In our patient the ganglionated skip segment was about 10 cm long. The appendix and cecum located 15 cm proximal to the ganglionated bowel at the first operation did not have ganglion cells but there has been a long standing debate about the clinical relevance of absent ganglion cells in the appendix.8 A careful assessment of the appendix is possible only on permanent sections as intra-operative frozen section of a single cross section can never be trusted as the normal appendix is not uniformly ganglionated. In our patient the appendix truly was aganglionic and would have guided stoma location accurately. The cecal pole and the terminal ileum near the ileo-cecal valve were both aganglionic and a cecal pole biopsy would have been representative of this pathological field defect. While one cannot make a judicious recommendation based on a single observation and each patient's pathology is likely to be different in our patient we could have avoided a second surgery by obtaining further biopsy samples at two proximal anatomic sites and this is the basis for our recommendation (Fig. 6). As the length of skip segment disease is unpredictable we recommend that such biopsies should include the cecal pole and the small bowel 10 cm away from the ileo-cecal valve. This change in practice may prevent many episodes of enterocolitis which is a common complication of surgery after Hirschsprung's disease due to retained aganglionic segment. It needs ongoing validation and prospective verification by surgeons encountering this rare disease.
Fig. 6.
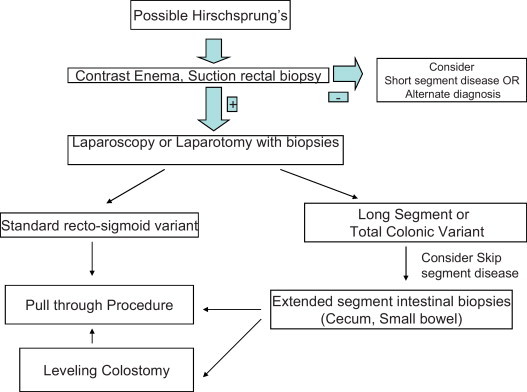
Proposed algorithm would facilitate accurate diagnosis of ‘skip-segment’ disease in total colonic and long segment variants of Hirschsprung's where it is more common.
Conflict of interest statement
None.
Funding
None.
Ethical approval
Written consent was obtained from family and will be provided at the request of editor in chief of journal.
Author contributions
Burjonrappa involved in design, writing, research and revision of the study. Rankin involved in writing and research of the study.
References
- 1.Georgeson K.E., Robertson D.J. Laparoscopic-assisted approaches for the definitive surgery for Hirschsprung's disease. Semin Pediatr Surg. 2004;13(November (4)):256–262. doi: 10.1053/j.sempedsurg.2004.10.013. [DOI] [PubMed] [Google Scholar]
- 2.Meyrat B.J., Lesbros Y., Laurini R.N. Assessment of the colon innervation with serial biopsies above the aganglionic zone before the pull-through procedure in Hirschsprung's disease. Pediatr Surg Int. 2001;17(March (2–3)):129–135. doi: 10.1007/s003830000507. [DOI] [PubMed] [Google Scholar]
- 3.O’Donnell A.M., Puri P. Skip segment Hirschsprung's disease: a systematic review. Pediatr Surg Int. 2010;26(November (11)):1065–1069. doi: 10.1007/s00383-010-2692-4. [DOI] [PubMed] [Google Scholar]
- 4.Das K., Kini U., Babu M.K., Mohanty S., D’Cruz A.J. The distal level of normally innervated bowel in long segment colonic Hirschsprung's disease. Pediatr Surg Int. 2010;26(June (6)):593–599. doi: 10.1007/s00383-010-2603-8. [DOI] [PubMed] [Google Scholar]
- 5.Meier-Ruge W.A., Brunner L.A., Engert J., Heminghaus M., Holschneider A.M., Jordan P. A correlative morphometric and clinical investigation of hypoganglionosis of the colon in children. Eur J Pediatr Surg. 1999;9(April (2)):67–74. doi: 10.1055/s-2008-1072216. [DOI] [PubMed] [Google Scholar]
- 6.Doi T., O’Donnell A.M., McDermott M., Puri P. Skip segment Hirschsprung's disease: a rare phenomenon. Pediatr Surg Int. 2011 doi: 10.1007/s00383-011-2903-7. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 7.Moore S.W., Zaahl M.G. A review of genetic mutation in familial Hirschsprung's disease in South Africa: towards genetic counseling. J Pediatr Surg. 2008;43(February (2)):325–329. doi: 10.1016/j.jpedsurg.2007.10.021. [DOI] [PubMed] [Google Scholar]
- 8.Anderson K.D., Chandra R. Segmental aganglionosis of the appendix. J Pediatr Surg. 1986;21(October (10)):852–854. doi: 10.1016/s0022-3468(86)80006-9. [DOI] [PubMed] [Google Scholar]
- 9.Kapur R.P., deSa D.J., Luquette M., Jaffe R. Hypothesis: pathogenesis of skip areas in long-segment Hirschsprung's disease. Pediatr Pathol Lab Med. 1995;15(January–February (1)):23–37. doi: 10.3109/15513819509026937. [DOI] [PubMed] [Google Scholar]
- 10.Rolle U., Piotrowska A.P., Nemeth L., Puri P. Altered distribution of interstitial cells of Cajal in Hirschsprung disease. Arch Pathol Lab Med. 2002;126:928–933. doi: 10.5858/2002-126-0928-ADOICO. [DOI] [PubMed] [Google Scholar]
- 11.Barshack I., Fridman E., Goldberg I., Chowers Y., Kopolovic J. The loss of calretinin expression indicates aganglionosis in Hirschsprung's disease. J Clin Pathol. 2004;57(July (7)):712–716. doi: 10.1136/jcp.2004.016030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kobayashi H., Wang Y., Hirakawa H., O’Briain D.S., Puri P. Intraoperative evaluation of extent of aganglionosis by a rapid acetylcholinesterase histochemical technique. J Pediatr Surg. 1995;30:248–252. doi: 10.1016/0022-3468(95)90569-3. [DOI] [PubMed] [Google Scholar]


