Abstract
Purpose
Adjuvant radiotherapy of breast cancer using a photon tangential field incurs a risk of late heart and lung toxicity. The use of free breathing (FB), expiration breath hold (EBH), and deep inspiration breath hold (DIBH) during tangential breast radiotherapy as a means of reducing irradiated lung and heart volume was evaluated.
Methods
In 10 women with left-sided breast cancer (mean age, 44 years) post-operative computed tomography (CT) scanning was done under different respiratory conditions using FB, EBH, and DIBH in 3 CT scans. For each scan, an optimized radiotherapy plan was designed with 6 MV photon tangential fields encompassing the clinical target volume after breast-conserving surgery.
Results
The results of dose-volume histograms were compared using three breathing pattern techniques for the irradiated volume and dose to the heart. A significant reduction dose to the irradiated heart volume for the DIBH breathing technique was compared to FB and EBH breathing techniques (p<0.05).
Conclusion
This study demonstrated that the irradiated heart volume can be significantly reduced in patients with left-sided breast cancer using the DIBH breathing technique for tangential radiotherapy.
Keywords: Breast neoplasms, Heart, Lung, Radiotherapy
INTRODUCTION
Breast cancer is a very common cancer in women. Breast cancer is a malignant tumor occurring in females, especially in developed countries. The incidence of breast cancer has been rapidly increasing and was the second most common cancer after thyroid cancer in Korea in 2006. The remarkable aspect of breast cancer in Korean females, however, is that the mean age of affected females is very young, 45-46 years of age, which is approximately 15 years younger than women in Western countries; and 25% of Korean females are <40 years of age compared to 5% of Caucasian women with breast cancer [1]. Currently, because screening examinations benefit patients with breast cancer in the early stages, surgery focuses on removal of the breast cancer. Breast-conserving surgery, which aims to retain the shape of breast, is preferable to a complete mastectomy. Patients undergo radiotherapy in an effort to prevent local recurrence of cancer after breast-conserving surgery [2].
The development of radiotherapy devices and techniques has resulted in radiotherapy as an important tool for curing breast cancer. The optimal radiotherapy plans must be designed to irradiate the cancer with a sufficient dose because of different locations and sizes of breast cancers. Geometric changes caused by organ motion during radiotherapy interfere with delivering a sufficient dose of radiation to the tumor and raise the risk of unnecessary radiation to normal organs. To reduce errors in radiotherapy, computed tomography (CT), magnetic resonance imaging (MRI), and positron emission tomography (PET) are utilized to determine the exact locations of tumors and adjacent organs and to establish treatment plans. Image fusion technology has also been developed; image-guided radiation therapy (IGRT), which considers the breathing patterns of the patient, is currently most commonly used [3]. For cases of breast cancer, breathing control is part of radiotherapy planning, but the tangential technique is generally used for patients with breast cancer. Patients with left-sided breast cancers, which lie on the left lung and heart, could lead to complications, such as pneumonitis or heart disease, after radiotherapy [4-7]. Hence, a clinician planning radiotherapy for a patient with left-sided breast-conserving surgery should consider breathing pattern movement to minimize unnecessary radiation doses to normal tissues including the left lung and the heart. In general, IGRT is not done, as it is difficult to position the patient for breathing pattern control due to the length of treatment [8-10].
This study evaluated patients who underwent left-sided breast-conserving surgery. The goal was to establish the optimal breathing technique to reduce the amount of normal tissue within the irradiated volume, which would lead to a decreased risk of complications. The dose of radiation was analyzed and the volumes of the heart and left lung were compared between free breathing (FB), voluntary expiration breath hold (EBH), and voluntary deep inspiration breath hold (DIBH).
METHODS
This study involved 10 female patients who were hospitalized with a mean age of 44 years (range, 32-62 years), and who had undergone radiotherapy after left-sided breast-conserving surgery in the Samsung Medical Center between March and August 2009. The stages of the disease were as follows: T1N0 (n=4); T2N0 (n=3); and T2N1 (n=3). All patients were able to breathe spontaneously. Before CT simulation, it was confirmed that all patients could suspend breathing for 30 seconds after a briefing on breathing techniques. A breast supporter was used to help patients remain in comfortable positions during CT simulation. Chest CT scans were performed without contrast media. The CT simulator bore size was 85 cm, which is larger than that of a diagnostic CT. A carbon-made table was used to maintain reproducibility of the patient's position on the radiotherapy table. Patients were supine on the breast angle board (MedTec, Orange City, USA) with the ipsilateral arm elevated. The scan with a CT simulator (CT High Advantage; General Electric Company, Waukesha, USA) was done from the middle of the neck to the upper abdomen, including the whole breasts, in the supine position. The slice thickness of the CT was 5 mm and the pitch was 1.35. Sixty images were acquired for each different breathing method. The order of testing breathing methods was FB, EBH, and DIBH, and the images transferred via DICOM described the contour of the surfaces of normal tissue of the heart and left lung with respect to each different breathing method using a treatment planning computer (Pinnacle, version 8.0h; Philips Medical System, Fitchburg, USA). A dose distribution plan was established using images of the breathing pattern differences for the patients in the clinical target volume (CTV) with a 1.5 cm beam margin.
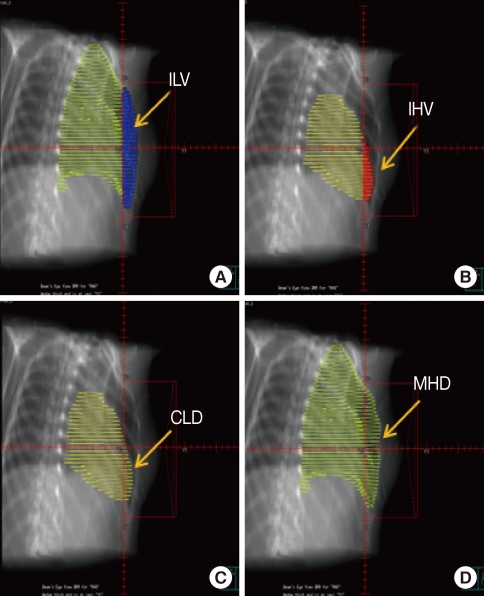
This study used 6 MV photon tangential fields in a linear accelerator (6EX; Varian, Palo Alto, USA) to choose the most correct energy, a multileaf collimator consisting of 120 leaves, including forty 5 mm and twenty 10 mm for radiation protection around the axilla, and an enhanced dynamic wedge (EDW) instead of a physical wedge. For patients in whom dose distribution was obtained by opposite parallel fields, a field-in-field technique was alternatively utilized for optimal plans of radiotherapy. The fields targeted for radiation exposure were determined to use a tangential technique with a half-beam, and the plans were determined to expose 50 Gy in total 2 Gy 25 fractions. All patients received 3 Gy of radiation 3-5 fractions to prevent the recurrence of cancer at the site where it was surgically removed by electron beam boost radiation therapy. The prescription dose was kept between 97% and 105% and the relationships between breathing techniques and dose volumes in the heart and left lung were assessed through a dose-volume histogram (Figure 1). The results were compared and assessed through analysis of doses and volumes of each organ. The comparison was done among total lung volume (TLV), total heart volume (THV), irradiated lung volume (ILV), and irradiated heart volume (IHV). Possible complications involving the heart and left lung by radiation were indirectly assessed as the distance from the back surface at the center of the Beam's Eye View (BEV) of the scheme for the left lung to the back surface of the anterior chest and maximum heart distance (MHD) from the back surface of the BEV of plans for the heart to the backward surface of the anterior heart. The central lung distance (CLD) is the parallel line distance from the centre of the exposed field to the back surface of the anterior chest of the backward surface (Figure 2).
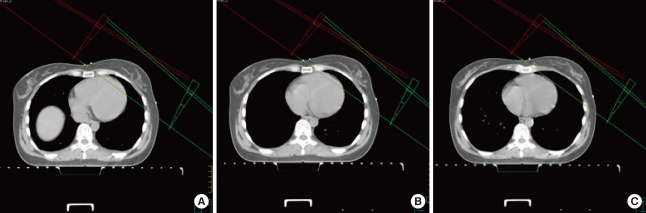
Figure 1.
Axial images of computed tomography. (A) Free breathing. (B) Expiration breath hold. (C) Deep inspiration breath hold.
Figure 2.
Digitally reconstructed radiograph images in chest. (A) Lung volume. (B) Heart volume. (C) Maximum heart distance. (D) Central lung distance.
ILV=irradiated lung volume; IHV=irradiated heart volume; CLD=central lung distance; MHD=maximum heart distance.
The doses for each method were analyzed through a histogram of the clinical target and normal tissue dose volumes. Moreover, the histogram was used to calculated the volume of the left lung, which was exposed to 20 Gy, and the minimum dose (D5), which reached >5% of the lung volume, when the dose distribution was within the clinical target dose and normal lung, and it estimated the heart volume (V18), which was exposed to 18 Gy, and the minimum dose (D5), which included 5% of the heart volume. The data were analyzed in SPSS for Windows version 17.0 (SPSS Inc., Chicago, USA). Dose analysis and volume comparisons of the heart and lung in different breathing techniques were assessed by the Kruskal-Walis test. All data were recorded with means and standard deviations, and p-values <0.05 were considered statistically significant.
RESULTS
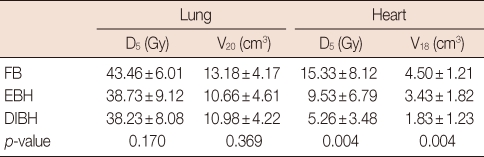
This study analyzed the dose (D5) and volume (V20) of the left lung, and the dose (D5) and volume (V18) of the heart using three different breathing methods. The dose (D5) of the left lung was 43.46±6.01 Gy with FB, 38.73±9.12 Gy with EBH, and 38.23±8.08 Gy with DIBH. The volume (V20) of the left lung was 13.18±4.17 cm3 with FB, 10.66±4.61 cm3 with EBH, and 10.98±4.22 cm3 with DIBH. The dose (D5) of the heart was 15.33±8.12 Gy with FB, 9.53±6.79 Gy with EBH, and 5.26±3.48 Gy with DIBH. The volume (V18) of the heart was 4.50±1.21 cm3 with FB, 3.43±1.82 cm3 with EBH, and 1.83±1.23 cm3 with DIBH (Table 1).
Table 1.
Dose and volume of lung and heart in FB, EBH, DIBH
FB=free breathing; EBH=expiration breath hold; DIBH=deep inspiration breath hold; D5=minimum dose which reached >5% of the lung volume; V20=volume of the left lung was exposed to 20 Gy; V18=heart volume was exposed to 18 Gy.
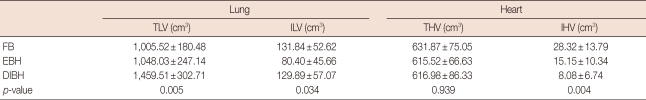
The total volume of the left lung was 1,005.52±180.48 cm3 with FB, 1,048.03±247.14 cm3 with EBH, and 1,459.51±302.71 cm3 with DIBH. The exposed actual volume of the left lung during radiotherapy was 131.84±52.62 cm3 with FB, 0.40±45.66 cm3 with EBH, and 129.89±57.07 cm3 with DIBH. The total volume of the heart was 631.87±75.05 cm3 with FB, 615.52±66.63 cm3 with EBH, and 616.98±86.33 cm3 with DIBH. The exposed actual volume of the heart was 28.32±13.79 cm3 with FB, 15.15±10.34 cm3 with EBH, and 8.08±6.74 cm3 with DIBH (Table 2).
Table 2.
Total volume and irradiated volume of lung and heart in FB, EBH, DIBH
FB=free breathing; EBH=expiration breath hold; DIBH=deep inspiration breath hold; TLV=total lung volume; ILV=irradiated lung volume; THV=total heart volume; IHV=irradiated heart volume.
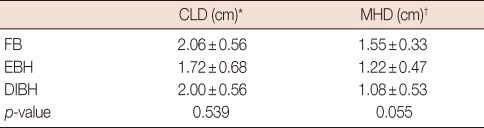
The dose (D5) of the left lung was significantly different p<0.170 than. For the volume (V20) was p<0.369. For the total lung volume during therapy was p<0.005, and the exposed actual volume of the left lung during therapy was p<0.034. The analysis of the heart dose (D5), volume (V18), and total heart volume of heart had statistical significance p<0.004 and p<0.939. The exposed actual volumes of the heart during therapy demonstrated statistical significance p<0.004. MHD is the maximum number of parallel lines from the backward surface to the back surface of the anterior heart with respect to the directions of the beam. The MHD of the left lung during radiotherapy was 1.55±0.33 cm with FB, 1.22±0.47 cm with EBH, and 1.08±0.53 cm with DIBH. MHD showed differences between EBH and DIBH because of the different heart beats and different heart positions. The MHD was diminished more with DIBH than with FB and EBH p<0.055. The CLD of the left lung during radiotherapy was 2.06±0.56 cm with FB, 1.72±0.68 cm with EBH, and 2.00±0.56 cm with DIBH. CLD decreased in EBH and FB and DIBH yielded similar results p<0.539 (Table 3). This is because the total area of the lung increases while breathing due to the optimal plan, but the area being treated is not increased.
Table 3.
Comparison of CLD and MHD in FB, EBH, DIBH
CLD=central lung distance; MHD=maximum heart distance; FB=free breathing; EBH=expiration breath hold; DIBH=deep inspiration breath hold.
*Parallel line distance from the centre of the exposed field to the back surface of the anterior chest of the backward surface; †Back surface of the beam's eye view of plans for the heart to the backward surface of the anterior heart.
The shortest distance was recorded with EBH; however, there were no problems in building therapy plans, with the exception of 1 patient because the distance in the plans did not exceed 3 cm.
DISCUSSION
In radiotherapy, which utilizes high-energy radiation, there has been an effort to minimize complications caused by radiation through various therapeutic techniques and development of therapeutic equipment. Recently, accurate therapy plans were built, as CT images are compromised with a therapy planning computer. Reconstruction technologies, like PET and MRI, help form a more precise and detailed scheme. Currently, breast cancer is the second most common cancer for women in Korea, and methods of diagnosis and treatment for breast cancer have drawn considerable attention. According to the Institute of Korean Breast Cancer in 2004, the age range of Korean patients initially threatened by breast cancer differed from American patients; in the USA most patients initially experience breast cancer after the menopause, but in Korea >60% of patients initially experience breast cancer when they are young (<50 years of age, and especially in their 40s) [11]. Breast cancer tends to recur within 5 years after treatment. According to the NSABP-06 report and the Milan study group, which monitored patients with histories of breast cancer for 20 years, breast cancer recurs even after 10 years [12]. For this recurrent disease, an appropriate therapy plan is required to prevent complications after therapy. As left-sided breast used to be the target for therapy, the doses to the heart and lung must be considered as an important factor in organizing therapy.
This study analyzed the doses to determine the most suitable breathing technique and therapy scheme through differences in doses and volumes of the heart and lung by different breathing methods during therapy for patients with breast cancer. This study was also able to confirm the differences in doses to each organ with respect to different breathing techniques [13]. The volume (V20) of the left lung with FB was increased for EBH and DIBH respectively. The dose (D5) of the heart with DIBH decreased for FB and EBH. The volume (V18) that can lead to heart disease with DIBH decreased the dose compared to FB. The results are in agreement with the earlier results in which DIBH diminished the dose from 4.50±1.21 cm3 to 1.83±1.23 cm3 compared to FB [6]. The irradiated heart volume and the dose (D5) to the heart decreased with DIBH. In the results for CLD and ILV of Chie et al. [14], it can be seen that as CLD increases, ILV also increases, but the results of this study suggests that when planning an optimal plan for the three breathing methods, ILV's and IHV's exposure was smaller in DIBH than in FB. The relationship between CLD and MHD according to the three types of breathing also showed that in the case of the optimal plan, the movement to the treatment center yielded more similar results in the DIBH to FB than CLD and MLD showed that the distance reduced vastly compared to between DIBH and FB. The distance reduction in CLD and MHD seems to have affected the reduction in exposure decrease of ILV and IHV. CLD changes by different breathing techniques are acceptable because CLD is kept under 3 cm during practical radiotherapy on a patient with breast cancer. For the MHD in parallel lines from the backward surface in the direction of the beam to the back surface of the anterior heart, the MHD was decreased with DIBH compared to FB. Differentiated breathing techniques in radiotherapy are applied to clinical practice for patients with lung and liver cancer. It is rare to perform radiotherapy on a patient with breast cancer; however, there is an opportunity to prevent complications to the heart and lung if image-guided radiotherapy is applied with the breathing techniques in a therapy scheme. Currently the interest in IGRT is limited to patients with tumors in the chest and abdominal organs. In patients with breast cancer, the treatment plan for the tangential technique is too generalized, and the use and studies for IGRT are limited to cases where the size interferes with the supine position, or of the comparison between supine and prone positions. If studies of the differences in breathing methods continue, IGRT that controls breathing in the tangential exposure method will be able to be devised [15,16].
Pederson et al. [13] was not able to obtain satisfactory outcomes because there was difficulty in educating elderly patients about breathing, even though image-guided radiotherapy was utilized. The current study recommends an effective way for a system that is not able to launch IGRT, and to select patients able to spontaneously control breathing and to develop therapy plans for these patients. Before the therapy plan, a confirmation X-ray must be taken every day to check aberrations of patient positions and to compare and match them with schemed digitally reconstructed radiograph images. Radiation to the heart would possibly be minimized as a patient with breast cancer breathes deeply for approximately 30 seconds for one beam at parallel opposite fields of radiotherapy because the current equipment mostly utilizes an enhanced dynamic wedge instead of a physical wedge. Therefore, as the movements of an organ of a patient with breast cancer by breathing during therapy are reduced by deep inspiration, it is thought that the absorbed dose to the lung and heart dose will be significantly less than with the current breathing method. Complications to normal tissues by radiation are minimized as the volumes and doses to the heart and left lung are decreased.
This study established an optimal radiotherapy plan to make use of radiation dose and volumes for the left lung and the heart according to different breathing techniques in radiotherapy for patients with breast cancer. The radiation dose and volumes for the left lung and heart were analyzed for FB, EBH, and DIBH in patients who underwent left-sided breast-conserving surgery and had undergone radiotherapy. Although normal tissue control probability and tumor control probability values from the Kutcher-Burman model were not gained, it appears that the exposure to the lung decreases in EBH and DIBH compared to FB, and the volume and exposure for the heart was significantly less in DIBH than in FB. Therefore, side effects and complications of radiation on normal tissue are minimized as the volumes and doses to the heart and left lung are decreased.
Footnotes
The authors declare that they have no competing interests.
References
- 1.Choi DH, Jin SY, Lee DW, Kim ES, Kim YH. A study on BRCA1/2 mutations, hormone status and HER-2 status in Korean women with early-onset breast cancer. J Korean Soc Ther Radiol Oncol. 2008;26:65–73. [Google Scholar]
- 2.Cho H, Kim C, Park S, Oh M, Lee J, Ahn K. Clinical outcome after breast conserving surgery and radiation therapy for early breast cancer. J Korean Soc Ther Radiol Oncol. 2008;26:204–212. [Google Scholar]
- 3.Mageras GS, Yorke E. Deep inspiration breath hold and respiratory gating strategies for reducing organ motion in radiation treatment. Semin Radiat Oncol. 2004;14:65–75. doi: 10.1053/j.semradonc.2003.10.009. [DOI] [PubMed] [Google Scholar]
- 4.Moon SH, Kim TJ, Eom KY, Kim JH, Kim SW, Kim JS, et al. Radiation-induced pulmonary toxicity following adjuvant radiotherapy for breast cancer. J Korean Soc Ther Radiol Oncol. 2007;25:109–117. [Google Scholar]
- 5.Korreman SS, Pedersen AN, Aarup LR, Nøttrup TJ, Specht L, Nyström H. Reduction of cardiac and pulmonary complication probabilities after breathing adapted radiotherapy for breast cancer. Int J Radiat Oncol Biol Phys. 2006;65:1375–1380. doi: 10.1016/j.ijrobp.2006.03.046. [DOI] [PubMed] [Google Scholar]
- 6.Stranzl H, Zurl B. Postoperative irradiation of left-sided breast cancer patients and cardiac toxicity. Does deep inspiration breath-hold (DIBH) technique protect the heart? Strahlenther Onkol. 2008;184:354–358. doi: 10.1007/s00066-008-1852-0. [DOI] [PubMed] [Google Scholar]
- 7.Kim HJ, Jang WI, Kim TJ, Kim JH, Kim SW, Moon SH, et al. Radiation-induced pulmonary toxicity and related risk factors in breast cancer. J Breast Cancer. 2009;12:67–72. [Google Scholar]
- 8.Moran JM, Ben-David MA, Marsh RB, Balter JM, Griffith KA, Hayman JA, et al. Accelerated partial breast irradiation: what is dosimetric effect of advanced technology approaches. Int J Radiat Oncol Biol Phys. 2009;75:294–301. doi: 10.1016/j.ijrobp.2009.03.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stranzl H, Zurl B, Langsenlehner T, Kapp KS. Wide tangential fields including the internal mammary lymph nodes in patients with left-sided breast cancer. Influence of respiratory-controlled radiotherapy (4D-CT) on cardiac exposure. Strahlenther Onkol. 2009;185:155–160. doi: 10.1007/s00066-009-1939-2. [DOI] [PubMed] [Google Scholar]
- 10.Lee R, Chung E, Suh H, Lee KJ, Lee J. Analysis of the movement of surgical clips implanted in tumor bed during normal breathing for breast cancer patients. J Korean Soc Ther Radiol Oncol. 2006;24:192–200. [Google Scholar]
- 11.The Korean Breast Cancer Society. Nationwide Korean breast cancer data of 2004 using breast cancer registration program. J Breast Cancer. 2006;9:151–161. [Google Scholar]
- 12.Kim SK, Shin SO, Kim MS. Radiotherapy treatment planning using computed tomography in breast cancer. Korean J Med Phys. 1992;3:59–65. [Google Scholar]
- 13.Pedersen AN, Korreman S, Nyström H, Specht L. Breathing adapted radiotherapy of breast cancer: reduction of cardiac and pulmonary doses using voluntary inspiration breath-hold. Radiother Oncol. 2004;72:53–60. doi: 10.1016/j.radonc.2004.03.012. [DOI] [PubMed] [Google Scholar]
- 14.Chie EK, Shin KH, Kim DY, Kim TH, Kang HS, Lee ES, et al. Radiation pneumonitis after adjuvant radiotherapy for breast cancer: a volumetric analysis using CT simulator. J Breast Cancer. 2009;12:73–78. [Google Scholar]
- 15.Albuquerque KV, Glaser S, Gao M. Initial set-up reproducibility for prone breast irradiation (PBI): comparative clinical data with supine breast irradiation (SBI) for women with different body mass indices (BMI) -- role for IGRT. Int J Radiat Oncol Biol Phys. 2010;78(3 Suppl):S235. [Google Scholar]
- 16.Topolnjak R, Sonke JJ, Nijkamp J, Rasch C, Minkema D, Remeijer P, et al. Breast patient setup error assessment: comparison of electronic portal image devices and cone-beam computed tomography matching results. Int J Radiat Oncol Biol Phys. 2010;78:1235–1243. doi: 10.1016/j.ijrobp.2009.12.021. [DOI] [PubMed] [Google Scholar]