“You are going to put what in my head?” It might seem like science fiction, but stents are a reality and prove helpful to many people. Health care professionals may find it an amazing concept to grasp; just imagine the patient perspective. Neurologists, neurosurgeons, and nurses often encounter many questions from patients and their families. How do you get that object in my brain? Can I still have X-Rays or an MRI? Am I doomed to set off alarms every time I pass through airport security? The information that follows serves to answer frequently asked questions about brain stent placement.
What conditions are brain stents used for?
Two common conditions that stents are used for are intracranial stenosis and brain aneurysms.
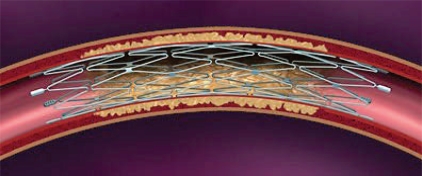
Intracranial stenosis is narrowing of brain blood vessels. Most often, the narrowing is due to atherosclerosis, and a buildup of fat and other substances (plaques) in the blood vessels. When enough plaques build up or a blood clot develops, the artery can become blocked. A stroke can occur if the blood supply to the brain is disrupted. Strokes due to blockages of blood vessels can happen in two main areas: the carotid artery in the neck (main blood supply route to the brain) or in an intracranial artery (an artery within the skull).
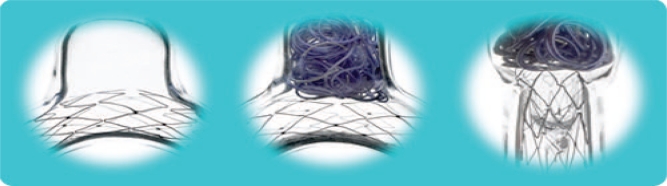
Brain aneurysms are a weak or thin spot on a blood vessel wall in the brain that balloons out and fills with blood. Often this wall is weakened by disease, injury, or an abnormality present at birth. Aneurysms are not always life-threatening, but serious consequences can result if one bursts (ruptures) in the brain, spilling blood into the surrounding tissue. Rupture can cause serious complications including stroke, permanent nerve damage, or death. After rupture, an aneurysm may burst again and re-bleed into the brain, and additional aneurysms may also occur. More commonly, rupture may cause a subarachnoid hemorrhage—bleeding into the space between the skull bone and the brain. A serious complication of subarachnoid hemorrhage is hydrocephalus, in which the excessive buildup of cerebrospinal fluid in the skull ultimately leads to dangerous swelling and pressure on the brain.
How does the doctor insert the stent?
Under angiography (a way to visualize the blood vessels), a catheter is inserted (usually in the groin) and then threaded through the arteries and in either the arteries of the neck or brain depending on the location of the problem. The stent delivery system follows the same path as the catheter, and thus, carries the stent to the treatment site. The stent is then placed. As it is positioned, it expands to conform to the inside contours of the artery wall. After placement, the catheter is removed and the stent stays in place.
Compared with the carotid arteries, the arteries inside the brain are very small and make a lot of twists and turns, so they're somewhat difficult to navigate with a catheter. Because of this, intracranial stent placement requires expertise and specialized equipment.
How do stents work?
When used to treat atherosclerosis in either the carotid arteries or intracranial arteries, stents act as a permanent implant that opens these blocked arteries, allowing improved blood to flow to the brain. Angioplasty (a procedure to widen blockages) along with placement of a stent may be an appropriate stroke treatment or stroke prevention option for some people who have had a stroke or transient ischemic attack (TIA). In angioplasty, a balloon catheter (hollow tube) opens the blocked artery to improve blood flow. The stent provides a barrier to reduce the risk of recurrent narrowing of the artery and also supports the artery wall. Sometimes the doctor may use angioplasty to widen the affected area first; in other cases, angioplasty is not used before stent placement.
When a stent is used to treat brain aneurysms, the doctor inserts a catheter into an artery and threads it through the body to the site of the aneurysm. Using a guide wire, detachable coils (spirals of platinum wire) are passed through the catheter and released into the aneurysm. The coils fill the aneurysm, block it from circulation, and cause the blood to clot, which obliterates the aneurysm. The stent is placed to stabilize the artery either before or after the coil placement to serve as a scaffold or barrier to prevent the coils from protruding back into the parent (main) blood vessel.
What does a stent look like?
A stent is a tube shaped mesh-like object typically made up of a metal called nitinol (nickel titanium alloy). The size of a stent is relatively small; diameters range from 2.5mm to 4.5mm (about 1/5 inch) and lengths between 10–20mm (about 3/4 inch).
Will the stent be drug eluting?
The stents commonly used today to treat intracranial stenosis and brain aneurysms are not drug eluting like some of the stents used for the heart (these kinds of stents are coated with a drug that is slowly released into the vessel wall). Historically, drug-eluting stents were used because of the potential of treating intracranial stenosis with lower rates of reoccurring narrowing of the artery. However, since these stents are designed for use in the heart, there are drawbacks to using them in the more complex arteries of the brain. However, with the advent of the new self-expanding brain stents, the rate of reoccurrence of artery narrowing may be lower.
Can any patient receive a stent?
Some patients who have intracranial stenosis have good results with medications like aspirin and blood thinners and by making lifestyle changes. Stent placement is recommended only for those experiencing symptoms along with severe intracranial stenosis that has not been benefitted by medical treatment. Severe intracranial stenosis is defined as 70% blockage or more. People with diabetes or who have blockages in arteries that can not be accessed with a catheter are not good candidates for this procedure.
Patients with aneurysms should not undergo stent placement if the aneurysm size or vessel size does not fall within the required range, cannot take blood-thinning drugs to help prevent blood clots, or if angiography shows the patient’s anatomy (position and structural makeup of the blood vessels) is not appropriate for endovascular treatment.
What medicines will be needed after the stent is placed?
Double antiplatelet drug therapy is typically prescribed to help prevent the formation of blood clots. The two drugs most often used are aspirin 81 to 325 mg plus clopidogrel 75 mg daily for approximately 1–3 months after stent placement.
Can I have an X-Ray, CT scan or MRI (magnetic resonance imaging) after a stent?
Yes, X-Ray’s and CT scans can be done. Stents are typically MRI-compatible, meaning most people can still have an MRI once the stent in place. However, before MRI testing, patients should check with their doctor and the MRI facility to confirm the type of stent they have and also the field strengths used at the MRI facility.
What about airport security checkpoints?
The stent will not trigger alarms when passing through airport security.
Are there any risks involved?
Yes. There are a variety of complications that can occur including, but not limited to, an artery puncture, stent movement, damage to the lining of the vessel causing an artery dissection, bleeding into the brain, and stroke from artery blockage. Nevertheless, there are also risks for certain patients that do not have a stent placed. For example, patients with 70% to 99% stenosis that are treated with medications alone experience a high rate of stroke. Untreated aneurysms have the potential to rupture. Thus, patients are advised to discuss options, risks, and benefits with their physician to make an informed decision about the best course of treatment for their individual situation.
What is the prognosis?
Because the use of stents for brain aneurysms and intracranial stenosis are relatively new procedures, the long-term results of stent placement are still being investigated. Data from some research studies suggest that stent placement has the potential to reduce the risk of stroke in patients with symptomatic intracranial stenosis as compared with medical therapy alone. The patients most likely to benefit from stent placement are those with stenosis of at least 70% in whom the risks of reccurring strokes are highest; hence, the benefits of stent placement outweigh the potential risks of the procedure. With regards to brain aneurysms, the vast majority of patients that received coiling and then stent placement have the aneurysm successfully blocked from circulation; consequently, the risk of rupture is reduced and deterioation in neurological function is halted.
In conclusion, many patient-derived questions surround the use of stents in the brain. This article serves as an educational resource for the patient, family and friends.
Sources:
- Boston Scientific
- Food and Drug Administration
- Lutsep, Helmi. “Symptomatic intracranial stenosis: best medical treatment vs. intracranial stenting”, Current Opinion in Neurology, Volume 22(1), Feb 2009, p 69–74
- Mayo Clinic
Figure 1.
Portrayal of stent used for treatment of intracranial stenosis (Photo courtesy of Boston Scientific)
Figure 2.
Portrayal of coils and mesh-like stent used for treatment of a brain aneurysm (Photo courtesy of Boston Scientific)