Abstract
Pediatric obesity occurs most frequently in underserved communities where families have difficulty accessing healthcare. Disproportionate obesity rates in rural children denote significant disparities warranting innovative solutions. However, intensive, tertiary-care treatment options outlined in recent expert recommendations may not be available to families living in rural areas. Telemedicine may be useful for providing pediatric obesity treatment to rural families. The aim of this study was to assess the impact of a new outreach program (TeleFIT), which placed telemonitors in four rural satellite clinics to increase access to a pediatric obesity clinic (Brenner Families In Training [FIT]). Before TeleFIT began, of five patients from rural counties enrolled in treatment over a 1-year period, all dropped out by their third visit. Within the first year of TeleFIT, the number of rural patients increased nearly threefold (to 14) and increased again in the second year by an additional 16 new patients (n=35). Preliminary outcomes indicate comparable attrition rates and improvement in weight status compared with patients in conventional treatment. Telemedicine allows rural families to access intensive obesity treatment from local pediatric offices, eliminating geographic barriers. Systems delivering state-of-the-art care in rural areas have tremendous potential for reducing health disparities in rural populations. Further research is needed to test the efficacy of such interventions.
Key words: telemedicine, technology, e-health
Introduction
Obesity effects more than 17% of American children, occurring disproportionately in rural areas,1,2 which have fewer specialty services and families with limited ability to travel for services.3,4 Expert recommendations advocate a staged, family-based approach to pediatric obesity treatment.5 As obesity levels persist, children and their families should participate in increasingly intensive treatments, culminating in referral to comprehensive interventions and tertiary-care clinics. Such services are not readily available to rural families, and the frequency of treatment visits required is also a barrier.6 With the urgent need for treatment, this situation presents a significant gap in healthcare for rural practitioners and families. A few studies have investigated telemedicine to provide pediatric obesity treatment;3,7–11 however, there are no reports of a clinical pediatric obesity treatment utilizing telemedicine to increase reach and decrease attrition in rural areas.
The following study details the experience of one tertiary-care, multidisciplinary pediatric obesity clinic implementing telemedicine technology to reach rural families, briefly assessing the impact on patients enrolling and remaining in treatment.
Subjects and Methods
Brenner Fit (Families in Training)
Brenner FIT (Families In Training) is a multidisciplinary, tertiary-care pediatric obesity clinic composed of a pediatrician, dietitian, family counselor, physical therapist, exercise physiologist, and social worker. Obese children (body mass index [BMI] ≥95th percentile for age and gender) between 2 and 18 years old with a diagnosis of one or more obesity-related comorbidities are seen by physician referral. Details of Brenner FIT have been published previously.12–14
Telefit
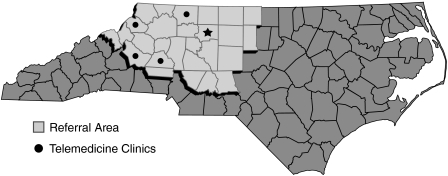
Northwest North Carolina has some of the highest rates of poverty in the state,15 characterized by poor access to quality healthcare and a diminished ability to travel significant distances to receive specialty care.16 Brenner Children's Hospital is the primary source of pediatric subspecialty care within this 19-county region, but the distance that must be traveled is challenging. To overcome travel barriers, four Polycom VSX 3000 Desktop System telemonitors were placed in pediatric offices in Hickory, Lenoir, Boone, and Elkin, NC (Fig. 1), starting in January 2009. Families travel to Brenner Children's Hospital for one intake visit with the Brenner FIT team. Subsequent visits occur every 2–4 weeks via telemonitor at the TeleFIT site closest to their residence, following established Brenner FIT treatment protocols. Medical review visits with the Brenner FIT pediatrician are held following each 4-month treatment phase at the main clinic. Through the TeleFIT program, families were able to reduce the number of trips to the main Brenner FIT clinic to four visits annually, as opposed to 16–18 visits.
Fig. 1.
TeleFIT locations in North Carolina.
The telemonitors feature a 17-inch liquid crystal display with a built-in videocamera, microphone, and speakers, providing an interactive experience between Brenner FIT clinicians and families through real-time bidirectional videoconferencing. Network connectivity to satellite clinics is provided over a Metro-E wide area network connection providing 6 megabits per second of bandwidth for data traffic, as well as videoconferencing communication, which provides exceptional image and sound quality. Videoconferencing with two sites are conducted over commodity Internet (768 kilobits per second) using a digital subscriber line service for Internet access, which has less desirable quality but sufficient to effectively interact with families in a typical treatment visit.
Based on patient referrals, Brenner FIT identified areas more than 60 miles from the main clinic where high rates of pediatric obesity were present without treatment options. Selected pediatric offices were trained in treatment protocols and how telemonitors would be used. Telemonitors were placed in a medical exam room at each respective clinic, installed on lockable cabinets that were used to store educational materials. To accommodate obese families, bariatric couches and chairs were also placed in telemedicine rooms.
Study Design
Brenner FIT uses a prospective, clinical database to track outcomes and patient progress13,14 and includes most clinical data from the intake visit, with follow-up data entered every 4 months during physician re-assessment. This retrospective study measured changes in patient enrollment from rural areas (>60 miles from Brenner FIT in an area of low population density) and in outcomes (attrition from treatment, improvements in BMI z-score) before and after the application of telemedicine technology. All patients seen from November 2007 to January 2011 were included, with outcomes assessment focused on the first 4 intensive months of treatment. This study was approved by the Wake Forest University School of Medicine Institutional Review Board.
Results
Prior to TeleFIT, only five patients from rural counties enrolled in treatment over the period of 1 year, all of whom dropped out by their third visit. In the first year of TeleFIT, the number of families participating from rural counties increased nearly threefold, from 5 to 14, and an additional 16 in the second year. Of the total Brenner FIT patient population, the number of rural families participating increased from 7% to 14% during the study period. There were no significant differences in sociodemographics between TeleFIT and Brenner FIT patients and families (Table 1). However, TeleFIT had significantly fewer total children of minority racial/ethnic background (48% versus 23%, p<0.005 by chi-squared test). Spanish-speaking families were excluded from analysis, as they participate in a separate program, but none were referred to TeleFIT during the study period.
Table 1.
Characteristics and Outcomes of the Study Population, November 2007–January 2011
| CHARACTERISTICa | TELEFITb | BRENNER FITb |
|---|---|---|
| n | 35 | 259 |
| Age (years) (mean±SD) | 11.2±3.49 | 12.1±3.47 |
| Gender | ||
| Female | 60% | 58.7% |
| BMI (kg/m2) (mean±SD) | 35.6±9.3 | 37.1±8.87 |
| BMI z-score | 2.6374±0.6299 | 2.5847±0.4946 |
| Race/ethnicity [% (n)]c | ||
| White | 77% (27) | 52% (134) |
| African American | 20% (7) | 41% (105) |
| Other | 3% (1) | 7% (20) |
| Health insurance [% (n)] | ||
| Medicaid | 57% (17) | 49% (119) |
| Commercial | 43% (13) | 51% (126) |
| Single parent household | 24% (8) | 37% (92) |
| Outcomesa | ||
| BMI z-score improvement [% (n)] | 64% (22) | 69% (179) |
| Attrition [% (n)] | 30% (11) | 32% (83) |
Some variables with missing data (totals may not equal 35 or 259 per respective group).
No significant differences between groups by chi squared test, Fisher's exact test, or t test at p≤0.05.
Excludes Hispanic participants.
BMI, body mass index; SD, standard deviation.
There were no significant differences in outcomes between groups (Table 1), although total study numbers are small. Nearly equal proportions improved their weight status, measured by decrease in BMI z-score, with no significant difference in magnitude of z-score decrease (0.03±0.03 in TeleFIT patients versus 0.09±0.112 in Brenner FIT, not significant by t test). Attrition was also similar (comparable programs, 49–73%17).
Discussion
TeleFIT successfully increased the number of families from rural areas enrolling in treatment. A decreased attrition rate was seen in rural patients after implementing telemedicine technology, and preliminary analysis demonstrates comparable clinical outcomes. Although TeleFIT is new and the sample population is small, our experience suggests that telemedicine technology is feasible for delivering effective multidisciplinary, tertiary-care obesity treatment within rural pediatricians' offices, particularly in light of treatment recommendations10 and an urgent need for services.18
The data presented here are from a small clinical sample and may not be applicable to other centers. Reimbursement for telemedicine services varies widely, as it does for obesity treatment. Whereas other studies have shown the feasibility of using technology in obesity treatment, this project demonstrates that telemedicine can be used to increase the reach of pediatric obesity clinics into rural areas. Additional research is warranted in the use of telemedicine for pediatric obesity treatment in rural populations.
Acknowledgments
The authors would like to thank Karen Klein, Research Support Core, Office of Research, Wake Forest University School of Medicine, for her assistance in editing this manuscript; Darryl Sterner, M.S., Academic Computing, Wake Forest University School of Medicine, for his assistance in technical support; and the participating pediatric offices involved in TeleFIT. Dr. Skelton was supported in part through NICHD/NIH Mentored Patient-Oriented Research Career Development Award K23 HD061597. Additional support was provided by the Duke Endowment Number 6110-SP, Kate B. Reynolds Charitable Trust Grant Number 2009-098, and the Northwest Area Health Education Center.
Disclosure Statement
No competing financial interests exist.
References
- 1.Ogden CL. Carroll MD. Curtin LR. McDowell MA. Tabak CJ. Flegal KM. Prevalence of overweight and obesity in the United States, 1999–2004. JAMA. 2006;295:1549–1555. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- 2.Ogden CL. Carroll MD. Curtin LR. Lamb MM. Flegal KM. Prevalence of high body mass index in US children and adolescents, 2007–2008. JAMA. 2010;303:242–249. doi: 10.1001/jama.2009.2012. [DOI] [PubMed] [Google Scholar]
- 3.Shaikh U. Cole SL. Marcin JP. Nesbitt TS. Clinical management and patient outcomes among children and adolescents receiving telemedicine consultations for obesity. Telemed J E Health. 2008;14:434–440. doi: 10.1089/tmj.2007.0075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Eberhardt MS. Ingram DD. Makuc DM, et al. Health, United States. Hyattsville, MD: National Center for Health Statistics; 2001. 2001. Urban and rural health chartbook. [Google Scholar]
- 5.Barlow SE. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: Summary report. Pediatrics. 2007;120(Suppl 4):S164–S192. doi: 10.1542/peds.2007-2329C. [DOI] [PubMed] [Google Scholar]
- 6.Spear BA. Barlow SE. Ervin C. Ludwig DS. Saelens BE. Schetzina KE. Taveras EM. Recommendations for treatment of child and adolescent overweight and obesity. Pediatrics. 2007;120(Suppl 4):S254–S288. doi: 10.1542/peds.2007-2329F. [DOI] [PubMed] [Google Scholar]
- 7.Schiel R. Beltschikow W. Radon S. Kramer G. Schmiedel R. Rold-Dietrich B. Stein G. Long-term treatment of obese children and adolescents using a telemedicine support programme. J Telemed Telecare. 2008;14:13–16. doi: 10.1258/jtt.2007.070504. [DOI] [PubMed] [Google Scholar]
- 8.Goulis GD. Boren SA. Bontis L. Balas EA. Maglaveras N. Avramides A. Effectiveness of home-centered care through telemedicine applications for overweight and obese patients: A randomized controlled trial. Int J Obes. 2004;28:1391–1398. doi: 10.1038/sj.ijo.0802773. [DOI] [PubMed] [Google Scholar]
- 9.Frisch S. Zittermann A. Berthold HK. Gotting C. Kuhn J. Kleesiek K. Stehle P. Korte H. A randomized controlled trial on the efficacy of carbohydrate-reduced or fat-reduced diets in patients attending a telemedically guided weight loss program. Cardiovasc Diabetol. 2009;8:36–46. doi: 10.1186/1475-2840-8-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Haugen HA. Tran ZV. Wyatt HR. Barry MJ. Hill J. Using telemedicine to increase participation in weight maintenance programs. Obesity. 2007;15:3067–3077. doi: 10.1038/oby.2007.365. [DOI] [PubMed] [Google Scholar]
- 11.McTigue KM. Conroy MB. Hess R. Using the internet to translate an evidence-based lifestyle intervention into practice. Telemed J E Health. 2009;15:851–858. doi: 10.1089/tmj.2009.0036. [DOI] [PubMed] [Google Scholar]
- 12.Irby M. Kaplan S. Garner-Edwards D. Kolbash S. Skelton JA. Motivational interviewing in a family-based pediatric obesity program: A case study. Families Systems Health. 2010;28:236–246. doi: 10.1037/a0020101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Halvorson E. Skelton JA. Appointment attendance in a pediatric weight management clinic. Clin Pediatr (Phila) 2011. May 27, [Epub ahead of print]. [DOI] [PMC free article] [PubMed]
- 14.Skelton JA. Goff DC., Jr Ip E. Beech BM. Attrition in a multidisciplinary pediatric weight management clinic. Child Obes. 2011;7:185–193. doi: 10.1089/chi.2011.0010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.U.S. Census Bureau. Small area income and poverty estimates. Dec 8, 2010. www.census.gov. [May 16;2010 ]. www.census.gov
- 16.Horner SD. Ambrogne J. Coleman MA. Hanson C. Hodnicki D. Lopez SA. Talmadge MC. Traveling for care: Factors influencing health care access for rural dwellers. Public Health Nurs. 1994;11:145–149. doi: 10.1111/j.1525-1446.1994.tb00393.x. [DOI] [PubMed] [Google Scholar]
- 17.Skelton JA. Beech BM. Attrition in paediatric weight management: A review of the literature and new directions. Obes Rev. 2011;12:e273–e281. doi: 10.1111/j.1467-789X.2010.00803.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Robinson TN. Treating pediatric obesity: Generating the evidence. Arch Pediatr Adolesc Med. 2008;162:1191–1192. doi: 10.1001/archpedi.162.12.1191. [DOI] [PubMed] [Google Scholar]