Abstract
Background
Immune reconstitution (IR) after hematopoietic stem cell transplantation (HSCT) reduces transplantation-related complications such as infection and improves HSCT outcomes.
Methods
We retrospectively analyzed IR of lymphocyte subpopulations in 38 pediatric patients for hematologic malignant diseases after allogeneic HSCT from April 2006 to July 2008. T-cell-, B-cell-, and natural killer (NK) cell-associated antigens were assayed in peripheral blood by flow cytometry analysis of 5 lymphocyte subsets, CD3+, CD3+/CD4+, CD4+/CD8+, CD16+/CD56+, and CD19+, before and 3 and 12 months after transplantation.
Results
Reconstitutions of CD16+/CD56+ and CD3+/CD8+ lymphocytes were achieved rapidly, whereas that of CD3+/CD19+ lymphocytes occurred later. Age was not related to reconstitution of any lymphocyte subset. Total body irradiation (TBI) and anti-thymocyte globulin (ATG) administration were related to delayed reconstitution of total lymphocytes and CD3+ lymphocytes, respectively. Reconstitutions of CD3+/CD4+ lymphocytes and CD3+/CD8+ lymphocytes were significantly delayed in patients who received umbilical cord blood stem cells. In patients with chronic graft-versus-host disease (cGVHD), recovery of the total lymphocyte count and CD19+ lymphocytes at 3 months post-transplant were significantly delayed. However, acute GVHD (aGVHD) and cytomegalovirus (CMV) reactivation did not influence the IR of any lymphocyte subset. Further, delayed reconstitution of lymphocyte subsets did not correspond to inferior survival outcomes in this study.
Conclusion
We observed that some lymphocyte reconstitutions after HSCT were influenced by the stem cell source and preparative regimens. However, delayed CD19+ lymphocyte reconstitution may be associated with cGVHD.
Keywords: Immune reconstitution, Hematopoietic stem cell transplantation, Children, Lymphocyte subset
INTRODUCTION
Hematopoietic stem cell transplantation (HSCT) has become the established therapy for numerous hematological, oncological, immunological, metabolic and autoimmune disorders in children [1]. Long-term host immune reconstitution (IR) after allogeneic HSCT (allo-HSCT) is critical because severe post-transplant infections, relapses, and secondary malignancies may be directly related to persistent immune defects [2]. Further, immune deficiencies, including cellular and antibody immunity, can last for more than a year, resulting in increased susceptibility to infections [2].
Various steps in the HSCT procedure can compromise pre-existing host immunity and IR after transplantation. Although treatment intensity may vary based on the disease and clinical condition of a patient, most treatment protocols destroy the recipient's immune system almost completely. Moreover, alloreactive donor T cells co-transfused with the graft will eradicate any remaining recipient cells of hematopoietic origin. In addition, graft-versus-host disease (GVHD) and infection can aggravate the situation [3].
Immune recovery after HSCT has been extensively studied in adults [3-6]. After transplantation, monocytes are the first cells to engraft, followed by granulocytes, macrophages, and natural killer (NK) cells [7, 8]. These cell populations restore most of the recipient's innate immune system, resulting in reduced need for antibacterial prophylaxis. In contrast to the rapid reconstitution of the innate immune system, reconstitution of lymphoid cells of the adaptive compartment is delayed, resulting in persistent deficits in global immunity. Circulating B cells may not reach normal levels for at least 12 months after transplantation and T-cell reconstitution may be delayed for more than 2 years [9].
Delayed immune recovery limits the clinical efficacy of HSCT, resulting in increased opportunistic infections, reactivation of latent viral and parasitic infections, chronic inflammation, development of autoimmunity, and high relapse rate [10, 11]. Several retrospective studies conducted in relatively small numbers of patients have shown that the rate of immune reconstitution is associated with clinical outcomes, such as relapse, survival, and non-relapse mortality [12-16].
IR after HSCT is influenced by various host- and transplantation-related factors, including stem cell and donor sources, recipient age, and method of T-cell depletion (TCD) [2, 3, 17]. Post-transplant factors, such as GVHD, prophylaxis or treatment of GVHD, antimicrobial drugs or administration of intravenous immunoglobulins (IVIgs) for prophylaxis, and donor lymphocyte infusion, can also affect post-transplant immune functions [2, 3, 17].
Although several studies have been conducted in relatively small numbers of patients, the data on IR after allogeneic HSCT in children are insufficient [11, 18-21]. Generally, the rate of immune function recovery after HSCT is rapid in children than in adults. In addition, in children, the donor type, stem cell source, TCD, GVHD, and/or cytomegalovirus (CMV) reactivation affect lymphocyte reconstitution, as in adults.
Here, IR, which is represented by recovery of each lymphocyte subset, in 38 children was analyzed. Further, the study analyzed potential factors affecting lymphocyte immune restoration after allogeneic HSCT in children, including age, type of donor, source of hematopoietic stem cells, GVHD and/or CMV reactivation. In addition, correlations between reconstitution of each lymphocyte subset and HSCT outcomes such as overall survival, relapse, and/or event-free survival were analyzed.
MATERIALS AND METHODS
1. Patients
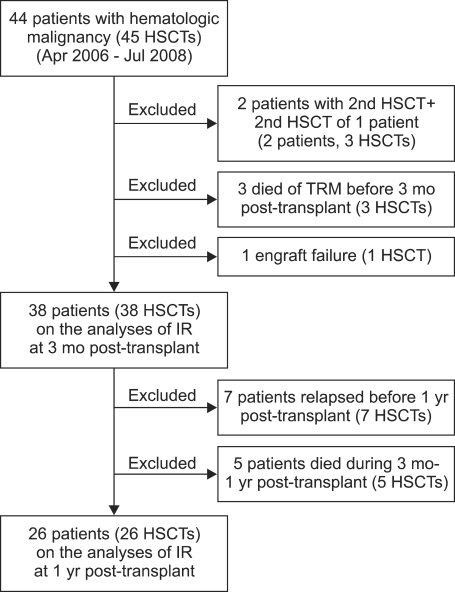
During April 2006 - July 2008, 44 children underwent 45 HSCT for hematologic malignancies in the Department of Pediatrics at the Asan Medical Center. Among the 44 patients, the IR data for the following patients were not included in the study: (1) Three patients who died of treatment-related complications before 3 months post-transplant; (2) Two patients, both of whom received their first transplants before 2006, who received their second transplants for relapsed diseases; (3) One patient who received 2 HSCTs because of disease relapse 7 months after the first transplant; in this case, the IR data for the second HSCT was not included; and (4) One patient who received cord blood stem cell and experienced secondary engraft failure after ganciclovir treatment against CMV reactivation. In summary, 38 reconstitution data from 38 patients who survived for more than 100 days after HSCT were included in the analysis of lymphocyte reconstitution at 3 months post-transplant (Fig. 1).
Fig. 1.
Patients included in the study.
For analyzing lymphocyte reconstitution at 1 year post-transplant, the data for 7 patients who experienced relapse before 1 year post-transplant and 5 patients who died during three months - 1 year post-transplant were not available; therefore, the reconstitution data of only 26 patients were included (Fig. 1). These 26 children remained disease-free and were followed up for at least 1 year post-transplant.
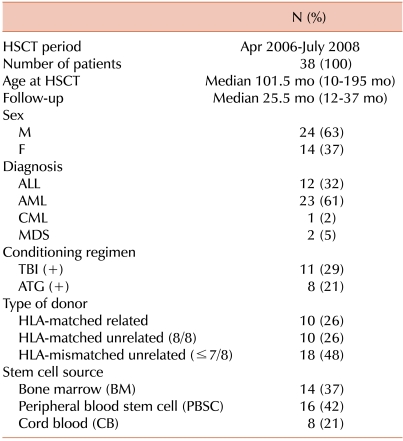
The patient characteristics are summarized in Table 1.
Table 1.
Patient characteristics.
Abbreviations: ALL, acute lymphoblastic leukemia; AML, acute myeloid leukemia; CML, chronic myeloid leukemia; MDS, myelodysplastic syndrome; HLA, human leukocyte antigen; TBI, total body irradiation; ATG, anti-thymocyte globulin.
2. Transplantation procedures
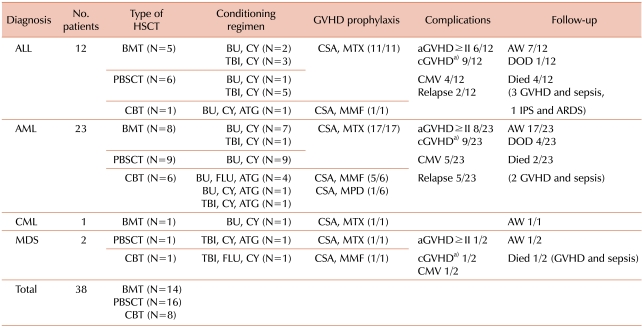
The preparative regimen for individual transplant varied according to the disease, donor type, and/or stem cell source (Table 2). All patients received high-dose myeloablative chemotherapy.
Table 2.
Summary of HSCT procedures and outcomes.
a)Limited or extensive.
Abbreviations: HSCT, hematopoietic stem cell transplantation; AW, alive and well; DOD, died of disease; ALL, acute lymphoblastic leukemia; AML, acute myeloid leukemia; CML, chronic myeloid leukemia; MDS, myelodysplastic syndrome; BMT, bone marrow transplantation; PBSCT, peripheral blood stem cell transplantation; CBT, cord blood stem cell transplantation; BU, busulfan; CY, cyclophosphamide; TBI, total body irradiation; FLU, fludarabine; ATG, anti-thymocyte globulin; CSA, cyclosporin A; MTX, methotrexate; MMF, mycophenolate mofetil; MPD, methyl prednisolone; IPS, idiopathic pneumonia syndrome; ARDS, acute respiratory distress syndrome.
Prophylaxis for GVHD for most patients consisted of a short course of methotrexate (MTX) and cyclosporine A (CsA). All patients who had cord blood stem cell transplantation (CBT) received CsA and mycophenolate mofetil (MMF), except 1 patient who received CsA and methyl prednisolone (MPD).
The first-line treatment for acute GVHD (aGVHD) was high-dose MPD. Further, if a favorable response to the MPD therapy was not evident within 5 to 7 days, the second-line medication was administered on a case by case basis.
All patients received prophylactic antibiotics until neutrophil engraftment was observed, and received antifungal agents for 75 days post-transplant unless GVHD developed, which required additional immunosuppressive treatment. A prophylactic dose of acyclovir was administered for 100 days or 1 year depending on the recipient's immunity to varicella. CMV reactivation, which is presence of the nuclear CMV-related antigen pp65 in the blood, was preemptively treated with ganciclovir and/or foscavir.
All patients received 500 mg/kg prophylactic IVIgs alternate weeks from 7 days post-transplant until 90 days; further, every 4 weeks until 180 days post-transplant, as long as the patient was alive and there was no concern of volume overload for IVIg infusion.
HSCT procedures and survival outcomes are summarized in Table 2.
3. Immunophenotypic studies
T-cell-, B-cell-, and NK-associated antigens in the peripheral blood (PB) were evaluated using fluorescence-activated cell sorter (FACS) system, after which we analyzed 5 lymphocyte subsets, namely CD3+, CD3+/CD4+, CD3+/CD8+, CD16+/CD56+, and CD19+ cells. The sequential analysis of lymphocyte recovery was performed at 3 time points: pre-transplant, 3 months post-transplant, and 12 months post-transplant. The absolute number of each lymphocyte subpopulation was calculated from the total number of PB lymphocytes. Owing to low total lymphocyte counts (TLC) in the early immune recovery phase after HSCT, we calculated the absolute counts of lymphocyte subsets and not their relative frequencies. These results were then related to age-matched reference values for healthy children [22]. A lymphocyte subset was considered immunophenotypically reconstituted or normalized if the absolute count of a lymphocyte subset surpassed fifth percentile for age-matched healthy population.
4. Statistical analysis
The standard deviation scores (SDSs) based on reference values for Korean children [23] were used as quantitative descriptors for each lymphocyte subpopulation, because these scores reflected the normal variations of lymphocyte counts according to age and sex.
Patients were subdivided according to their age, type of donor, type of stem cell source, CMV reactivation, and/or GVHD (grade ≥II). The SDSs of each immunophenotype was compared to detect statistically significant differences using Mann-Whitney's rank-sum test for 2 groups and Kruskal-Wallis variance analysis for more than 2 groups.
In addition, patients were divided into 2 groups: one with recovery of each lymphocyte subpopulation achieved at 3 months post-transplant and the other without recovery. Patient characteristics, conditions on transplant, complications, and outcome parameters, such as relapse, event, and survival in the 2 groups were compared using chi-square or Fischer's exact test. The probabilities of overall survival (OS), relapse-free survival (RFS), and event-free survival (EFS) at 2 years after HSCT for each group were estimated using Kaplan-Meyer method, where OS was defined as the time between date of HSCT and date of death/latest follow-up; RFS, the time between date of HSCT and date of diagnosis of relapse; and EFS, the time between date of HSCT and date of death, loss during follow-up, or diagnosis of relapse, whichever occurred first. Statistical differences were analyzed using Mann-Whitney's rank-sum test.
All reported P-values were 2-sided probability levels and those less than 0.05 were considered statistically significant. Statistical analyses were performed using Statistical Package for the Social Sciences (SPSS) 14.0 software.
RESULTS
1. Lymphocyte reconstitution in all patients
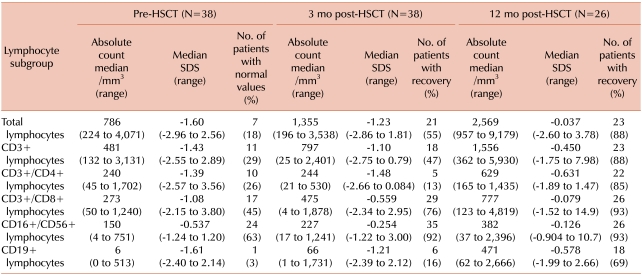
The lymphocyte recovery patterns in all 38 HSCTs are shown in Table 3.
Table 3.
Summary of lymphocyte reconstitution in all patients.
Abbreviation: SDS, standard deviation score; this was calculated on the bases of the reference values from Kim et al. (2001) [23].
CD19+ lymphocyte reconstitution was the slowest, followed by CD4+ lymphocytes. At 3 months post-transplant, only 16% of patients had recovered their CD19+ cell counts above the fifth percentile value for age-matched healthy population, and only 69% of patients who survived for more than 1 year after HSCT without disease relapse at 12 months post-transplant. CD3+/CD4+ lymphocyte counts showed the lowest median SDS at 3 months post-transplant, but reconstitution was achieved in 85% of patients without relapse for more than a year.
Conversely, rapid recovery was observed for CD16+/CD56+ and CD3+/CD8+ lymphocytes at 3 months post-transplant in 92% and 76% of patients, respectively.
2. Potential factors influencing lymphocyte reconstitution
The factors potentially influencing fast IR were age, conditioning regimen, donor type according to the level of HLA-matches, source of stem cells, GVHD, and/or CMV reactivation
1) Age
Patients were divided into 2 subgroups, patients below 10 years of age (N=23) and those aged above 10 years (N=15). The lymphocyte subtype reconstitution in both the groups showed no statistical differences with regard to the distribution of sex, disease, TBI, and/or ATG in the preparative regimen, donor type, and stem cell source; however, the younger group showed more numbers of CD34+ cells (P=0.049).
The younger patient group showed significantly high SDS for all lymphocyte subtypes and TLC at pre-transplant (data not shown). However, at 3 months and 12 months post-transplant, no statistical difference in SDS for any lymphocyte subset was observed, with the exception of CD3+/CD4+ lymphocytes at 3 months post-transplant, for which younger patients showed a significantly high SDS (P=0.010). Nonetheless, the proportion of recovered patients in each group was not statistically different for any lymphocyte subset (Table 4).
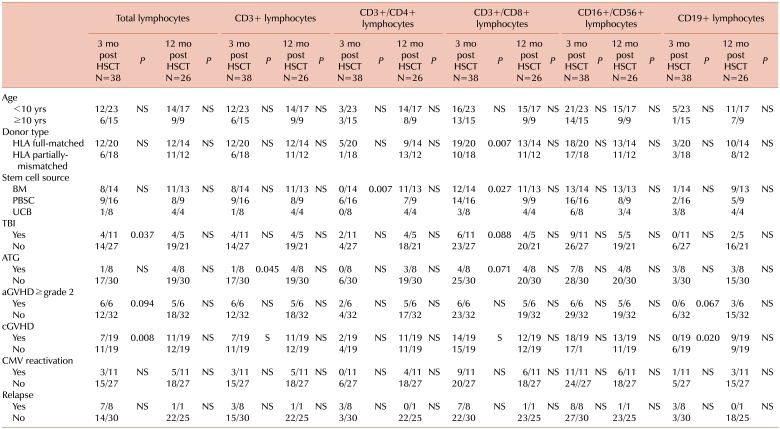
Table 4.
HSCT characteristics and complications affecting lymphocyte reconstitution.
All data are presented as (N patients with reconstitution of lymphocyte subset of the corresponding column)/(N patients with the condition of the corresponding row).
Abbreviation: NS, not significant; statistically significant results are shown in boxes; BM, bone marrow; PBSC, peripheral blood stem cell; UCB, umbilical cord blood stem cell.
2) TBI in conditioning regimen
There were no statistical differences in any other transplant-related conditions between the group of patients who received TBI and those who did not. aGVHD prevalence was not related to TBI but chronic GVHD (cGVHD) developed more frequently in patients who received TBI (P=0.013).
The TBI group showed low SDSs for all lymphocyte subsets before HSCT, but the values obtained were not statistically different. This tendency persisted after transplant, but only SDS of TLC at 3 months post HSCT showed statistical significance (P=0.026).
The proportion of patients who achieved normal TLC at 3 months after HSCT was significantly low in the TBI group (P=0.037), but no other lymphocyte reconstitution showed differences between the TBI and non-TBI group (Table 4).
3) ATG in conditioning regimen
Eight patients were administered ATG, of whom 7 received umbilical cord blood stem cells (UCB) (P=0.035, for stem cell source between ATG group and non-ATG group). At 3 months post-transplant, the SDSs of CD16+/CD56+ and CD19+ lymphocytes were significantly low in the ATG group (P=0.029 and <0.001, respectively), and the proportion of patients showing CD3+ lymphocyte reconstitution was significantly low in the ATG group (P=0.045; Table 4). At 12 months post-transplant, patients in the ATG group showed similar SDSs for all lymphocyte subsets and TLC. IR between ATG and non-ATG groups did not differ at 12 months post-transplant (Table 4).
4) Donor type and stem cell source
The IR differences were also analyzed according to the donor type. Patients were divided into 2 subgroups: one with complete donor HLA match and the other with partial donor HLA mismatch, regardless of kinship. Further, there were no other significant differences in conditions between the 2 groups. Although there were a high number of aGVHD patients in the HLA-mismatched group, no significant differences were observed between the 2 groups for any lymphocyte subsets, except for a high CD3+/CD8+ lymphocyte recovery in the HLA-matched group (P=0.007; Table 4).
The SDS of each lymphocyte subset showed no significant difference among the 3 stem cell sources [bone marrow (BM), PB stem cells (PBSC), and UCB], except for CD3+/CD4+ and CD3+/CD8+ lymphocytes at 3 months post-transplant, where the UBC group showed the lowest SDS (P=0.050 and 0.014, respectively). The IR achievement for both CD3+/CD4+ and CD3+/CD8+ lymphocytes was both high and statistically significant in the PBSC group (P=0.007 and 0.027, respectively; Table 4). However, at 12 months post-transplant, the proportion of patients who achieved reconstitution of any specific lymphocyte subset showed no statistical significance among the 3 groups (Table 4).
5) GVHD
At 3 months post-transplant, the SDS of CD19+ lymphocyte was significantly low in the aGVHD group (P=0.001). In addition, few patients in the aGVHD group showed total lymphocyte or CD19+ lymphocyte reconstitution at 3 months post-transplant, but the numbers were not statistically significant (Table 4).
The prevalence of cGVHD was significantly high in the TBI group (P=0.013). The proportion of the patients who achieved IR at 3 months post-transplant was significantly lower in the cGVHD group than in the non-cGVHD group (TLC and CD19+ lymphocyte, P=0.008 and 0.020, respectively; Table 4). In addition, only cGVHD, and not TBI was found to be independently related to delayed IR of total lymphocyte during multivariate analysis (P=0.009).
6) CMV reactivation
The SDSs of each lymphocyte subset did not differ with respect to CMV reactivation at 3 months post-transplant. However, at 12 months post-transplant, the SDS of CD3+/CD8+ lymphocytes was significantly high in the CMV reactivation group (P=0.039). IR of each lymphocyte subset did not differ between the 2 groups.
3. Comparisons of survival according to the reconstituted lymphocyte subset
The RFS, EFS, and OS were analyzed for all patients who survived more than 100 days after HSCT.
The probability of RFS at 48 months after HSCT for all patients was 75.1±8.1%. At any time point and for all lymphocyte subsets, no statistically significant difference in RFS was observed between patients who achieved a specific lymphocyte reconstitution and those who did not.
The probability of EFS at 48 months post-transplant for all patients was 61.1±8.4%. At 3 months post-transplant, higher EFS was observed in patients with CD3+ lymphocyte reconstitution than those without reconstitution; however, the P-value was not significant (77.8% vs 48.5%; P=0.09). CD3+/CD4+, CD3+/CD8+, CD16+/CD56+, and CD19+ lymphocyte reconstitution at months post-transplant was not related to change in EFS.
The probability of OS at 48 months post-transplant for all patients was 70.3±7.5%. There were no statistical differences in OS between the patients with reconstitution and those without reconstitution for any lymphocyte subset at 3 months after HSCT.
DISCUSSION
We analyzed IR of lymphocyte subpopulations after allogeneic HSCT in 38 patients with 38 HSCTs for hematological malignancies. Recovery in all patients, which was measured as IR values above the fifth percentile of age-matched reference values [22], was achieved most patients who survived more than 1 year without relapse. Notably, 92% of patients achieved IR of CD16+/CD56+ lymphocytes at 3 months post-transplant. However, IR for CD19+ cells was achieved in only 69% at 1 year post-transplant. In addition, CD3+/CD8+ lymphocyte recovery occurred faster than CD3+/CD4+ lymphocyte recovery. These results showed that each lymphocyte subset reconstitution develops at different rate, which was similar to that described in previous studies [7, 8]. Further, long-term imbalance between recovery of CD3+/CD4+ helper T cells and CD3+/CD8+ suppressor/cytotoxic T cells is a well-known phenomenon [24, 25].
Storek et al. [26] showed that advanced age, graft type (BM versus PBSC), CD34 cell dose, TBI in the conditioning regimen, and aGVHD and cGVHD impaired T-cell reconstitution in adults following T-cell replete HSCT. Studies at Memorial Sloan-Kettering Cancer Research Center (MSKCC) showed that age above 19 years and administrating ATG to prevent graft rejection following TCD related or unrelated BMT adversely impacted CD4+ T cell recovery and acquisition of normal T-cell function [27, 28]. Other studies also showed that adult recipients of TCD unrelated BM transplantation (BMT) experienced prolonged and profound CD3+, CD4+, and CD8+ T-cell deficiencies than in young recipients of unrelated BMT and adult recipients of related BM. Additionally, they showed significantly increased risk of life-threatening opportunistic infections and that the rate of recovery of CD4+ T cells correlated with the risk of developing these infections [29, 30].
We identified some factors influencing a specific lymphocyte IR.
Many studies have shown age as an important factor influencing IR, even in children [11, 20]. However, we did not observe age to affect the recovery of any lymphocyte subset. This might be partly because the fifth percentiles of absolute counts of CD3+/CD4+ T lymphocyte counts and other lymphocyte subsets are high in young children, which shows an increased "recovery threshold" with lower age [20]. The comparatively slow recovery of CD4+ T lymphocytes shown in this study was consistent with that shown in other studies on children [11, 20]; however, our results did not agree with that shown by Mackall et al. [25], in which thymus-dependent reconstitution of CD3+/CD4+ lymphocytes after cytotoxic therapy was delayed in adults than in children. CD8+ suppressor/cytotoxic lymphocytes rapidly recovered to normal absolute counts after allogeneic HSCT in children, despite potential damage to the thymus by myeloablative therapy [24, 28].
De Vries et al. [20] reported no significant difference in the recovery rate of main lymphocyte subpopulations between HLA-identical and HLA-matched unrelated transplants, which is consistent with that of our study, except for delay in CD8+ lymphocyte reconstitution in the HLA-mismatched group.
Stem cell source also influences the rate of lymphocyte reconstitution. Ottinger et al. [31] reported that IR of naïve (CD4+/CD45RA+) and memory (CD4+/CD45RO+) helper T cells and CD19+ B cells was faster in PBSC transplant (PBSCT) recipients than in BMT recipients. Morbidity and mortality because of opportunistic infections was high in CBT recipients, because of delayed or disturbed IR [32-34]. In this study, compared to BMT or PBSCT recipients, CBT recipients showed significantly delayed CD4+ and CD8+ T cell reconstitutions at 3 months post-transplant. Moreover, all 6 patients who achieved CD4+ lymphocyte recovery at 3 months post-transplant were PBSCT recipients. No differences in IR of CD8+ and CD16+/CD56+ lymphocytes were observed with regard to the stem cell source, which is in agreement with other studies [31, 32].
The composition of a preparative regimen is known to influence IR [3, 26]. All patients included in this study received various myeloablative conditioning. TBI was performed for 11 patients, of which 8 were ALL patients. A delayed TLC recovery was observed in these patients at 3 months post-transplant, than in non-TBI patients. There were no differences in IR according to the type of leukemia (lymphoid vs. myeloid; data not shown). Eight patients received ATG conditioning, of which 7 were CBT recipients. The CD3+ recovery in these patients was significantly lower than that in patients without ATG conditioning.
Immunophenotypic assessment showed that aGVHD has little impact on the rate of lymphoid reconstitution [2, 35]. However, aGVHD is a major predictor of cGVHD and both have been shown to negatively impact recipient thymic function, even after curing cGVHD [36]. Our study showed similar results, in that aGVHD was not related to IR of any lymphocyte subset. However, cGVHD patients showed significantly delayed total lymphocyte recovery and CD19+ lymphocyte IR at 3 months post-transplant.
We also noted an improved EFS tendency in patient with CD3+ lymphocyte reconstitution at 3 months post-transplant. However, impaired reconstitution of any lymphocyte subset examined in this study could not be correlated to impaired survival.
In conclusion, the IR of different lymphocyte subsets occurred at different rates after allogeneic HSCT in children. Further, although CD16+/CD56+ lymphocyte reconstitution was achieved in most patients by 3 months post-transplant, CD3+/CD4+ and CD19+ lymphocytes showed delayed reconstitution. In addition, stem cell source, TBI and/or ATG conditioning, and cGVHD were found to be related to delayed recovery of specific lymphocyte subset. However, impaired reconstitution of any lymphocyte subset examined in this study was not correlated to impaired survival outcome. Future studies involving large number of patients and entailing functional analysis of reconstituted lymphocyte subsets are necessary to confirm our findings.
Footnotes
This study was supported by a grant from the National R&D Program for Cancer Control, Ministry for Health and Welfare, Republic of Korea (0520290-3).
References
- 1.Gross TG, Egeler RM, Smith FO. Pediatric hematopoietic stem cell transplantation. Hematol Oncol Clin North Am. 2001;15:795–808. doi: 10.1016/s0889-8588(05)70252-5. [DOI] [PubMed] [Google Scholar]
- 2.Parkman R, Weinberg KI. Immune reconstitution following hematopoietic cell transplantation. In: Applebaum FR, Forman SJ, Negrin RS, Blume KG, editors. Thomas hematopoietic stem cell transplantation. 4th ed. West Sussex, UK: John Wiley & Sons; 2008. pp. 222–232. [Google Scholar]
- 3.Storek J, Geddes M, Khan F, et al. Reconstitution of the immune system after hematopoietic stem cell transplantation in humans. Semin Immunopathol. 2008;30:425–437. doi: 10.1007/s00281-008-0132-5. [DOI] [PubMed] [Google Scholar]
- 4.Lum LG. The kinetics of immune reconstitution after human marrow transplantation. Blood. 1987;69:369–380. [PubMed] [Google Scholar]
- 5.Verma UN, Mazumder A. Immune reconstitution following bone marrow transplantation. Cancer Immunol Immunother. 1993;37:351–360. doi: 10.1007/BF01526790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Storek J, Witherspoon RP, Storb R. T cell reconstitution after bone marrow transplantation into adult patients does not resemble T cell development in early life. Bone Marrow Transplant. 1995;16:413–425. [PubMed] [Google Scholar]
- 7.Williams KM, Gress RE. Immune reconstitution and implications for immunotherapy following haematopoietic stem cell transplantation. Best Pract Res Clin Haematol. 2008;21:579–596. doi: 10.1016/j.beha.2008.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Storek J, Zhao Z, Lin E, et al. Recovery from and consequences of severe iatrogenic lymphopenia (induced to treat autoimmune diseases) Clin Immunol. 2004;113:285–298. doi: 10.1016/j.clim.2004.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Petersen SL, Ryder LP, Bjork P, et al. A comparison of T-, B- and NK-cell reconstitution following conventional or nonmyeloablative conditioning and transplantation with bone marrow or peripheral blood stem cells from human leucocyte antigen identical sibling donors. Bone Marrow Transplant. 2003;32:65–72. doi: 10.1038/sj.bmt.1704084. [DOI] [PubMed] [Google Scholar]
- 10.Hollander GA. Lymphoid reconstitution following hematopoietic stem cell transplantation. Of mice and men: progress made in HSCT immunobiology. Semin Immunopathol. 2008;30:369–370. doi: 10.1007/s00281-008-0139-y. [DOI] [PubMed] [Google Scholar]
- 11.Kalwak K, Gorczynska E, Toporski J, et al. Immune reconstitution after haematopoietic cell transplantation in children: immunophenotype analysis with regard to factors affecting the speed of recovery. Br J Haematol. 2002;118:74–89. doi: 10.1046/j.1365-2141.2002.03560.x. [DOI] [PubMed] [Google Scholar]
- 12.Baron F, Baker JE, Storb R, et al. Kinetics of engraftment in patients with hematologic malignancies given allogeneic hematopoietic cell transplantation after nonmyeloablative conditioning. Blood. 2004;104:2254–2262. doi: 10.1182/blood-2004-04-1506. [DOI] [PubMed] [Google Scholar]
- 13.Kim DH, Sohn SK, Won DI, Lee NY, Suh JS, Lee KB. Rapid helper T-cell recovery above 200×106/L at 3 months correlates to successful transplant outcomes after allogeneic stem cell transplantation. Bone Marrow Transplant. 2006;37:1119–1128. doi: 10.1038/sj.bmt.1705381. [DOI] [PubMed] [Google Scholar]
- 14.Krause H, Hebart H, Jahn G, Muller CA, Einsele H. Screening for CMV-specific T cell proliferation to identify patients at risk of developing late onset CMV disease. Bone Marrow Transplant. 1997;19:1111–1116. doi: 10.1038/sj.bmt.1700801. [DOI] [PubMed] [Google Scholar]
- 15.Novitzky N, Davison GM, Hale G, Waldmann H. Immune reconstitution at 6 months following T-cell depleted hematopoietic stem cell transplantation is predictive for treatment outcome. Transplantation. 2002;74:1551–1559. doi: 10.1097/00007890-200212150-00012. [DOI] [PubMed] [Google Scholar]
- 16.Storek J, Espino G, Dawson MA, Storer B, Flowers ME, Maloney DG. Low B-cell and monocyte counts on day 80 are associated with high infection rates between days 100 and 365 after allogeneic marrow transplantation. Blood. 2000;96:3290–3293. [PubMed] [Google Scholar]
- 17.Geddes M, Storek J. Immune reconstitution following hematopoietic stem-cell transplantation. Best Pract Res Clin Haematol. 2007;20:329–348. doi: 10.1016/j.beha.2006.09.009. [DOI] [PubMed] [Google Scholar]
- 18.Foot AB, Potter MN, Donaldson C, et al. Immune reconstitution after BMT in children. Bone Marrow Transplant. 1993;11:7–13. [PubMed] [Google Scholar]
- 19.Kook H, Goldman F, Padley D, et al. Reconstruction of the immune system after unrelated or partially matched T-cell-depleted bone marrow transplantation in children: immunophenotypic analysis and factors affecting the speed of recovery. Blood. 1996;88:1089–1097. [PubMed] [Google Scholar]
- 20.de Vries E, van Tol MJ, van den Bergh RL, et al. Reconstitution of lymphocyte subpopulations after paediatric bone marrow transplantation. Bone Marrow Transplant. 2000;25:267–275. doi: 10.1038/sj.bmt.1702141. [DOI] [PubMed] [Google Scholar]
- 21.Moretta A, Maccario R, Fagioli F, et al. Analysis of immune reconstitution in children undergoing cord blood transplantation. Exp Hematol. 2001;29:371–379. doi: 10.1016/s0301-472x(00)00667-6. [DOI] [PubMed] [Google Scholar]
- 22.Comans-Bitter WM, de Groot R, van den Beemd R, et al. Immunophenotyping of blood lymphocytes in childhood: Reference values for lymphocyte subpopulations. J Pediatr. 1997;130:388–393. doi: 10.1016/s0022-3476(97)70200-2. [DOI] [PubMed] [Google Scholar]
- 23.Kim JS, Lee WK, Suh JS, et al. T and B cell changes with aging. Korean J Clin Pathol. 2001;21:135–140. [Google Scholar]
- 24.Favrot M, Janossy G, Tidman N, et al. T cell regeneration after allogeneic bone marrow transplantation. Clin Exp Immunol. 1983;54:59–72. [PMC free article] [PubMed] [Google Scholar]
- 25.Mackall CL, Hakim FT, Gress RE. T-cell regeneration: all repertoires are not created equal. Immunol Today. 1997;18:245–251. doi: 10.1016/s0167-5699(97)81664-7. [DOI] [PubMed] [Google Scholar]
- 26.Storek J, Joseph A, Dawson MA, Douek DC, Storer B, Maloney DG. Factors influencing T-lymphopoiesis after allogeneic hematopoietic cell transplantation. Transplantation. 2002;73:1154–1158. doi: 10.1097/00007890-200204150-00026. [DOI] [PubMed] [Google Scholar]
- 27.Small TN, Avigan D, Dupont B, et al. Immune reconstitution following T-cell depleted bone marrow transplantation: effect of age and posttransplant graft rejection prophylaxis. Biol Blood Marrow Transplant. 1997;3:65–75. [PubMed] [Google Scholar]
- 28.Small TN, Papadopoulos EB, Boulad F, et al. Comparison of immune reconstitution after unrelated and related T-cell-depleted bone marrow transplantation: effect of patient age and donor leukocyte infusions. Blood. 1999;93:467–480. [PubMed] [Google Scholar]
- 29.Mackall CL, Fleisher TA, Brown MR, et al. Age, thymopoiesis, and CD4+ T-lymphocyte regeneration after intensive chemotherapy. N Engl J Med. 1995;332:143–149. doi: 10.1056/NEJM199501193320303. [DOI] [PubMed] [Google Scholar]
- 30.Small TN. Immune reconstitution in pediatric patients following hematopoietic stem-cell transplantation. In: Kline RM, editor. Pediatric hematopoietic stem cell transplantation. New York, NY: Informa Healthcare; 2006. pp. 271–285. [Google Scholar]
- 31.Ottinger HD, Beelen DW, Scheulen B, Schaefer UW, Grosse-Wilde H. Improved immune reconstitution after allotransplantation of peripheral blood stem cells instead of bone marrow. Blood. 1996;88:2775–2779. [PubMed] [Google Scholar]
- 32.Giraud P, Thuret I, Reviron D, et al. Immune reconstitution and outcome after unrelated cord blood transplantation: a single paediatric institution experience. Bone Marrow Transplant. 2000;25:53–57. doi: 10.1038/sj.bmt.1702089. [DOI] [PubMed] [Google Scholar]
- 33.Niehues T, Rocha V, Filipovich AH, et al. Factors affecting lymphocyte subset reconstitution after either related or unrelated cord blood transplantation in children- a Eurocord analysis. Br J Haematol. 2001;114:42–48. doi: 10.1046/j.1365-2141.2001.02900.x. [DOI] [PubMed] [Google Scholar]
- 34.Szabolcs P, Niedzwiecki D. Immune reconstitution after unrelated cord blood transplantation. Cytotherapy. 2007;9:111–122. doi: 10.1016/j.bbmt.2007.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Noel DR, Witherspoon RP, Storb R, et al. Does graft-versus-host disease influence the tempo of immunologic recovery after allogeneic human marrow transplantation? An observation on 56 long-term survivors. Blood. 1978;51:1087–1105. [PubMed] [Google Scholar]
- 36.Weinberg K, Blazar BR, Wagner JE, et al. Factors affecting thymic function after allogeneic hematopoietic stem cell transplantation. Blood. 2001;97:1458–1466. doi: 10.1182/blood.v97.5.1458. [DOI] [PubMed] [Google Scholar]