Abstract
Tuberculosis has always been a menace for both clinicians and radiologists due to its often non-specific and protean manifestations. Isolated tubercular involvement of sacrum is very rare. The authors present the case of a 38-year-old man with history of low-grade fever, pain and swelling in the sacral region. Skiagram revealed an osteolytic lesion of sacrum leading to the provisional diagnosis of chordoma and osteoclastoma. However, MRI was suggestive of a chronic infective condition like tuberculosis and fine needle aspiration cytology was positive for acid-fast bacilli and revealed epitheloid granulomas with caseous necrosis. Culture was positive for Mycobacterium tuberculosis. Antitubercular therapy was commenced and surgical decompression of cold abscess was done and with good clinical response. This case highlights the importance of remaining cognisant of the manifestations and the importance of considering tuberculosis as a diagnosis at unusual sites of involvement.
Background
Tuberculosis has always been a menace in the developing world. According to WHO, 9.4 million new individuals developed tuberculosis in 2009.1 Despite increasing availability of better imaging techniques, extra-pulmonary tuberculosis remains a difficult diagnosis to make, due to its often non-specific and protean manifestations. It is not uncommon for this disease to mimic malignancy, leading to referral of patients to oncologists and surgeons, delaying correct diagnosis and the institution of appropriate therapy. Therefore, the prompt recognition of distinguishing imaging features and histopathological confirmation is vital for correct diagnosis and to facilitate timely antitubercular therapy.
Case presentation
A 38-year-old Indian male, presented to outpatient department of orthopaedics with a 3 month history of mild pain over lower back region, the pain aggravated while sitting or squatting. He also gave history of swelling for the past 2 months, and 6 kg loss of weight during this period. There were no other associated constitutional symptoms. The patient was a smoker since 12 years (20 pack years). The patient took medication for a period of 1 month (no records were available) but he did not get any relief.
On admission, the patient appeared well, was afebrile, and had no abnormality on chest or abdominal examination. On local examination, the swelling was around 5×4 cm in size over the sacral region, firm in consistency, non-tender, the temperature of the swelling was not raised.
Investigations
Radiograph lumbo-sacral spine lateral view showed destruction of dorsal sacrum with increased overlying soft-tissue thickness (figure 1). On the basis of these findings, a provisional diagnosis of chordoma and osteoclastoma was put forward. Therefore, a MRI was advised.
Figure 1.
Radiograph pelvis lateral view showing expansile lytic lesion involving sacrum. There is thickening of overlying soft tissues.
Laboratory investigations showed raised total leucocyte count-13 200 per cubic mm with neutrophils-19%, lymphocytes-79%, eosinphils-1%, monocytes-1%, while erythrocyte sedimentation rate (ESR) was 82 mm/h. Markers for HIV, hepatitis B surface antigen and hepatitis C virus were negative.
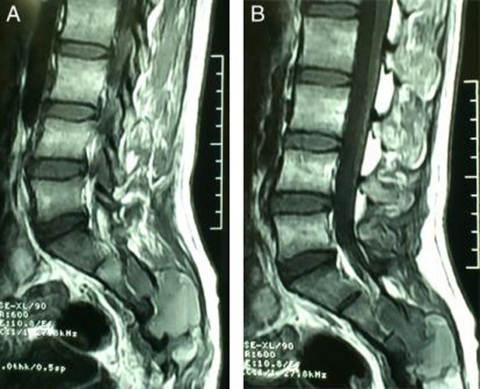
MRI revealed the presence of soft-tissue lesion involving sacrum, predominantly the posterior elements and posterior part of body, extending from S2 to S5 level. There was associated thick fluid collection (figure 2a,b). With this, chronic infective aetiology like tuberculosis was considered as a differential diagnosis.
Figure 2.
(a and b) T1 weighted sagittal MRI images showing soft-tissue lesion involving S2–S5 sacral vertebra, predominantly the posterior elements and posterior part of body. There is associated thick fluid collection.
Therefore, fine needle aspiration cytology was performed and sent for histopathological examination including staining for acid-fast bacilli and culture of material. The smears were positive for acid-fast bacilli whereas cytology revealed epitheloid granulomas with patches of caseous necrosis. Culture was positive for Mycobacterium tuberculosis which was sensitive to all the first line drugs. X-ray chest, however revealed no evidence of any pulmonary tuberculosis.
Differential diagnosis
Chordoma and osteoclastoma.
Treatment
Thus after patho-radiological correlation, the case was diagnosed as sacral tuberculosis with cold abscess. Antitubercular drugs were started immediately after smear examination. The patient weighed 56 kg, so accordingly antitubercular treatment was initiated (isoniazid 300 mg, rifampicin 600 mg, ethambutol 1200 mg and pyrazinamide 1500 mg daily). There was no significant improvement in patient’s symptoms after 3 weeks of continuous therapy. The patient also complained of severe pain while lying on bed, therefore surgical decompression was planned for the cold abscess and classical yellowish white cheesy material was obtained. All the dead and necrotic tissue along with the destroyed bone was removed.
Outcome and follow-up
Antitubercular therapy was continued and the patient was discharged after 35 days with the advice of complete bed rest preferably in lateral decubitus positions. After a period of 1 month, the patient was able to sit over soft surfaces and by the end of 2 months he was able to sit on hard surfaces also. At end of 3 months, the patient was remarkably relieved of his symptoms, his ESR was 18 mm/h, white cell count was 8700/cumm and the patient’s weight increased to 61 kg. Liver function tests were well within normal limit. Patient was given all four first line drugs for a period of 4 months then pyrazinamide and ethambutol were discontinued, with the total duration of antitubercular therapy being 18 months. At the end of therapy, the patient was completely relieved of his symptoms.
Discussion
Extra-pulmonary tuberculosis, a condition whose growing incidence can be ascribed to the emergence of multi-drug resistance and an increasing number of immune compromised individuals, remains a difficult diagnosis to make.2–4 It is one of the great mimickers in medicine, with non-specific clinical and radiological manifestations that can suggest numerous other disease entities in particular malignancy. Isolated sacral tuberculosis is rare but it should be the first and foremost differential diagnosis in the presence of atypical clinical and radiological features of a sacral lesion particularly in developing countries.5
Although a positive tuberculin test and chest imaging findings are supportive of the diagnosis, absence of these does not exclude it.6 7 In more than 50% of cases there is no evidence of concurrent active intrathoracic tuberculosis.6 Therefore, other diagnostic tests need to be used, combined with a high index of clinical suspicion.
Musculoskeletal involvement occurs in 1 to 3 per cent of patients with tuberculosis, usually due to haematogenous seeding.6 8 Roughly half of them involve vertebral column.9 While the most common site of osseous involvement is the spine, followed by the femur, tibia and the small bones of the hands and feet, any bone can potentially be affected.2 6 8 The first case of sacral tuberculosis described in medical literature was reported by Campbell in 1917.10 Pun reported 20-year follow-up of 26 patients of tuberculosis of lumbo-sacral junction. In majority of patients, the disease had started in lumbar spine and descended to the sacrum.11 The most common presenting symptoms are non-specific pain and swelling. Consequently, skeletal tuberculosis frequently mimics neoplasias like chordoma and osteoclastoma as in the above case, or sometimes metastasis leading to incorrect initial diagnosis and delay in the institution of treatment.
Plain radiograph findings in bony tuberculosis include osteopenia, osteolytic foci with poorly defined edges and varying amounts of sclerosis and periostitis.2 7 These findings are, however, non-specific, and can be found in a range of pathological processes, including neoplasia. CT provides better delineation of bone involvement than plain radiographs, however in developing countries like India most of the patients belong to poor socioeconomic status and cannot afford all the investigations. Therefore we prefer MRI which is a better investigation to evaluate soft-tissue involvement. In the above case, MRI revealed presence of abscess which favoured tuberculous infection over neoplasia. Regardless, the features of tubercular osteomyelitis are so variable and inconstant that further investigation is usually required.
Chordomas are the most common primary malignant sacral tumour with most individuals presenting in the 4th to 7th decade.12 However, chordoma typically manifests as a large destructive sacral mass with secondary soft-tissue extension. Radiographs may show sacral osteolysis with an associated pre or post sacral soft-tissue mass and calcifications.13 Areas of haemorrhage and calcification are strongly suggestive of a chordoma. Moreover, presence of abscess favoured infective process.
Giant cell tumour is the second most common primary sacral neoplasm after chordoma and tends to involve the upper sacrum and extend across the sacroiliac joint.14 Giant cell tumours occasionally demonstrate fluid-fluid levels due to components of the tumour.
Because of this overlap in imaging appearances between extra-pulmonary tuberculosis and malignancy, even in cases where the imaging and clinical features strongly suggest tuberculosis, the diagnosis requires histopathological and bacteriological confirmation. In the past, this often necessitated open surgical biopsy. Fine needle aspiration cytology has been shown to be quick, safe and effective alternative for obtaining tissue specimens.
Regarding treatment there are different opinions in literature. Many workers prescribe chemotherapy for 6 months while some continue it for 9 to 12 months.15 British Medical Research Council suggests that tuberculosis of the spine should be treated with combination chemotherapy for 6–9 months. However, most of the authorities in India prefer to give anti tubercular therapy for 18 months (4HRZE+14HR).16 According to the most recent recommendations issued in 2003 by the US Centres for Disease Control and Prevention, the Infectious Diseases Society of America and the American Thoracic Society, a four-drug regimen should be used empirically to treat Pott’s disease.17 These include isoniazid (H), rifampicin (R), pyrazinamide (Z) and ethambutol (E). In children, ethambutol is replaced by streptomycin.
Learning points.
-
▶
Tuberculosis often surprises by presenting at some very unusual site like sacrum.
-
▶
Although a rare cause of isolated sacral lesion, tuberculosis should be considered in differential diagnosis along with neoplasms.
-
▶
Radiographs alone are not reliable for making a correct diagnosis of skeletal tuberculosis. Other radiological investigations like MRI and histopathological confirmation are required for the same.
Footnotes
Competing interests None.
Patient consent Obtained.
References
- 1.World Health Organization. Stop TB Partnership. 2009 update Tuberculosis Factsheet http://www.who.int/tb/publications/2009/tbfactsheet_2009update_on_page.pdf (accessed 22 September 2011).
- 2.Engin G, Acunaş B, Acunaş G, et al. Imaging of extrapulmonary tuberculosis. Radiographics 2000;20:471–88 [DOI] [PubMed] [Google Scholar]
- 3.Goodman PC. Tuberculosis and AIDS. Radiol Clin North Am 1995;33:707–17 [PubMed] [Google Scholar]
- 4.Bloom BR, Murray CJ. Tuberculosis: commentary on a reemergent killer. Science 1992;257:1055–64 [DOI] [PubMed] [Google Scholar]
- 5.Kumar A, Varshney MK, Trikha V. Unusual presentation of isolated sacral tuberculosis. Joint Bone Spine 2006;73:751–2 [DOI] [PubMed] [Google Scholar]
- 6.Davidson PT, Horowitz I. Skeletal tuberculosis. A review with patient presentations and discussion. Am J Med 1970;48:77–84 [DOI] [PubMed] [Google Scholar]
- 7.Yao DC, Sartoris DJ. Musculoskeletal tuberculosis. Radiol Clin North Am 1995;33:679–89 [PubMed] [Google Scholar]
- 8.Harisinghani MG, McLoud TC, Shepard JA, et al. Tuberculosis from head to toe. Radiographics 2000;20:449–70 [DOI] [PubMed] [Google Scholar]
- 9.Punia VPS, Kumar S. Atypical manifestation of sacral tuberculosis as Cauda-conus syndrome. JIACM 2008;9:57–6 [Google Scholar]
- 10.Campbell WC. An analysis of 51 bone and joint affections treated by heliotherapy, with special reference to tuberculosis. J Bone Joint Surg Am 1917;2:1–16 [Google Scholar]
- 11.Pun WK, Chow SP, Luk KD, et al. Tuberculosis of the lumbosacral junction. Long-term follow-up of 26 cases. J Bone Joint Surg Br 1990;72:675–8 [DOI] [PubMed] [Google Scholar]
- 12.Murphey MD, Andrews CJ, Flemming DJ, et al. Primary tumors of the spine: radiologic pathologic correlation. RadioGraphics 1996;16:1131–58 [DOI] [PubMed] [Google Scholar]
- 13.Gerber S, Ollivier L, Leclère J, et al. Imaging of sacral tumours. Skeletal Radiol 2008;37:277–89 [DOI] [PubMed] [Google Scholar]
- 14.Llauger J, Palmer J, Amores S, et al. Primary tumors of the sacrum: diagnostic imaging. AJR Am J Roentgenol 2000;174:417–24 [DOI] [PubMed] [Google Scholar]
- 15.Cabral MML, Azevedo BCCDA, Montenegro LML, et al. Tuberculous spondylitis in teenager. J Bras Pneumol 2005;31:261–4 [Google Scholar]
- 16.Chauhan A, Gupta BB. Spinal tuberculosis. J Indian Acad Clin Med 2007;8:110–4 [Google Scholar]
- 17.Leibert E, Haralambou G. Tuberculosis. In: Rom WN, Garay S, eds. Spinal Tuberculosis. Needham, MA: Lippincott Williams and Wilkins; 2004:565–77 [Google Scholar]