Abstract
OBJECTIVES:
Though elderly persons with chronic atrial fibrillation have more comorbidities that could limit indications for the chronic use of anticoagulants, few studies have focused on the risk of falls within this particular group. To evaluate the predictors of the risk of falls among elderly with chronic atrial fibrillation, a cross-sectional, observational study was performed.
METHODS:
From 295 consecutive patients aged 60 years or older with a history of atrial fibrillation who were enrolled within the last 2 years in the cardiogeriatrics outpatient clinic of the Instituto do Coração do Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo, 107 took part in this study. Their age was 77.9±6.4 years, and 62 were female. They were divided into two groups: a) no history of falls in the previous year and b) a history of one or more falls in the previous year. Data regarding the history of falls and social, demographic, anthropometric, and clinical information were collected. Multidimensional assessment instruments and questionnaires were applied.
RESULTS:
At least one fall was reported in 55 patients (51.4%). Among them, 27 (49.1%) presented recurrent falls, with body lesions in 90.4% and fractures in 9.1% of the cases. Multivariate logistic regression showed that self-reported difficulty maintaining balance, use of amiodarone, and diabetes were independent variables associated with the risk of falls, with a sensitivity of 92.9% and a specificity of 44.9%.
CONCLUSION:
In a group of elderly patients with chronic atrial fibrillation who were relatively independent and able to attend an outpatient clinic, the occurrence of falls with recurrence and clinical consequences was high. Difficulty maintaining balance, the use of amiodarone and a diagnosis of diabetes mellitus were independent predictors of the risk for falls. Thus, simple clinical data predicted falls better than objective functional tests.
Keywords: Falls, Elderly Atrial Fibrillation, Questionnaires, Risk Assessment
INTRODUCTION
Atrial fibrillation (AF) and falls are common among the elderly, which has increasing relevance as the life expectancy of the population rises.
Not only do structural and functional alterations of the cardiovascular system upon aging predispose patients to AF, but they also reduce the capacity of hemodynamic tolerance to arrhythmia, which may lead to syncope and fall (1,2). The proportion of patients with relevant and highly fall-related functional disabilities following ischemic stroke related to AF may reach 59% (3).
Anticoagulation therapy is characterized by the strategy of preventing thromboembolic events in elderly persons with AF (4), but there is no consensus about the risk of its use among patients with a history of falls, particularly in recurrent cases of falls.
In patients with AF who are at a high risk for falls, Gage et al. (5) showed that warfarin is related to mortality associated with intracranial hemorrhage, but not to the occurrence of intracranial hemorrhage. Despite that, the use of anticoagulants was still beneficial owing to the high risk of embolic stroke in this group.
A meta-analysis of antithrombotic therapy in elderly patients at risk for falls concluded that the propensity for falling in elderly patients should not be an important factor when deciding whether a patient is a good candidate for the anticoagulation treatment for AF (6). However, in the randomized controlled trials evaluated in the meta-analysis, patients may have been monitored more intensely than is usual in clinical practice.
Recently, in a study that included 4,093 patients older than 80 years who were carefully monitored by an anticoagulation clinic, the rate of bleeding was low, suggesting that age itself should not be considered a contraindication to treatment. However, a history of two or more falls in a year was independently associated with bleeding risk, as assessed by Cox regression analysis (7).
Guidelines for the prevention of falls in the elderly recommend a series of instruments that should be applied in individuals at risk of falling (8,9). However, a thorough history, including questions about previous falls, medications, and balance, could be used for fall risk assessment (10).
Thus, the issue of anticoagulation treatment of patients with atrial fibrillation to prevent embolic stroke vis-à-vis the risk of falls has not been fully established in real-life elderly patients. To evaluate predictors of falls among elderly patients with chronic atrial fibrillation and indications for anticoagulant therapy, a cross-sectional, observational study was designed.
METHODS
A cross-sectional, observational study design was used. The project was approved by the Scientific and Ethics Committees of InCor-HCFMUSP (Scientific: PROTOCOL SDC 2775/06/020, approved on 20/04/2006, and Ethics: PROTOCOL No. 450/06, approved on 25/05/2006), and all participants agreed to participate and signed an Informed Consent Form.
Male and female patients aged 60 years or older with a diagnosis of AF from the cardiogeriatrics outpatient clinic of the Instituto do Coracao of the Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo (InCor-HCFMUSP) were recruited from their regular ambulatory visit or summoned through telephone calls from the outpatient clinic database registry of patients with AF from September 2006 to May 2007, in order of arrival.
The selected patients were divided into two groups: a) those with no history of falls in the previous year and b) those with a history of one or more falls in the previous year.
Data regarding the history of falls and social, demographic, anthropometric, and clinical information were collected. Furthermore, multidimensional assessment instruments and questionnaires were applied. The history of falls included the occurrence, number, local, characteristics and consequences of falls (according to the definition of Tinetti et al. (11) within the previous 12 months. Social and demographic data included gender, age, marital status, education level, people living in the same dwelling, remuneration and professional activity. Anthropometric data included weight, height, and body mass index (12).
Patients were further classified by whether they were symptomatic, their eating habits, physical exercise habits, smoking status, abuse of alcohol, medications used, and the presence of cardiovascular diagnoses and comorbidities. The physical examination, performed by the same physician, included simplified and systematized assessments of cranial pairs, ocular movements, pyramidal signals, muscle tonus and strength, reflexes and motor coordination, sensitivity and proprioception, and the Romberg balance test.
The following questionnaires and instruments validated in Portuguese were used: Brazilian Functional Assessment Questionnaire (BOMFAQ; Brazilian version of the OARS) (13,14), Mini Mental State Examination (MMSE) (15,16), Primary Care Evaluation for Mental Disorders (Prime MD) (17,18,19), and Health Assessment Questionnaire (HAQ)(20).
Sensorial assessment was performed by inquiring about hearing conditions with the following question (21,22): “Do you feel that you have experienced hearing loss?” Visual assessment included campimetry and the Snellen scale test (Herman Snellen, 1862) (23).
Balance and gait were assessed by applying the Berg Functional Balance Scale (24,25), Performance-Oriented Mobility Assessment (POMA) (26,27), Balance POMA and Gait POMA, and Timed Up & Go (TUG) (28).
Statistical analysis
Classification variables were descriptively presented in contingency tables comprising absolute (n) and relative (%) frequencies. The associations among variables were assessed with the chi-square test, likelihood test, or Fisher's exact test. Quantitative variables were presented descriptively in tables, including mean and standard deviation or median, minimum and maximum values. Means were compared using the Student's t-test or the Wilcoxon rank-sum test. Values of p<0.05 were considered statistically significant (29). Significant variables in the univariate analysis were used in the regression model adjustment to determine the sensitivity, specificity, estimated probability of falls and odds ratios. The logistic regression model was used to examine the relationships between independent variables for the risk of falling. All significant variables (p≤0.05) and the interactions between them were used to obtain a selection for the multivariate model. We opted not to correct the critical value of p in the function of multiple comparisons because the non-significant variables were not included and were deemed irrelevant to those that remained in the model, which meant that the variables in the model did not require correction. All significant variables in the univariate analysis were adjusted in the logistic regression model and related according to the “stepwise” procedure. The variables that remained in the model were independent predictor variables.
RESULTS
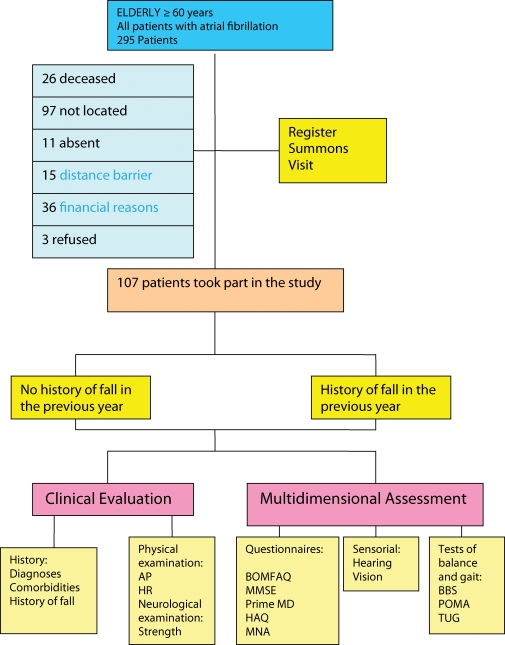
From the approximately 3,000 patients/year enrolled in the cardiogeriatrics outpatient clinic of the InCor-HCFMUSP, all 295 patients aged 60 years or older with a history of atrial fibrillation who were registered in the 24 months prior to the period of clinical evaluation, which was September 2006 to May 2007, were eligible to participate in the study. Between the date of registration and the date of evaluation, 26 patients died, 97 were not available through the telephone numbers given to the institution, 11 patients did not show up on the day of evaluation, 15 could not participate due to living outside of São Paulo, 36 were excluded because they lacked the clinical conditions required, and three refused to participate. Patients who were not contacted by telephone after three attempts on different days and times were excluded.
Ultimately, 107 patients took part in the full study (Figure 1).
Figure 1.
Study design.
They had an advanced age (77.9±6.4 years) and a predominance of shared dwellings (81.3%) and female gender (57.9%). Most patients reported cardiovascular symptoms (82.2%), were sedentary (80.4%), and used four or more medications (87%). The most frequent diagnoses were arterial hypertension (91%), osteoarthritis (47.7%), dyslipidemia (46.7%), New York Heart Association class I/II heart failure (41%), obesity (30.8%), diabetes mellitus (18.7%), and heart failure class III (12.2%). The presence of four or more comorbidities was frequent (44.9%). Patients were divided and compared according to the history of falls in the previous year (Table 1).
Table 1.
Characteristics and results of the elderly population with AF.
| Variable | FALL | TOTAL | p-value | ||||
| NO | YES | ||||||
| Female | 28 | 45.16% | 34 | 54.84% | 62 | 0.283 | *) |
| Age (years) | 77. 07 + 6. 58 | 78. 46 + 6. 29 | 77. 86 + 6. 42 | 0.276 | # | ||
| BMI (kg/m2) | 28 (19 - 55) | 26 (19 - 38) | 27 (19 - 55) | 0.444 | ## | ||
| Visual deficiency | 32 | 42.11% | 44 | 57.89% | 76 | 0.005 | *) |
| Hearing deficiency | 19 | 45.24% | 23 | 54.76% | 42 | 0.029 | ** |
| Physical activity | 10 | 45.45% | 12 | 54.55% | 22 | 0.705 | *) |
| Symptoms | 39 | 43.33% | 48 | 53.33% | 90 | 0.015 | *) |
| Palpitations | 25 | 41.67% | 35 | 58.33% | 60 | 0.044 | *) |
| Tiredness | 28 | 37.33% | 47 | 62.67% | 75 | 0.001 | *) |
| Paresthesias | 16 | 38.10% | 26 | 61.90% | 42 | 0.037 | *) |
| Cephalea | 4 | 26.67% | 11 | 73.33% | 15 | 0.041 | *) |
| Syncopes | 0 | 0.00% | 5 | 100.00% | 5 | 0.027 | *** |
| Muscle strength | |||||||
| Hand grip | 19 | 45.24% | 30 | 71.43% | 42 | 0.021 | *** |
| Quadríceps | 17 | 40.48% | 25 | 59.52% | 42 | 0.001 | ** |
| CHF FC I/II | 22 | 50.00% | 22 | 50.00% | 44 | 0.934 | *) |
| Dilated myocardiopathy | 26 | 39.39% | 40 | 60.61% | 66 | 0.085 | *) |
| Mitral failure | 11 | 55.00% | 9 | 45.00% | 20 | 0.586 | *) |
| Coronary failure | 5 | 29.41% | 12 | 70.59% | 17 | 0.077 | *) |
| CHF FC III | 2 | 15.38% | 11 | 84.62% | 13 | 0.009 | *) |
| Tricuspid failure | 7 | 53.85% | 6 | 46.15% | 13 | 0.739 | *) |
| Aortic failure | 6 | 85.71% | 1 | 14.29% | 7 | 0.112 | *** |
| Previous AMI | 1 | 16.67% | 5 | 83.33% | 6 | 0.205 | *** |
| COMORBIDITIES | |||||||
| Obesity | 17 | 51.52% | 16 | 48.48% | 33 | 0.731 | *) |
| Diabetes mellitus | 5 | 25.00% | 15 | 75.00% | 20 | 0.015 | *) |
| Neuropathies | 6 | 30.00% | 14 | 70.00% | 20 | 0.052 | *) |
| COPD | 6 | 33.33% | 12 | 66.67% | 18 | 0.131 | *) |
| Depression | 8 | 47.06% | 9 | 52.94% | 17 | 0.824 | *) |
| Thyropathies | 8 | 47.05% | 9 | 52.94% | 17 | 0.487 | ** |
| Peripheral vascular disease | 9 | 60.00% | 6 | 40.00% | 15 | 0.381 | *) |
| Rheumatological diseases | 3 | 33.33% | 6 | 66.67% | 9 | 0.488 | *** |
| Chronic renal failure | 3 | 37.50% | 5 | 62.50% | 8 | 0.716 | *** |
| Gastric disorders | 1 | 14.29% | 6 | 85.71% | 7 | 0.113 | *** |
| Prostatism | 5 | 71.43% | 2 | 28.57% | 7 | 0.265 | *** |
| Pulmonary hypertension | 2 | 28.57% | 5 | 71.43% | 7 | 0.437 | *** |
| Neoplasia | 2 | 33.33% | 4 | 66.67% | 6 | 0.678 | *** |
| Epilepsy | 2 | 66.67% | 1 | 33.33% | 3 | 0.598 | *** |
| Scores | |||||||
| HAQ | 0.72 0-2.25) | 1.20 (0-2.88) | 0.97 (0-2.88) | 0,002*) | ## | ||
| MMSE | 25 (9-30) | 23.98(7-30) | 24.47(7-30) | 0,1761 | ## | ||
| Timed Up & Go | 11 (6 - 30) | 13 (8 - 56) | 12 (6 - 56) | 0.063 | ## | ||
| Gait POMA | 11 (5 - 13) | 11 (2- 12) | 11 (2 - 13) | 0.148 | ## | ||
| Balance POMA | 16 (8 - 16) | 15 (1 - 16) | 16 (1 - 16) | 0.018 | ## | ||
| Berg Balance Scale | 51 (20 - 56) | 51 (15 - 56) | 51 (15 - 56) | 0.224 | ## | ||
Chi-square test **Likelihood ratio test *** Fisher's exact test.
# Student's t-test ## Wilcoxon's rank sum test.
Occurrence of falls: One fall was reported in 55 patients (51.4%). Of these, 49.1% presented recurrent falls, 32.7% fell at home, and 28.9% fell on the street. The most frequent reasons for falling were trips (35.3%) and slips (23.5%).
Dizziness and vertigo caused falls only in 6% of the reports. The falls had consequences of body lesions in 90.4% and fractures in 9.1% (five cases). Sixty percent of the fractures were in the pelvis, and these led to hospitalization in 7.7% (four cases) of the falling episodes.
Demographic data: There was no significant difference regarding the occurrence of falls between the genders (54.8% in female patients and 46.7% in male patients).
Only 19% of the patients lived alone, and 6% were single or had never lived with partners. However, there was no significant relationship between the occurrence of falls and marital status, scholarship or income level, nor was there any association between the occurrence of falls and age or BMI.
Clinical data: There was a significant correlation between the occurrence of falls and the presence of clinical symptoms (p = 0.015), mainly palpitations (p = 0.044), and tiredness (p = 0.001). There was no significant relationship between falling and a sedentary lifestyle, smoking, or alcohol consumption.
Regarding the use of medications, 86.9% of the patients used four or more medications, and only 2.8% (three patients) did not use any medication. There was no significant correlation between the occurrence of falls and the number of medications used.
There was a significant correlation between the occurrence of falls and the use of anticonvulsants and benzodiazepines (p = 0.0410) and amiodarone (p = 0.0046), despite the infrequent use of these drugs.
Among the diagnoses, there were significant relationships between falling and congestive heart failure class III (p = 0.009) and systolic hypertension (p = 0.034).
Among the comorbidities, type 2 diabetes mellitus was the only condition with a significant correlation with the occurrence of falls (p = 0.015). Decreased muscle strength in the upper or lower limbs was also associated with the occurrence of falls.
Questionnaires and instruments:
There was a significant association between the occurrence of falls and the domain of daily life activities of the BOMFAQ (OARS), which revealed correlations between falling and difficulty eating (p = 0.004), bathing without assistance (p = 0.026), getting to the bathroom in time (p = 0.009), preparing meals (p = 0.035), and trimming toenails (p = 0.049). Furthermore, low life satisfaction (p = 0.007), perception of poor health quality (p = 0.0001), a sense of uselessness (p = 0.005), hearing difficulties in noisy environments (p = 0.023), deglutition (p = 0.043), and balance difficulties (p = 0.0001) were also significantly associated with falls.
The relationships between the occurrence of falls and the Mini-mental questionnaire scores were not significant. However, the occurrence of falls was significantly associated with major depression due to physical illness, dysthymia and panic disorder according to the Prime MD, as well as with the HAQ scores.
There was a significant association between hearing or vision deficiencies and the occurrence of falls. From the balance and gait tests, only the score of the Balance POMA test revealed an association with the occurrence of falls.
Logistic regression
The logistic regression model was used to examine the relationships between independent variables on the risk of falling. All significant variables (p≤0.05) and the interactions between them were used in the multivariate model. The following independent variables were identified by logistic regression analysis: use of antiarrhythmics (amiodarone), difficulty maintaining balance as assessed by the BOMFAQ questionnaire, and the presence of diabetes mellitus. The sensitivity was 92.9%, and the specificity 44.9%.
A patient with these three independent variables had a 97% chance of falling within the next year (Table 2). Simulating possible results revealed that 1) patients taking amiodarone who had diabetes mellitus had an 86% chance of falling within the next year; 2) those on amiodarone and presenting balance difficulty, 89%; and 3) those with diabetes and balance alterations, 85%. Patients not presenting any of these variables had a 16.4% chance of falling within a year (Table 3). The odds ratios for falls in one year adjusted for all significant variables in the logistic regression model indicated that the use of amiodarone increased the risk of falls in one year seven times (odds ratio = 6.952); diabetes mellitus increased the risk five times (odds ratio = 4.909); and self-reported difficulty maintaining balance increased the risk six times (odds ratio = 5.862).
Table 2.
Logistic regression of the independent variables of the risk of falls.
| Variable | Estimated parameter | Standard error | p-value | Odds ratio | Confidence interval (95%) | |
| Antiarrhythmic drug (YES/NO) | 1.939 | 0.906 | 0.032 | 6.952 | 1.177 | 41.053 |
| Comorbid diabetes mellitus (YES/NO) | 1.591 | 0.629 | 0.011 | 4.909 | 1.432 | 16.832 |
| BOMFAQ: Difficulty maintaining balance walking? (YES/NO) | 1.768 | 0.507 | <0.001 | 5.862 | 2.171 | 15.828 |
| Constant | -1.630 | 0.457 | <0.001 | 0.196 | ||
Table 3.
Probability of the risk of a fall according to the simulation of combinations of independent variables.
| SimulationVariable combination group | Antiarrhythmia | Diabetes mellitus | Balance | Estimated probability of fall | Odds ratio |
| 1 | 1 | 1 | 1 | 0.975126662 | 5.95 |
| 2 | 1 | 0 | 0 | 0.576711639 | 3.52 |
| 3 | 0 | 1 | 0 | 0.490315301 | 2.99 |
| 4 | 0 | 0 | 1 | 0.534614124 | 3.26 |
| 5 | 1 | 1 | 0 | 0.869927606 | 5.31 |
| 6 | 1 | 0 | 1 | 0.888720802 | 5.42 |
| 7 | 0 | 1 | 1 | 0.84937512 | 5.18 |
| 8 | 0 | 0 | 0 | 0.163861359 | 3.52 |
Similarly, the positive likelihood ratios showed that the increased the risk of falling within the next year five times (positive likelihood ratio = 5). Positive likelihood ratio = sensitivity/1-specificity = 45/7 = 5; negative likelihood ratio = 1-sensitivity/specificity = 55/93 = 0.6.
DISCUSSION
The present study shows that use of amiodarone, the presence of diabetes mellitus and self-reported difficulty maintaining balance (as assessed by the BOMFAQ questionnaire) increase the likelihood of falls in elderly patients with AF. Therefore, simple clinical data predict the risk of falls better than validated functional tests (30,31,32).
Furthermore, the high number of recurrences confirms the higher risk for patients with previous falls (33,34).
In the literature, there is no clear definition of which patients are at risk of falls.
The study population was relatively small, and therefore inadequate to establish direct measures of risk prediction, but it did allow us to evaluate the relationships between many variables and the occurrence of falls.
In contrast with other studies, age, gender (35,36), use of anti-hypertensive drugs (37), and cognitive impairment were not associated with the occurrence of falls.
However, most of the variables considered as risk factors were associated with the occurrence of falls, and it is known that the risk of falls rises consistently with the number of associated risk factors present (38).
Multivariate logistic regression showed that the use of amiodarone, a diagnosis of diabetes and self-reported difficulty maintaining balance (BOMFAQ) were independent variables associated with the risk of falling. The estimated probability of the risk of falling within a year among patients with AF who did not present these three independent variables was 16.3%, but it was almost six times higher (97%) in the presence of all three variables.
Amiodarone is a highly effective drug, yet its use is limited in chronic AF (39). A prescription of amiodarone is a marker of disease severity associated with chronic AF, which could lead to a higher risk of falls by postural hypotension, embolic events and/or other heart rhythm disturbances. On the other hand, the increased risk of falls could be directly related to side effects of the drug, such as retinal pigmentation, pulmonary fibrosis, thyroid dysfunctions, optical and peripheral neuropathy, fatigue, tremors, ataxia, sleep disorders, vertigo, and headaches.
In early reports, the frequencies of neurologic toxic effects from amiodarone ranged from 27.5% to as high as 74% and could have been related to a much higher daily dose (40,41,42). The frequency of adverse neurologic effects in longer-term amiodarone clinical trials has been much lower, at less than 5% (43,44,45,46), as in the present study.
Diabetes could be associated with the risk of falls by several mechanisms, such as micro- and macroangiopathy (causing visual disturbances) and neuropathy (leading to postural hypotension and compromising proprioception and muscle strength).
Gerdhem et al. (10) concluded that for fall prediction in elderly women, the more time-consuming objective functional tests may be of limited importance compared to data obtained from the clinical history. Similarly, the present study emphasizes the value of clinical data in assessing the risk of falls in elderly patients with AF. Risk factors for falls are numerous and vary among patients and populations. The results of the current study have important clinical implications, as they could simplify the evaluation and improve the management of elderly patients with AF at risk of falling.
The generalization of the present findings to other populations without or with chronic AF should be performed with caution. This study was cross-sectional, and it did not compare the AF group with a non-AF group to determine whether AF itself increases the occurrence of falls.
Furthermore, the studied population may represent a select group with high functional status because a high number of patients were not able to participate in the study. Further prospective studies including a high number of AF and non-AF elderly patients, comparing the predictive value for falls of functional tests versus clinical data, are needed to confirm the present findings.
In a group of elderly patients with chronic AF who were relatively independent and able to attend an outpatient clinic, the occurrence of falls with recurrence and consequences was high. Self-reported difficulties maintaining balance, the use of amiodarone and a diagnosis of diabetes mellitus were identified as independent predictors of the risk for falls. Thus, simple clinical data predicted falls better than objective functional tests.
Footnotes
No potential conflict of interest was reported.
REFERENCES
- 1.Maurer MS, Bloomfield DM. Atrial fibrillation and falls in the elderly. Clin Geriatr Med. 2002;18(2):323–37. doi: 10.1016/s0749-0690(02)00013-7. [DOI] [PubMed] [Google Scholar]
- 2.Ott A, Breteler M, Bruyne M, Van Harskamp F, Grobbee DE, Hofman A. Atrial fibrillation and dementia in a population based study: The Rotterdam Study. Stroke. 1997;28(2):316–21. doi: 10.1161/01.str.28.2.316. [DOI] [PubMed] [Google Scholar]
- 3.Hylek EM, Go AS, Chang Y, Jensvold NG, Henault LE, Selby JV, et al. Effect of intensity of oral anticoagulantion on stroke severity and mortality in atrial fibrilation. N Engl J Med. 2003;349(11):1019–26. doi: 10.1056/NEJMoa022913. [DOI] [PubMed] [Google Scholar]
- 4.European Heart Rhythm Association, Heart Rhythm Society Fuster V, Rydén LE, Cannom DS, Crijns HJ, et al. ACC/AHA/ESC 2006 guidelines for the management of patients with atrial fibrillation--executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the European Society of Cardiology Committee for Practice Guidelines (Writing Committee to Revise the 2001 Guidelines for the Management of Patients With Atrial Fibrillation) J Am Coll Cardiol. 2006. Aug [cited 2011 Aug 31] 15;48(4):854-906 Erratum in: J Am Coll Cardiol. 2007;50(6)562 [DOI] [PubMed] [Google Scholar]
- 5.Gage BF, Birman-Deych E, Kerzner R, Radford MJ, Nilasena DS, Rich MW. Incidence of intracranial hemorrhage in patients with atrial fibrillation who are prone to fall. Am J Med. 2005;118(6):612–7. doi: 10.1016/j.amjmed.2005.02.022. [DOI] [PubMed] [Google Scholar]
- 6.Man-Son-Hing M, Nichol G, Lau A, Laupacis A. Choosing antithrombotic therapy for elderly patients with atrial fibrillation who are at risk for falls. Arch Intern Med. 1999;159(7):677–85. doi: 10.1001/archinte.159.7.677. [DOI] [PubMed] [Google Scholar]
- 7.Poli D, Antonucci E, Testa S, Tosetto A, Ageno W, Palareti G, et al. Bleeding Risk in Very Old Patients on Vitamin K Antagonist Treatment: Results of a Prospective Collaborative Study on Elderly Patients Followed by Italian Centres for Anticoagulation. Circulation. 2011;124(7):824–9. doi: 10.1161/CIRCULATIONAHA.110.007864. [DOI] [PubMed] [Google Scholar]
- 8.The National Institute for Clinical Excellence (NICE) Clinical practice guideline for the assessment and prevention of falls in older people [cited Aug 31] London: Royal College of Nursing (UK); Nov 2004. Available from http://www.ncbi.nlm.nih.gov/books/NBK55851/pdf/TOC.pdf. [PubMed]
- 9.ProFaNE, School of Nursing, Midwifery and Social, Coupland III, University of Manchester Oxford Road, Manchester M139PL [cited Aug 31] Great Britain. Available from: www.profane.eu.org.
- 10.Gerdhem P, Ringsberg KA, Akesson K, Obrant KJ. Clinical history and biology age predicted falls better than objective functional tests. J Clin Epidemiol. 2005;58(3):226–32. doi: 10.1016/j.jclinepi.2004.06.013. [DOI] [PubMed] [Google Scholar]
- 11.Tinetti ME. Preventing Falls in Elderly Persons. N England J Med. 2003;348(1):42–4. doi: 10.1056/NEJMcp020719. [DOI] [PubMed] [Google Scholar]
- 12.World Health Organization (WHO) Obesity Preventing and Management Global Epidemic Report of WHO Consultation on Obesity Geneva: Who; 1997 [Google Scholar]
- 13.Blay S, Ramos LR, Mari J. Validity of a Brazilian version of the older Americans resources and services (OARS) mental health screening questionnaire. J Am Geriatr Soc. 1988;36(8):687–92. doi: 10.1111/j.1532-5415.1988.tb07169.x. [DOI] [PubMed] [Google Scholar]
- 14.Perracini MR, Ramos LR. Fatores associados a quedas em uma coorte de idosos residentes na comunidade. Brazilian Multidimensional Functional Assessment Questionnarire (BOMFAQ) – versão brasileira do Multidimensional Functional Assessment Questionnaire. Rev Saúde Pública. 2002;36(6):709–16. doi: 10.1590/s0034-89102002000700008. [DOI] [PubMed] [Google Scholar]
- 15.Crum RM, Anthony JC, Basset SS, Folstein MF. Population-based norms for Mini-Mental State Examination by age and educational level. JAMA. 1993;269(18):2420–1. [PubMed] [Google Scholar]
- 16.Brucki S, Nitrini R, Caramelli P, Bertolucci PHF, Okamoto IH. Sugestões para o uso do Mini-Mental do estado mental no Brasil. Arq Neuropsiquiatr. 2003;61(3-B):777–81. doi: 10.1590/s0004-282x2003000500014. [DOI] [PubMed] [Google Scholar]
- 17.Spitzer RL, Williams JB, Kroenke K, Linzer M, de Gruy FV, III, Hahn SR, et al. Utility of a new procedure for diagnosing mental disorders in primary care. The PRIME-MD 1000 study. JAMA. 1994;272(14):1749–5. [PubMed] [Google Scholar]
- 18.Fraguas R, Jr, Henriques SG, Jr, De Lucia MS, Iosifescu DV, Schwartz FH, Menezes PR, et al. The detection of depression in medical setting: a study with PRIME-MD. J Affect Disord. 2006;91(1):11–7. doi: 10.1016/j.jad.2005.12.003. [DOI] [PubMed] [Google Scholar]
- 19.Ferreira MHF, Dalgalarrondo P.Prevalência de Transtornos Depressivos em hospital geral e validação do guia clínico Prime MD: XII Congresso Interno de Iniciação Científica da UNICAMP, 2004. [citado 2011 Set 01]. Disponível emhttp://www.prp.unicamp.br/pibic/congressos/xiicongresso/cdrom/pdfN/598.pdf
- 20.Fries JF, Spitz P, Kraines RG, Holman HR. Measurement of patient outcome in arthritis. Arthritis Rheum. 1980;23(2):137–45. doi: 10.1002/art.1780230202. [DOI] [PubMed] [Google Scholar]
- 21.Nondahl DM, Cruickshanks KJ, Wiley TL, Tweed TS, Klein R, Klein BE. Accuracy of self-reported hearing loss. Audiology. 1998;35(5):295–301. doi: 10.3109/00206099809072983. [DOI] [PubMed] [Google Scholar]
- 22.Lehman LF Orsini MBP, Fuzikawa PL, Lima RC, Gonçalves SD. Avaliação Neurológica Simplificada. Belo Horizonte. ALM International, 1997. 104p. CDU 616-002.73. Arquivo online www.saude.pr.gov.br/arquivos/File/hanseniase/public/ans.pdf.
- 23.Donders FC. Beiträge zur pathologischen Anatomie des Auges. Graefes Arch Clin Exp Ophthalmo. 1855;1(1):106–18. [Google Scholar]
- 24.Berg K, Wood-Dauphinee S, Williams JI. The Balance scale: Reliability assessment for elderly residents and patients with an acute stroke. Scand J Rehab Med. 1995;7(1):27–36. [PubMed] [Google Scholar]
- 25.Miyamoto ST, Lombardi I, Jr, Berg Ko, Ramos LR, Natour J. Brasilian version of the Berg balance scale. Braz J Med Biol Res. 2004;37(9):1411–21. doi: 10.1590/s0100-879x2004000900017. [DOI] [PubMed] [Google Scholar]
- 26.Tinetti ME. Performance-oriented assessment of mobility problems in elderly patients. J Am Geriatr Soc. 1986;34(2):114–26. doi: 10.1111/j.1532-5415.1986.tb05480.x. [DOI] [PubMed] [Google Scholar]
- 27.Gomes GC. Tradução, adaptação cultural e exame das propriedades de medida da escala “Performance Oriented Mobility Assessment”– POMA para amostragem de idosos brasileiros institucionalizados (dissertação) Campinas: Universidade Estadual de Campinas. 2003 [Google Scholar]
- 28.Podsiadlo D, Richard S. The Timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39(2):142–8. doi: 10.1111/j.1532-5415.1991.tb01616.x. [DOI] [PubMed] [Google Scholar]
- 29.Rosner B.Fundamentals of Biostatistics. 4a ed New York: Duxbury Press; 1994 [Google Scholar]
- 30.Andrade S, Santos SCM, Serro-Azul JB.Fibrilação Atrial Wajngarten M. Cardiogeriatria. São Paulo: Roca; 2004. p. 132–6. [Google Scholar]
- 31.Hill K, Schwarz J. Assessment and Management of falls in older people. Intern Med J. 2004;34(9-10):557–64. doi: 10.1111/j.1445-5994.2004.00668.x. [DOI] [PubMed] [Google Scholar]
- 32.Feder G, Cryer C, Donovan S, Carter Y. Guidelines for the prevention of falls in people over 65. BMJ. 2000;321(7267):1007–11. doi: 10.1136/bmj.321.7267.1007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ganz DA, Bao Y, Shekelle PG, Rubenstein LZ. Will my patient fall. JAMA. 2007;297(1):77–86. doi: 10.1001/jama.297.1.77. [DOI] [PubMed] [Google Scholar]
- 34.Brotman DJ, Walker E, Laure MS, O'Brien RG. In search of fewer independent risk factors. Arch Intern Med. 2005;165(2):138–45. doi: 10.1001/archinte.165.2.138. [DOI] [PubMed] [Google Scholar]
- 35.Feinberg WM, Blackshear A, Kronmal R, Hart RG. Prevalence, age, distribution, and gender of patients with atrial fibrillation. Arch Intern Med. 1995;155(5):469–73. [PubMed] [Google Scholar]
- 36.Masud T, Morris RO. Epidemiology of falls. Age Ageing. 2001;30(Suppl 4):S3–7. doi: 10.1093/ageing/30.suppl_4.3. [DOI] [PubMed] [Google Scholar]
- 37.Lawlor DA, Patel R, Ebrahim S. Association between falls in elderly women and chronic diseases and drug use: cross sectional study. BMJ. 2003;327(7417):712–7. doi: 10.1136/bmj.327.7417.712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Shumway- Cook A, Brauer S, Woollacott M. Predicting the probability for falls in Community-dwelling older adults using the timed up & go test. Phys Ther. 2000;80(9):896–903. [PubMed] [Google Scholar]
- 39.Cummings SR, Nevitt MC, Kidd SK. Forgetting falls. The limited accuracy of recall of falls in the elderly. J AM Geriatr Soc. 1988;36(7):613–6. doi: 10.1111/j.1532-5415.1988.tb06155.x. [DOI] [PubMed] [Google Scholar]
- 40.Maintenance of sinus rhythm in patient with atrial fibrillation: an AFFIRM substudy of the first antiarrhythmic drug. AFFIRM First Antiarrhythmic Drug Substudy Investigators. J Am Coll Cardiol. 2003;42(1):20–9. doi: 10.1016/s0735-1097(03)00559-x. [DOI] [PubMed] [Google Scholar]
- 41.Greene HL, Graham EL, Werner JA, Sears GK, Gross BW, Gorham JP, et al. Toxic and therapeutic effects of amiodarone in the treatment of cardiac arrhythmias. J Am Coll Cardiol. 1983;2(6):1114–28. doi: 10.1016/s0735-1097(83)80338-6. [DOI] [PubMed] [Google Scholar]
- 42.Charness ME, Morady F, Scheinman MM. Frequent neurologic toxicity associated with amiodarone therapy. Neurology. 1984;34(5):669–7. doi: 10.1212/wnl.34.5.669. [DOI] [PubMed] [Google Scholar]
- 43.Palakurthy PR, Iyer V, Meckler RJ. Unusual neurotoxicity associated with amiodarone therapy. Arch Intern Med. 1987;147(5):881–4. [PubMed] [Google Scholar]
- 44.Ahmed S, Rienstra M, Crijns HJGM, Links TP, Wiesfeld ACP, Hillege HL, et al. Continuous vs episodic prophylactic treatment with amiodarone for the prevention of atrial fibrillation: a randomized trial. JAMA. 2008;300(15):1784–92. doi: 10.1001/jama.300.15.1784. [DOI] [PubMed] [Google Scholar]
- 45.Cairns JA, Connolly SJ, Roberts R, Gent M. Randomised trial of outcome after myocardial infarction in patients with frequent or repetitive ventricular premature depolarisations: CAMIAT. Canadian Amiodarone Myocardial Infarction Arrhythmia Trial Investigators. Lancet. 1997;349(9053):675–82. doi: 10.1016/s0140-6736(96)08171-8. [DOI] [PubMed] [Google Scholar]
- 46.Julian DG, Camm AJ, Frangin G, Janse MJ, Munoz A, Schwartz PJ, et al. European Myocardial Infarct Amiodarone Trial Investigators. Lancet. 1997;349(9053):667–74. doi: 10.1016/s0140-6736(96)09145-3. [DOI] [PubMed] [Google Scholar]
- 47.Vorperian VR, Havighurst TC, Miller S, January CT. Adverse effects of low dose amiodarone: a meta-analysis. J Am Coll Cardiol. 1997;30(3):791–8. doi: 10.1016/s0735-1097(97)00220-9. [DOI] [PubMed] [Google Scholar]