Abstract
Background
The generally high job-related stress level among physicians may lead to various health impairments in the long run. Apart from job-related stress, stress during leisure time and certain personality traits might be risk factors for health impairments. However, very little research on the health situation of primary care physicians (PCPs) in Germany is available. Therefore, the objective of the present study was to systematically assess the stress experience and the health situation of German PCPs. One main focus was on mental health.
Methods
In 2009, a state-wide survey among practice-based PCPs in the federal German state of Rhineland-Palatinate (cross-sectional study, n = 2092) was carried out in order to assess stress and strain as well as the health situation.
Results
790 participants (37.7%) were eligible for the analyses. One in four PCPs exceeded the cut-off value ≥ 3 for depression in the PHQ-2 (PHQ, Patient Health Questionaire). Moreover, approximately one in six PCPs stated that he or she had used psychotropic drugs or other psychoactive substances at least once in the preceding year. Stress during leisure time, type D personality and low job satisfaction were associated with the presence of mental health impairments in the binary logistic regression analyses.
Conclusion
All in all, it appears that mental health impairments are a common health problem among the PCPs. Target-group-specific measures should be taken in order to reduce the subjective stress level, and to foster mental hygiene. Furthermore, the development of favorable personality profiles and the corresponding behavioral patterns should be supported.
Physicians are subject to intense occupational stress (e1– e3), and long-term stress harms their well-being. Health impairments such as high blood pressure (e4), burnout syndrome (e5, e6), depression (1– 3), and substance dependencies (e2, e7) have been linked to occupational stress. One established approach to the assessment of occupational stress is the so-called occupational gratification crisis model (4, 5), according to which stress arises when persistent hard work (effort) does not yield a corresponding gratification (reward). Another important component of this model is a personality-based tendency to devote excessive effort to work, to the individual’s own detriment (“overcommitment”).
Physician surveys have revealed a high degree of stress according to this model (6, 7), as well as associations between stress and impaired mental health (2, 3, 8). Although occupational stress among physicians and its effects on physicians’ health have been thoroughly investigated in other countries, there have been no more than a few empirical studies to date on the situation among primary care physicians (PCPs) in Germany. All surveys of German PCPs until now have been inadequate in one (or both) of the following ways: The questions dealt exclusively with the quantity of work (working hours, number of patients), and no standardized instruments were applied for the assessment of subjective occupational stress (9); or else the relation of stress to the physicians’ health was not studied, at least not explicitly (10, 11, e8). Moreover, little attention has been devoted to the stress that physicians experience in their leisure time, which may be important, in view of the possibility of inadequate mental hygiene. Physicians’ health and mental health may also be influenced by personality traits such as resilience and the type D personality pattern. Emotional resilience is generally considered to be a protective factor against health impairments (e9– e11), while type D personality has been found to be a risk factor for various health problems (e12– e15). Type D persons readily fall into negative emotional states (“negative affectivity”), while also tending to suppress the expression of negative feelings (“social inhibition”) (12).
We used standard instruments to study the effect of experienced stress and personality-related factors on the health of German PCPs. Our a priori expectations were that occupational stress, stress during leisure time, and the type D personality pattern would be positively associated with impaired mental health, while resilience would be negatively associated with impaired mental health.
Methods
Study design and recruitment of subjects
In June and July 2009, a written questionnaire was sent to all 2092 specialists in general medicine, primary care physicians, and physicians without postgraduate specialty training who were then in private practice in the German federal state of Rhineland-Palatinate. This cross-sectional survey was carried out anonymously and was announced in the newsletter of the Rhineland-Palatinate state medical association (Landesärzteblatt Rheinland-Pfalz).
Questionnaire
The questionnaire contained instruments for the assessment of occupational stress (the short form of the Effort-Reward Imbalance Questionnaire [ERI-Q] [13]), stress during leisure time (the B4 subscale of a questionnaire for the assessment of subjective stress and dissatisfaction at work [SBUS-B4] [14]), and personality traits (type D personality [12], resilience [15]), as well as screening instruments for the assessment of mental health and other health-related issues. It took about 30 minutes to fill out.
Mental health indicators
The Patient Health Questionnaire-2 (PHQ-2) (16) was used to screen for the presence of depressive symptoms. We used the recommended cutoff value of
≥ 3 points for the definition of depression. The participants were asked the global yes/no question whether they had taken any “psychoactive medications or other psychoactive substances” in the past year and were also asked whether they had a mental illness.
How we dealt with missing values of the ERI-Q (short form)
A relatively large number of participants did not respond to items 4 and 5 of the short form of the ERI-Q (61 and 51 missing responses, corresponding to 7.7% and 6.5% of the total, respectively.) These missing values were replaced by the mean of each participant’s responses to the remaining five items of the same subscale (“Reward”).
Statistical analysis
Only the participants whose main professional activity was primary care and who furnished some sociodemographic data (at least sex) were included in the statistical analysis. The results of univariate analyses are presented here in terms of absolute and relative frequencies and the corresponding 95% confidence intervals. Potential sex-specific differences were studied with chi-squared tests. Depressivity, mental illness, and the consumption of psychoactive drugs were analyzed with binary logistic regression models. First, an automatic backward selection was carried out for each dependent variable (p-value for exclusion: 0.05) with the potential predictors shown in Table 1. The resulting models were analyzed with an inclusion method to increase the power and generalizability of the findings.
Table 1. Initial set of independent variables for the prediction of depressive symptoms, mental illness, and consumption of psychoactive drugs in binary logistic regression models.
| Variable | Scale | Type of content |
| Age | categorical: 5 categories | sociodemographic |
| Sex | categorical: male, female | sociodemographic |
| Children | categorical: yes, no | sociodemographic |
| Life partner | categorical: yes, no | sociodemographic |
| Workweek | metrical (hours) | job-related |
| Length of midday break | metrical (minutes) | job-related |
| Cooperation with medical colleague(s) | categorical: yes, no | job-related |
| Job satisfaction | categorical: 3 categories | job-related |
| Resilience | categorical: quartiles | personality traits |
| Type D personality | categorical: yes, no | personality traits |
| SBUS-B B4 | categorical: quartiles | subjective stress in leisure time |
| Overcommitment | categorical: quartiles | subjective occupational stress |
| Effort–reward ratio | categorical: quartiles | subjective occupational stress |
SBUS-B: a questionnaire for the assessment of subjective stress and dissatisfaction at work
The probability of type I error was set a priori at α = 0.05. The statistical analysis was performed with SPSS 18.0 and Excel 2003.
Results
808 physicians responded to the questionnaire (response rate, 38.6%). 790 (37.7%) met the above criteria for inclusion in the statistical analysis.
Description of the study sample
551 of the PCPs (69.7%) were men, and 239 (30.3%) were women. 502 (63.5%) were between the ages of 46 and 60. Seventy-five (9.5%) were not living with a partner, and 92 (11.6%) had no children. The PCPs reported a mean weekly working time of 54.4 hours (standard deviaton [SD] 12.7 hours), of which roughly one-quarter (13.4 hours) was spent on administrative tasks.
Frequency of depressivity, mental illness, and the consumption of psychoactive drugs
Nearly one PCP in four (182, 23.0%) met or exceeded the PHQ-2 cutoff value for depression. Moreover, 74 (9.4%) stated that they had some type of mental illness. More than one in six (138, 17.5%) reported having taken psychoactive drugs or other psychoactive substances at least once in the past year. Male and female PCPs did not differ in the frequency of mental health impairments. The prevalences (with 95% confidence intervals) of depressive symptoms, mental illness, and the consumption of psychotropic substances in the past year are given as decimal fractions in Table 2.
Table 2. (Point) prevalences and 95% confidence intervals for mental illness, depressive symptoms, and the consumption of psychoactive drugs in the past year, expressed in decimal fractions.
| Men | Women | Overall | ||||
| Mental illness | 0.09 | 0.07–0.12 | 0.09 | 0.06–0.13 | 0.09 | 0.07–0.11 |
| Depressive symptoms (PHQ-2 ≥ 3) | 0.23 | 0.20–0.27 | 0.23 | 0.17–0.28 | 0.23 | 0.20–0.26 |
| Consumption of psychoactive drugs | 0.17 | 0.14–0.20 | 0.18 | 0.13–0.23 | 0.17 | 0.15–0.20 |
PHQ. Patient Health Questionnaire
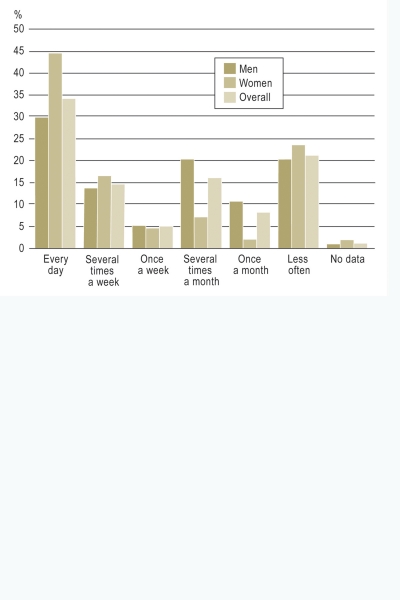
Among the 138 PCPs who said they had consumed psychoactive drugs or other psychoactive substances in the past year, female PCPs were more likely than male PCPs to have used such substances every day or multiple times a week (chi-square test for multiple times per week or more frequently, versus once a week or less frequently: p<0.05). The distribution of frequencies of consumption of psychoactive drugs and other substances among the PCPs who consumed them is shown in the Figure.
Figure.
The frequency of consumption of psychoactive drugs among primary care physicians (PCPs) who reported having consumed such drugs at least once in the past year (95 men, 43 women, 138 PCPs overall).
Multivariate contextual analyses
In the multivariate analysis of depressive symptoms, all measures of stress stayed in the regression model (Table 3). The SBUS-B B4 variable characterizing stress during leisure time was the measure most closely associated with depressivity: Persons in the second, third, and fourth quartiles on the SBUS-B4 scale were much more likely to have depressive symptoms than those in the first quartile. Persons in the third and fourth quartiles of the ERI-Q variable “overcommitment” were also more likely to have depressive symptoms. With respect to a further variable in the ERI-Q, namely, the effort–reward ratio, a significant difference in the frequency of depressive symptoms was seen only between the first and fourth quartiles. Moreover, participants with a type D personality were 1.8 times more likely than others to have depressive symptoms; on the other hand, high job satisfaction was negatively associated with the presence of depressive symptoms.
Table 3. Results of the multivariate analyses of depressive symptoms, mental illness, and consumption of psychoative drugs (binary logistic regression models, inclusion method).
| Predictor | Depressive symptoms, n = 720 | Mental illness, n = 717 | Consumption of psychoactive drugs in the past year, n = 773 | |||||||
| aOR*1 | 95% CI*2 | aOR*1 | 95% CI*2 | aOR*1 | 95% CI*2 | |||||
| Age (years) | 31–45 | ref.*3 | – | *5 | *5 | |||||
| 46–50 | 0.62 | n. s.*4 | ||||||||
| 51–55 | 1.08 | n. s.*4 | ||||||||
| 56–60 | 1.51 | n. s.*4 | ||||||||
| >60 | 2.206 | 1.07–4.50 | ||||||||
| SBUS-B B4 (quartiles) | 1st | ref.*3 | – | ref.*3 | – | *5 | ||||
| 2nd | 4.09*7 | 1.79–9.36 | 3.04*6 | 1.23–7.52 | ||||||
| 3rd | 3.41*7 | 1.59–7.32 | 2.10 | n. s.*4 | ||||||
| 4th | 9.46*7 | 4.21–21.27 | 4.04*7 | 1.74–9.36 | ||||||
| Overcommitment (quartiles) | 1st | ref.*3 | – | *5 | *5 | |||||
| 2nd | 1.16 | n. s.*4 | ||||||||
| 3rd | 2.17*6 | 1.03–4.58 | ||||||||
| 4th | 3.44*7 | 1.59–7.43 | ||||||||
| Effort–reward ratio (quartiles) | 1st | ref.*3 | – | *5 | *5 | |||||
| 2nd | 0.91 | n. s.*4 | ||||||||
| 3rd | 1.11 | n. s.*4 | ||||||||
| 4th | 2.32*6 | 1.00–5.38 | ||||||||
| Job satisfaction | little or none | ref.*3 | – | *5 | ref.*3 | – | ||||
| partial or moderate | 0.39*7 | 0.24–0.61 | 0.76 | n. s.*4 | ||||||
| near-total or total | 0.21*7 | 0.07–0.67 | 0.19*7 | 0.07–0.57 | ||||||
| Type D personality | no | ref.*3 | – | ref.*3 | – | ref.*3 | – | |||
| yes | 1.81*6 | 1.15–2.86 | 2.88*7 | 1.65–5.03 | 2.20*7 | 1.45–3.33 | ||||
| Resilience | 1st | *5 | ref.*3 | – | *5 | |||||
| (quartiles) | 2nd | 0.24*7 | 0.12–0.49 | |||||||
| 3rd | 0.50*6 | 0.25–0.99 | ||||||||
| 4th | 0.13*7 | 0.04–0.45 | ||||||||
| Children | no | *5 | *5 | 2.33*7 | 1.41–3.86 | |||||
| yes | ref.*3 | |||||||||
*1adjusted odds ratio;
*2 95% confidence interval;
*3reference category;
*4not significant at the 5% level;
*5 not contained in the final model after automatic backward selection;
*6 p<0.05;
*7 p<0.01; SBUS, questionnaire for the assessment of subjective stress and dissatisfaction at work
The multivariate analysis of mental illness revealed that stress during leisure time and type D personality were positively associated with this dependent variable (just as they were with depressive symptoms; see above). The chance of having mental illness was nearly three times higher in persons with a type D personality had a nearly three times greater chance of developing mental illness (compared to persons without a type D personality), and four times higher among persons in the highest leisure-time stress category (compared to persons in the corresponding reference group). Furthermore, resilience was negatively associated with the presence of mental illness: Among persons in the highest resilience category, the probability of mental illness was reduced by 87% (odds ratio 0.13).
With respect to the consumption of psychoactive substances, a strong positive association was found with type D personality, and a negative one with subjective job satisfaction. Nagelkerke’s R2, a statistical measure of explained variance, was 43.1% for depressive symptoms, 21.8% for mental illness, and 14.2% for the consumption of psychoactive substances.
Discussion
Main findings
23% of the PCPs surveyed met or exceeded the cutoff value for the presence of depression. It should be emphasized that the PHQ-2 is merely a screening instrument and is no substitute for the well-founded diagnosis of depression by a clinical specialist. The question whether depressive symptoms are any more frequent than usual in the study population can only be answered by comparison with a control group, e.g., the general population. A validation study was recently performed on a random sample of 5010 people that was representative of the German population (17); using the results of that study for comparison, we find that the mean total PHQ-2 score in our sample of PCPs (1.77, 95% confidence interval [CI] 1.67–1.87) was markedly higher than that in the overall population sample (0.94, 95% CI 0.90–0.97). Thus, PCPs apparently suffer from a higher degree of depressivity than the general population. This finding remains even when the validation sample is restricted to persons who have received higher education, and when age- and sex-specific comparisons are carried out. Likewise, in another validation study involving 580 patients of primary care physicians (16), the percentage of subjects meeting or exceeding the cutoff value for depression (15.2%, 95% CI 12.5–18.3) was lower than among the PCPs participating in the present study (Table 2).
Another way to characterize the extent of depressive symptoms in PCPs is to compare it with that among other types of professionals, and particularly with other types of physicians. International studies in which screening instruments for depression were used have mostly yielded lower rates of depression among PCPs, e.g., 10% in a British study of 620 PCPs (18) and comparable figures in other studies (2, e16). The only study with a higher rate was one carried out among Japanese medical residents in their first and second years, about 29% of whom met the screening criteria for depression (3). It must be borne in mind, however, that physicians beginning their training differ in many ways from physicians in the later stages of their professional lives. Overall, comparisons with the general population and with other types of physicians indicate that our sample of PCPs in Rhineland-Palatinate was indeed affected especially strongly by depressive symptoms. One reason may be their high degree of occupational stress (7); PCPs in Germany seem to be subject to more stress than their colleagues in the United States and the United Kingdom (10).
One PCP in six reported having consumed psychoactive drugs or other psychoactive substances at least once in the past year. This finding is comparable to that of a survey recently conducted among PCPs in twelve European countries (19), in which the consumption of psychoactive drugs or other psychoactive substances was assessed in the same way. Unfortunately, the PCPs were not asked what substances they had consumed. We may assume, however, that legal but potentially habit-forming substances such as alcohol or tobacco were not counted by the subjects as psychoactive substances, as their consumption had been assessed separately in earlier items of the questionnaire. The percentage of PCPs consuming psychoactive substances in our survey was much higher than the value of 7.3% among employees that was reported in the Health Report of the German Company Health Insurance Funds (BKK Gesundheitsreport) (e17). One reason may be that doctors have ready access to prescription drugs and may be prescribing them to themselves (e18).
The PCPs in our sample seemed to suffer from mental illness at about the same rate as the general population (20, 21, e19). This is paradoxical, in view of their higher frequency of depressive symptoms; perhaps the respondents consciously minimized their problems when they were directly asked about the presence of a mental illness, but were less likely to do so when indirectly asked about their depressive symptoms, by means of a group of questions whose role in assessing depression is not immediately obvious. The participants may also have a relatively low awareness of their own health.
The regression analyses revealed associations between certain indicators of mental health and especially type D personality, stress during leisure time, and job satisfaction. Type D personality and stress during leisure time were positively associated, and high job satisfaction negatively associated, with the presence of mental health problems. Occupational stress, as measured by the ERI-Q, was found to be associated with depressivity, but not with mental illness or with the consumption of psychoactive substances. Moreover, these associations were less marked than the associations with stress during leisure time; this indicates that, for PCPs, inadequate mental hygiene and a lack of stress reduction during leisure time may be major contributory causes of mental health problems. The strong association of the type D personality pattern with impaired mental health indicates that PCPs’ own personalities may play just as large a role in the development of mental health problems as any factors relating to personal or working environment.
Strengths and weaknesses of this study
This study differs from other surveys of German PCPs in employing validated, standardized instruments of assessment. Another one of its strengths is the large amount of information that was acquired for analysis.
The relatively low response rate of 38.6% raises the possibility of selection bias. We were able to compare responders and non-responders only with respect to sex and found no difference in the male-to-female ratio, but other types of bias remain possible. While it is conceivable that PCPs who were under intense stress took a stronger interest in the topic of our study and were thus better motivated to respond, we think it is more likely that those under intense stress were actually less willing to take the time to fill out our extensive questionnaire. Our measures of the prevalence of certain mental health problems are thus likely to be under- rather than overestimates. The lack of a control group is a further limitation.
Our method of dealing with missing values by imputation was studied in sensitivity analyses. There were only small differences with respect to a few predictors when the models with and without imputation were compared.
The cross-sectional study design does not permit the drawing of any conclusions about causation from the demonstrated associations. However, personality traits, which are defined as stable aspects of individual character, would seem more likely to exert an effect on the participants’ mood and behavior than to be affected by them; for the particular case of the type D personality, the results of prospective studies do, in fact, support this contention (e12– e15). On the other hand, when we consider the demonstrated associations with subjective stress and with job satisfaction, the causal link could conceivably be in either direction. The results of other studies, some of which were carried out prospectively, support the hypothesis that high levels of stress lead to mental health problems in the long term, rather than the other way around (2, 6, 22, 23).
The prevention of mental health problems
These findings suggest that preventive measures should be developed and implemented for stress reduction, and for the modification of unfavorable personality traits (type D personality, overcommitment) and the behavioral patterns associated with them. Regular exchanges with professional colleagues in Balint groups might help PCPs raise their job satisfaction and strengthen their resistance to stress (24). Evidence suggests that cognitive behavioral training for physicians can improve their ability to cope with stress over the long term (25), and that the beneficial use of leisure time should be discussed as a part of cognitive behavioral training. Such extended methods can also be used to modify unfavorable modes of experience and behavior that are associated with the individual’s personality. Nonetheless, before any measures of these types could be introduced, the formulators of government health policy would have to reach an agreement with representatives of the medical profession and with the health insurance carriers regarding the appropriate legal framework and sources of funding.
Conclusions
The PCPs in Rhineland-Palatinate who participated in this study had more depressive symptoms than the general German population. They consumed psychoactive drugs and other psychoactive substances about as much as the PCPs who responded to another survey conducted across Europe (19). Stress during leisure time, type D personality, occupational stress, and low job satisfaction were identified as potential risk factors. These findings suggest that measures should be taken to reduce the experience of stress, promote mental hygiene, and modify unfavorable personality traits and the associated behavioral patterns. Initial publications have already appeared with preventive approaches for the improvement of mental health among physicians (24, 25).
Key Messages.
Mental health problems were common in this sample of primary care physicians (PCPs).
Every fourth PCP had depressive symptoms, and every sixth reported having taken psychoactive drugs or other psychoactive substances at least once in the past year.
Occupational stress and personality-related features (type D personality, overcommitment) were identified as potential risk factors for mental health problems.
Preventive measures seem to be urgently needed, including both the reduction of occupational stress and the modification of unfavorable personality-related modes of experience and behavior, as well as the improved use of leisure time.
Acknowledgments
Translated from the original German by Ethan Taub, M.D.
The authors thank the Rhineland-Palatinate Medical Association for its kind support with data acquisition.
Footnotes
Conflict of interest statement
The authors state that no conflict of interest exists.
References
- 1.Angerer P, Petru R, Nowak D, Weigl M. Arbeitsbedingungen und Depressionen bei Ärzten. Deutsche Medizinische Wochenschrift. 2008;133:26–29. doi: 10.1055/s-2008-1017467. [DOI] [PubMed] [Google Scholar]
- 2.Buddeberg-Fischer B, Klaghofer R, Stamm M, Siegrist J, Buddeberg C. Work stress and reduced health in young physicians: prospective evidence from Swiss residents. Int Arch Occup Environ Health. 2008;82:31–38. doi: 10.1007/s00420-008-0303-7. [DOI] [PubMed] [Google Scholar]
- 3.Sakata Y, Wada K, Tsutsumi A, et al. Effort-reward imbalance and depression in Japanese medical residents. J Occup Health. 2008;50:498–504. doi: 10.1539/joh.l8043. [DOI] [PubMed] [Google Scholar]
- 4.Siegrist J. Adverse health effects of high-effort/low-reward conditions. J Occup Health Psychol. 1996;1:27–41. doi: 10.1037//1076-8998.1.1.27. [DOI] [PubMed] [Google Scholar]
- 5.Siegrist J, Dragano N. Psychosocial stress and disease risks in occupational life. Results of international studies on the demand-control and the effort-reward imbalance models. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2008;51:305–312. doi: 10.1007/s00103-008-0461-5. [DOI] [PubMed] [Google Scholar]
- 6.Von dem Knesebeck O, Klein J, Grosse Frie K, Blum K, Siegrist J. Psychosocial stress among hospital doctors in surgical fields. Results of a nationwide survey in Germany. Dtsch Arztebl Int. 2010;107(14):248–253. doi: 10.3238/arztebl.2010.0248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Unrath M, Zeeb H, Letzel S, Claus M, Escobar Pinzón LC. Working conditions and health of general practitioners in Rhineland-Palatinate, Germany: first results of a state-wide survey. Gesundheitswesen. 2011 doi: 10.1055/s-0031-1280758. Epub ahead of print, doi:10.1055/s-0031-1280758. [DOI] [PubMed] [Google Scholar]
- 8.Li J, Yang W, Cho SI. Gender differences in job strain, effort-reward imbalance, and health functioning among Chinese physicians. Soc Sci Med. 2006;62:1066–1077. doi: 10.1016/j.socscimed.2005.07.011. [DOI] [PubMed] [Google Scholar]
- 9.Steinhaeuser J, Joos S, Szecsenyi J, Miksch A. A comparison of the workload of rural and urban primary care physicians in Germany: analysis of a questionnaire survey. BMC Family Practice. 2011;12 doi: 10.1186/1471-2296-12-112. http://www.biomedcentral.com/1471-2296/12/112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Siegrist J, Shackelton R, Link C, Marceau L, von dem Knesebeck O, McKinlay J. Work stress of primary care physicians in the US, UK and German health care systems M. Soc Sci Med. 2010;71:298–304. doi: 10.1016/j.socscimed.2010.03.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Stiller J, Busse C. Berufliche Belastungen von Berufsanfängern in der klinischen Praxis. In: Brähler E, Alfermann D, Stiller J, editors. Karriereentwicklung und berufliche Belastung im Arztberuf. Göttingen: Vandenhoeck & Ruprecht; 2008. pp. 165–178. [Google Scholar]
- 12.Grande G, Jordan J, Kummel M, et al. Evaluation of the German Type D Scale (DS14) and prevalence of the Type D personality pattern in cardiological and psychosomatic patients and healthy subjects. Psychother Psychosom Med Psychol. 2004;54:413–422. doi: 10.1055/s-2004-828376. [DOI] [PubMed] [Google Scholar]
- 13.Siegrist J, Wege N, Puhlhofer F, Wahrendorf M. A short generic measure of work stress in the era of globalization: effort-reward imbalance. Int Arch Occup Environ Health. 2009;82:1005–1013. doi: 10.1007/s00420-008-0384-3. [DOI] [PubMed] [Google Scholar]
- 14.Weyer G, Hodapp V, Neuhäuser S. Weiterentwicklung von Fragebogenskalen zur Erfassung der subjektiven Belastung und Unzufriedenheit im beruflichen Bereich (SBUS-B) Psychologische Beiträge. 1980;22:335–355. [Google Scholar]
- 15.Leppert K, Koch B, Brähler E, Strauß B. Die Resilienzskala (RS) - Überprüfung der Langform RS-25 und einer Kurzform RS-13. Klinische Diagnostik und Evaluation. 2008;1:226–243. [Google Scholar]
- 16.Kroenke K, Spitzer RL, Williams JB. The Patient Health Questionnaire-2: validity of a two-item depression screener. Med Care. 2003;41:1284–1292. doi: 10.1097/01.MLR.0000093487.78664.3C. [DOI] [PubMed] [Google Scholar]
- 17.Löwe B, Wahl I, Rose M, et al. A 4-item measure of depression and anxiety: Validation and standardization of the Patient Health Questionnaire-4 (PHQ-4) in the general population. J Affect Disorders. 2010;122:86–95. doi: 10.1016/j.jad.2009.06.019. [DOI] [PubMed] [Google Scholar]
- 18.Chambers R, Campbell I. Anxiety and depression in general practitioners: associations with type of practice, fundholding, gender and other personal characteristics. Family Practice. 1996;13:170–173. [PubMed] [Google Scholar]
- 19.Soler JK, Yaman H, Esteva M, et al. Burnout in European family doctors: the EGPRN study. Fam Pract. 2008;25:245–265. doi: 10.1093/fampra/cmn038. [DOI] [PubMed] [Google Scholar]
- 20.Robert-Koch-Institut. http://www.gbe-bund.de/gbe10/owards.prc_show_pdf?p_id=9965&p_sprache=d. Berlin: Robert-Koch-Institut 2006 (online) (cited 13 July, 2011) available from; Gesundheit in Deutschland. Gesundheitsberichterstattung des Bundes 2006. [Google Scholar]
- 21.Fichter MM, Narrow WE, Roper MT, et al. Prevalence of mental illness in Germany and the United States. Comparison of the Upper Bavarian Study and the Epidemiologic Catchment Area Program. J Nerv Ment Dis. 1996;184:598–606. doi: 10.1097/00005053-199610000-00003. [DOI] [PubMed] [Google Scholar]
- 22.Dragano N, He Y, Moebus S, Jockel KH, Erbel R, Siegrist J. Two models of job stress and depressive symptoms. Results from a population-based study. Soc Psychiatry Psychiatr Epidemiol. 2008;43:72–78. doi: 10.1007/s00127-007-0267-z. [DOI] [PubMed] [Google Scholar]
- 23.Siegrist J. Chronic psychosocial stress at work and risk of depression: evidence from prospective studies. Eur Arch Psychiatry Clin Neurosci. 2008;258(Suppl5):115–119. doi: 10.1007/s00406-008-5024-0. [DOI] [PubMed] [Google Scholar]
- 24.Kjeldmand D, Holmstrom I. Balint groups as a means to increase job satisfaction and prevent burnout among general practitioners. Ann Fam Med. 2008;6:138–145. doi: 10.1370/afm.813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gardiner M, Lovell G, Williamson P. Physician you can heal yourself! Cognitive behavioural training reduces stress in GPs. Fam Pract. 2004;21:545–551. doi: 10.1093/fampra/cmh511. [DOI] [PubMed] [Google Scholar]
- e1.Firth-Cozens J, Greenhalgh J. Doctors’ perceptions of the links between stress and lowered clinical care. Soc Sci Med. 1997;44:1017–1022. doi: 10.1016/s0277-9536(96)00227-4. [DOI] [PubMed] [Google Scholar]
- e2.McCue JD. The effects of stress on physicians and their medical practice. N Engl J Med. 1982;306:458–463. doi: 10.1056/NEJM198202253060805. [DOI] [PubMed] [Google Scholar]
- e3.Burke RJ, Richardsen AM. Sources of satisfaction and stress among Canadian physicians. Psychol Rep. 1990;67:1335–1344. doi: 10.2466/pr0.1990.67.3f.1335. [DOI] [PubMed] [Google Scholar]
- e4.O’ Connor DB, O’ Connor RC, White BL, Bundred PE. Psychology. Vol. 5. Health & Medicine; 2000. Job strain and ambulatory blood pressure in British general practitioners: a preleminary study; pp. 241–250. [Google Scholar]
- e5.Goehring C, Bouvier Gallacchi M, Kunzi B, Bovier P. Psychosocial and professional characteristics of burnout in Swiss primary care practitioners: a cross-sectional survey. Swiss Med Wkly. 2005;135:101–108. doi: 10.4414/smw.2005.10841. [DOI] [PubMed] [Google Scholar]
- e6.Lee FJ, Stewart M, Brown JB. Stress, burnout, and strategies for reducing them: what’s the situation among Canadian family physicians? Can Fam Physician. 2008;54:234–235. [PMC free article] [PubMed] [Google Scholar]
- e7.Herschbach P. Psychische Belastung von Ärzten und Krankenpflegekräften. In: Koch U, editor. Psychologie in der Medizin. Weinheim: VCH; 1991. [Google Scholar]
- e8.Unrath M. Besteht ein Zusammenhang zwischen ärztlichem Stress und ärztlichem Kommunikationsverhalten? Saarbrücken: VDM Verlag Dr. Müller; 2008. Das Erkennen depressiver Beschwerden durch den Hausarzt. [Google Scholar]
- e9.Egan M. Resilience at the front lines: hospital social work with AIDS patients and burnout. Soc Work Health Care. 1993;18:109–125. doi: 10.1300/J010v18n02_07. [DOI] [PubMed] [Google Scholar]
- e10.Friborg O, Hjemdal O, Rosenvinge JH, Martinussen M, Aslaksen PM, Flaten MA. Resilience as a moderator of pain and stress. J Psychosom Res. 2006;61:213–219. doi: 10.1016/j.jpsychores.2005.12.007. [DOI] [PubMed] [Google Scholar]
- e11.Leppert K, Gunzelmann T, Schumacher J, Strauss B, Brahler E. Resilience as a protective personality characteristic in the elderly. Psychother Psychosom Med Psychol. 2005;55:365–369. doi: 10.1055/s-2005-866873. [DOI] [PubMed] [Google Scholar]
- e12.Denollet J, Holmes RV, Vrints CJ, Conraads VM. Unfavorable outcome of heart transplantation in recipients with type D personality. J Heart Lung Transplant. 2007;26:152–158. doi: 10.1016/j.healun.2006.11.600. [DOI] [PubMed] [Google Scholar]
- e13.Pedersen SS, Ong AT, Sonnenschein K, Serruys PW, Erdman RA, van Domburg RT. Type D personality and diabetes predict the onset of depressive symptoms in patients after percutaneous coronary intervention. Am Heart J. 2006;151(367):e1–e6. doi: 10.1016/j.ahj.2005.08.012. [DOI] [PubMed] [Google Scholar]
- e14.Schiffer AA, Pedersen SS, Broers H, Widdershoven JW, Denollet J. Type-D personality but not depression predicts severity of anxiety in heart failure patients at 1-year follow-up. J Affect Disord. 2008;106:73–81. doi: 10.1016/j.jad.2007.05.021. [DOI] [PubMed] [Google Scholar]
- e15.Schiffer AA, Smith OR, Pedersen SS, Widdershoven JW, Denollet J. Type D personality and cardiac mortality in patients with chronic heart failure. Int J Cardiol. 2009;142:230–235. doi: 10.1016/j.ijcard.2008.12.090. [DOI] [PubMed] [Google Scholar]
- e16.Wang L-J, Chen C-K, Hsu S-C, Lee S-Y, Wang C-S, Yeh W-Y. Active job, healthy job? Occupational stress and depression among hospital physicians in Taiwan. Ind Health. 2011;49:173–184. doi: 10.2486/indhealth.ms1209. [DOI] [PubMed] [Google Scholar]
- e17.BKK Bundesverband. http://www.bkk.de/fileadmin/user_upload/PDF/Arbeitgeber/gesundheitsreport/BKK_Gesundheitsreport_2010.pdf. Essen: Typografischer Betrieb Lehmann GmbH 2010 (online) (cited 09 August 2011) Available from; BKK Gesundheitsreport 2010. Gesundheit in einer älter werdenden Gesellschaft. [Google Scholar]
- e18.Schneider M, Bouvier Gallacchi M, Goehring C, Kunzi B, Bovier PA. Personal use of medical care and drugs among Swiss primary care physicians. Swiss Med Wkly. 2007;137:121–126. doi: 10.4414/smw.2007.11606. [DOI] [PubMed] [Google Scholar]
- e19.Bijl RV, de Graaf R, Hiripi E, et al. The prevalence of treated and untreated mental disorders in five countries. Health Aff (Millwood) 2003;22:122–133. doi: 10.1377/hlthaff.22.3.122. [DOI] [PubMed] [Google Scholar]
- e20.Buddeberg-Fischer B, Klaghofer R, Abel T, Buddeberg C. Junior physicians’ workplace experiences in clinical fields in German-speaking Switzerland. Swiss Med Wkly. 2005;135:19–26. doi: 10.4414/smw.2005.10830. [DOI] [PubMed] [Google Scholar]