Abstract
Vaccination using “naked” DNA is a highly attractive strategy for induction of pathogen-specific immune responses; however, it has been only weakly immunogenic in humans. Previously, we constructed DNA-launched Semliki Forest virus replicons (DREP), which stimulate pattern recognition receptors and induce augmented immune responses. Also, in vivo electroporation was shown to enhance immune responses induced by conventional DNA vaccines. Here, we combine these two approaches and show that in vivo electroporation increases CD8+ T cell responses induced by DREP and consequently decreases the DNA dose required to induce a response. The vaccines used in this study encode the multiclade HIV-1 T cell immunogen HIVconsv, which is currently being evaluated in clinical trials. Using intradermal delivery followed by electroporation, the DREP.HIVconsv DNA dose could be reduced to as low as 3.2 ng to elicit frequencies of HIV-1-specific CD8+ T cells comparable to those induced by 1 μg of a conventional pTH.HIVconsv DNA vaccine, representing a 625-fold molar reduction in dose. Responses induced by both DREP.HIVconsv and pTH.HIVconsv were further increased by heterologous vaccine boosts employing modified vaccinia virus Ankara MVA.HIVconsv and attenuated chimpanzee adenovirus ChAdV63.HIVconsv. Using the same HIVconsv vaccines, the mouse observations were supported by an at least 20-fold-lower dose of DNA vaccine in rhesus macaques. These data point toward a strategy for overcoming the low immunogenicity of DNA vaccines in humans and strongly support further development of the DREP vaccine platform for clinical evaluation.
INTRODUCTION
“Naked” DNA constitutes an attractive vaccine platform for delivery of pathogen- or cancer-derived immunogens. Three veterinary DNA vaccines have been licensed for use in dogs, salmon, and horses, demonstrating that DNA vaccines are capable of inducing protective immunity (8, 48). In humans, plasmid DNA vaccines have been shown to be safe and well tolerated in thousands of volunteers (14, 41, 48); however, their strong immunogenicity observed in smaller animals does not transfer to primates, including humans. Thus, the potency of DNA vaccines in humans must be significantly improved for the vaccines to become a practical and commercially attractive health care tool.
The use of in vivo electroporation (EP) was shown to improve DNA transfection into cells at the site of injection and to promote local inflammation, thereby increasing the immunogenicity of DNA vaccines (7, 18, 37, 39). Safety and tolerability of intramuscular (i.m.) and intradermal (i.d.) DNA EP were demonstrated in both preclinical and clinical settings (28, 49, 51). Although the i.m. delivery route has been more extensively studied, i.d. EP offers an attractive route of delivery due to the characteristics of the skin, with many resident antigen-presenting cells such as Langerhans and dermal dendritic cells. Intradermal EP is also considerably less painful, and any possible residual pain may be further controlled by topical anesthetics (38, 48).
The DNA vaccine vector can be constructed so that it itself carries intrinsic adjuvant properties. We and others have previously constructed DNA replicon (DREP) vectors based on alphaviruses such as Semliki Forest virus (SFV) (5, 33), Sindbis virus (10, 16), and Venezuelan equine encephalitis virus (VEE) (27). Transfection with DREP results in production of an mRNA that is self-amplifying due to the presence of the genes encoding the alphavirus replicase. RNA amplification occurs in the cytoplasm and results in the production of RNA intermediates that can stimulate pattern recognition receptors (PRRs) such as the endosomal Toll-like receptor 3 (TLR3) (44) and TLR7 and TLR8 (35). Cytoplasmic PRRs such as the melanoma differentiation-associated gene 5 product (MDA-5) (45) and RNA-activated protein kinase (PKR) (3, 50) are also activated. PRR signaling leads to production of large amounts of type I interferons (IFNs) (17) and apoptosis (4, 11) and promotes antigen-specific adaptive immune responses (21, 31). In mice, DREP has been shown to be more potent than conventional plasmid DNA vaccines in inducing antigen-specific CD8+ T cell and antibody responses (5, 16, 27, 33).
To further increase immunogenicity, nonreplicating vaccines such as plasmid DNA are often combined into prime-boost regimens with other heterologous vectors delivering a common, pathogen-derived immunogen (26, 34, 36, 42). This maximizes the induction of transgene-specific responses while avoiding buildup of antivector immunity (43). While simple vaccine modalities are better for priming, more complex vectors such as poxviruses (12–14, 29, 41) and adenoviruses (22) excel in boosting. Currently, numerous prime-boost regimens are in both preclinical and clinical development.
In this study, we compared the elicitation of HIV-1-specific T cell responses by novel plasmid pTH.HIVconsv and SFV-based replicon DREP.HIVconsv DNA vaccines and assessed whether or not the use of skin EP as a means of the DREP.HIVconsv delivery further increases the vaccine-induced T cell frequencies. HIVconsv is a second-generation T cell immunogen designed to deal with HIV-1 variability and escape by focusing immune responses on the conserved regions of the HIV-1 proteome (25, 40). These conventional plasmid or replicon DNA-primed responses were boosted by two heterologous vaccines modalities that are currently being evaluated in clinical trials, modified vaccinia virus Ankara MVA.HIVconsv or attenuated chimpanzee adenovirus ChAdV63.HIVconsv (25, 40). The results are discussed in the context of current HIV-1 vaccine development.
MATERIALS AND METHODS
Preparation of DNA vaccines.
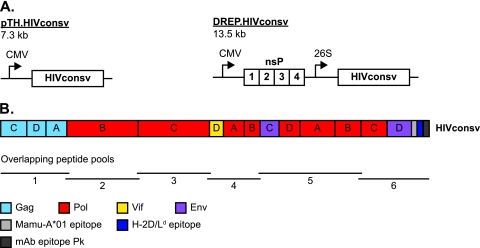
Two DNA constructs were used in these studies: pTH.HIVconsv, which has been described previously (25), and DREP.HIVconsv (Fig. 1A). DREP.HIVconsv was generated by excising the HIVconsv gene from pTH.HIVconsv and inserting it into digested DREP-NP (5, 33). Plasmids were prepared using the EndoFree Plasmid Giga kit (Qiagen, Hilden, Germany) and dissolved in phosphate-buffered saline (PBS) (Gibco, Invitrogen, Paisley, United Kingdom). A Limulus amebocyte lysate test (performed by the Swedish Institute for Communicable Disease Control, Stockholm, Sweden) showed that endotoxin levels were <0.005 endotoxin units (EU)/μg DNA in all DNA preparations.
Fig 1.
DNA constructs and HIVconsv immunogen. (A) Schematic illustration of DNA constructs pTH.HIVconsv and DREP.HIVconsv. CMV, cytomegalovirus promoter; nsP, nonstructural proteins (replicase); 26S, subgenomic 26S promoter. (B) Schematic illustration of the HIVconsv immunogen indicating clade alternation, overlapping peptide pool derivation, and protein origin by color coding.
Preparation of virus vaccines.
Production of VREP.HIVconsv (40), MVA.HIVconsv (25), and ChAdV63.HIVconsv (40) was performed as described previously.
Metabolic (pulse-chase) labeling.
Baby hamster kidney (BHK-21) cells were cultured in Glasgow BHK-21 minimal essential medium supplemented with 5% fetal calf serum (FCS), 10% tryptose phosphate broth, 10 mM HEPES, 2 mM l-glutamine, 0.1 U/ml penicillin, and 0.1 μg/ml streptomycin (all from Gibco, Invitrogen). Cells were infected with VREP.HIVconsv at a multiplicity of infection of 20, incubated overnight, starved for 30 min with minimum essential medium Eagle (MEM) lacking methionine (MP Biomedicals, Illkirch, France) and supplemented with 2 mM l-glutamine and 10 mM HEPES, and pulsed for 10 min with the same medium supplemented with 100 μCi/ml [35S]methionine. Cells were then washed and incubated with chase medium (MEM supplemented with 2 mM l-glutamine, 10 mM HEPES, and 150 μg/ml unlabeled methionine) for 15 min, 30 min, 1 h, 2 h, or 4.5 h. Lysis buffer (1% NP-40, 50 mM Tris-HCl [pH 7.6], 150 mM NaCl, 2 mM EDTA, 1 μg/μl phenylmethylsulfonyl fluoride, 10 mM iodoacetamide) was then added, and total cell lysates were collected. Protein contents in cell lysates were quantified with a bicinchoninic acid (BCA) protein assay kit (Thermo Scientific, Rockford, IL), and an equal amount of protein from each sample was analyzed on a denaturing gel (4 to 12% NuPAGE Novex Bis-Tris gel; Invitrogen). A Rainbow 14C-methylated protein molecular weight marker (Amersham, GE Healthcare, Buckinghamshire, England) was additionally run on the gel as a reference. The gel was then soaked in a 1 M sodium salicylate (Merck, Darmstadt, Germany) bath for 20 min. After the gel was dried, radioactive proteins were detected on an X-ray film (Fujifilm, Düsseldorf, Germany).
Mice.
Mice were bred and kept at the animal facility at the Department of Microbiology, Tumor and Cell Biology at Karolinska Institutet, Sweden. Female BALB/c mice were 6 to 12 weeks old at the initiation of experiments. Care and treatment of mice were in accordance with standards defined by the local ethics committee, Stockholms Norra Djurförsöksetiska Nämnd.
Mouse immunizations and in vivo EP.
Mice were immunized i.m. in the hind legs in the gastrocnemius muscle with either DREP.HIVconsv, pTH.HIVconsv, MVA.HIVconsv, or ChAdV63.HIVconsv. Prior to immunization, MVA.HIVconsv was sonicated in a water bath for 2 min. DREP.HIVconsv, pTH.HIVconsv, and MVA.HIVconsv were diluted in PBS and then administered in a volume of 100 μl per mouse. For ChAdV63.HIVconsv, 50 μl per mouse was given. The administered volume was divided equally between the two hind legs. Administered doses are indicated in the figure legends.
For i.d. immunization with or without in vivo EP, a small area at the base of the tail was shaved to allow for visualization of the skin as well as proper electrode insertion. Mice were then anesthetized with isoflurane, and 40 μl of pTH.HIVconsv or DREP.HIVconsv diluted in PBS was injected into two sites (20 μl each) within the shaved area using a 30-gauge insulin-grade syringe (BD Micro-Fine; BD Consumer Healthcare, Franklin Lakes, NJ). For EP, a needle array electrode was placed at the injected spot immediately after injection of DNA, and voltage was applied (2 pulses of 1,125 V/cm for 50 μs followed by 8 pulses of 275 V/cm for 10 ms). The electrode contained two parallel rows of four 2-mm pins (1.5- by 4-mm gaps) (Cellectis, Paris, France [formerly Cyto Pulse Sciences, Glen Burnie, MD]), and EP was performed using the DermaVax DNA vaccine skin delivery system (Cellectis Therapeutics).
Isolation of mouse splenocytes.
Single-cell suspensions were obtained by mashing fresh mouse spleens through 70-μm nylon cell strainers. Cells were washed in complete RPMI medium (RPMI 1640 supplemented with 5% FCS, 2 mM l-glutamine, 100 U/ml penicillin, and 100 μg/ml streptomycin [all from Gibco, Invitrogen]) and then treated with red blood cell lysis buffer (Sigma-Aldrich, St. Louis, MO) for 2 min and washed and resuspended in complete RPMI medium. Trypan blue was used for quantification of viable cells.
Rhesus macaques, vaccination, and isolation of PBMCs.
Eight adult Indian rhesus macaques (Macaca mulatta) were obtained from a breeding colony in the United Kingdom. Four macaques per group received the following vaccinations: 3 4-mg doses of pTH.HIVconsv i.m. or 3 400-μg doses of DREP.HIVconsv i.m., followed by 108 PFU of MVA.HIVconsv i.m. and 1010 viral particles (vp) of attenuated simian E3-deleted ChAdV63.HIVconsv i.m. Macaque peripheral blood mononuclear cells (PBMCs) were isolated using Lymphoprep cushion centrifugation (Nycomed Pharma) and were then either used fresh or cryopreserved in liquid nitrogen until use. All animal procedures and care strictly conformed to the United Kingdom Home Office guidelines. Experiments were conducted in the spirit of the National Center for the Replacement, Refinement, and Reduction of Animals in Research.
IFN-γ ELISpot assay.
The frequencies of cells that released IFN-γ upon restimulation with HIVconsv-derived peptides were assessed using an enzyme-linked immunosorbent spot (ELISpot) assay.
For mouse experiments, MultiScreen-IP plates (Millipore, Billerica, MA) were activated with 70% ethanol, washed four times with PBS, and coated with anti-IFN-γ antibodies (AN18; Mabtech, Nacka Strand, Sweden) diluted in PBS overnight at 4°C as recommended by the manufacturer. Plates were then washed five times with PBS and blocked with complete RPMI medium for at least 2 h at 37°C. Next, blocking medium was replaced by freshly isolated splenocytes at 1 × 105 or 2 × 105 cells/well with 2 μg/ml of RGPGRAFVTI peptide (ProImmune, Oxford, United Kingdom) or medium alone in triplicates or 2 μg/ml of concanavalin A (Sigma-Aldrich) in duplicates. After 20 h of incubation at 37°C with 5% CO2, plates were washed 6 times with PBS-Tween (0.05%) and incubated with a biotinylated anti-IFN-γ detector antibody (R4-6A2; Mabtech) for 2 h at room temperature. Plates were then washed as described above, and an avidin-peroxidase complex (ABC kit; Vector Laboratories, Peterborough, United Kingdom) was prepared according to the manufacturer's instructions and added. After 1 h of incubation at room temperature, plates were washed 6 times with PBS, and a 3-amino-9-ethylcarbazole (Sigma-Aldrich) substrate was added to the wells. After 4 min, the plates were washed with water to stop the enzymatic reaction. Plates were analyzed using the ImmunoSpot analyzer and ImmunoSpot software (Cellular Technology Ltd., Bonn, Germany).
In experiments with macaques, the procedures and reagents of a commercially available kit (Mabtech) were used throughout. For peptide stimulation, 199 80% pure 15-mer peptides overlapping by 11 amino acids and spanning the entire HIVconsv protein were generously provided by the International AIDS Vaccine Initiative. Individual peptides were dissolved in dimethyl sulfoxide (DMSO) (Sigma-Aldrich) to yield a stock of 40 mg/ml and stored at −80°C until use. Peptide pools 1 through 6 consisted of 32 to 35 peptides each and, in the IFN-γ ELISpot assay, were used at a final concentration of 1.5 μg/ml per individual peptide. Negative controls contained 0.45% DMSO in culture medium. Phytohemagglutinin (10 μg/ml; Sigma-Aldrich) was used as a nonspecific stimulant in positive-control wells. The released IFN-γ was captured by monoclonal antibody (MAb) GZ-4 immobilized on the bottoms of the assay wells, visualized using a combination of the secondary MAb 7-B6-1 coupled to an enzyme and a chromogenic substrate (Bio-Rad, Hertfordshire, United Kingdom), and quantified by spot counting using the AID ELISpot reader system. All assays were carried out in triplicate and the background subtracted from the experimental counts.
ICS.
In mouse experiments, intracellular cytokine staining (ICS) was performed on splenocytes after overnight storage at 4°C in complete RPMI medium. A 96-well round-bottom plate was set up with 3 × 106 splenocytes per well. Each sample was incubated with Golgi Stop (BD Biosciences, San Diego, CA) and either 2 μg/ml of RGPGRAFVTI, 2 μg/ml of concanavalin A, or complete RPMI medium alone. After 4.5 h of incubation at 37°C, cells were washed with fluorescence-activated cell sorting (FACS) buffer (0.1% bovine serum albumin [BSA] [Gibco, Invitrogen] in PBS) and incubated with Fc block (2.4G2; BD Biosciences) and anti-CD8-Pacific Blue (53-6.7; BD Biosciences) in FACS buffer. After excess antibody was washed away, cells were fixed with Cytofix/Cytoperm (BD Biosciences) according to the manufacturer's instructions and then washed again, followed by staining with anti-interleukin-2 (IL-2)–allophycocyanin (APC) (JES6-5H4), anti-IFN-γ–fluorescein isothiocyanate (FITC) (XMG1.2), and anti-tumor necrosis factor (TNF)–phycoerythrin (PE) (MP6-XT22) (all from BD Biosciences) in Perm/Wash buffer (BD Biosciences). Cells were then washed in Perm/Wash buffer, resuspended in FACS buffer, and analyzed on a flow cytometer (FACSCanto II; BD Biosciences), followed by data analysis using the FlowJo software (Tree Star, Inc., Ashland, OR). Gating was performed as illustrated in Fig. S1 in the supplemental material.
For experiments with rhesus macaques, frozen peripheral blood mononuclear cells (PBMCs) were thawed and washed twice with RPMI 1640 supplemented with 10% FCS and incubated overnight at 37°C with 5% CO2. The following day, cells were counted and placed at 2 × 106 PBMCs/ml in a 96-well round-bottom plate. Cells were stimulated with peptide pool 1 corresponding to the Gag regions of HIVconsv for 8 h and stained with the following MAbs: anti-CD3–APC-Cy7, anti-CD8–PE-Cy7, anti-CD–PE, anti-IFN-γ–FITC, anti-TNF-α–Pacific Blue (BD Biosciences), and anti-IL-2–APC (MACS Miltenyi Biotec, Surrey, United Kingdom). After a final wash, cells were fixed with 2% paraformaldehyde, acquired using a CyAn ADP flow cytometer (Dakocytomation; Dako, Cambridgeshire, United Kingdom), and analyzed with the FlowJo software.
Statistics.
Since normal distribution tests for relatively small sample sizes are unreliable, nonparametric tests were used for statistical comparisons. For pairwise analysis between two groups, we performed the nonparametric Mann-Whitney U test. For multiple comparisons, we used the Kruskal-Wallis test for a priori analysis, followed by a post hoc analysis using Dunn's test. A P value of less than 0.05 was used as an indicator of statistical significance. Statistical analyses were performed using the GraphPad Prism 5 software (GraphPad Software Inc., La Jolla, CA).
RESULTS
Construction of the DREP.HIVconsv vaccine.
Two DNA vaccines encoding the HIVconsv immunogen were used in this study (Fig. 1). The first, pTH.HIVconsv, is a conventional plasmid DNA encoding HIVconsv under control of a cytomegalovirus (CMV) promoter/enhancer/intron A cassette (25). The second vaccine, DREP.HIVconsv, is vectored by an SFV-based DNA replicon, DREP.HIVconsv, that encodes the SFV replicase under control of a CMV promoter and the HIVconsv immunogen under control of subgenomic promoter 26S. When cells are transfected with the DREP.HIVconsv DNA, DREP.HIVconsv RNA is transcribed from the CMV promoter in the cell nucleus and exported to the cytoplasm, where the SFV replicase is translated from the 5′ proximal portion of this RNA. The replicase amplifies the DREP.HIVconsv RNA and subsequently transcribes the HIVconsv mRNA from a subgenomic promoter on the negative-strand copy of the DREP.HIVconsv RNA (46).
To be able to analyze the expression of HIVconsv from a replicon, we infected BHK-21 cells with SFV replicons delivered as viral particles, designated VREP.HIVconsv, which infect cells with virtually 100% efficiency. In cells harboring replicon RNA, translation of host mRNA is inhibited and only RNA transcribed from the replicon will be translated (30). VREP.HIVconsv consists of RNA that is identical to the RNA produced after transfection with DREP.HIVconsv DNA. Therefore, the amplification cycles are identical for VREP.HIVconsv and DREP.HIVconsv. Cells were infected with VREP.HIVconsv and pulsed with [35S]methionine, followed by incubation with unlabeled medium for increasing periods of time up to 4.5 h. This revealed that HIVconsv protein levels were relatively stable for 1 to 2 h and decreased by 4.5 h (see Fig. S2 in the supplemental material).
Lower doses of DREP.HIVconsv than of plasmid pTH.HIVconsv DNA are required for induction of CD8+ T cell responses.
We compared the magnitudes of the cellular immune responses induced by pTH.HIVconsv and DREP.HIVconsv DNA. We used an IFN-γ ELISpot assay to quantify the cellular response on freshly isolated splenocytes. In previous studies, the strongest responses to the HIVconsv immunogen were directed to the major histocompatibility complex (MHC) class I-restricted RGPGRAFVTI reporter epitope (25), and thus this peptide was used for stimulation. CD8+ T cells are responsible for cytotoxic T lymphocyte (CTL) activity and IFN-γ secretion after stimulation with this epitope (19, 47).
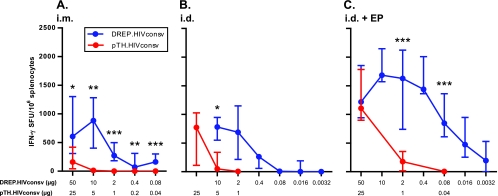
Following an i.m. mouse immunization, DREP.HIVconsv induced a higher CD8+ T cell response than pTH.HIVconsv at all doses tested (Fig. 2A). The DREP.HIVconsv responses reached a maximum at 10 μg and decreased slightly up to 50 μg. At the lowest tested dose of 80 ng, DREP.HIVconsv induced a response similar in magnitude to that with 25 μg of pTH.HIVconsv DNA, i.e., the molar equivalent of a 625-times-higher dose. A low but detectable response was observed also at 5 μg but not at lower doses of pTH.HIVconsv DNA.
Fig 2.
Dose titration of pTH.HIVconsv and DREP.HIVconsv with different routes of immunization. (A) Mice were injected with DNA i.m., and spleens were collected 10 days later. Results are pooled from two separate experiments, resulting in a total of 9 or 10 mice per group. (B) Mice were injected with DNA i.d., and spleens were collected 10 days later. Each group consisted of 4 or 5 mice. (C) Mice were injected with DNA i.d., followed by EP, and spleens were collected 10 to 12 days later. Results are pooled from three separate experiments, resulting in a total of 9 or 10 mice per group. For all panels, HIVconsv-specific CD8+ T cells were assessed by IFN-γ ELISpot assay. Equivalent molar doses of pTH.HIVconsv and DREP.HIVconsv are grouped in the graphs. Responses are shown as medians, with error bars representing interquartile ranges. Equimolar amounts of pTH.HIVconsv and DREP.HIVconsv administered by the same route were compared statistically by using a Mann-Whitney U test. *, P < 0.05; **, P < 0.01; ***, P < 0.0001.
DREP.HIVconsv was also superior to pTH.HIVconsv when given via the i.d. route (Fig. 2B). At 10 μg, DREP.HIVconsv induced a response via the i.d. route that was similar to that induced via the i.m. route (Fig. 2A). At 2 μg, the response was slightly lower in magnitude than the response induced by 10 μg, although it was higher than that induced by 2 μg of DNA administered i.m. At 400 ng, the response decreased, although it was still well detectable. At lower doses tested, median values indicated no response, although two of five mice responded to a mere 16 ng.
It has previously been shown that delivering conventional plasmid DNA with EP results in increased cellular immune responses (39). We therefore asked whether EP would similarly increase the T cell response following immunization with the DREP.HIVconsv replicon and whether the dose could be decreased without significantly compromising the immune response. Mice were immunized i.d. with decreasing doses of DREP.HIVconsv or pTH.HIVconsv DNA, followed by EP (Fig. 2C). At 50 μg, DREP.HIVconsv replicons induced a response similar in magnitude to that induced by an equivalent dose of plasmid pTH.HIVconsv. At the three following lower doses, i.e., 10 μg, 2 μg, and 400 ng of the DREP.HIVconsv DNA, the CD8+ T cell response was slightly higher. In contrast, decreasing the doses of the pTH.HIVconsv DNA rapidly reduced the response. At 1 μg, the pTH.HIVconsv-induced response was 9-fold lower than that induced by the corresponding DREP.HIVconsv dose, and at 40 ng, there was no detectable response. However, the DREP.HIVconsv replicon doses could be further decreased, and at 80 ng, the response decreased to a level similar in magnitude to the maximal response induced by i.m. or i.d. immunization without EP (Fig. 2A and B). The T cell response further decreased but was still at well-detectable levels at 3.2 ng. At this dose, DREP.HIVconsv still induced a response similar to that induced by 1 μg, or 625 times the molar equivalent dose, of the pTH.HIVconsv DNA.
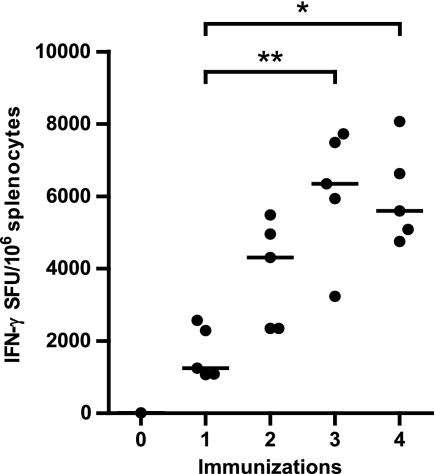
Multiple immunizations with the DREP.HIVconsv vaccine boost the CD8+ T cell response.
We next investigated whether the DREP.HIVconsv replicon-induced responses could be further boosted after multiple immunizations. We therefore immunized mice once and compared the responses for mice that were boosted monthly one, two, or three times after the prime. The peak of the CD8+ T cell response occurs after 10 to 11 days after a single DREP.HIVconsv DNA immunization (data not shown) and after 11 to 12 days after one booster immunization (see Fig. S3 in the supplemental material). We therefore analyzed the HIVconsv-specific CD8+ T cell response by IFN-γ ELISpot assay at 11 days after the last immunization. After one and two homologous boosts, the responses were over 3 and 5 times higher, respectively, than those after a single DNA administration (Fig. 3). A third boost did not increase the responses. This demonstrates that the CD8+ T cell response can be boosted at least twice by homologous delivery of the DREP.HIVconsv replicon DNA.
Fig 3.
CD8+ T cell responses following homologous boosts with DREP.HIVconsv. Mice were immunized i.d. with EP with 2.5 μg of DREP.HIVconsv the indicated number of times. Homologous boosts were administered monthly. Spleens were collected and analyzed 11 days after immunization. HIVconsv-specific CD8+ T cell responses were assessed with IFN-γ ELISpot. Each immunized group consisted of 5 mice, and 2 naïve mice were included. Lines represent group medians. The Kruskal-Wallis nonparametric test followed by Dunn's posttest was used to compare the response between all immunized groups. *, P < 0.05; **, P < 0.01.
The DREP.HIVconsv vaccine potently primes CD8+ T cells prior to a heterologous boost immunization.
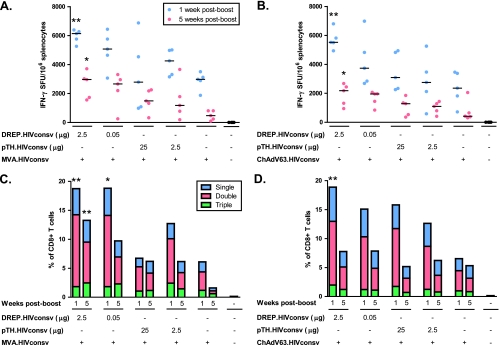
We next compared the abilities of i.d. EP of DREP.HIVconsv and pTH.HIVconsv DNA to prime HIV-1-specific T cells in a heterologous prime-boost regimen. Two different doses of the DREP.HIVconsv and pTH.HIVconsv vaccines were used: high doses of 2.5 μg of DREP.HIVconsv DNA and 25 μg of pTH.HIVconsv DNA, which induced maximal responses in the dose titration experiment described above (Fig. 2C), and lower doses of 50 ng of DREP.HIVconsv DNA and 2.5 μg of pTH.HIVconsv DNA, which induced intermediate T cell frequencies. Boosting immunizations were given 9 weeks after DNA EP with either the MVA.HIVconsv or ChAdV63.HIVconsv vaccine, which are currently being evaluated in clinical trials (T. Hanke, unpublished). CD8+ T cell responses were assessed during the acute and contraction phases of the T cell response at 1 and 5 weeks after the boost, respectively, using the IFN-γ ELISpot assay.
In mice boosted with the MVA.HIVconsv vaccine, the strongest response was observed in the group that was primed with the high dose of the DREP.HIVconsv replicon (Fig. 4A). This was the only group that showed a statistically significant priming effect. In mice given either dose of DREP.HIVconsv DNA or the high dose of pTH.HIVconsv, the frequency of CD8+ T cells at 5 weeks postboost was halved relative to that during the acute response. In mice given the low dose of the pTH.HIVconsv DNA and MVA.HIVconsv alone, the T cell frequencies decreased to 28% and 16% of the acute responses, respectively.
Fig 4.
CD8+ T cell responses following DNA prime and viral vector boost. Mice were immunized i.d. with EP with the indicated dose and boosted 9 weeks later with 5 × 106 PFU MVA.HIVconsv (A and C) or 7 × 109 vp ChAdV63.HIVconsv (B and D). Spleens were collected and analyzed at 7 days and 5 weeks postboost. HIVconsv-specific CD8+ T cell responses were assessed with IFN-γ ELISpot (A and B) and by ICS for IFN-γ, TNF-α, and IL-2 (C and D). Single, double, and triple denote how many of these cytokines the individual CD8+ T cells produced. Each group consisted of 5 mice. Results are displayed as group medians. The Kruskal-Wallis nonparametric test followed by Dunn's posttest was used to compare all primed groups with the corresponding nonprimed group at 7 days or 5 weeks postboost. In panels C and D, the total percentage of cytokine-positive cells was used for statistical comparison. *, P < 0.05; **, P < 0.01.
In mice given the ChAdV63.HIVconsv vaccine boost, the high-dose DREP.HIVconsv DNA priming induced the strongest response (Fig. 4B) and delivered a consistent, statistically significant enhancement of the adenovirus boost. The low-dose DREP.HIVconsv priming elicited weaker T cell responses, although these were still moderately stronger than those observed in both pTH.HIVconsv-primed groups. During the contraction of the T cell response (at five weeks postboost), the number of IFN-γ-secreting CD8+ T cells was close to twice as high in mice primed with the high dose of DREP.HIVconsv than it was in mice primed with either dose of pTH.HIVconsv. The proportion of IFN-γ-secreting cells that remained at 5 weeks postboost was 40 to 50% in all primed groups and only 18% in nonprimed animals.
As oligofunctional HIV-1-specific CD8+ T cells capable of producing multiple cytokines were in some studies associated with control of chronic HIV-1 infection (6, 15, 52), we also analyzed the ability of the vaccine-elicited HIVconsv-specific CD8+ T cells to produce IFN-γ, IL-2, and TNF-α by ICS analysis followed by flow cytometry. For mice boosted with MVA.HIVconsv, the ICS analysis showed a pattern of responses that was largely similar to that in the IFN-γ ELISpot assay (Fig. 4C). The highest T cell frequencies were seen in mice primed with the high or low dose of the DREP.HIVconsv vaccine, and the CD8+ T cell frequencies remained high for at least 5 weeks. In the acute response, all cytokine-positive cells produced IFN-γ, and double-positive cells additionally produced TNF-α. A population of TNF-α single-positive cells emerged during the contraction phase in all groups (see Fig. S4 in the supplemental material).
In the ICS analysis of mice boosted with ChAdV63.HIVconsv, the strongest response in the acute phase was seen in the group primed with the high dose of DREP.HIVconsv (Fig. 4D), in accordance with what was observed in the IFN-γ ELISpot assay (Fig. 4B). The three other primed groups all had a slightly smaller amount of cytokine-positive CD8+ T cells than this group. The group given ChAdV63.HIVconsv without a prime produced only a third of the amount of cytokine-positive cells produced by the group primed with the high dose of DREP.HIVconsv during the acute response. At 5 weeks postboost, the CD8+ T cell populations had contracted in all mice primed with DNA but not in mice given only ChAdV63.HIVconsv. This was in contrast to what was observed in the IFN-γ ELISpot assay, where a contraction was also observed in the nonprimed group. This could be explained by the TNF-α-positive (IFN-γ/IL-2-negative) population that emerged in the contraction phase, which was not accounted for in the IFN-γ ELISpot analysis (see Fig. S5 in the supplemental material). The proportions of single-, double-, and triple-positive CD8+ T cells were similar in all groups primed with either DREP.HIVconsv or pTH.HIVconsv (Fig. 4D). Again, the vast majority of all cytokine-positive cells in the acute phase produced IFN-γ, and double-positive cells also produced TNF-α (see Fig. S5 in the supplemental material). Like in the heterologous prime-boost experiment with MVA.HIVconsv boosting, a TNF-α single-positive population emerged during the contraction of the immune response.
Next we asked whether priming with 50 ng of DREP.HIVconsv or 2.5 μg of pTH.HIVconsv would allow for the use of lower doses of MVA.HIVconsv in boost immunization. Four weeks after the prime, mice were boosted with 5 × 106 PFU (high dose), 5 × 105 PFU (medium dose), or 5 × 104 PFU (low dose) of MVA.HIVconsv. The CD8+ T cell response was independent of the priming immunization; however, responses were highly dependent on the MVA.HIVconsv boosting dose, and increased doses correlated strongly with higher frequencies of IFN-γ-producing CD8+ T cells (Fig. 5). No qualitative differences in the immune responses were observed (Fig. 5B; see Fig. S6 in the supplemental material). Thus, a 100-fold-lower dose of DREP.HIVconsv than of pTH.HIVconsv could be used to efficiently prime mice for a boosting immunization.
Fig 5.
CD8+ T cell responses following DNA prime and different doses of viral vector boost. Mice were injected with 50 ng DREP.HIVconsv or 2.5 μg pTH.HIVconsv i.d. with EP and boosted 4 weeks later with one of three doses of MVA.HIVconsv: 5 × 106 PFU (high), 5 × 105 PFU (med), or 5 × 104 PFU (low). Spleens were collected and analyzed 7 days later with IFN-γ ELISpot and with ICS for IFN-γ, TNF-α, and IL-2. Single, double, and triple denote how many of these cytokines the CD8+ T cells produced. Each group consisted of 5 mice. Results are displayed as group medians. Pairs of groups that were administered the same boost were compared statistically with the Mann-Whitney U test. In panel B, the total percentage of cytokine-positive cells was used for statistical comparison.
A 20-fold-lower dose of DREP.HIVconsv than of plasmid DNA induces an equivalent response in rhesus macaques.
We also compared the T cell immunogenicities of DREP.HIVconsv and plasmid pTH.HIVconsv DNA in rhesus macaques. Two groups of animals received three doses of either 400 μg of DREP.HIVconsv or 4 mg of pTH.HIVconsv DNA i.m.; i.e., there was a 20-fold difference in the molar doses of the two DNA vaccines. DNA priming was followed by identical successive boosts using the MVA.HIVconsv and ChAdV63.HIVconsv vaccines. The HIV-1-specific, IFN-γ-producing PBMCs were enumerated in an IFN-γ ELISpot assay, and at no time point evaluated were the total T cell frequencies in the two groups of animals statistically separable (Fig. 6A). Also, the breadths of T cell responses induced by the two vaccine regimens, judging by frequencies detected using 6 pools of 15-mer peptides overlapping by 11 amino acids and spanning the entire HIVconsv protein, were comparable (Fig. 6B). Both vaccine regimens induced oligofunctional CD8+ T cells capable of producing several soluble intercellular signaling molecules (Fig. 6C). The functionalities of CD8+ and CD4+ T cell-mediated responses were broadly similar; the DREP.HIVconsv vaccine primed for consistently higher but not statistically separable responses. Thus, despite administration of 20-fold-lower molar doses of the priming DREP.HIVconsv DNA vaccine, the HIV-1-specific T cell responses elicited in rhesus macaques were equivalent to or higher than those with conventional plasmid pTH.HIVconsv DNA.
Fig 6.
DREP.HIVconsv immunization in rhesus macaques. Eight rhesus macaques were divided into two groups of 4 and vaccinated using regimens PPPMC (group 1) or DDDMC (group 2), where P, D, M, and C stand, respectively, for 4 mg of pTH.HIVconsv DNA i.m., 400 μg of DREP.HIVconsv DNA i.m., 108 PFU of MVA.HIVconsv i.m., and 1010 vp of ChAdV63.HIVconsv i.m. The times of vaccinations are depicted below the graphs in panels A and B. HIV-1-specific, vaccine-induced T cell responses were measured in an IFN-γ ELISpot assay using 6 pools of HIVconsv-derived 15-mer peptides overlapping by 11 amino acids (A and B) and by polychromatic flow cytometry using pool 1, corresponding to the Gag regions of HIVconsv for in vitro restimulation (C). Panel A shows the summed frequencies of cells responding to pools 1 to 6 for groups 1 and 2. The breadth of T cell specificity in respect to the six individual pools is shown for each group separately in panel B. Vaccine-elicited CD8+ and CD4+ T cell functionality is shown in panel C. All graphs show the group median frequencies.
DISCUSSION
In the work presented here, we demonstrate that the immunogenicity of DNA vaccines can be strongly enhanced by the use of an alphavirus replicon DNA vector and EP and that T cell responses primed by replicon DNA can be further boosted by recombinant MVA- and attenuated chimpanzee adenovirus-vectored vaccines. Combining these approaches, we have greatly augmented induction of T cells specific for the conserved, normally mostly subdominant regions of the HIV-1 proteome.
The molecular basis of the potent immunogenicity of DREP is not completely understood. For DNA replicon vectors based on the alphavirus Sindbis virus, apoptosis (24), type I IFNs (23), and TLR3 signaling (9) have been shown to be essential for their efficacy. For a DNA replicon based on VEE, however, type I IFNs did not have an effect on the T cell response (27). Similarly, experiments from our laboratory indicate that type I IFNs are not necessary for the enhanced immunogenicity of DREP and that at high doses type I IFNs actually suppress the response mounted against the encoded antigen (see Fig. S7 in the supplemental material) (32). This is probably due to the large amounts of type I IFNs induced, causing cells to enter an antiviral state in which production and amplification of the replicon are suppressed. The decrease in the CD8+ T cell response observed in response to high doses of DREP.HIVconsv probably reflects this effect.
DNA vaccines can be delivered using EP, which greatly improves DNA transfection into cells and causes local inflammation and infiltration of immune cells, collectively resulting in increased immune responses (1, 2, 37, 39). In addition, DREP alphavirus replicons themselves have immunogenic properties. Here, we show that EP of DREP.HIVconsv elicited HIV-1-specific frequencies of T cells that were higher than those induced by any one of these approaches used alone. This result was not obvious, since EP is a very strong inducer of local inflammation that might overshadow the inflammatory signals induced by the DREP replicon itself. Thus, combination of the DREP platform with EP provides an important avenue for increasing the potency of DNA vaccination.
The increased efficiency of DNA delivery translated into a decrease in dose requirement. The DREP.HIVconsv dose in mice could be reduced 125 times (from 10 μg with i.d. injection to 80 ng using electrovaccination) without a significant loss of T cell immunogenicity. Furthermore, compared to conventional DNA, a 625-fold reduction of the molar equivalent dose in an EP setting (1 μg of pTH.HIVconsv compared to 3.2 ng of DREP.HIVconsv DNA) is also significant. In macaques, priming with DREP.HIVconsv was equivalent or superior to the use of 20-fold more conventional plasmid DNA in inducing CD4+ and CD4+ T cell responses with multifunctional properties. However, to further characterize the dose-sparing effects of the DREP platform, dose titration in macaques would be valuable. Although we acknowledge that the significance of dose sparing based on immunogenicity needs to be validated by demonstration of increased vaccine efficacy, the results presented here strongly support clinical testing of the DREP platform as an alternative vaccination to conventional DNA.
The formation and maintenance of immunological memory are the ultimate aim of vaccination. This is significantly influenced by the magnitude of the initial immune response and secretion of type I IFNs (20, 53). Both of these factors may be favored by DREP.HIVconsv immunizations compared to immunization with conventional plasmid DNA. We observed that for mice primed with DREP.HIVconsv, a large population of T cells remained in the contraction phase at 5 weeks after a heterologous boost, suggesting that T cells are maintained into the memory phase.
In conclusion, the combination of the DREP platform with EP resulted in a strong induction of CD8+ T cell responses, requiring in mice only nanogram quantities of the replicon DNA. This increased T cell immunogenicity may be particularly important for induction of protective responses against epitopes that are in natural HIV-1 infection immunologically subdominant, such as those present in the conserved regions of HIV-1 proteins. These results strongly support replacement of plasmid DNA with alphavirus replicon DNA as the priming component of heterologous prime-boost regimens for studies in humans.
Supplementary Material
ACKNOWLEDGMENTS
We are extremely grateful to Cellectis Therapeutics for the use of equipment as well as technical support. We are thankful for the excellent and professional technical assistance provided by Kenth Andersson, Margareta Hagelin, and Anna-Karin Persson of the animal facility at the Department of Microbiology, Tumor and Cell Biology, Karolinska Institutet, Sweden.
This work was supported by the Swedish Research Council, the Swedish International Development Cooperation Agency, and the United Kingdom Medical Research Council.
Footnotes
Published ahead of print 8 February 2012
Supplemental material for this article may be found at http://jvi.asm.org/.
The authors have paid a fee to allow immediate free access to this article.
REFERENCES
- 1. Ahlén G, et al. 2007. In vivo electroporation enhances the immunogenicity of hepatitis C virus nonstructural 3/4A DNA by increased local DNA uptake, protein expression, inflammation, and infiltration of CD3+ T cells. J. Immunol. 179:4741–4753 [DOI] [PubMed] [Google Scholar]
- 2. Babiuk S, et al. 2004. Increased gene expression and inflammatory cell infiltration caused by electroporation are both important for improving the efficacy of DNA vaccines. J. Biotechnol. 110:1–10 [DOI] [PubMed] [Google Scholar]
- 3. Barry G, et al. 2009. PKR acts early in infection to suppress Semliki Forest virus production and strongly enhances the type I interferon response. J. Gen. Virol. 90:1382–1391 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Barry G, et al. 2010. Semliki Forest virus-induced endoplasmic reticulum stress accelerates apoptotic death of mammalian cells. J. Virol. 84:7369–7377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Berglund P, Smerdou C, Fleeton MN, Tubulekas I, Liljeström P. 1998. Enhancing immune responses using suicidal DNA vaccines. Nat. Biotechnol. 16:562–565 [DOI] [PubMed] [Google Scholar]
- 6. Betts MR, et al. 2006. HIV nonprogressors preferentially maintain highly functional HIV-specific CD8+ T cells. Blood 107:4781–4789 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Broderick KE, et al. 2011. Prototype development and preclinical immunogenicity analysis of a novel minimally invasive electroporation device. Gene Ther. 18:258–265 [DOI] [PubMed] [Google Scholar]
- 8. Davis BS, et al. 2001. West Nile virus recombinant DNA vaccine protects mouse and horse from virus challenge and expresses in vitro a noninfectious recombinant antigen that can be used in enzyme-linked immunosorbent assays. J. Virol. 75:4040–4047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Diebold SS, et al. 2009. Role of TLR3 in the immunogenicity of replicon plasmid-based vaccines. Gene Ther. 16:359–366 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Dubensky TW, Jr, et al. 1996. Sindbis virus DNA-based expression vectors: utility for in vitro and in vivo gene transfer. J. Virol. 70:508–519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Glasgow GM, McGee MM, Sheahan BJ, Atkins GJ. 1997. Death mechanisms in cultured cells infected by Semliki Forest virus. J. Gen. Virol. 78:1559–1563 [DOI] [PubMed] [Google Scholar]
- 12. Hanke T, et al. 1998. Enhancement of MHC class I-restricted peptide-specific T cell induction by a DNA prime/MVA boost vaccination regime. Vaccine 16:439–445 [DOI] [PubMed] [Google Scholar]
- 13. Hanke T, et al. 1999. Effective induction of simian immunodeficiency virus-specific cytotoxic T lymphocytes in macaques by using a multiepitope gene and DNA prime-modified vaccinia virus Ankara boost vaccination regimen. J. Virol. 73:7524–7532 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Harari A, et al. 2008. An HIV-1 clade C DNA prime, NYVAC boost vaccine regimen induces reliable, polyfunctional, and long-lasting T cell responses. J. Exp. Med. 205:63–77 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Harari A, et al. 2006. Functional signatures of protective antiviral T-cell immunity in human virus infections. Immunol. Rev. 211:236–254 [DOI] [PubMed] [Google Scholar]
- 16. Hariharan MJ, et al. 1998. DNA immunization against herpes simplex virus: enhanced efficacy using a Sindbis virus-based vector. J. Virol. 72:950–958 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Hidmark ÅS, et al. 2005. Early alpha/beta interferon production by myeloid dendritic cells in response to UV-inactivated virus requires viral entry and interferon regulatory factor 3 but not MyD88. J. Virol. 79:10376–10385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Hirao LA, et al. 2011. Multivalent smallpox DNA vaccine delivered by intradermal electroporation drives protective immunity in nonhuman primates against lethal monkeypox challenge. J. Infect. Dis. 203:95–102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Hocknell PK, et al. 2002. Expression of human immunodeficiency virus type 1 gp120 from herpes simplex virus type 1-derived amplicons results in potent, specific, and durable cellular and humoral immune responses. J. Virol. 76:5565–5580 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Huber JP, Farrar JD. 2011. Regulation of effector and memory T-cell functions by type I interferon. Immunology 132:466–474 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Kasturi SP, et al. 2011. Programming the magnitude and persistence of antibody responses with innate immunity. Nature 470:543–547 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Koup RA, et al. 2010. Priming immunization with DNA augments immunogenicity of recombinant adenoviral vectors for both HIV-1 specific antibody and T-cell responses. PLoS One 5:e9015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Leitner WW, Bergmann-Leitner ES, Hwang LN, Restifo NP. 2006. Type I Interferons are essential for the efficacy of replicase-based DNA vaccines. Vaccine 24:5110–5118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Leitner WW, et al. 2004. Apoptosis is essential for the increased efficacy of alphaviral replicase-based DNA vaccines. Vaccine 22:1537–1544 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Letourneau S, et al. 2007. Design and pre-clinical evaluation of a universal HIV-1 vaccine. PLoS One 2:e984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Liu MA. 2010. Immunologic basis of vaccine vectors. Immunity 33:504–515 [DOI] [PubMed] [Google Scholar]
- 27. Ljungberg K, et al. 2007. Increased immunogenicity of a DNA-launched Venezuelan equine encephalitis virus-based replicon DNA vaccine. J. Virol. 81:13412–13423 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Low L, et al. 2009. DNA vaccination with electroporation induces increased antibody responses in patients with prostate cancer. Hum. Gene Ther. 20:1269–1278 [DOI] [PubMed] [Google Scholar]
- 29. McCormack S, et al. 2008. EV02: a phase I trial to compare the safety and immunogenicity of HIV DNA-C prime-NYVAC-C boost to NYVAC-C alone. Vaccine 26:3162–3174 [DOI] [PubMed] [Google Scholar]
- 30. McInerney GM, Kedersha NL, Kaufman RJ, Anderson P, Liljeström P. 2005. Importance of eIF2alpha phosphorylation and stress granule assembly in alphavirus translation regulation. Mol. Biol. Cell 16:3753–3763 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Napolitani G, Rinaldi A, Bertoni F, Sallusto F, Lanzavecchia A. 2005. Selected Toll-like receptor agonist combinations synergistically trigger a T helper type 1-polarizing program in dendritic cells. Nat. Immunol. 6:769–776 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Näslund TI, Kostic L, Nordström EK, Chen M, Liljeström P. 2011. Role of innate signalling pathways in the immunogenicity of alphaviral replicon-based vaccines. Virol. J. 8:36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Nordström EK, et al. 2005. Enhanced immunogenicity using an alphavirus replicon DNA vaccine against human immunodeficiency virus type 1. J. Gen. Virol. 86:349–354 [DOI] [PubMed] [Google Scholar]
- 34. Paris RM, Kim JH, Robb ML, Michael NL. 2010. Prime-boost immunization with poxvirus or adenovirus vectors as a strategy to develop a protective vaccine for HIV-1. Expert Rev. Vaccines 9:1055–1069 [DOI] [PubMed] [Google Scholar]
- 35. Pichlmair A, Reis e Sousa C. 2007. Innate recognition of viruses. Immunity 27:370–383 [DOI] [PubMed] [Google Scholar]
- 36. Rerks-Ngarm S, et al. 2009. Vaccination with ALVAC and AIDSVAX to prevent HIV-1 infection in Thailand. N. Engl. J. Med. 361:2209–2220 [DOI] [PubMed] [Google Scholar]
- 37. Roos AK, et al. 2009. Skin electroporation: effects on transgene expression, DNA persistence and local tissue environment. PLoS One 4:e7226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Roos AK, Eriksson F, Walters DC, Pisa P, King AD. 2009. Optimization of skin electroporation in mice to increase tolerability of DNA vaccine delivery to patients. Mol. Ther. 17:1637–1642 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Roos AK, et al. 2006. Enhancement of cellular immune response to a prostate cancer DNA vaccine by intradermal electroporation. Mol. Ther. 13:320–327 [DOI] [PubMed] [Google Scholar]
- 40. Rosario M, et al. 2010. Long peptides induce polyfunctional T cells against conserved regions of HIV-1 with superior breadth to single-gene vaccines in macaques. Eur. J. Immunol. 40:1973–1984 [DOI] [PubMed] [Google Scholar]
- 41. Sandström E, et al. 2008. Broad immunogenicity of a multigene, multiclade HIV-1 DNA vaccine boosted with heterologous HIV-1 recombinant modified vaccinia virus Ankara. J. Infect. Dis. 198:1482–1490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Schell JB, et al. 2011. Significant protection against high-dose simian immunodeficiency virus challenge conferred by a new prime-boost vaccine regimen. J. Virol. 85:5764–5772 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Schneider J, et al. 1998. Enhanced immunogenicity for CD8+ T cell induction and complete protective efficacy of malaria DNA vaccination by boosting with modified vaccinia virus Ankara. Nat. Med. 4:397–402 [DOI] [PubMed] [Google Scholar]
- 44. Schulz O, et al. 2005. Toll-like receptor 3 promotes cross-priming to virus-infected cells. Nature 433:887–892 [DOI] [PubMed] [Google Scholar]
- 45. Schulz O, et al. 2010. Protein kinase R contributes to immunity against specific viruses by regulating interferon mRNA integrity. Cell Host Microbe 7:354–361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Strauss JH, Strauss EG. 1994. The alphaviruses: gene expression, replication, and evolution. Microbiol. Rev. 58:491–562 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Takahashi H, et al. 1988. An immunodominant epitope of the human immunodeficiency virus envelope glycoprotein gp160 recognized by class I major histocompatibility complex molecule-restricted murine cytotoxic T lymphocytes. Proc. Natl. Acad. Sci. U. S. A. 85:3105–3109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. van Drunen Littel-van den Hurk S, Hannaman D. 2010. Electroporation for DNA immunization: clinical application. Expert Rev. Vaccines 9:503–517 [DOI] [PubMed] [Google Scholar]
- 49. Vasan S, et al. 2011. In vivo electroporation enhances the immunogenicity of an HIV-1 DNA vaccine candidate in healthy volunteers. PLoS One 6:e19252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Ventoso I, et al. 2006. Translational resistance of late alphavirus mRNA to eIF2alpha phosphorylation: a strategy to overcome the antiviral effect of protein kinase PKR. Genes Dev. 20:87–100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Wallace M, et al. 2009. Tolerability of two sequential electroporation treatments using MedPulser DNA delivery system (DDS) in healthy adults. Mol. Ther. 17:922–928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Wijesundara DK, Jackson RJ, Ramshaw IA, Ranasinghe C. 2011. Human immunodeficiency virus-1 vaccine design: where do we go now? Immunol. Cell Biol. 89:367–374 [DOI] [PubMed] [Google Scholar]
- 53. Xiao Z, Casey KA, Jameson SC, Curtsinger JM, Mescher MF. 2009. Programming for CD8 T cell memory development requires IL-12 or type I IFN. J. Immunol. 182:2786–2794 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.