Abstract
Community-acquired pneumonia (CAP) continues to be a major health challenge in the United States and globally. Factors such as overprescribing of antibiotics and noncompliance with dosing regimens have added to the growing antibacterial resistance problem. In addition, several agents available for the treatment of CAP have been associated with serious side effects. Cethromycin is a new ketolide antibiotic that may provide prescribing physicians with an additional agent to supplement a continually limited armamentarium. Two global phase III noninferiority studies (CL05-001 and CL06-001) to evaluate cethromycin safety and efficacy were designed and conducted in patients with mild to moderate CAP. Study CL05-001 demonstrated an 83.1% clinical cure rate in the cethromycin group compared with 81.1% in the clarithromycin group (95% confidence interval [CI], −4.8%, +8.9%) in the intent to treat (ITT) population and a 94.0% cethromycin clinical cure rate compared with a 93.8% clarithromycin cure rate (95% CI, −4.5%, +5.1%) in the per protocol clinical (PPc) population. Study CL06-001 achieved an 82.9% cethromycin clinical cure rate in the ITT population compared with an 88.5% clarithromycin cure rate (95% CI, −11.9%, +0.6%), whereas the clinical cure rate in the PPc population was 91.5% in cethromycin group compared with 95.9% in clarithromycin group (95% CI, −9.1%, +0.3%). Both studies met the primary endpoints for clinical cure rate based on predefined, sliding-scale noninferiority design. Therefore, in comparison with clarithromycin, these two noninferiority studies demonstrated the efficacy and safety of cethromycin, with encouraging findings of efficacy in subjects with Streptococcus pneumoniae bacteremia. No clinically significant adverse events were observed during the studies. Cethromycin may be a potential oral therapy for the outpatient treatment of CAP.
INTRODUCTION
Community-acquired pneumonia (CAP) is the 8th leading cause of death in the United States and causes significant morbidity and mortality on a global scale (29, 37). Emerging bacterial resistance to the current armamentarium of anti-CAP agents, especially the emergence of macrolide-resistant Streptococcus pneumoniae, makes the choice of treatment agents challenging (9, 10, 15, 18, 24, 27). Bacterial resistance is an ever-evolving problem, and new agents under development today may play an even greater role in the future treatment of CAP. Marketed agents are well on their way to either losing efficacy in the eradication of CAP-causative pathogens (11) or joining the ever-expanding group of antibacterial agents with serious safety issues, limiting their effectiveness (19). In early 2008, an FDA advisory committee agreed to the necessity of antibiotic treatment for CAP and, along with the Infectious Diseases Society of America (IDSA), appeared to encourage the pharmaceutical industry to continue to develop new agents for the treatment of this condition (32).
Cethromycin, a novel ketolide agent, appears to address these issues by offering adequate pathogen coverage for the treatment of mild to moderate CAP, while providing a safety profile which appears to be void of the more serious adverse events associated with other ketolide or quinolone agents. There is speculation that the presence of the pyridine moiety and inhibition of nicotinic acetylcholine receptors by telithromycin may account for the incidences of hepatic toxicity, visual disturbances, and exacerbations of myasthenia gravis (2). It is noteworthy that there is no pyridine moiety in cethromycin. Cethromycin is a once-daily oral antibiotic targeting CAP caused by Gram-positive bacteria, specifically S. pneumoniae, Staphylococcus aureus, Haemophilus influenzae, and Moraxella catarrhalis (3, 36). In vitro, cethromycin has marked activity against these pathogens with the ability to overcome both efflux and methylation mechanisms of resistance in S. pneumoniae (17, 22).
The antibacterial activity of cethromycin is mediated through dual mechanisms of action: binding to the bacterial target, the 23S rRNA of the 50S subunit of the ribosome to prevent the translation of bacterial messenger RNAs into new proteins and interacting with partially assembled 50S subunit precursors to inhibit the complete formation of bacterial ribosomes (13). Cethromycin is able to overcome methylation-mediated resistance via a second point of contact with the ribosome (5). In addition, the enhanced binding of cethromycin is helpful in overcoming bacterial resistance mediated via efflux mechanisms, resulting in increases in antibacterial activity compared to both macrolide agents and the marketed ketolide agent, telithromycin (4, 31). Cethromycin retains activity against clinical isolates of telithromycin-resistant S. pneumoniae, a phenomenon believed to be the result of the enhanced binding kinetics (7).
Fluoroquinolones, such as levofloxacin and moxifloxacin, also provide adequate coverage against both susceptible and macrolide resistant CAP-causative pathogens (38). Unfortunately, the antibacterial coverage of these agents extends beyond common CAP-causative pathogens, resulting in the eradication of other bacterial species present in nontarget sites such as the gut. The destruction of these enteric Gram-negative bacteria allows for an overgrowth of other damaging bacterial species, such as Clostridium difficile, resulting in serious (and potentially fatal) side effects such as pseudomembranous colitis (26, 30). The reduced activity of cethromycin against enteric Gram-negative bacteria (14, 28) should limit the collateral damage often seen with quinolone treatment yet preserve the favorable activity against susceptible and resistant CAP-causative pathogens.
The aim of the two global studies was to demonstrate the efficacy and safety of cethromycin for the treatment of CAP, with the specific goal of collecting as much bacteriological efficacy information as possible.
MATERIALS AND METHODS
Two phase III, prospective, double-blinded, randomized, parallel-group, multicenter, multinational studies in patients with CAP were conducted in accordance with the International Conference on Harmonization good clinical practice guidelines. Study CL05-001 was conducted from January 2006 to October 2007 at 113 sites in the United States, Canada, and South Africa. Study CL06-001 was conducted from July 2006 to May 2007 at 90 sites in South America, Europe, and Israel. Target enrollment for each study was 500 subjects.
Study population.
Ambulatory male or female patients of ≥18 years with evidence of presumed bacterial pneumonia were eligible for enrollment. All inclusion and exclusion criteria are summarized in Table 1. Written informed consent was obtained from all patients prior to study-specific assessments and enrollment. The study was evaluated and approved by national, local, and institutional regulatory bodies and ethics committees as dictated by law.
Table 1.
Inclusion and exclusion criteria
| Inclusion criteria | Exclusion criteria |
|---|---|
| Written, voluntary informed consent was obtained from the subject (or legal representative) prior to initiation of any study related procedures | Hospitalized within the previous 4 weeks or was in residence at a chronic care facility |
| Evidence of any of the following: active tuberculosis, empyema, lung abscess, pulmonary embolism, pulmonary edema, cystic fibrosis, tumor (primary or metastatic) involving the lung, bronchial obstruction, a history of postobstructive pneumonia, known significant renal or hepatic impairment or disease, or severe immunosuppression (e.g., uncontrolled HIV infection with CD4+ <200/mm3) | |
| Male or female patients ≥18 years | |
| Investigator-assessed positive chest X ray with evidence of a new pulmonary infiltrate(s) (overread by a radiologist postenrollment) | |
| Females of childbearing potential who were pregnant or lactating | |
| Mucopurulent or purulent sputum sample | Refusal to use birth control during study participation (males and females) |
| At least two of the following signs and symptoms: | Concomitant infections which necessitated the use of additional antimicrobial agents |
| Cough | History of hypersensitivity or allergic reactions to macrolide, ketolide, quinolone, azalide, or streptogramin antimicrobials |
| Fever (oral temp >38.0°C or >100.4°F or equivalent tympanic or rectal temp) | |
| Treatment with an investigational drug within 4 weeks prior to enrollment | |
| Development of, or increase in, dyspnea or tachypnea (elevated respiratory rate ≥20/min) | Patients requiring concomitant administration of any of the following drugs were excluded due to the potential for drug interactions: theophylline or theophylline analogues (unless monitored), carbamazepine, dexamethasone, phenobarbital, phenytoin, St. John's wort, lamotrigine, troglitazone, warfarin, digitalis glycoside, barbiturates, midazolam, triazolam, alprazolam, rifampin, rifabutin, astemizole, pimozide, statins, or any other medication thought to interfere with the absorption of the study drug or comparator |
| Auscultatory findings on pulmonary examination of rales and/or evidence of pulmonary consolidation (i.e., dullness on percussion, bronchial breath sounds [crackles, rhonchi, wheezes, or egophony]) | |
| Elevated total peripheral WBC >10,000/min3, >15% immature neutrophils (bands), regardless of total peripheral WBC, or leukopenia with WBC <4,500/mm3 | |
| Suspected or known CNS disorder with the potential to lower seizure thresholdsa | |
| Subject was a suitable candidate for oral antibiotic therapy and was able to swallow capsules intact. | Evidence of septic shock |
| Previous treatment with cethromycin | |
| Any other condition that the investigator suspected would interfere with study participation |
CNS, central nervous system.
Procedures.
After consent, baseline assessments were collected (visit 1). Assessments obtained during standard-of-care treatment for pneumonia prior to enrollment (e.g., chest X ray) could carry over to baseline assessments. Patients provided a sputum sample with satisfactory purulent areas for culture and Gram's stain. Medical/social history, demographic data, concomitant medications, and presence and severity of clinical signs/symptoms of pneumonia (cough, sputum production/appearance, tachypnea, dyspnea, rales/crackling, rhonchi/wheezing, egophony/dullness, rigors, pleuritic chest pain, fever, white blood count [WBC] and bands [if available]) were recorded. Laboratory samples were obtained for serum chemistries (including hepatic enzyme analysis), hematological assays (including serological detection of evidence of atypical infections), blood cultures, and urinalysis. Electrocardiograms were performed to ensure safe participation in the protocol and to obtain baseline QT intervals. In areas of high tuberculosis incidence, an acid-fast bacillus (AFB) smear was performed. Samples were analyzed by a central laboratory with the exception of an onsite urine pregnancy test for females. Physicians also calculated a modified Fine score.
After eligibility was determined, but before blinded study therapy was dispensed, patients were randomized by an interactive voice response system (IVRS). Each study implemented a 1:1 randomization algorithm with each treatment assigned to subjects across all sites. The IVRS assigned a numerically coded blister card to each subject containing either cethromycin 300 mg once a day (QD) and matched placebo doses, or clarithromycin 250 mg twice a day (BID) and matched placebo doses, to be taken for seven consecutive days. The study medications and placebos were overencapsulated and appeared identical regardless of the treatment group. The blister card also has a diary for the subject to document the date and time of subsequent doses.
Subjects were instructed to return to the investigative site for three additional visits: V2, within 4 to 6 days postinitiation of therapy (days 4 to 6); V3, 24 to 72 h after the last dose (days 8 to 11); and V4 (test of cure), 7 to 14 days after taking the last dose of study medication (days 14 to 22). At each visit, patients were assessed for response to blinded therapy, study drug compliance, progression/improvement/resolution of signs and symptoms of CAP, adverse events, and changes in medical history or concomitant medications. Samples for serum chemistries, hematological analysis, and urinalysis were also obtained. Subjects producing sputum had samples collected for culture. Blood cultures were obtained for subjects with bacteremia confirmed by visit 1 culture or if bacteremia was suspected at any time. Electrocardiograms were performed at every visit to assess for changes in the QT interval.
At the visit 4 test-of-cure evaluation, investigators assigned an assessment of clinical response by comparing the clinical findings and chest X-ray results at visit 4 to the findings at visit 1. Bacteriology was not considered a factor when clinical responses were evaluated. Response definitions are included in Table 2. Indeterminate assessments were imputed as clinical failures. Subjects were queried for adverse events or reports of relapse at a telephone follow-up on days 37 to 40 (30 to 33 days after taking the last dose of study medication).
Table 2.
Clinical response definitions
| Clinical response | Definition |
|---|---|
| Clinical cure (applicable for evaluation 4; days 14–22) | Improvement or return to preinfection state or lack of progression in all pulmonary infiltrates originally consistent with pneumonia on chest radiograph and resolution of all signs and symptoms of CAP originally present at time of enrollment |
| Clinical failure | The subject was considered to be a therapy failure under the following conditions: |
| (applicable for all evaluations) | Persistence or worsening in signs or symptoms of the acute process after 3 to 5 days of therapy or requirement of additional antibiotic for initial pneumonia due to lack of improvement |
| Development of new pulmonary infection or extrapulmonary infection requiring antimicrobial therapy other than, or in addition to, the study medication | |
| Progression of chest radiological abnormalities | |
| Death due to pneumonia | |
| Indeterminate (applicable for evaluation 4 or at premature discontinuation) | The evaluation was not possible (e.g., lost to follow-up, disallowed medication use, premature discontinuation due to an adverse event, intercurrent illness, or major protocol violation); the reason was to be recorded on the case report form |
The co-primary endpoints for the study were clinical cure in the per protocol (PP) and intent to treat (ITT) populations at visit 4. ITT subjects had a diagnosis of CAP as confirmed by a radiologist and took at least one dose of study medication. The PP population was a subset of the ITT population, with the added requirement of having no significant protocol violations. All assessments of clinical response were performed prior to unblinding.
A secondary analysis population, the per protocol bacteriologically evaluable (PPb) population, included all PP subjects with tangible evidence of a protocol-specified bacteriological infection (e.g., a cultured pathogen, positive serology for the atypicals, or a positive urine antigen test for Legionella pneumophila). Microbiological response was evaluated by determining the bacteriological eradication rates (defined as all patients with evidence of a pathogen who demonstrated eradication of that pathogen at test of cure, either by culture [sputum or blood] or by not producing sputum for culture).
The safety population included all subjects who had taken at least one dose of study medication and had at least one postbaseline assessment. The frequency, severity, and relatedness of individual treatment-emergent adverse events were collected through day 40. All adverse events were followed to resolution.
Statistical analyses.
All statistical tests were two-tailed with a significant level of 0.05. Two-sided confidence intervals (CIs) were used. The primary objective was to demonstrate the noninferiority of cethromycin to clarithromycin in the clinical cure rate at the test of cure. Noninferiority was to be demonstrated when the lower limit of the two-sided 95% CI for the difference in the clinical cure rate at the test-of-cure visit between treatment groups (cethromycin-clarithromycin) was greater than delta, and included zero, for both the PP and ITT analyses. Delta was determined by the highest clinical cure rate between the cethromycin treatment group and the clarithromycin treatment group using a sliding method, that is, a cure rate of ≥90%, −10% delta; a cure rate of ≥80% but <90%, −15% delta; a cure rate of ≥70% yet <80%, −20% delta. It should be noted that regardless of the criteria and method utilized for determining an acceptable delta, the cure rates and CIs remain the same. In the statistical plan for the protocols, there were no provisions for alternate analyses. Patients with missing values or indeterminate outcomes were imputed as failures. Demographic and other baseline variables were analyzed to evaluate the comparability of the two groups and to assess the effectiveness of randomization. Quantitative variables were analyzed by one-way analysis of variance (ANOVA), and categorical variables were assessed by Cochran-Mantel-Haenszel (CMH) with stratification. As a supportive analysis, these variables were also compared using Fisher's exact test. Treatment-emergent adverse events were summarized by treatment group and compared using CMH. There were no interim analyses.
RESULTS
Demographic analyses.
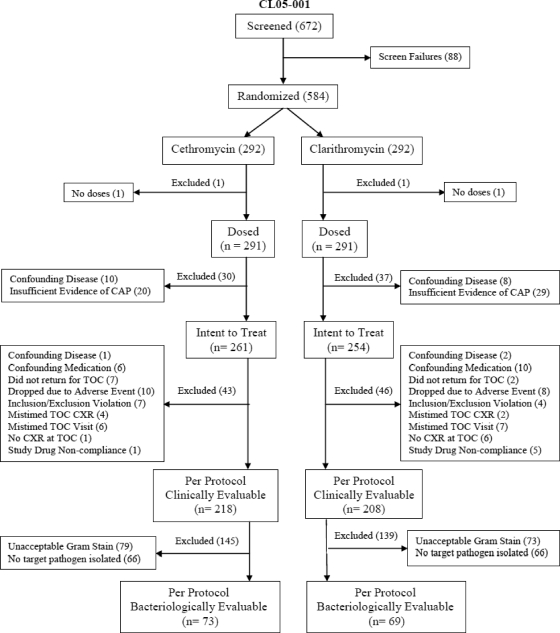
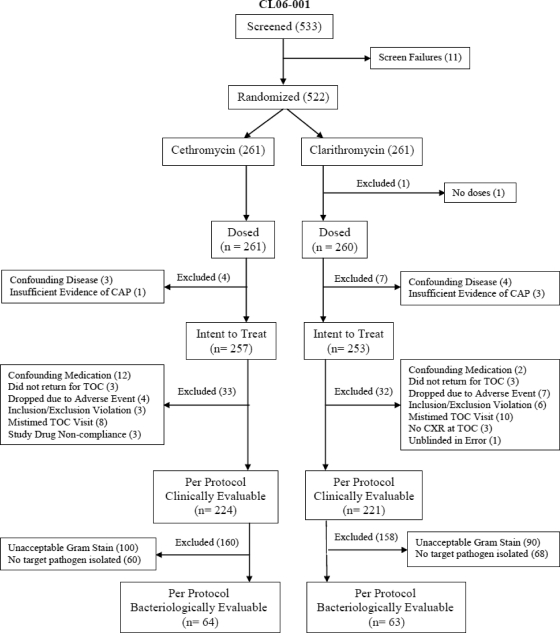
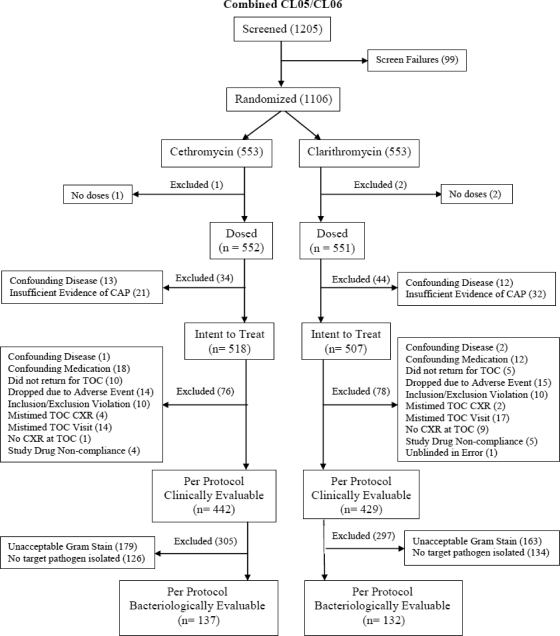
Figure 1 displays the subject distributions in the two individual and combined studies. In each study, there were no important treatment group differences for exclusion from any analysis population. Study CL05-001 had a greater number of subjects excluded from the ITT population due to insufficient radiological evidence of CAP, which was the result of a disagreement between the investigator and the radiologist, whose postrandomization overread of the chest X ray was considered the final confirmation of a CAP diagnosis. In the studies combined, 553 subjects were assigned at randomization to each treatment arm. Three patients were randomized but not dosed.
Fig 1.
Disposition of subjects by analysis population and efficacy (individual and combined studies).
Demographic data are summarized in Table 3. In the integrated analysis, most demographic variables were comparable between treatment groups and each study. The only notable inconsistency between the two studies was for race, where study CL06-001 had a greater percentage of subjects who were white compared to study CL05-001. This was not unexpected given geographical differences in site distribution, as study CL05-001 was conducted in the United States, Canada, and South Africa and study CL06-001 was conducted in Latin America, Europe, and Israel.
Table 3.
Demographic data by individual and combined studiesa
| Demographic characteristic | Study CL05-001 |
Study CL06-001 |
Combined studies CL05-001 and CL06-001 |
|||
|---|---|---|---|---|---|---|
| Cethromycin, 300 mg QD (n = 261) | Clarithromycin, 250 mg BID (n = 254) | Cethromycin, 300 mg QD (n = 257) | Clarithromycin, 250 mg BID (n = 253) | Cethromycin, 300 mg QD (n = 518) | Clarithromycin, 250 mg BID (n = 507) | |
| Age (yr) | ||||||
| Mean (±SD) | 48.8 (14.34) | 50.5 (16.29) | 47.8 (16.93) | 46.4 (17.42) | 48.3 (15.67) | 48.4 (16.97) |
| Minimum, maximum | 20.84 | 18.86 | 18.83 | 18.86 | 18.84 | 18.86 |
| Categoriesb | ||||||
| 18–24 | 6 (2.3%) | 19 (7.5%) | 27 (10.5%) | 35 (13.8%) | 33 (6.4%) | 54 (10.7%) |
| 25–44 | 103 (39.5%) | 77 (30.3%) | 84 (32.7%) | 76 (30.0%) | 187 (36.1%) | 153 (30.2%) |
| 45–64 | 111 (42.5%) | 105 (41.3%) | 98 (38.1%) | 92 (36.4%) | 209 (40.3%) | 197 (38.9%) |
| 65–74 | 27 (10.3%) | 34 (13.4%) | 35 (13.6%) | 42 (16.6%) | 62 (12.0%) | 76 (15.0%) |
| ≥65 | 41 (15.7%) | 53 (20.9%) | 48 (18.7%) | 50 (19.8%) | 89 (17.2%) | 103 (20.3%) |
| ≥75 | 14 (5.4%) | 19 (7.5%) | 13 (5.1%) | 8 (3.2%) | 27 (5.2%) | 27 (5.3%) |
| Gender | ||||||
| Male | 133 (51.0%) | 126 (49.6%) | 136 (52.9%) | 123 (48.6%) | 269 (51.9%) | 249 (49.1%) |
| Female | 128 (49.0%) | 128 (50.4%) | 121 (47.1%) | 130 (51.4%) | 249 (48.1%) | 258 (50.9%) |
| Race | ||||||
| White | 210 (80.5%) | 199 (78.3%) | 239 (93.0%) | 234 (92.5%) | 449 (86.7%) | 433 (85.4%) |
| Black | 31 (11.9%) | 27 (10.6%) | 1 (0.4%) | 1 (0.4%) | 32 (6.2%) | 28 (5.5%) |
| Asian | 12 (4.6%) | 17 (6.7%) | 1 (0.4%) | 0 | 13 (2.5%) | 17 (3.4%) |
| AI/AN | 0 | 1 (0.4%) | 0 | 0 | 0 | 1 (0.2%) |
| Other | 8 (3.1%) | 10 (3.9%) | 16 (6.2%) | 18 (7.1%) | 24 (4.6%) | 28 (5.5%) |
| Region | ||||||
| Non-U.S. | 147 (56.3%) | 136 (53.5%) | 257 (100%) | 253 (100%) | 404 (78.0%) | 389 (76.7%) |
| U.S. | 114 (43.7%) | 118 (46.5%) | NA | NA | 114 (22.0%) | 118 (23.3%) |
AI/AN, American Indian/Alaska native; NA, not applicable.
P value of 0.0380 for treatment group difference using a two-sided Fisher's exact test.
The most common pretreatment clinical signs and symptoms were moderate to severe cough, mucopurulent sputum, tachypnea, mild-to-moderate dyspnea, and rales/crackling (Table 4). No statistically significant differences were observed between the treatment groups for any of the pretreatment clinical signs and symptoms in the ITT or per protocol clinical (PPc) analysis populations. A statistically significant treatment group difference was observed in the PPb analysis population for cough, which appeared to be more severe in a higher percentage of subjects in the cethromycin group (30.7%) than in the clarithromycin group (18.2%). Results for the PPc and PPb populations were similar to those described for the ITT population. Inconsistencies between the two individual studies included the presence of dyspnea, rhonchi/wheezing, pleuritic chest pain, and fever, where study CL05-001 had greater percentages of subjects who had dyspnea, rhonchi/wheezing, and pleuritic chest pain at baseline and study CL06-001 had a greater percentage of subjects who had fever at baseline.
Table 4.
ITT populations: baseline characteristics and fine score distribution by individual and combined studies
| Sign/symptom | Study CL05-001 |
Study CL06-001 |
Combined studies CL05-001 and CL06-001 |
|||
|---|---|---|---|---|---|---|
| Cethromycin, 300 mg QD (n = 261) | Clarithromycin, 250 mg BID (n = 254) | Cethromycin, 300 mg QD (n = 257) | Clarithromycin, 250 mg BID (n = 253) | Cethromycin, 300 mg QD (n = 518) | Clarithromycin, 250 mg BID (n = 507) | |
| Cough | ||||||
| Absent | 0 | 1 (0.4%) | 1 (0.4%) | 1 (0.4%) | 1 (0.2%) | 2 (0.4%) |
| Mild | 28 (10.7%) | 31 (12.2%) | 28 (10.9%) | 25 (9.9%) | 56 (10.8%) | 56 (11.0%) |
| Moderate | 156 (59.8%) | 169 (66.5%) | 175 (68.1%) | 178 (70.4%) | 331 (63.9%) | 347 (68.4%) |
| Severe | 77 (29.5%) | 53 (20.9%) | 53 (20.6%) | 49 (19.4%) | 130 (25.1%) | 102 (20.1%) |
| Sputum production | ||||||
| Present | 261 (100%) | 253 (99.6%) | 257 (100%) | 253 (100%) | 518 (100%) | 506 (99.8%) |
| Mucopurulent | ||||||
| Present | 155 (59.4%) | 151 (59.4%) | 169 (65.8%) | 180 (71.1%) | 324 (62.5%) | 331 (65.3%) |
| Purulent | ||||||
| Present | 105 (40.2%) | 101 (39.8%) | 87 (33.9%) | 72 (28.5%) | 192 (37.1%) | 173 (34.1%) |
| Hemoptoic | ||||||
| Present | 18 (6.9%) | 17 (6.7%) | 6 (2.3%) | 13 (5.1%) | 24 (4.6%) | 30 (5.9%) |
| Tachypnea | ||||||
| Present | 161 (61.7%) | 147 (57.9%) | 171 (66.5%) | 164 (64.8%) | 332 (64.1%) | 311 (61.3%) |
| Dyspnea | ||||||
| Absent | 22 (8.4%) | 19 (7.5%) | 99 (38.5%) | 96 (37.9%) | 121 (23.4%) | 115 (22.7%) |
| Mild | 122 (46.7%) | 142 (55.9%) | 105 (40.9%) | 95 (37.5%) | 227 (43.8%) | 237 (46.7%) |
| Moderate | 113 (43.3%) | 90 (35.4%) | 52 (20.2%) | 59 (23.3%) | 165 (31.9%) | 149 (29.4%) |
| Severe | 4 (1.5%) | 3 (1.2%) | 1 (0.4%) | 3 (1.2%) | 5 (1.0%) | 6 (1.2%) |
| Rales/crackling | ||||||
| Present | 229 (87.7%) | 222 (87.4%) | 238 (92.6%) | 238 (94.1%) | 467 (90.2%) | 460 (90.7%) |
| Rhonchi/wheezing | ||||||
| Present | 207 (79.3%) | 187 (73.6%) | 97 (37.7%) | 97 (38.3%) | 304 (58.7%) | 284 (56.0%) |
| Egophony and/or dullness | ||||||
| Present | 141 (54.0%) | 151 (59.4%) | 110 (42.8%) | 105 (41.5%) | 251 (48.5%) | 256 (50.5%) |
| Rigors or shaking chills | ||||||
| Present | 168 (64.4%) | 136 (53.5%) | 113 (44.0%) | 114 (45.1%) | 281 (54.2%) | 250 (49.3%) |
| Pleuritic chest pain | ||||||
| Present | 189 (72.4%) | 180 (70.9%) | 105 (40.9%) | 92 (36.4%) | 294 (56.8%) | 272 (53.6%) |
| Fever (oral, >38.0°C or 100.4°F) | ||||||
| Present | 103 (39.5%) | 98 (38.6%) | 164 (63.8%) | 174 (68.8%) | 267 (51.5%) | 272 (53.6%) |
| Missing | 0 | 0 | 1 (0.4%) | 0 | 1 (0.2%) | 0 |
| Fine criteria | ||||||
| Risk class I | 136 (52.1%) | 110 (43.3%) | 126 (49.0%) | 132 (52.2%) | 262 (50.6%) | 242 (47.7%) |
| Risk class II | 101 (38.7%) | 117 (46.1%) | 99 (38.5%) | 91 (36.0%) | 200 (38.6%) | 208 (41.0%) |
| Risk class III | 16 (6.1%) | 24 (9.4%) | 23 (8.9%) | 24 (9.5%) | 39 (7.5%) | 48 (9.5%) |
| Risk class IV | 8 (3.1%) | 3 (1.2%) | 9 (3.5%) | 6 (2.4%) | 17 (3.3%) | 9 (1.8%) |
There were no statistically significant differences between the treatment groups in the distribution of subjects by baseline Fine criteria in any of the analysis populations (Table 4). The majority of the subjects in the ITT population in both treatment groups were determined to be at low risk of mortality (Fine criteria I, II, and III). The percentage of subjects who were determined to be at moderate risk of mortality (Fine criteria IV) was slightly higher in the cethromycin (3.3%) group compared with the clarithromycin (1.8%) group. No major inconsistencies in Fine criteria were observed between the two individual studies.
Efficacy.
The primary efficacy endpoint for both studies was the clinical cure rate (defined as the percentage of subjects who had a clinical response of “clinical cure”) at the test-of-cure visit. The clinical cure rates for the two individual studies, along with the integrated analysis, in both the ITT and PP populations are shown in Table 5. Study CL05-001 met the primary endpoint of noninferiority for clinical cure rate in both ITT and PPc populations. In the ITT population, the clinical cure rate was 83.1% in the cethromycin group compared with 81.1% in the clarithromycin group, with a 95% CI of −4.8% to +8.9%. The PPc population achieved the clinical cure rate of 94.0% in the cethromycin group compared with 93.8% in the clarithromycin group, with a 95% CI of −4.5% to +5.1%. Study CL06-001 also met predefined noninferiority with lower confidence bounds of −9.1% and −11.9% in the PPc and ITT populations, respectively. In the ITT population, the clinical cure rate was 82.9% in the cethromycin group compared with 88.5% in the clarithromycin group, (95% CI, −11.9%, +0.6%), whereas the clinical cure rate in the PPc population was 91.5% in the cethromycin group compared with 95.9% in the clarithromycin group (95% CI, −9.1%, +0.3%). Furthermore, the integrated analyses (CL05-001 and CL06-001 combined) also met the primary endpoint for clinical cure rate, demonstrating the noninferiority with a lower 95.0% confidence bound exceeding −10% (Table 5). The clinical cure rate in the ITT population of the integrated analysis was 83.0% in the cethromycin group compared with 84.8% in the clarithromycin group, and the PPc population displayed a 92.8% clinical cure rate in the cethromycin group compared with 94.9% in the clarithromycin group. Comparisons using Fisher's exact test supported noninferiority in both analysis populations. Analyses repeated using various imputation methods for missing data supported the results of the primary efficacy analysis. No major inconsistencies in the clinical cure rate were observed between the two individual studies, with the exception of the high clinical cure rate for clarithromycin in CL06-001. Signs and symptoms, geographical differences, and local practices were examined for possible impact on clinical outcomes. No correlations were observed.
Table 5.
Primary efficacy analyses: clinical cure rates in the ITT and PPc populations by individual and combined studies
| Study population | Study CL05-001 |
Study CL06-001 |
Integrated analysis: combined studies CL05-001 and CL06-001 |
|||
|---|---|---|---|---|---|---|
| Cethromycin, 300 mg QD | Clarithromycin, 250 mg BID | Cethromycin, 300 mg QD | Clarithromycin, 250 mg BID | Cethromycin, 300 mg QD | Clarithromycin, 250 mg BID | |
| ITTa | ||||||
| Clinical cure rates | 217/261 (83.1%) | 206/254 (81.1%) | 213/257 (82.9%) | 224/253 (88.5%) | 430/518 (83.0%) | 430/507 (84.8%) |
| CI for clinical cure ratesb | (78.0%, 87.5%) | (75.7%, 85.7%) | (77.7%, 87.3%) | (84.0%, 92.2%) | (79.5%, 86.1%) | (81.4%, 87.8%) |
| Difference in rates (ceth-clari)c | 2.0% | −5.7% | −1.8% | |||
| CI for difference in ratesd | (−4.8%, 8.9%) | (−11.9%, 0.6%) | (−6.4%, 2.8%) | |||
| Fisher's exact teste | 0.5667 | 0.0769 | 0.4454 | |||
| PPc | ||||||
| Clinical cure rates | 205/218 (94.0%) | 195/208 (93.8%) | 205/224 (91.5%) | 212/221 (95.9%) | 410/442 (92.8%) | 407/429 (94.9%) |
| CI for clinical cure ratesb | (90.0%, 96.8%) | (89.5%, 96.6%) | (87.1%, 94.8%) | (92.4%, 98.1%) | (89.9%, 95.0%) | (92.3%, 96.8%) |
| Difference in rates (ceth-clari)c | 0.3% | −4.4% | −2.1% | |||
| CI for difference in ratesd | (−4.5%, 5.1%) | (−9.1%, 0.3%) | (−5.4%, 1.2%) | |||
| Fisher's exact teste | >0.9999 | 0.0775 | 0.2086 | |||
Subjects with “indeterminate” or “missing/not done” outcomes were treated as clinical failures in the analyses of the ITT population.
The 95% CI was computed using the incomplete beta function to give exactly 95% confidence.
Ceth, cethromycin; clari, clarithromycin.
The 95% CI was computed using normal approximation for the binomial distribution with the continuity correction method, CC = 1/(2 min (N1, N2)), where N1 is the number of subjects treated with cethromycin and N2 is the number of subjects treated with clarithromycin.
The 95% CI was computed from an exact binomial distribution.
In the integrated analysis, no significant treatment group differences were noted in the bacterial eradication rates of the individual pathogens (Tables 6 and 7). The most common pathogens were H. influenzae, Mycoplasma pneumoniae, and S. pneumoniae, with eradication rates ranging from 81.4% to 96.8% in the treatment groups in the ITT population and from 88.9% to 100% in the treatment groups in the PPc population. It is worth noting that the clinical efficacies of clarithromycin and cethromycin against a very limited number of erythromycin-resistant S. pneumoniae isolates were very similar to each other; these rates were also similar to the cure rates against erythromycin-susceptible S. pneumoniae isolates. Cethromycin, however, appeared more effective at treating S. pneumoniae bacteremic subjects (Table 8).
Table 6.
Bacterial eradication rates in the ITT and PPc populations for target pathogens isolated pretreatment by study and combined
| Study population | Study CL05-001 |
Study CL06-001 |
Integrated analysis: combined studies CL05-001 and CL06-001 |
|||
|---|---|---|---|---|---|---|
| Cethromycin, 300 mg QD | Clarithromycin, 250 mg BID | Cethromycin, 300 mg QD | Clarithromycin, 250 mg BID | Cethromycin, 300 mg QD | Clarithromycin, 250 mg BID | |
| ITTa | ||||||
| S. pneumoniaeb | 10/12 (83.3%) | 20/22 (90.9%) | 16/19 (84.2%) | 8/12 (66.7%) | 26/31 (83.9%) | 28/34 (82.4%) |
| H. influenzaec,d | 34/36 (94.4%) | 23/28 (82.1%) | 23/34 (67.6%) | 21/24 (87.5%) | 57/70 (81.4%) | 44/52 (84.6%) |
| S. aureuse | 9/14 (64.3%) | 13/14 (92.9%) | 7/9 (77.8%) | 8/11 (72.7%) | 16/23 (69.6%) | 21/25 (84.0%) |
| M. catarrhalis | 3/3 (100%) | 6/6 (100%) | 2/4 (50.0%) | 4/4 (100%) | 5/7 (71.4%) | 10/10 (100%) |
| C. pneumoniae | 6/6 (100%) | 5/7 (71.4%) | 6/6 (100%) | 6/6 (100%) | 12/12 (100%) | 11/13 (84.6%) |
| L. pneumophila | 4/4 (100%) | 3/5 (60.0%) | 1/1 (100%) | 4/4 (100%) | 5/5 (100%) | 7/9 (77.8%) |
| M. pneumoniae | 11/11 (100%) | 17/18 (94.4%) | 19/20 (95.0%) | 20/23 (87.0%) | 30/31 (96.8%) | 37/41 (90.2%) |
| PPc | ||||||
| S. pneumoniae | 9/9 (100%) | 17/18 (94.4%) | 15/17 (88.2%) | 8/10 (80.0%) | 24/26 (92.3%) | 25/28 (89.3%) |
| H. influenzae | 34/35 (97.1%) | 20/22 (90.9%) | 22/28 (78.6%) | 21/24 (87.5%) | 56/63 (88.9%) | 41/46 (89.1%) |
| S. aureus | 9/10 (90.0%) | 13/13 (100%) | 6/8 (75.0%) | 8/9 (88.9%) | 15/18 (83.3%) | 21/22 (95.5%) |
| M. catarrhalis | 2/2 (100%) | 6/6 (100%) | 2/3 (66.7%) | 4/4 (100%) | 4/5 (80.0%) | 10/10 (100%) |
| C. pneumoniae | 6/6 (100%) | 5/5 (100%) | 5/5 (100%) | 4/4 (100%) | 11/11 (100%) | 9/9 (100%) |
| L. pneumophila | 4/4 (100%) | 3/3 (100%) | 0/0 | 4/4 (100%) | 4/4 (100%) | 7/7 (100%) |
| M. pneumoniae | 11/11 (100%) | 16/16 (100%) | 18/19 (94.7%) | 19/19 (100%) | 29/30 (96.7%) | 35/35 (100%) |
Subjects with “indeterminate” or “missing/not done” outcomes were treated as noneradication in the analyses of the ITT population.
One clarithromycin subject is included that had an S. pneumoniae pathogen isolated after the initiation of treatment; the subject had an outcome of colonization.
One cethromycin subject is included that had an H. influenzae pathogen isolated after the initiation of treatment; the subject had an outcome of colonization.
Four clarithromycin subjects are included that had H. influenzae pathogens isolated after the initiation of treatment; 2 subjects had outcomes of colonization, 1 subject had an outcome of superinfection, and 1 subject had an outcome of new infection.
One cethromycin subject is included that had an S. aureus pathogen isolated after the initiation of treatment; the subject had an outcome of new infection.
Table 7.
Clinical cure rates and bacteriological eradication rates by pretreatment erythromycin susceptibility for S. pneumoniae isolates (ITT population)
| Treatment | Clinical cure rate |
Bacteriological eradication rate |
||
|---|---|---|---|---|
| % erythromycin-susceptible S. pneumoniae (no. of cures/total) | % erythromycin-resistant S. pneumoniae (no. of cures/total) | % erythromycin-susceptible S. pneumoniae (no. eradicated/total) | % erythromycin-resistant S. pneumoniae (no. eradicated/total) | |
| Cethromycin, 300 mg QD | 80.8 (21/26) | 80.0 (4/5) | 84.6 (22/26) | 80.0 (4/5) |
| Clarithromycin, 250 mg BID | 70.8 (17/24) | 83.3 (5/6) | 87.5 (21/24) | 83.3 (5/6) |
Table 8.
Clinical and bacteriological outcomes for subjects with S. pneumoniae bacteremia (ITT population)
| Subject no. | Fine criterion classification | S. pneumoniae susceptibilitya | Clinical response | Bacteriological response |
|---|---|---|---|---|
| Cethromycin | ||||
| 1074-0008 | Fine I | Ery S, Pen S | Indeterminate | Indeterminate |
| 1085-0001 | Fine II | Ery S, Pen S | Cure | Presumed eradication |
| 3013-0026 | Fine IV | Ery S, Pen S | Cure | Eradication |
| 4118-0004 | Fine IV | Ery S, Pen S | Indeterminate | Eradication |
| 5101-0004 | Fine III | Ery S, Pen S | Cure | Eradication |
| Cure rate | 3/5 (60%) | 4/5 (80%) | ||
| Clarithromycin | ||||
| 1082-0012 | Fine II | Ery S, Pen S | Indeterminate | Eradication |
| 3004-0013 | Fine II | Ery R, Pen S | Indeterminate | Indeterminate |
| 3013-0028 | Fine II | Ery S, Pen S | Cure | Eradication |
| 3023-0004 | Fine I | Ery S, Pen S | Failure | Eradication |
| 3025-0004 | Fine II | Ery S, Pen S | Failure | Eradication |
| Cure rate | 1/5 (20%) | 4/5 (80%) | ||
Ery, erythromycin; Pen, penicillin; S, susceptible; R, resistant.
Safety.
Cethromycin was generally safe and well tolerated. A summary of treatment-emergent adverse events experienced by ≥2.0% of subjects in either treatment group in the combined studies is presented in Table 9. The most common treatment-emergent adverse events experienced in both treatment groups were diarrhea, nausea, dysgeusia, and headache. A statistically significantly greater proportion of cethromycin subjects reported dysgeusia compared with clarithromycin subjects (9.3% versus 4.0%). The experience did not impact compliance or discontinuation from study compared to subjects not reporting dysgeusia.
Table 9.
Treatment-emergent adverse events experienced by ≥2.0% of subjects integrated analysis: combined studies CL05-001 and CL06-001a
| System organ class | Cethromycin, 300 mg QD (n = 548) | Clarithromycin, 250 mg BID (n = 548) | P value |
|---|---|---|---|
| Gastrointestinal disorders | 74 (13.5) | 61 (11.1) | 0.270 |
| Diarrhea | 26 (4.7) | 24 (4.4) | 0.885 |
| Nausea | 20 (3.6) | 13 (2.4) | 0.289 |
| Vomiting | 11 (2.0) | 6 (1.1) | 0.328 |
| Nervous system disorders | 66 (12.0) | 45 (8.2) | 0.045 |
| Dysgeusia | 51 (9.3) | 22 (4.0) | 0.001 |
| Headache | 15 (2.7) | 23 (4.2) | 0.247 |
Percentages are displayed in parentheses. P values were obtained from Fisher's exact test.
Due to safety concerns reported for the ketolide telithromycin, including visual disturbances, sudden loss of consciousness, hepatotoxicity, and exacerbation of myasthenia gravis, considerable efforts were made to identify, monitor, and investigate these side effects during the study. No similar safety signals were detected. For example, even though transient liver function test elevations, such as alanine aminotransferase (ALT), aspartate transaminase (AST), gamma-glutamyltranspeptidase (GGT), and total and direct bilirubin, were reported in some patients in both treatment arms (who were followed to resolution to baseline), no subjects exhibited symptoms of any hepatotoxicity. Importantly, no subjects experienced simultaneous significant elevation of aminotransferases and bilirubin (Hy's law). However, as with any new agent, continued diligence is merited.
DISCUSSION
These results demonstrate that cethromycin achieved protocol-defined noninferiority compared to clarithromycin for the treatment of mild to moderate CAP. Clinical cure rates for cethromycin were consistent between the two trials; however, the clinical cure rates for clarithromycin in the CL06-001 trial were extraordinarily high. Interestingly, a review of published clarithromycin clinical trial results shows that cure rates of this magnitude have never been seen before with clarithromycin in a similar patient population (23, 33). Examination of the data, including subgroup analysis, geographical differences, seasonality, or disease severity, has been unsuccessful in explaining this result (1).
While cethromycin demonstrates efficacy in the treatment of many Gram-positive pathogens which play a role in the etiology of mild to moderate CAP, particular attention must be paid to activity in S. pneumoniae-infected individuals as infection with S. pneumoniae is the most common bacterial cause of CAP. Indeed, cethromycin was developed with S. pneumoniae, and, specifically, macrolide-resistant S. pneumoniae infection, as a primary clinical target (31). Results presented here (Table 7) demonstrate that while cethromycin did show impressive clinical activity in patients infected with both macrolide-resistant and macrolide-susceptible S. pneumoniae, total numbers of these patients were low. We believe several factors contributed to these low numbers.
Obtaining culturable pathogens from sputum of CAP patients remains a significant challenge. Unstained sputum smears were collected by the clinical site and forwarded to a central laboratory for staining and qualification. Contamination of these samples by epithelial cells was a major reason for patient exclusion from the bacteriologically evaluable population. Additionally, sputum samples were collected in transport media and shipped to a central laboratory for culture, possibly reducing the number of S. pneumoniae pathogens isolated due to sample lability (6, 21). Finally, less than 24 h of antibiotic therapy was permissible for inclusion in the trial. Recent results suggest that a single dose of antibiotic may be adequate in eliminating the detectability of CAP-causative pathogens in sputum samples (8). Taken together, these reasons may help to explain the reduced numbers of subjects seen with qualifying pathogens, specifically, S. pneumoniae. Capturing study patients infected with macrolide-resistant S. pneumoniae becomes an even larger challenge in light of the above. Future clinical trials may involve the enrichment of the S. pneumoniae-infected patient population at screening using antigen detection rapid screening and conducting trials in areas of the world which demonstrate increased rates of macrolide resistance. One encouraging result seen was the efficacy of cethromycin, compared to clarithromycin, in the clinical and bacterial cure of individuals with S. pneumoniae bacteremia. This small sample of subjects showed impressive response to cethromycin treatment and future trials should attempt to capture more information regarding subjects with invasive disease. Demonstrating clinical utility of a ketolide agent in precisely the patient population most likely to benefit from this intervention remains a development challenge.
The applicability and utility of noninferiority trials in determining the efficacy of new treatment regimens for mild to moderate CAP has come under scrutiny by regulatory agencies (16) and academic investigators since the initiation of this program (12). Specifically, the determination of an acceptable noninferiority margin in the absence of a supported treatment effect of the comparator agent has proven problematic. Rigorously defining this effect is challenging in CAP due to the general consensus that the use of placebo controlled trials is inappropriate (20, 25). The statistical plan developed for these trials required that the delta used to establish noninferiority be determined by the clinical cure rates obtained in the trial. This sliding delta method has since been suggested to be inadequate in assessing noninferiority by statisticians in this field. Indeed, the determination of noninferiority in this indication and in this patient population has become problematic (12).
Clinical response was determined by the principal investigator based on prespecified criteria for assessment. This method has also been recently debated, as researchers contest the objectivity of investigator-based assessments as well as their potential to introduce intra- and interobserver variability (16). Current discussion regarding appropriate outcome measurements often centers on the use of patient-reported outcome assessments to circumvent these potential biases. Significant effort will be required, however, to qualify such an instrument (34, 35) for use in a pivotal clinical program.
Finally, the severity of illness of patients has also been questioned, with reference specifically to the Fine criterion categorization. We argue that, in a separate analysis not presented here, the number and severity of signs and symptoms specific to CAP were similar in all Fine score categories. While the Fine score is a useful and well-regarded tool for assessing the risk of mortality in a treatment setting, it is not a tool that should be employed to stratify patients into pools which define the extent of a patient's CAP pathology, especially in an outpatient trial.
Conclusions.
In these trials, cethromycin was efficacious and safe in the treatment of mild to moderate CAP in adult patients. Several currently available agents lack the antibacterial activity to address the pathogen challenges facing the CAP treatment provider, while others have the antibacterial activity but this activity comes at the expense of collateral damage and patient safety. Cethromycin may provide the prescribing community with an agent which retains the antibacterial profile necessary for the treatment of common and more difficult-to-treat community-acquired pneumonia, while maintaining an acceptable safety profile, ensuring that patients benefit from the treatment. The results presented here suggest that in the population examined thus far, the benefits of oral cethromycin treatment appear to exceed the risks for the treatment of mild to moderate CAP in an outpatient setting.
ACKNOWLEDGMENTS
This work was funded and conducted by Advanced Life Sciences. We report no conflicts of interest and are employees of Advanced Life Sciences.
Footnotes
Published ahead of print 30 January 2012
REFERENCES
- 1. Advanced Life Sciences, Inc. 2009. FDA Anti-Infective Drugs Advisory Committee held on June 2, 2009 to discuss NDA 22-398 for cethromycin oral tablets. http://www.fda.gov/downloads/AdvisoryCommittees/CommitteesMeetingMaterials/Drugs/Anti-InfectiveDrugsAdvisoryCommittee/UCM166989.pdf Accessed 14 December 2010
- 2. Bertrand D, Bertrand S, Neveu E, Fernandes P. 2010. Molecular characterization of off-target activities of telithromycin: a potential role for nicotinic acetylcholine receptors. Antimicrob. Agents Chemother. 54:5399–5402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Brueggemann AB, et al. 2000. In vitro activity of ABT-773, a new ketolide, against recent clinical isolates of Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis. Antimicrob. Agents Chemother. 44:447–449 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Capobianco JO, et al. 2000. Studies of the novel ketolide ABT-773: transport, binding to ribosomes, and inhibition of protein synthesis in Streptococcus pneumoniae. Antimicrob. Agents Chemother. 44:1562–1567 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Douthwaite S, Champney WS. 2001. Structures of ketolides and macrolides determine their mode of interaction with the ribosomal target site. J. Antimicrob. Chemother. 48(Suppl 2):1–8 [DOI] [PubMed] [Google Scholar]
- 6. Drake C, Barenfanger J, Lawhorn J, Verhulst S. 2005. Comparison of Easy-Flow Copan Liquid Stuart's and Starplex Swab transport systems for recovery of fastidious aerobic bacteria. J. Clin. Microbiol. 43:1301–1303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Eiznhamer DA, et al. 2007. In vitro activity of cethromycin, a novel antibiotic under clinical development, against S. pneumoniae not susceptible to telithromycin. Abstr. 47th Intersci. Conf. Antimicrob. Agents Chemother., abstr E-1633. [Google Scholar]
- 8. Endeman H, et al. 2008. Clinical features predicting failure of pathogen identification in patients with community acquired pneumonia. Scand. J. Infect. Dis. 40:715–720 [DOI] [PubMed] [Google Scholar]
- 9. File TM., Jr 2004. Streptococcus pneumoniae and community-acquired pneumonia: a cause for concern. Am. J. Med. 117(Suppl 3A):39S–50S [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. File TM, Jr, et al. 2004. Guidelines for empiric antimicrobial prescribing in community-acquired pneumonia. Chest 125:1888–1901 [DOI] [PubMed] [Google Scholar]
- 11. File TM. 2009. The science of selecting antimicrobials for community-acquired pneumonia (CAP). J. Manag. Care Pharm. 15(Suppl):S5–S11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Fleming TR, Powers JH. 2008. Issues in noninferiority trials: the evidence in community-acquired pneumonia. Clin. Infect. Dis. 47(Suppl 3):S108–S120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Franceschi F, Kanyo Z, Sherer EC, Sutcliffe J. 2004. Macrolide resistance from the ribosome perspective. Curr. Drug Targets Infect. Disord. 4:177–191 [DOI] [PubMed] [Google Scholar]
- 14. Goldstein EJ, et al. 2001. In vitro activities of ABT-773, a new ketolide, against aerobic and anaerobic pathogens isolated from antral sinus puncture specimens from patients with sinusitis. Antimicrob. Agents Chemother. 45:2363–2367 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Goossens H, et al. 2005. Outpatient antibiotic use in Europe and association with resistance: a cross-national database study. Lancet 365:579–987 [DOI] [PubMed] [Google Scholar]
- 16. Higgins K, et al. 2008. Overview of recent studies of community-acquired pneumonia. Clin. Infect. Dis. 47(Suppl 3): S150–S156 [DOI] [PubMed] [Google Scholar]
- 17. Jorgensen JH, Crawford SA, McElmeel ML, Whitney CG. 2004. Activities of cethromycin and telithromycin against recent North American isolates of Streptococcus pneumoniae. Antimicrob. Agents Chemother. 48:605–607 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Levy SB, Marshall B. 2004. Antibacterial resistance worldwide: cause, challenge and responses. Nat. Med. 10(Suppl 12):S122–S129 [DOI] [PubMed] [Google Scholar]
- 19. Lode H. 2010. Safety and tolerability of commonly prescribed oral antibiotics for the treatment of respiratory tract infections. Am. J. Med. 123(Suppl 4):S26–S38 [DOI] [PubMed] [Google Scholar]
- 20. Mandell LA, et al. 2007. Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clin. Infect. Dis. 44(Suppl 2):S27–S72 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Mason CK, et al. 2010. Optimisation of storage conditions for maintaining culturability of penicillin-susceptible and penicillin-resistant isolates of Streptococcus pneumoniae in transport medium. Br. J. Biomed. Sci. 67:1–4 [DOI] [PubMed] [Google Scholar]
- 22. Mason EO, Jr, et al. 2003. In vitro activities of cethromycin (ABT-773), a new ketolide, against Streptococcus pneumoniae strains that are not susceptible to penicillin or macrolides. Antimicrob. Agents Chemother. 47:166–169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Mathers Dunbar L, Hassman J, Tellier G. 2004. Efficacy and tolerability of once-daily oral telithromycin compared with clarithromycin for the treatment of community-acquired pneumonia in adults. Clin. Ther. 26:48–62 [DOI] [PubMed] [Google Scholar]
- 24. Metlay JP. 2004. Antibacterial drug resistance: implications for the treatment of patients with community-acquired pneumonia. Infect. Dis. Clin. North Am. 18:777–790 [DOI] [PubMed] [Google Scholar]
- 25. Murphy TF. 2008. Placebo-controlled trials of treatments for community-acquired pneumonia: review of the literature and discussion of feasibility and potential value. Clin. Infect. Dis. 47(Suppl 3):S145–S149 [DOI] [PubMed] [Google Scholar]
- 26. Muto CA, et al. 2005. A large outbreak of Clostridium difficile-associated disease with an unexpected proportion of deaths and colectomies at a teaching hospital following increased fluoroquinolone use. Infect. Control Hosp. Epidemiol. 26:273–280 [DOI] [PubMed] [Google Scholar]
- 27. Niederman MS. 2004. Review of treatment guidelines for community-acquired pneumonia. Am. J. Med. 117(Suppl 3A):51S–57S [DOI] [PubMed] [Google Scholar]
- 28. Nilius AM, et al. 2001. Comparative in vitro activity of ABT-773, a novel antibacterial ketolide. Antimicrob. Agents Chemother. 45:2163–2168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Nugent R, Back E, Beith A. 2010. The race against drug resistance. Center for Global Development's Drug Resistance Working Group, Washington, DC [Google Scholar]
- 30. Pépin J, et al. 2005. Emergence of fluoroquinolones as the predominant risk factor for Clostridium difficile-associated diarrhea: a cohort study during an epidemic in Quebec. Clin. Infect. Dis. 41:1254–1260 [DOI] [PubMed] [Google Scholar]
- 31. Shortridge VD, et al. 2002. Comparison of in vitro activities of ABT-773 and telithromycin against macrolide-susceptible and -resistant streptococci and staphylococci. Antimicrob. Agents Chemother. 46:783–786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Spellberg B, Fleming TR, Gilbert DN. 2008. Executive summary: workshop on issues in the design and conduct of clinical trials of antibacterial drugs in the treatment of community-acquired pneumonia. Clin. Infect. Dis. 47(Suppl 3): S105–S107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Tellier G, et al. 2004. Clinical and bacteriological efficacy and safety of 5 and 7 day regimens of telithromycin once daily compared with a 10 day regimen of clarithromycin twice daily in patients with mild to moderate community-acquired pneumonia. J. Antimicrob. Chemother. 54:515–523 [DOI] [PubMed] [Google Scholar]
- 34. U. S. Department of Health and Human Services, Food and Drug Administration Center for Drug Evaluation and Research (CDER), Center for Biologics Evaluation and Research (CBER), Center for Devices and Radiological Health (CDRH) 2009. Guidance for industry. Patient reported outcome measures: use in medical product development to support labeling claims. [Google Scholar]
- 35. U. S. Department of Health and Human Services, Food and Drug Administration Center for Drug Evaluation and Research (CDER) 2010. Guidance for industry. Qualification process for drug development tools (draft). [Google Scholar]
- 36. von Eiff C, Peters G. 2002. Comparative in vitro activity of ABT-773 and two macrolides against staphylococci. J. Antimicrob. Chemother. 49:189–192 [DOI] [PubMed] [Google Scholar]
- 37. Xu J, Kochanek KD, Murphy SL, Tejada-Vera B. 2010. Deaths: final data for 2007. Natl. Vital Stat. Rep. 58:1–136 [PubMed] [Google Scholar]
- 38. Zhanel GG, et al. 2002. A critical review of the fluoroquinolones: focus on respiratory infections. Drugs 62:13–59 [DOI] [PubMed] [Google Scholar]