Abstract
Background
Treatment planning for vascular occlusive disease depends in part on quantitative assessment of the degree of occlusion. Digital subtraction angiography is the gold standard for quantitative imaging although other modalities can also be used.
Discussion:
Three different schemes for measuring percent stenosis of an occluded artery are all valid but may produce different results.
Conclusion:
The choise of method for measurement is less important than consistency of application.
Keywords: vascular occlusion, stenosis, measurement
Introduction
Many modalities are available for assessment of the cerebral arterial anatomy including Doppler ultrasound (U/S), computed tomographic angiography (CTA), magnetic resonance angiography (MRA), and digital subtraction angiography (DSA). DSA remains the gold standard for diagnosis, but the other non-invasive modalities are improving and are being utilized more extensively.
Extracranial Doppler U/S is used in many institutions as the first line tool for assessment of carotid arterial disease. Although an inexpensive, readily available technique, its assessment of cervical arteries is limited as portions of the arteries are difficult to visualize and some portions may not be visualized at all. In addition, a great amount of inter-observer variability exists.1 Studies comparing extracranial Doppler U/S to DSA have shown sensitivities of 91–95% and specificities of 86–97% for carotid arterial diseases. Accuracy in assessment of the degree of stenosis in the vertebral arteries is poorer, with sensitivities of only 65–77% and specificities of 88–93%.2
Intracranial vasculature can be assessed using transcranial Doppler U/S. In order to allow sufficient transmission through the skull, a low frequency transducer is used, resulting in poor spatial resolution but allowing assessment of blood flow velocities.3 Use of this technique for intracranial occlusive disease is showing promise, as published recently in guidelines from the American Academy of Neurology.4 Intracranial occlusive disease can be reasonably detected, and data to define > 50% stenosis is emerging. More research into this area is necessary.
MRA has rapidly improved in terms of vascular imaging. The main techniques include time of flight angiography, or phase-contrast angiography, which may be acquired and reconstructed in either a two- or three-dimensional format.5 A recent meta-analysis found the pooled sensitivity and specificity of MRA to be 95% and 90% respectively, when assessing carotid stenosis of > 70%.6 Intracranial occlusive disease can also be assessed, with reasonable sensitivities and specificities for vessels which are greater than 1 mm in size, including the internal carotid, anterior cerebral, middle cerebral, and posterior cerebral arteries. Maximum intensity projections showed higher specificity than source images, but the sensitivity is similar for both.7
CTA has also generated interest, as it is readily available in most centers and it can be acquired rapidly in the setting of acute stroke. Sensitivity and specificity compared to DSA are 89% and 100% respectively, and CTA offers the advantage of being able to visualize calcifications, which may influence therapeutic decisions. Many feel that CTA is now comparable to MRA, and in some cases may be the superior non-invasive method. However, CTA requires iodinated contrast, and does not visualize the carotid siphon.5
Although DSA remains the gold standard for assessment of extra- or intracranial occlusive disease, it is an invasive procedure and as such has risks of bleeding, infection, renal failure, and minor or major stroke. A review of several series found the mortality rate to be 0.1%, with an overall risk of neurological complication at 4% and permanent neurological sequelae at 1%.8 DSA allows direct visualization of arterial anatomy and the plaque surface, and offers the option of therapeutic intervention.
Quantification can be done by several methods. The basic formula for calculation of the degree of stenosis is:
Where Docclusion is the diameter of the vessel at the point of greatest stenosis and Dnormal is the diameter of a reference vessel.
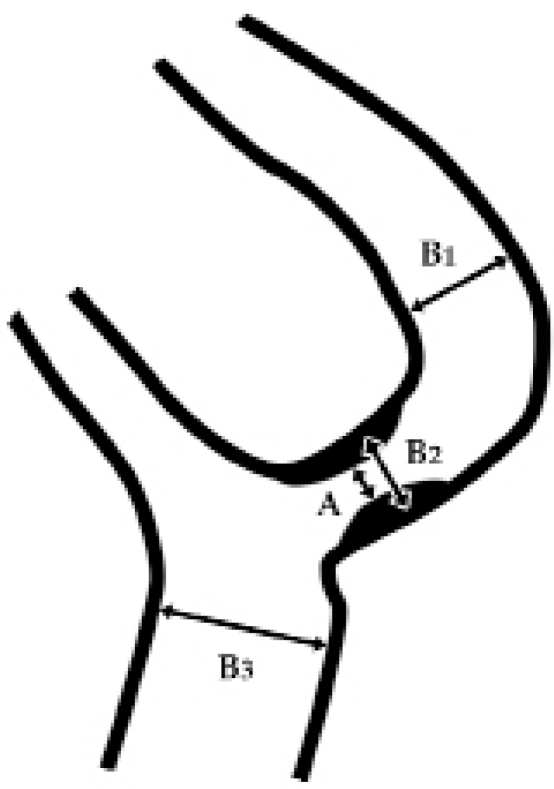
In North America, extracranial occlusions are most often measured by the NASCET (North American Symptomatic Carotid Endarterectomy Trial) criteria. In this method, the reference vessel is the presumed “normal” vessel distal to the stenosis, excluding post-stenotic dilation (Figure 1).9 Other methods include the ECST (European Carotid Surgery Trial) method, in which the reference is the estimated diameter of the “normal” vessel at the same point (Figure 1).10 A third method, called the common carotid technique, uses the diameter of the lumen in the common carotid artery as the reference (Figure 1). Controversy exists over which method is the best, but overall the methods appear to be comparable.11
Figure 1.
Three methods of measuring stenosis. Percent stenosis is (1-A/B)*100, where A is the smallest diameter in the occluded segment and B is the reference (presumably normal) diameter. In the NASCET scheme, B is B1; in the ECST scheme, B is B2; and in the common carotid artery scheme, B is B3 when measuring occlusion in the internal carotid artery.
For measurement of intracranial stenosis, the WASID (Warfarin-Aspirin Symptomatic Intracranial Disease) method is the most commonly used.12 The carotid artery and other intracranial arteries are assessed in different fashions. For all vessels, the diameter of the lumen of the stenotic vessel is used as the numerator. For the denominator, the diameter of the lumen of the “normal” vessel proximal to the stenosis is taken. If the proximal vessel is also diseased, as a second choice, the diameter of the lumen of the distal vessel is taken as the denominator. If this too is diseased, the diameter of the lumen of the feeding vessel is taken as a third choice. This method is used for most intracranial vessels, except for the intracranial portion of the carotid artery. For this vessel, the diameter of the lumen of the vessel at the level of greatest stenosis is compared to the widest portion of the petrous portion of the carotid artery. If the entire petrous portion of the carotid is diseased, the diameter of the lumen of the distal most portion of the extracranial carotid artery is substituted as a second choice.12
Summary
A variety of methods are available for imaging and quantitative assessment of extracranial and intracranial occlusive disease. Although non-invasive techniques are improving, DSA remains the best method for assessment. When evaluating the degree of an arterial occlusion, there are several rational methods of measurement, and the reference standards should always be documented.
Glossary
Abbreviations, in the order used in this report
- U/S:
ultrasound
- CTA:
computed tomographic angiography
- MRA:
magnetic resonance angiography
- DSA:
digital subtraction angiography
References
- 1.Jenkins RH, Mahal R, MacEneaney PM. Noninvasive imaging of carotid artery disease: critically appraised topic. Can Assoc Radiol J. 2003;54:121–123. [PubMed] [Google Scholar]
- 2.Landwehr P, Schulte O, Voshage G. Ultrasound examination of carotid and vertebral arteries. Eur Radiol. 2001;11:1521–1534. doi: 10.1007/s003300100963. [DOI] [PubMed] [Google Scholar]
- 3.Markus HS. Transcranial Doppler ultrasound. Br Med Bull. 2000;56:378–388. doi: 10.1258/0007142001903021. [DOI] [PubMed] [Google Scholar]
- 4.Sloan MA, Alexandrov AV, Tegeler CH, Spencer MP, Caplan LR, Feldmann E, Wechsler LR, Newell DW, Gomez CR, Babikian VL, Lefkowitz D, Goldman RS, Armon C, Hsu CY, Goodin DS. Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology. Assessment: Transcranial Doppler ultrasonography. Report of the Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology. Neurology. 2004;62:1468–1481. doi: 10.1212/wnl.62.9.1468. [DOI] [PubMed] [Google Scholar]
- 5.Bowen BC, Saigal G, Ruiz A. Computed tomographic and magnetic resonance vascular imaging. In: Bradley WG, Daroff RB, Genichel GM, et al., editors. Neurology in Clinical Practice. 4th ed. Elsevier Inc; Philadelphia: 2004. [Google Scholar]
- 6.Nederkoorn PJ, van der Graaf Y, Hunink M. Duplex ultrasound and magnetic resonance angiography compared with digital subtraction angiography in carotid artery stenosis: A systematic review. Stroke. 2003;34:1324–1332. doi: 10.1161/01.STR.0000068367.08991.A2. [DOI] [PubMed] [Google Scholar]
- 7.Stock KW, Wetzel S, Kirsch E, Bongartz G, Steinbrich W, Radue EW. Anatomic evaluation of the circle of Willis: MR angiography versus intraarterial digital subtraction angiography. Am J Neuroradiol. 1996;17:1495–1499. [PMC free article] [PubMed] [Google Scholar]
- 8.Hankey GJ, Warlow CP, Sellar RJ. Cerebral angiography risk in mild cerebrovascular disease. Stroke. 1990;21:209–222. doi: 10.1161/01.str.21.2.209. [DOI] [PubMed] [Google Scholar]
- 9.Barnett HJ, Taylor DW, Eliasziw M, Fox AJ, Ferguson GG, Haynes RB, Rankin RN, Clagett GP, Hachinski VC, Sackett DL, Thorpe KE, Meldrum HE, Spence JD. Benefit of carotid endarterectomy in patients with symptomatic moderate or severe stenosis. North American Symptomatic Carotid Endarterectomy Trail collaborators. N Engl J Med. 1998;339:1415–1425. doi: 10.1056/NEJM199811123392002. [DOI] [PubMed] [Google Scholar]
- 10.European carotid surgery trialists collaborative group Randomized trail of endarterectomy for recently symptomatic carotid stenosis: Final results of the MRC European Carotid Surgery Trial (ECST) Lancet. 1998;351:1379–1387. [PubMed] [Google Scholar]
- 11.Young GR, Humphrey PRD, Nixon TE, Smith ETS. Variability in measurement of extracranial internal carotid artery stenosis as displayed by both digital subtraction and magnetic resonance angiography. Stroke. 1996;27(3):467–473. doi: 10.1161/01.str.27.3.467. [DOI] [PubMed] [Google Scholar]
- 12.Samuels OB, Joseph GJ, Lynn MJ, Smith HA, Chimowitz MI. A standardized method for measuring intracranial arterial stenosis. Am J Neuroradiol. 2000;21:643–646. [PMC free article] [PubMed] [Google Scholar]