Abstract
At one major urban academic medical center, patients aged 50 years and older with fragility fractures were identified and scheduled or assisted in referral into osteoporosis medical management appointments. We evaluated the efficacy of an active intervention program at overcoming the logistical barriers and improving proper osteoporosis follow-up for persons who have sustained a fragility fracture. Of 681 patients treated for defined fractures, 168 were eligible and consented for the study of fragility fractures. Of those enrolled, 91 (54.2%) had appropriate osteoporosis follow-up on initial interview, and overall 120 (71.4%) had successful osteoporosis follow-up following our active intervention. Seventy patients (41.7%) were deemed to have no osteoporosis follow-up, and, of these, 48 were successfully referred to a scheduling coordinator. The scheduling coordinator was able to contact 37 (77%) patients to schedule proper follow-up, and, of these, 29 (78.4%) confirmed receiving an appropriate follow-up appointment. Active intervention and assisted scheduling for patients with recent fragility fractures improved the self-reported rate of osteoporosis follow-up from 54.2% to 71.4%.
1. Introduction
Osteoporosis is a worldwide public health problem that is preventable and treatable with appropriate medical follow-up and care. It is the primary etiology of fragility fractures among the elderly and represents a significant factor of morbidity and mortality within this population. Despite substantial evidence that a prior fragility fracture results in an increased risk of a subsequent fracture, less than 30% of postmenopausal women and less than 10% of men with prior fracture are treated for osteoporosis [1–3].
With increasing life expectancy and a concomitant growth in the proportion of the elderly population, fracture incidence is expected to increase 2- to 4-fold in the next decade [1]. As a prior history of fracture is one of the biggest risk factors for future fractures, effective interventions to improve osteoporosis care in this particular at-risk patient population are needed.
The aim of this interventional study was to evaluate a large academic institution's active program to improve osteoporosis follow-up after being treated for a fragility fracture. We hypothesized that by identifying, actively scheduling, and referring these patients, we could improve the rate of osteoporosis follow-up treatment over current national figures.
2. Methods
The eligible study population included patients over the age of 50 years with fragility fractures treated at an orthopaedic hospital in Los Angeles, CA between April, 2009 and March, 2010. Potential study subjects were identified by ICD-9 codes representing the following fracture types: (1) vertebral column 805.8; (2) pubis 808.2; (3) humerus 812.00; (4) distal radius 813.42; (5) femoral neck 820.00; (6) pertrochanteric, open 820.03; (7) pertrochanteric, closed 820.20; (8) intertrochanteric 820.21; (9) subtrochanteric 820.22; (10) unspecified part of femoral neck, closed 820.80 (Table 1). Additional inclusion criteria were age greater than 50 years for females and 55 years for males and a fracture sustained during a low-energy fall (fall from standing height or less). Exclusion criteria were fractures sustained as a result of a primary or metastatic tumor or high-energy mechanism (e.g., motor vehicle accident) and if the patient was deceased, unable to communicate in English, unable to clearly communicate (e.g., due to dementia, other), refused to participate in the study, or was unavailable for interview following 3 separate telephone attempts.
Table 1.
ICD-9 codes and number of study patients corresponding to defined fragility fractures.
| ICD-9 Code | Fracture | N |
|---|---|---|
| 805.8 | Vertebral column | 39 |
| 808.2 | Pubis | 19 |
| 812.00 | Humerus | 6 |
| 813.42 | Distal radius | 37 |
| 820.00 | Femoral neck | 1 |
| 820.03 | Pertrochanteric, open | 0 |
| 820.20 | Pertrochanteric, closed | 2 |
| 820.21 | Intertrochanteric | 34 |
| 820.22 | Subtrochanteric | 6 |
| 820.80 | Unspecified part of femoral neck, closed | 24 |
Between April 2009 and March 2010, 681 patients treated for the fractures described above were treated at our institution. Based on fragility fracture study criteria, initial telephone screening of 520 fragility fracture patients was performed by three research staff within 8–12 weeks of the patient's discharge date. Three hundred and thirty patients were ineligible for study: 253 were below inclusion age criteria, 6 were deceased, 16 were too ill, 8 denied having a fracture, 9 were unable to communicate in English, 9 reported having a fracture due to high-energy trauma, 3 were considered to have a pathologic fracture, and 26 were not included for reasons including having an incorrectly coded discharge diagnosis or previous history of fracture that occurred outside of the study period. Of the 681 patients treated for the above fractures, 161 (37.6%) were unable to be contacted following 3 separate telephone attempts, leaving 351 patients eligible for fragility fracture study. One hundred ninety patients (36.5%) were successfully contacted and deemed eligible to participate in the study. Twenty-two (11.6%) refused to participate. Once the patient consented to study participation, a telephone-administered questionnaire (Table 2) was used to identify those fragility fracture patients who were not medically treated or who did not have osteoporosis follow-up care within 8–12 weeks following initial fracture. Researchers recorded the responses to a 5-point questionnaire in a unique password-protected spreadsheet. If patients answered “no” to question 3 (“Are you currently seeing a primary care doctor or osteoporosis specialist for your bone health?”) and a successive “no” to question 5 of the telephone script (“Are you currently being treated for osteoporosis?”), they were deemed to have insufficient or no osteoporosis follow-up care. Appropriate follow-up care in our initial and closeout interviews included vitamin D and calcium, and/or a bisphosphonate, a completed or scheduled appointment with a physician regarding osteoporosis, or a completed or scheduled DXA scan. These patients' names and contact information were recorded in a separate referral list for intervention. Patients who responded “yes” to question 3 or 5 were counted as receiving appropriate care.
Table 2.
Initial telephone script used to survey patients who sustained a fragility fracture 6–8 weeks after hospital encounter.
| (1) Do you know what osteoporosis is? (a) Yes (b) No (c) Not sure If answers (b) or (c), then read: let me explain osteoporosis and how it may relate to you. Osteoporosis is a disease that makes the bones in the body fragile. Some people have this disease and do not know it. Because you have had a fracture, you are at higher risk of fracturing again. |
|
|
| |
| (2) Have you ever been diagnosed with osteoporosis? (a) Yes (b) No |
|
|
| |
| (3) Are you currently seeing a primary care doctor or osteoporosis specialist for your bone health? (a) Yes (b) No (C) I do not know |
|
|
| |
| (4) Have you had a bone density study performed since your fracture? (a) Yes (b) No (c) I do not know |
|
|
| |
| (5) Are you currently being treated for osteoporosis? (a) Yes If yes, please specify prescription treatment (medication). FDA approved: bisphosphonates [fosamax (alendronate), actonel (risedronate), boniva (ibandronate), reclast (zoledronic acid)]; estrogen replacement therapy; evista (raloxifene); Forteo (teriparaitide); miacalcin nasal spray (only for vertebral fractures) (b) No (c) I do not know |
|
Education: The fracture (broken bone) that you sustained is associated with osteoporosis. Osteoporosis is a disorder of bones that results in weakened bones that are more susceptible to fracturing (breaking). Having sustained a break in your bone like you have this time places you at a significant increased risk for breaking a bone again in the future if you do not seek treatment. The National Osteoporosis Foundation recommends that patients who have had an osteoporotic fracture (as is likely in your case) have a bone density study and be placed on a prescription medication to prevent further fractures. The UCLA Department of Orthopaedic Surgery recommends that you have a follow-up visit with your primary care physician or specialist for your osteoporosis. A representative from the Osteoporosis Center will be contacting you to make an appointment in the near future.
For the active intervention, the eligible patient list was transferred on a weekly basis to an office administrator who then recontacted the patient to authorize, schedule, and refer patients to their primary care doctor, an osteoporosis specialist, or the institution's osteoporosis center.
To assess the effectiveness of the active intervention, the 3 research staff members administered a closeout interview (e.g., second telephone interview) consisting of a six-question standardized telephone script (Table 3) approximately 6–8 weeks after the first telephone interview. All patients who were contacted in the active intervention phase were eligible and contacted for a closeout interview. If the patient answered “yes” to question 1 (Did you receive follow-up care for osteoporosis since our initial phone call?), question 2 (Do you have a future appointment scheduled to follow-up on your osteoporosis?), question 4 (Did you or are you planning to have a bone density scan done?) or question 5 (Are you currently being treated for osteoporosis?), the patient was determined to have achieved proper osteoporosis follow-up and/or care. We used Chi-squared or 2-sided Student's t-tests difference of the characteristics between those who reported being treated for osteoporosis or at least seeing a MD for osteoporosis and those who did not. SAS Software was used for all analyses (SAS Institute, version 9.1, Cary, NC). The above study protocol was approved by our Institutional Review Board.
Table 3.
Follow-up telephone script used to contact patients who were deemed to have insufficient screening and treatment following a defined fragility fracture. Conducted 12–14 weeks after hospital encounter or 6 weeks following initial telephone interview.
| (1) Did you receive follow-up care for osteoporosis since our initial phone call? (a) Yes (proceed to question 3) (b) No |
|
|
| |
| (2) Do you have a future appointment scheduled to follow-up on your osteoporosis? (a) Yes (If so, when): … (skip to bottom of questionnaire and thank patient for his/her time). (b) No (If no, skip to question 6) |
|
|
| |
| (3) Did you see your primary care physician or an osteoporosis specialist? (a) Primary care physician (b) Osteoporosis specialist (c) Both |
|
|
| |
| (4) Did you or are you planning to have a bone density scan done? (a) Yes (b) No (c) I do not know |
|
|
| |
| (5) Are you currently being treated for osteoporosis? (a) Yes (Please specify treatment): … (b) No |
|
|
| |
| (6) Only if answered No on question 2: Is the reason for not seeing a primary care physician or osteoporosis specialist because of insurance issues? (a) Yes (b) No |
|
3. Results
Overall, 168 out of 190 (88%) eligible patients consented to participate in the study and were initially queried as to their awareness of osteoporosis and follow-up care achieved following their fragility fracture. The study patients' mean age was 77 (SD = 11) years. One hundred and thirty-two (79%) were female and 36 were male (Table 4). Most patients in our study sample experienced hip fractures (n = 67), with the remainder of study patients having sustained vertebral fractures (n = 39), wrist or humeral fractures (n = 43), or pelvic fractures (n = 19). Among the enrolled study participants, 91 (54.2%) were found after data analysis to either have MD follow-up for their osteoporosis or were being treated for osteoporosis. Those who reported being treated for osteoporosis or at least seeing a MD for osteoporosis were more likely to be females than males (80/91; P = 0.0004). Seventy patients (41.2%) were deemed to have insufficient follow-up following a fragility fracture and were referred to our study coordinator for the active intervention program (Figure 1). Ninety-one percent of these patients with no treatment following a fragility fracture were unaware of the association of their fracture with osteoporosis.
Table 4.
Characteristics and interview data of study participants at baseline.
| Age | 77.5 ± 11.0 |
| Sex, N (% female) | 132 (78.6%) |
| Initial interview: | N (% Yes) |
| Know what osteoporosis is? | 144 (85.7%) |
| Diagnosed with osteoporosis? | 67 (39.9%) |
| Seeing a primary care doctor or osteoporosis specialist for bone health? | 87 (51.8%) |
| Ever had bone density study performed since fracture? | 40 (23.8%) |
| Being treated for osteoporosis? | 67 (39.9%) |
Figure 1.
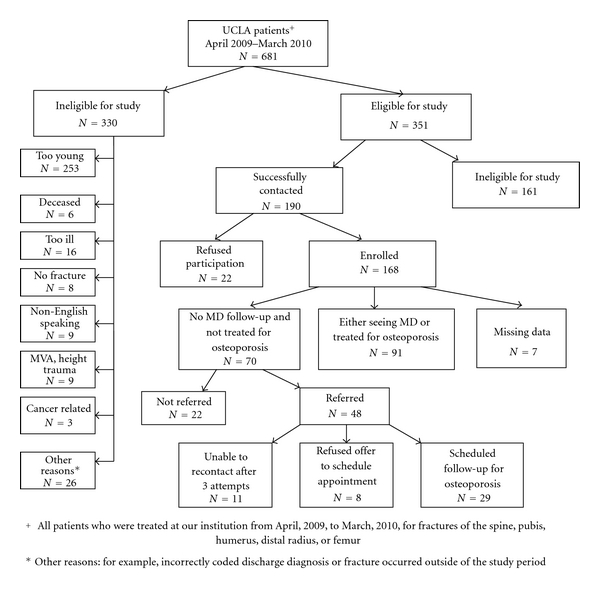
Flow chart of study enrollment and success.
Seventy-eight percent of the enrolled patients entered into the active intervention program and successfully recontacted after the initial telephone screening achieved proper medical treatment or follow-up for osteoporosis (29/37). By the closeout interview, 19 patients had already received follow-up care and were being treated by their primary care provider or osteoporosis specialist. Nine patients had a confirmed appointment scheduled with the institution Osteoporosis Center, 5 had scheduled appointments with outside providers for bone health, and 4 had scheduled appointments for a DXA scan. Our study osteoporosis follow-up rate following initial interview was 54.2% (91/168), and, with an improvement of 17.2% (29/168) following active intervention, our study overall osteoporosis follow-up rate was 71.4%.
4. Discussion
A number of interventional studies have attempted to increase rates of screening and treatment for osteoporosis with varying success. One of the key barriers has been the low rates of referral by orthopaedic surgeons to osteoporosis services and primary care physicians for secondary prevention of fragility fractures [4]. In the majority of these studies, emergency room personnel or nurse assistants conducted the interventions. Orthopaedic surgeons have conducted osteoporosis interventions in the inpatient and outpatient clinical setting [5–8]; however, to our knowledge, no published studies have examined the success of a simple telephone intervention on osteoporosis treatment following a fragility fracture.
In a prospective, randomized trial involving 80 patients admitted to an academic medical center for a low-energy fracture, Gardner et al. conducted 15-minute discussions with patients regarding the association between their fracture and osteoporosis [5]. Upon discharge, these patients were provided with 5 questions regarding osteoporosis treatment to be given to their primary care providers and were reminded about the questions during a telephone follow-up call six weeks after discharge. Patients in the control group received an informational brochure describing methods for fall prevention. The authors concluded that patients in the study group had significantly higher rates of osteoporosis follow-up compared to the control group (P = 0.04). Though osteoporosis education and intervention in an inpatient setting by orthopaedic surgeons is ideal and has been demonstrated to be effective, it is difficult to standardize the quality and compliance of this intervention in a large academic institution, where residents and nurse practitioners often complete the discharge process.
The rate of osteoporosis follow-up following a fragility fracture has been reported to be between 19% and 76% with the use of clinical intervention protocols. One recent study from Spain that examined long-term compliance with bisphosphonate treatment reported the most promising results. Ojeda-Bruno et al. utilized an educational system, telephone follow-up, and scheduled follow-up visits to determine the effect of their intervention on long-term compliance with bisphosphonate treatment. In this study, patients who sustained a fragility fracture, based on inclusion criteria similar to that of our study, were scheduled for an office visit for osteoporosis assessment. Of all patients eligible for the study, a randomly selected intervention group also received a two-hour education session given by a nurse or physician regarding bone health. Two additional clinical visits were scheduled over a one-year period for all study participants. While the authors found that only 20% of the group randomized to the intervention attended the educational session, they concluded that it was the baseline office visit for patients determined to be at risk for osteoporosis that was responsible for increasing the frequency of bisphosphonate use from 17% before consultation to 76% after the initial visit [9]. These study results support the premise of our study that just ensuring proper outpatient office follow-up appointments will result in improved post-fragility-fracture care and are consistent with the 2011 Healthcare Effectiveness Data and Information Set (HEDIS) Guidelines for osteoporosis management that recommend postmenopausal women (67 years of age and older) who have had a low-impact fracture be referred for a DXA or prescription for a drug to treat osteoporosis within six months of the their fracture [10].
In another inpatient study conducted on all patients hospitalized with a fragility fracture, Collinge et al. utilized calcaneal quantitative ultrasound (QUS) to stratify patients by low, moderate, and high risk for osteoporosis [11]. For patients identified as high risk, intervention was initiated with patient education and calcium and vitamin D therapy. Education consisted of a 15–20-minute meeting with a nurse clinician about osteoporosis and a one-page summary of references to obtain more information. Upon discharge, a prescription for calcium and vitamin D, a summary of their QUS test results, and instructions to follow up with their primary care physician were provided. At 12 months after discharge, 57% of high-risk patients had seen their primary care physician for a bone health discussion. The authors concluded that although patient education is key, the efficacy of any intervention program ultimately depends on patient compliance and attributed lack of follow-up to limited access to a primary care provider, lack of money for follow-up, and belief that follow-up was not important.
In the American Orthopaedic Association “Own the Bone” Initiative, which was the basis for our pilot and present study, a quality-based improvement registry was utilized to initiate and improve patient education strategies involving osteoporosis education, prevention, diagnosis, and treatment [4]. Though the study was unable to demonstrate an increase use in DXA screening or use of pharmacotherapy, it did find that establishment of an ancillary team to support osteoporosis care was key. It suggested that orthopaedic surgeons are not used to obtaining and often do not have the time to obtain a detailed patient history that includes data on osteoporosis risk factors, current medication, and comorbid conditions.
In a follow-up study to “Own the Bone,” Edwards and colleagues conducted a prospective cohort study at two different hospitals to assess the effect of immediate treatment for osteoporosis, which included initiation of pharmacologic therapy during hospitalization, as compared to delayed care [8]. In the delayed care group, the orthopaedic surgery team recommended osteoporosis counseling, DXA, and potential treatment for their osteoporosis that was communicated to the patient's primary care physician after hospital discharge. Although the rate of osteoporosis treatment of patients with a fragility fracture increased when an orthopaedic surgeon intervened in either group, the highest success rate for treatment was experienced with immediate initiation of osteoporosis care during hospitalization for the fragility fracture, resulting in sixty-seven percent of the patients receiving therapy six months after fracture, compared to delayed initiation of treatment which was only thirty percent when referred back to the primary care physician [8]. Similar to the Gardner et al. study [5], the value of having an inpatient orthopaedic surgery team that is educated in osteoporosis management initiate treatment while hospitalized for the fragility fracture is highlighted. Further educational efforts should be explored within the American Academy of Orthopaedic Surgery, the American Orthopaedic Association, and other orthopaedic surgery organizations to educate orthopaedic surgeons in the area of osteoporosis management, especially in the post-fragility-fracture patient.
Within the Department of Orthopaedic Surgery at our institution, following our active intervention program, we appreciated increased rates of osteoporosis screening and treatment among patients who sustained a fragility fracture that could be sustainable with a rather minimal increased use of existing resources. While there exist reported successful interventions in clinical settings by orthopaedic surgeons, the associated costs of personnel and materials and other barriers presented in the literature led us to create a simple protocol utilizing few resources, time, and costs. First, we obtained basic patient medical information from the screening of fragility fracture ICD-9 codes from our institution's billing department on a monthly basis at no extra cost. Then, unpaid research staff (medical students) administered a telephone-screening questionnaire to determine whether patients had appropriate osteoporosis follow-up care. Those patients without osteoporosis follow-up were then referred to a scheduling coordinator who was compensated $8,000 over the course of the year to authorize, refer, or schedule patients for osteoporosis treatment. Based upon the numbers of patients ultimately scheduled, the actual costs of our intervention were $275.86 per patient. The majority of the cost-effectiveness data on osteoporosis interventions are presented in costs per quality-adjusted life years (QALYs) [12]. Our study was not designed to assess cost-effectiveness. However, if our intervention were to be continually implemented at our institution or other practice settings, the costs would be higher because of the initial time and costs involved in contacting the patients to assess osteoporosis awareness and follow-up care. However, based on facts that osteoporosis causes 1.5 million fractures in the USA annually, with an estimated cost of treating at $17 billion, and a reported mortality rate of 24% in the first year following a hip fracture [13], our intention in conducting such a study was to gain departmental and institutional awareness so that some financial resources might be directed towards developing an effective fracture intervention program.
Our study had some limitations. First, there was a high rate of data drop-off between the researchers and scheduling coordinator. Despite the 70 patients that met criteria for referral to the scheduling coordinator, only 48 patients were referred. The reasons for this are likely twofold: (1) there were three different student researchers who collected their own data in password-protected files that were not collated until the end of the study period so that missing referrals were not detected until beyond the study's timeline; (2) the scheduling coordinator was not given the original patient eligibility list and had no way of tracking whether or not patients might or might not have been appropriately referred. To minimize this data drop-off, a single follow-up coordinator responsible for data management should be appointed to ensure that appropriate patient follow-up is achieved. A second limitation is that our study population was likely not representative of most fragility fracture patient populations. First, our participation rate was very high at 88%. Second, the self-reported osteoporosis follow-up care was about 30% higher than the national average, indicating that our patient population might have been more willing to comply with follow-up recommendations than the general population or may have better access to a primary care physician [14].
Orthopaedic surgeons have a unique opportunity to improve osteoporosis care for their patients with a fragility fracture through assessment, education, simple treatment measures, and, most importantly, a referral for long-term osteoporosis management. Our telephone-based intervention demonstrated that a simple protocol, not based upon a specific orthopaedic surgeon's referral, was relatively inexpensive and leads to increased osteoporosis evaluation and treatment in patients with fragility fractures.
With further centralized coordination and continued implementation of our protocol, we will plan to further evaluate the success and sustainability of this program at our institution with the hopes that our practical experience may be generalized to other orthopaedic surgery departments.
Conflict of Interests
The authors report no actual or potential conflict of interests in relation to this paper.
References
- 1.Center JR, Bliuc D, Nguyen TV, Eisman JA. Risk of subsequent fracture after low-trauma fracture in men and women. Journal of the American Medical Association. 2007;297(4):387–394. doi: 10.1001/jama.297.4.387. [DOI] [PubMed] [Google Scholar]
- 2.Klotzbuecher CM, Ross PD, Landsman PB, Abbott TA, Berger M. Patients with prior fractures have an increased risk of future fractures: a summary of the literature and statistical synthesis. Journal of Bone and Mineral Research. 2000;15(4):721–739. doi: 10.1359/jbmr.2000.15.4.721. [DOI] [PubMed] [Google Scholar]
- 3.Majumdar SR, Rowe BH, Folk D, et al. A controlled trial to increase detection and treatment of osteoporosis in older patients with a wrist fracture. Annals of Internal Medicine. 2004;141(5):366–273. doi: 10.7326/0003-4819-141-5-200409070-00011. [DOI] [PubMed] [Google Scholar]
- 4.Tosi LL, Gliklich R, Kannan K, Koval KJ. The american orthopaedic association’s “own the bone“ initiative to prevent secondary fractures. Journal of Bone and Joint Surgery Series A. 2008;90(1):163–173. doi: 10.2106/JBJS.G.00682. [DOI] [PubMed] [Google Scholar]
- 5.Gardner MJ, Brophy RH, Demetrakopoulos D, et al. Interventions to improve osteoporosis treatment following hip fracture: a prospective, randomized trial. Journal of Bone and Joint Surgery Series A. 2005;87(1):3–7. doi: 10.2106/JBJS.D.02289. [DOI] [PubMed] [Google Scholar]
- 6.Johnson SL, Petkov VI, Williams MI, Via PS, Adler RA. Improving osteoporosis management in patients with fractures. Osteoporosis International. 2005;16(9):1079–1085. doi: 10.1007/s00198-004-1814-z. [DOI] [PubMed] [Google Scholar]
- 7.Schulman JE, Williams S, Khera O, Sahba T, Michelson J, Fine K. Effective osteoporosis education in the outpatient orthopaedic setting. Journal of Bone and Joint Surgery Series A. 2007;89(2):301–306. doi: 10.2106/JBJS.F.00491. [DOI] [PubMed] [Google Scholar]
- 8.Edwards BJ, Koval K, Bunta AD, et al. Addressing secondary prevention of osteoporosis in fracture care: follow-up to “own the bone”. Journal of Bone and Joint Surgery Series A. 2011;93(15):e87.1–e87.7. doi: 10.2106/JBJS.I.00540. [DOI] [PubMed] [Google Scholar]
- 9.Ojeda-Bruno S, Naranjo A, Francisco-Hernández F, et al. Secondary prevention program for osteoporotic fractures and long-term adherence to bisphosphonates. Osteoporosis International. 2011;22(6):1821–1828. doi: 10.1007/s00198-010-1414-z. [DOI] [PubMed] [Google Scholar]
- 10.HEDIS 2011. HEDIS Technical Specifications. Vol. 2. Washington, DC, USA: National Committee for Quality Assurance; 2005. [Google Scholar]
- 11.Collinge C, Lebus G, Gardner MJ, Gehrig L. Osteoporosis in orthopaedic trauma patients: a diagnosis and treatment protocol. Journal of Orthopaedic Trauma. 2008;22(8):541–547. doi: 10.1097/BOT.0b013e31817d9c99. [DOI] [PubMed] [Google Scholar]
- 12.Zethraeus N, Borgström F, Ström O, Kanis JA, Jönsson B. Cost-effectiveness of the treatment and prevention of osteoporosis—a review of the literature and a reference model. Osteoporosis International. 2007;18(1):9–23. doi: 10.1007/s00198-006-0257-0. [DOI] [PubMed] [Google Scholar]
- 13.Lim LS, et al. Screening for osteoporosis in the adult U.S. population. American Journal of Preventive Medicine. 2010;36(4):366–375. doi: 10.1016/j.amepre.2009.01.013. [DOI] [PubMed] [Google Scholar]
- 14.California Cooperative Healthcare Reporting Initiative. 2008 Report on Quality. San Francisco, C.C.C.H.R.I., 2008, 2009, pp. 1–104.


