Abstract
Analysis of two clonally related multiresistant Pseudomonas aeruginosa isolates led to the identification of a novel IMP-type metallo-β-lactamase. IMP-29 was significantly different from the other IMP variants (the closest variant being IMP-5 with 93% amino acid identity). The blaIMP-29 gene cassette was carried by a class 1 integron in strain 10.298, while in strain 10.266 it was located in a rearranged DNA region on a 30-kb conjugative plasmid. Biochemical analysis confirmed that IMP-29 efficiently hydrolyzed carbapenems.
TEXT
Pseudomonas aeruginosa is a major opportunistic pathogen responsible for mild to severe nosocomial infections. Over the past decade, the emergence and spread of strains resistant to multiple antibiotics, including carbapenems, have become a serious clinical concern in many countries (12, 28). Resistance to carbapenems is usually due to mutational alteration of the imipenem-specific porin OprD but may also result from production of horizontally acquired β-lactamase genes (22). Most of the carbapenem-hydrolyzing enzymes (i.e., carbapenemases) found in P. aeruginosa belong to the Ambler class B of β-lactamases (27). These enzymes have been grouped into different types such as IMP, VIM, SPM, GIM, AIM, DIM, and NDM according to their amino acid sequences (4, 10). Of particular clinical importance are the IMP- and VIM-type metallo-β-lactamases (MBLs), which efficiently inactivate most of the antipseudomonal β-lactams except monobactams (7, 27). So far, 28 IMP-type β-lactamases have been identified in various Gram-negative species (K. Bush and G. Jacoby, http://www.lahey.org/Studies/).
Our study was initiated by the isolation of P. aeruginosa 10.266 (serotype O:12) from the blood culture of a 74-year-old male patient admitted in March 2010 to the medical intensive care unit of the teaching hospital of Besançon, France, for unstable diabetes associated with signs of pulmonary infection. The patient initially received a course of piperacillin-tazobactam, ciprofloxacin, rovamycin, and metronidazole for 16 days. Despite this aggressive therapy, he developed an acute respiratory distress syndrome, which prompted physicians to switch to imipenem and linezolid. This treatment failed, and the patient died from a septic shock 10 days later. A second serotype O:12 isolate, named 10.298, was recovered in June 2010 from a rectal swab of a 48-year-old male patient hospitalized for an acute myeloid leukemia in the hematology unit of the same hospital. The patient, who had no signs of infection, was not receiving antibiotics. Both isolates were highly resistant to all of the antipseudomonal β-lactams tested (ticarcillin, piperacillin-tazobactam, ceftazidime, cefepime, imipenem, and meropenem) except aztreonam (Table 1). They were also resistant to aminoglycosides (amikacin, tobramycin, and gentamicin) and ciprofloxacin but were susceptible to colistin (MIC of 0.5 μg/ml). Pulsed-field gel electrophoresis (PFGE) experiments using total DNA digested with endonuclease DraI (11) revealed that 10.266 and 10.298 were closely related (differing by only one band) and belonged to the same clone endemic in the hospital (23). The epidemiological link between the two patients carrying these bacteria could not be established (data not shown). The production of an MBL in both isolates was suggested by positive double-disk synergy tests between imipenem and EDTA (10 μl, 100 mM). Then, PCR experiments were carried out on purified DNA with primers specific for known MBL genes (blaIMP, blaVIM, blaNDM, blaSPM, blaAIM, blaDIM, and blaGIM) (15, 18, 21, 26). A blaIMP gene was amplified in both isolates, and sequencing identified a novel IMP-type MBL that was termed IMP-29 accordingly (http://www.lahey.org/Studies/).
Table 1.
Susceptibilities to β-lactams of P. aeruginosa and E. coli strains harboring gene blaIMP-29
| β-Lactam | MIC (μg/ml) for strain |
||||||
|---|---|---|---|---|---|---|---|
|
P. aeruginosa |
E. coli |
||||||
| 10.266 | 10.298 | PU21(pIMP266) | PU21 | DH5α(pK-IMP29) | DH5α(pK-IMP266) | DH5α(pK18) | |
| Amoxicillin | >256 | >256 | >256 | >256 | 64 | 128 | 0.5 |
| Ticarcillin | >256 | >256 | 256 | 8 | 256 | >256 | 0.5 |
| Piperacillin | 256 | 256 | 8 | 2 | 1 | 2 | ≤0.06 |
| Cefotaxime | >256 | 256 | >256 | 8 | 4 | 16 | ≤0.06 |
| Ceftazidime | >256 | 128 | 256 | 1 | 16 | 64 | ≤0.06 |
| Cefepime | >256 | 64 | 256 | 1 | 0.5 | 4 | ≤0.06 |
| Imipenem | 128 | 64 | 8 | 1 | 0.5 | 1 | 0.12 |
| Meropenem | >256 | 128 | 64 | 0.5 | 0.25 | 4 | ≤0.06 |
| Doripenem | >256 | 64 | 64 | 0.25 | 0.25 | 4 | ≤0.06 |
| Ertapenem | >256 | 256 | 256 | 8 | 0.12 | 4 | ≤0.06 |
| Aztreonam | 8 | 4 | 4 | 2 | ≤0.06 | 0.12 | ≤0.06 |
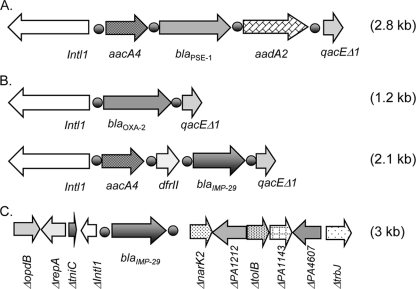
Since blaIMP genes are usually associated with class 1 integron sequences, PCR experiments were performed with primers annealing to the 5′ conserved sequence (CS) and 3′ CS of class 1 integrons (3). This yielded a single amplicon in 10.266 (2.8 kb) and three amplicons in 10.298 (2.8, 2.1, and 1.2 kb, respectively). Sequencing of the 2.8-kb PCR products revealed the presence of the gene (blaPSE-1) encoding narrow-spectrum penicillinase PSE-1 (also termed CARB-2), flanked by two gene cassettes, aacA4 and aadA2, encoding the aminoglycoside-modifying enzymes AAC(6)′-Ib and ANT(3)′, respectively (Fig. 1A). Production of the two latter enzymes is consistent with the high resistance of the isolates to aminoglycosides. The 1.2-kb fragment from 10.298 contained the blaOXA-2 gene encoding narrow-spectrum oxacillinase OXA-2 (Fig. 1B), while the 2-kb fragment appeared to carry the blaIMP-29 gene located downstream of the aacA4 and dfrII gene cassettes encoding the AAC(6′)-Ib and dihydrofolate reductase enzymes, respectively (Fig. 1B).
Fig 1.
Schematic map of class 1 integrons identified in clinical strains 10.266 and 10.298. The genes and their transcriptional orientations are indicated by arrows. The 59-base elements are indicated by a solid circle. (A) Structure of class 1 integron identified in both 10.266 and 10.298. (B) Structures of the two integrons identified in P. aeruginosa 10.298. (C) Structure of the cloned region containing the blaIMP-29 gene from the plasmid pIMP266.
Sequence alignments showed that IMP-29 was quite distant from other IMP-type MBLs (88.6% and 83.6% amino acid sequence identities with IMP-1 and IMP-8, respectively). Its closest relatives were IMP-5, IMP-22, and IMP-16 with 93, 92, and 91% sequence identity, respectively (5, 16, 19).
Interestingly, PCR experiments failed to detect a class 1 integron structure associated with blaIMP-29 in strain 10.266. To get further insight into the genetic environment of that gene, the plasmid content of isolate 10.266 was analyzed (13). A plasmid of ca. 30 kb was detected, which was named pIMP266. The potential of pIMP266 for conjugative transfer was assessed between 10.266 and a rifampin-resistant P. aeruginosa strain, PU21 (9). Transconjugant PU21(pIMP266) was selected on Mueller-Hinton agar plates supplemented with 100 μg/ml ticarcillin and 200 μg/ml rifampin. All the clones tested exhibited a high resistance to ticarcillin, cefotaxime, ceftazidime, and cefepime, associated with a reduced susceptibility to piperacillin and almost unchanged susceptibility to aztreonam compared with PU21 (Table 1). Plasmid pIMP266 conferred a higher resistance to meropenem (64 μg/ml) and doripenem (64 μg/ml) than to imipenem (8 μg/ml). Similar results have been reported in P. aeruginosa PAO1, PAO4141 (an AmpC-deficient mutant of PAO1), and Escherichia coli transformed with plasmids carrying blaIMP-12, blaIMP-10, and blaIMP-6, respectively (6, 8, 25). No coresistance marker was transferred by plasmid pIMP266.
To identify the genetic environment of the blaIMP-29 gene on plasmid pIMP266, a Sau3AI library of pIMP266 DNA was cloned into the BamHI-restricted plasmid pK18 (Kmr). Transformants of E. coli DH5α were selected on Mueller-Hinton agar plates containing 100 μg/ml ampicillin and 30 μg/ml kanamycin. In comparison to recipient strain DH5α, all the recombinant clones tested displayed a high level of resistance to β-lactams except aztreonam (Table 1). Sequence analysis of the 3-kb insert from one of these clones (plasmid pK-IMP266) revealed that the blaIMP-29 gene was flanked by several partial gene sequences belonging to loci distantly located on the P. aeruginosa genome such as narK (nitrite transport, PA3876) and PA1212 (major facilitator superfamily [MFS] pump) (Fig. 1C). This complex genetic environment likely reflects multiple rearrangements of the region surrounding blaIMP-29. Supporting this notion, the presence of a truncated tniC/R gene (encoding the resolvase of Tn401-like transposons), the integrase gene intl1, and a core site (59-base element) upstream of blaIMP-29 indicated that blaIMP-29 was initially associated with a mobile class 1 integron structure.
Since the MICs of carbapenems for isolate 10.266 were much higher than those for transconjugant PU21(pIMP266), the presence of an additional resistance mechanism was suspected (Table 1), such as the alteration of the OprD porin (17, 22, 24). Sequencing of the oprD gene revealed a premature stop codon in isolate 10.266 leading to a truncated peptide of 295 amino acid residues instead of 443 (wild-type OprD of P. aeruginosa PAO1). In 10.298, the oprD gene was also interrupted prematurely, resulting in a polypeptide lacking the last 28 C-terminal amino acids of OprD. However, the impact of the latter deletion on the porin function is likely to be modest since the MICs of carbapenems were relatively similar for 10.298 and PU21(pIMP266) (Table 1).
In order to better evaluate the impact of IMP-29 on the levels of resistance to β-lactams, the blaIMP-29 gene was expressed into E. coli. An 822-bp PCR fragment carrying blaIMP-29 was amplified by using specific primers cloIMP266F (5′-GTCGCCCGAAAACAAAGTTA-3′) and cloIMP266R (5′-AACTGTCCAAGGAGCGTAGC-3′). Once purified through a High Pure PCR product column (Roche Diagnostics, France), the amplicon was cloned into plasmid vector pCRScript CampR (Agilent Technologies) and subcloned into pK18 to yield recombinant plasmid pK-IMP29. As expected, transformant DH5α(pK-IMP29) exhibited an increased resistance to all the β-lactams tested except aztreonam (Table 1). However, the resistance levels conferred by pK-IMP29 were 2 to 32 times lower than those provided by pK-IMP266, suggesting a difference in blaIMP-29 expression between the two recombinant plasmids. E. coli DH5α(pK-IMP29) remained susceptible to imipenem, meropenem, doripenem, and ertapenem according to the current CLSI breakpoints (Table 1) (2).
To determine the catalytic properties of IMP-29, kinetic studies were carried out as previously described (20). Briefly, IMP-29 was purified from crude extracts of E. coli DH5α(pK-IMP29) by two-step anion-exchange chromatography in a Q-Sepharose column, first at pH 5.4 and then at pH 7.4. Since no enzymatic data have been reported for IMP-5, the closest relative to IMP-29, IMP-1 was used as the reference enzyme. Overall, the hydrolytic activities of IMP-29 were lower than those of IMP-1, in particular toward cefotaxime (35-fold lower), ceftazidime (72-fold lower), and cefepime (70-fold lower) (Table 2). IMP-29 hydrolyzed carbapenems at similar rates that were close to (meropenem) or lower than (imipenem, 20-fold; ertapenem, 17-fold) that of IMP-1. These assays confirmed that the enzyme has virtually no activity on aztreonam.
Table 2.
Kinetic parameters for β-lactamases IMP-29 and IMP-1a
| Substrate |
Km (μM) |
kcat (s−1) |
kcat/Km (μM−1 · s−1) |
|||
|---|---|---|---|---|---|---|
| IMP-29 | IMP-1 | IMP-29 | IMP-1 | IMP-29 | IMP-1 | |
| Benzylpenicillin | 130 | 520 | 140 | 320 | 1.1 | 0.62 |
| Piperacillin | 10 | 356 | 50 | 5 | 0.72 | |
| Cefotaxime | 300 | 4 | 3 | 1.3 | 0.01 | 0.35 |
| Ceftazidime | 800 | 44 | 2 | 8 | 0.0025 | 0.18 |
| Cefepime | 110 | 11 | 1 | 7 | 0.01 | 0.63 |
| Aztreonam | ND | >1,000 | NH | <0.01 | ND | ND |
| Imipenem | 50 | 39 | 3 | 46 | 0.06 | 1.17 |
| Meropenem | 90 | 10 | 6 | 5 | 0.07 | 0.50 |
| Ertapenem | 150 | 16 | 7 | 21 | 0.045 | 0.76 |
In conclusion, this work describes a novel transferable IMP variant acquired by an endemic O:12 clone. Both isolates were highly resistant to piperacillin because of production of penicillinase PSE-1 and to carbapenems as a result of alteration of porin OprD. While the characterization of IMP-29 was in progress, five other blaIMP-29-positive, clonally related P. aeruginosa isolates were identified from January to July 2011 in patients hospitalized in the hematology unit of the hospital in Besançon. All of these isolates possessed the pIMP266 plasmid. This indicates an ongoing nosocomial dissemination of the multidrug-resistant P. aeruginosa strain 10.266 with a potential risk of transfer of pIMP266 to other Gram-negative bacteria.
Nucleotide sequence accession numbers.
The nucleotide sequence data reported in this work have been deposited in the GenBank database under accession numbers JQ041634 and HQ438058.
ACKNOWLEDGMENT
The National Reference Center for Antibiotic Resistance was funded by the French ministry of health (InVS).
Footnotes
Published ahead of print 30 January 2012
REFERENCES
- 1. Borgianni L, et al. 2011. Genetic context and biochemical characterization of the IMP-18 metallo-beta-lactamase identified in a Pseudomonas aeruginosa isolate from the United States. Antimicrob. Agents Chemother. 55:140–145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. CLSI 2010. Performance standards for antimicrobial susceptibility testing; 20th information supplement (June 2010 update). M100-S20-U Clinical and Laboratory Standards Institute, Wayne, PA [Google Scholar]
- 3. Collis CM, Hall RM. 1992. Site-specific deletion and rearrangement of integron insert genes catalyzed by the integron DNA integrase. J. Bacteriol. 174:1574–1585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Cornaglia G, Giamarellou H, Rossolini GM. 2011. Metallo-beta-lactamases: a last frontier for beta-lactams? Lancet Infect. Dis. 11:381–393 [DOI] [PubMed] [Google Scholar]
- 5. Da Silva GJ, et al. 2002. Molecular characterization of bla(IMP-5), a new integron-borne metallo-beta-lactamase gene from an Acinetobacter baumannii nosocomial isolate in Portugal. FEMS Microbiol. Lett. 215:33–39 [DOI] [PubMed] [Google Scholar]
- 6. Docquier JD, et al. 2003. IMP-12, a new plasmid-encoded metallo-beta-lactamase from a Pseudomonas putida clinical isolate. Antimicrob. Agents Chemother. 47:1522–1528 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Gupta V. 2009. Metallo beta lactamases in Pseudomonas aeruginosa and Acinetobacter species. Expert Opin. Invest. Drugs 17:131–143 [DOI] [PubMed] [Google Scholar]
- 8. Iyobe S, et al. 2002. Detection of a variant metallo-beta-lactamase, IMP-10, from two unrelated strains of Pseudomonas aeruginosa and an Alcaligenes xylosoxidans strain. Antimicrob. Agents Chemother. 46:2014–2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Jacoby GA. 1974. Properties of R plasmids determining gentamicin resistance by acetylation in Pseudomonas aeruginosa. Antimicrob. Agents Chemother. 6:239–252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Jovcic B, et al. 2011. Emergence of NDM-1 metallo-β-lactamase in Pseudomonas aeruginosa clinical isolates from Serbia. Antimicrob. Agents Chemother. 55:3929–3931 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Kaufmann M. 1998. Pulsed-field gel electrophoresis. Methods Mol. Med. 15:33–50 [DOI] [PubMed] [Google Scholar]
- 12. Kerr KG, Snelling AM. 2009. Pseudomonas aeruginosa: a formidable and ever-present adversary. J. Hosp. Infect. 73:338–344 [DOI] [PubMed] [Google Scholar]
- 13. Kieser T. 1984. Factors affecting the isolation of CCC DNA from Streptomyces lividans and Escherichia coli. Plasmid 12:19–36 [DOI] [PubMed] [Google Scholar]
- 14. Laraki N, et al. 1999. Biochemical characterization of the Pseudomonas aeruginosa 101/1477 metallo-beta-lactamase IMP-1 produced by Escherichia coli. Antimicrob. Agents Chemother. 43:902–906 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Mendes R, et al. 2007. Rapid detection and identification of metallo-beta-lactamase-encoding genes by multiplex real-time PCR assay and melt curve analysis. J. Clin. Microbiol. 45:544–547 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Mendes RE, et al. 2004. Integron carrying a novel metallo-β-lactamase gene, blaIMP-16, and a fused form of aminoglycoside-resistant gene aac(6′)-30/aac(6′)-Ib′: report from the SENTRY Antimicrobial Surveillance Program. Antimicrob. Agents Chemother. 48:4693–4702 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Nikaido H. 1989. Outer membrane barrier as a mechanism of antimicrobial resistance. Antimicrob. Agents Chemother. 33:1831–1836 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Nordmann P, Poirel P, Carrer A, Toleman MA, Walsh T. 2011. How to detect NDM-1 producers. J. Clin. Microbiol. 49:718–721 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Pellegrini C, et al. 2009. Identification of bla(IMP-22) in Pseudomonas spp. in urban wastewater and nosocomial environments: biochemical characterization of a new IMP metallo-enzyme variant and its genetic location. J. Antimicrob. Chemother. 63:901–908 [DOI] [PubMed] [Google Scholar]
- 20. Poirel L, Le Thomas I, Naas T, Karim A, Nordmann N. 2000. Biochemical sequence analyses of GES-1, a novel class A extended-spectrum beta-lactamase, and the class 1 integron In52 from Klebsiella pneumoniae. Antimicrob. Agents Chemother. 44:622–632 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Poirel L, Rodriguez-Martinez JM, Al Naiemi N, Debets-Ossenkopp YJ, Nordmann P. 2010. Characterization of DIM-1, an integron-encoded metallo-beta-lactamase from a Pseudomonas stutzeri clinical isolate in the Netherlands. Antimicrob. Agents Chemother. 54:2420–2424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Rodriguez-Martinez JM, Poirel L, Nordmann P. 2009. Molecular epidemiology and mechanisms of carbapenem resistance in Pseudomonas aeruginosa. Antimicrob. Agents Chemother. 53:4783–4788 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Tenover FC, et al. 1995. Interpreting chromosomal DNA restriction patterns produced by pulsed-field gel electrophoresis: criteria for bacterial strain typing. J. Clin. Microbiol. 33:2233–2239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Trias J, Nikaido H. 1990. Outer membrane protein D2 catalyzes facilitated diffusion of carbapenems and penems through the outer membrane of Pseudomonas aeruginosa. Antimicrob. Agents Chemother. 34:52–57 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Yano H, et al. 2001. Plasmid-encoded metallo-beta-lactamase (IMP-6) conferring resistance to carbapenems, especially meropenem. Antimicrob. Agents Chemother. 45:1343–1348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Yong D, et al. 2007. A novel sub-group metallo-β-lactamase (MBL), AIM-1 emerges in Pseudomonas aeruginosa (PSA) from Australia, abstr C1-593, p 75 Abstr. 47th Intersci. Conf. Antimicrob. Agents Chemother [Google Scholar]
- 27. Zhao WH, Hi ZQ. 2010. Beta lactamases identified in clinical isolates of Pseudomonas aeruginosa. Crit. Rev. Microbiol. 36:245–258 [DOI] [PubMed] [Google Scholar]
- 28. Zilberberg MD, Chen J, Mody SH, Ramsey AM, Shorr AF. 2010. Imipenem resistance of Pseudomonas in pneumonia: a systematic literature review. BMC Pulm. Med. 10:45. [DOI] [PMC free article] [PubMed] [Google Scholar]