Abstract
While parity (number of children) reportedly is related to tooth loss, the relationship between parity and dental caries has not been extensively investigated. We used path analysis to test a theoretical model that specified that parity influences dental caries levels through dental care, psycho- social factors, and dental health damaging behaviors in 2635 women selected from the NHANES III dataset. We found that while increased parity was not associated with a greater level of total caries (DFS), parity was related to untreated dental caries (DS). The mechanisms by which parity is related to caries, however, remain undefined. Further investigation is warranted to determine if disparities in dental caries among women are due to differences in parity and the likely changes that parallel these reproductive choices.
Keywords: parity, dental caries, health disparities, path analysis
Introduction
There is a widely held belief among women that childbearing is related to oral disease (Habashneh et al., 2005; Payscale.com, 2007; Yahoo, 2010). Indeed, several studies over the last decade have shown that parity (number of children) is related to tooth loss (Rundgren and Osterberg, 1987; Halling and Bengtsson, 1989; Christensen et al., 1998; Russell et al., 2008), but the reason for this relationship is unclear. Few studies have examined whether parity is related to dental caries (Walker et al., 1983; Scheutz et al., 2002), a prerequisite to tooth loss. The purpose of this study was to determine whether parity is related to dental caries, and to examine whether this relationship can be explained by the effect of parity on socio-behavioral variables related to dental caries.
Methods
Study Population and Sample Selection
We used data from the Third National Health and Nutrition Examination Survey (NHANES III, 1988-1994). Of 7073 Black and White non-Hispanic women aged 18-64 yrs, we included women who (1) had received a dental examination, (2) retained at least one tooth, (3) reported at least one pregnancy, and (4) were not missing parity or socio-economic status (SES—income, education, occupation) data. Of the 6501 White and Black women who received a dental examination, 95.2% (6186/6501) retained at least one tooth. Of these, 18.9% (1172/6501) reported no pregnancies, and 9.6% (593/6501) were missing data on SES or parity (number of live births). Since the aim of this analysis was to identify pathways by which parity affects dental caries, we excluded those with multiple missing explanatory variables (1786/4421), and our analysis therefore included 60.0% of the eligible women (2635/4421). The Institutional Review Boards of New York and Yale Universities approved this study.
Theoretical Model
Our theoretical model of the parity-caries relationship was adapted from that of Adler et al. (1993), who suggested that socio-economic status (SES) may affect health through three pathways: (1) health care, (2) psychosocial factors, and (3) health behaviors. We hypothesized that parity (which is closely related to SES) would influence dental caries through: (1) dental health care, (2) psychosocial factors, and (3) dental-health-damaging behaviors. (See online Appendix for theoretical model.)
Measurements
Tooth surfaces were scored as sound, decayed, missing, or filled according to the DMFS Index (USDHHS, 1998). Dental caries was expressed as the proportion of surfaces/total examined surfaces, and included: (1) cumulative caries experience (DFS), (2) the proportion of filled surfaces (FS), and (3) the proportion of decayed surfaces (DS).
All women were asked: “What is the total number of live births (live-born children) you have had?” SES included: (1) the poverty income ratio (PIR), (2) education (years of school), and (3) occupation [Duncan Socioeconomic Index (SEI), a measure of occupational prestige]. Dental care included dental insurance (covered by health insurance paying for dental care) and frequency of dental visits. We included two measures of psychosocial status: financial stress and social support. Women reporting one or more days during the previous month with no food/money for food were considered to have financial stress. Social support was measured with six questions exploring frequency of social contacts, attendance at church/meetings, and club memberships. Dental-health-damaging behaviors included smoking, which included (1) self-reported smoking, (2) number of cigarettes smoked/day, and (3) serum cotinine level, and cariogenic diet, which combined a monthly consumption of four groups of cariogenic foods [cakes/cookies, chocolate candy, sugared beverages (e.g., Kool-Aid®), and sugared sodas]. Age, marital status (yes/no), time since last live birth (yrs), and race were included in all models.
Statistical Analysis
We created summated standardized scales for SES, smoking, and age/time since last live birth, to maximize use of the available data and avoid collinearity for modeling. To create scales, we examined correlations between items, standardized the items, and examined Cronbach-α reliabilities. We then stratified by parity, and by SES, and conducted univariate and bivariate analyses using ANOVA or the Kruskal-Wallis test. Since we found that many respondents had missing values on multiple explanatory variables in the model (dental insurance, etc.), we used multiple imputation with PRELIS 2 (SSI, Chicago, IL, USA). We began with candidate regression models to predict non-missing endogenous variables with assorted other explanatory/auxiliary variables and used Monte Carlo analysis with multiple chains to simulate five datasets with which to impute missing values along with the covariance structure among them. For all other analyses, we used Stata/SE (Stata Corporation, College Station, TX, USA). We used Dunn-Sidak corrections for multiple comparison adjustment.
We used path analysis to explore complex relationships among variables. Because of skewed and non-normal distributions of multiple variables, and influential outliers and notable heteroskedasticity in the data, we performed robust path analyses using two algorithms: the first symptotically attenuated heteroskedasticity with a White sandwich variance estimator (White, 1980), and the second down-weighted the influence of the outliers. Path analysis for each robust regression algorithm included: (1) performing general-to-specific regressions for variables loading significantly on the outcome variable (Hendry and Richard, 1982), (2) trimming the full models of non-significant paths, and (3) creating path diagrams based on the final models. To compute total effects, we calculated zero-order relationships between the exogenous variables that loaded on each endogenous variable in the path diagram. We performed intermediate regressions for each of these variables, identified all indirect paths, and calculated the sums of each of these indirect effects as the products of direct paths. Finally, we computed the unexplained effects for each independent variable as the difference of zero order and total effects, and calculated an error term for each endogenous variable.
Since our participants represented only a small subpopulation compared with that anticipated by the sample design, we chose not to perform a weighted analysis. When comparing our sample with the US population of women giving birth over the years 1988-1992 in the National Vital Health Statistics birth records for the same years as the NHANES III (1988-1992), we indeed found the demographics of our sample to be dissimilar to that of the general US population of childbearing age (i.e., giving birth). Consequently, because our analysis was unweighted, our results cannot be generalized to the US population.
Results
Scale Construction
Education, PIR, and SEI were correlated at levels of 0.42 (education, PIR), 0.36 (PIR, SEI), and 0.49 (education, SEI). Smoking, number of cigarettes, and serum cotinine were correlated at levels of 0.67 (smoking, number of cigarettes), 0.70 (numbers of cigarettes, cotinine), and 0.64 (smoking, cotinine). Age and time since last live birth were correlated at 0.84. Cronbach-α reliabilities for the summary variables SES, smoking, and age/time were 0.69, 0.87, and 0.89, respectively.
Women with missing data were older (47 vs. 39 yrs, Mann-Whitney test, p ≤ 0.001), had higher parity (2.9 vs. 2.3 births, Mann-Whitney test, p ≤ 0.001), were less educated (11.9 vs. 13.1 yrs, p ≤ 0.001), had lower incomes (PIR 2.1 vs. 3.0, Mann-Whitney test, p ≤ 0.001), and were more likely to be Black (56.0% vs. 49.1%, χ2 = 26.14, df = 1, p ≤ 0.001) than those in our selected subsample.
Descriptive Analyses
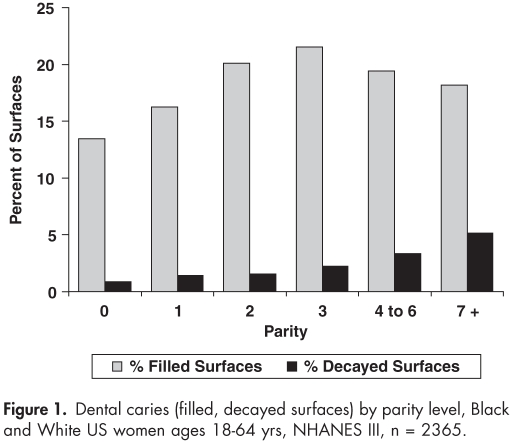
Parity was inversely related to SES (Table 1). Women with the highest parity levels (4-6, 7+ births) exhibited similar total amounts of filled + decayed surfaces (median of 17.9% and 18.5%), but had more untreated decay (21.7% vs. 6.1% of all affected surfaces) than women with lower parity (Fig. 1).
Table 1.
Demographic Characteristics of the Study Participants, NHANES III, by Socioeconomic Status (n = 2635)
| Socio-economic Status (tertile) |
||||
|---|---|---|---|---|
| Characteristic | Low (n = 878) | Middle (n = 878) | High (n = 879) | |
| Age (yrs) | Mean (SD) | 36.8 (13.0) | 38.7 (12.7) | 41.2 (11.3) |
| Race | Black | 61.3% | 38.8% | 26.5% |
| Income (PIR) | Mean (SD) | 1.5 (0.8) | 3.0 (1.0) | 4.6 (1.8) |
| Education (yrs) | ≤ 11 | 36.3% | 6.5% | 0.9% |
| = 12 | 53.8% | 51.0% | 19.1% | |
| 13+ | 9.9% | 42.4% | 80.0% | |
| Occupational prestige (SEI) | Mean (SD) | 23.6 (6.4) | 31.4 (9.1) | 58.0 (21.1) |
| Parity | 0 | 14.7% | 24.6% | 27.9 % |
| 1 | 17.1% | 19.3% | 18.8% | |
| 2 | 27.1% | 27.9% | 30.8% | |
| 3 | 19.8% | 15.8% | 12.5% | |
| 4-6 | 18.5% | 11.3% | 9.7% | |
| 7+ | 2.9% | 0.9% | 0.3% | |
| Mean (SD) | 2.4 (1.9) | 1.8 (1.6) | 1.6 (1.4) | |
| Time since last birth | Mean yrs (SD) | 11.7 (10.6) | 13.6 (10.9) | 14.1 (10.3) |
| Dental insurance | 53.4% | 67.2% | 68.5% | |
| Dental visit frequency | Reporting ≥ once/yr | 37.6% | 60.8% | 77.6% |
| Marital status | Married | 49.1% | 61.9% | 73.6% |
| Social support | Median contacts/wk | 50.7 | 52.0 | 46.3 |
| Financial stress | Reporting ≥ 1 days with no food/money for food | 7.3% | 1.8% | 0.5% |
| Cariogenic food frequency | Mean (SD) servings/mo. | 64.4 (55.7) | 50.1 (46.75) | 41.8 (33.3) |
All demographic factors differed between the socio-economic tertiles, p ≤ 0.001, except for social support (p = 0.60).
Figure 1.
Dental caries (filled, decayed surfaces) by parity level, Black and White US women ages 18-64 yrs, NHANES III, n = 2365.
Robust Regression Modeling
Race, SES, dental insurance, dental care frequency, and age/time since last live birth were significant predictors of (a) the proportion of filled surfaces, and (b) the proportion of decayed surfaces (Table 2). Parity was an important predictor of decayed, but not filled, surfaces, and marital status was an important predictor of filled, but not decayed, surfaces.
Table 2.
Results of Robust Regression for Dependent Variables: Filled Surfaces (%FS) and Decayed Surfaces (%DS), Women Ages 18-64 yrs, NHANES III (n = 2635)
| Regression Algorithm Results (management of heteroskedasticity) (regress, robust beta) |
|||
|---|---|---|---|
| Robust Beta | Robust SE for Beta | p | |
| Filled Surfaces | |||
| Socio-economic status | 0.121 | 0.441 | ≤ 0.001 |
| Race | −0.191 | 0.576 | ≤ 0.001 |
| Dental insurance | −0.030 | 0.591 | = 0.045 |
| Dental care frequency | −0.181 | 0.622 | ≤ 0.000 |
| Marital status | −0.043 | 0.559 | = 0.007 |
| Age/time | 0.370 | 0.323 | ≤ 0.001 |
| R2 = 0.32, F (6, 2628) = 192.36, p ≤ 0.001 | |||
| Decayed Surfaces | |||
| Socio-economic status | −0.132 | 0.006 | ≤ 0.001 |
| Race | 0.233 | 0.012 | ≤ 0.001 |
| Births | 0.081 | 0.004 | = 0.001 |
| Dental insurance | 0.060 | 0.011 | = 0.002 |
| Dental care frequency | 0.273 | 0.012 | ≤ 0.000 |
| Age/time | −0.016 | 0.005 | = 0.003 |
| R2 = 0.25, F (6, 2488) = 98.21, p ≤ 0.001 | |||
Robust Path Analysis
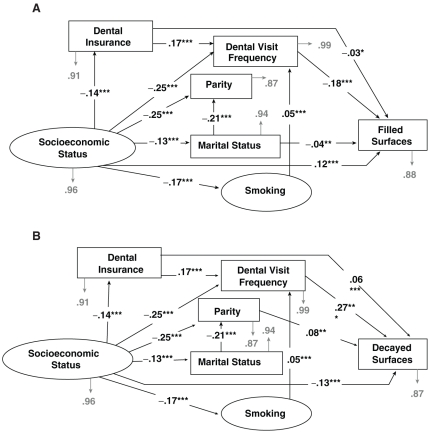
Robust path models show variables that significantly (via both algorithms) relate to (a) the % filled surfaces (model a) and (b) the % of decayed surfaces (model b) (Fig. 2). Standardized robust regression coefficients (betas) are on the paths, and error terms are in grey. With the exception of SES and social support, higher measurements of all variables indicate less favorable characteristics.
Figure 2.
Path diagrams, parity, and dental caries, Black and White US women ages 18-64 yrs, NHANES III. (A) Path model for filled surfaces. Model controlled for: race, age, and time since last live birth; *p ≤ 0.05, **p ≤ 0.01, ***p ≤ 0.001. (B) Path model for decayed surfaces. Model controlled for: race, age, and time since last live birth; **p ≤ 0.01, ***p ≤ 0.001.
Direct paths leading to both filled surfaces and decayed surfaces include those from SES to dental insurance and dental frequency. The directionality of these relationships was reversed between the two path models: Higher SES, having dental insurance, and visiting the dentist at least once a year were all related to more filled and fewer decayed surfaces. The relationship between dental visit frequency and decayed surfaces was especially strong (robust beta = 0.27, p ≤ 0.001).
Common paths for both models included those from SES to dental insurance and to dental frequency, and the path between these two variables. Women of higher SES were more likely to report going to the dentist at least once a year and were more likely to have dental insurance. The relationship between SES and dental visit frequency, however, was almost twice as strong as the relationship between SES and dental insurance (robust beta of -0.25 vs. -0.14, both p ≤ 0.001).
Additional consistent paths included those between SES and parity, SES and marital status, and marital status and parity. Higher-SES women were more likely to be married, and married women had higher parity. The SES-parity relationship was twice as strong as the SES-marital status relationship (robust beta of -0.25 vs. -0.13, both p ≤ 0.001). Cariogenic diet was unrelated to caries. A small indirect effect of SES through smoking and dental frequency was found for both filled and decayed surfaces (-0.002).
Major differences between the two path diagrams included: (1) a path between marital status and filled surfaces, indicating that married women were more likely to have more filled surfaces; and (2) a path between parity and decayed surfaces, demonstrating that higher-parity women were more likely to have more decayed surfaces.
Discussion
This is the first evidence in a large, heterogeneous sample of US women that parity is related to untreated dental caries, regardless of SES, race, and age. Despite the public perception that childbearing causes oral health deterioration, only two studies have specifically examined the relationship between parity and caries (Walker et al., 1983; Scheutz et al., 2002). While neither of these previous investigations identified a relationship between parity and caries, it is possible that, because these existing studies were performed in Africa, the results are not completely relevant to women with access to dental care.
The old wives’ tale “a tooth for every child” is generally attributed to the idea that pregnancy depletes maternal teeth of calcium, making them more caries-susceptible. In truth, the developing fetus actually draws needed calcium from the skeleton (Casamassimo, 2001), but other biologic mechanisms for an increase in susceptibility to caries during pregnancy have been proposed. Many of these physiologic mechanisms—including variations in saliva (Laine, 2002), oral flora alterations (Laine, 2002), and the immunosuppressed state of pregnancy (Luppi, 2003)—are those that possibly contribute to a documented mild, but persistent, sex/gender disparity in caries rates in the US (Brown et al., 2002; Dye et al., 2007; Lukacs, 2008).
Our finding that increased parity is associated with untreated decay, along with other evidence that relates parity to tooth loss (Rundgren and Osterberg, 1987; Halling and Bengtsson, 1989; Christensen et al., 1998; Russell et al., 2008), suggests that greater caries susceptibility associated with higher parity may not be solely biological, but also socio-behavioral.
It is possible that higher-parity women are more likely to have carious teeth extracted, while lower-parity women are likely to have teeth restored. Pregnancy and maternity alter patterns of dental treatment, and traditionally dentists have been advised that routine dental care for pregnant women should occur only during a limited window, the second trimester (Gaffield et al., 2001; Pistorius et al., 2003; AAP, 2004; ADA, 2006). Also, because of a lack of knowledge regarding the safety of treatment during pregnancy, fear of malpractice, or fear that a woman may go into labor, dentists may refuse outright to treat pregnant women (Strafford et al., 2008), may revise treatment plans when they discover a woman’s pregnancy, or may postpone care until after the woman has given birth (Livingston et al., 1998; Pistorius et al., 2003). Additionally, some pregnant women feel that going to the dentist is unsafe during pregnancy (Strafford et al., 2008) and may postpone treatment until after the birth, but at that point access to dental care may be restricted due to childcare and time or financial constraints (Redford, 1993).
Pregnant women in the US have high levels of dental disease (Silberman et al., 1980) and treatment needs (Gaffield et al., 2001; Lydon-Rochelle et al., 2004), but the proportion of pregnant women who report having a dental visit is low (22.4-43.2%) (Mangskau and Arrindell, 1996; Gaffield et al., 2001). In fact, even pregnant women with a dental problem are unlikely to see a dentist (Gaffield et al., 2001). Our finding that being married was related to filled surfaces supports the findings from a previous study that most pregnant women who reported a dental visit were non-minority, married, and educated beyond high school (Timothe et al., 2005). Unfortunately, since rates of dental access and utilization among pregnant women vary significantly by SES (Timothe et al., 2005), those pregnant women most at risk for dental disease are least likely to receive dental care when pregnant.
There are several limitations to this study. Because we did not use the sampling weights supplied by NHANES III, our results are not generalizable to the US population. Second, because of the complexity of our analysis, we chose to limit the study to only Black and White women. Mexican-American women are likely different from non-Hispanic women regarding issues related to parity, including culture and psychological factors related to parity, such as social support. In the future, studies should examine the parity-oral health relationship among different ethnic/cultural groups. Third, we were limited to those variables measured as a part of NHANES III. Finally, these data are cross-sectional, and although the directionality of the associations in the path models were created based on judgment of how relationships would work in reality, we should emphasize that one cannot assume directionality in the case of this study (i.e., models in Fig. 2 would be equivalent if the arrows were reversed).
Receiving dental care during pregnancy is safe (Michaelowicz, 2009), and guidelines have been published that advocate for dental care for pregnant women (Kumar and Samelson, 2006; Russell and Mayberry, 2008). Interventions aimed at pregnant women, and women with small children, could have a bearing on the dental health status of this significant proportion of the US population, not only because most women do have children, but also since maternal oral health is related to a child’s oral health. Efforts to correct disparities in parity-related dental caries may serve to correct this imbalance by addressing specific needs of women with children regarding issues including care of dental disease during pregnancy, access to dental care, and dental programs aimed at families.
Supplementary Material
Acknowledgments
This work was supported by Grant DE14257 from the National Institute of Dental and Craniofacial Research, NIH, Bethesda, MD, USA.
Footnotes
A supplemental appendix to this article is published electronically only at http://jdr.sagepub.com/supplemental.
References
- Adler NE, Boyce WT, Chesney MA, Folkman S, Syme SL. (1993). Socioeconomic inequalities in health. No easy solution. J Am Med Assoc 269:3140-3145 [PubMed] [Google Scholar]
- American Academy of Periodontology (2004). Statement regarding per- iodontal management of the pregnant patient. J Periodontol 75:495. [DOI] [PubMed] [Google Scholar]
- American Dental Association (2006). Women’s health issues. http://www.ada.org/sections/professionalResources/pdfs/healthcare_womens.pdf (URL accessed 05/11/2010).
- Brown LJ, Wall TP, Lazar V. (2002). Trends in caries among adults 18 to 45 years old. J Am Dent Assoc 133:827-834 [DOI] [PubMed] [Google Scholar]
- Casamassimo P. (2001). Maternal oral health. Dent Clin North Am 45:469-478 [PubMed] [Google Scholar]
- Christensen K, Gaist D, Jeune B, Vaupel JW. (1998). A tooth per child? Lancet 352:204. [DOI] [PubMed] [Google Scholar]
- Dye BA, Tan S, Smith V, Lewis BG, Barker LK, Thornton-Evans G, et al. (2007). Trends in oral health status, United States, 1988-1994 and 1999-2004. National Center for Health Statistics. Vital Health Stat 248:1-92 [PubMed] [Google Scholar]
- Dye JL. (2008). Fertility of American Women: 2006. Current Population Reports. Washington, DC: US Census Bureau, P20-558 [Google Scholar]
- Gaffield ML, Gilbert BJ, Malvitz DM, Romaguera R. (2001). Oral health during pregnancy: an analysis of information collected by the pregnancy risk assessment monitoring system. J Am Dent Assoc 132:1009-1016 [DOI] [PubMed] [Google Scholar]
- Habashneh R, Guthmiller JM, Levy S, Johnson GK, Squier C, Dawson DV, et al. (2005). Factors related to utilization of dental services during pregnancy. J Clin Periodontol 32:815-821 [DOI] [PubMed] [Google Scholar]
- Halling A, Bengtsson C. (1989). The number of children, use of oral contraceptives and menopausal status in relation to the number of remaining teeth and the periodontal bone height. A population study of women in Gothenburg, Sweden. Community Dent Health 6:39-45 [PubMed] [Google Scholar]
- Hendry DF, Richard JF. (1982). On the formulation of empirical models in dynamic econometrics. J Econometrics 20:3-33 [Google Scholar]
- Kumar J, Samelson R, editors (2006). New York State Department of Health. Oral health care during pregnancy and early childhood. Practice guidelines; available at http://www.health.state.ny.us/publications/0824.pdf (URL accessed 05/11/2010).
- Laine MA. (2002). Effect of pregnancy on periodontal and dental health. Acta Odontol Scand 60:257-264 [DOI] [PubMed] [Google Scholar]
- Livingston HM, Dellinger TM, Holder R. (1998). Considerations in the management of the pregnant patient. Spec Care Dentist 18:183-188 [DOI] [PubMed] [Google Scholar]
- Lukacs JR. (2008). Fertility and agriculture accentuate sex differences in dental caries rates. Curr Anthropol 49:901-914 [Google Scholar]
- Luppi P. (2003). How immune mechanisms are affected by pregnancy. Vaccine 21:3352-3357 [DOI] [PubMed] [Google Scholar]
- Lydon-Rochelle MT, Krakowiak P, Hujoel PP, Peter RM. (2004). Dental care use and self-reported dental problems in relation to pregnancy. Am J Public Health 4:765-771 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mangskau KA, Arrindell B. (1996). Pregnancy and oral health: utilization of the oral health care system by pregnant women in North Dakota. Northwest Dent 75:23-28 [PubMed] [Google Scholar]
- Michalowicz BS, DiAngelis AJ, Novak MJ, Buchanan W, Papapanou PN, Mitchell DA, et al. (2008). Examining the safety of dental treatment in pregnant women. J Am Dent Assoc 139:685-695 [DOI] [PubMed] [Google Scholar]
- Payscale.com: statement from Birkeland CP, January 24, 2007, available at http://blogs.payscale.com/job_mom/2007/01/post_partum_den.html (URL accessed 05/11/2010).
- Pistorius J, Kraft J, Willershausen B. (2003). Dental treatment concepts for pregnant patients—results of a survey. Eur J Med Res 8:241-246 [PubMed] [Google Scholar]
- Redford M. (1993). Beyond pregnancy gingivitis: bringing a new focus to women’s oral health. J Dent Educ 57:742-748 [PubMed] [Google Scholar]
- Rundgren A, Osterberg T. (1987). Dental health and parity in three 70-year-old cohorts. Community Dent Oral Epidemiol 15:134-136 [DOI] [PubMed] [Google Scholar]
- Russell SL, Ickovics J, Yaffee R. (2008). Exploring potential pathways between parity and tooth loss among American women. Am J Public Health 98:1263-1270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell SL, Mayberry LJ. (2008). Pregnancy and oral health: a review and recommendations to reduce gaps in practice and research. MCN Am J Matern Child Nurs 33:32-37 [DOI] [PubMed] [Google Scholar]
- Scheutz F, Baelum V, Matee MI, Mwangosi I. (2002). Motherhood and dental disease. Community Dent Health 19:67-72 [PubMed] [Google Scholar]
- Silberman SL, Cohen LA, Meydrech EF. (1980). Dental anxiety and needs in low-income pregnant women. Community Dent Oral Epidemiol 8:114-115 [DOI] [PubMed] [Google Scholar]
- Strafford KE, Shellhaas C, Hade EM. (2008). Provider and patient perceptions about dental care during pregnancy. J Matern Fetal Neonatal Med 21:63-71 [DOI] [PubMed] [Google Scholar]
- Timothe P, Eke PI, Presson SM, Malvitz DM. (2005). Dental care use among pregnant women in the United States reported in 1999 and 2002. Prev Chronic Dis 2:A10. [PMC free article] [PubMed] [Google Scholar]
- USDHHS: NHANES III Reference Manuals and Reports (1998). CD-ROM Series 11, Number 2A Hyattsville, MD: Centers for Disease Control and Prevention [Google Scholar]
- Walker AR, Dison E, Walker BF. (1983). Dental caries in South African rural black women who had large families and long lactations. J Trop Med Hyg 86:201-205 [PubMed] [Google Scholar]
- White H. (1980).A heteroskedasticity-consistent covariance matrix estimator and a direct test for heteroskedasticity. Econometrica 48:817-838 [Google Scholar]
- Yahoo (2010). http://uk.answers.yahoo.com/question/index?qid=20090325031148AAzi2YU Accessed June 15, 2010
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.