Abstract
Current efforts to develop plague vaccines focus on LcrV, a polypeptide that resides at the tip of type III secretion needles. LcrV-specific antibodies block Yersinia pestis type III injection of Yop effectors into host immune cells, thereby enabling phagocytes to kill the invading pathogen. Earlier work reported that antibodies against Y. pestis LcrV cannot block type III injection by Yersinia enterocolitica strains and suggested that lcrV polymorphisms may provide for escape from LcrV-mediated plague immunity. We show here that polyclonal or monoclonal antibodies raised against Y. pestis KIM D27 LcrV (LcrVD27) bind LcrV from Y. enterocolitica O:9 strain W22703 (LcrVW22703) or O:8 strain WA-314 (LcrVWA-314) but are otherwise unable to block type III injection by Y. enterocolitica strains. Replacing the lcrV gene on the pCD1 virulence plasmid of Y. pestis KIM D27 with either lcrVW22703 or lcrVWA-314 does not affect the ability of plague bacteria to secrete proteins via the type III pathway, to inject Yops into macrophages, or to cause lethal plague infections in mice. LcrVD27-specific antibodies blocked type III injection by Y. pestis expressing lcrVW22703 or lcrVWA-314 and protected mice against intravenous lethal plague challenge with these strains. Thus, although antibodies raised against LcrVD27 are unable to block the type III injection of Y. enterocolitica strains, expression of lcrVW22703 or lcrVWA-314 in Y. pestis did not allow these strains to escape LcrV-mediated plague protective immunity in the intravenous challenge model.
INTRODUCTION
Three Yersinia species—Yersinia enterocolitica, Yersinia pestis, and Yersinia pseudotuberculosis—are pathogenic to humans (13). All three species use virulence plasmid-encoded type III secretion machines to transport effector proteins (Yops) into host cells, thereby disabling innate immune defenses (16, 17). Due to their modes of entry and dissemination, Yersinia species cause distinct pathologies (13). Y. enterocolitica and Y. pseudotuberculosis are enteric pathogens that invade the mucosa and lymphoid tissues of the gastrointestinal tract (24). Y. pestis is the causative agent of plague (59), a potentially catastrophic disease due to its high mortality and dissemination following entry into the skin via arthropod vectors or into the lung via aerosol droplets (53). Plague is endemic in many geographical areas and causes an estimated annual mortality of 3,000 cases worldwide, with disease foci in Madagascar and Uganda (5, 6). Y. pestis has been used as a biological weapon (31). Possible illegitimate use of Y. pestis as well as the possibility of naturally occurring plague epidemics or pandemics represent an impetus for the development of a protective vaccine (29, 30).
Two antigens have been studied extensively for the development of subunit vaccines (49). Caf1 (F1) subunits are assembled into pili (61), and antibodies against this protein can protect against bubonic or pneumonic plague challenge (3, 4). Nevertheless, caf1 is not absolutely required for the pathogenesis of pneumonic plague in mice, rats, guinea pigs, nonhuman primates, or humans, indicating that F1 pilin cannot be used alone as a protective antigen (12, 25, 46, 58). The second protective antigen, LcrV (10, 11), is absolutely essential for plague pathogenesis (44). When used as a purified subunit vaccine, LcrV generates humoral immune responses that are protective against Y. pestis bubonic or pneumonic plague challenge in every animal model examined (48, 49).
Induction of Yersinia type III secretion leads to the assembly of needle complexes, whose function is to insert into the plasma membrane of host immune cells and to provide for the injection of effector Yops, thereby blocking phagocytosis and other innate immune functions (15, 34). LcrV is a substrate of the type III secretion pathway and also deposited at the tip of needle complexes (38, 54). In addition to other type III machine components, LcrV requires binding to a cytoplasmic regulatory factor, LcrG, for its secretion and needle tip assembly (21, 41). Antibodies directed against LcrV block Y. pestis and Y. pseudotuberculosis type III injection of host cells (45, 56).
LcrV exerts immunosuppressive effects owing to its activation of TLR2/6 and JNK2 signaling pathways, thereby repressing proinflammatory cytokines (tumor necrosis factor alpha and gamma interferon) and promoting the release of interleukin-10 (23, 39, 40). The rV10 antigen, which lacks residues 271 to 300 of Y. pestis LcrV, is devoid of these immunosuppressive attributes (42). When used as a subunit vaccine, rV10 raises antibodies that protect mice, rats, guinea pigs, and nonhuman primates against lethal plague challenge (1, 19, 22, 49). Further, a monoclonal antibody that binds LcrV residues 196 to 225 (MAb-BA5) can block Y. pestis type III injection and may be useful for postexposure prophylaxis of plague (49).
Two distinct lineages of lcrV have been described (50). One is comprised of the V antigen of the closely related Y. pestis and Y. pseudotuberculosis, where LcrV-specific antibodies provide cross-protection against infection with either species but not with the Y. enterocolitica O:8 strain WA-314 (36). Roggenkamp and coworkers suggested a hypervariable region, LcrV residues 225 to 232, could be the structural basis for strain specific immune protection (50). If so, lcrV polymorphisms that maintain the functional attributes of the type III secretion pathway could result in variants that escape plague protective immunity. This possibility was examined here by expressing the lcrV gene from Y. enterocolitica O:8 and O:9 serotypes in Y. pestis.
MATERIALS AND METHODS
Bacterial strains and plasmids.
The Yersinia strains used in the present study are listed in Table 1. Plasmid pVL49 has been previously described (33). In order to generate pNM77, lcrV from Y. pestis was amplified using the primers lcrVD27 5′ NdeI (5′-CATATGATTAGAGCCTACGAACAAAACCCACAA-3′) and lcrVD27 3′ BamHI (5′-GGATCCTCATTTACCAGACGTGTCATCTAGCAGACG-3′) and ligated with pCR2.1 (Invitrogen). The resulting plasmid, pNM78, was then digested with NdeI and BamHI, and the resulting lcrV fragment was ligated with pDA112 that had also been digested with NdeI and BamHI to yield pNM77.
Table 1.
Bacterial strains used in this study
| Strain | Genotype | Source or reference |
|---|---|---|
| Yersinia enterocolitica | ||
| W22703 | Serotype O:9 clinical isolate | 18 |
| WA-314 | Serotype O:8 clinical isolate | 2 |
| CT1 | Stop codon, +1 frameshift mutation at position 11 of lcrV in W22703 pYV227 | 33 |
| Yersinia pestis | ||
| KIM D27 | Nonpigmented (pgm) variant of medievalis isolate KIM | 9 |
| KLD29 | Stop codon, +1 frameshift mutation at position 2 of lcrV in KIM D27 pCD1 | 34 |
| NCM3 | KIM D27 pCD1 variant expressing lcrVW22703 | This study |
| NCM4 | KIM D27 pCD1 variant expressing lcrVWA-314 | This study |
To construct Y. pestis NCM3 and NCM4, lcrV from Y. enterocolitica W22703 and WA-314 was amplified from the virulence plasmids using the primers lcrH 96-120 (5′-GTAGAGTTGCTCTAAAGTGTCACTT-3′) and lcrG 258-288 (5′-CCAACGATGATGCGAGGGCAAATTATTTAA-3′) (reaction product 1). A region upstream of lcrV in Y. pestis that contained sequence homologous to that of the region amplified from Y. enterocolitica was amplified using the primers one-kb-down 3′ XmaI (5′-CCCGGGGCCAAAAATCTTTGATGCGATGCC-3′) and lcrH 1-27 (5′-ATGCAACAAGAGACGACAGACACTCAA-3′) (reaction product 2). A region downstream of lcrV on pCD1 was amplified using primers lcrV 90-114 (5′-TAACTGAACCAATTCTTCTAAAACTG-3′) and one-kb-up 5′ XbaI (5′-TCTAGAGGAGTTATTTGGCATTGGAGCCTG-3′) (reaction product 3). Reaction products 1 and 2 were mixed together to serve as a template for PCR amplification with primers one-kb-down 3′ XmaI and lcrH 96-120. The resulting PCR product was mixed with reaction product 3 to serve as a new template and amplified using the primers one-kb-down 3′ XmaI and one-kb-up 5′ XbaI. The 3-kb PCR product was cloned into pCR2.1 to yield pNM72. pNM72 and pLC28, a plasmid for allelic exchange (14), were digested with XmaI and XbaI and ligated together to yield pNM70. This plasmid was then used to replace Y. pestis lcrV on pCD1 with Y. enterocolitica lcrV alleles without disrupting the surrounding sequence.
Type III secretion and injection.
Y. enterocolitica strains were grown overnight in 5 ml of tryptic soy broth (TSB) at 26°C in a rotary wheel at 150 rpm, with or without chloramphenicol (30 μg/ml) for plasmid maintenance. Y. pestis strains were grown overnight in 5 ml of heart infusion broth (HIB) at 26°C in a rotary wheel at 150 rpm with or without 10 μg of chloramphenicol/ml for plasmid maintenance. The following day, Y. enterocolitica cultures were diluted 1:50 into fresh medium to a total volume of 4 ml containing 5 mM EGTA and grown at 26°C in a rotary wheel at 150 rpm for 2 h. Y. pestis strains were diluted 1:40 into M9 minimal medium to a total volume of 4 ml and grown at 26°C in a rotary wheel at 150 rpm for 2 h. For type III secretion measurements, cultures were shifted to 37°C in a rotary wheel at 150 rpm for 3 h. Cultures were centrifuged at 15,000 × g and separated into supernatant (S) and pellet (P) fractions. Proteins in both fractions were precipitated with 5% trichloroacetic acid, washed with acetone, and suspended in sodium dodecyl sulfate (SDS) sample buffer. Samples were subjected to SDS–15% PAGE and immunoblotting with rabbit antibodies.
To analyze Yersinia type III injection of tissue culture cells, bacteria were grown overnight as described above and then diluted 1:20 the next day into fresh media to a total volume of 4 ml. After 2 h of growth at 26°C in a rotary wheel at 150 rpm, bacteria were added to 75-cm2 tissue culture flasks of 80 to 90% confluent HeLa cells grown in 15 ml of Opti-MEM I (Invitrogen) at a multiplicity of infection (MOI) of 10. Three hours after infection, the medium was removed from the flask and centrifuged at 15,000 × g for 15 min to separate the nonadherent bacteria from soluble proteins secreted into the medium. Aliquots of 7 ml of medium were precipitated with methanol-chloroform. The remaining medium was removed, and the pellets were suspended in 1× phosphate-buffered saline (PBS)–1% SDS. Proteins in 7-ml aliquots of such samples were precipitated with methanol-chloroform. Digitonin (1% in 1× PBS) was added to the tissue culture flasks. After 20 min of shaking at room temperature, the flasks were scraped, and the resulting suspension was centrifuged at 15,000 × g to separate the supernatant and sediment (pellet). Proteins in both fractions were precipitated with methanol-chloroform as described above. Precipitates were suspended in SDS sample buffer and analyzed by SDS-PAGE and immunoblotting.
Antibody binding to purified LcrV.
To measure the affinity of antibodies for LcrV proteins, 96-well plates were coated with a 100-μl solution of LcrV (100 μg of protein/ml) from Y. pestis KIM D27 (LcrVD27), Y. enterocolitica W22703 (LcrVW22703), or Y. enterocolitica WA-314 (LcrVWA-314) purified from recombinant E. coli strains (42) and incubated in carbonate buffer (1.6 g of sodium carbonate/liter, 2.9 g of sodium bicarbonate/liter) overnight at 4°C. The plates were washed twice with 1% PBS-Tween, blocked with 1% bovine serum albumin (BSA) in PBS at room temperature for 1 h, and then washed twice with 1% PBS-Tween. Known quantities of affinity-purified rabbit anti-V10 were serially diluted 2-fold starting at 500 ng of IgG/ml in PBS containing 1% BSA to a final volume of 100 μl and used as a reference standard. Both undiluted and diluted rabbit anti-V10 sera IgG (1:25,000, 1:35,000, and 1:45,000) or mouse MAb-BA5 IgG (60 ng/ml) antibodies were added to the various LcrV antigens to a final volume of 100 μl. Samples were incubated for 2 h at room temperature. The plates were washed three times with 1% PBS-Tween, after which,100 μl of horseradish peroxidase-linked donkey anti-rabbit IgG (Jackson Immunoresearch) diluted 1:10,000 in PBS containing 1% BSA was added to each well. The samples were incubated for 1 h at room temperature and then washed three times with 1% PBS-Tween. The samples were developed using a BD OptElA TMB substrate reagent kit (BD Biosciences), the absorbance at 450-nm light was measured, and the data were analyzed using GraphPad Prism. Absorbance values were measured for each sample and antibody dilution. The absorbance values of control reactions lacking primary antibodies were subtracted from the absorbance data obtained with primary antibodies to correct for nonspecific binding.
Cytotoxicity assays.
Portions (5 ml) of bacterial cultures were grown overnight in either TSB (Y. enterocolitica) or HIB (Y. pestis) in a rotary wheel at 150 rpm, supplemented with chloramphenicol where appropriate. The cultures were diluted 1:20 into fresh medium to a total volume of 4 ml with or without antibiotic the following day and incubated at 26°C in a rotary wheel at 150 rpm for 2 h. The cultures were incubated at 37°C in a rotary wheel at 150 rpm for 1 h, and bacteria were added to HeLa cell monolayers in 12-well dishes that were seeded the day before at 105 cells per well at an MOI of 10. Where indicated, 75 μl of naive rabbit serum, 1 mg of purified MAb-BA5, or 1 mg of rV10-specific polyclonal antibody was added just prior to the addition of bacteria to HeLa cells. The infection was allowed to proceed for 3 h, after which the medium was removed, and the samples were fixed for 20 min in 3.7% formaldehyde. Samples were quenched with 0.1 M glycine (pH 7.0) for 5 min and then washed once with PBS. Triton X-100 was added to a final concentration of 0.1%, and the cells were permeabilized for 30 min at 4°C. PBS was used to wash the wells three times, after which 5% nonfat dried milk in PBS was added, followed by incubation at room temperature for 20 min. Three units (99 nM) of rhodamine-phalloidin were added to samples, followed by 20 min of incubation at room temperature. Samples were washed with PBS three times and imaged with a Nikon TE-2000 inverted microscope.
Macrophage killing assays.
J774.1 macrophages were infected with refreshed bacterial cultures at an MOI of 10 in either the presence or the absence of 1 mg of purified anti-rV10 or MAb-BA5 antibodies. Infections were allowed to proceed for 3 h, after which gentamicin was added to 100 μg/ml. After an additional 2.5 h, the samples were stained with 2.5 μM propidium iodide and imaged, and apoptotic cells were enumerated using a Nikon TE-2000 inverted microscope. At least three independent determinations were obtained for each condition, totaling more than 1,000 cells. Control conditions (naive serum and PBS) were individually compared to each specific test condition. The data were analyzed with Student's two-tailed, unpaired t test to examine statistical significance.
Animal challenge experiments.
Six- to eight-week-old naive BALB/c mice (n = 10) were challenged by intravenous injection with 0.1-ml aliquots of either 102 or 104 CFU of Y. pestis KIM D27, Y. pestis NCM3, or Y. pestis NCM4. Y. pestis strains were grown in HIB overnight at 26°C in a rotary wheel at 150 rpm, washed, and diluted into sterile PBS to the desired concentration. The animals were monitored for morbidity, mortality, and recovery for 14 days after infection. Challenge experiments were performed twice for each strain. For passive-transfer experiments, 200-μl portions of naive rabbit serum, rabbit anti-LcrV serum, or rabbit anti-rV10 serum were injected into the peritoneal cavities of 6- to 8-week-old naive BALB/c mice 1 h prior to intravenous infection with 2 × 103 CFU of Y. pestis KIM D27, Y. pestis NCM3, or Y. pestis NCM4. The mice were observed for morbidity, mortality, and recovery over 14 days after infection. Passive-transfer experiments were performed twice for each strain and test condition. All animal experiments were performed in accordance with institutional guidelines following experimental protocol review and approval by the Institutional Biosafety Committee and the Institutional Animal Care and Use Committee at the University of Chicago.
RESULTS
Anti-rV10 and MAb-BA5 antibodies block Y. pestis KIM D27 but not Y. enterocolitica W22703 or WA-314 type III injection of HeLa cells.
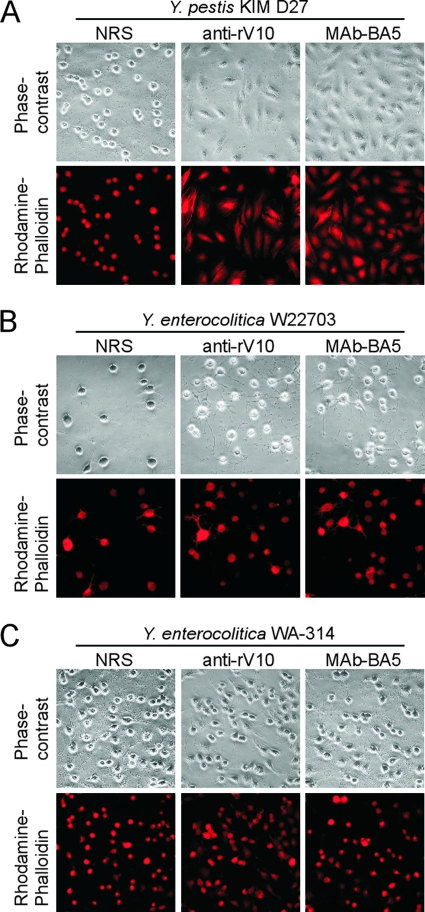
To assess whether antibodies generated against Y. pestis KIM D27 LcrV (LcrVD27) are broadly cross-protective against Y. enterocolitica, we first utilized a tissue culture model of infection (32). Y. pestis strain KIM D27 or Y. enterocolitica strains W22703 and WA-314 were added to HeLa cell monolayers in the presence of either naive rabbit serum, 1.0 mg of purified MAb-BA5 (47)/ml, or of affinity-purified rabbit polyclonal antibodies directed against the rV10 vaccine antigen (anti-rV10) (22). After 3 h of infection, the samples were fixed, stained with rhodamine-phalloidin, and analyzed by fluorescence microscopy (52, 55). Naive rabbit serum had no effect on the ability of Yersinia strains to inject HeLa cells and cause cell rounding as well as actin-cable rearrangements (51) (Fig. 1). MAb-BA5 and anti-rV10 antibodies provided protection against Y. pestis KIM D27 type III injection (Fig. 1A). In contrast, neither of the two antibody preparations was able to provide protection against Y. enterocolitica W22703 or WA-314 injection of effector Yops (Fig. 1BC). Motin et al. reported that antibodies against Y. pestis LcrV protect experimental animals against Y. pestis plague challenge but not against Y. enterocolitica WA (serotype O:8) challenge (36). The data in Fig. 1 suggest that this phenomenon may be due to the inability of LcrV-specific antibodies to block Y. enterocolitica type III injection of host cells.
Fig 1.
Antibodies against Y. pestis LcrV inhibit type III injection of Y. pestis KIM D27 (A) but not of Y. enterocolitica W22703 (B) or WA-314 (C). Bacterial cultures were grown overnight and diluted into fresh medium, followed by growth for 2 h at 26°C. HeLa cells (105) were seeded in 12-well dishes with Opti-MEM 1 day prior to infection. Immediately prior to infection, HeLa cells were treated with naive rabbit serum, 1 mg of polyclonal anti-rV10 rabbit antibody (anti-rV10)/ml or 1 mg of the mouse monoclonal antibody MAb-BA5/ml, followed by incubation for 3 h. Samples were fixed, stained with rhodamine-phalloidin, and imaged by fluorescence or phase-contrast microscopy.
Anti-rV10 and MAb-BA5 antibodies bind LcrV from Y. pestis and Y. enterocolitica strains with similar affinity.
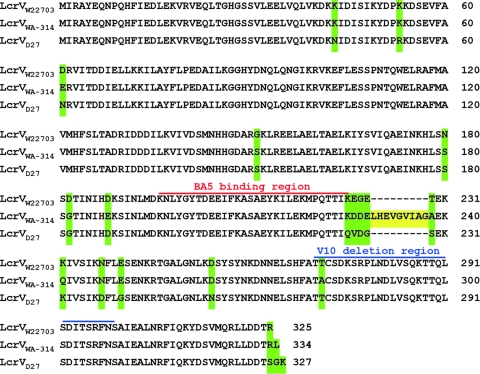
Figure 2 displays an amino acid alignment of the lcrV products from Y. pestis KIM D27, Y. enterocolitica W22703, and Y. enterocolitica WA-314 assembled with the EMBOSS pairwise alignment algorithm. LcrV proteins from Y. pestis and Y. enterocolitica strains W22703 or WA-314 are highly homologous, exhibiting 94.8 and 92.5% identities, respectively. In addition, the lcrV gene products of the two Y. enterocolitica strains are 93.7% identical. When Y. pestis LcrV and Y. enterocolitica W22703 LcrV were compared, a five-amino-acid segment (LcrV residues 225 to 229) represented the only striking difference (Fig. 2). Y. enterocolitica WA-314 harbors an additional nine amino acids inserted at the same site (Fig. 2). Earlier work referred to this site as the hypervariable region of LcrV (50). The hypervariable region is located immediately adjacent to the MAb-BA5 binding site (47). We wondered whether LcrV from Y. enterocolitica W22703 (LcrVW22703) and WA-314 (LcrVWA-314) bind MAb-BA5 or anti-rV10 antibodies in the same manner as Y. pestis LcrV (LcrVD27). As examined by quantitative enzyme-linked immunosorbent assay (ELISA) using purified recombinant LcrV from each Yersinia species, MAb-BA5 as well as anti-rV10 bound LcrVD27, LcrVW22703, and LcrVWA-314 with similar affinity over a dilution range of 1:25,000, 1:35,000, and 1:45,000 (Table 2).
Fig 2.
Primary structure of LcrV from Y. enterocolitica W22703, Y. enterocolitica WA-314, and Y. pestis KIM D27. The amino acid sequences of LcrV from Y. enterocolitica W22703 (LcrVW22703) (GenBank accession no. AF102990.1), WA-314 (LcrVWA-314) (GenBank accession no. X96796.1), and Y. pestis KIM D27 (LcrVD27) (GenBank accession no. NC_003131.1) were compared using the EMBOSS pairwise alignment algorithm program. Residues that differ between the species are highlighted in green. The binding site of MAb-BA5 is overlined in red, while residues of Y. pestis LcrVD27 that were deleted for the generation of the V10 antigen are overlined in blue. The hypervariable region in LcrVWA-314 is highlighted in yellow.
Table 2.
Binding of MAb-BA5 or anti-rV10 antibodies to polymorphic LcrV proteins
| ELISA antigen | Mean IgG concn ± SEM bound to antigen |
|
|---|---|---|
| Anti-rV10a | MAb-BA5b | |
| LcrVD27 | 2.61 ± 0.22 | 61.94 ±1.04 |
| LcrVW22703 | 2.71 ± 0.09 | 63.69 ± 2.89 |
| LcrVWA-314 | 3.31 ± 0.51 | 69.73 ± 3.16 |
The average amount of anti-rV10 IgG antibody (in mg/ml) in undiluted rabbit anti-rV10 serum that bound to purified recombinant LcrV from Y. pestis KIM D27 (LcrVD27), Y. enterocolitica W22703 (LcrVW22703), or Y. enterocolitica WA-314 (LcrVWA-314) immobilized in 96-well plates was calculated from three independent experimental determinations. Samples were developed using a BD OptElA TMB substrate reagent kit (BD Biosciences), the absorbance of 450-nm light was measured, and the data were analyzed using GraphPad Prism. The absorbance values of control reactions lacking primary antibodies were subtracted from the absorbance data obtained with primary antibodies to correct for nonspecific binding. Two-tailed unpaired Student's t test was used to examine differences in antibody binding, which were judged not to be significant (LcrVD27 versus LcrVW22703, P = 0.6950; LcrVD27 versus LcrVWA-314, P = 0.2741; and LcrVW22703 versus LcrVWA-314, P = 0.3096). The experiment was repeated with three different dilutions of anti-rV10 serum (1:25,000, 1:35,000, and 1:45,000). Absorbance values were measured for each sample and antibody dilution, which generated results similar to those obtained with undiluted serum. For example, the average amounts of anti-rV10 IgG antibody (in ng/ml) in 1:35,000-diluted rabbit anti-rV10 serum were 92.95 ± 38.91 for LcrVD27, 84.01 ± 28.89 for LcrVW22703, and 97.01 ± 23.98 for LcrVWA-314 (LcrVD27 versus LcrVW22703, P = 0.7090; LcrVD27 versus LcrVWA-314, P = 0.5877; and LcrVW22703 versus LcrVWA-314, P = 0.8105).
The average amount of MAb-BA5 antibody (in ng/ml) bound to purified LcrVD27, LcrVW22703, or LcrVWA-314 immobilized in 96-well plates was calculated from three independent experimental determinations as described above. Two-tailed unpaired Student's t test was used to examine differences in antibody binding, which were judged not to be significant (LcrVD27 versus LcrVW22703, P = 0.5992; LcrVD27 versus LcrVWA-314, P = 0.0795; and LcrVW22703 versus LcrVWA-314, P = 0.2310).
Plasmid-carried polymorphic Y. enterocolitica lcrV alleles are functional and enable in vitro type III secretion and HeLa cell cytotoxicity of Y. pestis.
Plasmids expressing lcrV from Y. enterocolitica W22703(plcrVW22703), Y. enterocolitica WA-314(plcrVWA-314), or Y. pestis KIM D27(plcrVD27) were transformed into Y. pestis variants carrying a mutation in the lcrV gene (strain KLD29) (34). Type III secretion of Y. pestis cultures was induced via bacterial growth in medium lacking calcium ions and shifting the temperature to 37°C. After 3 h of incubation, the cultures were centrifuged to separate proteins secreted into the culture medium (S, supernatant) from those in the bacterial sediment (P, pellet). Both samples were subjected to immunoblotting with rabbit antisera raised against purified recombinant Yersinia proteins (Fig. 3A and B). As expected, the Y. pestis lcrV mutant KLD29 failed to secrete YopE or YopH into the culture medium (Fig. 3A). This defect was restored to wild-type levels when KLD29 was transformed with plcrVW22703 or plcrVD27 (Fig. 3A). As a fractionation control, RNA polymerase subunit A (RpoA) was not secreted into the culture medium (Fig. 3A). The YopE species of the lcrV mutant strain KLD29 migrated more slowly on SDS-PAGE than YopE of the wild-type Y. pestis parent; the molecular basis for this phenomenon is not known.
Fig 3.
Expression of polymorphic lcrV genes in Y. pestis. The lcrV mutant Y. pestis strain KLD29 was transformed with plasmids encoding either Y. enterocolitica W22703 lcrV (plcrVW22703), Y. enterocolitica WA-314 lcrV (plcrVWA-314), or Y. pestis KIM D27 lcrV (plcrVD27). (A) Wild-type Y. pestis KIM D27 (WT) and the KLD29 strains were analyzed for type III secretion in laboratory broth, following growth at 37°C in medium with chelated calcium ions. Briefly, cultures were centrifuged to separate the extracellular medium with the supernatant (S) from the bacterial pellet (P). Proteins in both samples were identified by immunoblotting with rabbit antibodies specific for type III secretion substrates (YopE, YopH, and LcrV), as well as RNA polymerase A (RpoA), which resides in bacterial cells. (B) Y. pestis strains were used to infect HeLa tissue culture cells for 3 h. The culture medium (M) was centrifuged to generate supernatant (S, extracellular medium) and pellet (P, nonadherent bacteria) fractions. Cells were extracted with digitonin (D) and centrifuged to separate proteins in the supernatant (S, cytosolic extract) from the pellet (P, cellular organelles and adherent bacteria). YopE (the Yersinia type III effector), LcrV, and RpoA, as well as IκB, a HeLa cell cytoplasmic protein, were analyzed by immunoblotting. (C) Control sample of uninfected HeLa cells examined as described below. (D) HeLa cultures (2 × 105 cells) were treated with naive rabbit serum (NRS), 1 mg of polyclonal anti-rV10 rabbit antibody (anti-rV10)/ml or 1 mg of the mouse monoclonal antibody MAb-BA5/ml immediately prior to infection with Y. pestis KLD29 harboring plcrVW22703, plcrVWA-314, plcrVD27 or no plasmid and incubation for 3 h. Samples were fixed, stained with rhodamine-phalloidin, and imaged by fluorescence or phase-contrast microscopy.
To examine whether Y. enterocolitica lcrV is functional for Y. pestis type III injection of tissue cultures, infected HeLa cells were analyzed by digitonin fractionation (32). The tissue culture medium (M) was decanted and centrifuged to sediment nonadherent bacteria and separate supernatant (S) and pellet (P) fractions. HeLa cells with adherent Y. pestis were extracted with digitonin, a cholesterol-specific detergent that disrupts the host cell plasma membrane but not the bacterial envelope. Digitonin extracts (D) were centrifuged to sediment Y. pestis and separate the bacterial pellet and insoluble membranes (P) from soluble cytoplasmic proteins in the supernatant (S). Proteins in all four fractions were precipitated with chloroform-methanol and analyzed by immunoblotting. When HeLa cells were infected with Y. pestis KLD29(plcrVD27), the type III effector YopE could be extracted with digitonin from the cytoplasm of tissue culture cells (Fig. 3B). The lcrV mutation in strain KLD29 lacking the plcrV plasmid abrogated type III injection of YopE (Fig. 3B). This defect was restored when the lcrV mutant was transformed with plcrVW22703 (Fig. 3B). As controls, digitonin extraction solubilized IκB from the cytoplasm of host cells but not the bacterial protein RpoA (Fig. 3B).
The ability of Y. pestis strains to inject effector Yops into host cells was also examined with the HeLa cell cytotoxicity assay and compared to uninfected control cells (Fig. 3CD). The lcrV mutant Y. pestis strain KLD29 failed to cause cell rounding and actin cable rearrangements. This defect was restored when KLD29 was transformed with plasmid plcrVD27, plcrVW22703, or plcrVWA-314 (Fig. 3D). Polyclonal anti-rV10 antibodies or MAb-BA5 blocked HeLa cell cytotoxicity mediated by Y. pestis KLD29 harboring plcrVD27, plcrVW22703, or plcrVWA-314 (Fig. 3D).
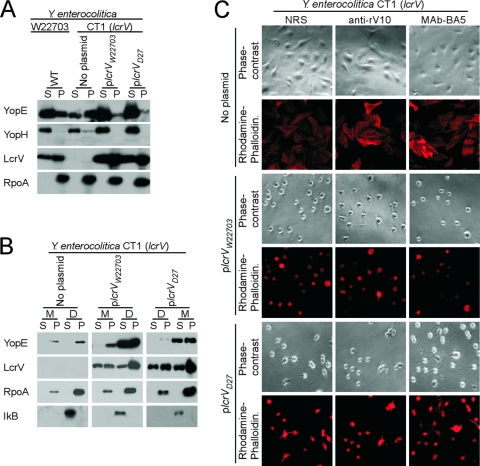
Plasmid-carried Y. pestis lcrV is functional for Y. enterocolitica type III injection.
Plasmids expressing lcrV from Y. enterocolitica W22703(plcrVW22703) or Y. pestis KIM D27(plcrVD27) were transformed into the Y. enterocolitica W22703 variant carrying a mutation in the lcrV gene (strain CT1) (33). Type III secretion of Y. enterocolitica cultures was induced via the chelation of calcium ions and shifting the temperature to 37°C. As expected, strain CT1 failed to express lcrV, a defect that was restored by transformation with either plcrVW22703 or plcrVD27 (Fig. 4A). Unlike Y. pestis, the Y. enterocolitica lcrV mutant continued to secrete YopE and YopH (Fig. 4A). After Y. enterocolitica infection of HeLa cells, strain CT1 was unable to inject YopE into the cytoplasm (Fig. 4B). This defect was restored after transformation with either plcrVW22703 or plcrVD27 (Fig. 4B). The ability of Y. enterocolitica strains to inject effector Yops into host cells was also examined by using a HeLa cell cytotoxicity assay (Fig. 4C). The lcrV mutant strain CT1 failed to cause cell rounding and actin cable rearrangements. This defect was restored with the plasmids plcrVW22703 and plcrVD27 (Fig. 4C). Polyclonal anti-rV10 antibodies or MAb-BA5 failed to block HeLa cell cytotoxicity mediated by Y. enterocolitica CT1 harboring plcrVW22703 or plcrVD27 (Fig. 4C).
Fig 4.
Y. pestis lcrV is functional when expressed in lcrV mutant Y. enterocolitica. (A) Wild-type Y. enterocolitica W22703 (WT) and its isogenic lcrV mutant Y. enterocolitica CT1 (33), without or with plasmids expressing Y. pestis (plcrVD27) or Y. enterocolitica lcrV (plcrVW22703), were analyzed for type III secretion in TSB. Briefly, in vitro type III secretion was induced through the chelation of calcium ions, and cultures were centrifuged to separate the extracellular medium with the supernatant (S) from the bacterial pellet (P). Proteins in both samples were identified by immunoblotting with rabbit antibodies specific for type III secretion substrates (YopE, YopH, and LcrV), as well as RNA polymerase A (RpoA), which resides in bacterial cells. (B) Y. enterocolitica strains were used to infect HeLa tissue culture cells for 3 h. The culture medium (M) was centrifuged to generate supernatant (S, extracellular medium) and pellet (P, nonadherent bacteria) fractions. Cells were extracted with digitonin (D) and centrifuged to separate proteins in the supernatant (S, cytosolic extract) from the pellet (P, cellular organelles and adherent bacteria). YopE (the Yersinia type III effector), LcrV, and RpoA, as well as IκB, a HeLa cell cytoplasmic protein, were analyzed by immunoblotting. (C) HeLa cultures (2 × 105 cells) were treated with naive rabbit serum, 1 mg of polyclonal anti-rV10 rabbit antibody (anti-rV10)/ml, or 1 mg of the mouse monoclonal antibody BA5 (MAb-BA5)/ml immediately prior to infection with Y. enterocolitica CT1 harboring plcrVW22703, plcrVD27, or no plasmid, followed by incubation for 3 h. The samples were fixed, stained with rhodamine-phalloidin, and imaged by fluorescence or phase-contrast microscopy.
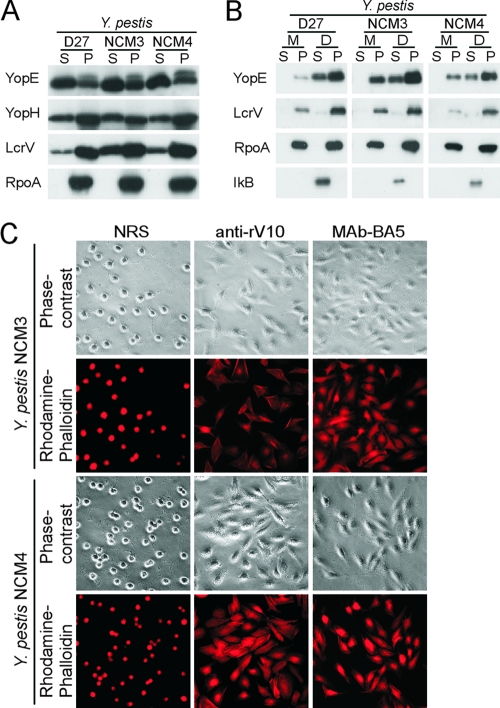
Y. pestis pCD1 variants expressing lcrVW22703 (NCM3) or lcrVWA-314 (NCM4) promote type III secretion.
To exclude the possibility of experimental artifacts introduced by multicopy plasmids, we recombined the polymorphic Y. enterocolitica lcrV alleles, lcrVW22703 and lcrVWA-314, into the pCD1 plasmid of Y. pestis KIM D27 and generated Y. pestis NCM3 (lcrVW22703) and Y. pestis NCM4 (lcrVWA-314), respectively. Type III secretion of Y. pestis cultures was induced via bacterial growth in chemically defined medium lacking calcium ions and shifting the temperature to 37°C. Compared to Y. pestis KIM D27, strains NCM3 and NCM4 expressed and secreted similar amounts of LcrV, YopE, and YopH into the culture medium (Fig. 5A). After Y. pestis infection of HeLa cells, strains KIM D27, NCM3, and NCM4 injected similar amounts of YopE into the cytoplasm of tissue culture cells (Fig. 5B). Strains KIM D27, NCM3, and NCM4 expressed similar amounts of LcrV in this assay; we noted some degradation of LcrVWA-314 secreted by strain NCM4. The ability of Y. pestis strains NCM3 and NCM4 to inject effector Yops into host cells was also examined with the HeLa cell cytotoxicity assay (Fig. 5C). Both strains caused cell rounding and actin cable rearrangements. Unlike Y. enterocolitica, the type III injection of effector Yops by NCM3 and NCM4 could be blocked with anti-rV10 and MAb-BA5 (Fig. 5C).
Fig 5.
Expression of polymorphic lcrV from the pCD1 virulence plasmid of Y. pestis KIM D27. The lcrV gene of Y. pestis KIM D27 was replaced with that of Y. enterocolitica W22703 (lcrVW22703) or Y. enterocolitica WA-314 (lcrVWA-314) via allelic exchange to generate Y. pestis strains NCM3 and NCM4, respectively. (A) The type III secretion of Y. pestis was induced through growth in a chemically defined medium lacking calcium ions; cultures were centrifuged to separate the extracellular medium with the supernatant (S) from the bacterial pellet (P). Proteins in both samples were identified by immunoblotting using rabbit antibodies specific for type III secretion substrates (YopE, YopH, and LcrV), as well as RNA polymerase A (RpoA), which resides in bacterial cells. (B) Y. pestis strains were used to infect HeLa tissue culture cells for 3 h. The culture medium (M) was centrifuged to generate supernatant (S, extracellular medium) and pellet (P, nonadherent bacteria) fractions. Cells were extracted with digitonin (D) and centrifuged to separate proteins in the supernatant (S, cytosolic extract) from the pellet (P, cellular organelles and adherent bacteria). Yersinia type III effector (YopE), secreted product (LcrV), RNA polymerase (RpoA), or HeLa cytoplasmic protein IκB was detected by immunoblotting. (C) HeLa tissue cultures were infected at an MOI of 10 with Y. pestis NCM3 or NCM4 for 3 h. Samples were fixed, stained with rhodamine-phalloidin, and imaged by fluorescence or phase-contrast microscopy. Prior to infection, tissue cultures were treated either with naive rabbit serum (NRS), 1 mg of polyclonal anti-rV10 rabbit antibody/ml, or 1 mg of MAb-BA5/ml.
Y. pestis-induced apoptosis of J774A.1 macrophages as a measure for type III injection of effector Yops.
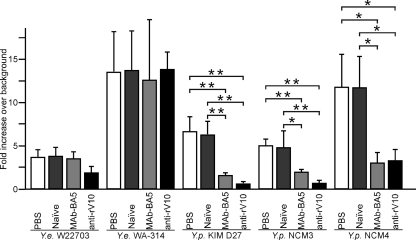
Earlier work demonstrated that Y. pestis injection of effector Yops into macrophages induces apoptosis, which serves as a quantifiable measure for protein transport via the type III pathway (28). After infection of mouse J774.1 macrophages with Y. enterocolitica or Y. pestis strains, the cultures were incubated with propidium iodide to distinguish live cells from apoptotic remnants. Compared to mock-infected cells, macrophages incubated in the presence of Y. enterocolitica strains W22703 and WA-314, as well as Y. pestis strains KIM D27, NCM3, and NCM4, all displayed a severalfold increase in apoptosis (Fig. 6). The addition of MAb-BA5 to infected macrophages had no impact on the apoptotic demise of cells infected with Y. enterocolitica strains W22703 or WA-314 (Fig. 6). Nevertheless, the monoclonal antibody reduced the type III injection of Y. pestis strains KIM D27, NCM3, and NCM4 into J774A.1 cells (Fig. 6). Similarly, polyclonal rabbit anti-rV10 antibodies caused a severalfold reduction in the type III injection of all Y. pestis strains into macrophages but did not affect Y. enterocolitica WA-314-mediated apoptosis (Fig. 6). Of note, anti-rV10 antibodies caused a 2-fold reduction in Y. enterocolitica W22703-mediated apoptosis. However, this reduction was not significant compared to cells treated with naive serum (P = 0.0615) or PBS (P = 0.051). In contrast, the reduction in apoptosis of macrophages infected with Y. pestis strains pretreated with anti-rV10 antibodies was significant (KIM D27 naive serum or PBS versus anti-rV10, P = 0.0025 and P = 0.002, respectively; NCM3 naive serum or PBS versus anti-rV10, P = 0.0063 and P = 0.001, respectively; and NCM4 naive serum or PBS versus anti-rV10, P = 0.0365 and P = 0.043, respectively).
Fig 6.
Y. pestis-induced apoptosis of J774.1 macrophages can be prevented with anti-rV10 or MAb-BA5 antibodies. Y. enterocolitica W22703, Y. enterocolitica WA-314, Y. pestis KIM D27, Y. pestis NCM3, and Y. pestis NCM4 were used to infect J774.1 macrophages at an MOI of 10 in the absence or presence of 1 mg of anti-rV10 or MAb-BA5 antibody. Samples were stained with propidium iodide to identify and enumerate apoptotic remnants of macrophages. The data from at least three independent determinations with more than 1,000 cells counted for each condition were averaged, and the standard errors of the means were calculated. Control conditions (naive serum and PBS) were compared individually to each specific test condition. The statistical significance was calculated using two-tailed unpaired Student's t test comparing PBS (mock) or naive serum samples with anti-rV10 or MAb-BA5 (*, P < 0.05; **, P < 0.01).
Y. pestis strains expressing polymorphic lcrV are virulent in mice.
Nonpigmented plague strains such as Y. pestis KIM D27 retain the ability to cause septicemic plague when injected into the bloodstreams of immunocompetent animals (35). To examine the virulence attributes of Y. pestis KIM D27 variants expressing polymorphic lcrV, BALB/c mice (n = 10) were infected with 102 or 104 CFU of plague bacteria and monitored for septicemic plague morbidity. All animals infected with 104 CFU of Y. pestis KIM D27, NCM3, or NCM4 succumbed to septicemic plague disease within 3 to 6 days of challenge (Fig. 7A). Animals infected with 102 CFU displayed variable degrees of morbidity. Y. pestis KIM D27 caused 50% mortality, whereas strains NCM3 (60%) and NCM4 (80%) killed larger numbers of animals; these differences were not statistically significant (Fig. 7A).
Fig 7.

Polymorphisms in the lcrV gene of Y. enterocolitica do not provide for escape from plague protective immunity. (A) Polymorphic lcrV genes from Y. enterocolitica W22703 (lcrVW22703) or Y. enterocolitica WA-314 (lcrVWA-314) are functional when expressed from the pCD1 plasmid of Y. pestis KIM D27. BALB/c mice (n = 10) were inoculated intravenously with 102 or 104 CFU of Y. pestis KIM D27, Y. pestis NCM3, or Y. pestis NCM4, and animal survival was monitored over 14 days. Statistical significance of animal survival following challenge with 102 CFU was examined with the log-rank test: KIM D27 versus NCM3, P = 0.9188; KIM D27 versus NCM4, P = 0.6313; and NCM3 versus NCM4, P = 0.7137. The data were reproduced with a second, independent experimental determination. (B) Naive BALB/c mice were passively immunized by intraperitoneal injection with 200 μl of rabbit serum derived from a naive rabbit (NRS), a rabbit immunized with rLcrV (α-LcrV), or a rabbit immunized with rV10 (α-V10). One hour later, the animals were challenged by intravenous injection with 2 × 103 CFU of Y. pestis KIM D27, Y. pestis NCM3, or Y. pestis NCM4. The mice were monitored for mortality over 14 days after infection. The statistical significance of animal survival was examined with the log-rank test: for KIM D27, NRS versus α-LcrV, P = 0.0035, and NRS versus α-V10, P = 0.0035; for NCM3, NRS versus α-LcrV, P = 0.0035, and NRS versus α-V10, P = 0.0035; and for NCM4, NRS versus α-LcrV, P = 0.0023, and NRS versus α-V10, P = 0.0023. The data were reproduced with a second, independent experimental determination.
LcrV-specific antibodies protect mice against plague challenge with Y. pestis strains expressing polymorphic lcrV.
Rabbit antisera raised against purified LcrVD27 or rV10 (46) were injected into the peritoneal cavities of BALB/c mice (n = 10). Compared to control animals, which received serum from a naive rabbit (NRS), passive transfer of rLcrV- or rV10-specific antibodies provided BALB/c mice with protection against lethal septicemic plague challenge with 2 × 103 CFU of Y. pestis strains KIM D27, NCM3, or NCM4 (Fig. 7B). Passive transfer of diluted anti-rV10 rabbit serum into BALB/c mice was used to test for differences in vaccine protection against Y. pestis strains expressing lcrVKIM D27 (KIM D27) or lcrVWA-314 (NCM4). Passively immunized animals displayed the same level of vaccine protection against both nonpigmented plague strains (Table 3). These data suggest that the expression of polymorphic lcrV from Y. enterocolitica does not affect the virulence of Y. pestis strains or the protective immunity of animals endowed with antibodies raised against Y. pestis LcrV.
Table 3.
rV10 antibody protection against intravenous challenge with nonpigmented plague strainsa
| Y. pestis challenge strainb | Mouse mortality (no. of surviving animals/total no. of animals) |
||||
|---|---|---|---|---|---|
| NRS (undiluted) | Dilution of anti-rV10 rabbit serum passively transferred into mice |
||||
| Undiluted | 1:50 | 1:500 | 1:1,000 | ||
| KIM D27 | 0/5 | 5/5 | 9/10 | 0/10 | 0/10 |
| NCM4 | 0/5 | 5/5 | 9/10 | 0/10 | 0/10 |
Naive BALB/c mice were passively immunized by intraperitoneal injection with 200 μl of rabbit serum derived from a naive rabbit (NRS) or with 200 μl of either undiluted serum or a 1:50, 1:500, or 1:1,000 dilution of serum in PBS from a rabbit that had been hyperimmunized with rV10 (anti-rV10). Mice were monitored for mortality (expressed as the number of surviving animals/number of animals in cohort) over 14 days after infection. Statistically significant differences in survival (KIM D27 versus NCM4) were not detected when the data were analyzed with the log-rank test.
At 1 h after the passive transfer of serum, the animals were challenged by intravenous injection with 5 × 104 CFU of Y. pestis KIM D27 or Y. pestis NCM4 as indicated.
DISCUSSION
Y. pestis, the causative agent of plague, is a zoonotic pathogen that in the United States is endemic in rodent populations west of the 100° meridian, sporadically transmitting disease to humans via flea bite, direct contact, or aerosol transmission (43). Plague is a global disease, endemic in many countries with unique rodent reservoirs, claiming approximately 1,000 to 3,000 lives worldwide each year. During epidemic outbreaks, the disease can spread by aerosol or arthropod vector transmission at a rapid pace through countries and continents, which has earned Y. pestis a reputation as one of the most lethal and dangerous infectious disease agents (29).
Vaccine protection against plague has been sought for centuries (49). Considering the possibility of an illegitimate use of Y. pestis as a weapon, the ultimate research goal is the development of a vaccine that cannot be defeated by naturally occurring or engineered mutational variants (49). Live-attenuated vaccine strains, lacking the HPI/pgm locus, generate protective immunity against plague; however, this immunity is based on capsular fraction 1 (Caf1 or F1)-specific antibodies that interfere with the type III injection of immune cells by this pathogen (46). Mutations that abrogate caf1 expression or F1 pilus assembly can occur spontaneously, either due to random mutagenesis (25) or via IS1541 insertional inactivation of a structural gene (caf1A) that resides on the pFra virulence plasmid of plague bacteria (20). The resulting mutants could escape the natural immunity of plague survivors or individuals immunized with the live-attenuated strain and cause lethal plague in immune individuals (20). For these reasons, Caf1 (F1) cannot be used as a sole plague vaccine antigen.
Y. pestis expression of lcrV and the assembly of functional type III secretion needles with LcrV at their tip are absolutely essential molecular events during the pathogenesis of plague, i.e., bubonic and pneumonic plague (8, 37, 44). Antibodies directed against LcrV can block Y. pestis type III injection of host immune cells, allowing phagocytes to escape the paralyzing and intoxicating action of type III needles to subsequently phagocytose and kill the invading pathogen (22, 60). Positive correlation between the presence of LcrV-specific antibody and protective immunity in vitro or in experimental animals can be used as a measure for vaccine efficacy in human volunteers (57). Nevertheless, the important question of whether LcrV-mediated protective immunity can be defeated by naturally occurring or engineered lcrV variants has thus far not been addressed. Early studies by Motin et al. revealed that antibodies against Y. pestis LcrV cannot block the virulence of the Y. enterocolitica O:8 strain WA-314 (36). Here, we corroborated this finding and extended it to Y. enterocolitica O:9 strain W22703. The lcrV genes of O:8 and O:9 strains harbor a number of codon changes compared to the lcrV gene of Y. pestis, most of them located in a region encoding the hypervariable loop (resides 225 to 232) (50). Taken together, these earlier observations suggested that Y. enterocolitica lcrV products may provide for escape from LcrV-mediated immunity against plague if they can be functionally expressed in Y. pestis.
This possibility was addressed here. Our initial findings showed that antibodies generated against LcrVD27 were unable to prevent in vitro type III injection into HeLa cells by either Y. enterocolitica W22703 or Y. enterocolitica WA-314. We found that the Y. enterocolitica W22703 (O:9) and WA-314 (O:8) lcrV genes can indeed complement the lcrV mutation of Y. pestis in strain KLD29 to restore the lcrV-regulated phenotypes on in vitro type III secretion or type III injection of tissue culture cells by plague bacteria. Further, Y. pestis strains engineered to express lcrVW22703 or lcrVWA-314 display virulence in a mouse model for septicemic plague. The critical experiment, whether Y. pestis LcrVD27-specific antibodies block the type III injection and virulence of plague strains harboring lcrVW22703 or lcrVWA-314, suggested no significant difference in protective immunity regardless of which lcrV allele was expressed. These data suggest that polymorphisms in the lcrV gene may not provide for Y. pestis escape from LcrV-mediated plague immunity.
We considered the possibility that Y. enterocolitica type III injection occurs by a mechanism that cannot be blocked by LcrV antibodies directed against Y. pestis LcrV. In such a scenario, even the expression of lcrVD27 in lcrV mutant Y. enterocolitica cannot lead to a block in type III injection; this was indeed observed. Nevertheless, lcrVD27 restored the functional defects of lcrV mutant Y. enterocolitica CT1 and the ability to catalyze type III injection of tissue culture cells. Why then are Y. enterocolitica type III needles decorated with LcrV at least partially refractory to the blocking effects of LcrV-specific antibodies? We do not know the answer to this question. Our current efforts at modeling the mechanism of type III injection assumes that needles harboring LcrV at their tips represent a functional state of the secretion machine that is not engaged in the transport of effectors (YopE, YopH, and others). The structural features of type III needles that have inserted into the plasma membrane of host cells and are fully engaged in effector transport have not yet been revealed (37). Molecular genetic studies and in vitro biochemical work report the association between LcrV, YopB, and YopD, all of which are required at the same stage of type III injection (7, 27, 52). We think it may be plausible that LcrV-specific antibodies prevent positional changes of the molecule associated with opening the tip of the needle for subsequent transport of type III effectors or prevent physical associations between LcrV and the two translocation factors YopB and YopD (26). Whatever the mechanism of the anti-LcrV-mediated blockade of type III injection, there must exist subtle differences between Y. pestis and Y. enterocolitica that determine the generic resistance of the latter type III pathway to antibodies raised against Y. pestis LcrV.
ACKNOWLEDGMENTS
We thank members of our laboratory for critical comments and discussion, Hwan Kim for help with statistical analysis, and the Animal Research and Immunology Core (University of Chicago) for assistance with animal experiments.
The authors acknowledge membership within and support from the Region V “Great Lakes” Regional Center of Excellence in Biodefense and Emerging Infectious Diseases Consortium (NIH award 1-U54-AI-057153). This study supported in part by the NIH/NIAID Challenge Award U01-AI070559 “LcrV Plague Vaccine with Altered Immune Modulatory Properties.”
Footnotes
Published ahead of print 17 January 2012
The authors have paid a fee to allow immediate free access to this article.
REFERENCES
- 1. Anderson DA, et al. 2009. Pneumonic plague pathogenesis and immunity in brown Norway rats. Am. J. Pathol. 174:910–921 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Autenrieth IB, Beer M, Bohn E, Kaufmann SH, Heesemann J. 1994. Immune responses to Yersinia enterocolitica in susceptible BALB/c and resistant C57BL/6 mice: an essential role for gamma interferon. Infect. Immun. 62:2590–2599 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Baker EE, Sommer H, Foster LE, Meyer E, Meyer KF. 1947. Antigenic structure of Pasteurella pestis and the isolation of a crystalline antigen. Proc. Soc. Exp. Biol. 64:139–141 [DOI] [PubMed] [Google Scholar]
- 4. Baker EE, Sommer H, Foster LE, Meyer E, Meyer KF. 1952. Studies on immunization against plague. I. The isolation and characterization of the soluble antigen of Pasteurella pestis. J. Immunol. 68:131–145 [PubMed] [Google Scholar]
- 5. Begier EM, et al. 2006. Pneumonic plague cluster, Uganda, 2004. Emerg. Infect. Dis. 12:460–467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Boisier P, et al. 2002. Epidemiologic features of four successive annual outbreaks of bubonic plague in Mahajanga, Madagascar. Emerg. Infect. Dis. 8:311–316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Boland A, et al. 1996. Status of YopM and YopN in the Yersinia yop virulon: YopM of Y. enterocolitica is internalized inside the cytosol of PU5-1.8 macrophages by the YopB, D, N delivery apparatus. EMBO J. 15:5191–5201 [PMC free article] [PubMed] [Google Scholar]
- 8. Broz P, et al. 2007. Function and molecular architecture of the Yersinia injectisome tip complex. Mol. Microbiol. 65:1311–1320 [DOI] [PubMed] [Google Scholar]
- 9. Brubaker RR. 1969. Mutation rate to non-pigmentation in Pasteurella pestis. J. Bacteriol. 98:1404–1406 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Burrows TW. 1956. An antigen determining virulence in Pasteurella pestis. Nature 177:426–427 [DOI] [PubMed] [Google Scholar]
- 11. Burrows TW. 1957. Virulence of Pasteurella pestis. Nature 179:1246–1247 [DOI] [PubMed] [Google Scholar]
- 12. Burrows TW, Bacon GA. 1958. The effect of loss of different virulence determinants on the virulence and immunogenicity of strains of Pasteurella pestis. Br. J. Exp. Pathol. 39:278–291 [PMC free article] [PubMed] [Google Scholar]
- 13. Butler T. 1995. Yersinia species, p 1748–1756 In Mandell GL, Douglas RG, Bennett JE. (ed), Infectious diseases, 5th ed Churchill Livingstone, New York, NY [Google Scholar]
- 14. Cheng LW, Anderson DM, Schneewind O. 1997. Two independent type III secretion mechanisms for YopE in Yersinia enterocolitica. Mol. Microbiol. 24:757–765 [DOI] [PubMed] [Google Scholar]
- 15. Cornelis GR. 2006. The type III injectisome. Nat. Rev. Microbiol. 4:811–825 [DOI] [PubMed] [Google Scholar]
- 16. Cornelis GR. 2002. Yersinia type III secretion: send in the effectors. J. Cell Biol. 158:401–408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Cornelis GR, et al. 1998. The virulence plasmid of Yersinia, an antihost genome. Microbiol. Mol. Biol. Rev. 62:1315–1352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Cornelis GR, Colson C. 1975. Restriction of DNA in Yersinia enterocolitica detected by the recipient ability for a derepressed R factor from Escherichia coli. J. Gen. Microbiol. 87:285–291 [DOI] [PubMed] [Google Scholar]
- 19. Cornelius CA, Quenee LE, Elli D, Ciletti NA, Schneewind O. 2008. V10 subunit vaccine protects cynomolgus macaques from lethal pneumonic plague. Infect. Immun. 76:5588–5597 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Cornelius CA, Quenee LE, Elli D, Ciletti NA, Schneewind O. 2009. Yersinia pestis IS1541 transposition provides for escape from plague immunity. Infect. Immun. 77:1807–1816 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. DeBord K, Lee VT, Schneewind O. 2001. On the role of LcrG and LcrV during the type III targeting of effector Yops by Yersinia enterocolitica. J. Bacteriol. 183:4588–4598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. DeBord KL, et al. 2006. Immunogenicity and protective immunity against bubonic and pneumonic plague by immunization of mice with the recombinant V10 antigen, a variant of LcrV. Infect. Immun. 74:4910–4914 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. DePaolo RW, et al. 2008. TLR6 drives differentiation of tolerogenic dendritic cells and contributes to LcrV-mediated plague pathogenesis. Cell Host Microbe 4:350–361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Ellison DW, Lawrenz MB, Miller VL. 2004. Invasin and beyond: regulation of Yersinia virulence by RovA. Trends Microbiol. 12:296–300 [DOI] [PubMed] [Google Scholar]
- 25. Friedlander AM, et al. 1995. Relationship between virulence and immunity as revealed in recent studies of the F1 capsule of Yersinia pestis. Clin. Infect. Dis. 21:S178–S181 [DOI] [PubMed] [Google Scholar]
- 26. Goure J, Broz P, Attree O, Cornelius GR, Attree I. 2005. Protective anti-V antibodies inhibit Pseudomonas and Yersinia translocon assembly within host membranes. J. Infect. Dis. 192:218–225 [DOI] [PubMed] [Google Scholar]
- 27. Hakansson S, Bergman T, Vanooteghem J-C, Cornelis G, Wolf-Watz H. 1993. YopB and YopD constitute a novel class of Yersinia Yop proteins. Infect. Immun. 61:71–80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Hill J, et al. 2009. N255 is a key residue for recognition by a monoclonal antibody which protects against Yersinia pestis infection. Vaccine 27:7073–7079 [DOI] [PubMed] [Google Scholar]
- 29. Inglesby TV, et al. 2000. Plague as a biological weapon: medical and public health management. JAMA 283:2281–2290 [DOI] [PubMed] [Google Scholar]
- 30. Inglesby TV, Grossman R, O'Toole T. 2001. A plague on your city: observations from TOPOFF. Clin. Infect. Dis. 32:436–445 [DOI] [PubMed] [Google Scholar]
- 31. Jacobs MK. 2004. The history of biologic warfare and bioterrorism Dermatol. Clin. 22:231–246 [DOI] [PubMed] [Google Scholar]
- 32. Lee VT, Anderson DM, Schneewind O. 1998. Targeting of Yersinia Yop proteins into the cytosol of HeLa cells: one-step translocation of YopE across bacterial and eukaryotic membranes is dependent on SycE chaperone. Mol. Microbiol. 28:593–601 [DOI] [PubMed] [Google Scholar]
- 33. Lee VT, Tam C, Schneewind O. 2000. LcrV, a substrate for Yersinia enterocolitica type III secretion, is required for toxin targeting into the cytosol of HeLa cells. J. Biol. Chem. 275:36869–36875 [DOI] [PubMed] [Google Scholar]
- 34. Marketon MM, DePaolo RW, DeBord KL, Jabri B, Schneewind O. 2005. Plague bacteria target immune cells during infection. Science 309:1739–1741 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Meyer KF, Smith G, Foster L, Brookman M, Sung MH. 1974. Live, attenuated Yersinia pestis vaccine: virulent in non-human primates, harmless to guinea pigs. J. Infect. Dis. 129:S85–S112 [DOI] [PubMed] [Google Scholar]
- 36. Motin VL, Nakajima R, Smirvov GB, Brubaker RR. 1994. Passive immunity to yersiniae mediated by anti-recombinant V antigen and Protein A-V antigen fusion peptide. Infect. Immun. 62:4192–4201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Mueller CA, Broz P, Cornelis GR. 2008. The type III secretion system tip complex and translocon. Mol. Microbiol. 68:1085–1095 [DOI] [PubMed] [Google Scholar]
- 38. Mueller CA, et al. 2005. The V-antigen of Yersinia forms a distinct structure at the tip of injectisome needles. Science 310:674–676 [DOI] [PubMed] [Google Scholar]
- 39. Nakajima R, Brubaker RR. 1993. Association between virulence of Yersinia pestis and suppression of gamma interferon and tumor necrosis factor alpha. Infect. Immun. 61:23–31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Nakajima R, Motin VL, Brubaker RR. 1995. Suppression of cytokines in mice by protein A-V antigen fusion peptide and restoration of synthesis by active immunization. Infect. Immun. 63:3021–3029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Nilles ML, Williams AW, Skrzypek E, Straley SC. 1997. Yersinia pestis LcrV forms a stable complex with LcrG and may have a secretion-related regulatory role in the low-Ca2+ response. J. Bacteriol. 179:1307–1316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Overheim KA, et al. 2005. LcrV plague vaccine with altered immunomodulatory properties. Infect. Immun. 73:5152–5159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Perry RD, Fetherston JD. 1997. Yersinia pestis: etiologic agent of plague. Clin. Microbiol. Rev. 10:35–66 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Perry RD, Harmon PA, Bowmer WS, Straley SC. 1986. A low-Ca2+ response operon encodes the V antigen of Yersinia pestis. Infect. Immun. 54:428–434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Petterson J, et al. 1999. The V-antigen of Yersinia is surface exposed before target cell contact and involved in virulence protein translocation. Mol. Microbiol. 32:961–976 [DOI] [PubMed] [Google Scholar]
- 46. Quenee L, Cornelius CA, Ciletti NA, Elli D, Schneewind O. 2008. Yersinia pestis caf1 (F1) variants and the limits of plague vaccine protection. Infect. Immun. 76:2025–2036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Quenee LE, et al. 2010. Amino acid residues 196–225 of LcrV represent a plague protective epitope. Vaccine 28:1870–1876 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Quenee LE, Ciletti NA, Elli D, Hermanas T, Schneewind O. 2011. Prevention of pneumonic plague in mice, rats, guinea pigs and non-human primates with clinical grade rV10, rV10-2, or F1-V vaccines. Vaccine 29:6572–6583 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Quenee LE, Schneewind O. 2009. Plague vaccines and the molecular basis of immunity against Yersinia pestis. Hum. Vaccines 5:817–823 [DOI] [PubMed] [Google Scholar]
- 50. Roggenkamp A, Geiger AM, Leitritz L, Kessler A, Heesemann J. 1997. Passive immunity to infection with Yersinia spp. mediated by recombinant V antigen is dependent on polymorphism of V antigen. Infect. Immun. 65:446–451 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Rosqvist R, Forsberg A, Rimpilainen M, Bergman T, Wolf-Watz H. 1990. The cytotoxic protein YopE of yersinia obstructs the primary host defense. Mol. Microbiol. 4:657–667 [DOI] [PubMed] [Google Scholar]
- 52. Rosqvist R, Magnusson K-E, Wolf-Watz H. 1994. Target cell contact triggers expression and polarized transfer of Yersinia YopE cytotoxin into mammalian cells. EMBO J. 13:964–972 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Simond PL. 1898. La propagation de la peste. Ann. Inst. Pasteur 12:625–687 [Google Scholar]
- 54. Skrzypek E, Straley SC. 1995. Differential effects of deletions in lcrV on secretion of V antigen, regulation of the low-Ca2+ response, and virulence of Yersinia pestis. J. Bacteriol. 177:2530–2542 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Sorg JA, Miller NC, Marketon MM, Schneewind O. 2005. Rejection of impassable substrates by Yersinia type III secretion machines. J. Bacteriol. 187:7090–7102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Weeks S, Hill J, Friedlander A, Welkos S. 2002. Anti-V antigen antibody protects macrophages from Yersinia pestis-induced cell death and promotes phagocytosis. Microb. Pathog. 32:227–237 [DOI] [PubMed] [Google Scholar]
- 57. Williamson ED, et al. 2005. Human immune response to a plague vaccine comprising recombinant F1 and V antigens. Infect. Immun. 73:3598–3608 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Worsham PL, Stein MP, Welkos SL. 1995. Construction of defined F1 negative mutants of virulent Yersinia pestis. Contrib. Microbiol. Immunol. 13:325–328 [PubMed] [Google Scholar]
- 59. Yersin A. 1894. La peste bubonique à Hong-Kong. Ann. Inst. Pasteur 2:428–430 [Google Scholar]
- 60. Zauberman A, et al. 2008. Neutralization of Yersinia pestis-mediated macrophage cytotoxicity by anti-LcrV antibodies and its correlation with protective immunity in a mouse model of bubonic plague. Vaccine 26:1616–1625 [DOI] [PubMed] [Google Scholar]
- 61. Zavialov AV, et al. 2003. Structure and biogenesis of the capsular F1 antigen from Yersinia pestis: preserved folding energy drives fiber formation. Cell 113:587–596 [DOI] [PubMed] [Google Scholar]