Abstract
This study investigated associations between child temperament and DSM-IV disorders in children. A total of 156 probands (97 boys, 59 girls; mean age = 10.78 years) and 154 randomly selected siblings were assessed using the Junior Temperament and Character Inventory (JTCI) and a structured DSM-IV interview. Subjects were placed in nonoverlapping groups of (1) attention-deficit hyperactivity disorder (ADHD) only, (2) disruptive behavior disorders (DBD) only, (3) DBD plus an affective and/or anxiety disorder (DBD+Int), and (4) controls with no diagnosis. Many JTCI scales were found to differ between diagnostic groups and controls. Regression analyses showed independent associations between low persistence and ADHD-only group membership, high novelty seeking (NS), and the DBD-only group and between high harm avoidance (HA) and DBD+Int group membership. The interaction NS × HA was related to the ADHD-only group. Future research is needed to determine the mechanism of these association.
Index terms: temperament, personality, children, attention-deficit hyperactivity disorder, disruptive behavior disorders
Temperament refers to individual differences in a person’s typical emotional and behavioral responses. Although details of the definition vary,1 key components of temperament include its manifestation early in life,2 genetic influence,3,4 and at least moderate stability across time.5–7
Since the classic work by Thomas and Chess,2 several organizational structures of temperament have emerged. One widely used method of temperament and character conceptualization is Cloninger’s psychobiological model, which has shown good criterion and construct validity.8,9 This model proposes four temperament dimensions of novelty seeking (NS), harm avoidance (HA), and reward dependence (RD), which reflect variability in an individual’s propensity to initiate, maintain, and inhibit behavior and emotions in response to various stimuli.10 The dimension of persistence (P) was later added as an additional temperamental factor. In addition, three higher order character dimensions of self-directedness (SD), cooperativeness (C), and self-transcendence (ST) refer to differences in self-concept as an autonomous person, an integral part of humanity, and an integral part of the universe, respectively.
Although research on temperament existed for many years outside the purview of most clinicians, there have been progressive advances in our understanding of the role of temperament in developmental psychopathology.11 One factor that has slowed consensus in this important area of research is the use across studies of different measures of both temperament and psychopathology.12
Nevertheless, several cross-sectional studies have linked various temperamental traits to behavioral problems in children and adolescents. Schmeck and Poustka13 found that high NS and low HA were significantly associated with a diagnosis of conduct disorder as well as with externalizing symptoms such as aggression and delinquency as measured by the Child Behavior Checklist (CBCL).14 A recent report found that the temperamental factors of lower task orientation and higher general activity were related to attention-deficit hyperactivity disorder (ADHD) versus controls,15 whereas oppositional defiant disorder was related to a lower mood quality. Few other temperamental differences were found between children with ADHD and controls, and the diagnosis was not associated with measures of an overall “difficult” temperament. Among internalizing disorders, major depression has been associated with higher levels of emotionality,16 as assessed by the EAS (Emotionality, Activity, and Sociability Scale) Temperment Survey.17
To gain better understanding of possible cause-and-effect relations, longitudinal designs have been employed. Using Cloninger’s taxonomy, high NS and low HA was found to predict adolescent substance abuse18,19 and early-onset antisocial behavior.20 Using multiple parent- and teacher-rated instruments, inflexibility, high emotionality, and low persistence at age 3 years was found to predict behavioral problems at age 12 years.21 The Dunedin Multidisciplinary Health and Development Study,5,22 which followed a large cohort of children from ages 3 to 21 years, found that temperamentally “undercontrolled” children at age 3 years showed more externalizing problems from ages 5 to 11 years and more externalizing and internalizing problems in adolescence. Longitudinal studies using the EAS Temperament Survey have found that high emotionality predicts levels of both internalizing and externalizing problems, as measured by the CBCL.23,24 Interestingly, neither of these studies demonstrated significant associations between activity levels and later attention problems.
One well-studied temperamental trait is behavioral inhibition, which categorically refers to a tendency toward fear and restraint when a child is faced with novel situations and people.7 Children who showed behavioral inhibition as toddlers had more anxiety disorders in childhood25 and social anxiety in adolescence26 compared with children without behavioral inhibition. In addition, behavioral disinhibition has been linked with both ADHD and comorbid mood and disruptive behavior disorders (DBD).27
In summary, a number of variously described temperamental dimensions have been associated with child psychopathology in both cross-sectional and longitudinal studies. Specific links have been found between temperament measures of risk taking and disinhibition and externalizing disorders. Corresponding relations have been found between temperamental dimensions of fearfulness, shyness, and restraint in novel situations and later anxiety disorders. Dimensions that assess a higher propensity to experience negative emotions and a relative lack of self-regulation skills have been associated with many types of behavioral problems and disorders that span diagnostic categories.
The current study was undertaken to compare temperamental dimensions across different diagnoses in a sample recruited for high rates of externalizing disorders. In contrast to much of the previous literature on this topic, we chose to use diagnosed disorders according to the Diagnostic and Statistical Manual, Fourth Edition (DSM-IV)28 rather than more dimensional measures of child psychopathology for two reasons: to maximize the relevance of this study to clinicians who typically work within a diagnosis framework and to minimize the overlap between items related to temperament and those related to psychopathology. Because diagnostic criteria require not only the presence of a symptom but also evidence of severity and impairment, they can potentially offer a more independent measure than nondiagnostic scales that do not require these thresholds. We hypothesized that many temperamental differences would be found, similar to those of some previous reports. Based on a previous investigation with youths using the same temperament instrument as this study,13 NS was expected to be higher in subjects with ADHD or other DBD compared with controls. Because the HA scale contains many items that resemble descriptions of children with behavioral inhibition, this dimension was expected to be higher in children with comorbid mood and anxiety disorders. Dimensions related to poor self-regulation, such as P and SD, were also expected to be nonspecifically associated across externalizing disorders as has been documented in longitudinal studies.5,21
An additional aim of the study was to move beyond previous work testing linear one-to-one relations between a single temperament scale and a particular diagnosis and to begin exploring the possibility that temperamental dimension may interact with each other in their associations with psychiatric illness. An interaction hypothesis would predict that the impact of a particular trait would be maximally observed only in the presence of another trait. High NS, for example, may be related to DBD but only in the presence of low P. Interactions between traits have been suggested, but not specifically tested, in previous reports13,19,21 and have been found in the relation between parent personality traits and child psychopathology.29 We predicted that the interaction between high NS and low P would be related to DBD above and beyond their individual contribution. A similar finding was predicted in the interaction between high HA and high RD in its association with internalizing disorders. Based on previous hypotheses of temperamental interactions that may underlie childhood antisocial behavior,9 we hypothesized that the interactions between high NS, low HA, and low RD would be associated with conduct and oppositional defiant disorders.
METHODS
Subjects
Subjects for this study were recruited for a family study conducted in the northeastern United States designed to examine the genetic and environmental contributions to attention and aggression. Potential families for this study were recruited from local pediatricians and psychiatrists in a university-based outpatient clinic based on a review of clinical records as well as through local newspaper advertisements and posters. Families were screened by telephone for the following demographic inclusion criteria: (1) proband child between the ages of 6 and 18 years; (2) proband child living with at least one biological parent; and (3) proband child with at least one sibling between the ages of 6 and 18 years. Those families who met these inclusion criteria where then sent the parent-rater Child Behavior Checklist (CBCL) to assess levels of behavioral problems. Four groups of probands were recruited based on the CBCL, including subjects with (1) t scores greater than 67 on the attention problems scale and less then 60 on the aggressive behavior scale; (2) t scores greater than 67 on aggressive behavior but less than 60 on the attention problems scale; (3) t scores greater than 67 on both scales; and (4) t scores less than 60 on both scales. It should be noted, however, that these CBCL groupings were only used for proband recruitment. Analyses for this study used DSM-IV diagnoses as the grouping variable. Furthermore, although siblings of the proband were rated also with the CBCL, no cutoff scores were imposed for study inclusion, and the remainder of the assessment procedures were the same for probands and siblings.
For this study, two samples were considered. The first was the group of probands as described above. The other sample consisted of one randomly selected sibling. This was done to confirm or qualify findings from the proband sample. The siblings were considered as a separate sample in order not to violate statistical assumptions of independence that would have other occurred in combining multiple family members into a single sample.
A total of 206 families were recruited into the family study. Of these, Junior Temperament and Character Inventory (JTCI) data but not diagnostic data (which required an in-person visit) were obtained for 24 probands and 26 siblings, diagnoses but not JTCI data were available for 10 probands and five siblings, and both types of data were missing for nine probands and 10 siblings. Consequently, mother-rated temperament and diagnostic data were obtained for 163 probands (101 boys, 62 girls) and 165 siblings (93 boys and 72 girls). Age, gender distribution, and socioeconomic status30 did not differ between those subjects with and without complete data. We report in this study data rated by mothers. Although an attempt was made to collect the same data from fathers about their children, we were unable to obtain a sufficient sample size for these analyses.
Measures
Diagnostic Assessment
Families participated in a 2-hour visit that took place either at the research center or their home. Diagnostic data were obtained using the Vermont Structured Diagnostic Interview,31 a structured clinical interview modified for DSM-IV28 in which mothers reported on symptoms for their children. Interviews were performed by trained interviewers and supervised by a board-certified child psychiatrist. The psychometric properties of this interview are described elsewhere.32 Briefly, the mean kappa statistics for disruptive behavior disorders (DBD) were 0.62 (range, 0.43 [conduct disorder] to 0.85 [ADHD]), whereas the mean kappa for internalizing disorders was 0.69 (range, 0.46 [separation anxiety] to 0.88 [generalized anxiety disorder]). The mean intraclass correlation coefficients for past and current symptom counts were .83 for DBD (range, .74 –.88) and .74 for internalizing disorders (range, .57–.95). Demographic variables as well as the frequencies of the rates of lifetime disorders are shown in Table 1.
Table 1.
Demographic Variables by Diagnostic Group
| Probands (N = 156)
| |||||
|---|---|---|---|---|---|
| ADHD Only (n = 25) | DBD Only (n = 30) | DBD+Int (n = 43) | No Diagnosis (n = 58) | Statistic (df) | |
| Gender (male) | 52% | 73% | 81% | 47% | χ2(3) = 15.46** |
| Age (yr), mean (SD) | 10.56 (2.40) | 10.97 (3.22) | 11.05 (2.56) | 10.59 (3.21) | F(3,152) = 0.29 |
| SES, mean (SD) | 6.52 (2.00) | 6.10 (2.35) | 6.39 (2.26) | 6.48 (2.15) | F(3,152) = 0.61 |
| CBCL total problems, mean (SD) | 40.92 (22.03)b | 58.14 (26.04)b,c | 67.64 (29.86)c | 22.22 (19.62)a | F(3,148) = 31.85*** |
| Diagnosis | |||||
| ADHD % yes | 100 | 77 | 86 | ||
| ODD % yes | 0 | 93 | 74 | ||
| CD % yes | 0 | 47 | 46 | ||
| SUD % yes | 0 | 0 | 2 | ||
| GAD % yes | 0 | 0 | 70 | ||
| OCD % yes | 0 | 0 | 2 | ||
| SAD % yes | 0 | 0 | 37 | ||
| MDD % yes | 0 | 0 | 65 | ||
| BDP % yes | 0 | 0 | 42 | ||
| Dysth % yes | 0 | 0 | 9 | ||
|
| |||||
| Siblings (N = 154)
| |||||
| ADHD Only (n = 24) | DBD Only (n = 32) | DBD+Int (n = 23) | No Diagnosis (n = 75) | Statistic (df) | |
|
| |||||
| Gender (male) | 62% | 81% | 65% | 45% | χ2(3) = 12.76** |
| Age (yr), mean (SD) | 10.13 (3.15) | 10.56 (2.75) | 11.70 (3.11) | 10.84 (3.73) | F(3,150) = 0.92 |
| SES, mean (SD) | 7.04 (1.80) | 6.00 (2.21) | 5.65 (2.67) | 7.03 (1.72) | F(3,150) = 4.19** |
| CBCL total problems, mean (SD) | 34.35 (17.36)b | 42.78 (23.62)b | 64.26 (31.71)c | 13.67 (11.11)a | F(3,141) = 43.57*** |
| Diagnosis | |||||
| ADHD % yes | 100 | 62 | 87 | ||
| ODD % yes | 0 | 97 | 74 | ||
| CD % yes | 0 | 28 | 39 | ||
| SUD % yes | 0 | 3 | 4 | ||
| GAD % yes | 0 | 0 | 39 | ||
| OCD % yes | 0 | 0 | 4 | ||
| SAD % yes | 0 | 0 | 48 | ||
| MDD % yes | 0 | 0 | 43 | ||
| BDP % yes | 0 | 0 | 43 | ||
| Dysth % yes | 0 | 0 | 4 | ||
DBD+Int, disruptive behavior disorder plus an affective and/or anxiety disorder; SES, socioeconomic status; CBCL, Child Behavior Checklist; ADHD, attention deficit hyperactivity disorder; ODD, oppositional defiant disorder; CD, conduct disorder; SUD, substance use disorder; GAD, generalized anxiety disorder; OCD, obsessive-compulsive disorder; SAD, separation anxiety disorder; MDD, major depressive disorder; BPD, bipolar disorder; Dysth, dysthymic disorder.
Groups with the same letter do not significantly differ (p < .05) from each other using pairwise comparison (Tukey’s honestly significant difference test).
p < .05;
p < .01;
p < .001.
For the current study, four nonoverlapping diagnostic groups were created: (1) subjects meeting criteria for attention-deficit hyperactivity (ADHD)-only, (2) subjects with or without ADHD who also met criteria for at least one other DBD, i.e., oppositional defiant disorder and/or conduct disorder (DBD-only group), (3) subjects meeting criteria for a DBD (ADHD, oppositional defiant disorder, conduct disorder) and an internalizing disorder including an affective disorder, anxiety disorder, or both (DBD+Int), and (4) a control group of subjects without a psychiatric diagnosis. Because of the recruitment strategies described above, we did not have enough subjects to include a group with only an affective and/or anxiety disorder. Those subjects (six probands and 11 siblings) were excluded from these analyses. One proband with only a substance abuse diagnosis was also not included in these analyses. This left a total of 156 in the proband group and 154 in the sibling group. As shown in Table 1, the DBD+Int appeared to have higher overall severity than the other groups as assessed by the Total Problems scale of the CBCL.
Temperament Assessment
Child temperament was assessed using the JTCI.33 This scale is the downward extension of the Temperament and Character Inventory (TCI),34 which is an internationally used instrument of temperament and character assessment with good psychometric properties demonstrated across cultures.10,35,36 The JTCI itself has received validation from several studies, although the Fantasy and Spirituality scales have shown lower reliability.37–39
The JTCI consists of 108 statements that the respondent rates as true or false. The measure is designed to be a trait as opposed to a state instrument by instructing respondents to rate how the person usually acts and feels. In this study, we report on the parent-rated version in which the mother completed the questionnaire on each proband and sibling.
The dimensions of the JTCI are very similar to the those of the TCI. The four temperament dimensions, novelty seeking (NS), harm avoidance (HA), reward dependence (RD), and persistence (P) are identical with the TCI. The NS dimension includes items relating to exploratory and risk-taking behavior, e.g., “Even when my child is aware of potential danger, he/she still takes risks.” Harm avoidance (HA) includes items related to shyness, fatigability, and anticipatory worry, e.g., “My child worries more than others that bad things will happen.” Reward dependence (RD) refers to a tendency toward affiliation and sentimentality, e.g., “My child seems to talk about personal things with his/her friends.” The persistence (P) factor measures levels of effort and perseverance, e.g., “My child pushes him/herself to the limit when pursuing a goal.”
There are also four character dimensions of the JTCI. These character dimensions reflect somewhat higher order structures incorporating greater environmental and cultural influence. Self-directedness (SD) includes goal-directed activity, responsibility, and self-satisfaction, e.g., “My child is good at keeping promises.” Cooperativeness (C) includes aspects of helpfulness and compassion, e.g., “My child really likes to help others.” The one structural difference between the TCI and JTCI is that the self-transcendence dimension on the TCI is divided on the JTCI into fantasy, which rates levels of imagination, unconventional thinking, and propensity to daydream, e.g., “My child sometimes feels he/she can predict the future,” and spirituality, which measures religious experiences and spiritual connections to others and the universe, e.g., “My child feels sometimes feels that all living things are connected.”
Each question on the JTCI loads onto one of the eight subscales. The number of items for each dimension ranges from five (fantasy and spirituality) to 22 (harm avoidance). Total scores on each dimension are obtained by summing the number of positive responses for each dimension.
Data Analysis
One-way analysis of variance (ANOVA) procedures were used to compare the eight JTCI scores among the four diagnostic groups. Using a Bonferroni correction, significance level for these analyses was set at p < .006 to account for the eight ANOVAs performed for probands and siblings, respectively. Post hoc Tukey honestly significant difference comparisons were used to examine pairwise differences between groups only when the overall ANOVA was found to be significant. Because six pairwise comparisons were done for each significant ANOVA, the significance level for these analyses was set at p < .008. To investigate the independent effect of each JTCI dimension on the diagnostic group, those dimensions found to be significantly different from controls were entered into a logistic regression model. These variables were entered in a second step after the inclusion of any demographic variables found to significantly differ between groups. Odds ratios (OR) with 95% confidence intervals (CI) are presented. Finally, the six potential interaction terms among the four temperamental dimensions (e.g., NS × HA) were entered as a third step in the regression models to test their independent association with each child diagnostic group. Three regressions were done for each proband and sibling, and we thus set the significance level of the overall model at .01. Because of a violation of independence, probands and siblings of probands were analyzed and presented separately.
RESULTS
Junior Temperament and Character Inventory Profiles and Child DSM-IV Diagnoses
Some Junior Temperament and Character Inventory (JTCI) dimensions showed significant differences across nearly every diagnosis studied, whereas others appeared to show differences that were more diagnosis specific, as shown in Table 2. There was generally good agreement between the sibling and control samples.
Table 2.
Mean Scores of (Mother-Rated) Junior Temperament and Character Inventory Scales by DSM-IV Diagnostic Group
| Probands (N = 156)
| |||||||||
|---|---|---|---|---|---|---|---|---|---|
| ADHD Only (n = 25)
|
DBD Only (n = 30)
|
DBD+Int (n = 43)
|
No Diagnosis (n = 58)
|
F | |||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | ||
| Novelty seeking | 9.12 | 3.24a,b | 12.47 | 2.60c | 10.49 | 4.27b,c | 6.90 | 3.74a | 17.58* |
| Harm avoidance | 7.43 | 4.66a | 7.11 | 4.84a | 13.06 | 5.45b | 8.22 | 5.06a | 11.73* |
| Reward dependence | 6.96 | 1.90a,b | 4.97 | 2.53b,c | 4.65 | 2.97c | 6.99 | 2.14a | 10.64* |
| Persistence | 1.44 | 1.08b | 1.37 | 1.38b | 2.10 | 1.77a,b | 3.13 | 1.62a | 11.64* |
| Self-directedness | 10.60 | 3.55b | 9.90 | 4.02b | 9.44 | 9.44b | 15.21 | 3.67a | 22.44* |
| Cooperativeness | 16.20 | 2.53a | 11.80 | 4.61b | 12.60 | 5.26b | 16.96 | 2.73a | 17.10* |
| Fantasy | 1.88 | 1.09b | 0.71 | 1.09a | 1.31 | 0.73a,b | 0.73 | 0.83a | 10.51* |
| Spirituality | 2.08 | 1.44 | 1.07 | 1.20 | 1.64 | 1.44 | 1.84 | 1.62 | 2.58 |
|
| |||||||||
| Siblings (N = 154)
| |||||||||
| ADHD Only (n = 24)
|
DBD Only (n = 32)
|
DBD+Int (n = 23)
|
No Diagnosis (n = 75)
|
F | |||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | ||
|
| |||||||||
| Novelty seeking | 9.04 | 3.04a,b | 11.53 | 3.55b | 9.70 | 4.34a,b | 7.21 | 3.21a | 12.57* |
| Harm avoidance | 6.84 | 4.58a | 8.97 | 5.26a | 13.57 | 4.93b | 6.99 | 4.13a | 13.23* |
| Reward dependence | 7.00 | 2.48a,b | 4.78 | 2.61c | 5.16 | 2.43b,c | 7.20 | 1.86a | 11.90* |
| Persistence | 1.71 | 1.68b | 1.97 | 1.75b | 2.00 | 1.83a,b | 3.37 | 1.74a | 9.12* |
| Self-directedness | 12.04 | 4.64b | 10.60 | 4.03b | 8.79 | 5.49b | 15.89 | 3.37a | 24.75* |
| Cooperativeness | 16.25 | 3.63a | 11.68 | 4.39b | 12.59 | 4.94b | 17.17 | 2.60a | 22.74* |
| Fantasy | 1.08 | 0.88 | 0.94 | 1.08 | 1.78 | 1.59 | 0.86 | 0.90 | 2.93 |
| Spirituality | 1.79 | 1.61a,b | 0.94 | 1.08b | 1.78 | 1.59a,b | 1.99 | 1.57a | 3.74 |
ADHD, attention-deficit hyperactivity disorder; DBD, disruptive behavior disorder; DSD+Int, DBD plus an affective and/or anxiety disorder. Groups with the same letter do not significantly differ (p < .008) from each other using pairwise comparison (Tukey’s honestly significant difference test).
p< .001.
For both probands and siblings, the dimension self-directedness was significantly lower in affected children versus controls regardless of diagnostic group, whereas the diagnostic groups did not differ from each other. A similar pattern was found for persistence with the exception that the disruptive behavior disorder (DBD) plus an affective and/or anxiety disorder (DBD+Int) group did not significantly differ from controls ( p = .008) at this more conservative level. Novelty seeking was higher in the DBD-only group compared with controls and in the proband group also in comparison to the ADHD-only group. The DBD+Int group also had higher NS scores compared with controls in probands, whereas the ADHD-only and control groups did not significantly differ from each other. Harm avoidance was significantly higher in the DBD+Int group compared with all other groups. Cooperativeness, and to a lesser degree reward dependence, were rated lower in the DBD-only and the DBD+Int group compared with the ADHD-only group and controls.
The fantasy and spirituality dimensions showed a somewhat less consistent pattern. In the proband sample, levels of fantasy were significantly higher in the ADHD-only compared with the DBD-only and control groups. The spirituality dimension, however, was not significantly different between groups. In siblings, the overall ANOVAs for both the fantasy and spirituality dimensions were not significant.
To further examine the complex pattern of results with regards to NS, comparisons of NS scores were performed between subjects with inattentive ADHD versus those with the combined or hyperactive/impulsive subtype as further inspection revealed that the ADHD-only group contained a relatively high proportion of inattentive subtype subjects (in probands, 76% compared with 35% and 24% of subjects with inattentive ADHD within the DBD-only and DBD+Int groups, respectively). ANOVA revealed that ADHD pro-bands with the combined/hyperactive-impulsive subtype had significantly higher NS scores than those with the inattentive subtype (NS = 12.16 versus 9.31; F(1,83) = 15.22, p < .001). The corresponding analysis with siblings, however, was significant only at the trend level (NS = 11.28 versus 9.63; F(1,62) = 3.13, p = .08).
Logistic Regressions
To further test relations between the JTCI and diagnostic group, those dimensions and demographic variables that significantly differed between each diagnostic group and controls were entered into a logistic regression. Proband or sibling diagnostic group versus controls (e.g., proband DBD-only group membership versus control group membership) was the dependent variable. Those demographic variables that significantly differed between groups (sex in probands; sex and socioeconomic status for siblings) were entered into the first step of the model. In step 2, those JTCI dimensions found to be significantly different from controls were entered. As an example, the model to predict proband DBD-only versus control group status contained sex entered in step 1 followed by NS, RD, persistence, self-directedness, and cooperativeness all entered simultaneously in step 2.
The regression models predicting diagnostic group status versus controls from the JTCI dimensions were in each case highly significant ( p < .001). For the ADHD-only group, lower persistence (odds ratio [OR] 0.49, 95% CI 0.27–0.89) and higher fantasy (OR 2.90, 95% CI 1.47–5.72) made significant independent contributions in probands, although this was not the case for siblings. For the DBD-only group, higher NS (OR 1.38, 95% CI 1.09–1.74) emerged as the only independent predictor for the proband sample only. For the DBD+Int group, higher HA (OR 1.27, 95% CI 1.09–1.46 in probands; OR 1.35, 95% CI 1.11–1.66 in siblings) was a significant independent predictor for both samples with the addition of high NS (OR 1.32, 95% CI 1.06–1.65) and low self-directedness (OR 0.77, 95% CI 0.62–0.96) also making significant independent contributions in the proband sample. Using separate analyses, the JTCI dimensions in total showed strong overall associations with diagnostic group, accounting for 54% and 25% of variance within the ADHD-only group, 52% and 39% of variance in the DBD-only group, and 46% and 50% of variance in the DBD+Int group, for proband and siblings, respectively, after controlling for sex, age, and socioeconomic status.
Logistic Regressions with Interaction Terms
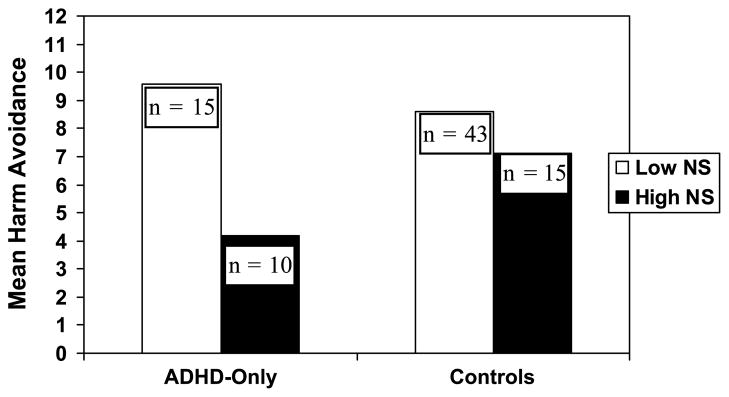
The third step in each regression was the addition of interaction terms for the four JTCI temperament variables (NS, HA, RD, P) to test their independent associations with diagnoses. A total of six interactions terms (for example, NS × HA) were entered for each diagnostic group. Results revealed one significant interaction term after controlling for significant demographic variables and the main effects of the significant JTCI scales. This was the interaction between NS and HA in predicting proband ADHD-only group membership versus controls (β = .97, p < .05). To further understand the nature of this interaction, subjects were grouped into having high or low NS based on the mean value of the total sample. As shown in Figure 1, high NS was related to low HA in children with ADHD, whereas in controls, HA scores did not relate to levels of NS. In addition, of the 15 subjects with ADHD with the combination of lower NS and higher HA, 14 (93%) of them had the inattentive subtype of ADHD.
FIGURE 1.
Interaction between novelty seeking and harm avoidance in probands with attention-deficit hyperactivity disorder (ADHD) only. Harm avoidance (HA) × novelty seeking (NS) interaction (β = .97, p < .05).
DISCUSSION
This study compared child temperament and character scores among children with different psychiatric diagnoses and controls. Although many temperament and character differences were found across diagnostic groups, the pattern of these differences varied depending on the dimension studied. Some dimensions, such as lower self-directedness and lower persistence, were present across diagnostic categories and appeared to be related to any psychiatric diagnosis relative to controls. These scales assess a person’s degree of self-acceptance, purposefulness, and self-discipline and bear resemblance to other temperamental measures of self-regulation found to be important in other reports.21,22,40,41 It is possible that low levels of self-determination and persistence convey general risk to many psychiatric disorders. The fantasy and spirituality dimensions, by contrast, showed a less consistent pattern across probands and controls. This may be accounted for by the questionable reliability and validity of these two dimensions in pediatric populations.
Reward dependence and cooperativeness were lower in the disruptive behavior disorder (DBD)-only and DBD plus an affective and/or anxiety disorder (DBD+Int) groups compared with controls and the attention-deficit hyperactivity disorder (ADHD)-only group. The RD dimension describes a tendency to seek out others’ confidence and support as well as having an ability to respond emotionally to others’ distress. Scores on this dimension were lower among children with externalizing disorders compared with controls and also lower among children with comorbid internalizing disorders. Levels of RD in depressed adults42 or of sociability in depressed adolescents16 have been found to be comparable with controls. As RD levels between the DBD-only and DBD+Int group did not statistically differ, it is likely that this finding represents an association with DBD more than with affective or anxiety disorders.
Other dimensions showed more specific associations within diagnostic categories. Harm avoidance was higher only in subjects in the DBD+Int group compared with all other groups. This dimension, which somewhat parallels other measures of negative affectivity, may be particularly related to internalizing disorders,43 although our lack of an affective/anxiety disorder-only group limits the ability to make a firm conclusion in this regard. The HA dimension also includes several items in questionnaire form that parallel descriptions from other research on behavioral inhibition.7
High novelty seeking emerged as being associated with DBD, although the pattern was more complex. NS has had perhaps the most association with psychiatric diagnoses as shown in previous reports.13,18,19 In this study, subjects with inattentive ADHD were rated as having significantly lower NS compared with the other subtypes in probands. This result is similar to that of other reports that have not found strong associations between attentions problems and activity levels.23,24 Because 76% of the proband ADHD-only group had the inattentive subtype, this may have accounted for the lack of difference in NS between the ADHD-only group and controls. As molecular genetic studies of both ADHD and NS have identified common candidate genes,44,45 future investigations may be advised to account carefully for ADHD subtype.
Logistic regression models confirmed the associations particularly between low P and ADHD, high NS and DBD and between high HA and comorbid DBD and internalizing disorders. As in many studies of children with externalizing disorders, the high degree of comorbidity in this sample limits conclusions that can be drawn between temperamental traits and individual diagnoses other than ADHD. Within each diagnostic group as defined, however, regression models demonstrated that temperamental variables explained a substantial proportion of the variance.
Only one temperament interaction term was also found to make an independent contribution to diagnostic group, after controlling for demographics and the main effects of the JTCI scales themselves. Thus, although particular combinations of temperamental traits are associated with DSM-IV externalizing disorders, the effect of a single dimension appears to be relatively independent of the effects of other dimensions. This result is not inconsistent with the finding that the main domains of temperament are independently heritable.8
In ADHD, however, high NS was related to low HA, whereas in controls, this relation was not present. This significant interaction may have occurred by chance given the number of interaction terms tested and lack of replication in the sibling sample. Nevertheless, as neither NS nor HA was found to be different in the ADHD-only group compared with controls, it is possible that in ADHD, levels of NS and HS are more strongly related to each other compared with the general population. Another possibility is that the temperament combination of high NS and low HA underlies a subset of children with ADHD, particularly those with prominent hyperactive-impulsive symptoms.
Limitations
This study recruited, in particular, families with children who have problems with attention and/or aggression from an area with little ethnic diversity. Consequently, the generalizability of the above findings to other diagnoses or racial groups may be limited.
Another potentially limiting factor is that the DBD+Int group and, to a lesser extent, the DBD-only group may have been simply more impaired groups in general by virtue of their higher number of diagnoses and that any temperamental associations with these groups are related more to overall psychiatry morbidity than any particular diagnostic category. This confound between comorbidity and overall severity is a common complicating factor in naturalistic studies.46 Although it remains a possibility with these data, the fact that different JTCI scales showed different patterns relative to the three diagnostic groups argues against this being the primary force behind these findings for all dimensions. The lower RD and lower C found mainly in the DBD-only and DBD+Int groups relative to the control and ADHD-only groups, however, are consistent with the possibility that some dimensions may be nonspecifically related to overall psychiatric load.
Also problematic is the overlap between temperament items and diagnostic symptoms, which could have elevated the association between these two supposedly different constructs. For example, questions on the NS dimension ask parents if their child “loses his/her temper more easily than other children” or “makes decisions quickly because he/she doesn”t like to wait.” Although these questions are similar to individual criterion of oppositional defiant disorder and ADHD, respectively, the temperament items, which for the JTCI are rated simply as “true” or “false,” do not probe for the required impairment needed for DSM-IV diagnoses. The issue of item overlap is certainly a methodological one, but it also is a theoretical one that raises questions about the difference between extreme temperament and diagnoses if parallel language is used to assess both. Furthermore, associations between temperament and psychopathology have been shown to remain when overlapping items are removed.47 Many DSM-IV disorders may be conceptualized as extreme temperament plus impairment. Although the presence of impairment may represent important and meaningful distinctions between a disorder and its corresponding temperamental profile with regards to cause, course, and treatment, future research is needed to test this specific hypothesis.
The cross-sectional nature of this study also precludes conclusions as to how temperament and psychopathology are related. One hypothesis that has been put forth is that the temperament represents a vulnerability or risk factor for psychiatric disorders but is itself a qualitatively distinct entity.7 Another hypothesis is that extreme temperaments and many psychiatric disorders are better conceptualized as lying on a spectrum.48 Finally, the relations between temperament and psychopathology could be bidirectional with temperament having an impact on specific diagnoses and a specific diagnosis having important effects on temperament.49 These hypotheses are not mutually exclusive, and, furthermore, there is no reason to expect that a uniform relation is characteristic of all temperament or personality dimensions in relation to all psychiatric diagnoses.50
To date, the data suggest that temperament and psycho-pathology, although closely related, are not identical and that qualitative differences do exist between the constructs. This evidence comes, in part, from behavioral genetic studies that have revealed different magnitudes of environmental and genetic effects between individuals with extreme or disorder levels of a trait versus those with more intermediate levels.51,52 These findings are consistent with goodness-of-fit models of development that propose that many factors beyond the simple attributes of the child contribute to the degree to which behaviors become “disordered.” Indeed, recent evidence suggests that the effect of particular genes on temperamental dimensions themselves is partially dependent on particular environments for full expression.53
Clinical Implications
Extreme levels of temperamental traits could serve as an indication for closer monitoring by clinicians. Furthermore, modality to a child’s temperamental profile. For example, a child with an anxiety disorder and high levels of persistence may be better able to take advantage of the coping strategies taught in cognitive behavioral therapy. Conversely, an anxious child with poor persistence may respond better to family- and school-based interventions devoted to reducing directly the amount of environmental stressors or their physiological manifestations. Before these strategies could be employed in regular clinical practice, however, greater consensus is needed as to the optimal methods of temperament assessment and boundaries of the core temperamental dimensions. Finally, these findings suggest that temperamental profiles may provide an alternative method of phenotyping children with behavioral problems and may yield important targets for future research in behavioral genetics and studies of underlying pathophysiology.
Acknowledgments
This research was funded by a Physician Scientist Award from the University of Vermont College of Medicine (D. Rettew) and NIMH grants K08 MH069562 (D. Rettew, PI) and K08 MH01265 (J. Hudziak, PI).
References
- 1.Goldsmith HH, Buss AH, Plomin R, et al. Roundtable: what is temperament? Child Dev. 1987;58:505–529. [PubMed] [Google Scholar]
- 2.Thomas A, Chess S. Temperament and Development. New York: Bruner/Mazel; 1977. [Google Scholar]
- 3.Clark LA, Watson D. Temperament: A New Paradigm for Trait Psychology. New York: Guilford Press; 1999. [Google Scholar]
- 4.Goldsmith HH, Buss AH, Lemery KS. Toddler and childhood temperament: expanded context, stronger genetic evidence, new evidence for the importance of environment. Dev Psychol. 1997;33:891–905. doi: 10.1037//0012-1649.33.6.891. [DOI] [PubMed] [Google Scholar]
- 5.Caspi A. The child is father to the man: personality continuities from childhood to adulthood. J Pers Soc Psychol. 2000;78:158–172. doi: 10.1037//0022-3514.78.1.158. [DOI] [PubMed] [Google Scholar]
- 6.Cohen P. Personality development in childhood: old and new findings. In: Cloninger CR, editor. Personality and Psychopathology. Washington, DC: American Psychiatric Press; 1999. pp. 101–127. [Google Scholar]
- 7.Kagan J. Galen’s Prophecy. Boulder, CO: Westview Press; 1994. [Google Scholar]
- 8.Cloninger CR, Svrakic DM, Przybeck TR. A psychobiological model of temperament and character. Arch Gen Psychiatry. 1993;50:975–990. doi: 10.1001/archpsyc.1993.01820240059008. [DOI] [PubMed] [Google Scholar]
- 9.Svrakic DM, Whitehead C, Przybeck TR, Cloninger CR. Differential diagnosis of personality disorders by the seven-factor model of temperament and character. Arch Gen Psychiatry. 1993;50:991–999. doi: 10.1001/archpsyc.1993.01820240075009. [DOI] [PubMed] [Google Scholar]
- 10.Cloninger CR, Przybeck TR, Svrakic DM. The Tridimensional Personality Questionnaire: U.S. normative data. Psychol Rep. 1991;69:1047–1057. doi: 10.2466/pr0.1991.69.3.1047. [DOI] [PubMed] [Google Scholar]
- 11.Frick PJ. Integrating research on temperament and childhood psychopathology: its pitfalls and promise. J Clin Child Adolesc Psychol. 2004;1:2–7. doi: 10.1207/S15374424JCCP3301_1. [DOI] [PubMed] [Google Scholar]
- 12.Rothbart MK. Commentary: differentiated measures of temperament and multiple pathways to childhood disorders. J Clin Child Adolesc Psychol. 2004;1:82–87. doi: 10.1207/S15374424JCCP3301_8. [DOI] [PubMed] [Google Scholar]
- 13.Schmeck K, Poustka F. Temperament and disruptive behavior disorders. Psychopathology. 2001;34:159–163. doi: 10.1159/000049300. [DOI] [PubMed] [Google Scholar]
- 14.Achenbach TM. Manual for the Child Behavior Checklist/4-18 and 1991 Profile. Burlington, VT: Department of Psychiatry, University of Vermont; 1991. [Google Scholar]
- 15.Bussing R, Gary FA, Mason DM, Leon CE, Sinha K, Garvan CW. Child temperament, ADHD, and caregiver strain: exploring relationships in an epidemiological sample. J Am Acad Child Adolesc Psychiatry. 2003;42:184–192. doi: 10.1097/00004583-200302000-00012. [DOI] [PubMed] [Google Scholar]
- 16.Goodyer IM, Ashby L, Altham PME, Vice C, Cooper PJ. Temperament and major depression in 11 to 16 year olds. J Child Psychol Psychiatry. 1993;34:1409–1423. doi: 10.1111/j.1469-7610.1993.tb02099.x. [DOI] [PubMed] [Google Scholar]
- 17.Buss AH, Plomin R. The EAS Approach to Temperament. Hillsdale, NJ: Erlbaum; 1986. [Google Scholar]
- 18.Cloninger CR, Sigvardsson S, Bohman M. Childhood personality predicts alcohol abuse in young adults. Alcohol Clin Exp Res. 1988;12:494–505. doi: 10.1111/j.1530-0277.1988.tb00232.x. [DOI] [PubMed] [Google Scholar]
- 19.Wills TA, Vaccaro D, McNamara G. Novelty seeking, risk taking, and related constructs as predictors of adolescent substance use: an application of Cloninger’s theory. J Subst Abuse. 1994;6:1–20. doi: 10.1016/s0899-3289(94)90039-6. [DOI] [PubMed] [Google Scholar]
- 20.Tremblay RE, Pihl RO, Vitaro F, Dobkin PL. Predicting early onset of male antisocial behavior from preschool behavior. Arch Gen Psychiatry. 1994;51:732–739. doi: 10.1001/archpsyc.1994.03950090064009. [DOI] [PubMed] [Google Scholar]
- 21.Prior M, Smart D, Sanson A, Oberklaid F. Longitudinal predictors of behavioural adjustment in pre-adolescent children. Aust N Z J Psychiatry. 2001;35:297–307. doi: 10.1046/j.1440-1614.2001.00903.x. [DOI] [PubMed] [Google Scholar]
- 22.Silva PA, Stanton W. From Child to Adult: The Dunedin Study. Oxford, England: Oxford University Press; 1996. [Google Scholar]
- 23.Gjone H, Stevenson J. A longitudinal twin study of temperament and behavior problems: common genetic or environmental influences? J Am Acad Child Adolesc Psychiatry. 1997;36:1448–1456. doi: 10.1097/00004583-199710000-00028. [DOI] [PubMed] [Google Scholar]
- 24.Rende RD. Longitudinal relations between temperament traits and behavioral syndromes in middle childhood. J Am Acad Child Adolesc Psychiatry. 1993;32:297–290. doi: 10.1097/00004583-199303000-00008. [DOI] [PubMed] [Google Scholar]
- 25.Biederman J, Rosenbaum JF, Bolduc-Murphy EA, et al. A 3-year follow-up of children with and without behavioral inhibition. J Am Acad Child Adolesc Psychiatry. 1993;32:814–821. doi: 10.1097/00004583-199307000-00016. [DOI] [PubMed] [Google Scholar]
- 26.Schwartz CE, Snidman N, Kagan J. Adolescent social anxiety as an outcome of inhibited temperament in childhood. J Am Acad Child Adolesc Psychiatry. 1999;38:1008–1015. doi: 10.1097/00004583-199908000-00017. [DOI] [PubMed] [Google Scholar]
- 27.Hirshfeld-Becker DR, Biederman J, Faraone SV, Violette H, Wrightsman J, Rosenbaum JF. Temperamental correlates of disruptive behavior disorders in young children: preliminary findings. Biol Psychiatry. 2002;51:563–574. doi: 10.1016/s0006-3223(01)01299-9. [DOI] [PubMed] [Google Scholar]
- 28.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4. Washington, DC: American Psychiatric Press; 1994. [Google Scholar]
- 29.Nigg JT, Hinshaw SP. Parent personality traits and psychopathology associated with antisocial behaviors in childhood attention-deficit hyperactivity disorder. J Child Psychol Psychiatry. 1998;39:145–159. [PubMed] [Google Scholar]
- 30.Hollingshead AB. Four Factor Index of Social Status. New Haven, CT: Yale University, Department of Sociology; 1975. [Google Scholar]
- 31.Hudziak JJ, Helzer JE, Wetzel MW, et al. The use of the DSM-III-R Checklist for initial diagnostic assessments. Compr Psychiatry. 1993;34:375–383. doi: 10.1016/0010-440x(93)90061-8. [DOI] [PubMed] [Google Scholar]
- 32.Hudziak JJ, Copeland W, Stanger C, Wadsworth M. Screening for DSM-IV externalizing disorders with The Child Behavior Checklist: a receiver-operating characteristic analysis. J Child Psychol Psychiatry. 2004;45:1299–1307. doi: 10.1111/j.1469-7610.2004.00314.x. [DOI] [PubMed] [Google Scholar]
- 33.Luby JL, Svrakic DM, Przybeck TR, Cloninger CR. The Junior Temperament and Character Inventory: preliminary validation of a child self-report measure. Psychol Rep. 1999;84:1127–1246. doi: 10.2466/pr0.1999.84.3c.1127. [DOI] [PubMed] [Google Scholar]
- 34.Cloninger CR, Przybeck TR, Svrakic DM, Wetzel RD. The Temperament and Character Inventory (TCI): A Guide to Its Development and Use. St. Louis: Center for Psychobiology of Personality, Washington University; 1994. [Google Scholar]
- 35.Parker G, Cheah YC, Parker K. Properties of the Temperament and Character Inventory in a Chinese sample. Acta Psychiatr Scand. 2003;108:367–373. doi: 10.1034/j.1600-0447.2003.00192.x. [DOI] [PubMed] [Google Scholar]
- 36.Pelissolo A, Lepine JP. Normative data and factor structure of the Temperament and Character Inventory (TCI) in the French version. Psychiatr Res. 2000;1:67–76. doi: 10.1016/s0165-1781(00)00127-x. [DOI] [PubMed] [Google Scholar]
- 37.Kuo PH, Chih YC, Soong WT, Yang HJ, Chen WJ. Assessing personality features and their relations with behavior problems and adolescents: Tridimensional Personality Questionnaire and Junior Eysenck Personality Questionnaire. Comp Psychiatry. 2004;45:20–28. doi: 10.1016/j.comppsych.2003.09.011. [DOI] [PubMed] [Google Scholar]
- 38.Lyoo IK, Han CH, Lee SJ, et al. The reliability and validity of the Junior Temperament and Character Inventory. Comp Psychiatry. 2004;45:121–128. doi: 10.1016/j.comppsych.2003.12.002. [DOI] [PubMed] [Google Scholar]
- 39.Landry K, Copeland W, Hudziak JJ, Stanger C. Reliability and validity of a childhood temperament and character inventory. Poster presented at the 49th annual conference of the American Academy of Child and Adolescent Psychiatry; October 22–27, 2002; San Francisco, CA. [Google Scholar]
- 40.Wills TA, Dishion TJ. Temperament and adolescent substance use: a transactional analysis of emerging self-control. J Clin Child Adolesc Psychol. 2004;1:69–81. doi: 10.1207/S15374424JCCP3301_7. [DOI] [PubMed] [Google Scholar]
- 41.Nigg JT, Goldsmith HH, Sachek J. Temperament and attention deficit hyperactivity disorder: the development of a multiple pathway model. J Clin Child Adolesc Psychol. 2004;1:42–53. doi: 10.1207/S15374424JCCP3301_5. [DOI] [PubMed] [Google Scholar]
- 42.Mulder RT, Joyce PR, Cloninger CR. Temperament and early environment influence comorbidity and personality disorders in major depression. Comp Psychiatry. 1994;35:225–233. doi: 10.1016/0010-440x(94)90195-3. [DOI] [PubMed] [Google Scholar]
- 43.Compas BE, Conner-Smith J, Jaser SS. Temperament, stress reactivity, and coping: implications for depression in childhood and adolescence. J Clin Child Adolesc Psychol. 2004;1:21–31. doi: 10.1207/S15374424JCCP3301_3. [DOI] [PubMed] [Google Scholar]
- 44.Epstein RP, Novick O, Umansky R, et al. Dopamine D4 receptor (D4DR) exon III polymorphism associated with the human personality trait of Novelty Seeking. Nat Genet. 1996;12:78–80. doi: 10.1038/ng0196-78. [DOI] [PubMed] [Google Scholar]
- 45.Swanson JM, Sunohara GA, Kennedy JL, et al. Association of the dopamine receptor D4 (DRD4) gene with a refined phenotype of attention deficit hyperactivity disorder (ADHD): a family based approach. Mol Psychiatry. 1998;3:38–41. doi: 10.1038/sj.mp.4000354. [DOI] [PubMed] [Google Scholar]
- 46.MacDonald VM, Achenbach TM. Attention problems versus conduct problems as six-year predictors of problem scores in a national sample. J Am Acad Child Adolesc Psychiatry. 1996;35:237–1246. doi: 10.1097/00004583-199609000-00021. [DOI] [PubMed] [Google Scholar]
- 47.Lemery KS, Essex MJ, Smider NA. Revealing the relation between temperament and behavior problem symptoms by eliminating measurement confounding: expert ratings and factor analysis. Child Dev. 2002;73:867–882. doi: 10.1111/1467-8624.00444. [DOI] [PubMed] [Google Scholar]
- 48.Graham P, Stevenson J. Temperament and psychiatric disorders: the genetic contribution to behaviour in childhood. Aust N Z Psychiatry. 1987;21:267–274. doi: 10.1080/00048678709160922. [DOI] [PubMed] [Google Scholar]
- 49.Widiger TA, Verheul R, van den Brink W. Personality and psycho-pathology. In: Pervin LA, John OP, editors. Handbook of Personality: Theory and Research. New York: Guilford Press; 1999. pp. 347–366. [Google Scholar]
- 50.Rutter M. Temperament: conceptual issues and clinical implications. In: Kohnstamm GA, Bates JE, Rothbart MK, editors. Temperament in Childhood. Chicester, UK: Wiley; 1989. pp. 463–479. [Google Scholar]
- 51.Nigg JT, Goldsmith HH. Developmental psychopathology, personality, and temperament: reflections on recent behavioral genetics research. Hum Biol. 1998;70:387–412. [PubMed] [Google Scholar]
- 52.Gjone H, Stevenson J. A longitudinal twin study of temperament and behavior problems: common genetic or environmental influences? J Am Acad Child Adolesc Psychiatry. 1997;36:1448–1456. doi: 10.1097/00004583-199710000-00028. [DOI] [PubMed] [Google Scholar]
- 53.Keltikangas-Jarvinen L, Raikkonen K, Ekelund J, Peltonen L. Nature and nurture in novelty seeking. Mol Psychiatry. 2004;9:308–311. doi: 10.1038/sj.mp.4001433. [DOI] [PubMed] [Google Scholar]