Abstract
This study examined the impact of breathing awareness meditation (BAM), life skills (LS) training, and health education (HE) interventions on self-reported hostility and 24-hour ambulatory blood pressure (ABP) in 121 African American (AA) ninth graders at increased risk for development of essential hypertension. They were randomly assigned to BAM, LS, or HE and engaged in intervention sessions during health class for 3 months. Before, after, and 3 months following intervention cessation, self-reported hostility and 24-hour ABP were measured. Results indicated that between pre- and postintervention, BAM participants displayed significant reductions in self-reported hostility and 24-hour systolic ABP. Reductions in hostility were significantly related to reductions in 24-hour systolic ABP. Between postintervention and follow-up, participants receiving LS showed a significant reduction in hostility but not in 24-hour ABP. Significant changes were not found for the HE group in 24-hour ABP or self-reported hostility, but these change scores were significantly correlated. The implications of the findings are discussed with regard to behavioral stress reduction programs for the physical and emotional health of AAs.
Keywords: essential hypertension, hostility, behavioral interventions, clinical trial, stress
Essential hypertension (EH) continues to be a major health problem in the United States (Gillum, 1994). This is especially the case among African Americans (AAs), who experience a higher prevalence rate and earlier onset of EH, as well as greater EH-related organ system damage resulting in premature mortality, than other ethnic groups (Nesbitt, 2004).
The antecedents of EH have their origin in childhood (Berenson, 2002; Berenson et al., 1982; Harshfield, Treiber, Wilson, Kapuku, & Davis, 2002; Wang et al., 2006). Epidemiologic studies have demonstrated that ethnic differences in blood pressure (BP) levels begin to manifest during childhood. For example, the Bogalusa Heart Study, a longitudinal study of BP levels of 3,500 AA and White school-age children, was one of the first studies to show that beginning at 10 years, AA children had significantly higher BP readings than their peers (Berenson, 2002; Berenson, Voors, Webber, Dalferes, & Harsha, 1979; Gidding, Bao, Srinivasan, & Berenson, 1995).
Systolic BP (SBP) and diastolic BP (DBP) levels are monotonically associated with future development of cardiovascular morbidity and mortality (Kannel, Vasan, & Levy, 2003). Adult normotensives (i.e., those with SBP/ DBP 120-129/80-84 mmHg) have a 40% increased risk, and those with high normal levels (SBP/DBP 130-139/85-89 mmHg) have two times the risk of developing EH compared with those with optimal BP levels (<120/<80 mmHg; Kannel et al., 2003). BP percentile ranking tracks from late childhood into adulthood in AA adolescents show greater stability of tracking than in the case of Whites (Bao, Threefoot, Srinivasan, & Berenson, 1995; Dekkers, Snieder, Van den Oord, & Treiber, 2002; Manatunga, Jones, & Pratt, 1993). Thus, AA adolescents with BP between the 50th and 95th percentiles for age and sex (i.e., normotensive to prehypertensive) are more likely to later develop EH or manifest early target organ damage during their young-adult years and have an increased risk of developing cardiovascular disease (CVD; Manatunga et al., 1993).
Numerous hypotheses have been posited to address the genesis of the disparate rates of EH prevalence among AAs compared with other ethnic groups, including genetic predisposition, salt sensitivity, diet and nutrition, and other contextual factors (N. B. Anderson & McNeilley, 1993; Dressler, 1993; Fray, 1993; Peters & Flack, 2000; Sowers, Zemel, & Zemel, 1993; Wilson & Grim, 1991). In regard to contextual factors, in recent decades, considerable attention has been focused on the role of chronic environmental stress as a possible cause of some of the disproportionate rates of EH among AAs (N. B. Anderson & McNeilly, 1993; N. B. Anderson, Myers, Pickering, & Jackson, 1989; Bowen-Reid & Harrell, 2002; R. Cooper, 1991; Dressler, 1993; Krieger, Rowley, Herman, Avery, & Phillips, 1993). Environmental stress-related factors (e.g., limited educational and employment opportunities, neighborhood and/or school dysfunction, unfair treatment, and discrimination related to ethnicity and/or socioeconomic status [SES] inequality) have been implicated in the development of EH (Dressler, 1993; Fray, 1993). These types of chronic environmental stress have been associated with psychological (e.g., anger, hostility, anxiety, helplessness, depression) and physical (e.g., low birth weight, infant mortality, breast cancer, chronic obstructive pulmonary disease, EH, heart disease) health problems among AAs (Armstead, Lawler, Gordon, Cross, & Gibbens, 1989; Bullock & Houston, 1987; Clark, Anderson, Clark & Williams, 1999; R. S. Cooper, 1993; Cornell, Peterson, & Richards, 1999; Harris, 1992; Novaco, 1985; D. R. Williams, Yu, Jackson, & Anderson, 1997). Since such environmental stress experiences remain an integral part of the Black experience for many in the United States (D. R. Williams & Collins, 1995), it is understandable that these stressors may play a contributory role in AAs’ disproportionate development of EH.
Increasingly, these forms of environmental stress have been viewed as being predominantly outgrowths of racism and discrimination (Clark et al., 1999). Several models have been developed in an effort to better understand the pathogenic processes and pathways in which culture-specific factors such as racism and discrimination can play a role in the health outcomes of AAs (N. B. Anderson & McNeiley, 1993; Clark et al., 1999; Dressler, 1993; Myers & McClure, 1993). For example, a primary premise of Clark et al.'s (1999) biopsychosocial model is that one's perception of a situation as a form of racism results in exaggerated psychological and physiological stress responses. Chronic exposure to environmental stress factors such as racism (e.g., sub-standard housing, lower-level employment, lower wages) is believed to influence one's personality and coping responses, which have been shown to modulate the physiological impact that can result from these stressors (Armstead et al., 1989; Jones, Harrell, Morris-Prather, Thompson, & Omowale, 1996; Morris-Prather et al., 1996). Utilization of nonadaptive coping styles/personality characteristics in response to such chronic stressors has been associated with development of EH (N. B. Anderson et al., 1989).
Hostility, as measured by the Cook Medley Hostility Inventory (CMI), is conceptualized as a multifaceted personality trait comprising a combination of suspiciousness, resentment, and cynical distrust of others that reflects a propensity for anger (Barefoot, Dodge, Peterson, Dahlstrom, & Williams, 1989; Cook & Medley, 1954). Among adults, self-reported hostility, often measured using the CMI, has been linked to EH, higher level of resting BP, and ambulatory daytime and nighttime BP (Carels, Sherwood, & Blumenthal, 1998; Durel et al., 1989; Miller, Smith, Turner, Guijarro, & Hallet, 1996; Shapiro, Goldstein, & Jamner, 1996). In addition, associations have been reported with coronary and peripheral artery disease and increased rates of all-cause and CV mortality in multiple prospective and cross-sectional investigations involving AAs and other ethnic groups (Barefoot, Dahlstrom, & Williams, 1983; D. C. Cooper & Waldstein, 2004; Durel et al., 1989; Matthews, Gump, Harris, Haney, & Barefoot, 2004; Miller et al., 1996; Shapiro et al., 1996; Shekelle, Gale, Ostfeld, & Paul, 1983). Importantly, AAs compared with Caucasian Americans report higher levels of cynical, distrusting hostility (Barefoot et al., 1991; Johnson, 1989; Musante, Treiber, Davis, Waller, & Thompson, 1999; Scherwitz, Perkins, Chesney, & Hughes, 1991). This personality/response pattern characterized by cynicism and distrust could be largely the result of the AA experience of repeated exposures from childhood onward to unfair treatment and discrimination related to ethnicity and SES inequality (Clark, Coleman, Novak, & Jeremy, 2004; Clark & Gochett, 2006; Dressler, 1993; Krieger et al., 1993; D. R. Williams et al., 1997).
Cognitive-behavioral interventions in adults have shown promise in reducing self-reported hostility levels and/or associated CVD risk factors. Gidron, Davidson, and Bata (1999) found that coronary heart disease patients who received cognitive-behavioral hostility reduction strategies once a week for 2 months significantly reduced self-reported hostility when compared with a single-session informational control group. The effects were maintained at a 2-month follow-up. Additionally, at the 2-month follow-up, intervention patients exhibited significantly greater reductions in DBP, and reductions in hostility were positively related to reductions in DBP. Davidson, Gidron, Mostofsky, and Trudeau (2007) conducted a 6-month follow-up evaluation on the participants involved in the Gidron et al. (1999) study. The cognitive-behavioral group therapy participants had fewer days of hospitalization than the control group. The average hospitalization costs were also significantly lower for the intervention group.
Few hostility reduction intervention programs have been conducted among AAs or youth. S. Williams, Waymouth, Lipman, Mills, and Evans (2004) conducted a 2-month group cognitive-behavioral skills intervention program designed to reduce hostility, anger, and aggression among 7- to 13-year olds with aggressive-behavior problems. Parents attended three sessions to learn the coping skills their children were taught. At postintervention, the children reported significant reductions in the intensity of anger, and the parents reported significant reductions in the frequency of hostility and aggression in their children. Unfortunately, the study did not provide a control group, limiting the ability to conclude whether intervention efficacy, maturational changes, or positive parental response bias led to the reported decreases in the detrimental behaviors.
Yahav and Cohen (2008) evaluated the effect of a 2-month, 1-hour/week school-based intervention program that provided cognitive-behavioral stress management training and biofeedback-assisted relaxation training for coping with stressful situations in a nonclinical group of ninth-grade adolescents. Significant improvements in self-reported state anxiety, test anxiety, and self-esteem were observed in the intervention group compared with the control group. However, self-reported hostility (Gidron, Davidson, & Ilia, 2001) was not significantly affected by the intervention program. The authors noted that in contrast to some of the other end points, hostility was not specifically addressed during the intervention. The researchers suggested that techniques that specifically focus on conflict and self-regulation may be needed before changes in hostility will be realized.
While few studies have assessed the efficacy of cognitive-behavioral intervention strategies in reducing hostility and ineffective coping styles among AAs, a number of stress reduction programs have assessed reductions in BP, primarily in AA adults (J. W. Anderson, Liu, & Kryscio, 2008; Ospina et al., 2007; Rainforth et al., 2007). Controlled studies using the Transcendental Meditation® (TM) program have shown significant BP decreases in randomized clinical trials primarily involving AA adult hypertensives (for a recent review, see J. W. Anderson et al., 2008; Rainforth et al., 2007). Mindfulness-based stress reduction (MBSR) has reduced BP in uncontrolled trials involving AA adult normotensives (Carlson, Speca, Faris, & Patel, 2007; Rosenzweig et al., 2007). Few BP-related stress reduction interventions have been conducted in AA youth; however, the findings are promising. Two controlled randomized clinical trials in AA adolescents with high normal BP found that after 2- and 4-month interventions, TM significantly lowered resting SBP/ DBP and daytime ambulatory SBP/DBP compared with health education (HE) controls (Barnes, Johnson, & Treiber, 2004; Barnes, Treiber, & Davis, 2001). A study with middle school students practicing breathing awareness meditation (BAM) reported greater decreases in resting SBP, and daytime ambulatory SBP and heart rate (HR) than in a control group (Barnes, Davis, Murzynowski, & Treiber, 2004). A 3-month randomized controlled clinical trial comparing BAM with HE among AA youth with high normal SBP found that BAM resulted in significantly greater decreases in ambulatory daytime SBP and HR and nighttime SBP (Barnes, Pendergrast, Harshfield, & Treiber, 2008).
There remains a need for development of effective and easily disseminated EH primary prevention programs for AAs. To date, no clinical trial has assessed the effectiveness of behavioral interventions in reducing self-reported hostility or the impact of changes in hostility on ambulatory BP levels. Twenty-four-hour ABP monitoring has been shown to be a better predictor of EH, and CV morbidity and mortality than office BP readings (Pickering, Shimbo, & Haas, 2006; Staessen, Gasowski, Thijs, & Fagard, 1999).
The purpose of this study was to examine among AA youth at risk for EH (i.e., SBP between the 50th and 95th percentiles) the impact of three 12-week school-based behavioral intervention strategies (i.e., HE, cognitive-behavioral life skills [LS] training, and BAM) on self-reported hostility and their association with changes in 24-hour ABP on intervention completion and at the 3-month follow-up.
Method
Participants
A total of 1,698 students who would be participating in a semester-long ninth-grade HE class were screened over the 4-year study period to determine eligibility for participation. Eligibility criteria included (1) resting SBP between the 50th and 95th percentiles for age, height, and sex on three consecutive occasions at school (National High Blood Pressure Education Program Working Group on Hypertension Control in Children and Adolescents, 1996); (2) no history of congenital heart defect, diabetes, sickle cell anemia, asthma, or any chronic illness or health problem that requires regular pharmacological treatment; (3) no current or planned engagement in a formal exercise or health promotion program (including organized individual or team sports) outside regular school physical education courses; (4) a willingness to accept randomization into treatment groups; (5) being “African American” or “Black” based on parental report; and (6) having never been pregnant at any point in the study.
Procedure
Prior to randomization, 170 students met the eligibility criteria and were available to participate in the study. Written informed consent was obtained from these individuals, who were then randomly assigned by the school to a treatment group. Twenty-six students were omitted from the statistical analyses because they were absent from school more than 30% of the time the intervention took place, and 23 were not present for posttest and/or follow-up data. No differential loss of subjects to follow-up was noted by treatment group, χ2 = 2.66, df = 2 (p = .265). The final sample consisted of 121 participants: 35 on BAM (12 males), 42 on LS (20 males), and 44 on health education (HE; 17 males). The study was approved by the Human Assurance Committee of the Medical College of Georgia. The research personnel involved with the data collection were blind to the treatment allocation.
School-based BP-screening procedures
Weight was measured by the Detecto CN20 scale (Cardinal Scale Manufacturing Co., Webb City, MO), and height was measured using a stadiometer. Resting seated SBP was recorded from the right arm with Dinamap 1846SX monitors (Critikon, Inc., Tampa, FL) for 10-minute periods (four measurements at 0, 5, 7, and 9 minutes). Each day, the first measurement was discarded, and the average of the other three measurements was used.
ABP monitoring
Ambulatory SBP, DBP, and heart rate (HR) were recorded for 24 hours pre-intervention, postintervention, and at the follow-up to the intervention. Measurements were recorded every 30 minutes during school, every 20 minutes during self-reported after-school waking hours, and every 30 minutes during self-reported sleep hours using Spacelab 90207 monitors (Spacelab, Inc., Issaquah, WA). These instruments have been validated (O'Brien, Mee, Atkins, & O'Malley, 1991), and acceptability of the ambulatory readings was based on established criteria (Barnes, Treiber, & Johnson, 2002; Harshfield et al., 2002; Treiber et al., 1994). Hourly averages were obtained by averaging all readings for each clock hour and reduced by averaging hourly averages into 24-hour periods. To be included in the analyses, means for SBP, DBP, and HR required a minimum of 50% of the total possible observations (i.e., a minimum of 26 of 51 readings for 24 hours).
Hostility measurement
The adolescent version of the Cook-Medley Hostility Inventory (ACMI) was used to assess hostility (Liehr et al., 2000). It was administered to each participant via paper-and-pencil tests at pre-intervention, postintervention, and follow-up evaluation. The ACMI comprises a 4-point response format: strongly agree, agree, disagree, and strongly disagree. It is a 23-item subset of the 50-item adult scale. To make it more age appropriate, items in the scale were altered from the adult version (Liehr et al., 2000). It is highly correlated with the 50-item scale (r = .95) and has good test-retest reliability (Woodall & Matthews, 1993). Internal consistency has been reported as .81 (Woodall & Matthews, 1989) and .75 (Liehr et al., 2000). Using pre-intervention data, it was found to be .82.
Behavioral interventions
Health/physical education teachers conducted the 12-week behavioral interventions during their regular class periods. Interventions were conducted across two high schools by six health/physical education teachers. The students taking these classes did not take physical education during that term. In each school, one teacher was randomly assigned per semester to teach an intervention and was provided supervised training by program instructors. Each teacher was certified by the program instructors as being competent to teach, and qualitative assessments of the teachers’ implementations of the programs were conducted on a weekly basis using Likert-type scale ratings (of 0-4) for thoroughness, class attentiveness, and enthusiasm. A score of 3 or 4 was used as the criterion.
Breathing awareness meditation
BAM is the primary exercise in the Mindfulness-Based Stress Reduction Program (Kabat-Zinn, & Hanh, 1990). Practice involves focusing on the moment, sustaining attention on the breathing process, and passively observing one's thoughts. The individual sits upright in a comfortable position with the eyes closed and focuses on the movements of the diaphragm while breathing in a slow, deep, relaxed manner. Each weekday, 10-minute sessions were conducted during the HE classes. The subjects were instructed to practice a 10-minute session at home each weekday and twice daily during the weekends. BAM home practice compliance was 86.6 ± 7.4% by self-reports. Average in-school attendance for participants receiving the BAM treatment was 91%.
Health education
HE lessons were conducted on a weekly basis and consisted of 50-minute sessions on CV-health-related lifestyle behaviors that were based on National Heart, Lung and Blood Institute (NHLBI) guidelines for youth (National High Blood Pressure Education Program Working Group on Hypertension Control in Children and Adolescents, 1996). Brochures, handouts, videotapes, discussions, and recommendations for increasing physical activity (e.g., walking, sports), and establishing and maintaining a prudent diet (e.g., reducing fat and sodium intake) were a part of the program. Average in-school attendance for members receiving HE treatment was 95%.
Life skills training
The 50-minute sessions were conducted on a weekly basis using selected components of Botvin Life Skills Training (Botvin, 1998), which included passive and active modeling, group discussions, behavioral homework assignments, feedback, and behavioral rehearsal and reinforcement. The selected program components provided training in problem-solving skills, reflective listening, conflict resolution, and anger management to enhance social skills, assertiveness, and personal and social competence (Botvin, Baker, Renick, Filazzola, & Botvin, 1984). Average in-school attendance for the members receiving the LS group treatment was 93%. There were no relaxation or stress reduction techniques taught in the LS or HE sessions.
Statistical analyses
Analyses of variance (ANOVA) were conducted on pre-intervention hostility values, and no significant differences were observed among the treatment groups. The ACMI hostility scores were analyzed in a 3 (treatment group) × 3 (time: pre-intervention, postintervention, follow-up evaluation) repeated-measures ANOVA. A group-by-time interaction effect was further examined using a series of two sets of paired t tests for each treatment group. The first pair examined pre- and post-ACMI score differences. The second pair examined post- and follow-up ACMI score differences.
Changes in 24-hour ambulatory measures were analyzed using a 3 (treatment group) × 3 (time: pre-intervention, postintervention, follow-up evaluation) repeated-measures ANOVA. Any significant group-by-time interaction effects were further examined using a series of two sets of paired t tests for each treatment group. The first pair examined pre- and post-score differences. The second pair examined post- and follow-up score differences. ANOVA analyses were initially conducted on pre-intervention ambulatory values, and no significant initial differences were found among the groups (all p > .42).
For significant group-by-time interactions, correlations were computed between the changes in ACMI and the changes in the dependent variables (pre to post and post to follow-up) for each of the treatment groups separately. Pearson's correlations were transformed to Fisher's z's, and confidence intervals were created to examine the differences between the correlations among groups.
Results
Anthropometric Analyses
Pre-intervention demographic and anthropometric data are shown in Table 1.
Table 1.
Demographic and Anthropometric Characteristics by Treatment Group
| Characteristic | HE (n = 44) | BAM (n = 35) | LS (n = 42) |
|---|---|---|---|
| Age (years) | 15.14 ± 0.84 | 14.93 ± 0.64 | 14.86 ± 0.61 |
| Sex ratio (male/female) | 17/27 | 12/23 | 20/22 |
| Weight (kg) | 68.18 ± 17.24 | 66.96 ± 17.80 | 70.54 ± 18.19 |
| Height (cm) | 163.62 ± 8.23 | 163.70 ± 8.10 | 166.73 ± 10.0 |
| BMI | 25.34 ± 5.78 | 24.93 ± 6.16 | 25.20 ± 5.24 |
| Percent married | 39 | 39 | 43 |
| SES | 31.02 ± 11.40 | 36.55 ± 12.63 | 36.29 ± 15.01 |
Note: BAM = breathing awareness meditation; BMI = body mass index; HE = health education; LS = life skills training; SES = socioeconomic status. Data represent means ± SD. No significant differences by treatment group observed on any characteristics. SES calculated using Hollingshead four-factor indexes.
There were no significant differences between the treatment groups on any of these parameters (all p > .10). In addition, there were no significant group-by-time interactions on any of the anthropometric variables (all p > .10).
To test for the effects of schools, a 2 (school) × 3 (intervention) ANOVA was conducted on the change scores for all dependent measures. No significant main effect of school or interactions of school by treatment were found on any of the outcome measures (all p > .10). Values for the pre-, post-, and follow-up-intervention 24-hour ambulatory hemodynamic measures by treatment group are displayed in Table 2.
Table 2.
Ambulatory Measures by Treatment Group and Evaluation Period
| Characteristic | HE (44) | BAM (35) | LS (42) |
|---|---|---|---|
| Pre-SBP24 | 121.22 ± 7.04 | 119.39 ± 6.23 | 120.07 ± 7.34 |
| Post-SBP24 | 120.85 ± 7.42 | 116.77 ± 8.00 | 119.96 ± 7.02 |
| Follow-up SBP24 | 120.34 ± 6.82 | 117.28 ± 8.08 | 121.88 ± 7.75 |
| Pre-DBP24 | 69.56 ± 6.31 | 68.11 ± 5.82 | 67.61 ± 5.49 |
| Post-DBP24 | 68.24 ± 5.96 | 66.76 ± 6.33 | 68.41 ± 5.20 |
| Follow-up DBP24 | 67.97 ± 5.79 | 66.60 ± 6.51 | 68.49 ± 5.44 |
| Pre-HR24 | 83.12 ± 9.01 | 83.01 ± 10.45 | 82.47 ± 11.81 |
| Post-HR24 | 81.36 ± 7.97 | 81.41 ± 9.16 | 83.35 ± 11.35 |
| Follow-up HR24 | 80.67 ± 9.74 | 80.19 ± 8.79 | 81.82 ± 10.87 |
Note: BAM = breathing awareness meditation; DBP = diastolic blood pressure; HE = health education; HR = heart rate; LS = life skills training; SBP = systolic blood pressure. Data represent means ± SD.
ACMI Ratings
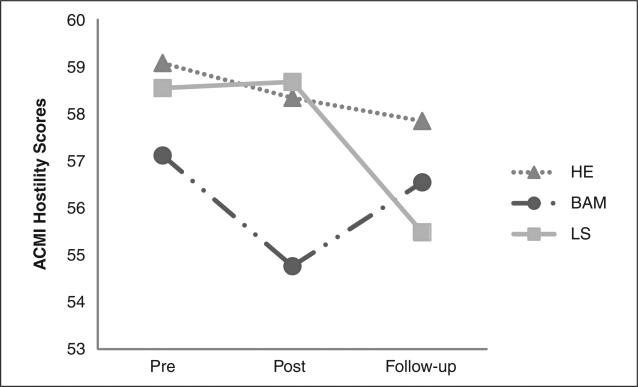
The interaction of time of measurement by treatment group was significant, F(4, 236) = 2.51, p = .04, and is displayed in Figure 1. Participants who received HE exhibited small, nonsignificant mean decreases in ACMI scores from pre- to post-intervention and from post-intervention to follow-up evaluation (both p > .70). The BAM group revealed a significant mean reduction on ACMI scores from pre- to postintervention of −2.43 ± 6.59, t(34) = 2.18, p = .036, and a slight, nonsignificant increase from postintervention to follow-up evaluation (p > .17). The LS treatment group revealed a nonsignificant decrease on ACMI scores from pre- to post-intervention (p > .88) and a significant mean increase from post-intervention to follow-up evaluation of 2.81 ± 6.18, t(41) = 2.94, p = .005.
Figure 1.
Treatment × time interaction on hostility scores
Ambulatory Hemodynamic Measures
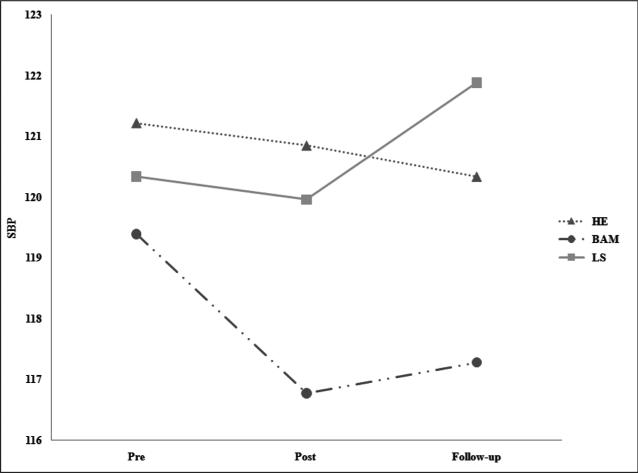
There was a significant group-by-time interaction for 24-hour SBP, F(4, 236) = 3.12, p = .016, which is depicted in Figure 2. No other significant group-by-time interactions were present (all p > .10).
Figure 2.
Treatment × time interaction on 24-hour systolic blood pressure
The subsequent paired t-test comparisons indicated that the HE and LS groups exhibited no significant mean differences in 24-hour SBP across any of the comparisons (all p > .10). The BAM group exhibited a significant reduction of 2.62 ± 6.22 mmHg between pre- and post-intervention, t(34) = 2.49, p = .018. A slight, nonsignificant increase from postintervention to follow-up evaluation was observed for the BAM group (p > .40).
Comparison of ACMI Changes With ABP Changes
Because of the treatment-by-time interaction on the ACMI, correlations comparing changes from pre- to post-intervention and from post-intervention to follow-up evaluation for 24-hour ambulatory SBP, DBP, and HR by ACMI were calculated separately for each treatment group. As can be seen in Table 3, a pattern of positive correlations was observed between changes in ACMI scores and changes in the ambulatory measurements for the BAM and HE groups. The pattern indicated that as hostility scores declined, so did hemo-dynamic parameters. In a similar fashion, if hostility scores increased, ambulatory parameters tended also to increase. The BAM group displayed a significant positive correlation between changes on the ACMI and 24-hour HR (r = .34, p < .05). The HE group displayed a significant positive correlation between changes on the ACMI and 24-hour SBP (r = .35, p < .05). The correlations between changes in the ACMI and 24-hour SBP, DBP, and HR were considerably smaller for the LS group. Examination of the magnitude of these correlations across treatment groups using Fisher's r-to-z transformation indicated higher associations for BAM and HE than for LS (both p < .05).
Table 3.
Pre- to Post- Changes in ACMI Correlated With Pre- to Post- Changes in Ambulatory Hemodynamic by Treatment Groups
| HE | BAM | LS | |
|---|---|---|---|
| N | 44 | 35 | 42 |
| ACMI | ACMI | ACMI | |
| SBP24a | .432** | .269 | –.065 |
| DBP24a | .287 | .188 | .022 |
| HR24c | .204 | .338* | –.119 |
Note: ACMI = adolescent version of the Cook-Medley Hostility Inventory; BAM = breathing awareness meditation; DBP = diastolic blood pressure; LS = life skills training; SBP = systolic blood pressure; HE = health education; HR = heart rate.
a-c Represent significant groups r to z differences at p < .05. There were no significant differences found for b.
LS vs. HE.
BAM vs. HE.
BAM vs. LS.
p < .05.
p < .001.
As seen in Table 4, during the period from postintervention to follow-up evaluation, BAM and HE exhibited significant positive correlations between changes on the ACMI and 24-hour SBP (r = .46, p < .001 and r = .35, p < .05, respectively). Similar to the pre-to-post comparisons, correlations between changes on the ACMI and 24-hour SBP, DBP, and HR were considerably smaller for the LS group. Fisher's r-to-z transformations indicated that the positive associations between change scores for 24-hour SBP and ACMI were significantly larger for BAM and HE than for the LS group (p < .05). Finally, compared with the LS group, the BAM group exhibited significantly higher positive correlations between changes on the ACMI and 24-hour DBP (p < .05).
Table 4.
Post- to Follow-Up Changes in ACMI Correlated With Post- to Follow-up Changes in Ambulatory Hemodynamics by Treatment Group
| HE | BAM | LS | |
|---|---|---|---|
| N | 44 | 35 | 42 |
| ACMI | ACMI | ACMI | |
| SBP24a,c | .351* | .460** | –.086 |
| DBP24a | .001 | .322 | –.037 |
| HR24 | .017 | –.075 | –.114 |
Note: ACMI = adolescent version of the Cook-Medley Hostility Inventory; BAM = breathing awareness meditation; DBP = diastolic blood pressure; HE = health education; HR = heart rate; LS = life skills training; SBP = systolic blood pressure.
a-c Represent significant groups r to z differences at p < .05. There were no significant differences found for b.
BAM vs. LS.
b. = BAM vs. HE.
LS vs. HE.
p < .05.
p < .001.
Discussion
This clinical trial addressed two important questions. The first was whether 3 months of school-based stress-reduction-related behavioral interventions would reduce self-reported hostility levels among a group of AA adolescents and, if so, whether the changes would be maintained 3 months following cessation of the intervention. The second question was whether the changes in hostility would be associated with changes in ABP levels on completion of the intervention and at follow-up.
Our findings indicated that the BAM and LS interventions resulted in significant reductions in self-reported hostility, which occurred at different evaluation points. Little change in hostility levels were observed for those in the HE intervention. The BAM intervention resulted in significant reductions in self-reported hostility post-intervention, whereas the LS group exhibited significant declines in hostility from post-intervention to follow-up evaluation. One possible explanation for these findings is that the LS training requires the entire 12 weeks to develop the various hostility-related coping skills, including anger management, reflective listening, effective assertiveness without aggressiveness, and so forth. With the BAM intervention, one learns the stress reduction techniques within the first day or two of practice. The fact that LS shows promise as an intervention tool for reducing hostility is in line with other school-based studies that have found LS training to be a useful tool for youth who have problematic behaviors (e.g., substance abuse conduct or behavioral problems), especially inner-city youth (Botvin et al., 1984; Botvin, Eng, & Williams, 1980; Botvin et al., 1997; Botvin & Griffin, 2002).
The HE findings support Yahav and Cohen's (2008) speculation that hostility reduction may only occur when one is taught specific skills for dealing with hostility. However, the BAM findings do not support this contention because, as in the HE program, no specific hostility or anger management skills training was provided during the intervention. The BAM technique is similar to the Benson Relaxation Response and other meditation techniques that involve slow, deep breathing. These techniques have been shown to increase parasympathetic nervous system activity, which counters sympathetic nervous system (SNS) drive (Bernardi et al., 2001; Peng et al., 1999, Pent et al., 2004). Hostility has been associated with increased SNS activity (Sherwood, Hughes, Kuhn, & Hinderliter, 2004; Virtanen et al., 2003). Thus, BAM may possibly have reduced hostility via the mechanistic pathway of increased para-sympathetic activity countering SNS drive (Bernardi et al., 2001; Peng et al., 1999; Peng et al., 2004; Sherwood et al., 2004; Virtanen et al., 2003).
Measures of 24-hour SBP and HR were affected by changes in self-reported hostility within treatment groups. In the BAM group, reductions in self-reported hostility from pre- to post-intervention were associated with reductions in 24-hour SBP and HR. Even though there were slight increases in hostility from post-intervention to follow-up evaluation for participants who received training in BAM, those who continued to show declines in hostility levels also showed continued to have declines in 24-hour SBP and HR. While the magnitude of the decrease in 24-hour SBP among the BAM group (i.e., 2.1-2.6 mmHg) may appear modest at first glance, these findings should be viewed within the context of what is known about the natural progression of BP from adolescence to adulthood. Adolescents between the 50th and 95th percentiles have been found to experience a natural increase in 24-hour SBP that ranges from 0.3 to 2.8 mmHg from 15 to 16 years of age (Urbina et al., 2008). Among adults, studies have found that the risk for stroke or coronary mortality doubles with every 20-mmHg increase in SBP throughout the range of SBP (Kannel et al., 2003; Lewington, Clarke, Qizilbash, Peto, & Collins, 2002). Therefore, a 2- to 3-mmHg lower SBP maintained from adolescence onward could result in a 12.5% lower risk of stroke- or coronary-related mortality in adulthood. Thus, the magnitude of the change in 24-hour hemodynamic function, if maintained, has considerable implications with regard to reduction of CVD risk.
The HE group exhibited significant relationships between declines in hostility and declines in 24-hour SBP from pre- to post-intervention and from post-intervention to follow-up evaluation. Although the LS group did show a significant decline in hostility from post-intervention to follow-up, no significant associations were observed for any of the 24-hour ambulatory comparisons. This study is the first to examine the impact of three types of behavioral interventions on self-reported hostility and ABP among AA youth who are at risk for later development of hypertension. The fact that the participants were not selected for any identified behavioral and anger control problems suggests that the BAM and LS interventions may hold promise in reducing levels of hostility and ABP among all AA youth. To our knowledge, this is the first study to suggest that levels of self-reported hostility among AA youth can be positively affected by breathing meditation or a cognitive-behavioral coping skills program implemented by HE teachers as part of the regular curriculum.
While these results are encouraging, they need to be interpreted cautiously until the findings are replicated. For example, there was an overall loss of 29% of the cohort over the course of the 3-month intervention and the subsequent 3-month follow-up. Attrition was to the result of low exposure to the school-based interventions (i.e., 53% of the subject loss was due to the <70% attendance rate), and the remaining sample size loss was due to missing or invalid ambulatory BP data at postintervention or follow-up evaluation. The low exposure to the school interventions was primarily the result of several of the cohorts across the 4-year period experiencing repeated cessations of classes due to bomb threats and fire alarm activations. Fortunately, every one of these occurrences was a false alert. However, this characterizes the types of background environmental stressors AAs and others living in lower-SES areas experience only too frequently. There were no treatment group differences in the percentage of losses by these categories, leading to greater confidence in the preliminary findings.
A second issue is whether the timings of the changes in hostility by treatment approach are stable. That is, if replicated, there would be implications for conducting BAM for quicker reductions in hostility and ABP, with LS being useful in reducing hostility levels but requiring a longer period of utilization of the learned coping skills.
Finally, it is unclear whether LS may result in significant improvements in ABP, which were not detected using only one 24-hour assessment at each evaluation. Situations leading to stressful interpersonal encounters are fairly infrequent. Future studies would benefit from repeated 24-hour ABP evaluations in conjunction with personal digital assistant techniques to monitor the frequency and intensity of anger- or hostility-provoking situations prior to and following the interventions. This information will provide greater clarity regarding the impact of the interventions on such feelings of emotional distress and their associations with ABP variability in the natural environment (Brondolo et al., 2003; Enkelmann et al., 2005).
If the present findings are replicated with a larger cohort, it would provide stronger evidence that these interventions could become viable nonpharmacologic approaches for improving both the physical and the emotional health of AA youth. Replication would also strengthen the argument for dissemination of these programs into the regular classroom HE curriculum. The relative low cost and ease of implementation of the programs, especially BAM, leads to their great potential for dissemination in other settings involving youth, such as churches, recreation centers, and so on.
In summary, if these preliminary findings are replicated, BAM and/or LS may be very useful prevention and intervention approaches to help curb the damaging physical and psychological impacts of repeated exposure to environmental stressors such as unfair treatment, discrimination, community violence, poor and overcrowded school settings, dysfunctional neighborhood and/or family settings, and so forth, often a continued part of the Black experience in the United States.
Acknowledgments
Funding
The author(s) disclosed receipt of the following financial support for the research and/or authorship of this article: This research was supported by NIH HL 078216.
Footnotes
Declaration of Conflicting Interests
The author(s) declared no conflicts of interest with respect to the authorship and/or publication of this.
References
- Anderson JW, Liu C, Kryscio RJ. Blood pressure response to transcendental meditation: A meta-analysis. American Journal of Hypertension. 2008;21:310–316. doi: 10.1038/ajh.2007.65. [DOI] [PubMed] [Google Scholar]
- Anderson NB, McNeilly M. Autonomic reactivity and hypertension in Blacks: Toward a contextual model. In: Fray JCS, Douglas JG, editors. Pathophysiology of hypertension in Blacks. Oxford University Press; New York, NY: 1993. pp. 107–139. [Google Scholar]
- Anderson NB, Myers HF, Pickering T, Jackson JS. Hypertension in blacks: Psychosocial and biological perspectives. Journal of Hypertension. 1989;7:161–172. [PubMed] [Google Scholar]
- Armstead C, Lawler K, Gordon G, Cross J, Gibbons J. Relationship of racial stressors to blood pressure responses and anger expression in black college students. Health Psychology. 1989;8:541–556. doi: 10.1037//0278-6133.8.5.541. [DOI] [PubMed] [Google Scholar]
- Bao W, Threefoot SA, Srinivasan SR, Berenson GS. Essential hypertension predicted by tracking of elevated blood pressure from childhood to adulthood: The Bogalusa heart study. American Journal of Hypertension. 1995;8:657–665. doi: 10.1016/0895-7061(95)00116-7. [DOI] [PubMed] [Google Scholar]
- Barefoot JC, Dahlstrom WG, Williams RB. Hostility, CHD incidence, and total mortality: A 25-year follow-up study of 255 physicians. Psychosomatic Medicine. 1983;45:59–63. doi: 10.1097/00006842-198303000-00008. [DOI] [PubMed] [Google Scholar]
- Barefoot JC, Dodge KA, Peterson BL, Dahlstrom WG, Williams RB. The Cook-Medley Hostility Scale: Item content and ability to predict survival. Psychosomatic Medicine. 1989;51:46–57. doi: 10.1097/00006842-198901000-00005. [DOI] [PubMed] [Google Scholar]
- Barefoot JC, Peterson BL, Dahlstrom WG, Siegler IC, Anderson NB, Williams RB. Hostility patterns and health implications: Correlates of Cook-Medley Hostility Scale scores in a national survey. Health Psychology. 1991;10:18–24. doi: 10.1037//0278-6133.10.1.18. [DOI] [PubMed] [Google Scholar]
- Barnes VA, Davis HC, Murzynowski JB, Treiber FA. Impact of meditation on resting and ambulatory blood pressure and heart rate in youth. Psychosomatic Medicine. 2004;66:909–914. doi: 10.1097/01.psy.0000145902.91749.35. [DOI] [PubMed] [Google Scholar]
- Barnes VA, Johnson MH, Treiber FA. Impact of transcendental meditation on ambulatory blood pressure in African American adolescents. American Journal of Hypertension. 2004;17:366–369. doi: 10.1016/j.amjhyper.2003.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnes VA, Pendergrast RA, Harshfield GA, Treiber FA. Impact of breathing awareness meditation on ambulatory blood pressure and sodium handling in prehypertensive African American adolescents. Ethnicity & Disease. 2008;8:1–5. [PMC free article] [PubMed] [Google Scholar]
- Barnes VA, Treiber FA, Davis H. Impact of transcendental meditation on cardiovascular function at rest and during acute stress in adolescents with high normal blood pressure. Journal of Psychosomatic Research. 2001;51:597–605. doi: 10.1016/s0022-3999(01)00261-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnes VA, Treiber FA, Johnson MH. Impact of stress reduction on ambulatory blood pressure in African American adolescents.. Paper presented at the American Heart Association Research Symposium; Dallas, TX. 2002. [Google Scholar]
- Berenson GS. Childhood risk factors predict adult risk associated with sub-clinical cardiovascular disease. The Bogalusa heart study. American Journal of Cardiology. 2002;90:3–7. doi: 10.1016/s0002-9149(02)02953-3. [DOI] [PubMed] [Google Scholar]
- Berenson GS, Frank GC, Hunter SM, Srinivasan SR, Voors SW, Webber LS. Cardiovascular risk factors in children. American Journal of Diseases of Children. 1982;136:855–862. doi: 10.1001/archpedi.1982.03970450097024. [DOI] [PubMed] [Google Scholar]
- Berenson GS, Voors AW, Webber LS, Dalferes ER, Harsha DW. Racial differences of parameters associated with blood pressure levels in children—The Bogalusa heart study. Metabolism: Clinical & Experimental. 1979;28:1218–1228. doi: 10.1016/0026-0495(79)90134-3. [DOI] [PubMed] [Google Scholar]
- Bernardi L, Sleight P, Bandinelli G, Cencetti S, Fattorini L, Wdowczyc-Szule J, Lagi A. Effect of rosary prayer and mantras on autonomic cardiovascular rhythms: comparative study. British Medical Journal. 2001;323:1446–1449. doi: 10.1136/bmj.323.7327.1446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Botvin GJ. Preventing adolescent drug abuse through life skills training: Theory, methods, and effectiveness. In: Crane J, editor. Social programs that work. Russell Sage Foundation; New York, NY: 1998. pp. 225–257. [Google Scholar]
- Botvin GJ, Baker E, Renick NL, Filazzola AD, Botvin EM. A cognitive-behavioral approach to substance abuse prevention. Addictive Behaviors. 1984;9:137–147. doi: 10.1016/0306-4603(84)90051-0. [DOI] [PubMed] [Google Scholar]
- Botvin GJ, Eng A, Williams CL. Preventing the onset of cigarette smoking through life skills training. Preventive Medicine. 1980;9:135–143. doi: 10.1016/0091-7435(80)90064-x. [DOI] [PubMed] [Google Scholar]
- Botvin GJ, Epstein JA, Baker E, Diaz T, Ifill-Williams M, Miller N, Cardwell J. School-based drug abuse prevention with inner-city minority youth. Journal of Child and Adolescent Substance Abuse. 1997;6:5–20. [Google Scholar]
- Botvin GJ, Griffin KW. Life skills training as a primary prevention approach for adolescent drug abuse and other problem behaviors. International Journal of Emergency Mental Health. 2002;4:41–47. [PubMed] [Google Scholar]
- Bowen-Reid TL, Harrell JP. Racist experiences and health outcomes: An examination of spirituality as a buffer. Journal of Black Psychology. 2002;28:18–36. [Google Scholar]
- Brondolo E, Rieppi R, Erickson SA, Bagiella E, Shapiro PA, McKinley P, Sloan RP. Hostility, interpersonal interactions, and ambulatory blood pressure. Psychosomatic Medicine. 2003;65:1003–1011. doi: 10.1097/01.psy.0000097329.53585.a1. [DOI] [PubMed] [Google Scholar]
- Bullock SC, Houston E. Perceptions of racism by black medical students attending white medical schools. Journal of National Medical Association. 1987;79:601–608. [PMC free article] [PubMed] [Google Scholar]
- Carels RA, Sherwood A, Blumenthal JA. Psychosocial influences on blood pressure during daily life. International Journal of Psychophysiology. 1998;28:117–129. doi: 10.1016/s0167-8760(97)00090-1. [DOI] [PubMed] [Google Scholar]
- Carlson LE, Speca M, Faris P, Patel KD. One year pre-post intervention follow-up of psychological, immune, endocrine and blood pressure outcomes of mindfulness-based stress reduction (MBSR) in breast and prostate cancer outpatients. Brain Behavior and Immunity. 2007;2021:1038–1049. doi: 10.1016/j.bbi.2007.04.002. [DOI] [PubMed] [Google Scholar]
- Clark R, Anderson NB, Clark VR, Williams DR. Racism as a stressor for African Americans: A biopsychosocial model. American Psychologist. 1999;54:805–816. doi: 10.1037//0003-066x.54.10.805. [DOI] [PubMed] [Google Scholar]
- Clark R, Coleman AP, Novak JD, Jeremy D. Brief report: Initial psychometric properties of the everyday discrimination scale in black adolescents. Journal of Adolescence. 2004;27:363–368. doi: 10.1016/j.adolescence.2003.09.004. [DOI] [PubMed] [Google Scholar]
- Clark R, Gochett P. Interactive effects of perceived racism and coping responses predict a school-based assessment of blood pressure in black youth. Annals of Behavioral Medicine. 2006;32:1–9. doi: 10.1207/s15324796abm3201_1. [DOI] [PubMed] [Google Scholar]
- Cook WW, Medley DM. Proposed hostility and Pharisaic-virtue scales for the MMPI. Journal of Applied Psychology December. 1954;38:414–418. [Google Scholar]
- Cooper R. Hypertension in Blacks—A puzzle waiting to be solved. Ethnicity and Disease. 1991;1:111–113. [PubMed] [Google Scholar]
- Cooper RS. Health and the social status of Blacks in the United States. Annals of Epidemiology. 1993;3:137–144. doi: 10.1016/1047-2797(93)90126-o. [DOI] [PubMed] [Google Scholar]
- Cooper DC, Waldstein SR. Hostility differentially predicts cardiovascular risk factors in African American and White young adults. Journal of Psychosomatic Research. 2004;57:491–499. doi: 10.1016/j.jpsychores.2004.02.017. [DOI] [PubMed] [Google Scholar]
- Cornell DG, Peterson CS, Richards H. Anger as a predictor of aggression among incarcerated adolescents. Journal of Consulting and Clinical Psychology. 1999;67:108–115. doi: 10.1037//0022-006x.67.1.108. [DOI] [PubMed] [Google Scholar]
- Davidson KW, Gidron Y, Mostofsky E, Trudeau KJ. Hospitalization cost offset of a hostility intervention for coronary heart disease patients. Journal of Consulting Clinical Psychology. 2007;75:657–662. doi: 10.1037/0022-006X.75.4.657. [DOI] [PubMed] [Google Scholar]
- Dekkers JC, Snieder H, Van den Oord EJCG, Treiber FA. Moderators of blood pressure development from childhood to adulthood: A 10-year longitudinal study in African- and European American youth. Journal of Pediatrics. 2002;141:770–779. doi: 10.1067/mpd.2002.128113. [DOI] [PubMed] [Google Scholar]
- Dressler WW. Social and cultural dimensions of hypertension in Blacks: Underlying mechanisms. In: Fray JCS, Douglas JG, editors. Pathophysiology of hypertension in blacks. Oxford University Press; New York, NY: 1993. pp. 69–89. [Google Scholar]
- Durel LA, Carver CS, Spitzer SB, Llabre MM, Weintraub JK, Saab PG, Schneiderman N. Associations of blood pressure with self-report measures of anger and hostility among black and white men and women. Health Psychology. 1989;8:557–575. doi: 10.1037//0278-6133.8.5.557. [DOI] [PubMed] [Google Scholar]
- Enkelmann HC, Bishop GD, Tong EM, Diong SM, Why YP, Khader M, Ang J. The relationship of hostility, negative affect and ethnicity to cardiovascular responses: An ambulatory study in Singapore. International Journal of Psychophysiology. 2005;56:185–197. doi: 10.1016/j.ijpsycho.2004.12.003. [DOI] [PubMed] [Google Scholar]
- Fray JCS. Hypertension in Blacks: Physiological, psychosocial, theoretical and therapeutic challenges. In: Fray JCS, Douglas JG, editors. Pathophysiology of hypertension in blacks. Oxford University Press; New York, NY: 1993. pp. 3–22. [Google Scholar]
- Gidding SS, Bao W, Srinivasan SR, Berenson GS. Effects of secular trends in obesity on coronary risk factors in children: The Bogalusa heart study. Journal of Pediatrics. 1995;127:868–874. doi: 10.1016/s0022-3476(95)70020-x. [DOI] [PubMed] [Google Scholar]
- Gidron Y, Davidson K, Bata I. The short-term effects of a hostility-reduction intervention on male coronary heart disease patients. Health Psychology. 1999;18:416–420. doi: 10.1037//0278-6133.18.4.416. [DOI] [PubMed] [Google Scholar]
- Gidron Y, Davidson K, Ilia R. Development and cross-cultural and clinical validation of a brief comprehensive scale for assessing hostility in medical settings. Journal of Behavioral Medicine. 2001;24:967–976. doi: 10.1023/a:1005631819744. [DOI] [PubMed] [Google Scholar]
- Gillum RF. Prevalence of cardiovascular and pulmonary diseases and risk factors by region and urbanization in the United States. Journal of the National Medical Association. 1994;86:105–112. [PMC free article] [PubMed] [Google Scholar]
- Harris MB. Beliefs about how to reduce anger. Psychological Reports. 1992;70:203–210. doi: 10.2466/pr0.1992.70.1.203. [DOI] [PubMed] [Google Scholar]
- Harshfield GA, Treiber FA, Wilson ME, Kapuku GK, Davis HC. A longitudinal study of ethnic differences in ambulatory blood pressure patterns in youth. American Journal of Hypertension. 2002;15:525–530. doi: 10.1016/s0895-7061(02)02267-7. [DOI] [PubMed] [Google Scholar]
- Johnson EH. The role of the experience and expression of anger and anxiety in elevated blood pressure among black and white adolescents. Journal of the National Medical Association. 1989;81:573–584. [PMC free article] [PubMed] [Google Scholar]
- Jones DR, Harrell JP, Morris-Prather CE, Thomas J, Omowale N. Affective and physiological responses to racism: The roles of Afrocentrism and mode of presentation. Ethnicity and Disease. 1996;6:109–122. [PubMed] [Google Scholar]
- Kabat-Zinn J, Hanh TN. Full catastrophe living: Using the wisdom of your body and mind to face stress, pain and illness. The program of the Stress Reduction Clinic at the University of Massachusetts Medical Center. Delta; New York, NY: 1990. [Google Scholar]
- Kannel WB, Vasan RS, Levy D. Is the relation of systolic blood pressure to risk of cardiovascular disease continuous and graded, or are there critical values? Hypertension. 2003;42:453–456. doi: 10.1161/01.HYP.0000093382.69464.C4. [DOI] [PubMed] [Google Scholar]
- Krieger W, Rowley DL, Herman AA, Avery B, Phillips MT. Racism, sexism, and social class: Implications for studies of health, disease, and well-being. American Journal of Preventive Medicine. 1993;9(Suppl. 6):82–122. [PubMed] [Google Scholar]
- Liehr P, Meininger JC, Mueller WH, Chan W, Frazier L, Reyes LR. Psychometric testing of the adolescent version of the Cook-Medley hostility scale. Issues in Comprehensive Pediatric Nursing. 2000;23:103–116. doi: 10.1080/01460860050121420. [DOI] [PubMed] [Google Scholar]
- Lewington S, Clarke R, Qizilbash N, Peto R, Collins R. Age-specific relevance of usual blood pressure to vascular mortality: A met-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360:1903–1913. doi: 10.1016/s0140-6736(02)11911-8. [DOI] [PubMed] [Google Scholar]
- Manatunga AK, Jones JJ, Pratt JH. Longitudinal assessment of blood pressures in black and white children. Hypertension. 1993;22:84–89. doi: 10.1161/01.hyp.22.1.84. [DOI] [PubMed] [Google Scholar]
- Matthews KA, Gump BB, Harris KF, Haney TL, Barefoot JC. Hostile behaviors predict cardiovascular mortality among men enrolled in the Multiple Risk Factor Intervention Trial. Circulation. 2004;109:66–70. doi: 10.1161/01.CIR.0000105766.33142.13. [DOI] [PubMed] [Google Scholar]
- Miller TQ, Smith TW, Turner CW, Guijarro ML, Hallet AJ. A meta-analytic review of research on hostility and physical health. Psychogical Bulletin. 1996;119:322–348. doi: 10.1037/0033-2909.119.2.322. [DOI] [PubMed] [Google Scholar]
- Morris-Prather C, Harrell JP, Collins R, Jefferies-Leonard K, Boss M, Lee J. Gender differences in mood and cardiovascular responses to socially stimuli. Ethnicity & Disease. 1996;6:123–131. [PubMed] [Google Scholar]
- Musante L, Treiber FA, Davis HC, Waller JL, Thompson WO. Assessment of self-reported anger expression in youth. Assessment. 1999;6:225–234. doi: 10.1177/107319119900600303. [DOI] [PubMed] [Google Scholar]
- Myers HF, McClure FH. Psychosocial factors in hypertension in Blacks: The case for an interactional perspective. In: Fray JCS, Douglas JG, editors. Pathophysiology of hypertension in blacks. Oxford University Press; New York, NY: 1993. pp. 90–106. [Google Scholar]
- National High Blood Pressure Education Program Working Group on Hypertension Control in Children and Adolescents Update on the 1987 Task Force Report on high blood pressure in children and adolescents: A working group report from the National High Blood Pressure Education Program. Pediatrics. 1996;9:649–658. [PubMed] [Google Scholar]
- Nesbitt SD. Hypertension in black patients: Special issues and considerations. Current Cardiology Reports. 2004;6:416–420. doi: 10.1007/s11886-004-0048-1. [DOI] [PubMed] [Google Scholar]
- Novaco RW. Anger and its therapeutic regulation. In: Chesney MA, Roseman RM, editors. Anger and hostility in cardiovascular and behavioral disorders. Hemisphere; New York, NY: 1985. [Google Scholar]
- O'Brien E, Mee F, Atkins N, O'Malley K. Accuracy of the Spacelabs 90207 determined by the British Hypertension Society Protocol. Journal of Hypertension. 1991;9:573–574. doi: 10.1097/00004872-199106000-00016. [DOI] [PubMed] [Google Scholar]
- Ospina MB, Bond TK, Karkhaneh M, Tjosvold L, Vandermeer B, Liang Y, Klassen TP. Meditation practices for health: State of the research. Agency for Healthcare Research and Quality; Rockville, MD: 2007. (Evidence Report/ Technology Assessment No. 155; prepared by the University of Alberta Evidence-based Practice Center under Contract No. 290-02-0023).
- Peng CK, Henry IC, Mietus JE, Hausdorff JM, Khalsa G, Benson H, Goldberger AL. Heart rate dynamics during 3 forms of meditation. International Journal of Cardiology. 2004;95:19–27. doi: 10.1016/j.ijcard.2003.02.006. [DOI] [PubMed] [Google Scholar]
- Peng CK, Mietus JE, Liu Y, Khalsa G, Douglas PS, Benson H, Goldberger AL. Exaggerated heart rate oscillations during two meditation techniques. International Journal of Cardiology. 1999;70:101–107. doi: 10.1016/s0167-5273(99)00066-2. [DOI] [PubMed] [Google Scholar]
- Peters RM, Flack JM. Salt sensitivity and hypertension in African Americans: Implications for cardiovascular nurses. Progress in Cardiovascular Nursing. 2000;15:138–144. doi: 10.1111/j.0889-7204.2000.080404.x. [DOI] [PubMed] [Google Scholar]
- Pickering TG, Shimbo D, Haas D. Ambulatory blood-pressure monitoring. New England Journal of Medicine. 2006;354:2368–2374. doi: 10.1056/NEJMra060433. [DOI] [PubMed] [Google Scholar]
- Rainforth MV, Schneider RH, Nidich SI, Gaylord-King C, Salerno J, Anderson JW. Stress reduction programs in patients with elevated blood pressure: A systematic review and meta-analysis. Current Hypertension Reports. 2007;9:520–528. doi: 10.1007/s11906-007-0094-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenzweig S, Reibel DK, Greeson JM, Edman JS, Jasser SA, McMearty KD, Goldstein BJ. Mindfulness-based stress reduction is associated with improved glycemic control in type 2 diabetes mellitus: A pilot study. Alternative Therapies in Health and Medicine. 2007;13:36–38. [PubMed] [Google Scholar]
- Scherwitz L, Perkins L, Chesney M, Hughes G. Cook-Medley Hostility Scale and subsets: Relationship to demographic and psychosocial characteristics in young adults in the CARDIA study. Psychomatic Medicine. 1991;53:36–49. doi: 10.1097/00006842-199101000-00004. [DOI] [PubMed] [Google Scholar]
- Shapiro D, Goldstein IB, Jamner LD. Effects of cynical hostility, anger out, anxiety, and defensiveness on ambulatory blood pressure in black and white college students. Psychosomatic Medicine. 1996;58:354–364. doi: 10.1097/00006842-199607000-00008. [DOI] [PubMed] [Google Scholar]
- Shekelle RB, Gale M, Ostfeld AM, Paul O. Hostility, risk of coronary heart disease, and mortality. Psychosomatic Medicine. 1983;45:109–114. doi: 10.1097/00006842-198305000-00003. [DOI] [PubMed] [Google Scholar]
- Sherwood A, Hughes JW, Kuhn C, Hinderliter AL. Hostility is related to blunted data-adrenergic receptor responsiveness among middle-aged women. Psychosomatic Medicine. 2004;66:507–513. doi: 10.1097/01.psy.0000132876.95620.04. [DOI] [PubMed] [Google Scholar]
- Sowers JR, Zemel PC, Zemel MB. Role of nutrition in Black hyper-tension: Calcium and other dietary factors. In: Fray JCS, Douglas JG, editors. Pathophysiology of hypertension in blacks. Oxford University Press; New York, NY: 1993. pp. 166–180. [Google Scholar]
- Staessen JA, Gasowski J, Thijs L, Fagard R. Diagnostic thresholds for the clinical use of ambulatory blood pressure monitoring. ACTA Physiologica et Pharmacologica Bulgarica. 1999;24:53–64. [PubMed] [Google Scholar]
- Treiber FA, Murphy JK, Davis H, Raunikar A, Pflieger K, Strong WB. Pressor reactivity, ethnicity, and 24-hour ambulatory monitoring in children from hypertensive families. Behavioral Medicine. 1994;20:133–142. doi: 10.1080/08964289.1994.9934628. [DOI] [PubMed] [Google Scholar]
- Urbina E, Alpert B, Flynn J, Hayman L, Harshfield GA, Jacobson M, Mahoney L, Daniels S. Ambulatory blood pressure monitoring in children and adolescents: Recommendations for standard assessment. Hypertension. 2008;52:433–451. doi: 10.1161/HYPERTENSIONAHA.108.190329. [DOI] [PubMed] [Google Scholar]
- Virtanen R, Jula A, Salminen JK, Voipio-Pulkki LM, Helenius H, Kuusela T, Airaksinen J. Anxiety and hostility are associated with reduced barore-flex sensitivity and increased beat-to-beat blood pressure variability. Psychosomatic Medicine. 2003;65:751–756. doi: 10.1097/01.psy.0000088760.65046.cf. [DOI] [PubMed] [Google Scholar]
- Wang X, Poole JC, Treiber FA, Harshfield GA, Hanevold CD, Snieder H. Ethnic and gender differences in ambulatory blood pressure trajectories: results from a 15-year longitudinal study in youth and young adults. Circulation. 2006;114:2780–2787. doi: 10.1161/CIRCULATIONAHA.106.643940. [DOI] [PubMed] [Google Scholar]
- Williams DR, Collins C. US socioeconomic and racial differences in health: Patterns and explanations. Annual Review of Sociology. 1995;21:349–386. [Google Scholar]
- Williams DR, Yu Y, Jackson J, Anderson N. Racial differences in physical and mental health: Socioeconomic status, stress, and discrimination. Journal of Health Psychology. 1997;2:335–351. doi: 10.1177/135910539700200305. [DOI] [PubMed] [Google Scholar]
- Williams S, Waymouth M, Lipman E, Mills B, Evans P. Evaluation of a children's temper-taming program. Canadian Journal of Psychiatry. 2004;49:607–612. doi: 10.1177/070674370404900906. [DOI] [PubMed] [Google Scholar]
- Wilson TW, Grim CE. Biohistory of slavery and blood pressure differences in blacks today. A hypothesis. Hypertension. 1991;17(Suppl. 1):122–128. doi: 10.1161/01.hyp.17.1_suppl.i122. [DOI] [PubMed] [Google Scholar]
- Woodall KL, Matthews KA. Familial environment associated with type A behaviors and psychophysiological responses to stress in children. Health Psychology. 1989;8:403–426. doi: 10.1037//0278-6133.8.4.403. [DOI] [PubMed] [Google Scholar]
- Woodall KL, Matthews KA. Changes in and stability of hostile characteristics: Results from a 4-year longitudinal study of children. Journal of Personality and Social Psychology. 1993;64:491–499. doi: 10.1037//0022-3514.64.3.491. [DOI] [PubMed] [Google Scholar]
- Yahav R, Cohen M. Evaluation of a cognitive-behavioral intervention for adolescents. International Journal of Stress Management. 2008;15:173–178. [Google Scholar]