Abstract
Existing literature related to HIV in the Dominican Republic has tended to neglect the unique role of tourism areas as distinct ecologies facilitative of sexual risk behavior, particularly HIV vulnerability and transmission. Furthermore, limited attention has focused on Dominican adolescents living in close proximity to tourism areas who have become increasingly exposed to alcohol due to the expanding tourism industry in the Dominican Republic. While most previous analyses of the effects of alcohol on adolescent sexual risk behavior have focused on the transient effects of alcohol on judgment and decision making, the effects of chronic alcohol use on sexual behavior has been a neglected area of research. Our study explores the relationship between chronic alcohol use, the parent–adolescent relationship, affective factors such as self-esteem, and intentions to engage in sex. We examine the above factors within the context of tourism areas which represent a unique ecology of alcohol availability and consumption and HIV risk. We discuss implications for developing applied family-based programs to target Dominican adolescent alcohol use and sexual risk behavior in tourism areas of high alcohol exposure.
Keywords: adolescent risk behavior, alcohol, Dominican Republic, HIV, tourism
In Dominican Republic, HIV/AIDS is a serious public health concern. The Caribbean region has the second highest rate of HIV in the world outside of sub-Saharan Africa, with a regional HIV prevalence rate1 of 1%. Among the many countries in the Caribbean, the Dominican Republic has one of the highest rates of HIV infection.2 Sentinel surveillance data suggest that 1.1% of the general Dominican population are HIV positive.2 Currently, the primary mode of HIV transmission in the Dominican Republic is via sexual behavior through both heterosexual and same sex/bisexual contacts.3 HIV prevalence rates ranging from 1% to 12% have been documented among the country’s most vulnerable populations including commercial sex workers, Haitians, and men who have sex with men (MSM).4,5 Furthermore, epidemiological data suggest that HIV prevalence in the Dominican Republic varies as a function of geographic location. Specifically, tourism areas have been documented as particularly high-prevalence locations that contribute to the spread of HIV due to factors such as population mixing, high rates of commercial sex work, and heavy alcohol and illicit drug use.6
Most research related to HIV in the Dominican Republic has tended to focus on populations deemed as being “high risk,” including, commercial sex workers, Haitians, and MSM.7–14 The extant literature related to HIV in the Dominican Republic has tended to neglect the unique role of tourism and tourism areas as distinct ecologies facilitative of HIV vulnerability and transmission.15,16 Furthermore, almost no attention has been focused on Dominican families and in particular, adolescents residing in close proximity to tourism areas. The lack of attention to the HIV prevention needs of youth is troublesome, given that Dominican adolescents are particularly vulnerable to HIV infection.10 At the end of 2008, an estimated 2700 children and adolescents under the age of 15 in the Dominican Republic were living with HIV.17 Epidemiological data about young people reveal that 18% of AIDS cases in the country occur in 15- to 24-year-olds.18 This suggests that initial HIV infection occurs in early adolescence. Among this young population group, almost half (48%) are female, double the percentage found in the adult population.18 Furthermore, factors such as early sexual debut, high birth rates, and high incidence of sexually transmitted infections (STIs) among adolescent girls and young women have compounded the risk among young people.19 For example, higher prevalence rates of STIs including syphilis and hepatitis B were reported among 15- to 29-year-olds.20 Furthermore, among young people aged 15 to 24, 29% have engaged in sexual intercourse before the age of 15 (24% of males and 33% of females).2 In terms of sexual debut, the median age at first sexual intercourse is about 13.7 years for girls and 14.8 years for boys.21 Lastly, fertility rates among women of childbearing age in the Dominican Republic are approximately 2.8 per person, a significantly high rate compared with developed countries.22 Taken together, these indicators suggest that Dominican youth are at considerable risk.
As previous research suggests, high-prevalence rates of HIV in the Dominican Republic have been found within tourism areas.6 This finding is underscored by the fact that of the more than 4.1 million tourists that visit the Dominican Republic annually, the majority come from countries with high rates of HIV infection, including the United States and western European countries such as Germany and Italy.17,23,24 This transnational connection between the DR and other high-prevalence countries constitutes an important mechanism for population mixing and greater vulnerability for the spread of HIV.24 Furthermore, in light of the burgeoning tourism economy in the DR, demographic and social changes have resulted in a large-scale convergence of internal migrants and foreign nationals in tourism areas.6 These tourism areas are characterized by a number of factors that lend themselves to high-risk behaviors. Specifically, transactional sex, engaged in and supported by both native Dominicans and tourists, has become a defining feature of these areas and has been implicated as a key factor in the region’s HIV/AIDS epidemic.6,15,16 Moreover, tourism areas typically have a high concentration of venues whose design and location have been shown to promote easy sexual encounters.6,25,26 The impact of this tourism environment on local populations cannot be underestimated. Adolescents living in and around tourism areas may be at a considerably higher risk of HIV, given their increased exposure to risk factors including greater access to alcohol and illicit drugs, early sexual debut, and involvement in commercial sex work.
Alcohol and Sexual Risk Behavior
One factor that impacts sexual risk behavior is alcohol use.27,28 Specifically, alcohol consumption has been associated with an increased risk of HIV infection.28 For example, in one study, alcohol consumers were found to be at a 77% higher risk of acquiring HIV, and those consuming alcohol prior to, or at the time of sexual relations were at an 87% higher risk.28 In developing countries such as the Dominican Republic, transnational alcohol companies have marketed and invested heavily in major tourist destinations, expanding the supply and availability of alcohol as a way to support the tourism industry.29–31 This trend has led to an increase in the number of alcohol venues for tourists, increasing exposure to alcohol among Dominican youths and families residing in close proximity to tourism areas. Among youth, the link between alcohol consumption and sexual risk-taking behaviors has been well documented.32–36 Given this association, it is important to understand the mechanisms by which alcohol affects sexual risk taking in adolescents so that effective interventions can be targeted to reduce the effects of alcohol on sexual risk.
Theories concerning the relationship between alcohol use and risky sexual behavior have largely focused on how intoxication in a given situation impacts disinhibition and cognitions about risk behavior. For instance, alcohol myopia theory contends that alcohol reduces the capacity to process multiple pieces of information during decision making and that intoxicated individuals focus more on immediate cues surrounding the sexual situation rather than the more distal cues of contracting an STI or becoming pregnant.37 Support for this theory has been mixed.38,39 A second theory emphasizes disinhibition effects and the belief that consuming alcohol reduces sexual inhibition and increases sexual pleasure. According to this theory, once drunk, these cognitions become salient and encourage people to engage in sex even if protection is not available.40–42 Support for this theory has also been somewhat mixed.43–45
Most alcohol-based interventions on sexual risk behavior have been guided by myopia theory and disinhibition (ie, expectancy) theory by targeting sexual expectancies regarding alcohol.46–53 Apart from situational effects, however, alcohol also can impact sexual risk behavior based on more chronic use. One mechanism by which chronic alcohol use may impact sexual risk taking is by its effect on affective states and disorders, such as depression and self-esteem. For example, heavy alcohol use may adversely affect youth in their dating relationships, family relationships, friendships, and school/work.46 As these facets of an adolescent’s context are adversely affected, youth may experience depression, lowered self-esteem, or other negative affective states in response to these adverse effects. These higher levels of negative affect, in turn, can impact sexual risk taking. To the extent that the effects of alcohol on sexual risk taking are mediated by adverse changes in context and, in turn, negative affective states, then these factors should be addressed in alcohol-based interventions to reduce adolescent sexual risk taking.
Alcohol, the Parent–Adolescent Relationship, and Adolescent Affective States
Self-concept is a construct that refers to an individual’s self-representations that change from situation to situation. The self-concept comprises self-conceptions that are invoked by cues in one’s immediate social environment and, by enduring, chronically accessible self-conceptions.54 The self-concept is not restricted to a person’s view of themselves in the present but also includes conceptions of future selves (eg, ideas of who a person hopes to become, who they expect to become, and who they are afraid of becoming). Previous research has shown that aspects of the self-concept can predict normal and heavy drinking behaviors.54–56 For example, self-medication models argue that as an individual’s sense of self-esteem diminishes, they tend to drink alcohol as a means of coping with diminished self-concept.48,49 Thus, negative self-esteem and negative affect lead to alcohol use. By contrast, adverse-effect models argue that alcohol use leads to negative consequences which, in turn, cause the individual to have a lowered sense of self-concept.50,51 These competing models have been evaluated in a wide range of studies, with results tending to support the prominence of adverse-effect mechanisms over self-medication mechanisms,52,52,57 though the results are not unequivocal.58,59
Previous research has established a relationship between parenting behaviors and adolescent alcohol consumption.60–63 Various family-based factors have been identified as predictors of adolescent alcohol use, including family structure, parental attitude toward alcohol use, and family bonding.64,65 Among these factors, increased parental involvement in the lives of adolescents has been shown to reduce adolescent alcohol consumption.66 Parents who foster a supportive and loving environment for their adolescents are less apt to encounter adolescent disengagement from their family, which, in turn, has been shown to be a predictor of chronic alcohol use.60,67 By the same token, low parental involvement is thought to predict higher chronic alcohol use, as adolescents use alcohol to deal with difficult relationships with their parents.68,69 Alcohol use has been viewed as a developmental strategy by which adolescents seek to disengage from their parents, become more involved with peer groups, and increase their contact with members of the opposite sex.67 Alcohol use and, in particular, chronic use, also may negatively influence an adolescent’s sense of self-esteem.54,56 Taken together, these findings strongly suggest a link between adolescent chronic alcohol use and sexual behavior. Specifically, chronic alcohol use can impact the quality of the parent–adolescent relationship and adolescent self-esteem/self-concept, which, in turn, can influence adolescent inclinations toward sexual behavior.
Chronic Alcohol Use and Early Adolescent Sexual Behavior
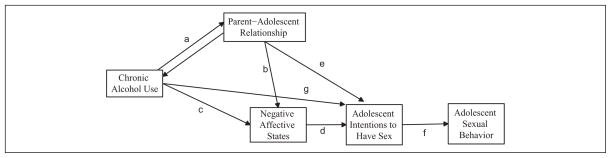
Most analyses of the effects of alcohol on adolescent sexual risk behavior have focused on the transient effects of alcohol on adolescent judgment and decision making in sexual situations. A neglected area of research has been the effects of more chronic alcohol use on adolescent sexual behavior. We collected data on a sample of 11- to 14-year-olds living in the Dominican Republic in order to address this gap in the literature. The operative model is presented in Figure 1.
Figure 1.
Chronic alcohol use and adolescent sexual behavior
Chronic alcohol use (eg, heavy drinking over the past year) is thought to create difficulties in the family as it adversely affects interactions with and the overall relationship between parents and adolescents (Figure 1, path a). Reciprocal causality is almost certainly operative, such that poor parent–adolescent relations impact adolescent alcohol use, just as adolescent alcohol use worsens parent–adolescent relations. As adolescents experience problems with their parents, they are more susceptible to negative affective states, such as low self-esteem and depression (Figure 1, path b). These negative affective states, in turn, lead adolescents to seek out sex (Figure 1, path d) and result in earlier sexual debut and sexual activity (Figure 1, path f). Chronic alcohol use can lead to negative affective states over and above its adverse impact on parent–adolescent relationships (Figure 1, path c), and adverse parent–adolescent relationships can affect sexual risk taking over and above its effects on negative affective states (Figure 1, path e). Finally, chronic alcohol use can affect sexual risk orientations over and above the particular mediators included in Figure 1 (path g).
Method
Participants
Respondents were 271 adolescents recruited using purposive sampling from 2 communities or “barrios” adjacent to the tourism town of Sosúa. Sosúa is located on the north coast of the Dominican Republic and is a popular destination for foreigners who visit the island. Project recruiters conducted door-to-door recruitment. Families with an eligible adolescent child aged 11 to 14 years were invited to participate in the study. Both mothers and adolescents were invited to participate. Informed consent was obtained from all the mothers for themselves and their adolescent children. Adolescents provided assent. The present report focuses on data gathered only from adolescents. However, mothers also were assessed on key dimensions of family life and youth involvement in risk behavior. Families were offered 500 pesos or approximately $15 dollars, $10 dollars for mothers and $5 for adolescents. Institutional review approval was obtained.
Measures
Self-esteem
A short version of the Rosenberg self-esteem scale consisting of 5 items was used to reflect negative affective states (α = 0.85). Ratings were on a 4-point disagree–agree scale, with higher scores indicating higher levels of self-esteem. The total score (ranging from 1 to 4) was the mean response across the 5 items.
Problem behaviors
Whether the adolescent had engaged in vaginal sexual intercourse was assessed by first providing an explicit definition of sexual intercourse and then asking “Have you ever had sexual intercourse?” Alcohol use was measured with 2 questions. First, youth were asked, “Have you had a drink of beer, wine, or liquor–not just a sip or taste of someone else’s drink–more than 2 or 3 times in your life?” Second, they were asked the number of days in the past year that they had 4 or more drinks in a row on a single occasion, and responded on a scale where 0 = never, 1 = 1 to 2 days, 2 = once a month, 3 = 2 to 3 days a week, 4 = 1 to 2 days a week, 5 = 3 to 5 days a week, and 6 = daily. For marijuana use, youth were asked, “have you ever smoked marijuana, even just one or two puffs?”
Adolescent relationship satisfaction
Relationship satisfaction with the mother was measured by asking adolescents to rate how satisfied they were with and how much they liked their relationship with their mother on two 4-point agree–disagree scales (α = 0.82). Higher scores indicated greater levels of satisfaction, with the total scores being the mean response on the 2 items (scored 1–4).
Intentions to engage in sexual intercourse
Intentions to engage in sex in the future were measured by the mean response to 4 items responded to on 4-point agree–disagree scales (“If I had the opportunity and it was with a boy/girl I liked a lot, I would engage in sexual intercourse;” “I think I am ready to have sexual intercourse;” “I would have sexual intercourse now if I had a boy/girl who would do it with me;” “I plan on having sexual intercourse in the next six months”). Scores could range from 1 to 4, with higher scores indicating greater intent. The α coefficient for the items was .92.
Results
Table 1 presents the percentage of adolescents who have transitioned to sexual activity, who have used alcohol, and who report having used marijuana, as a function of age and gender. Several important trends are noted. First, adolescent sexual behavior is more common among boys relative to girls. At each level of age, boys report higher percentages of having engaged in sexual intercourse than girls. The percentage of adolescents reporting having had sexual intercourse for both boys and girls significantly increased from age 13 to 14. These data suggest that preventive interventions targeting adolescents in the Dominican Republic should target youth before the age of 14, because by age 14, a significant number of youth have already transitioned to sexual intercourse.
Table 1.
Sex, Drug, and Alcohol Behaviors in Dominican Adolescents
| Had Sexual Intercourse | Tried Alcohol | At Least 1 Episode of Heavy Drinking in Past 12 Months | Smoked Marijuana | |
|---|---|---|---|---|
| Age 11 | ||||
| Male | 2.9 | 20.0 | 17.6 | 0.0 |
| Female | 0.0 | 16.7 | 16.7 | 0.0 |
| Age 12 | ||||
| Male | 3.1 | 42.4 | 39.4 | 0.0 |
| Female | 4.2 | 29.2 | 29.2 | 0.0 |
| Age 13 | ||||
| Male | 4.6 | 60.9 | 47.3 | 0.0 |
| Female | 8.8 | 64.7 | 64.7 | 0.0 |
| Age 14 | ||||
| Male | 50.0 | 93.8 | 93.8 | 0.0 |
| Female | 27.7 | 80.0 | 73.1 | 3.3 |
Table 1 also provides data related to alcohol consumption and drug use among Dominican youth. Alcohol use is considerable across all age groups, with about 1 in 3 youth reporting having had 4 or more drinks in a row at least once in the past 12 months by age 12. The percentage of girls who reported heavy episodic drinking 1 or 2 days a week or more in the past 12 months at ages 11, 12, 13, and 14, was 0%, 8.3%, 23.5%, and 25.8%, respectively. For boys, the corresponding percentages were 2.9%, 9.1%, 36.8%, and 35.7%, respectively. Thus, chronic alcohol use is not uncommon in our sample. Our data suggest that many adolescents have already had experience with alcohol as they approach decisions to engage in sexual activity. Another interesting trend in our data was the low levels of marijuana use between the ages of 11 and 14.
The model in Figure 1 was tested using structural equation modeling (SEM) for boys and girls separately. Sexual activity was not included in the model because we only had a retrospective measure of it. However, past research has consistently observed strong relationships between adolescent intentions to engage in sexual activity and future sexual activity.70 We also included a path from chronic alcohol use to intentions to engage in sex, to recognize that traditional maximum likelihood algorithms were used in the SEM, as nonnormality was not problematic (none of the absolute skewness or kurtosis indices exceeded 1.30).
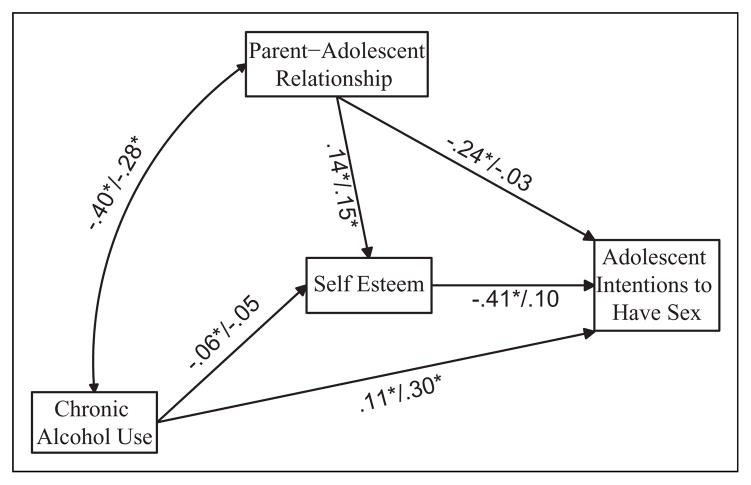
The model was just identified, hence no fit indices are presented. Figure 2 presents the unstandardized path coefficients for girls and boys, with the former listed first in parentheses. Age of the adolescent was included as a covariate for all endogenous variables, though this is omitted from the diagram to reduce clutter. Because the bidirectional path (path a) in Figure 1 is statistically underidentified, only the correlation between chronic drinking and parent–adolescent relationship is reported. This correlation can be conceptualized as representing the totality of the bidirectional dynamics but without the ability to decompose it into the separate direction effects. Residuals are expressed in standardized form.
Figure 2.
Unstandardized path coefficients for girls and boys
For adolescent girls, heavy drinking in the past year was associated with a worsening of mother–adolescent relationships (correlation = −.40, P < .05). Poor mother–daughter relationships, in turn, were associated with lower self-esteem (path coefficient = −0.14, P < .05), probably as girls lose the support of their mothers and pull away from them. Girls with low self-esteem were, in turn, more likely to turn to sexual intercourse (path coefficient = −0.41, P < .05), perhaps as a way of dealing with their lowered sense of self. These data suggest that if we can help parents to address alcohol consumption early on with their daughters so that it does not disrupt their relationships and be supportive of their daughters to prevent low self-esteem from developing, then this may help reduce HIV by reducing the likelihood of early sexual debut. Chronic alcohol use had an independent association with intentions to have sex over and above the mediators identified in Figure 2.
For boys, the dynamic is somewhat different. Heavy drinking was associated with worsening of mother–adolescent relationships and this, in turn, was associated with lower levels of self-esteem. However, lower levels of self-esteem were not significantly associated with intentions to have sexual intercourse, suggesting that boys with low self-esteem want to have sex just as much as boys with high self-esteem. Thus, the chronic drinking-lowered self-esteem-sexual intercourse dynamic was operative for Dominican girls but not boys. To be sure, parent interventions aimed at chronic drinking for adolescent boys should still be effective in reducing future risks of HIV, as evidence by the significant path linking chronic alcohol use to intentions to have sexual intercourse in the near future. But the dynamics we observed do not implicate self-esteem as a mediator of these effects for boys.
Discussion
The findings from this research have important, applied implications for the development of targeted public health programs that address Dominican adolescent alcohol use and sexual risk behavior in tourist areas in the Dominican Republic that are similar to Sosúa. The study found that there was a dramatic increase in both boys and girls reporting sexual debut by age 14 relative to earlier ages. By age 14, more than one third of girls and one half of boys in the sample reported having sexual intercourse. Given the associated risks of early sexual debut including teenage pregnancy, STIs, and HIV, these findings indicate the need for early, targeted interventions aimed at delaying adolescent sexual debut. These interventions should start in middle school, before youth turn 14 years.
A second important finding from the study was that a significant number of adolescents were experimenting with alcohol at an early age, and, indeed, a substantial minority of youth were already chronic users of alcohol by ages 13 and 14. Alcohol is very much a part of the lives of many youth, pointing to the need for programs that target alcohol use and sexual risk taking in early adolescence. With respect to drug use, we found few adolescents had experimented with marijuana prior to age 15. Further research regarding adolescent transitions to drug use is warranted, particularly in light of the widespread use of marijuana and cocaine in the Dominican Republic and the broader Caribbean region.71,72
Third, we observed statistically significant associations between chronic alcohol use and intentions to engage in sexual behavior, suggesting a link between these constructs. The vast majority of research to date on alcohol and sexual risk taking has emphasized the situational effects of alcohol use on adolescent judgment and decision making. Our research raises the distinct possibility that chronic alcohol use and mechanisms surrounding it also are important to take into account.
Most importantly, our research identified trends toward gender differences with regard to the mechanisms by which chronic alcohol use impacts sexual risk behavior. The most plausible dynamic suggested by our data is that for Dominican girls, chronic alcohol use can interfere with relationships with their mothers, which, in turn, leads to lower self-esteem as girls lose the support and respect of their parents. This lower self-esteem then motivates girls to seek out sexual partnerships, perhaps as a compensatory mechanism to deal with lowered feelings of self-worth. Such dynamics were not evident in Dominican boys. To be sure, chronic alcohol use was associated with higher intentions to engage in sexual intercourse in the future. But this effect was not mediated by the effects of alcohol use on self-esteem: boys with low self-esteem were just as motivated as boys with high self-esteem to have sex with girls. These results suggest that interventions to address the effects of alcohol on sexual risk taking may have to be structured somewhat differently for Dominican boys as opposed to girls.
As with any study, the results of our study must be interpreted within the design constraints of the research. The data were correlational, hence no causal inferences can be made with confidence. The measures of problem behavior relied on self-reports, which may reduce the validity of the measures. Specification and measurement error can produce bias in parameter estimates, and interpretations must be qualified accordingly. Finally, our results should not be generalized beyond populations typical of the youth we studied in Sosúa, a tourism area comparable to other tourism areas in the Dominican Republic that are characterized by a high concentration of alcohol venues, a large influx of international tourists, and high HIV prevalence rates. Despite these limitations, the results of the research are intriguing and suggestive and set the stage for further investigations of the timing and nature of interventions aimed at alcohol use and sexual risk taking among early adolescents residing in tourism ecologies in the Dominican Republic.
Acknowledgments
We would like to acknowledge Dr. Mark Padilla at the University of Michigan, School of Public Health for shaping the contextual information related to tourism areas and HIV transmission. We would also like to thank Dr. Jean Howard at Columbia University for support of Dr. Guilamo-Ramos’ program of research in the Dominican Republic.
Funding
Institutions that provided funding for parts of this research included Columbia University: the Vice Provost’s Office of Diversity Initiatives, the Center for the Study of Ethnicity and Race, and the Institute for Latin American Studies.
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1.Joint United Nations Program on HIV/AIDS (UNAIDS) and World Health Organization (WHO) AIDS Epidemic Update: November 2009. Geneva: World Health Organization; 2009. [Google Scholar]
- 2.Joint United Nations Program on HIV/AIDS (UNAIDS) and World Health Organization (WHO) Epidemiological Fact Sheet on HIV and AIDS: Dominican Republic 2008 Update. Geneva: World Health Organization; 2009. [Google Scholar]
- 3.Pan American Health Organization (PAHO) AIDS Surveillance in the Americas: Biannual Report. Washington, DC: World Health Organization; 2002. [Google Scholar]
- 4.Calleja JM, Walker N, Cuchi P, Lazzari S, Ghys PD, Zacarias F. Status of the HIV/AIDS epidemic and methods to monitor it in the Latin America and Caribbean region. AIDS. 2002;16(suppl 3):S3–S12. doi: 10.1097/00002030-200212003-00002. [DOI] [PubMed] [Google Scholar]
- 5.Joint United Nations Programme on HIV/AIDS (UNAIDS) Caribbean AIDS Epidemic Summary: Regional Summary. Geneva: World Health Organization; 2008. [Google Scholar]
- 6.Padilla MB, Guilamo-Ramos V, Bouris A, Reyes AM. HIV/AIDS and tourism in the Caribbean: an ecological systems perspective. Am J Public Health. 2010;100(1):70–77. doi: 10.2105/AJPH.2009.161968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Padilla MB. The embodiment of tourism among bisexually-behaving Dominican male sex workers. Arch Sex Behav. 2008;37(5):783–793. doi: 10.1007/s10508-008-9358-5. [DOI] [PubMed] [Google Scholar]
- 8.Padilla M, Castellanos D, Guilamo-Ramos V, Reyes AM, Sanchez Marte LE, Soriano MA. Stigma, social inequality, and HIV risk disclosure among Dominican male sex workers. Soc Sci Med. 2008;67(3):380–388. doi: 10.1016/j.socscimed.2008.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Padilla MB. ‘Western Union daddies’ and their quest for authenticity: an ethnographic study of the Dominican gay sex tourism industry. J Homosex. 2007;53(1–2):241–275. doi: 10.1300/J082v53n01_11. [DOI] [PubMed] [Google Scholar]
- 10.Halpern DT, de Moya A, Perez-Then E, Pappas G, Garcia Calleja JM. Understanding the HIV epidemic in the Dominican Republic: a prevention success story in the Caribbean? J Acquir Immune Defic Syndr. 2009;51(suppl 1):S52–S59. doi: 10.1097/QAI.0b013e3181a267e4. [DOI] [PubMed] [Google Scholar]
- 11.Kerrigan D, Moreno L, Rosario S, et al. Environmental-structural interventions to reduce HIV/STI risk among female sex workers in the Dominican Republic. Am J Public Health. 2006;96(1):120–125. doi: 10.2105/AJPH.2004.042200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Murray L, Moreno L, Rosario S, Ellen J, Sweat M, Kerrigan D. The role of relationship intimacy in consistent condom use among female sex workers and their regular paying partners in the Dominican Republic. AIDS Behav. 2007;11(3):463–470. doi: 10.1007/s10461-006-9184-5. [DOI] [PubMed] [Google Scholar]
- 13.Sweat M, Kerrigan D, Moreno L, et al. Cost-effectiveness of environmental-structural communication interventions for HIV prevention in the female sex industry in the Dominican Republic. J Health Commun. 2006;11(suppl 2):123–142. doi: 10.1080/10810730600974829. [DOI] [PubMed] [Google Scholar]
- 14.Brennan D. Women work, men sponge, and everyone gossips: macho men and stigmatized/ing women in a sex tourist town. Anthropol Q. 2004;77(4):705–733. [Google Scholar]
- 15.Brennan D. What’s Love Got to do With it? Transnational Desires and Sex Tourism in the Dominican Republic. Durham: Duke University Press; 2004. [Google Scholar]
- 16.Padilla M. Caribbean Pleasure Industry: Tourism, Sexuality and AIDS in the Dominican Republic. Chicago: University of Chicago Press; 2007. [Google Scholar]
- 17.Joint United Nations Programme on HIV/AIDS (UNAIDS) 2008 Report on the Global AIDS Epidemic. Geneva: World Health Organization; 2008. [Google Scholar]
- 18.Joint United Nations Programme on HIV/AIDS (UNAIDS) 2004 Epidemiological Fact Sheets on HIV/AIDS and Sexually Transmitted Infections: Dominican Republic. Geneva: World Health Organization; 2004. [Google Scholar]
- 19.United States Agency for International Development (USAID) [Accessed December 11, 2009];HIV/AIDS Health Profile: Dominican Republic. http://www.usaid.gov/our_work/global_health/aids/Countries/lac/domrep-pub_profile.pdf.
- 20.Pan American Health Organization (PAHO) Health in the Americas: Dominican Republic. Washington, DC: PAHO; 2007. [Google Scholar]
- 21. [Accessed December 11, 2009];Dominican Republic DHS Key Indicators. 2002 http://www.measuredhs.com/topics/Youth/profiles/Indicators/key_indicator_tmp.cfm?title=Dominican%20Republic%202002%20DHS.
- 22. [Accessed December 11, 2009];UNICEF: Information by country. http://www.unicef.org/infoby-country/index.html.
- 23.Caribbean Tourism Organization (CTO) Latest Statistics 2010. Barbados: Caribbean Tourism Organization; 2011. [Google Scholar]
- 24.HIV/AIDS Transnational Collaborative. Transnational Applied Research and service collaborative to address the HIV/AIDS needs of the Dominican Community in Santo Domingo and New York City Discussion Document. New York, NY: Columbia University; 2003. [Google Scholar]
- 25.Kerrigan D, Moreno L, Rosario S, Butler M, de Moya EA, Sweat M. Formative Research for a 100% Condom Program in the Dominican Report: final report prepared for the AIDSCAP project of Family Health International (FHI) Santo Domingo: USAID; 1997. [Google Scholar]
- 26.Kerrigan D, Moreno L, Rosario S, et al. Environmental-structural factors significantly associated with condom use among female sex workers in the Dominican Republic. AIDS. 2003;17(3):415–423. doi: 10.1097/00002030-200302140-00016. [DOI] [PubMed] [Google Scholar]
- 27.Shuper PA, Joharchi N, Irving H, Rehm J. Alcohol as a correlate of unprotected sexual behavior among people living with HIV/AIDS: review and meta-analysis. AIDS Behav. 2009;13(6):1021–1036. doi: 10.1007/s10461-009-9589-z. [DOI] [PubMed] [Google Scholar]
- 28.Baliunas D, Rehm J, Irving H, Shuper P. Alcohol consumption and risk of incident human immunodeficiency virus infection: a meta analysis. Int J Public Health. 2010;55(3):159–166. doi: 10.1007/s00038-009-0095-x. [DOI] [PubMed] [Google Scholar]
- 29.Parry CDH. Alcohol problems in developing countries: challenges for the new millennium. Suchtmed. 2000;2(4):216–220. [Google Scholar]
- 30.Room R, Jernigan D. The ambiguous role of alcohol in economic and social development. Addiction. 2000;95(suppl 4):S523–S535. doi: 10.1080/09652140020013755. [DOI] [PubMed] [Google Scholar]
- 31.Jernigan DH. Global status report: alcohol and young people. Geneva: World Health Organization; 2001. [Accessed May 30, 2011]. Retrieved from http://whqlibdoc.who.int/hq/2001/WHO_MSD_MSB_01.1.pdf. [Google Scholar]
- 32.Brookmeyer KA, Henrich CC. Disentagling adolescent pathways of sexual risk taking. J Prim Prev. 2009;30(6):677–696. doi: 10.1007/s10935-009-0196-6. [DOI] [PubMed] [Google Scholar]
- 33.Morrison DM, Gillmore MR, Hoppe MJ, Gaylord J, Leigh BC, Rainey D. Adolescent drinking and sex: findings from a daily diary study. Perspect Sex Reprod Health. 2003;35(4):162–168. doi: 10.1363/psrh.35.162.03. [DOI] [PubMed] [Google Scholar]
- 34.Castilla J, Barrio G, Belza MJ, de la Fuente L. Drug and alcohol consumption and sexual risk behavior among young adults: results from a national survey. Drug Alcohol Depend. 1999;56(1):47–53. doi: 10.1016/s0376-8716(99)00008-3. [DOI] [PubMed] [Google Scholar]
- 35.Cook R, Comer D, Wiesenfeld H, et al. Alcohol and drug use and related disorders: an under recognized health issue among adolescents and young adults attending sexually transmitted disease clinics. Sex Transm Dis. 2006;33(9):565–570. doi: 10.1097/01.olq.0000206422.40319.54. [DOI] [PubMed] [Google Scholar]
- 36.Cook RL, Pollock NK, Rao AK, Clark DB. Increased prevalence of herpes simplex virus type 2 among adolescent women with alcohol use disorders. J Adolesc Health. 2002;30(3):169–174. doi: 10.1016/s1054-139x(01)00339-1. [DOI] [PubMed] [Google Scholar]
- 37.Steele CM, Josephs RA. Alcohol myopia: its prized and dangerous effects. Am Psychol. 1990;45(8):921–933. doi: 10.1037//0003-066x.45.8.921. [DOI] [PubMed] [Google Scholar]
- 38.Cooper ML. Alcohol and increased behavioral risk for AIDS. Alcohol Health Res World. 1992;16(1):64–72. [Google Scholar]
- 39.Leigh BC, Stall R. Substance use and risky sexual behavior for exposure to HIV: issues in methodology, interpretation, and prevention. Am Psychol. 1993;48(10):1035–1045. doi: 10.1037//0003-066x.48.10.1035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Abbey A, Parkhill MR, Buck PO, Saenz C. Condom use with a casual partner: what distinguishes college students’ use when intoxicated? Psychol Addict Behav. 2007;21(1):76–83. doi: 10.1037/0893-164X.21.1.76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Curtin JJ, Fairchild BA. Alcohol and cognitive control: implications for regulation of behavior during response conflict. J Abnorm Psychol. 2003;112(3):424–436. doi: 10.1037/0021-843x.112.3.424. [DOI] [PubMed] [Google Scholar]
- 42.Fillmore MT, Blackburn J. Compensating for alcohol-induced impairment: alcohol expectancies and behavioral disinhibition. J Stud Alcohol. 2002;63(2):237–246. doi: 10.15288/jsa.2002.63.237. [DOI] [PubMed] [Google Scholar]
- 43.Fromme K, D’Amico EJ, Katz EC. Intoxicated sexual risk taking: an expectancy or cognitive impairment explanation? J Stud Alcohol. 1999;60(1):54–63. doi: 10.15288/jsa.1999.60.54. [DOI] [PubMed] [Google Scholar]
- 44.George WH, Stoner SA, Norris J, Lopez PA, Lehman GL. Alcohol expectancies and sexuality: a self-fulfilling prophecy analysis of dyadic perceptions and behavior. J Stud Alcohol. 2000;61(1):168–176. doi: 10.15288/jsa.2000.61.168. [DOI] [PubMed] [Google Scholar]
- 45.George WH, Stoner SA. Understanding acute alcohol effects on sexual behavior. Annu Rev Sex Res. 2000;11:92–124. [PubMed] [Google Scholar]
- 46.Bachman JG, O’Malley PM, Schulenberg JE, Johnston LD, Freedman-Doan P, Messersmith EE. The Education-Drug Use Connection: How Successes and Failures in School Relate to Adolescent Smoking, Drinking, Drug Use, and Delinquency. New York, NY: Taylor & Francis Group/Lawrence Erlbaum Associates; 2008. [Google Scholar]
- 47.Roberts RE, Andrews JA, Lewinsohn PM, Hops H. Assessment of depression in adolescents using the center for epidemiologic studies depression scale. Psychol Assessment J Consult Clin Psychol. 1990;2(2):122–128. [Google Scholar]
- 48.Johnson R, Kaplan H. Stability of psychological symptoms: drug use consequences and intervening processes. J Health Soc Behav. 1990;31(3):277–291. [PubMed] [Google Scholar]
- 49.Hesselbrock MN, Hesselbrock VM. Gender, alcoholism, and psychiatric comorbidity. In: Wilsnak R, Wilsnak S, editors. Gender and Alcohol: Individual and Social Perspectives. Piscataway: Rutgers Center of Alcohol Studies; 1997. [Google Scholar]
- 50.Tapert S, Caldwell L, Burke C. Alcohol and the adolescent brain: human studies. Alcohol Res Health. 2004;28:205–212. [Google Scholar]
- 51.Baumrind D, Moselle K. A developmental perspective on adolescent drug abuse. Adv Alcohol Subst Abuse. 1985;4(3–4):41–67. doi: 10.1300/J251v04n03_03. [DOI] [PubMed] [Google Scholar]
- 52.Mason WA, Kosterman R, Haggerty K, et al. Dimensions of adolescent alcohol involvement as predictors of young adult major depression. J Stud Alcohol Drugs. 2008;69(2):275–285. doi: 10.15288/jsad.2008.69.275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Brook DW, Brook JS, Zhang C, Cohen P, Whiteman M. Drug use and the risk of major depressive disorder. Alcohol dependence and substance use disorders. Arch Gen Psychiatry. 2002;59(11):1039–1044. doi: 10.1001/archpsyc.59.11.1039. [DOI] [PubMed] [Google Scholar]
- 54.Quinlan S, Jaccard J, Blanton H. A decision theoretic and prototype conceptualization of possible selves: implications for the prediction of risk behavior. J Pers. 2006;74(2):599–612. doi: 10.1111/j.1467-6494.2006.00386.x. [DOI] [PubMed] [Google Scholar]
- 55.Hicks JA, Schlegel RJ, Friedman RS, McCarthy DM. Alcohol primes, expectancies and the working self-concept. Psychol Addict Behav. 2009;23(3):534–538. doi: 10.1037/a0016259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Gerrard M, Gibbons FX, Reis-Bergan M, Trudea L, Vande Lune L, Buunk BP. Inhibitory effects of drinker and non-drinker prototypes on adolescent alcohol consumption. Health Psychol. 2002;21(6):601–609. doi: 10.1037//0278-6133.21.6.601. [DOI] [PubMed] [Google Scholar]
- 57.Hallfors D, Waller H, Bauer D, et al. Which comes first in adolescence–sex and drugs or depression? Am J Prev Med. 2005;29(3):163–170. doi: 10.1016/j.amepre.2005.06.002. [DOI] [PubMed] [Google Scholar]
- 58.Chassin L, Pitts S, Delucia C, Todd M. A longitudinal study of children of alcoholics: predicting young adult substance use disorders. J Abnorm Psychol. 1999;108(1):106–119. doi: 10.1037//0021-843x.108.1.106. [DOI] [PubMed] [Google Scholar]
- 59.Wells J, Horwood L, Fergusson D. Drinking patterns in mid-adolescence and psychosocial outcomes in late adolescence and early adulthood. Addiction. 2004;99(12):1529–1541. doi: 10.1111/j.1360-0443.2004.00918.x. [DOI] [PubMed] [Google Scholar]
- 60.Guilamo-Ramos V, Turrisi R, Jaccard J, Wood E, Gonzalez B. Progressing from light experiementation to heavy episodic drinking in early and middle adolescence. J Stud Alcohol. 2004;65(4):494–500. doi: 10.15288/jsa.2004.65.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Guilamo-Ramos V, Jaccard J, Turrisi R, Johansson M. Parental and school correlates of binge drinking among middle school students. Am J Public Health. 2005;95(5):894–899. doi: 10.2105/AJPH.2003.018952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Guilamo-Ramos V, Jaccard J, Turrisi R, Johansson M, Bouris A. Maternal perceptions of alcohol use by adolescents who drink alcohol. J Stud Alcohol. 2006;67(5):730–737. doi: 10.15288/jsa.2006.67.730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Abar C, Abar B, Turrisi R. The impact of parental modeling and permissibility on alcohol use and experienced negative drinking consequences in college. Addict Behav. 2009;34(6–7):542–547. doi: 10.1016/j.addbeh.2009.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Kuntsche E, van der Vorst H, Engels R. The earlier the more? Differences in the links between age at first drink and adolescent alcohol use and related problems according to quality of parent-child relationships. J Stud Alcohol Drugs. 2009;70(6):991–999. doi: 10.15288/jsad.2009.70.346. [DOI] [PubMed] [Google Scholar]
- 65.Martino S, Ellickson PL, McCarffrey D. Multiple trajectories of peer and parental influence and their association with the development of adolescent heavy drinking. Addict Behav. 2009;34(8):693–700. doi: 10.1016/j.addbeh.2009.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Dishion TJ, Nelson SE, Kavanagh K. The family check-up with high-risk adolescents: preventing early-onset substance use by parent monitoring. Behav Ther. 2003;34(4):553–571. [Google Scholar]
- 67.Dishion TJ, Poulin F, Medici Skaggs N. The ecology of premature autonomy in adolescence: biological and social influences. In: Kerns KA, Contreras JM, Neal-Barnett AM, editors. Family and Peers: Linking Two Social Worlds. Westport, CT: Praeger; 2000. pp. 27–45. [Google Scholar]
- 68.Kuntsche EN, Kuendig H. What is worse? A hierarchy of family-related risk factors predicting alcohol use in adolescence. Subst Use Misuse. 2006;41(1):71–86. doi: 10.1080/10826080500368694. [DOI] [PubMed] [Google Scholar]
- 69.McNally AM, Palfai TP, Levine RV, Moore BM. Attachment dimensions and drinking-related problems among young adults: the meditational role of coping motives. Addict Behav. 2003;28(6):1115–1127. doi: 10.1016/s0306-4603(02)00224-1. [DOI] [PubMed] [Google Scholar]
- 70.Webb TL, Sheeran P. Does changing behavioral intentions engender behavior change? A meta-analysis of the experimental evidence. Psychol Bull. 2006;132(2):249–268. doi: 10.1037/0033-2909.132.2.249. [DOI] [PubMed] [Google Scholar]
- 71.Council on Hemispheric Affairs. [Accessed December 11, 2009];Hispaniola: the Caribbean’s new be leaguers in the drug trafficking trade. http://www.coha.org/2007/07/hispaniola-the-caribbeans-new-big-leaguers-in-the-drug-trafficking-trade.
- 72.Ribando C. Dominican Republic: political and economic conditions and relations with the United States. Library of Congress. Congressional Research Service Report RS21718; 2005. [Google Scholar]