Many cancer patients continue to smoke after diagnosis, increasing their risk for treatment complications, reduced treatment efficacy, secondary cancers, and reduced survival. Outpatient oncology providers may not be using the “teachable moment” of cancer diagnosis to provide smoking cessation assistance. Additional training and clinic-based interventions may improve adherence to tobacco cessation practice guidelines in the outpatient oncology setting.
Keywords: Smoking cessation, Clinical oncology, Health care providers, Cancer
Learning Objectives
After completing this course, the reader will be able to:
Describe current smoking cessation assessment and counseling behaviors of outpatient oncology providers.
Identify key barriers to providing smoking cessation services identified by oncology providers.
Describe available resources for enhancing training in smoking cessation counseling.
This article is available for continuing medical education credit at CME.TheOncologist.com
Abstract
Purpose.
Many cancer patients continue to smoke after diagnosis, increasing their risk for treatment complications, reduced treatment efficacy, secondary cancers, and reduced survival. Outpatient oncology providers may not be using the “teachable moment” of cancer diagnosis to provide smoking cessation assistance.
Providers and Methods.
Physicians and midlevel providers (n = 74) who provide outpatient oncology services completed an online survey regarding smoking cessation counseling behaviors, beliefs, and perceived barriers. Outpatient medical records for 120 breast, lung, head and neck, colon, prostate, and acute leukemia cancer patients were reviewed to assess current smoking cessation assessment and intervention documentation practices.
Results.
Providers reported commonly assessing smoking in new patients (82.4% frequently or always), but rates declined at subsequent visits for both current smokers and recent quitters. Rates of advising patients to quit smoking were also high (86.5% frequently or always), but <30% of providers reported frequently or always providing intervention to smoking patients (e.g., nicotine replacement therapy or other medications, self-help materials, and/or referrals). Only 30% of providers reported that they frequently or always followed up with patients to assess progress with quitting. Few providers (18.1%) reported high levels of confidence in their ability to counsel smoking patients. Patients' lack of motivation was identified as the most important barrier to smoking cessation.
Conclusions.
Although beliefs about providing cessation services to smoking patients were generally positive, few providers reported commonly providing interventions beyond advice to quit. Additional training and clinic-based interventions may improve adherence to tobacco cessation practice guidelines in the outpatient oncology setting.
Introduction
Continued smoking after a cancer diagnosis has been linked with several adverse outcomes for cancer patients, including treatment complications [1–4], reduced treatment efficacy or need for increased treatment dose [5, 6], reductions in survival [7, 8], increased risk of secondary cancers [9], and diminished quality of life [10, 11] (for reviews, see [12–14]). Unfortunately, an estimated 10%–60% of cancer patients smoke after cancer diagnosis [15–18], with variation depending on the cancer site and time since diagnosis.
Although cancer diagnosis and treatment may be “teachable moments” for smoking cessation [19, 20], these opportunities may be underutilized by health care professionals. The impact of physicians' advice on smoking behavior may be particularly compelling during cancer treatment, when patients rely heavily on clinicians for support and are generally more motivated to quit [5]. Despite the demonstrated efficacy of provider interventions [21, 22], only about 40% of cancer survivors in national surveys report that a provider had asked them about their smoking in the last year [23, 24]. Advice to quit by a medical professional, most commonly a physician, is reported by 60%–80% of cancer patients who currently smoke [24–26]. In one recent study, 65% of smoking patients being treated for lung or head and neck cancer reported that they were offered smoking cessation assistance by a medical professional [26]. Half of the current smokers reported interest in smoking cessation programs.
In the oncology setting, minimal research concerning patient-provider interactions regarding tobacco use has occurred. In one survey, 61% of U.S. oncologists reported providing smoking cessation counseling, but no information was available about specific services provided or provider beliefs [26, 27]. A study of 63 Russian oncologists reported that they rarely offered cessation treatment but desired additional training in smoking cessation counseling [28]. Smoking cessation practices and beliefs might differ in countries where smoking cessation treatments are more accessible. In one small qualitative study of U.S. oncology patients and providers [29], oncology providers reported high levels of comfort in discussing smoking with patients, but both patients and providers described limited direct physician involvement in cessation assistance. Oncology patients did not view the message to quit as strong or helpful, and relapsed patients were reluctant to discuss their smoking behavior with their oncology providers.
There may be both general and oncology-specific reasons for the lack of communication about smoking cessation between oncology providers and cancer patients. Some oncology providers may feel that it is not their role [29] or may find that smoking is overlooked in the initial treatment plan. Others may lack knowledge and training about tobacco cessation [28]. Negative beliefs among general practitioners and family physicians include views that such discussions are too time-consuming, ineffective, or unpleasant [30]. It is unknown if these beliefs are common among oncology providers.
The purpose of this study was to (a) describe smoking assessment and intervention practices of oncology providers at a comprehensive cancer center using a survey and medical record review and (b) examine beliefs regarding smoking cessation counseling and perceived barriers toward providing cessation services in the outpatient oncology setting. Understanding the beliefs and current practices of oncology providers with regards to smoking cessation will provide crucial data to inform provider, systems, and policy interventions to promote smoking cessation among cancer patients.
Materials and Methods
Participants
We consulted cancer center and oncology service line administrators, and reviewed the cancer center website and physician directories to locate health care providers (physicians, nurse practitioners, and physician assistants) who provide outpatient oncology services at a comprehensive cancer center in the southeast United States. Providers were e-mailed a link to complete a confidential online survey in July and August 2011, with a reminder e-mail 10 days later. The study was approved by the institutional review board. All participants provided informed consent and were offered a chance to win one of two $25 gift cards.
Survey Questions
We used an initial screening question to confirm that respondents provide outpatient services to cancer patients before they completed additional survey questions. Eligible providers were asked about the frequency with which they (a) assess and document smoking at the initial visit, (b) ask identified smokers and recent quitters about their smoking at subsequent visits, and (c) document smoking status at subsequent visits. Providers were also asked how frequently they engage in seven tobacco intervention strategies during outpatient oncology encounters (advise the patient to quit smoking, advise setting a quit date, follow-up after the quit date, refer to smoking cessation programs, discuss withdrawal symptoms, prescribe/recommend nicotine replacement therapy (NRT), prescribe/recommend other pharmacotherapies [e.g., varenicline (Chantix) or bupropion], and provide self-help materials) using questions adapted from Gottlieb and colleagues [31]. These assessment and intervention items were coded on a 5-point Likert-type scale from rarely (0%–20% of the time) to always (81%–100% of the time). Additional questions assessed average length of smoking cessation counseling, confidence in ability to counsel smokers, perceived success in helping patients quit smoking, referrals to the state tobacco quit line, and interest in obtaining smoking cessation training.
We adapted eight questions about beliefs from existing surveys [28, 32] to assess the perception that providing smoking cessation counseling is an appropriate role for oncology providers, is effective, can be an unpleasant interpersonal experience, benefits cancer patients, and is appropriate for patients with advanced disease. These questions were rated on a 6-point Likert-type scale from 1 (strongly disagree) to 6 (strongly agree). Nine questions assessing barriers to addressing smoking in three domains—patient (lack of motivation, not an immediate concern, not listening to advice), physician (lack of training, not a priority, forgetting to discuss), and structural (lack of time, lack of reimbursement, lack of information/knowledge on referrals)—were adapted from Young and Ward [33]. These items were coded on a 4-point Likert-type scale ranging from 1 (not at all important) to 4 (very important). We also asked providers to identify their profession, primary cancer sites treated, area of specialization, years in practice, gender, age, race/ethnicity, and personal smoking history. Providers were also asked to estimate the percent of their outpatient oncology patients who smoke cigarettes.
Medical Record Review
We obtained lists of patients diagnosed with breast, lung, head and neck, colon, prostate, and acute leukemia in 2009 from the institutional cancer registry. These are among the most commonly treated cancers at the institution and are both smoking-related and not smoking-related. After stratifying by cancer type, we generated a random list of patients. We eliminated patients without at least three outpatient oncology visits before June 2010 and/or who were under 18 years of age, until we obtained 20 patients per site (n = 120). A medical student reviewed three outpatient encounters (the first and the two most recent encounters) from the electronic medical record for each selected case and coded documentation of smoking status and smoking cessation interventions for current smokers. We did not include encounters limited to treatment or procedures (e.g., administration of chemotherapy or surgery notes).
Statistical Analyses
Descriptive statistics were calculated to characterize provider characteristics, smoking assessment and documentation practices, frequency of cessation intervention behaviors, and beliefs and perceived barriers. We also used multivariable logistic regression to identify significant predictors of “frequently” or “always ” providing assistance to quit (setting quit date, referring to program, preparing for withdrawal, prescribing or recommending NRT or other medications, or providing self-help materials) and assessing progress with quitting. These models controlled for provider type (physician versus other), gender, and years in practice. All statistical tests were performed at a two-sided alpha level of 0.05 using SAS (v. 9.2, Cary, NC).
Results
Provider Characteristics
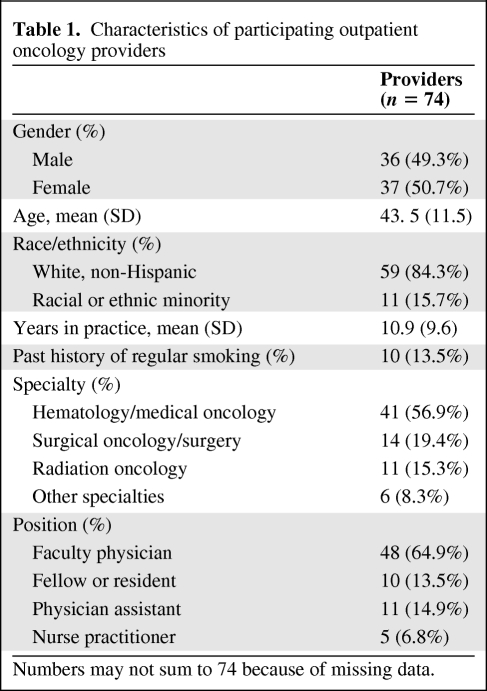
We e-mailed 174 potentially eligible providers; 111 completed the initial screening question. Of these, 93 provided cancer care to outpatients and were eligible to continue. After excluding providers who completed less than half of the survey, the final analytic sample was 74 providers (47.1% of study population minus known ineligible providers). Demographic characteristics of these providers are shown in Table 1. Most respondents were physicians (78.4%). A regular history of prior smoking (>100 cigarettes ever) was reported by 13.5% of the providers, but there were no current smokers. Approximately half of the respondents identified their specialty as hematology or medical oncology (56.9%). The most common cancer types treated by respondents included breast (36.5%), leukemias/lymphomas (35.1%), pancreatic (27.0%), urologic (25.7%), and thoracic (25.7%). Provider estimates of current smokers among their patients ranged from 3% to 90% (mean = 36.9%).
Table 1.
Characteristics of participating outpatient oncology providers
Numbers may not sum to 74 because of missing data.
Smoking Cessation Practices
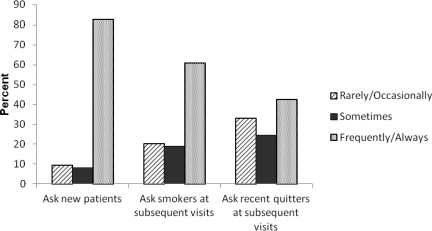
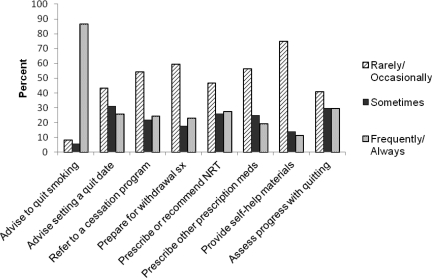
Providers reported commonly assessing smoking in new patients (82.4% frequently or always), but assessment rates declined at subsequent visits for both current smokers (60.8% frequently or always) and recent quitters (42.5% frequently or always) (Fig. 1). Rates of advising patients to quit smoking were also high (86.5% frequently or always), but the frequency of any other cessation interventions was much lower (see Fig. 2). Less than 30% of outpatient oncology providers reported frequently or always providing intervention to smoking patients, including referrals, NRT or other medications, self-help materials, preparation for withdrawal, or advice to set a specific quit date. Only 30% of providers reported that they frequently or always followed up with patients to assess progress with quitting. Only 28.4% of providers had referred a patient to the free state tobacco quit line; 48.7% were unaware of this service.
Figure 1.
Frequency of oncology provider smoking assessment behaviors (self-reported).
Figure 2.
Frequency of oncology provider smoking cessation behaviors with smoking patients (self-reported).
Abbreviations: NRT, nicotine replacement therapy; sx, symptoms.
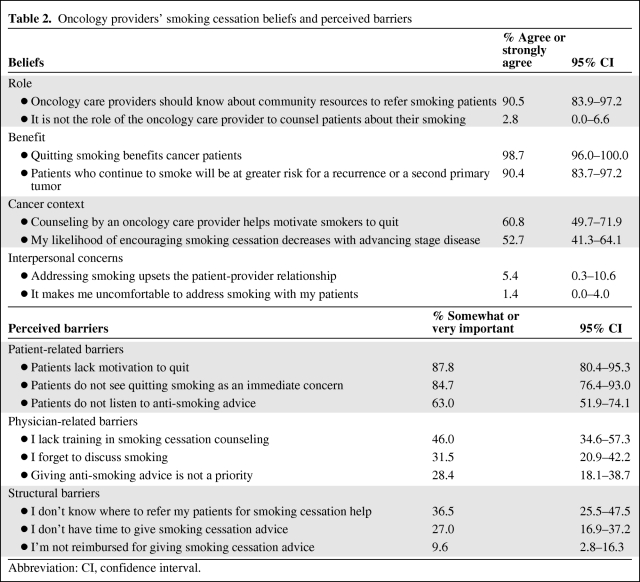
Smoking Cessation Beliefs
In general, providers held positive beliefs about smoking cessation interventions with their patients (see Table 2) and believed that counseling they delivered helped motivate smokers. Approximately half agreed or strongly agreed that they would be less likely to encourage smoking cessation among patients with advanced disease. There were few interpersonal concerns about addressing smoking. Only one respondent reported that addressing smoking with a patient was uncomfortable.
Table 2.
Oncology providers' smoking cessation beliefs and perceived barriers
Abbreviation: CI, confidence interval.
Few providers (18.1%) reported that they were very confident in their ability to counsel smokers in their outpatient oncology clinic, with 59.7% somewhat confident and 22.2% not at all confident. No providers felt their efforts at helping patients quit smoking were very successful; 68.9% reported that their efforts were somewhat successful, and 31.1% reported that they were not at all successful. Almost all providers reported that they would like further training to provide cessation assistance (9.5% not at all, 39.2% a little bit, 31.1% quite a bit, and 20.3% very much).
Smoking Cessation Barriers
Oncology providers viewed patient-related barriers (i.e., lack of motivation, not seeing quitting as an immediate concern, and not listening to anti-smoking advice) as key barriers to smoking cessation, with 60%–88% reporting them as somewhat or very important influences on their interactions with smoking patients. Lack of training, forgetting, and not knowing where to refer were cited by 30%–40% of providers. Fewer providers viewed low prioritization of smoking cessation (28.4%), lack of time (27.0%), and lack of reimbursement (9.6%) as important barriers.
Predictors of Providing Assistance To Quit and Assessing Progress with Quitting
Providing Assistance
After controlling for provider type, gender, and years in practice, providers who reported that lack of referral sources was an important barrier were more likely (OR = 4.9, 95% confidence interval [CI] = 1.4–16.3) to frequently or always provide assistance to quit. In addition, those who reported that lacking training was an important barrier were less likely (OR = 0.3, 95% CI = 0.1–0.8) to report providing assistance to quit. There was a trend towards increased assistance among providers who perceived themselves as more successful (OR = 3.3, 95% CI = 0.9–12.1), but it was not statistically significant. Smoking cessation beliefs were not a significant predictor of assistance to quit.
Assessing Progress
Providers who endorsed lack of training as a very or somewhat important barrier were less likely (OR = 0.2, 95% CI = 0.07–0.77) to assess progress, and those who were very confident compared to not at all confident were significantly more likely to frequently or always assess progress (OR = 15.7, 95% CI = 1.4–171.6). Neither provider specialty nor sites treated (head/neck/lung versus others) was a significant predictor of providing quit assistance or assessing progress.
Documentation of Smoking Information in Medical Records
Smoking status at the initial visit was documented in the medical record for most patients (rates ranging from 60% to 95% by cancer type), but there was significant variability across cancer sites [χ2 (5 degrees of freedom (df)) = 25.64, p < .0001]. Prostate and lung cancer patients had the highest rates, and acute leukemia patients had the lowest rates. Documentation dropped off significantly at follow-up appointments [χ2 (1 df) = 72.05, p < .0001], with rates ranging from 5% to 80%. At follow-up, the prostate and lung cancer patients had the highest rates of smoking documentation. We identified 40 of the patients as either current smokers (n = 34) or recent quitters who reported quitting within the last 6 months (n = 6). Of this subset, 19 (47.5%) had documentation of their current smoking status at one or more of the follow-up visits. Only 11.8% of the 34 current smokers had documentation of smoking cessation interventions delivered at the initial visit. Of current smokers documented at follow-up (n = 15), 40% had documentation of intervention.
Discussion
To our knowledge, this study is the first to describe the smoking cessation beliefs and behaviors of a sample of U.S. oncology physicians and midlevel providers. Although most oncology providers reported advising patients to quit smoking, only 15%–30% reported providing interventions to assist their patients in smoking cessation. Providers reported moderate confidence and success in their counseling efforts. Up to 40% of clinicians stated that they lacked training in, forgot about, or did not know where to refer patients for further tobacco treatment. Our finding that providers who did not know where to refer provided more intervention may reflect more intervention efforts by those who perceived great need but few resources for smoking cancer patients. Our results are consistent with the findings of a national survey of non-oncology health care providers that also found relatively low rates of self-reported smoking cessation interventions by specialists (15%–29% of emergency medicine and 29%–64% of psychiatry providers [34]). The results are also similar to a previous study of oncology nurses, which found limited knowledge and relatively low rates of tobacco cessation intervention and also identified perceived low patient motivation as a key barrier [35].
It has recently been argued that oncologists have an ethical responsibility to strongly advise all their patients to quit smoking and to offer cessation treatment [36]. The American Society of Clinical Oncology (ASCO) has also urged all oncologists to integrate tobacco cessation and control in their practices [37] and has developed a tobacco control module in its Cancer Prevention Curriculum [38]. Smoking status documentation and cessation counseling by the second visit are included as ASCO Quality Oncology Practice Initiative (QOPI) quality measures. The National Cancer Institute (NCI) recently sponsored a meeting on treatment of tobacco dependence at NCI-designated cancer centers [39]. Recommendations from this conference included treating tobacco use as a “vital sign” on patient charts and implementation of evidence-based tobacco treatment guidelines in the oncology setting. Barriers identified qualitatively during this conference were confirmed by our survey (e.g., limited knowledge about tobacco treatment, perception that patients are not motivated to quit). However, our respondents placed less importance on other identified barriers (e.g., low prioritization of smoking by providers, lack of time, and lack of reimbursement) [39].
The high perceived importance of smoking cessation but only moderate levels of confidence and perceived success among oncology providers in our sample suggest that provider education might increase the proportion of cancer patients who receive evidence-based treatment for tobacco cessation, especially because providers who expressed that lack of training was a barrier to offering tobacco interventions were significantly less likely to do so. Our data suggest that oncology providers are open to receiving such training. Rx for Change [40], an online training program, offers a tailored program targeted to cancer care providers drawing on the Public Health Service (PHS) guidelines [22].
A recent meta-analysis suggests that even 3 minutes of provider advice and counseling may increase the odds of tobacco abstinence by 30% [22]. However, in a study of physician-based intervention consisting of quit advice and assistance in 432 cancer patients, no significant differences emerged between the usual care and intervention groups at either 6 or 12 months, and quit rates were relatively low (12%–14%) [41]. Physician-based interventions may need to be combined with higher-intensity behavioral and pharmacologic interventions to increase long-term cessation among cancer patients.
The PHS Guidelines also recommend the following system-level interventions: (a) implementing a tobacco-user identification system; (b) providing education, resources, and feedback to promote provider intervention; (c) dedicating staff to provide tobacco dependence treatment; (d) promoting policies that support services; (e) including evidence-based tobacco treatments as paid or covered services; and (f) reimbursing clinicians for delivery of evidence-based treatments. Research is needed to test whether these system-level strategies would effectively augment provider training in the oncology setting. Smoking cessation in the oncology setting has also been highlighted as an area for dissemination and implementation research in the cancer survivorship context [42].
Although rates of documentation of smoking status at the initial visit were high, less than half of current or recent smokers had smoking status documented at one or more follow-up visits. This finding is consistent with our provider reports. Higher rates of smoking assessment documentation may have been related to use of clinic note templates that included a field for smoking history. Medical records do not indicate whether smoking status was actually assessed at follow-up rather than simply copied forward from a previous note. We found that smoking cessation interventions were documented in the charts of <20% of identified smokers at the initial visit. These data are very similar to those reported from oncology practices participating in the QOPI program, which found documentation of smoking cessation counseling in only 25% of smoking oncology patients [43]. Lack of documentation does not mean lack of intervention, but documentation is necessary for reimbursement for smoking cessation counseling (allowable under new Medicare guidelines) and to ensure continuity between visits and among providers. Continuity is especially important for a condition like nicotine addiction, characterized by high rates of relapse and the need for multiple interventions to achieve lasting cessation.
Primary limitations of this study include collection of data at a single institution and exclusion of oncology nurses who may also provide smoking cessation advice and treatment [44]. Although non-advanced practice nurses cannot be reimbursed for smoking cessation advice, they may offer more informal interventions to cancer patients. At the time of the survey, there was not a formal tobacco dependence treatment program for cancer patients at the surveyed institution. The results of this survey would likely not generalize to institutions with more comprehensive treatment programs in place. Our response rate, while modest, mirrors other non-oncology physician study samples on this topic [34]. Future studies should include a national sample of outpatient oncology providers (physicians, physician assistants, and nurses) and examine both local and national provider training efforts. In addition, future studies should examine the frequency and types of tobacco cessation interventions delivered to hospitalized oncology patients.
National data suggest that 40% of smoking cancer survivors report a quit attempt in the prior year [24], but their success at achieving lasting cessation may be limited without effective treatment. Both physician training and clinic-based systems for tobacco treatment could improve rates of delivery of empirically supported tobacco dependence treatments in the outpatient oncology setting, ultimately improving the health and well-being of oncology patients who smoke. These survey data suggest clear opportunities for oncology healthcare providers to encourage and assist patients in smoking cessation efforts that will likely have an impact on treatment-related outcomes.
Acknowledgments
Preliminary results were presented at the American Society of Preventive Oncology Annual Meeting in March 2011.
The authors take full responsibility for the content of the paper but thank Karen Potvin Klein, MA, ELS (Research Support Core, Wake Forest School of Medicine) for her assistance in copyediting the manuscript.
Footnotes
- (C/A)
- Consulting/advisory relationship
- (RF)
- Research funding
- (E)
- Employment
- (H)
- Honoraria received
- (OI)
- Ownership interests
- (IP)
- Intellectual property rights/inventor/patent holder
- (SAB)
- Scientific advisory board
Author Contributions
Conception/Design: Kathryn E. Weaver, Janet A. Tooze, A. William Blackstock, John Spangler, Leslie Thomas, Erin L. Sutfin
Provision of study material or patients: Kathryn E. Weaver
Collection and/or assembly of data: Kathryn E. Weaver, Janet A. Tooze, Leslie Thomas
Data analysis and interpretation: Kathryn E. Weaver, Suzanne C. Danhauer, Janet A. Tooze, Erin L. Sutfin
Manuscript writing: Kathryn E. Weaver, Suzanne C. Danhauer, Janet A. Tooze, A. William Blackstock, John Spangler, Erin L. Sutfin
Final approval of manuscript: Kathryn E. Weaver, Suzanne C. Danhauer, Janet A. Tooze, A. William Blackstock, John Spangler, Leslie Thomas, Erin L. Sutfin
References
- 1.Porock D, Nikoletti S, Cameron F. The relationship between factors that impair wound healing and the severity of acute radiation skin and mucosal toxicities in head and neck cancer. Cancer Nurs. 2004;27:71–78. doi: 10.1097/00002820-200401000-00009. [DOI] [PubMed] [Google Scholar]
- 2.Avritscher EB, Cooksley CD, Elting LS. Scope and epidemiology of cancer therapy-induced oral and gastrointestinal mucositis. Semin Oncol Nurs. 2004;20:3–10. doi: 10.1053/j.soncn.2003.10.002. [DOI] [PubMed] [Google Scholar]
- 3.Zevallos JP, Mallen MJ, Lam CY, et al. Complications of radiotherapy in laryngopharyngeal cancer. Cancer. 2009;115:4636–4644. doi: 10.1002/cncr.24499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sørensen LT, Horby J, Friis E, et al. Smoking as a risk factor for wound healing and infection in breast cancer surgery. Eur J Surg Oncol. 2002;28:815–820. doi: 10.1053/ejso.2002.1308. [DOI] [PubMed] [Google Scholar]
- 5.Gritz ER, Dresler C, Sarna L. Smoking, the missing drug interaction in clinical trials: ignoring the obvious. Cancer Epidemiol Biomarkers Prev. 2005;14:2287–2293. doi: 10.1158/1055-9965.EPI-05-0224. [DOI] [PubMed] [Google Scholar]
- 6.Waller LL, Miller AA, Petty WJ. Using erlotinib to treat patients with non-small cell lung cancer who continue to smoke. Lung Cancer. 2010;67:12–16. doi: 10.1016/j.lungcan.2009.08.014. [DOI] [PubMed] [Google Scholar]
- 7.Gritz ER, Demark-Wahnefried W. Health behaviors influence cancer survival. J Clin Oncol. 2009;27:1930–1932. doi: 10.1200/JCO.2008.21.3769. [DOI] [PubMed] [Google Scholar]
- 8.Holmes MD, Murin S, Chen WY, et al. Smoking and survival after breast cancer diagnosis. Int J Cancer. 2007;120:2672–2677. doi: 10.1002/ijc.22575. [DOI] [PubMed] [Google Scholar]
- 9.Kawahara M, Ushijima S, Kamimori T, et al. Second primary tumours in more than 2-year disease-free survivors of small-cell lung cancer in Japan: the role of smoking cessation. Br J Cancer. 1998;78:409–412. doi: 10.1038/bjc.1998.507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schnoll RA, Malstrom M, James C, et al. Correlates of tobacco use among smokers and recent quitters diagnosed with cancer. Patient Educ Couns. 2002;46:137–145. doi: 10.1016/s0738-3991(01)00157-4. [DOI] [PubMed] [Google Scholar]
- 11.Garces YI, Yang P, Parkinson J, et al. The relationship between cigarette smoking and quality of life after lung cancer diagnosis. Chest. 2004;126:1733–1741. doi: 10.1378/chest.126.6.1733. [DOI] [PubMed] [Google Scholar]
- 12.National Cancer Institute. Smoking Cessation and Continued Risk in Cancer Patients (PDQ) Health Professional Version. 2008. [accessed June 10, 2011]. Available at http://www.cancer.gov/cancertopics/pdq/supportivecare/smokingcessation/healthprofessional.
- 13.de Moor JS, Elder K, Emmons KM. Smoking prevention and cessation interventions for cancer survivors. Semin Oncol Nurs. 2008;24:180–192. doi: 10.1016/j.soncn.2008.05.006. [DOI] [PubMed] [Google Scholar]
- 14.Waller LL, Weaver KE, Petty WJ, et al. Effects of continued tobacco use during treatment of lung cancer. Expert Rev Anticancer Ther. 2010;10:1569–1575. doi: 10.1586/era.10.140. [DOI] [PubMed] [Google Scholar]
- 15.Walker MS, Vidrine DJ, Gritz ER, et al. Smoking relapse during the first year after treatment for early-stage non-small-cell lung cancer. Cancer Epidemiol Biomarkers Prev. 2006;15:2370–2377. doi: 10.1158/1055-9965.EPI-06-0509. [DOI] [PubMed] [Google Scholar]
- 16.McBride CM, Ostroff JS. Teachable moments for promoting smoking cessation: The context of cancer care and survivorship. Cancer Control. 2003;10:325–333. doi: 10.1177/107327480301000407. [DOI] [PubMed] [Google Scholar]
- 17.Cooley ME, Sarna L, Kotlerman J, et al. Smoking cessation is challenging even for patients recovering from lung cancer surgery with curative intent. Lung Cancer. 2009;66:218–225. doi: 10.1016/j.lungcan.2009.01.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bellizzi KM, Rowland JH, Jeffery DD, et al. Health behaviors of cancer survivors: examining opportunities for cancer control intervention. J Clin Oncol. 2005;23:8884–8893. doi: 10.1200/JCO.2005.02.2343. [DOI] [PubMed] [Google Scholar]
- 19.Gritz ER, Fingeret MC, Vidrine DJ, et al. Successes and failures of the teachable moment: smoking cessation in cancer patients. Cancer. 2006;106:17–27. doi: 10.1002/cncr.21598. [DOI] [PubMed] [Google Scholar]
- 20.McBride CM, Emmons KM, Lipkus IM. Understanding the potential of teachable moments: the case of smoking cessation. Health Educ Res. 2003;18:156–170. doi: 10.1093/her/18.2.156. [DOI] [PubMed] [Google Scholar]
- 21.Gorin SS, Heck JE. Meta-analysis of the efficacy of tobacco counseling by health care providers. Cancer Epidemiol Biomarkers Prev. 2004;13:2012–2022. [PubMed] [Google Scholar]
- 22.Fiore MC, Jaen CR, Baker TB, et al. Treating tobacco use and dependence: 2008 update US Public Health Service Clinical Practice Guideline executive summary. Respir Care. 2008;53:1217–1222. [PubMed] [Google Scholar]
- 23.Sabatino SA, Coates RJ, Uhler RJ, et al. Provider counseling about health behaviors among cancer survivors in the United States. J Clin Oncol. 2007;25:2100–2106. doi: 10.1200/JCO.2006.06.6340. [DOI] [PubMed] [Google Scholar]
- 24.Coups EJ, Dhingra LK, Heckman CJ, et al. Receipt of provider advice for smoking cessation and use of smoking cessation treatments among cancer survivors. J Gen Intern Med. 2009;24(Suppl 2):S480–S486. doi: 10.1007/s11606-009-0978-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Demark-Wahnefried W, Peterson B, McBride C, et al. Current health behaviors and readiness to pursue life-style changes among men and women diagnosed with early stage prostate and breast carcinomas. Cancer. 2000;88:674–684. [PubMed] [Google Scholar]
- 26.Cooley ME, Emmons KM, Haddad R, et al. Patient-reported receipt of and interest in smoking-cessation interventions after a diagnosis of cancer. Cancer. 2011;117:2961–2969. doi: 10.1002/cncr.25828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ganz PA, Kwan L, Somerfield MR, et al. The role of prevention in oncology practice: results from a 2004 Survey of American Society of Clinical Oncology Members. J Clin Oncol. 2006;24:2948–2957. doi: 10.1200/JCO.2006.05.8321. [DOI] [PubMed] [Google Scholar]
- 28.Schnoll R, Engstrom P, Subramanian S, et al. Smoking cessation counseling by russian oncologists: opportunities for intervention in the Russian federation. Int J Behav Med. 2006;13:8–15. doi: 10.1207/s15327558ijbm1301_2. [DOI] [PubMed] [Google Scholar]
- 29.Simmons VN, Litvin EB, Patel RD, et al. Patient-provider communication and perspectives on smoking cessation and relapse in the oncology setting. Patient Educ Couns. 2009;77:398–403. doi: 10.1016/j.pec.2009.09.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Vogt F, Hall S, Marteau TM. General practitioners' and family physicians' negative beliefs and attitudes towards discussing smoking cessation with patients: a systematic review. Addiction. 2005;100:1423–1431. doi: 10.1111/j.1360-0443.2005.01221.x. [DOI] [PubMed] [Google Scholar]
- 31.Gottlieb NH, Guo JL, Blozis SA, et al. Individual and contextual factors related to family practice residents' assessment and counseling for tobacco cessation. J Am Board Fam Pract. 2001;14:343–351. [PubMed] [Google Scholar]
- 32.O'Loughlin J, Makni H, Tremblay M, et al. Smoking cessation counseling practices of general practitioners in Montreal. Prev Med. 2001;33:627–638. doi: 10.1006/pmed.2001.0937. [DOI] [PubMed] [Google Scholar]
- 33.Young JM, Ward JE. Implementing guidelines for smoking cessation advice in Australian general practice: opinions, current practices, readiness to change and perceived barriers. Fam Pract. 2001;18:14–20. doi: 10.1093/fampra/18.1.14. [DOI] [PubMed] [Google Scholar]
- 34.Tong EK, Strouse R, Hall J, et al. National survey of U.S. health professionals' smoking prevalence, cessation practices, and beliefs. Nicotine Tob Res. 2010;12:724–733. doi: 10.1093/ntr/ntq071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sarna LP, Brown JK, Lillington L, et al. Tobacco interventions by oncology nurses in clinical practice: report from a national survey. Cancer. 2000;89:881–889. [PubMed] [Google Scholar]
- 36.Pentz RD, Berg CJ. Smoking and ethics: what are the duties of oncologists? The Oncologist. 2010;15:987–993. doi: 10.1634/theoncologist.2010-0034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zon RT, Goss E, Vogel VG, et al. American Society of Clinical Oncology policy statement: the role of the oncologist in cancer prevention and risk assessment. J Clin Oncol. 2009;27:986–993. doi: 10.1200/JCO.2008.16.3691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.American Society of Clinical Oncology. Alexandria, VA: 2011. [accessed on September 10, 2011]. ASCO Cancer Prevention Resources. Available at http://www.asco.org/ascov2/Practice+&+Guidelines/Quality+Care/Cancer+Prevention. [Google Scholar]
- 39.Morgan G, Schnoll RA, Alfano CM, et al. National Cancer Institute Conference on Treating Tobacco Dependence at Cancer Centers. J Oncol Pract. 2011;7:178–182. doi: 10.1200/JOP.2010.000175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.University of California San Francisco. Rx for change: clinician-assisted tobacco cessation program. 2011. [accessed on August 8, 2011]. Available at http://rxforchange.ucsf.edu.
- 41.Schnoll RA, Zhang B, Rue M, et al. Brief physician-initiated quit-smoking strategies for clinical oncology settings: a trial coordinated by the Eastern Cooperative Oncology Group. J Clin Oncol. 2003;21:355–365. doi: 10.1200/JCO.2003.04.122. [DOI] [PubMed] [Google Scholar]
- 42.Wolin KY, Colditz GA, Proctor EK. Maximizing benefits for effective cancer survivorship programming: defining a dissemination and implementation plan. The Oncologist. 2011;16:1189–1196. doi: 10.1634/theoncologist.2011-0054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Tobacco cessation and quality cancer care. J Oncol Pract. 2009;5:2–5. doi: 10.1200/JOP.0913501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cooley ME, Sipples RL, Murphy M, et al. Smoking cessation and lung cancer: oncology nurses can make a difference. Semin Oncol Nurs. 2008;24:16–26. doi: 10.1016/j.soncn.2007.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]