Abstract
Benign metastasising leiomyoma (BML) is a rare entity characterised by uterine leiomyoma that, later on, develops slow-growing metastasis mainly to the lung. In general, these lung metastases are incidentally discovered, but sometimes can become symptomatic with dyspnoea, cough and chest pain. The expression of oestrogen and progesterone receptors by these tumours supports the idea that they respond to hormone therapy (chemical, with oestrogen receptor modulators, aromatase inhibitors or luteinising hormone releasing hormone analogues and surgical, with bilateral adnexectomy). The authors present a case report of BML with two peculiarities: a less common pattern of metastisation (soft tissue), in addition to lung; and disease progression despite treatment with chemical and surgical castration.
Background
Benign metastasising leiomyoma (BML) is a rare entity (74 cases reported so far, mostly in Japan) first described by Steiner; it is characterised by uterine leiomyoma that, later on, develop slow-growing metastasis.1–4 These metastases develop mainly in the lung, but can occur also in the lymph nodes and central nervous system.2 3 In general, the lung metastisation is indolent and incidentally discovered; however it can become symptomatic with dyspnoea, cough and chest pain.4
There are three hypotheses about BML pathogenesis: (1) Benign uterine leiomyoma colonising the lung; (2) Metastatic low-grade uterine leiomyosarcoma; (3) Multicentric leiomyoma. Nowadays, the first theory is the most accepted based on several aspects: this disease is more common in women than in man; the pulmonary lesions have a benign histology and they express oestrogen and progesterone receptors in immunohistochemistry; the telomers’ length of uterine myomas is the same found in the lung lesions; and there is a subendothelial involvement.1 4 5
The expression of oestrogen and progesterone receptors by these tumours and the fact that there is a regression of the metastasis during pregnancy and menopause, support the idea that they respond to hormone therapy (chemical, with oestrogen receptor modulators, aromatase inhibitors or luteinising hormone releasing hormone analogues; and surgical, with bilateral adnexectomy).1 2 6–8
This clinical case is particularly relevant because it reports a rare disease – BML – that presented with a less common pattern of metastisation (soft tissue), in addition to lung; and that presented with a worse prognosis due to disease progression under treatment with chemical and surgical castration.
Case presentation
A 50 year-old, Caucasian female patient was referred to our Cancer Institute in January 1999 with the diagnosis of BML of the lung. Sixteen years before she had abundant menometrorrhagia, the diagnosis of uterine myoma was made and she was submitted to total hysterectomy.
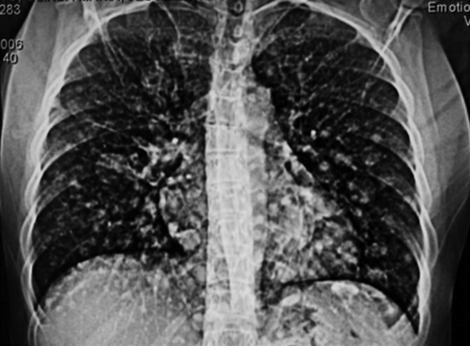
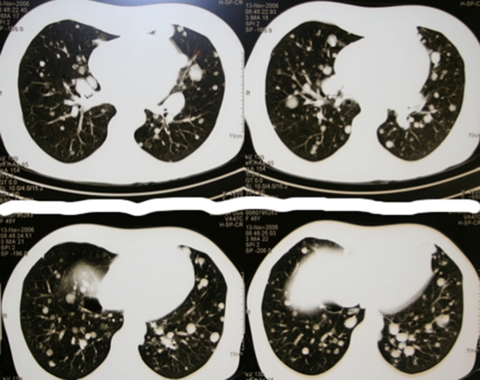
Two years before referral, because of a pulmonary infection, a chest x-ray showed several pulmonary nodules (figures 1 and 2). The chest CT confirmed these findings, and she was referred to the pneumology department in another institution.
Figure 1.
Multiple lung leiomyoma metastisation pattern in chest x-ray.
Figure 2.
Multiple lung leiomyoma metastisation pattern in chest CT.
Investigations
In the referred hospital, several diagnostic exams were performed: (A) lab investigation (CBC, coagulation, renal and hepatic function tests and ionogram), bronchofibroscopy, abdominopelvic CT and thyroid ultrasound were normal. (B) Pulmonary function tests documented a moderate small airway obstruction, with hypoxemia (PaO2 62 mm Hg). (C) Surgical pulmonary biopsy with atypical resection of right upper lobe revealed metastasing leiomyoma in pathology. The histological report showed pulmonary nodules formed by the proliferation of smooth muscular fibers, with a benign pattern (regularity, dimensions and shape, regular nucleus and absence of mitosis) (figure 3).
Figure 3.
Biopsy of lung nodule disclosing leiomyoma features (H&E-amplification 40x).
She was asymptomatic until 1 year later, when she reported dyspnoea on moderate exertion. She repeated the chest CT that showed an increased number and dimension of lung nodes compared with the previous CT, leading to referral to our cancer institute.
Treatment
As she was symptomatic, in April 2010, therapy with goserelin (chemical castration) was started and in June of the same year she is submitted to bilateral adnexectomy (surgical castration). The histological exam revealed an endometrioid cyst in the right ovary, with no other abnormality.
Outcome and follow-up
One month later a new skin lesion showed up in the forearms, back and pectoral regions (figure 4). One of the forearm lesions was biopsied and the diagnosis of leiomyoma was confirmed.
Figure 4.
Soft tissue metastasising leiomyoma of the forearm.
A new chest-CT showed a similar bilateral nodular involvement of the lungs.
She was maintained in close surveillance in Medical Oncology, Dermatology, Pneumology and Gynecology clinics, performing chest-CT biannually.
Six years later the chest-CT showed an increase in the number and dimension of the pulmonary lesions. Despite this evolution, in July of the same year she performed chest PET-scan, that did not show hypermetabolic lesions.
She is still asymptomatic, PS 0, with a stable disease.
Discussion
This clinical case is particularly relevant besides the fact that it reports a rare disease. First, presents a less common pattern of metastisation (soft tissues) in addition to the lung. Second, despite the fact that BML is considered a hormone-dependent tumour, this case registered a disease progression even with chemical and surgical castration.
Since the uterine leiomyoma is hormone-dependent tumour, the treatment is based on oestrogen and progesterone suppression. Therefore, several treatment modalities have been proposed: (1) surgical castration – bilateral adnexectomy; (2) Gonadotropin-releasing hormone (GnRH) analogues (goserelin, leuprolide) – their effect is generally incomplete, since part of oestrogen origin derive from the androgen’s aromatisation in the peripheral tissues2 7; (3) Progesterone antagonists (mifepristone) – they inhibit the hypothalamus-hypophysis-gonadal axis, inactivate the estradiol and decrease the androgen’s aromatisation in 30%; they should not be used alone, since they increase the number of estrogen receptors9 10; (4) Selective oestrogen receptor modulators (SERM – raloxifen) – they antagonise the oestrogen action in the peripheral tissues receptors11; (5) Aromatase inhibitors (anastrazole) – they decrease the oestrogen production by the peripheral tissues.
There are no straightforward guidelines on the best therapy or association of different therapies. Clinical trials are needed in order to define these guidelines. However, nowadays the GnRH agonists and SERMs seem to be the most efficient treatment for the BML.2 7 9 10 12
Learning points.
-
▶
BML is a rare condition, affecting predominantly females, characterised by soft tissue tumours at distant sites that are histologically identical to leiomyomas of the uterus.
-
▶
Being a hormone-dependent tumour, BML’s treatment strategy is based on oestrogen and progesterone suppression.
-
▶
This BML’s clinical case is peculiar for its pattern of soft tissue metastisation and progression despite hormonal and surgical castration.
Footnotes
Competing interests None.
Patient consent Obtained.
References
- 1.Patton KT, Cheng L, Papavero V, et al. Benign metastasizing leiomyoma: clonality, telomere length and clinicopathologic analysis. Mod Pathol 2006;19:130–40 [DOI] [PubMed] [Google Scholar]
- 2.Alessi G, Lemmerling M, Vereecken L, et al. Benign metastasizing leiomyoma to skull base and spine: a report of two cases. Clin Neurol Neurosurg 2003;105:170–4 [DOI] [PubMed] [Google Scholar]
- 3.Joseph V, Chacko G, Raghuram L, et al. Benign metastasizing leiomyoma causing spinal cord compression. Surg Neurol 2003;60:575–7; discussion 577–8 [DOI] [PubMed] [Google Scholar]
- 4.Koh DM, Burn PR, King DM. Benign metastasizing leiomyoma with intracaval leiomyomatosis. Br J Radiol 2000;70:435–7 [DOI] [PubMed] [Google Scholar]
- 5.Kayser K, Zink S, Schneider T, et al. Benign metastasizing leiomyoma of the uterus: documentation of clinical, immunohistochemical and lectin-histochemical data of ten cases. Virchows Arch 2000;437:284–92 [DOI] [PubMed] [Google Scholar]
- 6.Sumitani H, Shozu M, Segawa T, et al. In situ estrogen synthesized by aromatase P450 in uterine leiomyoma cells promotes cell growth probably via an autocrine/intracrine mechanism. Endocrinology 2000;141:3852–61 [DOI] [PubMed] [Google Scholar]
- 7.Abramson S, Gilkeson RC. Multiple pulmonary nodules in an asymptomatic patient. Chest 1999;116:245–7 [DOI] [PubMed] [Google Scholar]
- 8.Arai T, Yasuda Y, Takaya T, et al. Natural decrease of benign metastasizing leiomyoma. Chest 2000;117:921–2 [DOI] [PubMed] [Google Scholar]
- 9.Palomba S, Orio F, Jr, Morelli M, et al. Raloxifene administration in premenopausal women with uterine leiomyomas: a pilot study. J Clin Endocrinol Metab 2002;87:3603–8 [DOI] [PubMed] [Google Scholar]
- 10.Palomba S, Sammartino A, Di Carlo C, et al. Effects of raloxifene treatment on uterine leiomyomas in postmenopausal women. Fertil Steril 2001;76:38–43 [DOI] [PubMed] [Google Scholar]
- 11.Shozu M, Murakami K, Segawa T, et al. Successful treatment of a symptomatic uterine leiomyoma in a perimenopausal woman with a nonsteroidal aromatase inhibitor. Fertil Steril 2003;79:628–31 [DOI] [PubMed] [Google Scholar]
- 12.Rivera JA, Christopoulos S, Small D, et al. Hormonal manipulation of benign metastasizing leiomyomas: report of two cases and review of the literature. J Clin Endocrinol Metab 2004;89:3183–8 [DOI] [PubMed] [Google Scholar]