Abstract
Background:
Stroke can occasionally manifest with non-lateralizing findings such as somnolence and stuttering. We describe a case and discuss the anatomical and physiological implications of this rare combination of symptoms.
Case report:
A 51-year-old woman presented with 3 days of “feeling drunk”. She could further specify her symptoms as blurry vision, slurred speech, and gait instability. She had a history of hypertension and hyperlipidemia. Her examination at presentation was remarkable only for marked somnolence. Over the next several hours she developed mild upgaze limitation and vertical nystagmus. Non-enhanced computed tomography of the brain was normal. Brain magnetic resonance imaging (MRI) revealed a 5 mm acute infarct in the caudal midbrain. The first week the patient remained somnolent and manifested marked stuttering. The patient improved gradually with speech therapy.
Conclusion:
Strokes affecting the diencephalic-mesencephalic junction can manifest with stuttering. Defective projections of the reticular formation to the supplementary motor area, damaged extrapyramidal circuits, and/or aberrant propioceptive feedback due to involvement of the mesencephalic nucleus of the trigeminal nerve are the proposed pathophysiological mechanisms. Somnolence can also be part of the presentation and is likely due to disruptions of sleep pathways subserved by the reticular activating system. The accurate diagnosis of these cases depends on careful clinical assessment and high index of suspicion for stroke, especially in lieu of preexisting vascular risk factors and lack of an alternative explanation such as toxic-metabolic encephalopathy.
Keywords: Midbrain stroke, somnolence, stuttering, reticular activating system, magnetic resonance imaging
Stuttering is an interruption of the normal rhythm of speech caused by involuntary repetition, prolongation, or arrest of sound. In school-age children the incidence estimates have varied from 0.7% to 4%, whereas in adults the incidence is 0.5%.1 Acquired stuttering can involve mono- or polysyllabic words, is not exclusively confined to the initial syllables, continues with singing, exhibits lack of adaptation, absence of anxiety, and is not accompanied by secondary motor manifestations such as grimacing or fist clenching.2 It usually has a sudden onset due to a clear precipitating factor (toxic-metabolic, psychogenic, or neurologic). The neurologic causes include stroke, head trauma, migraine, multiple sclerosis, and degenerative disorders.3
We present the case of a patient presenting with changes in mental status and acquired stuttering resulting from an acute stroke and discuss the possible underlying pathophysiological correlates.
Case Report
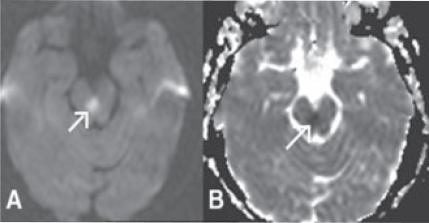
A 51-year-old right-handed woman presented with 3 days of “feeling drunk”, further described as blurry vision, slurred speech, and gait unsteadiness. She had a history of hypertension and hyperlipidemia, but no history of childhood stuttering. Her exam at presentation was remarkable only for marked somnolence. Over the next several hours she developed mild upgaze limitation and vertical nystagmus. Routine labs including toxicology screen were normal. A non-enhanced head computed tomography scan was normal. Brain magnetic resonance imaging (MRI) revealed a 5 mm acute infarct in the midbrain (Figure 1). Further work-up was unrevealing, and the stroke was finally attributed to small vessel disease.
Figure 1.
Brain magnetic resonance imaging, Diffusion-weighted imaging (A), Apparent diffusion coefficient map (B). The arrows point at the area of ischemia.
During the first week, the patient’s somnolence improved gradually, but she developed diplopia, nystagmus, marked stuttering, and ataxia. Repeat brain MRI was unchanged. She was discharged to a rehabilitation facility, where she improved gradually with physical and speech therapy.
Discussion
Stuttering does not localize to a specific anatomic region. Most published cases of acquired stuttering due to stroke resulted from left cortical or bilateral cortical lesions (all cerebral lobes), typically with associated aphasia. Less commonly, stuttering arose from subcortical lesions in the corpus callosum, basal ganglia, bilateral thalami, mesencephalon, and pons.4–6 It has been suggested that the corpus callosum provides the interhemispheric connections responsible for prosody and that the brainstem reticular activating system, the diencephalon, and the basal ganglia participate in the motor execution of speech through their projections to the supplementary motor area.7–8
Consequently, disruptions of these connections can manifest with acquired stuttering.6, 7 An interesting additional theory of stuttering postulates a propioceptive deficit among the adults who stutter. Defective proprioceptive feedback from the jaw in one study was thought to disrupt sensorimotor integration during speech production in the same way movement control is impaired in patients with peripheral neuropathy.9
Infarcts can occasionally manifest with mental status changes. Lesions located in the diencephalic-mesencephalic junction can impair arousal, wakefulness, and the related function of “tonic” attention, while cortical lesions in locations such as the inferior frontal gyrus, inferior parietal lobule, medial frontal lobe, and inferomedial temporal lobe present with a deficit in selective attention without associated somnolence.10 However, in a study of 109 patients with acute change in mental status, only 3 (2.7%) without focal findings were ultimately diagnosed with an ischemic stroke, resulting in a 97% negative predictive value of the neurologic examination.11
In our patient, the sudden onset of stuttering may have been due to involvement of the reticular activating system projecting to the supplementary motor area, involvement of extrapyramidal tracts participating in speech execution and/or impairment of the mesencephalic nucleus of the trigeminal nerve in the periaqueductal gray resulting in impaired proprioception and abnormal sensorimotor integration of speech. The decreased level of wakefulness was likely due to impaired function in the reticular activating system. Thus, the symptom complex of stuttering and somnolence in our patient pointed to a lesion in the diencephalic-mesencephalic junction.
Conclusion
Acquired stuttering can in occasional cases be a manifestation of acute stroke. The relation between brain anatomy and physiology of speech is complex and there is no single focus that localizes to stuttering. On the other hand, stroke can have other non-lateralizing manifestations such as somnolence, particularly in lesions affecting the diencephalic-mesencephalic junction. The accurate diagnosis of these cases becomes challenging when focal neurological findings are not apparent and mental status changes predominate. Physicians should suspect stroke, especially in patients with vascular risk factors and no obvious underlying toxic-metabolic derrangement.
References
- 1.Espir MLE, Rose FC. Stammering. In: Espir MLE, Rose FC, editors. The basic neurology of speech. Blackwell Scientific; Publication, Oxford and Edinburgh: 1970. pp. 122–125. [Google Scholar]
- 2.Helm NA, Butler RB, Benson DF. Acquired stuttering. Neurology. 1978;11:1159–65. doi: 10.1212/wnl.28.11.1159. [DOI] [PubMed] [Google Scholar]
- 3.Sahin HA, Krespi Y, Yilmaz A, Coban O. Stuttering due to ischemic stroke. Behav Neurol. 2005;16:37–9. doi: 10.1155/2005/941926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kakishita K, Sekiguchi E, Maeshima S, Okada H, Okita R, Ozaki F, Moriwaki H. Stuttering without callosal apraxia resulting from infarction in the anterior corpus callosum. A case report. J Neurol. 2004;251:1140–1. doi: 10.1007/s00415-004-0424-1. [DOI] [PubMed] [Google Scholar]
- 5.Ciabarra AM, Elkind MS, Roberts JK, Marshall RS. Subcortical infarction resulting in acquired stuttering. J Neurol Neurosurg Psychiatry. 2000;69:546–9. doi: 10.1136/jnnp.69.4.546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Abe K, Yokoyama R, Yorifji S. On stuttering-like hesitation resulting from infarct in the midbrain and the mesial thalami. Rinsho Shinkeigaku. 1992;32:822–5. [PubMed] [Google Scholar]
- 7.Klouda GV, Robin DA, Graff-Radford NR, Cooper WE. The role of callosal connections in speech prosody. Brain Lang. 1988;35:154–71. doi: 10.1016/0093-934x(88)90106-x. [DOI] [PubMed] [Google Scholar]
- 8.Bhatnagar SC, Andy OJ. Alleviation of acquired stuttering with human centremedian thalamic stimulation. J Neurol Neurosurg Psychiatry. 1989;52:1182–4. doi: 10.1136/jnnp.52.10.1182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Loucks TM, De Nil LF. Anomalous sensorimotor integration in adults who stutter: a tendon vibration study. Neurosci Lett. 2006;402(1–2):195–200. doi: 10.1016/j.neulet.2006.04.002. Epub 2006. [DOI] [PubMed] [Google Scholar]
- 10.Mesulam MM, Waxman SG, Geschwind N, Sabin TD. Acute confusional states with right middle cerebral artery infarctions. J Neurol Neurosurg Psychiatry. 1976;39:84–9. doi: 10.1136/jnnp.39.1.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Benbadis SR, Sila CA, Cristea RL. Mental status changes and stroke. J Gen Intern Med. 1994;9:485–7. doi: 10.1007/BF02599217. [DOI] [PubMed] [Google Scholar]