Abstract
The Stroke and Neurovascular Program at the Medical College of Wisconsin and Froedtert Hospital, in Milwaukee, is a comprehensive, interdisciplinary center for stroke medicine. The program encompasses an acute stroke team, a neuro-intensive care unit, a stroke care unit, and a stroke rehabilitation program. The staff includes specialists with fellowship training in stroke, neurocritical care, neurointerventional therapy, vascular neurosurgery, interventional neuroradiology, and stroke rehabilitation. Fellowships are offered in interventional neurology, neurocritical care, and vascular neurology. In addition to clinical service and education, the faculty are actively engaged in research. The program is certified by the Joint Commission as a Primary Stroke Center.
Keywords: Primary Stroke Center, neurocritical care, neuro-intervention, neurointensive care, fellowship training
Introduction
The Medical College of Wisconsin & Froedtert Stroke and Neurovascular Program includes a multidisciplinary team of stroke neurologists, interventional neurologists, neurointensivists, neurosurgeons, emergency medicine specialists and rehabilitation specialists (Figure 1) with subspecialty training and a primary clinical focus in the field of cerebrovascular disease. This program is the first full-service, Joint Commission-certified Primary Stroke Center in Wisconsin. Our mission is to provide the best available clinical care for the devastations of stroke and neurovascular illness. Certification by The Joint Commission provides patients and referring physicians with objective evidence of ongoing excellence in quality stroke care.
Figure 1.
Interventional Neurology Team: Front row (left to right): Tom Wolfe (Interventional Neurology Fellow), Brian-Fred Fitzsimmons (Fellowship Program Director), Osama O. Zaidat (Interventional Neurology Director), Joanna Delap (Nurse Coordinator), Charles Sardegna (Research Nurse). Second row (left to right) Syed I. Hussain (Interventional Neurology Fellow), John Lynch (Interventional Neurology Fellow), Kerry Jasin (Fellowship Program Coordinator), Erin Brandenburg (Research Coordinator).
The Neurovascular Program is located at Froedtert Hospital in Milwaukee, Wisconsin, the only academic hospital in Milwaukee. It is the premier neuroscience center in the state of Wisconsin, accounting for 15–20% of overall hospital admissions. It is one of the largest stroke centers in the nation with eight fellowship trained vascular neurologists on the staff. It is the only hospital in Wisconsin with a dedicated Neuroscience Critical Care Unit staffed with fellowship trained neurointensivists.
Premier features of the MCW-Froedtert Stroke and Neurovascular service
Extensive IV tPA experience
Endovascular chemical and mechanical thrombolysis provided by two interventional neurologists with fellowship training in neurointerventional procedures and neurocritical care
Twelve beds in a dedicated Neuro-Intensive Care Unit run by four fellowship trained neurocritical care neurologists
A specialty care Stroke Unit with specially trained stroke and neurocritical care nurses
Second opinion stroke and neurovascular program
Vascular neurosurgery
Stroke Rehabilitation Program
Hyper-Acute Stroke Treatment
Neurons die rapidly after stroke onset and limiting the extent of damage requires urgent, expert evaluation and treatment. The Froedtert & the Medical College of Wisconsin Acute Stroke Team (FAST; Figure 2) implemented rigorous protocols in 1996 for treating ischemic stroke patients with tPA in the first 3 hours after stroke, and has over 30 years of combined experience applying these protocols to hundreds of patients. In addition, they offer intra-arterial thrombolysis and mechanical clot extraction using endovascular methods in the 3–8 hour window after stroke onset in suitable patients.
Figure 2.
The Froedtert & the Medical College of Wisconsin Acute Stroke Team (FAST). Seated (left to right): Brian-Fred Fitzsimmons, MD; Osama O. Zaidat, MD; Conrad Nievera, MD; Joanna Delap, RN; Ann Carol, ANP; and Michel Torbey, MD. Standing (left to right): Ann Helms, MD; Diane Book, MD; Jeffrey Binder, MD; Erin Brandenburg, RN; John Lynch, MD; Denise Lemke, ANP; Charles Sardegna, RN; and Ann Hansen, OT.
Some FAST Facts
24-7-365 Emergency Room coverage by stroke specialists.
Specialized protocols for rapid evaluation.
Average door-to-CT time less than 40 minutes.
Average door-to-tPA time less than 60 minutes.
Neurosciences Intensive Care Unit
Specialized care continues in a dedicated Neuroscience Intensive Care Unit (NICU) where stroke patients receive coordinated care and expert intervention. The NICU is equipped with state-of-the-science monitoring equipment and is the only NICU in Wisconsin staffed by full-time fellowship-trained neuro-intensivists, as well as an experienced team of nurses, therapists, pharmacists and other health professionals.
Vascular Neurosurgery
The Vascular Neurosurgery Program offers a complete range of treatment options for cerebrovascular disorders, including cerebral vascular malformations (cavernous angiomas and arteriovenous malformations), cerebral aneurysms, cerebral insufficiency, and carotid stenosis. Treatment options range from minimally invasive radiosurgery (gamma knife), neuro-endoscopy, and microsurgery, to complex skull base approaches.
Interventional Neurology and Endovascular Therapy
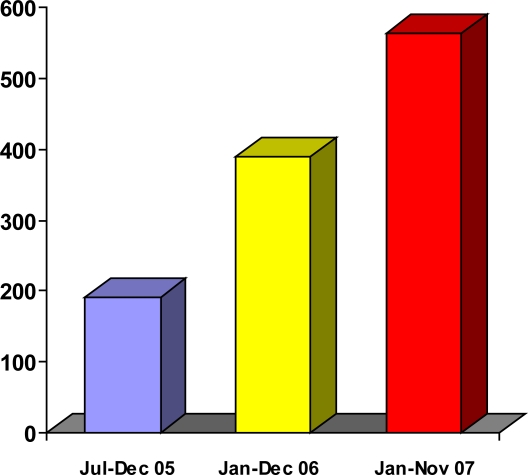
The fellowship trained neurointerventionalists (Figure 3) are supported by nurses and technicians with specialty training in interventional neuroradiology. Endovascular stroke therapy encompasses a wide range of up-to-date advances in intra-arterial treatment of stroke, including thrombolysis in acute ischemia, prevention of recurrent ischemic stroke in the setting of extracranial or intracranial stenosis, treatment of cerebral aneurysms, and non-surgical management of arteriovenous malformations (AVMs). The volume of cases in their interventional neurology practice has significantly increased over the last three years to approximately triple its original volume (Figures 3 and 4). Their clinical outcomes are collectively among the best in the nation.
Figure 3.
Neurointerventionalists performing a case in our state-of-the-art facility (left to right: Drs. Zaidat, Fitzsimmons and Lynch).
Figure 4.
MCW-Milwaukee Neurointerventional Service caseload in the last 3 years.
Endovascular Services
IA thrombolysis up to 6 hours after stroke
Mechanical clot extraction with the Merci Retriever device up to 8 hours after onset
Carotid & vertebral artery stenting/angioplasty
Intracranial stenting using the first approved intracranial stent
Aneurysm coiling, AVM embolization
Acute Stroke Unit
The Acute Stroke Unit is a dedicated inpatient service run by fellowship trained stroke neurologists and staffed by nurses with specialized training in stroke care. Diagnostic, stroke prevention, and risk management protocols consistently exceed national standards of care for stroke established by The Joint Commission and the University Health System Consortium.
Stroke Unit Services
Expert diagnostic evaluation for cause of stroke
State-of-the-art MRI, CT angiography, diagnostic cerebral catheterization, and perfusion imaging
-
Management of complex syndromes:
○ Stroke in the young, hypercoagulable states
○ Stroke with patent foramen ovale, cerebral vein thrombosis
○ Dissection, vasculitis
○ Extracranial carotid disease and occlusion
○ Extracranial vertebral artery disease with proximal subclavian occlusion with subclavian steal syndrome.
○ Intracranial stenosis
○ Cerebral aneurysm
○ Cerebral arteriovenous malformation and fistula
Research Studies
MCW-Froedtert hospital is involved with cutting edge treatments for ischemic and hemorrhagic stroke.
Current Research
Interventional Management of Stroke (IMS-III) study of combined IV and IA thrombolysis in acute ischemic stroke within three hours of symptoms onset versus IV only.
Penumbra mechanical clot retrieval device for acute ischemic stroke within 8 hours of symptoms onset
Wingspan intracranial stenting versus medical therapy in symptomatic intracranial stenosis (SAMMPRIS study)
Neuroflow balloon in acute ischemic stroke
Albumin in acute ischemic stroke therapy
Neuroprotective in ischemic stroke therapy
Micrus coil cerebral aneurysm registry
A Randomized trial of Unruptured Brain AVMs (ARUBA) study
Carotid stent registries
Merci Retriever clot retrieval device registry
Ancrod study
Fellowship Training and Education Opportunities
The Neurovascular Program at the MCW-Froedtert Hospital offers fellowship training for neurologists in five pathways.
Interventional Neurology fellowship: Two years of neurointerventional training with the first year focusing on diagnostic procedures and electives and the second year concentrating on interventional procedures. The pre-requisite is completion of a neurology residency with either vascular neurology or neurocritical care fellowship training.
Neurocritical care fellowship: Duration is two years. Completion of a neurology residency is required.
Combined fellowship of interventional and neurocritical care: Duration is three years. The pre-requisite is completion of a neurology residency. In the first two years the fellow will obtain a certificate of neurocritical care with special qualification in diagnostic neurointervention. The third year focuses on interventional procedures.
Vascular neurology fellowship: Duration is one year. Completion of a neurology residency is required.
Combined fellowship of interventional and vascular neurology: Duration is three years. Completion of a neurology residency is a prerequisite. In the first two years the fellow will obtain a certificate of vascular neurology with special qualification in diagnostic neurointervention and the third year focuses on interventional procedures.
Stroke and Neurovascular Program Faculty at the Medical College of Wisconsin
Jeffrey Binder, MD
Vascular Neurologist
Professor of Neurology
Fellowship training in stroke at Columbia University, New York
Primary interests: stroke diagnosis, acute therapy and prevention, aphasia and cognitive disorders after stroke, functional neuro-imaging of stroke recovery
Diane Book, MD
Vascular Neurologist
-
Medical Director, Stroke Program;
Assistant Professor of Neurology
Fellowship training in stroke at the Medical College of Wisconsin
Primary interests: stroke diagnosis, treatment and prevention, stroke care quality and education, vascular and degenerative dementia
Brian-Fred M. Fitzsimmons, MD
Interventional Neurologist
-
Interventional and Vascular Neurology Fellowship Training Program Director;
Assistant Professor of Neurology and Neurosurgery
Fellowship training in stroke and neurocritical care at Columbia University, New York, and in interventional neuroradiology at New York University Medical Center
Primary interests: endovascular treatment of stroke, carotid and intracranial stenosis, cerebral aneurysms, arteriovenous malformations
Ann Helms, MD, MS
Vascular Neurologist
Assistant Professor of Neurology
Fellowship training in stroke at the Medical College of Wisconsin
Primary interests: stroke diagnosis, treatment and prevention, hyperacute stroke therapy, women’s issues in stroke, hyper-baric medicine
John R. Lynch, MD, FAHA
Vascular Neurologist / Neurointensivist
Assistant Professor of Neurology, Neurosurgery and Internal Medicine
Fellowship training in stroke and neurocritical care at Duke University; completing fellowship in interventional neurology at the Medical College of Wisconsin
Primary interests: acute ischemic stroke therapy, endovascular treatment of stroke, intracerebral hemorrhage, traumatic brain injury, subarachnoid hemorrhage, advanced neurological monitoring, medical complications of acute CNS disease, critical care
John McGuire, MD
Neurovascular Physiatrist
Associate Professor of Physical Medicine and Rehabilitation
Fellowship training in stroke rehabilitation at the Rehabilitation Institute of Chicago
Primary interests: motor recovery, spasticity therapy, electrodiagnosis, motion analysis
Conrad Nievera, MD, DABPN, FPNA
Vascular Neurologist
Assistant Professor of Neurology
Fellowship training in stroke at Indiana University
Primary interests: stroke diagnosis, therapy and secondary prevention, post-stroke seizures
Grant Sinson, MD
Vascular Neurosurgeon
Associate Professor of Neurosurgery
Fellowship training in vascular neurosurgery at the University of Arkansas
Primary interests: cerebral aneurysms and vascular malformations, carotid and intracranial stenosis, tumors of the skull base
Michel Torbey, MD, MPH, FAHA
Vascular Neurologist and Neurointensivist
-
Director, Neuro Intensive Care Unit (NICU);
Associate Professor of Neurology and Neurosurgery
Fellowship training in stroke and critical care neurology at the Johns Hopkins School of Medicine
Primary interests: stroke acute therapy and prevention, intracerebral hemorrhage, neuro-monitoring, neuro-sonology
Osama O. Zaidat, MD, MS
Interventional Neurologist
Director, Interventional Neurology; Associate Professor of Neurology and Neurosurgery
Fellowship training in stroke and neurocritical care at Case Western Reserve University and in neurointerventional therapy at Duke University
Primary interests: acute stroke therapy, endovascular treatment of stroke, carotid, vertebral and intracranial stenosis and stenting, AVM, aneurysm, embolization
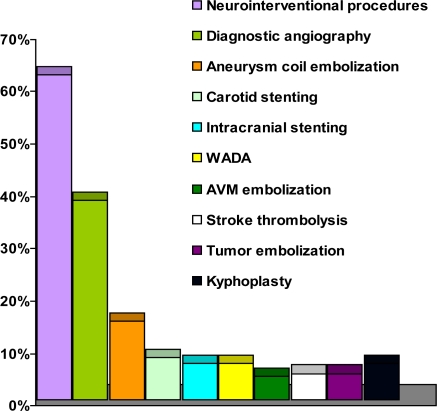
Figure 5.
MCW-Milwaukee types of cases in the last three years.
Glossary
Abbreviations, in the order used in this report
- MCW:
Medical College of Wisconsin
- IV:
intravenous
- tPA:
tissue plasminogen activator
- FAST:
Froedtert acute stroke team
- CT:
external carotid artery
- NICU:
neuro-intensive care unit
- AVM:
arteriovenous malformation
- MRI:
magnetic resonance imaging
- IA:
intra-arterial
- CNS:
central nervous system
Commercial products, in the order referenced in this report
- Merci Retriever®
Concentric Medical, Inc, Mountain View, California, USA