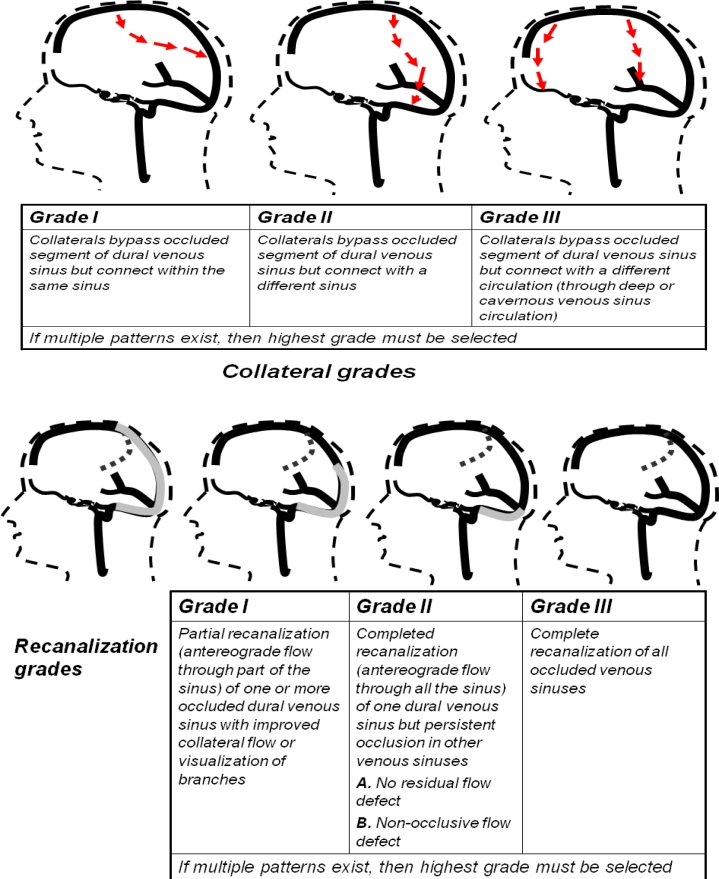
There has been substantial emphasis placed on categorizing recanalization and collateral formation in patients with acute arterial occlusion resulting in ischemic stroke.1–4 Such methods of semi-quantitatively classifying the severity of arterial occlusion for prognostic purposes and assessing the response to treatment have become an integral part of clinical studies.3–4 However, no such method exists for classifying either recanalization or collateral formation in patients with cerebral venous thrombosis. A method with two components is described that can be used to classify recanalization and collateral formation in patients with cerebral venous thrombosis using serial magnetic resonance (MR) or computed tomographic (CT) venography or catheter based angiography with venous phase imaging. The recanalization is classified as follows (see Figure): grade I, partial recanalization of one or more occluded dural sinus with improved collateral flow; grade II, complete recanalization of one sinus but persistent occlusion of the other sinuses [A-no residual flow, B-non occlusive flow]; and grade III, complete recanalization. The collateral formation is classified as follows: grade I, collaterals-bypass occluded segment of dural venous sinus but connect within the same sinus; grade II, collaterals bypass occluded segment but connect with a different sinus; and grade III, collaterals bypass the occluded segment and connect with different circulation. The classification recognizes the superficial and deep venous circulation as distinct pathways with different prognostic implications5 that can be linked through collateral pathways. Further studies are required to assess the inter-observer reliability of the proposed classification and assess the ease of use in clinical studies and practice. Identification of patterns of recanalization and/or collateral formation associated with minimal residual deficits may assist in selecting patients with cerebral venous thrombosis who can benefit from early trans-venous thrombolysis6.
References:
- 1.Qureshi AI. New grading system for angiographic evaluation of arterial occlusions and recanalization response to intra-arterial thrombolysis in acute ischemic stroke. Neurosurgery. 2002;50:1405–14. doi: 10.1097/00006123-200206000-00049. [DOI] [PubMed] [Google Scholar]
- 2.Mohammad Y, Xavier AR, Christoforidis G, et al. Qureshi grading scheme for angiographic occlusions strongly correlates with the initial severity and in-hospital outcome of acute ischemic stroke. J Neuroimaging. 2004;14:235–41. doi: 10.1177/1051228404265716. [DOI] [PubMed] [Google Scholar]
- 3.Khatri P, Neff J, Broderick JP, et al. Revascularization end points in stroke interventional trials: Recanalization versus reperfusion in IMS-I. Stroke. 2005;36:2400–3. doi: 10.1161/01.STR.0000185698.45720.58. [DOI] [PubMed] [Google Scholar]
- 4.Tomsick T, Broderick J, Carrozella J, et al. Revascularization results in the interventional management of stroke II trial. AJNR Am J Neuroradiol. 2008;29:582–7. doi: 10.3174/ajnr.A0843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ferro JM, Bacelar-Nicolau H, Rodrigues T, et al. ISCVT and VENOPORT investigators Risk score to predict the outcome of patients with cerebral vein and dural sinus thrombosis. Cerebrovasc Dis. 2009;28:39–44. doi: 10.1159/000215942. [DOI] [PubMed] [Google Scholar]
- 6.Philips MF, Bagley LJ, Sinson GP, et al. Endovascular thrombolysis for symptomatic cerebral venous thrombosis. J Neurosurg. 1999;90:65–71. doi: 10.3171/jns.1999.90.1.0065. [DOI] [PubMed] [Google Scholar]