Abstract
The difficulty in successfully treating infections caused by methicillin-resistant Staphylococcus aureus (MRSA) has led to them being referred to as highly virulent or pathogenic. In our study of one of the major healthcare-associated MRSA (HA-MRSA) clones, we show that expression of the gene responsible for conferring methicillin resistance (mecA) is also directly responsible for reducing the ability of HA-MRSA to secrete cytolytic toxins. We show that resistance to methicillin induces changes in the cell wall, which affects the bacteria's agr quorum sensing system. This leads to reduced toxin expression and, as a consequence, reduced virulence in a murine model of sepsis. This diminished capacity to cause infection may explain the inability of HA-MRSA to move into the community and help us understand the recent emergence of community-associated MRSA (CA-MRSA). CA-MRSA typically express less penicillin-binding protein 2a (encoded by mecA), allowing them to maintain full virulence and succeed in the community environment.
Methicillin-resistant Staphylococcus aureus (MRSA) is a major cause of nosocomial infections worldwide, with factors such as exposure to broad-spectrum antibiotics, presence of indwelling catheters, and recent surgery leading to increased susceptibility to infection [1–3]. Genetic analyses of healthcare-associated MRSA (HA-MRSA) have shown that certain clones have become endemic in these environments, but these MRSA are rarely found to cause infections in individuals with no healthcare contact (ie, in the community environment [2, 3]). The recent emergence of community-associated MRSA (CA-MRSA), which can cause infections outside healthcare settings among otherwise healthy individuals, is a growing concern [2, 3]. Comparisons of HA-MRSA with CA-MRSA have revealed genetic differences between these 2 groups [3–6] but none that explain why HA-MRSA is restricted to healthcare environments when CA-MRSA is not.
Resistance to methicillin and oxacillin (the clinically used derivative of methicillin) is conferred by the acquisition of a mobile genetic element: staphylococcal chromosomal cassette mec (SCCmec) [4]. The elements vary in size (20–70 kb) and genetic content, but they all contain the mecA gene, which encodes an alternative penicillin-binding protein (PBP), PBP2a [5, 6]. Genetic analyses of HA-MRSA and CA-MRSA have shown that HA-MRSA tends to carry the large types I, II, and III SCCmec elements, whereas CA-MRSA tends to carry the smaller type IV and V elements [5, 6]. Penicillin-binding proteins are membrane-bound enzymes that catalyze the transpeptidation and transglycosylation of peptidoglycan, the major structural component of the bacterial cell wall [6]. β-Lactam antibiotics irreversibly acylate the catalytic serine within the transpeptidase active site of PBPs [7]. This impairs effective peptide cross-linking, destabilizing the cell wall and resulting in bacterial lysis. Methicillin-resistant S. aureus strains are resistant because PBP2a has a lower affinity for β-lactam antibiotics, enabling it to continue its catalytic activity even in the presence of the antibiotic [7]. However, the expression of PBP2a alone is often not sufficient to confer resistance; many other contributing cell wall and membrane proteins have been identified [8–10].
Studies comparing the relative virulence of MRSA types and methicillin-susceptible S. aureus (MSSA) suggest a contradictory virulence hierarchy: HA-MRSA > MSSA [11–13]; CA-MRSA > HA-MRSA [14, 15] and MSSA = CA-MRSA [16, 17]. This illustrates the need for further characterization of their relative virulence. The environments in which these infections occur will select for the most successful pathogen. An understanding of how (and if) the relative virulence of these strains vary depending on environment will inform us of strategies to employ to control and contain their success.
We previously reported that MRSA strains containing the hospital-associated type II SCCmec element were less toxic (as measured by their ability to lyse T cells) than their antibiotic-sensitive relatives, whereas the toxicity of strains carrying the smaller community-associated type IV elements were not affected [18, 19]. Here we demonstrate that the reduced toxicity of HA-MRSA is a direct result of mecA expression, mediated by interference with the S. aureus accessory gene regulator (agr) quorum sensing system. We found that this MRSA was impaired in its ability to respond to the agr auto-inducing peptide (AIP), but removal of the cell wall restored this ability. This suggests that the expression of mecA and either its potential to subtly affect peptidoglycan structure or its interaction with other cell wall–associated proteins prevent the AIP from being detected. This results in an unresponsive agr system and subsequent low-level toxicity. To compare the virulence of MRSA to its isogenic MSSA strain, we used a murine infection model and found that the expression of the antibiotic-resistant gene mecA reduced the virulence of MRSA. As a direct consequence of its high level of antibiotic resistance, HA-MRSA is impaired in its ability to cause infection, which can explain its inability to cause infection in community settings, where antibiotic usage and the prevalence of susceptible patients are low.
MATERIALS AND METHODS
Strains and Plasmids Used in This Study
Construction of mecA Mutation in BH1CC
The mecA gene was amplified by polymerase chain reaction (PCR) from BH1CC using Phusion high-fidelity DNA polymerase (NEB) and cloned into PCR-Blunt II-TOPO plasmid (Invitrogen) and inactivated by cloning the tetracycline resistance gene from pBlue::tet into its internal MfeI-NheI sites (Table 1). This was subcloned into a temperature-sensitive Escherichia coli–Staphylococcus shuttle vector pBT2-bga and transformed by electroporation into S. aureus RN4220 and finally into S. aureus MRSA BH1CC. Allelic replacement of the temperature-sensitive pSAmecA8 in BH1CC was achieved following repeated growth (3 subcultures) at 42°C for 24 hours without antibiotic selection, followed by selection of tetracycline-resistant (10 μg/mL) colonies on brain-heart infusion (BHI) agar plates. The colonies were then screened for chloramphenicol sensitivity to confirm plasmid loss, and PCR analysis was used to verify the presence of the mecA::Tcr allele on the chromosome. The mutation was confirmed by Western immunoblot analysis of PBP2a expression and reduced oxacillin minimum inhibitory concentration (MIC; data not shown).
Table 1.
Strains and Plasmids Used in the Study
| Strain | Relevant Characteristics | Reference |
| BH1CC | Clinical isolate, type II MRSA CC8 | [19] |
| BH1CCΔSCCmec | SCCmec excised from the chromosome via the recombinase activity of the ccrA and ccrB genes encoded on the plasmid pSR2 | [18] |
| BH1CCΔmecA | Construced via allele replacement to produce a ΔmecA::Tcr mutant. Tetracycline resistant | This study |
| BH1CCΔSCCmec +pmecA | SCCmec mutation complemented with the mecA gene under tetracycline-inducible control | This study |
| BH1CC ΔSCCmec +pS403A | As above with a serine to alanine substitution at position 403 in the mecA gene. Serine residue responsible for cross-linkage of PBP2a [7] | This study |
| RN4220 | Restriction negative derivative of 8325-4 | [20] |
| RN6390B | agr positive control strain | [21] |
| RN6911 | agr negative derivative of RN6390B | [22] |
| 8325-4 | Laboratory oxacillin/methicillin-sensitive Staphylococcus aureus strains | [23] |
| 8325-4 (pmecA2) | Oxacillin resistant | This study |
| MRSA252 | MRSA (type II SCCmec) | [24] |
| MRSA45 | MRSA (type II SCCmec | [24] |
| MRSA137 | MRSA (type II SCCmec) | [24] |
| MRSA281 | MRSA (type II SCCmec) | [24] |
| MRSA370 | MRSA (type II SCCmec) | [24] |
| MRSA504 | MRSA (type II SCCmec) | [24] |
| MRSA858 | MRSA (type II SCCmec) | [24] |
| MRSA720 | MRSA (type IV SCCmec) | [24] |
| 90/10685 | MRSA (type IV SCCmec) | [25] |
| BTN170 | MRSA (type IV SCCmec) | [26] |
| BTN1626 | MRSA (type IV SCCmec) | [26] |
| SwedenAO | MRSA (type IV SCCmec) | [25] |
| Plasmids | ||
| pRMC2 | Plasmid containing a tetracycline-inducible promoter system | [27] |
| pmecA | pRMC2 plasmid containing the mecA gene under the control of a tetracycline-inducible promoter | This study |
| pS403A | pRMC2 plasmid containing the mecA gene under the control of a tetracycline-inducible promoter with a serine-to-alanine substitution at position 403 | This study |
| pRB474 | Escherichia coli−Staphylococcus shuttle vector | [28] |
| pmecA2 | pRB474 containing the mecA under the control of its own promoter | This study |
| pRNAIII::GFP | Plasmid containing a fusion of RNA III to GFP | [29] |
Abbreviations: GFP, green fluorescent protein; MRSA, methicillin-resistant Staphylococcus aureus.
Cloning and Expression of mecA and Construction of the S403A Mutation
Controlled expression of mecA was achieved using a tetracycline-inducible system previously described [27]. The mecA coding region was amplified by PCR using the primers TTTGGTACCAGTCTTATATAAGGAGGATATTGATG and AAAGAGCTCCGTTATCGCTGAAATTAC and cloned into plasmid pRMC2 to make pmecA. This was electroporated into S. aureus RN4220 and subsequently into S. aureus BH1CC ΔSCCmec to complement the mecA mutation. A serine-to-alanine substitution at position 403 (critical catalytic codon [7]) was made in pmecA using the primers GTGAAGTTGTAATCTGGAACTTGTTGAGC and CAGGTGCAACTCAAAAAATATTAACAGCAATG in an inverse PCR approach, followed by ligation and transformation into DH5α to make pS403A. Mutation was verified by sequencing and reduced MIC to oxacillin, and the plasmid was transformed into BH1CCΔSCCmec, as described above.
Construction of Oxacillin Resistant 8325-4
Although tetracycline-induced expression of mecA from the plasmid pmecA was sufficient to restore oxacillin resistance to BH1CCΔSCCmec, it was not sufficient to confer oxacillin resistance to the MSSA strain 8325-4 (determined using Etest strips [Biomérieux]). Instead the mecA gene was recloned under the control of its own promoter into the shuttle vector pRB474 [22]. The mecA gene was amplified using primers SAmecA3 (TGACGATTCCAATGACGAAC) and SAmecA4 (GCATCTGGCATGCATACACT) and cloned initially into pCR-Blunt II-TOPO (pSAmecA5) and subsequently on an EcoRI fragment into pRB474 to create pmecA2. The MSSA strain 8325-4 was transformed with pmecA2, and homogeneously resistant 8325-4 colonies were selected on BHI agar containing 100 μg/mL of oxacillin.
T-Cell Toxicity Assays
T-cell toxicity assays were performed as described previously [18, 30]. Where relevant, 200 ng/mL anhydrous tetracycline was added to induce expression from the tetracycline-inducible promoter pmecA and pS403A.
Growth Curves and RNAIII::GFP Readings
BHI broth (100 mL in 250-mL conical flasks) was inoculated with 100 μL of overnight cultures (grown in BHI at 37°C, shaking at 180 rpm). Cultures were grown at 37°C, 180 rpm; samples were taken every hour; and optical density of 600 nm (OD600) was measured. Fluorescence intensity of samples was measured using a FARcyte XFLURO4 V 4.50 plate reader between 485 nm and 535 nm.
RNA Isolation
BHI broth (100 mL in 250-mL conical flask) was inoculated with 100 μL of overnight cultures and grown at 37°C, 180 rpm. RNA was isolated after 20 hours of growth using the Qiagen RNeasy Midi Kit according to the manufacturer’s instructions with an addition of 0.2 μg/μL of lysostaphin to the lysis step. RNA quality and concentration were determined using the Bio-Rad Experion RNA Analysis System.
Reverse Transcription and qRT-PCR
Complementary DNA (cDNA) was generated from messenger RNA (mRNA) using the NEB First Strand Synthesis kit in accordance with the manufacturer’s instructions using random hexamers. The following gyrB and RNAIII primers were used—RNA III forward: GAAGGAGTGATTTCAATGGCACAAG; and reverse: GAAAGTAATTAATTATTCATCTTATTTTTTAGTGAATTTG; gyrB forward: CCAGGTAAATTAGCCGATTGC; and reverse: AAATCGCCTGCGTTCTAGAG. Standard curves were performed for each primer set on serial dilutions of cDNA to determine primer efficiency. The quantitative reverse-transcriptase PCR (qRT-PCR) reactions were set up as follows: 5 μL cDNA, 7.5 μL of SYBR reagent, 0.5 μL forward primer (10 μM), 0.5 μL reverse primer (10 μM), and RNase-free water to a total volume of 15 μL. Cycle threshold values were subsequently determined for 3 biological repeats in triplicate. For each reaction, the ratio of RNAIII and gyrB transcript number was calculated as follows: 2(Ct gyrB − Ct RNAIII).
AIP Induction Assay
Synthetic AIP-1 [31] was reconstituted in dimethyl sulfoxide (DMSO) to a concentration of 10 mM. Bacterial strains were grown overnight in BHI and used to inoculate 5 mL BHI (10 μg/mL of chloramphenicol) in 30-mL tubes. The bacteria were grown for 2–3 hours to an OD600 of 0.2. The bacteria were washed and resuspended in 30% raffinose and 10% BHI. This medium was sufficient to maintain spheroplast integrity while providing sufficient nutrients for RNAIII transcription and GFP translation to take place. To each strain, combination of AIP-1, DMSO and lysostaphin (0.1 μg/mL) were added and incubated at 37°C for 3 hours. RNAIII::GFP expression was measured as described above every 30 minutes.
Animal Experiment
Casein casein yeast broth (10 mL in 50-mL flask) was inoculated with 200 μL of overnight cultures and grown at 37°C, 225 rpm to exponential phase (OD600 = 0.8), harvested by centrifugation, washed, and resuspended in sterile phosphate-buffered saline to the desired infection dose. Bacterial density in the inoculum was verified by culturing serial dilutions on tryptic soy agar plates.
For the low inoculum infections, the mice were injected intravenously with 3–5 × 106 S. aureus in a volume of 500 μL. Mice were weighed daily for 2 weeks, and weight change differences were analyzed for statistical differences using the Student t test. For the high inoculum infections, the mice were injected intravenously with 1–2 × 107 S. aureus in a volume of 500 μL. Mortality was assessed up to 7 days after infection; statistical differences between groups were analyzed using the Student t test. All surviving mice were euthanized at day 7 after inoculation.
Criteria for determining morbidity/sickness in mice included hunched posture, decreased activity, ruffled fur, and labored breathing. All animal experiments conformed to the National Institutes of Health guidelines and were approved by the Institutional Animal Care Use Committee at the Texas A&M Health Science Center Institute of Bioscience and Technology.
Measurement of MIC to Oxacillin
Measurement of MIC to oxacillin was performed in accordance with the Clinical and Laboratory Standards Institute guidelines using Etest strips from Biomérieux on Mueller Hinton agar containing 2% sodium chloride.
Analysis of PBP2a Expression
Total cell protein preparations were made from overnight cultures of bacteria grown in BHI. The cells were harvested and lysed in water containing 10 μg/mL lysostaphin, 4 units of DNAase, 4 units of RNAase, and 0.05 mg/mL sodium dodecyl sulphate by incubating at 37°C for 1 hour. Insoluble material was removed by centrifugation, and protein concentrations were determined by Bradford assay. Western blots were performed using anti-PBP2a antibodies (Abnova) and ProteinG-HRP (Sigma) and visualized using a colorimetric detection system (4CN, Bio-Rad). Band intensity was quantified using the ImageJ software (http://rsbweb.nih.gov/ij/) and is expressed relative to the positive control run on each gel.
RESULTS
Expression of mecA Reduces Toxicity
In previous work, we reported that clinical MRSA isolates (n = 24) carrying the type II SCCmec element were less toxic than clonally matched MSSA strains [30]. We subsequently demonstrated that the carriage of the type II element was directly responsible for this by deleting it from the hospital-acquired MRSA strain BH1CC and showing that it restored cytolytic activity to MSSA levels [18]. While attempting to identify the gene(s) on this SCCmec element responsible for this phenotype, we found that deletion of the mecA gene alone was sufficient to restore toxicity (Figure 1A). Expression of the mecA gene from a tetracycline-inducible promoter (pmecA) in the BH1CCΔSCCmec strain reduced toxicity to wild-type MRSA levels in a dose-dependent manner (Figure1A). (The abundance of antibiotic resistance markers in the BH1CCΔmecA mutant prevented us from complementing mecA in this strain.) By contrast, expression of a mutant of mecA encoding a catalytically inactive PBP2a (expressed on pS403A [7]) failed to reduce toxicity. This effect was additionally verified by expressing oxacillin resistance in an MSSA strain (8325-4), in which the ability of the resistant strain to lyse T cells was reduced (Figure 1B).
Figure 1.
The expression of the mecA gene lowers toxicity. Survival of T cells after exposure to bacterial culture supernatants. Open circles represent individual data points, closed circles represent the mean of the data sets, the error bars represent the 95% confidence intervals and the asterisks indicate differences with p values of less than .05. A, The BH1CC strain is less toxic than BH1CCΔSCCmec and BH1CCΔmecA (P = .002 and .002, respectively), demonstrating that the presence of the mecA gene is responsible for the reduced toxicity. Complementation of BH1CCΔSCCmec with a plasmid expressing the mecA gene from a tetracycline-inducible promoter (pmecA) reduces the toxicity of the strain in a dose-dependent manner (P = .02), whereas the catalytically inactive version of mecA (pS403A) does not affect toxicity (P = .63). B, T-cell survival following exposure to the supernatent of S. aureus strain 8325-4 containing the empty plasmid vector (pRB474), and expressing mecA(pmecA2) (p< .001).
Expression of the agr-Regulated β-Toxin Is Affected by the Presence of mecA
The agr quorum sensing system is a major regulator of toxin expression in S. aureus [20], and several studies have reported a high incidence of agr dysfunction among clinical HA-MRSA strains based on their hemolytic profiles [30, 32]. The immortalized T cells used in this assay are sensitive to β-toxin [30], which is regulated by agr [33]. The functional expression of β-toxin by BH1CC, BH1CCΔSCCmec, and BH1CCΔmecA was determined by hot-cold lysis of sheep blood [34], in which we found the expression of β-toxin to be lower in the MRSA strain BH1CC compared with its MSSA mutants (data not shown). Deletion of the entire SCCmec element had a more significant effect than deletion of mecA alone, perhaps as a consequence of the additional regulatory elements found on these SCCmec elements [35, 36]. To verify that the observed effect on toxicity was not a result of adventitious mutations within the agr locus [37, 38], we sequenced it in BH1CC, BH1CCΔSCCmec, and BH1CCΔmec. We found them to be identical to each other and to that of strain Newman, which has a functional agr system.
Induction of the agr Quorum Sensing System Is Affected by the Presence of mecA
We have previously shown that T cells are less susceptible to lysis when incubated with the supernatant of an agr mutant [30]. To examine whether altered agr activity contributed to the reduced MRSA toxicity, we introduced a plasmid containing the RNAIII promoter fused to the green fluorescent protein (RNAIII::GFP [29]) into BH1CC, BH1CCΔSCCmec, BH1CCΔmecA, and isogenic control strains RN6390B (agr+ [21]) and RN6119 (agr− [22]). No differences in the ability of these strains to grow was detected by measuring the OD600 over a growth curve (data not shown); however, their ability to induce expression of RNAIII was affected by the presence of the mecA gene (Figure 2). The MRSA strain BH1CC and the agr− strain RN6119 did not display the typical stationary phase induction of RNAIII as displayed by the control agr+ strain RN6390B. Deletion of the SCCmec element or the mecA gene alone restored the stationary phase induction of RNAIII. These results were verified by qRT-PCR, in which the expression of RNAIII (relative to gyrB) was 5.8-fold higher in BH1CCΔmecA than in wild-type MRSA strain BH1CC (P = .005). From this we conclude that the presence of the mecA gene inhibits the expression of RNAIII, the effector molecule of the agr quorum sensing system.
Figure 2.
The presence of the mecA gene prevents stationary phase activation of RNAIII. The activity of the RNAIII promoter (fused to green fluorescent protein) over 12 hours of growth for the following strains: RN6390B (agr+, closed triangles), RN6119 (agr−, open triangles), BH1CC (methicillin-resistant Staphylococcus aureus [MRSA], closed squares), BH1CCΔSCCmec (isogenic methicillin-susceptible S. aureus [MSSA], open squares), and BH1CCΔmecA (isogenic MSSA, gray squares). The data show that BH1CC and RN6119 did not display the typical stationary phase RNAIII induction, whereas deletion of the SCCmec element or mecA alone restored this induction to levels similar to the control agr+ strain RN6390B. The data is presented as the mean of five independent replicates, and the error bars are the 95% confidence intervals.
MRSA Cell Wall Prevents RNAIII Induction by Extracellular agr AIP
To switch on toxin expression, a threshold density of the secreted agr AIP is sensed, and this triggers expression of the agr regulatory effector-molecule RNAIII [21, 22]. That the MRSA strain BH1CC is unable to switch on the agr quorum sensing system, despite reaching high cell densities, suggested that it may be unable to respond to extracellular AIP. To test this, we developed an AIP induction assay by growing cells to early exponential phase in which RNAIII is not expressed. Synthetic AIP was added to these cells, and the induction of RNAIII::GFP expression was assayed. A gradual induction of RNAIII was observed in the control strain RN6390B (agr+) over 3 hours after addition of synthetic AIP (Figure 3A). When compared with the control agr+ strain, the MRSA strain BH1CC expressed lower levels of RNAIII in the presence of the AIP (P < .001), but deletion of the entire SCCmec element (BH1CCΔSCCmec) or mecA alone (BH1CCΔmecA) restored the ability of this strain to express RNAIII to control levels (P > .05) (Figure 3B). This demonstrates that mecA affects the ability of the MRSA strain to respond to extracellular AIP.
Figure 3.
The methicillin-resistant Staphylococcus aureus (MRSA) cell wall prevents the detection of the agr quorum sensing system auto-inducing peptide (AIP). A, Induction of RNAIII expression by the agr+ strain RN6390B as measured by green fluorescent protein fluorescence over time in response to either synthetic AIP (squares) or dimethyl sulfoxide (solvent control, circles). B, The ability of strains to respond to AIP is represented as the percentage RNAIII expression relative to the agr+ control strain RN6390B 180 minutes after the addition of AIP. Whole cells of the MRSA strain BH1CC displayed significantly lower levels of RNAIII expression compared with the agr+ strain in response to the AIP, whereas the deletion of the entire SCCmec element or just mecA alone restored the ability of the strain to respond. The removal of the cell wall by digestion with lysostaphin (spheroplasts) enabled the MRSA strain BH1CC to respond to the AIP (P = .0002) but had no effect on the other strains. The asterisks indicate statistically significant differences (< .05).
MecA-encoded PBP2a is a membrane protein that directly affects the cell wall and requires additional cell wall and membrane proteins to be expressed to confer oxacillin resistance [8–10]. We hypothesized that cell wall changes associated with oxacillin resistance may affect AIP detection. To test this, we produced spheroplasts by digesting the cell wall of these strains in an osmotic solution of raffinose that maintained membrane integrity. The AIP induction assay was repeated and, as shown in Figure 3B, digestion of the cell wall from BH1CC enabled it to respond to AIP. These data indicate that expression of mecA, either directly or indirectly through its auxillary proteins [8–10], results in cell wall changes that interfere with the ability of the agr system to detect or respond to the AIP. This may be a consequence of decreased permeability associated with subtle changes to the structure of the peptidoglycan [39, 40] in the cell wall associated with methicillin resistance, or it may be that these changes somehow interfere with the activity of AgrC, the systems membrane receptor protein.
The mecA Gene on the Type II SCCmec Element Reduces Virulence
To directly compare the virulence of an isogenic set of MRSA and MSSA strains, and to verify that the effect of the mecA gene on the toxicity of a strain is not an in vitro phenomenon, we compared BH1CC, BH1CCΔSCCmec, and BH1CCΔmecA in a murine sepsis model. The relative weight loss of the mice infected with these strains can be seen in Figure 4A, and the percentage survival of the mice can be seen in Figure 4B. These data show a significant difference in morbidity and mortality between these isogenic MRSA and MSSA strains, demonstrating that the presence of the mecA gene significantly reduces the virulence of this MRSA strain.
Figure 4.
The mecA gene reduces virulence in a murine bacteremia model. Mice were inoculated intravenously with either the methicillin-resistant Staphylococcus aureus (MRSA) strain BH1CC (squares) or the isogenic methicillin-susceptible S. aureus (MSSA) strains ΔSCCmec (triangles) or ΔmecA (circles). A, Weight change in mice following intravenous infection. Balb/c mice (7–9 animals per group) were intravenously infected with 3–5 × 106 S. aureus in a volume of 500 μL and weighed before and after infection. *P < .02, BH1CC vs BH1CC ΔSCCmec or ΔmecA; **P < .02, BH1CC vs BH1CCΔmecA (unpaired t test with Welch correction). B, Percentage of survival following intravenous injection with S. aureus. Balb/c mice (16–18 animals per group) were injected intravenously with 1–2 × 107 S. aureus in a volume of 500 μL. Mortality was assessed up to 7 days after infection. The percentage of survival of mice infected with BH1CC was significantly different compared with those infected with BH1CCΔSCCmec and BH1CCΔmecA (*P < .0008, **P < .00004; Student t test).
MRSA Strains Carrying the Type IV SCCmec Element Express Less PBP2a and Are More Toxic Than Those Carrying the Type II Element
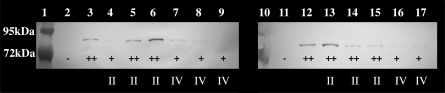
We previously reported that MRSA strains carrying the community-associated type IV SCCmec element were as toxic as MSSA strains [18, 30]. We hypothesized that because these strains tend to be less resistant to oxacillin than HA-MRSA [41], they may express lower levels of PBP2a and, as a consequence, may be able to fully express toxins. To test this, we compared the toxicity, the MIC of oxacillin, and the expression of PBP2a of a set of clinical MRSA strains carrying either the hospital-associated type II or the community-associated type IV SCCmec element. As presented in Table 2 and Figure 5, those carrying the type II SCCmec element all had an MIC of greater than 256 μg/mL to oxacillin, a T-cell survival rate between 28.6% and 88%, and a relatively high level of expression of PBP2a, whereas those carrying the type IV SCCmec element had lower MICs (12–32 μg/mL) and higher toxicity (T-cell survival, 0%–13%) and expressed less PBP2a (on average 13-fold less). This lower level of PBP2a expression may explain why MRSA strains carrying the type IV SCCmec elements, although oxacillin resistant, are more toxic than those carrying type II elements.
Table 2.
Phenotypic Characteristics of Methicillin-Resistant Staphylococcus aureu Strains Carrying Type II and Type IV SCCmec Elements
| Strain | SCCmec Type | T-Cell Survival, % (±95% CI) | Oxacillin MIC (μg/mL) | PBP2a Expression (Arbitrary Relative Units) |
| MRSA252 | II | 88 (1.4) | >256 | Not done |
| MRSA45 | II | 69.6 (15.4) | >256 | 865 |
| MRSA137 | II | 45 (29) | >256 | 3830 |
| MRSA281 | II | 28.6 (8.2) | >256 | 11356 |
| MRSA370 | II | 66.6 (12.8) | >256 | 6588 |
| MRSA504 | II | 69.7 (8.4) | >256 | 1395 |
| MRSA858 | II | 71.5 (7.3) | >256 | 819 |
| MRSA720 | IV | 13 (9) | 32 | 703 |
| 90/10685 | IV | 0.33 (.6) | 12 | 584 |
| BTN170 | IV | 0 (0) | 24 | 156 |
| BTN1626 | IV | 2.1 (2.4) | 16 | 127 |
| SwedenAO | IV | 3.6 (2) | 32 | 175 |
Abbreviations: CI, confidence interval; MIC, minimum inhibitory concentration; MRSA, methicillin-resistant Staphylococcus aureus; PBP, penicillin-binding protein.
Figure 5.
Expression of penicillin-binding protein 2a (PBP2a) by clinical methicillin-resistant Staphylococcus aureus (MRSA) strains carrying either the type II or type IV SCCmec element. The relative PBP2a expression is indicated with +, ++, or −. The SCCmec element type is indicated as either II or IV where relevant. Lanes 1 and 10: Molecular weight marker. Lanes 2 and 11: negative control (BH1CCΔSCCmec [pRMC2]). Lanes 3 and 12: positive control (BH1CCΔSCCmec [pmecA]). Lane 4: MRSA45. Lane 5: MRSA137. Lane 6: MRSA281. Lane 7: MRSA720. Lane 8: BTN170. Lane 9: BTN1626. Lane 13: MRSA370. Lane 14: MRSA504. Lane 15: MRSA858. Lane 16: SWEDEN. Lane 17: 90/10685.
DISCUSSION
For HA-MRSA, the evolution of resistance to oxacillin has a clear selective advantage in environments where antibiotic usage is high. The secondary effect of a decrease in virulence associated with resistance has not undermined its ability to become a successful nosocomial pathogen. It is likely that the high prevalence of susceptible patients in these environments and an additional transmission route via healthcare workers, compensate for reduced virulence. The reduced toxicity is, however, a likely explanation for why these HA-MRSA strains have not been successful outside hospital settings among healthy communities. The emergence of successful MRSA strains infecting healthy populations with no contact with healthcare settings (CA-MRSA) is a growing concern [2, 4, 14], and here we show that despite the presence of mecA on the type IV SCCmec elements, toxicity is not affected due to their lower level of PBP2a expression. This has allowed these strains to maintain both virulence and antibiotic resistance and succeed where HA-MRSA could not.
In addition to mecA, another putative virulence regulatory locus has been identified on the hospital-associated type II SCCmec element [36], as well as a cytolytic, phenol-soluble modulin, psm-mec [35]. Alongside our findings of the dual activity of mecA (antibiotic resistance and virulence regulation), this suggests that linkage between antibiotic resistance and virulence regulation has played an important role in shaping the success of this pathogen. Future in-depth studies on the molecular interactions of these regulatory systems with those already characterized (agr, sae, rot, etc) may fundamentally change our understanding of virulence regulation for this important human pathogen.
That an antibiotic resistance mechanism decreases the virulence of a pathogen complicates our understanding of pathogenicity and virulence. If we consider pathogenicity to be environment dependent, then the HA-MRSA strains are more pathogenic in hospitals because they can persist despite intense antibiotic pressure. In contrast, HA-MRSA strains are less pathogenic in the community because their impaired ability to express toxins is not compensated for by the benefits of being antibiotic resistant. This is reflected in their relative success and prevalence in these environments. Virulence, however, is independent of its environment, and in this study we show that HA-MRSA strains are less virulent as a direct consequence of expressing the mecA gene at high levels. This may seem an argument in semantics, but it is important to clearly understand these differences if we are to continue to study the means by which this pathogen causes disease in the hopes of identifying targets for the development of novel control and treatment strategies [42].
Notes
Acknowledgments.
We would like to thank Professor Mark Enright for providing the clinical strains.
Financial support.
This work was supported by the Medical Research Council (G0700836) and a Biotechnology and Biological Sciences Research Council studentship.
Potential conflicts of interest.
All authors: No reported conflicts.
All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1.Lowy FD. Staphylococcus aureus infections. N Engl J Med. 1998;339:520–32. doi: 10.1056/NEJM199808203390806. [DOI] [PubMed] [Google Scholar]
- 2.Gordon RJ, Lowy FD. Pathogenesis of methicillin-resistant Staphylococcus aureus infection. Clin Infect Dis. 2008;46:S350–9. doi: 10.1086/533591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Deleo FR, Otto M, Kreiswirth BN, Chambers HF. Community-associated meticillin-resistant Staphylococcus aureus. Lancet. 2010;375:1557–68. doi: 10.1016/S0140-6736(09)61999-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ito T, Katayama Y, Hiramatsu K. Cloning and nucleotide sequence determination of the entire mec DNA of pre-methicillin-resistant Staphylococcus aureus N315. Antimicrob Agents Chemother. 1999;43:1449–58. doi: 10.1128/aac.43.6.1449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hiramatsu K, Cui L, Kuroda M, Ito T. The emergence and evolution of methicillin-resistant Staphylococcus aureus. Trends Microbiol. 2001;9:486–93. doi: 10.1016/s0966-842x(01)02175-8. [DOI] [PubMed] [Google Scholar]
- 6.Hiramatsu K, Katayama Y, Yuzawa H, Ito T. Molecular genetics of methicillin-resistant Staphylococcus aureus. Int J Med Microbiol. 2002;292:67–74. doi: 10.1078/1438-4221-00192. [DOI] [PubMed] [Google Scholar]
- 7.Sun Y, Bauer MD, Lu W. Identification of the active site serine of penicillin-binding protein 2a from methicillin-resistant Staphylococcus aureus by electrospray mass spectrometry. J Mass Spectrom. 1998;33:1009–16. doi: 10.1002/(SICI)1096-9888(1998100)33:10<1009::AID-JMS717>3.0.CO;2-4. [DOI] [PubMed] [Google Scholar]
- 8.Schulthess B, Meier S, Homerova D, et al. Functional characterization of the sigmaB-dependent yabJ-spoVG operon in Staphylococcus aureus: role in methicillin and glycopeptide resistance. Antimicrob Agents Chemother. 2009;53:1832–9. doi: 10.1128/AAC.01255-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Berger-Bächi B, Rohrer S. Factors influencing methicillin resistance in staphylococci. Arch Microbiol. 2002;178:165–71. doi: 10.1007/s00203-002-0436-0. [DOI] [PubMed] [Google Scholar]
- 10.de Lencastre H, Wu SW, Pinho MG, et al. Antibiotic resistance as a stress response: complete sequencing of a large number of chromosomal loci in Staphylococcus aureus strain COL that impact on the expression of resistance to methicillin. Microb Drug Resist. 1999;5:163–75. doi: 10.1089/mdr.1999.5.163. [DOI] [PubMed] [Google Scholar]
- 11.Cosgrove SE, Sakoulas G, Perencevich EN, et al. Comparison of mortality associated with methicillin-resistant and methicillin-susceptible Staphylococcus aureus bacteremia: a meta-analysis. Clin Infect Dis. 2003;36:53–9. doi: 10.1086/345476. [DOI] [PubMed] [Google Scholar]
- 12.Gastmeier P, Sohr D, Geffers C, et al. Mortality risk factors with nosocomial Staphylococcus aureus infections in intensive care units: results from the German Nosocomial Infection Surveillance System (KISS) Infection. 2005;33:50–5. doi: 10.1007/s15010-005-3186-5. [DOI] [PubMed] [Google Scholar]
- 13.Reed SD, Friedman JY, Engemann JJ, et al. Costs and outcomes among hemodialysis-dependent patients with methicillin-resistant or methicillin-susceptible Staphylococcus aureus bacteremia. Infect Control Hosp Epidemiol. 2005;26:175–83. doi: 10.1086/502523. [DOI] [PubMed] [Google Scholar]
- 14.Otto M. Basis of virulence in community-associated methicillin-resistant Staphylococcus aureus. Annu Rev Microbiol. 2010;64:143–62. doi: 10.1146/annurev.micro.112408.134309. [DOI] [PubMed] [Google Scholar]
- 15.Li M, Diep BA, Villaruz AE, et al. Evolution of virulence in epidemic community-associated methicillin-resistant Staphylococcus aureus. Proc Natl Acad Sci U S A. 2009;106:5883–8. doi: 10.1073/pnas.0900743106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vardakas KZ, Matthaiou DK, Falagas ME. Comparison of community-acquired pneumonia due to methicillin-resistant and methicillin-susceptible Staphylococcus aureus producing the Panton-Valentine leukocidin. Int J Tuberc Lung Dis. 2009;13:1476–85. [PubMed] [Google Scholar]
- 17.Miller LG, Quan C, Shay A, et al. A prospective investigation of outcomes after hospital discharge for endemic, community-acquired methicillin-resistant and -susceptible Staphylococcus aureus skin infection. Clin Infect Dis. 2007;44:483–92. doi: 10.1086/511041. [DOI] [PubMed] [Google Scholar]
- 18.Collins J, Rudkin J, Recker M, et al. Offsetting virulence and antibiotic resistance costs by MRSA. ISME J. 2010;4:577–84. doi: 10.1038/ismej.2009.151. [DOI] [PubMed] [Google Scholar]
- 19.O’Neill E, Pozzi C, Houston P, et al. A novel Staphylococcus aureus biofilm phenotype mediated by the fibronectin-binding proteins, FnBPA and FnBPB. J Bacteriol. 2008;190:3835–50. doi: 10.1128/JB.00167-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Novick RP, Geisinger E. Quorum sensing in staphylococci. Annu Rev Genet. 2008;42:541–64. doi: 10.1146/annurev.genet.42.110807.091640. [DOI] [PubMed] [Google Scholar]
- 21.Peng HL, Novick RP, Kreiswirth B, Kornblum J, Schlievert P. Cloning, characterization, and sequencing of an accessory gene regulator (agr) in Staphylococcus aureus. J Bacteriol. 1988;170:4365–72. doi: 10.1128/jb.170.9.4365-4372.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Novick RP, Ross HF, Projan SJ, et al. Synthesis of staphylococcal virulence factors is controlled by a regulatory RNA molecule. EMBO J. 1993;12:3967–75. doi: 10.1002/j.1460-2075.1993.tb06074.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Novick RP. Properties of a cryptic high-frequency transducing phage in Staphylococcus aureus. Virology. 1967;33:155–66. doi: 10.1016/0042-6822(67)90105-5. [DOI] [PubMed] [Google Scholar]
- 24.Enright MC, Day NP, Davies CE, et al. Multilocus sequence typing for characterization of methicillin-resistant and methicillin-susceptible clones of Staphylococcus aureus. J Clin Microbiol. 2000;38:1008–15. doi: 10.1128/jcm.38.3.1008-1015.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cookson BD, Robinson DA, Monk AB, et al. Evaluation of molecular typing methods in characterizing a European collection of epidemic methicillin-resistant Staphylococcus aureus strains: the HARMONY collection. J Clin Microbiol. 2007;45:1830–7. doi: 10.1128/JCM.02402-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Price J, Baker G, Heath I, et al. Clinical and microbiological determinants of outcome in Staphylococcus aureus bacteraemia. Int J Microbiol. 2010:654858. doi: 10.1155/2010/654858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Corrigan RM, Foster TJ. An improved tetracycline-inducible expression vector for Staphylococcus aureus. Plasmid. 2009;61:126–9. doi: 10.1016/j.plasmid.2008.10.001. [DOI] [PubMed] [Google Scholar]
- 28.Bruckner R. A series of shuttle vectors for Bacillus subtilis and Escherichia coli. Gene. 1992;122:187–92. doi: 10.1016/0378-1119(92)90048-t. [DOI] [PubMed] [Google Scholar]
- 29.Qazi SN, Counil E, Morrissey J, et al. Agr expression precedes escape of internalized Staphylococcus aureus from the host endosome. Infect Immun. 2001;69:7074–82. doi: 10.1128/IAI.69.11.7074-7082.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Collins J, Buckling A, Massey RC. Identification of factors contributing to T-cell toxicity of Staphylococcus aureus clinical isolates. J Clin Microbiol. 2008;46:2112–4. doi: 10.1128/JCM.00156-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.McDowell P, Affas Z, Reynolds C, et al. Structure, activity and evolution of the group I thiolactone peptide quorum-sensing system of Staphylococcus aureus. Mol Microbiol. 2001;41:503–12. doi: 10.1046/j.1365-2958.2001.02539.x. [DOI] [PubMed] [Google Scholar]
- 32.Fowler VG, Sakoulas G, McIntyre LM, et al. Persistent bacteremia due to methicillin-resistant Staphylococcus aureus infection is associated with agr dysfunction and low-level in vitro resistance to thrombin-induced platelet microbicidal protein. J Infect Dis. 2004;190:1140–9. doi: 10.1086/423145. [DOI] [PubMed] [Google Scholar]
- 33.Recsei P, Kreiswirth B, O'Reilly M, et al. Regulation of exoprotein gene expression in Staphylococcus aureus by agr. Mol Gen Genet. 1986;202:58–61. doi: 10.1007/BF00330517. [DOI] [PubMed] [Google Scholar]
- 34.Haque R, Baldwin JN. Purification and properties of staphylococcal beta-hemolysin. J Bacteriol. 1964;88:1304–9. doi: 10.1128/jb.88.5.1304-1309.1964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Queck SY, Khan BA, Wang R, et al. Mobile genetic element-encoded cytolysin connects virulence to methicillin resistance in MRSA. PLoS Pathog. 2009;5:e1000533. doi: 10.1371/journal.ppat.1000533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kaito C, Saito Y, Nagano G, et al. Transcription and translation products of the cytolysin gene psm-mec on the mobile genetic element SCCmec regulate Staphylococcus aureus virulence. PLoS Pathog. 2011;7:e1001267. doi: 10.1371/journal.ppat.1001267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Traber K, Novick R. A slipped-mispairing mutation in AgrA of laboratory strains and clinical isolates results in delayed activation of agr and failure to translate delta- and alpha-haemolysins. Mol Microbiol. 2006;59:1519–30. doi: 10.1111/j.1365-2958.2006.04986.x. [DOI] [PubMed] [Google Scholar]
- 38.Shopsin B, Eaton C, Wasserman GA, et al. Mutations in agr do not persist in natural populations of methicillin-resistant Staphylococcus aureus. J Infect Dis. 2010;202:1593–9. doi: 10.1086/656915. [DOI] [PubMed] [Google Scholar]
- 39.de Jonge BLM, Tomasz T. Abnormal peptidoglycan produced in a methicillin-resistant strain of Staphylococcus aureus grown in the presence of methicillin: functional role for penicillin-binding protein 2A in cell wall synthesis. Antimicrob Agents Chemother. 1993;37:342–6. doi: 10.1128/aac.37.2.342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.de Jonge BLM, Chang YS, Gage D, Tomasz A. Peptidoglycan composition of a highly methicillin-resistant Staphylococcus aureus strain. J Biol Chem. 1992;267:11248–64. [PubMed] [Google Scholar]
- 41.Okuma K, Iwakawa K, Turnidge JD, et al. Dissemination of new methicillin-resistant Staphylococcus aureus clones in the community. J Clin Microbiol. 2002;40:4289–94. doi: 10.1128/JCM.40.11.4289-4294.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kreiswirth BN, Löfdahl S, Betley MJ, et al. The toxic shock syndrome exotoxin structural gene is not detectably transmitted by a prophage. Nature. 1983;305:709–12. doi: 10.1038/305709a0. [DOI] [PubMed] [Google Scholar]