Abstract
Background
Atherosclerosis, endothelial dysfunction, coronary artery calcification (CAC), and left ventricular hypertrophy are the most commonly encountered risk factors in the pathogenesis of cardiovascular disease in end-stage renal disease patients. Epicardial adipose tissue (EAT) is the true visceral fat depot of the heart. The relationship between coronary artery disease and EAT has been shown in healthy subjects and patients with a high risk of coronary artery disease. In the present study, we aimed to investigate the relationship between EAT and CAC in peritoneal dialysis (PD) patients. Patients and Methods: Forty-five PD patients (18 females, 27 males, with a mean age of 50.6 ± 15 years) and 25 healthy subjects (12 females, 13 males, with a mean age of 52.4 ± 10.7 years) were enrolled in the study. EAT and CAC score (CACS) measurements were performed by a multidetector computed tomography scanner.
Results
EAT of the PD patients was significantly higher than that of the healthy subjects (p = 0.02). When patients were divided into two subgroups (group 1: CACS ≤10, n = 20; group 2: CACS >10, n = 25), EAT was also significantly higher in group 2 patients than in group 1 patients and healthy subjects. Age and EAT were also found to be correlated with CACS ≥10.
Conclusion
There is a relationship between the anatomic assessment of coronary artery lesions by multidetector computed tomography and EAT in PD patients. This relationship might be attributed to increased inflammation and proinflammatory cytokines in uremic patients.
Key Words: Peritoneal dialysis, Epicardial adipose tissue, Coronary artery calcification, End-stage renal disease
Introduction
Cardiovascular disease (CVD) is the most common cause of mortality and morbidity in patients with end-stage renal disease (ESRD) receiving hemodialysis (HD) or peritoneal dialysis (PD) [1]. Atherosclerosis, endothelial dysfunction, coronary artery calcification (CAC), and left ventricular hypertrophy are the most commonly encountered risk factors in the pathogenesis of CVD in ESRD patients [2, 3, 4, 5]. The CAC score (CACS) reflects the severity of atherosclerotic vascular disease and predicts cardiovascular events in uremic patients [6, 7, 8]. Multidetector computerized tomography (MDCT) is non-invasive and quantitatively measures the CACS, which is associated with the presence of atherosclerotic plaque [9, 10]. Although, in ESRD patients, CAC may occur in the absence of occlusive coronary atherosclerosis, recent studies have shown an association between CAC and obstructive atherosclerosis in this population. Haydar et al. [7] reported that severe CAC predicted the presence of coronary artery disease (CAD) with a sensitivity of 92.8% and a specificity of 44% in HD patients.
Epicardial adipose tissue (EAT) is the true visceral fat depot of the heart that accounts for approximately 20% of the total heart weight and covers 80% of the cardiac surfaces, mostly in the grooved segments along the paths of the coronary arteries [11, 12, 13]. Recent studies have shown a close relationship between CAD and EAT by using MDCT and echocardiography in healthy subjects and in patients with a high risk of CAD [14, 15, 16, 17]. The CACS in ESRD patients reflects the severity of the atherosclerotic vascular disease and predicts cardiovascular events [7, 8]. In the literature, to date there are not enough data regarding EAT in ESRD patients. Therefore, in the present study we aimed to investigate the relationship between EAT and CACS in PD patients.
Patients and Methods
Patients
This is a cross-sectional study involving patients with ESRD receiving PD for at least 6 months in the outpatient Peritoneal Dialysis Unit of Selcuk University Meram School of Medicine, Konya, Turkey, and 25 healthy control subjects. Exclusion criteria included: (i) congestive heart failure; (ii) active infection; (iii) autoimmune disease, and (iv) secondary hyperparathyroidism. Among the 60 patients initially evaluated, 4 patients had congestive heart failure (NYHA class III–IV), 3 patients had active infection, 5 patients had secondary hyperparathyroidism, and 3 patients had autoimmune disease including systemic lupus erythematosus and microscopic polyangiitis. None of the patients included in the study had arrhythmia based on ECG. All 45 (18 females, 27 males) remaining patients were enrolled in the study. Demographic data, medications, primary disease of ESRD, and dialysis duration of the patients were recorded. Systolic and diastolic blood pressures of both patients and healthy subjects were measured in an upright sitting position after at least 5 min of rest using an Erka sphygmomanometer (PMS Instruments Ltd., Berkshire, UK) with an appropriate cuff size. Two readings were recorded for each individual. The average of these two readings was defined as the subject's blood pressure. Patients with systolic and diastolic blood pressures above 140 and 90 mm Hg, respectively, or already on antihypertensive treatment were assumed as hypertensive.
Fifteen patients were on treatment with antihypertensive drugs (7 of them on angiotensin-converting enzyme inhibitors, 5 of them receiving angiotensin receptor blockers, and 2 of them receiving both a calcium channel blocker and angiotensin-converting enzyme inhibitor). Twenty-two patients were taking calcium-containing phosphate binders.
The study protocol was approved by the institutional medical ethics committee of Selcuk University, and written informed consent was obtained from all subjects included in the study.
Biochemical Analyses
Venous blood samples for biochemical analyses were drawn after an overnight fast between 8:00 p.m. and 8:00 a.m. All biochemical analyses including glucose, creatinine, total cholesterol, low-density lipoprotein (LDL) cholesterol, high-density lipoprotein (HDL) cholesterol, and plasma triglyceride concentrations were performed with an oxidase-based technique by Roche/Hitachi Modular System (Mannheim, Germany) in the Central Biochemistry Laboratory of our faculty.
CACS and EAT Measurement
Unenhanced coronary CT was quantified on retrospectively electrocardiography-gated cardiac CT scans using 64-slice MDCT (Sensation 64; Siemens Medical Solutions, Erlangen, Germany). In this study, the coronary CT protocol was applied as follows: slice collimation 64 × 0.6 mm; gantry rotation time 0.33 s; pitch 0.2; tube voltage 120 kV, and tube current 600 mAs. In case of heart rate exceeding 65 bpm, heart rate control was achieved with a beta-blocker. Multiplanar data reconstructions were obtained in the standardized ventricular short-axis planes at the basal, midcavity, and apical as well as the horizontal long-axis plane with 3-mm slice thickness and 2-mm slice interval [18]. To quantify CAC, all reconstructions were transferred to a PC-based workstation (Syngo CaScoring Wizard; Siemens Medical Solutions). CACS was defined as the presence of more than two contiguous pixels with Hounsfield units greater than 130, which was designed by Agatston et al. [9]. All values of the left anterior descending coronary artery (LAD), circumflex coronary artery (Cx), and right coronary artery (RCA) were added to calculate the calcium scores. To quantify the epicardial fat volume, all reconstructions were transferred to a PC-based workstation (Syngo Volume Wizard; Siemens Medical Solutions). A CT attenuation threshold between −200 and −20 Hounsfield units was used to isolate the epicardial fat. Both EAT and CACS measurements were evaluated by 2 blinded radiologists with an interobserver variability lower than 10.
Statistical Analyses
Statistical analyses were carried out by the Statistical Package for Social Sciences for Windows ver. 15.0 (SPSS Inc., Chicago, Ill., USA). Data were expressed as the mean ± SD, with a significance level of p < 0.05. For dichotomous variables, the frequency of positive occurrences was given, along with their corresponding percentages. Statistical comparisons of individual groups were based on Student's t test for continuous variables, whereas the correlations between groups were evaluated by Spearman's test. Significant determinants identified from univariate analysis were studied in a stepwise multiple regression model. ANCOVA (general linear model) was used to determine the relationship between PD and EAT after the correction of variables on EAT. In addition, logistic regression analysis was performed to define variables associated with CACS >10. For all tests, p < 0.05 was considered significant.
Results
Patients’ Baseline Characteristics
The baseline characteristics of the 45 PD patients and 25 healthy subjects are depicted in table 1. The etiologies of the PD patients were diabetic nephropathy (n = 12), chronic glomerulonephritis (n = 8), hypertensive nephropathy (n = 15), polycystic kidney disease (n = 1), nephrolithiasis (n = 2), and unknown etiology (n = 7). There were no significant differences in age, gender, body mass index (BMI), predialysis systolic and diastolic blood pressure levels, and biochemical parameters including serum LDL and HDL cholesterol, triglycerides, and hs-CRP between the PD patients and healthy subjects.
Table 1.
Demographic and laboratory features of the PD patients and healthy subjects
| Healthy subjects | PD patients | p value | |
|---|---|---|---|
| (n = 25) | (n = 45) | ||
| Characteristics | |||
| Age, years | 52.4 ± 10.7 | 50.6 ± 15 | NS |
| Male/female | 13/12 | 27/18 | NS |
| BMI | 25.9 ± 5.3 | 26.8 ± 5.0 | NS |
| Dialysis vintage, months | – | 52 ± 26 | – |
| SBP, mm Hg | 131 ± 19 | 134 ± 28 | NS |
| DBP, mm Hg | 80 ± 11 | 85 ± 17 | NS |
| Laboratory data | |||
| Hemoglobin, mg/dl | 12.7 ± 2.1 | 11.2 ± 1.9 | NS |
| Albumin, g/dl | 3.8 (3.5–4.0) | 3.7 (3.4–3.9) | NS |
| LDL cholesterol, mg/dl | 94.3 ± 6.0 | 119.8 ± 35 | NS |
| HDL cholesterol, mg/dl | 37.9 ± 11.9 | 36.4 ± 13.0 | NS |
| Triglyceride, mg/dl | 124.8 ± 89 | 156.3 ± 99 | NS |
| A1c, % | – | 8.2 ± 1.4 | – |
| Calcium, mg/dl | – | 8.9 ± 0.8 | – |
| Phosphorus, mg/dl | – | 4.3 ± 1.0 | – |
| hs-CRP, mg/dl | 8.25 (3.75–14.5) | 9.8 (6.1–17.1) | NS |
| PTH, pg/ml | – | 353 ± 309 | – |
| Total CACS | 41 ± 112 | 144 ± 278 | 0.01 |
| EAT, cm3 | 121.5 ± 37.5 | 160 ± 77 | 0.02 |
Values are mean ± SD or median (IQR). SBP = Systolic blood pressure; DBP = diastolic blood pressure; PTH = parathyroid hormone; NS = not significant.
CACS and EAT Measurement
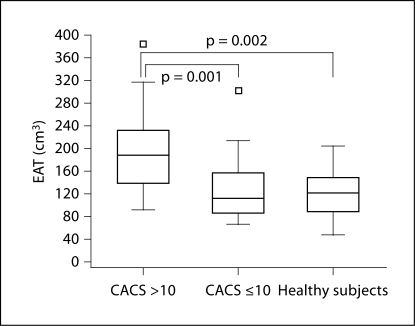
Mean total CACS of the PD patients and healthy subjects were 144 ± 278 with a median of 12.8 (interquartile range, 0.20–153.7) and 41 ± 112 with a median of 0.0 (interquartile range, 0.0–3.0), respectively. Total CACS of the PD patients were significantly higher than those of the healthy subjects (p = 0.01) (table 1). EAT of the PD patients were also significantly higher when compared with healthy subjects (p = 0.02) (table 1). The patients were divided into two subgroups (group 1: CACS ≤10, n = 20; group 2: CACS >10, n = 25) according to the total CACS proposed by Rumberger et al. [19]. Age, serum LDL cholesterol, and CACS were significantly higher in patients with CACS >10 (group 2) than in patients with CACS ≤10 (group 1) (table 2). EAT was also significantly higher in group 2 patients than in group 1 patients and healthy subjects (fig. 1).
Table 2.
Demographic and clinical characteristics of the subgroups of PD patients according to CACS (mean ± SD)
| Group 1 CACS ≤10 | Group 2 CACS >10 | p value | |
|---|---|---|---|
| (n = 20) | (n = 25) | ||
| Patients’ characteristics | |||
| Gender (M/F) | 12/8 | 14/11 | NS |
| Age, years | 41.7 ± 12.5 | 57.7 ± 13.4 | 0.0001 |
| Dialysis vintage, months | 53 ± 29 | 55 ± 24 | NS |
| BMI | 25.9 ± 5.7 | 27.6 ± 4.4 | NS |
| SBP, mm Hg | 128 ± 31 | 138 ± 26 | NS |
| DBP, mm Hg | 83 ± 19 | 86 ± 16 | NS |
| Laboratory data | |||
| Hemoglobin, g/dl | 11.0 ± 2.1 | 11.3 ± 1.8 | NS |
| Serum albumin, g/dl | 3.5 ± 0.5 | 3.6 ± 0.4 | NS |
| A1c, % | 9.0 ± 1.8 | 7.6 ± 0.9 | NS |
| LDL cholesterol, mg/dl | 134 ± 10 | 129 ± 35 | 0.022 |
| HDL cholesterol, mg/dl | 34 ± 10 | 38 ± 15 | NS |
| Triglycerides, mg/dl | 145 ± 95 | 165 ± 102 | NS |
| hs-CRP, mg/dl | 14.5 ± 4.6 | 16.4 ± 3.6 | NS |
| Calcium, mg/dl | 8.7 ± 0.9 | 9.2 ± 0.8 | NS |
| Phosphorus, mg/dl | 4.3 ± 0.9 | 4.2 ± 1.0 | NS |
| PTH, pg/ml | 330 ± 46 | 372 ± 74 | NS |
| CaXP, mg2/dl | 37.5 ± 10 | 38.5 ± 10.6 | NS |
| EAT, cm3 | 129 ± 62 | 185 ± 80 | 0.013 |
| Total calcium score | 5.4 ± 2.4 | 258.5 ± 67 | 0.001 |
SBP = Systolic blood pressure; DBP = diastolic blood pressure; PTH = parathyroid hormone; NS = not significant.
Fig. 1.
The relationship between EAT values in patients with CACS >10 and CACS ≤10 and healthy subjects.
When patients were evaluated according to their body mass index (BMI), morbid obese patients (BMI ≥30) had higher CACS and EAT than patients with a BMI <30 (p = 0.05).
In the univariate correlation analysis, EAT was positively correlated with age, BMI, and serum triglyceride (table 3), and CACS. We performed a linear regression analysis to define the variables of increased EAT. CACS, triglyceride, BMI, age, hs-CRP, albumin, Kt/v, calcium, and phosphorus were included in this model (table 4). According to the linear regression analysis, age, BMI, triglyceride, and CACS were found to be correlated with increased EAT.
Table 3.
Univariate correlation analysis of parameters of PD patients related to EAT
| Parameters | r | p value |
|---|---|---|
| Age (years) | 0.619 | 0.0001 |
| BMI | 0.454 | 0.002 |
| Triglyceride (mg/dl) | 0.329 | 0.03 |
| CACS (cm3) | 0.507 | 0.01 |
r = Correlation coefficient.
Table 4.
Variables of EAT
| Parameters | Standardized β | t | p value |
|---|---|---|---|
| Age (years) | 2.49 | 4.709 | <0.001 |
| BMI | 5.94 | 3.095 | 0.004 |
| Triglyceride (mg/dl) | 0.21 | 2.170 | 0.036 |
| CACS (cm3) | 0.116 | 3.40 | 0.001 |
r2 = 0.45, adjusted r2 = 0.39, p = 0.001 for regression model of variables of EAT.
In the univariate covariance analysis (ANCOVA), the PD modality was significantly associated with increased EAT volume when corrected for age and BMI (f = 11.23, p = 0.0001). After adjustment for age, there was a correlation between EAT and CACS in the PD patients (r = 0.25, p = 0.05).
In the separate evaluation of the different coronary arteries, the relationships between CACS of LAD, RCA, and Cx and EAT were also found to be statistically significant (table 5).
Table 5.
Relationship between calcification scores of coronary artery segments and EAT
| Coronary artery segment | r | p value |
|---|---|---|
| LAD | 0.45 | 0.002 |
| Cx | 0.39 | 0.001 |
| RCA | 0.31 | 0.004 |
| Total | 0.51 | 0.001 |
r = Correlation coefficient.
We also performed a logistic regression analysis to define the variables of CACS >10 (table 6). EAT, gender, hypertension, diabetes mellitus, hs-CRP, phosphorus, triglyceride, total cholesterol, Kt/v, and age were included in this model. Age and EAT were found to be associated with CACS >10.
Table 6.
Variables of CACS
| Parameters | Standardized β | Odds | p value | 95% CI |
|---|---|---|---|---|
| Age (years) | 0.90 | 1.10 | 0.002 | 1.05–1.16 |
| EAT (cm3) | 0.14 | 1.14 | 0.01 | 1.05–1.26 |
CI = Confidence interval. r2 = 0.337, p = 0.02 for regression model of CACS.
Discussion
The main findings of the present study were as follows: (i) EAT volumes measured by MDCT were increased in PD patients when compared with healthy subjects; (ii) EAT measurements were significantly correlated with arterial calcification of the main segments of the coronary arteries including LAD, RCA, and Cx in PD patients; (iii) morbid obese patients with a BMI ≥30 had increased CACS and EAT compared with patients who had a BMI <30, and (iv) the patients’ age and BMI were found to be correlated with increased EAT. To our knowledge, this is the first study to evaluate the relationship between EAT and CACS in PD patients.
The most common cause of death in ESRD patients is CVD, despite recent developments in renal replacement therapies [3]. This can be attributed to many factors including advanced age, atherosclerosis, endothelial dysfunction, hypertension, anemia, hyperparathyroidism, chronic inflammation, diabetes and its macro-microvascular complications, left ventricular hypertrophy, malnutrition, and vascular calcification (VC). CAC is a part of the extended state of VC which can be detected in ESRD patients even in the early stages [20]. This may contribute to premature CVD and markedly increased mortality in patients with ESRD. A number of clinical studies have shown that the amount of EAT, measured by either echocardiography or MDCT, is correlated with coronary atherosclerosis and the prevalence of CVD including myocardial infarction [21, 22, 23]. However, in studies showing a positive association between total EAT volume and the presence of CAC or atherosclerotic plaques, the EAT volume was paradoxically not related to the severity of coronary atherosclerosis or plaque burden in a dose-dependent manner [24, 25].
Hypertriglyceridemia and obesity are commonly seen in PD patients especially secondary to high-glucose ingredients of peritoneal dialysates [26, 27]. In the present study, hypertriglyceridemia and increased BMI were also found to be associated with increased EAT.
In recent studies, a preferential association between EAT thickness in the left atrioventricular groove and atherosclerosis in the embedded left circumflex artery was determined, indicating a local atherogenic role of EAT accumulated in the left atrioventricular groove [28]. Despite these results, EAT was found to be positively correlated with CACS of all segments of the coronary arteries in the present study. We conclude that atherosclerosis and VC are extensively found in all of the vasculature, possibly secondary to the uremic state of PD patients.
EAT and intra-abdominal visceral fat depots originate from the splanchnopleuric mesoderm [29]. Mazurek et al. [15] concluded that like abdominal visceral adipose tissue, EAT is also metabolically active by secreting proinflammatory cytokines and utilizing free fatty acids (FFAs). Under ischemic conditions, EAT provides FFAs for the increased metabolism of the myocardium [30]. However, in normal conditions EAT acts as a buffering system by scavenging excess FFAs that are toxic to the myocardium [28]. In ESRD patients, proinflammatory cytokines, such as TNF-α, IL-1β, IL-6, etc., are generally increased and have been found to be associated with both atherosclerosis and CACS [31, 32, 33]. In the present study, increased EAT volume was related to CACS, and this association might be attributed to increased proinflammatory cytokines secreted by EAT. However, hs-CRP levels were not correlated with CACS and EAT in the present study. Caliskan et al. [34] recently evaluated the relationship between CACS and coronary flow velocity reserve in HD patients and found similar results about the relationship between hs-CRP levels and CACS and coronary flow velocity reserve. We assume that in a cross-sectional study, it may be difficult to assess the relationship between hs-CRP and CACS and EAT, as VC is a slowly progressive process and serum hs-CRP levels may fluctuate, possibly dependent on flares of inflammation.
Wilund et al. [35] examined the effects of intradialytic exercise training on oxidative stress and EAT determined by echocardiography in ESRD patients and found that the thickness of the epicardial fat layer was reduced by 11% in patients with exercise training during the intradialytic period. Based on the results of their study, the authors concluded that exercise training might improve CVD risk factors including both EAT and oxidative stress. In our study, we found that the PD modality was associated with increased EAT, even when corrected for BMI.
Despite the simplicity of evaluating EAT with echocardiography, EAT should be measured by MDCT in three dimensions including regional thickness, cross-sectional areas, and total volume [28]. Therefore, MDCT can be used to assess both CACS and EAT in patients with ESRD for the first evaluation, and then echocardiography can be used for the follow-up period.
Our study has some limitations. First, this was a cross-sectional analysis of PD patients regarding CACS and EAT. Second, the sample size was relatively small. Another potential limitation was that CT could not determine whether calcium was in the intima or media of the arterial wall. Since this is not a prospective controlled study, we cannot draw cause-and-effect relations from our findings.
In conclusion, we found a relationship between the anatomic assessment of coronary artery lesions by MDCT and EAT in PD patients. This relationship might be attributed to increased inflammation and proinflammatory cytokines in uremic patients. Further studies are needed to determine the relationship between VC and EAT.
Disclosure Statement
The authors have no conflict of interest to declare.
References
- 1.United States Renal Data System: USRDS 2006 Annual Data Report: Atlas of End-Stage Renal Disease in United States. National Institute of Health. Bethesda: National Institute of Diabetes and Digestive and Kidney Diseases, 2006.
- 2.Parfrey PS, Foley RN, Harnett JD, Kent GM, Murray D, Barre PE. Outcome and risk factors of ischemic heart disease in chronic uremia. Kidney Int. 1996;49:1428–1434. doi: 10.1038/ki.1996.201. [DOI] [PubMed] [Google Scholar]
- 3.Collins AJ. Cardiovascular mortality in end-stage renal disease. Am J Med Sci. 2003;325:163–167. doi: 10.1097/00000441-200304000-00002. [DOI] [PubMed] [Google Scholar]
- 4.Parfrey PS, Foley RN, Harnett JD, Kent GM, Murray DC, Barre PE. Outcome and risk factors for left ventricular disorders in chronic uraemia. Nephrol Dial Transplant. 1996;11:1277–1285. [PubMed] [Google Scholar]
- 5.Turkmen K, Gorgulu N, Uysal M, Ozkok A, Sakaci T, Unsal A, Yildiz A. Fetuin-A, inflammation, and coronary artery calcification in hemodialysis patients. Indian J Nephrol. 2011;21:90–94. doi: 10.4103/0971-4065.82128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Robinson J, Tan AU, Wilensky RL, Matthai W, Munoz M, Rosas SE. Electron-beam computerized tomography correlates with coronary angiogram in chronic kidney disease patients. Am J Nephrol. 2007;27:247–252. doi: 10.1159/000101370. [DOI] [PubMed] [Google Scholar]
- 7.Haydar AA, Hujairi NM, Covic AA, Pereira D, Rubens M, Goldsmith DJ. Coronary artery calcification is related to coronary atherosclerosis in chronic renal disease patients: a study comparing EBCT-generated coronary artery calcium scores and coronary angiography. Nephrol Dial Transplant. 2004;19:2307–2312. doi: 10.1093/ndt/gfh120. [DOI] [PubMed] [Google Scholar]
- 8.Raggi P, Boulay A, Chasan-Taber S, Amin N, Dillon M, Burke SK, Chertow GM. Cardiac calcification in adult hemodialysis patients. A link between end-stage renal disease and cardiovascular disease? J Am Coll Cardiol. 2002;39:695–701. doi: 10.1016/s0735-1097(01)01781-8. [DOI] [PubMed] [Google Scholar]
- 9.Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M, Jr, Detrano R. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol. 1990;15:827–832. doi: 10.1016/0735-1097(90)90282-t. [DOI] [PubMed] [Google Scholar]
- 10.Pontone G, Andreini D, Bartorelli AL, Bertella E, Mushtaq S, Annoni A, Formenti A, Chiappa L, Cortinovis S, Baggiano A, Conte E, Bovis F, Veglia F, Foti C, Ballerini G, Fiorentini C, Pepi M: Radiation dose and diagnostic accuracy of multidetector computed tomography for the detection of significant coronary artery stenoses: a meta-analysis. Int J Cardiol 2011, E-pub ahead of print. [DOI] [PubMed]
- 11.Iacobellis G, Corradi D, Sharma AM. Epicardial adipose tissue: anatomic, biomolecular and clinical relationships with the heart. Nat Clin Pract Cardiovasc Med. 2005;2:536–543. doi: 10.1038/ncpcardio0319. [DOI] [PubMed] [Google Scholar]
- 12.Corradi D, Maestri R, Callegari S, Pastori P, Goldoni M, Luong TV, Bordi C. The ventricular epicardial fat is related to the myocardial mass in normal, ischemic and hypertrophic hearts. Cardiovasc Pathol. 2004;13:313–316. doi: 10.1016/j.carpath.2004.08.005. [DOI] [PubMed] [Google Scholar]
- 13.Shirani J, Berezowski K, Roberts WC. Quantitative measurement of normal and excessive (cor adiposum) subepicardial adipose tissue, its clinical significance, and its effect on electrocardiographic QRS voltage. Am J Cardiol. 1995;76:414–418. doi: 10.1016/s0002-9149(99)80116-7. [DOI] [PubMed] [Google Scholar]
- 14.Djaberi R, Schuijf JD, van Werkhoven JM, Nucifora G, Jukema JW, Bax JJ. Relation of epicardial adipose tissue to coronary atherosclerosis. Am J Cardiol. 2008;102:1602–1607. doi: 10.1016/j.amjcard.2008.08.010. [DOI] [PubMed] [Google Scholar]
- 15.Mazurek T, Zhang L, Zalewski A, Mannion JD, Diehl JT, Arafat H, Sarov-Blat L, O'Brien S, Keiper EA, Johnson AG, Martin J, Goldstein BJ, Shi Y. Human epicardial adipose tissue is a source of inflammatory mediators. Circulation. 2003;108:2460–2466. doi: 10.1161/01.CIR.0000099542.57313.C5. [DOI] [PubMed] [Google Scholar]
- 16.Park MJ, Jung JI, Oh YS, Youn HJ. Assessment of epicardial fat volume with threshold-based 3-dimensional segmentation in CT: comparison with the 2-dimensional short axis-based method. Korean Circ J. 2010;40:328–333. doi: 10.4070/kcj.2010.40.7.328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Eroglu S, Sade LE, Yildirir A, Bal U, Ozbicer S, Ozgul AS, Bozbas H, Aydinalp A, Muderrisoglu H. Epicardial adipose tissue thickness by echocardiography is a marker for the presence and severity of coronary artery disease. Nutr Metab Cardiovasc Dis. 2009;19:211–217. doi: 10.1016/j.numecd.2008.05.002. [DOI] [PubMed] [Google Scholar]
- 18.Abbara S, Desai JC, Cury RC, Butler J, Nieman K, Reddy V. Mapping epicardial fat with multi-detector computed tomography to facilitate percutaneous transepicardial arrhythmia ablation. Eur J Radiol. 2006;57:417–422. doi: 10.1016/j.ejrad.2005.12.030. [DOI] [PubMed] [Google Scholar]
- 19.Rumberger JA, Brundage BH, Rader DJ, Kondos G. Electron beam computed tomographic coronary calcium scanning: a review and guidelines for use in asymptomatic persons. Mayo Clin Proc. 1999;74:243–252. doi: 10.4065/74.3.243. [DOI] [PubMed] [Google Scholar]
- 20.London GM, Guerin AP, Marchais SJ, Metivier F, Pannier B, Adda H. Arterial media calcification in end-stage renal disease: impact on all-cause and cardiovascular mortality. Nephrol Dial Transplant. 2003;18:1731–1740. doi: 10.1093/ndt/gfg414. [DOI] [PubMed] [Google Scholar]
- 21.Chaowalit N, Somers VK, Pellikka PA, Rihal CS, Lopez-Jimenez F. Subepicardial adipose tissue and the presence and severity of coronary artery disease. Atherosclerosis. 2006;186:354–359. doi: 10.1016/j.atherosclerosis.2005.08.004. [DOI] [PubMed] [Google Scholar]
- 22.Wang CP, Hsu HL, Hung WC, Yu TH, Chen YH, Chiu CA, Li LF, Chung FM, Shin SJ, Lee YJ. Increased epicardial adipose tissue (EAT) volume in type 2 diabetes mellitus and association with metabolic syndrome and severity of coronary atherosclerosis. Clin Endocrinol (Oxf) 2009;70:876–882. doi: 10.1111/j.1365-2265.2008.03411.x. [DOI] [PubMed] [Google Scholar]
- 23.Ahn SG, Lim HS, Joe DY, Kang SJ, Choi BJ, Choi SY, Yoon MH, Hwang GS, Tahk SJ, Shin JH. Relationship of epicardial adipose tissue by echocardiography to coronary artery disease. Heart. 2008;94:e7. doi: 10.1136/hrt.2007.118471. [DOI] [PubMed] [Google Scholar]
- 24.Gorter PM, de Vos AM, van der Graaf Y, Stella PR, Doevendans PA, Meijs MF, Prokop M, Visseren PL. Relation of epicardial and pericoronary fat to coronary atherosclerosis and coronary artery calcium in patients undergoing coronary angiography. Am J Cardiol. 2008;102:380–385. doi: 10.1016/j.amjcard.2008.04.002. [DOI] [PubMed] [Google Scholar]
- 25.Rosito GA, Massaro JM, Hoffmann U, Ruberg FL, Mahabadi AA, Vasan RS, O'Donnell CJ, Fox CS. Pericardial fat, visceral abdominal fat, cardiovascular disease risk factors, and vascular calcification in a community-based sample: the Framingham Heart Study. Circulation. 2008;117:605–613. doi: 10.1161/CIRCULATIONAHA.107.743062. [DOI] [PubMed] [Google Scholar]
- 26.Little J, Phillips L, Russell L, Griffiths A, Russell GI, Davies SJ. Longitudinal lipid profiles on CAPD: their relationship to weight gain, comorbidity, and dialysis factors. J Am Soc Nephrol. 1998;9:1931–1939. doi: 10.1681/ASN.V9101931. [DOI] [PubMed] [Google Scholar]
- 27.McDonald SP, Collins JF, Johnson DW. Obesity is associated with worse peritoneal dialysis outcomes in the Australia and New Zealand patient populations. J Am Soc Nephrol. 2003;14:2894–2901. doi: 10.1097/01.asn.0000091587.55159.5f. [DOI] [PubMed] [Google Scholar]
- 28.Wang TD, Lee WJ, Shih FY, Huang CH, Chen WJ, Lee YT, Shih TT, Chen MF. Association of epicardial adipose tissue with coronary atherosclerosis is region-specific and independent of conventional risk factors and intra-abdominal adiposity. Atherosclerosis. 2010;213:279–287. doi: 10.1016/j.atherosclerosis.2010.07.055. [DOI] [PubMed] [Google Scholar]
- 29.Ho E, Shimada Y. Formation of the epicardium studied with the scanning electron microscope. Dev Biol. 1978;66:579–585. doi: 10.1016/0012-1606(78)90263-4. [DOI] [PubMed] [Google Scholar]
- 30.Marchington JM, Pond CM. Site-specific properties of pericardial and epicardial adipose tissue: the effects of insulin and high-fat feeding on lipogenesis and the incorporation of fatty acids in vitro. Int J Obes. 1990;14:1013–1022. [PubMed] [Google Scholar]
- 31.Stenvinkel P, Heimburger O, Paultre F, Diczfalusy U, Wang T, Berglund L, Jogestrand T. Strong association between malnutrition, inflammation, and atherosclerosis in chronic renal failure. Kidney Int. 1999;55:1899–1911. doi: 10.1046/j.1523-1755.1999.00422.x. [DOI] [PubMed] [Google Scholar]
- 32.Tintut Y, Patel J, Parhami F, Demer LL. Tumor necrosis factor-alpha promotes in vitro calcification of vascular cells via the cAMP pathway. Circulation. 2000;102:2636–2642. doi: 10.1161/01.cir.102.21.2636. [DOI] [PubMed] [Google Scholar]
- 33.Yildiz A, Tepe S, Oflaz H, Yazici H, Pusuroglu H, Besler M, Ark E, Erzengin F. Carotid atherosclerosis is a predictor of coronary calcification in chronic haemodialysis patients. Nephrol Dial Transplant. 2004;19:885–891. doi: 10.1093/ndt/gfh001. [DOI] [PubMed] [Google Scholar]
- 34.Caliskan Y, Demirturk M, Ozkok A, Yelken B, Sakaci T, Oflaz H, Unsal A, Yildiz A. Coronary artery calcification and coronary flow velocity in haemodialysis patients. Nephrol Dial Transplant. 2010;25:2685–2690. doi: 10.1093/ndt/gfq113. [DOI] [PubMed] [Google Scholar]
- 35.Wilund KR, Tomayko EJ, Wu PT, Ryong Chung H, Vallurupalli S, Lakshminarayanan B, Fernhall B. Intradialytic exercise training reduces oxidative stress and epicardial fat: a pilot study. Nephrol Dial Transplant. 2010;25:2695–2701. doi: 10.1093/ndt/gfq106. [DOI] [PubMed] [Google Scholar]