Abstract
A meta-analysis was performed on studies employing the ventricular-brain ratio to compare schizophrenic subjects to that of normal controls. This was a follow-up to a similar meta-analysis published in 1992 in which study-, in addition to clinical-, factors were found to contribute significantly to the reported difference between patients with schizophrenia and controls. Seventy-two (N=72) total studies were identified from the peer reviewed literature, 39 from the original meta-analysis, and 33 additional studies published since which met strict criteria for inclusion and analysis– thus representing ~30 years of schizophrenia ventricular enlargement research. Sample characteristics from schizophrenics and controls were coded for use as predictor variables against within sample VBR values as well as for between sample VBR differences. Additionally, a number of factors concerning how the studies were conducted and reported were also coded. Obtained data was subjected to unweighted univariate as well as multiple regression analyses. In particular, results indicated significant differences between schizophrenics and controls in ventricular size but also the influence of the diagnostic criteria used to define schizophrenia on the magnitude of the reported VBR. This suggests that differing factors of the diagnostic criteria may be sensitive to ventricular enlargement and might be worthy of further examination. Interestingly, we observed an inverse relationship between VBR difference and the number of co-authors on the study. This latter finding suggests that larger research groups report smaller VBR differences and may be more conservative or exacting in their research methodology. The diagnostic criteria used for defining schizophrenia were also predictive of between group differences. Analyses weighted by sample size provided identical conclusions. The effects of study factors such as these are helpful for understanding the variation in the size of the reported differences in VBR between patients and controls as well as for understanding the evolution of research on complex clinical syndromes employing neuroimaging morphometrics.
1. INTRODUCTION
Since the advent of the neuroimaging era, researchers have routinely applied computed tomography (CT) and, later, magnetic resonance imaging (MRI), to explore and quantify anatomical alterations in the brains of patients with schizophrenia relative to normal controls. Johnstone et al. (1976) were the first to note neuroimaging-based changes in the ventricular system of patients that appeared to be related to the disease process. Since that time, with few exceptions, subsequent studies have tended to find evidence of an increase in the size of the lateral cerebral ventricles in patients having schizophrenia. So much so that ventricular enlargement, as measured using morphometric neuroimaging techniques, is arguably the most consistent neuroanatomical biomarker present in the disease.
Following the earliest reports, it was hypothesized in some studies that ventricular size might be related to disease chronicity. This prompted researchers to speculate that schizophrenia existed as a syndrome possessing two key forms (Andreasen and Olsen 1982): Type I – in which acute patients suffered from neurotransmitter imbalances giving rise to ‘positive’ symptoms but that had not yet experienced significant ventricular size alterations; and, Type II – in which chronic subjects experienced greater ‘negative’ symptoms and had appreciable ventricular enlargement. While this concept of schizophrenia was not born out and since lost favor (Abi-Dargham 2004), the findings of ventricular enlargement as a hallmark of the disease have continued even into the most recent studies.
The underlying biological factors that contribute to ventricular enlargement in schizophrenia have remained under investigation despite over 30 years of study though few, if any, necessarily reliable predictive features have emerged. Recent editorials have indicated that break-throughs in understanding relevant clinical variables in schizophrenia (Insel 2009), notably from neuroimaging (Meyer-Lindenberg 2010), may be forthcoming. However, it was noted in a meta-analytic treatment of the literature that there are several study-based factors that predict the magnitude of the reported difference between schizophrenic and normal samples. Van Horn and McManus (1992) examined 39 studies published between 1976 and 1991 which utilized the measure of the ventricular brain ratio (VBR) as its dependent variable. The VBR is a measure of ventricular area or volume divided by total brain area or volume (sometimes taken on the CT or MRI slice in which the lateral ventricles appeared their largest) then multiplied by 100 to produce a percentage. These authors noted that the size of the mean difference between schizophrenics and controls was significant, while additionally this difference was also related to the diagnostic criteria used to define schizophrenia, and, interestingly, correlated negatively with the year of publication of the study. This effect was due to the control VBR being reported systematically higher over time while the schizophrenic VBR remaining constant over the same period.
While other meta-analyses on brain morphometry including ventricular size have been performed since (Wright, Rabe-Hesketh et al. 2000; Arnone, Cavanagh et al. 2009), the Van Horn and McManus article was particularly relevant in that it was the first to demonstrate the effects of study-related variables have on the reporting of ventricular size differences between patients and controls. That such variables themselves modulate the reported size of the difference between patients and controls is indicative that despite efforts to adequately control for extraneous variables within a particular study, what happens between studies, using the same basic neurological measurement can significantly influence an entire literature. This has implications for how enlarged lateral ventricles should be considered clinically and whether it is possible to clearly and consistently identify predictive factors that give rise to ventricular-wall degradation (e.g. changes in the composition of the cerebro-spinal fluid, white matter demyelination, mild-encephalopathies, etc). Meta-analyses that include study variables as well as variables related to the samples under study can be helpful by providing an assessment that might permit better standards for defining illness, measuring the effects in question, and how to more clearly interpret study outcomes and turn them into effective treatments.
Since the meta-analysis of Van Horn and McManus was published nearly 20 years ago, a number of additional empirical reports of ventricular enlargement in schizophrenia have been published in the literature. Despite more modern approaches being available, analyses based on the VBR represent a major segment of the literature on ventricular enlargement over the past three decades. As such, we were curious if the same effects remained present in studies examining ventricular size using neuroimaging methods and whether additional study factors might also play a role in the reported size of the experimental effects related to the differences between patients and controls. In the present article, we provide a detailed follow-up to, and extension of, the original Van Horn and McManus meta-analysis article to examine a range of pertinent study factors that may help to contextualize the meaning of ventricular enlargement and the role of study factors in predicting the size of reported experimental effects.
2. METHODS
In what follows, we describe the approach employed to identify research articles as well as detail our criteria for inclusion and exclusion of articles for consideration in further meta-analysis.
2.1 Literature searches
The majority of VBR studies published since 1991 were located through computerized literature searches using two primary sources: PubMed and Google Scholar. PubMed (http://www.ncbi.nlm.nih.gov/pubmed/) keyword search phrases included variations “schizophrenia VBR,” “schizophrenia ventricle brain ratio,” “schizophrenia ventricular enlargement”, “schizophrenia ventricles”, “schizophrenia ventriculomegaly”, and “psychosis ventricular enlargement”. Additional articles were identified from those cited in the articles obtained through our PubMed searches. Likewise. Google Scholar (http://www.scholar.google.com) also utilized the same keyword search phrases. Once search results were established, the abstracts and PDF (Portable Document Format) files were scrutinized to determine if studies would be taken into consideration. Studies published after December 31, 2010 were not considered.
While studies were found through computerized literature searches, there were often instances when manual literature searches were necessary, as well. These manual searches necessitated tracking citations through numerous journals, the more common studies being discovered in journals such as Archives of General Psychiatry, British Journal of Psychiatry, Biological Psychiatry, Psychiatry Research, and Schizophrenia Research. Manual searching was mainly vital if PDF files were not available when attempting to research computerized literature. This was often true for research articles published during the early 1990’s. These manual literature searches were conducted at the Louise M. Darling Biomedical Library at the University of California, Los Angeles (12-077 Center for the Health Sciences, Los Angeles, CA 90025). Studies from the original meta-analysis of Van Horn and McManus were often not available online and had to be located through manual searches and hard copies obtained via photocopier. Only studies published prior to December 2010 were considered. Through this process, a total of 121 studies were identified from the literature in which the VBR of schizophrenic patients was compared with that of controls.
2.2 Meta-analysis inclusion criteria
There were several factors that contributed to a study being considered for inclusion in further meta-analysis. We wished to identify only those studies which had a minimally acceptable amount of consistent meta-data and neuroimaging measurements so that we might more readily analyze studies collectively as well as compare studies against one another. Studies minimally had to have conducted their examination on both a schizophrenic sample as well as a normative control group. The schizophrenic groups were analyzed as patients with any form of schizophrenic disorder (e.g. first-episode, late-onset, or chronic), and the control groups were required to be normal, otherwise healthy “non-neurological” patients, or listed as “volunteers”. Other psychiatric samples included in the study (e.g. bipolar or depressed subjects) were disregarded and only the reported results from schizophrenics and the control samples were considered. Studies also had to have specifically utilized the VBR as their measure of ventricular size and reported mean and standard deviations for mean VBR in both samples – as was done similarly in Van Horn and McManus. The earliest journal article considered in this updated collection of studies was that of Shiraishi et al (1990) while the latest journal article examined was that of Reite et al. (2010). Journal impact factor was not used as a basis for article inclusion/exclusion from our study but was used as a potential moderator variable (see below). Details of each study included in our collection of studies, along with the original list from Van Horn and McManus are illustrated in Table 1. The complete list of studies along with all VBR measurements and predictor variables is available as supplemental material.
Table 1.
Summary of N=72 Articles included By Journal
| Journal | Number of Articles | Years of Publication |
|---|---|---|
| Acta Psychiatr Scand | 8 | 1985–1997 |
| Am J Psychiatry | 10 | 1982–1994 |
| Arch Gen Psychiatry | 7 | 1979–2002 |
| Arq Neuropsiquiatr | 1 | 2006 |
| Biol Psychiatry | 4 | 1984–1998 |
| BMC Psychiatry | 1 | 2010 |
| Br J Psychiatry | 11 | 1982–1995 |
| Eur Arch Psychiatry Clin Neurosci | 1 | 1998–2003 |
| J Nerv Ment Dis | 1 | 1992 |
| Johns Hopkins Medical Journal | 1 | 1981 |
| Jpn J Psychiatry Neurol | 1 | 1992 |
| Neuropsychopharmacology | 2 | 1992–1997 |
| Prog Neuropsychopharmacol Biol Psychiatry | 1 | 1998 |
| Psychiatry Res | 15 | 1983–2003 |
| Psychiatry Res: Neuroimaging | 3 | 1997–2001 |
| Psychol Med | 2 | 1990–1995 |
| Schizophr Bull | 2 | 1992–1993 |
| Schizophr Res | 1 | 2000 |
| GRAND TOTAL | 72 | 1979–2006 |
2.3 Exclusion criteria for literature studies
For a majority of the excluded articles, the reason was that the authors only studied the VBR of schizophrenics, and there was no mention of a normal comparison control group anywhere in the study. There were also occasions when an author did use a comparison control group; however, this control group was not considered to be normal. For instance, a comparison group in these studies may have only comprised of other schizophrenic patients, neurological patients, etc. Another reason for exclusion was that some authors did compare schizophrenics with normal controls, but they only reported the VBR results of the schizophrenic cohort. There were example studies where authors do not report actual mean VBR values for either the schizophrenic group or the control group but only reported the results of the statistical difference or p-values between groups. Studies of this type were considered to have poor reliability. Other reasons for excluding studies were if the articles studied the VBR of patients with bipolar disorder, unipolar or bipolar depression, etc, and they did not study the VBR of patients with schizophrenia. In one particular case, Ohara et al (2006), the authors studied the VBR of parents of schizophrenics, and not the patients with schizophrenia themselves. Forty-seven such studies were removed from consideration and further meta-analysis. Six additional articles that studied ventricular size in patients and controls were excluded due to their reporting only scaled ventricular size measurements which appeared inconsistent with the typical range of values observed in other articles (e.g. being very close to zero compared to the mean and SDs of the pre-1991 study set). On closer examination, the ventricular size values of these six studies were not reported as traditional VBR ratios but given as the results of a non-conventional mathematical approach, reported as only statistical p-values or, for instance, reported only residualized VBRs after statistical correction for subject age, duration of illness, gender, etc. The details and reasons for study exclusion are illustrated in Table 2.
Table 2.
Details of Excluded VBR Studies
| Lead Author | Year of Publication | Journal Name | Reason for Exclusion |
|---|---|---|---|
| Aso | 1995 | Eur Arch Psychiatry Clin Neurosci | no normal control group used |
| Barak | 2002 | J Nerv Ment Dis | used a comparison control group that also comprised of schizophrenic patients (not normal) |
| Benson | 1996 | Psychiatry Res | only reported VBR results of patients with schizophrenia and not of the control group |
| Bersani | 1995 | Human Psychopharmacology - Clinical and Experimental- | no normal control group used |
| Bornstein | 1992 | Biol Psychiatry | Reported method of determining VBRs inconsistent with that of other studies |
| Caputo | 1998 | Eur Arch Psychiatry Clin Neurosci | Reported only p-values |
| Chang | 2005 | Biol Psychiatry | VBR of patients with bipolar disorder, and not patients of schizophrenia |
| Curtis | 1999 | Biol Psychiatry | only reported VBR results of patients with schizophrenia and not of the control group |
| Davis | 1998 | Biol Psychiatry | only reported VBR results of patients with schizophrenia and not of the control group |
| Dequardo | 1997 | Prog Neuropsychopharmacol Biol Psychiatry | studied the VBR of patients with unipolar or bipolar depression, and not patients of schizophrenia |
| Dequardo | 1996 | Schizophr Res | no normal control group used |
| Dequardo | 1994 | Biol Psychiatry | no normal control group used |
| Emsley | 1995 | Br J Psychiatry | used a comparison control group that also comprised of schizophrenic patients (not normal) |
| Farmer | 1997 | Health Soc Work | no normal control group used |
| Ford | 1992 | Psychiatry Res | no normal control group used |
| Friedman | 1991 | Biol Psychiatry | no normal control group used |
| Gaser | 2004 | Am J Psychiatry | no normal control group used |
| Goldberg | 1991 | Am J Psychiatry | no normal control group used |
| Goldman | 1996 | Schizophr Res | no normal control group used |
| Hata | 2003 | Acta Psychiatr Scand | no normal control group used |
| Hoffman | 1991 | Biol Psychiatry | no normal control group used |
| Juckel | 1994 | Eur Arch Psychiatry Clin Neurosci | no normal control group used |
| Keshavan | 1991 | Psychiatry Res | no normal control group used |
| King | 1991 | Br J Psychiatry | no normal control group used |
| Kirch | 1992 | J Neural Transmission | reported VBR results of patients with schizophrenia and not of the control group |
| Lauer | 1998 | Biol Psychiatry | no normal control group used |
| Leadbetter | 1999 | Am J Psychiatry | no normal control group used |
| Lesser | 1993 | Schizophr Res | reported VBR results of patients with schizophrenia and not of the control group |
| Levitt | 1994 | Schizophr Res | do not display actual VBR values for either schizophrenic patients or the normal comparison control group in the study |
| Mauri | 1994 | Int Clin Psychopharmacol | no normal control group used |
| McCreadie | 2002 | Arch Gen Psychiatry | Reported method of determining VBRs inconsistent with that of other studies |
| Ohara | 2006 | Prog Neuropsychopharmacol Biol Psychiatry | studied the VBR of parents of schizophrenics, and not the schizophrenic patients themselves |
| Ohrmann | 2005 | Schizophr Res | Reported method of determining VBRs inconsistent with that of other studies |
| Pandurangi | 1994 | Schizophr Res | no normal control group used |
| Puri | 1999 | Int J Psychophysiology | no normal control group used |
| Puri | 2005 | Int J Clin Pract | Reported method of determining VBRs inconsistent with that of other studies |
| Sandyk | 1991 | Int J Neurosci | no normal control group used |
| Sandyk | 1992 | Int J Neurosci | no normal control group used |
| Sandyk | 1993 | Int J Neurosci | no normal control group used |
| Schroder | 1995 | Psychopathology | reported VBR results of patients with schizophrenia and not of the control group |
| Schroder | 1992 | Psychiatry Res | no normal control group used |
| Shiori | 2000 | Eur Arch Psychiatry Clin Neurosci | no normal control group used |
| Shiraishi | 1990 | Jpn J Psychiatry Neurol | used a comparison control group that comprised of neurological patients (not normal) |
| Tabarés- Seisdedos | 2001 | Psychiatry Res: Neuroimaging | no normal control group used |
| Tandon | 2000 | Schizophr Res | no normal control group used |
| Tandon | 1991 | Biol Psychiatry | no normal control group used |
| Tsai | 1998 | Biol Psychiatry | only presented VBR results of patients with schizophrenia and not of the control group |
| van Kammen | 1998 | Psychiatry Res: Neuroimaging | no normal control group used |
| van Kammen | 1994 | Am J Psychiatry | only presented VBR results of patients with schizophrenia and not of the control group |
| Vita | 1991 | Am J Psychiatry | only reported VBR results of patients with schizophrenia and not of the control group |
| Walker | 1996 | Schizophr Res | no normal control group used |
| Young | 1991 | Br J Psychiatry | Reported method of determining VBRs inconsistent with that of other studies |
| Zorrilla | 1997 | Biol Psychiatry | do not report actual VBR values for either schizophrenic patients or the normal comparison control group in the study |
Note: Exclusion of these articles from this meta-analysis is not a comment on the rigor or validity of the individual studies, per se. Rather, we chose to focus on those that reported VBRs in patient as well as normal control samples as well as that satisfied the inclusion criteria described in the text. Journal impact factor was not a criterion for study inclusion or exclusion.
2.4 Variables extracted from research studies
Thirty-four (34) remaining studies met the above criteria for inclusion, were retained for further analysis, and included with the N=38 studies using the Van Horn and McManus 1992 meta-analysis. From these N=72 studies, numerous independent variables were extracted and data was collected from each study. These studies were classified in terms of a variety of independent characteristics. It should be noted that there are a few measures that refer to the study as a whole (e.g. method of brain area measurement), and therefore refer to both the schizophrenic as well as control subject cohorts. Other measures refer specifically to one group of subjects or the other (e.g. diagnostic criterion of the schizophrenics, or the nature of the controls), but can still be used as a predictor variable for the other type of subject (e.g. diagnostic criterion of the schizophrenics can be used as a predictor of VBR in control subjects of that study). Where multiple schizophrenic sub-types were examined in a particular study, the demographic, VBR measurements, were pooled across the samples to form a single weighted average measurement for the schizophrenic cohort as a whole. The extracted variables are classified into four types: variables pertaining to study information, those specific to the study’s schizophrenic cohort demographics, those specific to controls, and the relevant VBR information. This is to aid in the organization of the variables and should make data interpretation straightforward. These variables are as follows:
2.4.1 Study Information Variables
Total number of authors
The total number of authors included in a published article is frequently recommended by meta-analysis practitioners as a predictor variable relating to peer-related constraints on the calculation, interpretation, and publication of results (Glass, McGaw et al. 1981; Hedges 1985).
Year of publication
As previously shown by Van Horn and McManus (1992), the year of study publication can offer a window into secular trends in the dependent variable of interest and/or systematic changes in experimental control.
Country in which study was performed
This was recorded to see if cultural differences may exist between what is considered to define schizophrenia outside of formal diagnostic criteria.
Journal impact factor
Specifically, we used Harzing’s “Publish or Perish” software program (www.harzing.com) to compute journal-specific h-indices (reference here) accumulated for all articles published in that journal up to and including the year of publication. As the h-index tends to rise linearly with the age of the journal, we adjusted the calculation of the h statistic to subtract out the numbers of articles cited with respect to the very first VBR study (Johnson et al., 1976). This has the effect of equalizing the time-spans being considered so that “older” journals (e.g. Archives of General Psychiatry) and “younger” journals (e.g. the Japanese Journal of Psychiatric Neurology) are treated more equally with the exception of perceived relative impact at the time of article publication. Journal impact factor, its h-index, or other form of journal ranking was not used to include or exclude studies in the analysis.
Meta-analytic cohort
We were curious if studies included in our original 1991 study differed in their mean VBRs and differences compared to those published afterward. We created a variable coding for “old” versus “new” articles, the dividing point of publication being the appearance in the literature of our initial meta-analysis in 1991 (20 years ago) to determine if there had been a general change in reported VBR sizes between these two epochs.
Funding source
The source of funding can often influence the size or direction of between group differences (Alasbali, Smith et al. 2009; Noordin, Wright et al. 2010). This was coded as being government funding, having received private support, both, or not given.
2.4.2 Schizophrenia Group Variables
Subject type
Diagnostic classification would be expected to present considerable variation between psychiatric groups relative to controls. As described in the articles, these were categorized as first-episode, acute, chronic, late-life onset, or a mixed diagnosis sample schizophrenic patients. It was unclear if the diagnosis of “acute” also included “first-episode” patients as well, however, which, in particular, may confound differences between these two groups in some studies.
Diagnostic criteria
Whether the study defined schizophrenia using DSM-III, DSM-III-R, DSM-IV, RDC, multiple criteria used, or none given.
Mean age
The mean age (±SD) of the schizophrenic sample.
Sample size
The number of subjects included in the computed VBR statistics. This was also, where possible, broken down by gender by which the proportion of males in the sample was used as a variable of interest.
Duration of illness
This measure was not often reported. We include illness duration (±SD) where available explicitly as well as where it could be computed based on knowledge of mean age and mean onset of illness.
Age of onset
Likewise with illness duration, the onset of illness (±SD) was frequently not reported by study authors. We include it where available explicitly as well as where it could be computed based on knowledge of mean age and mean illness duration.
Years of education
The number of years of education for the patient samples was also not frequently reported. Due to insufficient instances of this value, we merely provide values for the few instances in which it was presented here for the reader’s information. We otherwise did not include it in our statistical analyses.
Handedness
Where available, the percent of the sample that were right handed, as measured or indicated by the study authors, was used as a predictor variable.
2.4.3 Control Group Variables
Subject type
Normal control subjects were classified into two types based on the descriptions provided by the authors. These were groups who were recruited specifically to be a part of the study as “volunteers” (paid or otherwise) or subjects who were patients themselves, e.g. undergoing neuroimaging to rule out neurological issues, etc, but were deemed neurologically normal and made available for use as control subjects in the study.
Mean age
The mean age (±SD) of the normal control sample.
Sample size
The number of subjects included in the computed VBR statistics for the control sample. This was also, where possible, broken down by gender by which the proportion of males in the sample was used as a variable of interest.
Years of education
As in the case of the schizophrenic samples, the number of years of education for the patient samples was also not frequently reported. Due to insufficient instances of this value, we merely report it here for the reader’s information.
Handedness
Like in the case of the schizophrenic samples, where this information was available, the percent of the sample that were right handed, as indicated by the study authors, was used as a predictor variable.
2.4.4 Ventricular Measurement Variables
Imaging modality
The method used to obtain neuroimaging data was coded as being either computed tomography (CT) or magnetic resonance imaging (MRI).
Method of brain area measurement
The method to measuring ventricular and brain size was coded as being either 2D planimetry (e.g. 2D volumes of the lateral ventricles on slices in which they appeared the largest) or volumetric (e.g. in which the full 3D volume of the ventricles was determined either manually or via computer algorithm).
Mean VBR of schizophrenics
The reported (or pooled as appropriate) mean VBR (±SD) of the schizophrenic patient sample.
Mean VBR of controls
The reported (or pooled as appropriate) mean VBR (±SD) of the normal control sample.
2.5 Statistical Testing
In many forms of meta-analyses it is conventional to employ measures of effect size, which are typically dimensionless numbers of summarizing a difference between group means in terms of such measure of the variability of the groups (such as the standard deviation) (e.g. Pearson’s r or the d-statistic, calculated as (Mean1-Mean2)/(combined standard decision) – see Rosenthal (1984) for a discussion of these and other related measures). Such an approach is sensible if studies are heterogeneous in their absolute units of measurement. However, in the present case all of the studies we having identified from the literature use VBR as the dependent variable and, therefore, it is sensible to carry out a meta-analysis in terms of that specific variable; the logic here is precisely akin to that arising in structural modeling in this typically (dimensionless) correlation matrices are used, but in which, if units of measurement are homogeneous, it makes more sense to use covariance matrices.
Although we here present only analyses of absolute VBR measures, it should also be pointed out that re-analysis of our data using d as an effect size statistic results in identical conclusions. Effect size values are also helpful for evaluating the presence of publication bias in meta-analyses, which we discuss below. We present the effect size measure d and its complementary effect size metric r for each study in Table 1 as a convenience for the reader.
A particular challenge with any meta-analysis is that studies vary in sample size (and hence differ in their potential accuracy or relative reliability), and that independent (or moderator or predictor) variables are not altogether uncorrelated. Several authors on meta-analysis recommend weighting analyses by study sample size (Rosenthal 1984; Hedges 1985; Egger, Smith et al. 2001), although, vigorous differences of opinion have emerged over the universal appropriateness of sample size weighting (Shuster 2010) which suggest that weighting itself can negatively bias results. Van Horn and McManus (1991), in using univariate and multivariate analysis of studies followed Glass et al (1981) in not attempting to take any account of the differing sample sizes in studies (and hence different sampling errors and variance heterogeneity). They note that such problems tend to pale into inconsequential in comparison with the problems posed by low power in the collection of studies.
In our follow-up meta-analysis, we performed both unweighted and sample size weighted analyses of schizophrenic patient and control subject VBRs. The relative statistical effects obtained using unweighted VBR values were not qualitatively different than when we employed weighted values and, hence, did not alter their interpretation. Thus, we report here un-weighted univariate and multiple regression analyses to assess the independent effects of correlated predictors, and do not report regression results obtained by weighting the various studies according to their sample sizes. In doing so, we are aware of the issue that in examining meta-analytic data for effects of moderator variables the crucial characteristic is the number of studies and not the number of subjects, which paradoxically can sometimes mean that their statistical power is surprisingly low, despite apparently large subject numbers. However, we do consider the role of sample size in the context of identifying potential evidence for publication bias in VBR studies (see below).
3. RESULTS
The un-weighted mean VBR for schizophrenic samples (collapsed across sub-diagnoses) obtained across all studies was 6.35±2.35 while that of normal control samples was 4.77±2.23. The difference between mean study VBRs was highly significant (t=9.67, df=71, p<0.0001) and confirms the finding from many of the individual investigations that schizophrenia syndrome involves the enlargement of the lateral cerebral ventricles.
3.1 Univariate T-tests
To examine factors that might influence the reported size in VBR differences, we assessed between group effects based on whether the study was statistically significant or not (p-value ≤0.05 n=48, or p-value >0.05 n=24) and also based on what time period the study took place in (pre-1991 n=39, or post-1991 n=32). We suspected that the VBR measures would be different and that the number of authors may have been influential as well. An independent samples t-test analysis revealed that the number of authors (p=0.0031) as well as the VBR of controls (p=0.0035), but not the VBR of the schizophrenic group, were significantly different between the significant and non-significant groups, with the number of authors greater and the VBR of controls larger in the non-significant group. We also found that the number of authors was significantly different (p=0.0031) between the early group (papers written before 1991) and the later group (papers written after 1991), with a greater number of authors in the later group.
We observed that the main factors in determining whether a study was significant or not were (1) the control VBR and (2) the number of authors on the study. (1) Since it was only the control VBR that differed between groups, and not the VBR of the schizophrenics, the reported significance differences might be due to how rigorously control subjects were screened and age/gender matched to their patient counterpart. The VBR of the schizophrenics are roughly the same (not statistically different) whether the study was significant or not, so if there is a true difference between controls and schizophrenics, it depends highly on the definition of “control”, and may be only a slight difference at best. (2) The number of authors was another statistically significant difference between significant and non-significant results. Papers that did NOT find a significant difference between controls and schizophrenics had a higher mean number of authors. This, along with other findings below, may suggest that having more authors on a study lends a higher quality control to subject screening, recruitment, etc., since more experienced eyes have examined the protocol. More authors may tend to lead to a higher overall n as well (if the number of authors was ≤5, n=28 studies the average n in the study was 64.1 subjects; if the number of authors was >5 (max 15), n=43 studies the average n in the study was 96.7; significant, p=0.043), which may lead to more reliable statistical results due to higher power.
No significant differences were observed between patient and control groups in studies that employed CT (n=60) vs. MRI (n=12) (p<0.16 in patients, and p<0.26 in controls). Additionally, no significant differences were observed between studies that employed hand-planimetry (n=36) and computer-based (n=35) approaches (p<0.89 in patients, and p<0.91 in controls).
3.2 Multiple Regression
First we dummy coded variables such as region/continent in which the study took place, the diagnostic criteria, and type of controls and schizophrenics. Then we ran a backwards elimination variable selection (using the SAS default criterion of p<0.1 significance) to find which factors significantly contributed to the dependent variable (either VBR of Schizophrenics, VBR of controls, or VBR of Schizophrenics controlling for VBR of controls). Then, using the outcome we performed a multiple linear regression on the selected variables.
3.2.1 Multiple Regression of Schizophrenic VBR scores
Following backward elimination, four variables were significant in the regression analysis, F(4,65) = 50.64 p<0.0001 (R2 = 0.81, adjusted for shrinkage). Significant factors were: the number of co-authors on the study (p=0.0017) – studies with more authors having lower mean VBRs; the dummy variable indicating a diagnosis of acute schizophrenia (p=0.009) – studies with patients with a diagnosis of acute schizophrenia having lower VBRs; whether the study was part of the original Van Horn and McManus meta-analysis versus the newly added collection of studies (p=0.05) – earlier studies having higher VBRs than more recent studies; the standard deviation of the VBR of acute schizophrenic subjects (p<0.0001) – studies with higher standard deviations of the VBR of schizophrenics having higher VBRs; and the VBR of the control subjects (p<0.0001) – studies with a higher VBR of controls having higher VBR of the schizophrenic subjects, after controlling for the other covariates.
3.2.2 Multiple Regression of Control VBR Scores
Backwards elimination identified eight variables of interest F(9,62) = 26.60, p<0.0001 (R2 = 0.76, adjusted for shrinkage) and three were significant in the regression analysis,. Significant factors were: the number of co-authors on the study (p=0.0014) – studies with more authors having higher VBRs; the standard deviation of the VBR in schizophrenic subjects (p=0.0025; note here we are analyzing the VBR of control subjects) – studies with higher standard deviations of the VBR of schizophrenics having lower VBRs in control subjects; and the VBR of the schizophrenic patients (p<0.0001) studies with higher VBRs of schizophrenics having higher VBRs in controls, after controlling for the other covariates.
While more authors led to a smaller measurement in the VBR of schizophrenics, it lead to a higher VBR of controls, decreasing the overall difference between the two groups (and thus why more authors led to non-significant findings). We also found that a higher SD of the VBR in schizophrenics led to a lower VBR in the control subjects. So as the measurements for schizophrenic VBR varied more widely, the VBR of controls decreased, possibly due to both samples being more heterogeneous and variable – e.g. neither the schizophrenic population nor the control population were well defined. Again, the VBR of the controls and the VBR of the schizophrenics are highly correlated so it is not surprising that this was significant.
3.2.3 Multiple Regression of Schizophrenic Subjects Using Control Subjects as Covariate
The control VBR was entered in the first step of the regression and was highly significant, F(1,70)=146.91 (p<0.0001). 67.7% of the variance of the VBR of schizophrenics is explained by the VBR of controls. The addition of the predictor variables, followed by backwards elimination, showed that three predictor variables were significant predictors of the residualized schizophrenic VBRs, resulting in an overall significance level of F(5, 66) = 10.48 , p<0.0001 (R2 = 0.4425). The significant variables were: the number of authors on the study (p=0.0008) – studies with a larger number of authors having lower VBRs; the dummy variable indicating a diagnosis of acute schizophrenia (p=0.0106); and the standard deviation of the VBR of schizophrenics (p<0.0001) – studies with higher standard deviations having higher VBRs, after controlling for the other covariates. While the date of study publication was not statistically significant (p=0.0628), it bordered on significance with later studies having slightly higher VBRs.
3.2.4 Multiple Regression of the Standard Deviation of the VBR of Schizophrenics
Backwards elimination revealed eleven variables, of which five were significant in the regression, F(12,59) = 6.24, p<0.0001 (R2 = 0.47). The significant variables were: the period the study took place (p=0.014) – later studies having lower standard deviations of the VBR of schizophrenics; the dummy variable indicating a diagnosis of acute schizophrenia (p=0.029) – studies with an acute schizophrenia diagnosis having higher standard deviations of the VBR SDs of other schizophrenics; the standard deviation of the VBR of controls (p=0.0005) – studies with higher standard deviations of the VBR of controls having higher standard deviation of the VBR of schizophrenic subjects; the VBR of the schizophrenic patients (p=0.0116) – studies with higher VBRs of schizophrenics having higher standard deviations of the VBR; and the VBR of the control samples (p=0.006) – studies with a higher VBR of the controls having lower standard deviations of the VBR of schizophrenics.
3.2.5 Multiple Regression of the Standard Deviation of the VBR of Controls
Backwards elimination selected nine variables, all of which were significant in the regression analysis, F(9,54) = 19.07 p<0.0001 (R2 = 0.76). The significant variables were: the dummy variables indicating the study took place in Europe (p=0.0202) – studies in this region having lower standard deviations of the VBR of controls; the mean age of the schizophrenic patients (p=0.0173) – studies with a higher mean age in the schizophrenic group had lower standard deviations of the VBR of controls; the SD of the age of schizophrenic subjects (p=0.0108) – studies with higher standard deviations of the age of schizophrenics having higher standard deviations of the VBR of controls; the dummy variables indicating a diagnosis of any form of schizophrenia except late-life onset schizophrenia (acute schizophrenia p<0.0001, chronic schizophrenia p<0.0001, first episode schizophrenia p<0.0001, mixed diagnosis p=0.0001) – studies with patients with these diagnoses having lower standard deviations of the VBR of controls; the standard deviation of the VBR of schizophrenics (p=0.0001) – studies with higher standard deviations of the VBR in schizophrenics having higher standard deviations of the VBR of controls; and the VBR of the schizophrenics (p<0.0001) – studies with high VBRs of schizophrenics having higher standard deviations of the VBR of controls, after controlling for the other covariates.
3.2.6 Multiple Regression of the Standard Deviation of the VBR of Schizophrenics using SD of the Control Subjects as a Covariate
The control SD of the VBR was entered in the first step of the regression and was highly significant, p<0.0001. The addition of the predictor variables for the residual variation, followed by backwards elimination, showed that five predictor variables were significant, resulting in an overall significance level of F(5,66) = 6.16, p=0.0001 (R2 = 0.32). The significant variables were: the period when the study took place (p=0.0086) – later studies having lower standard deviations of the VBR; the dummy variable for studies using multiple diagnostic criteria (p=0.0375) – studies using multiple criteria having higher standard deviations of the VBR; the dummy variable indicating the study took place in Europe (p=0.0132); studies taking place in Europe having higher standard deviations of the VBR; the VBR of schizophrenics (p=0.0049) – studies with higher mean VBRs of the schizophrenics having higher standard deviations of the VBR; and VBR of controls (p=0.0109) – studies with higher VBRs of controls having lower standard deviations of the VBR, after controlling for the other covariates.
4. DISCUSSION
In this meta-analysis of 72 studies of ventricular enlargement in schizophrenia and normal control subjects obtained from the peer-reviewed literature between the years 1979 and 2010, we found that schizophrenics present VBR measurements larger than that of their normal control samples in all but only a few instances. Here we summarize the main findings:
4.1 Ventricular Enlargement in General
Significant ventricular enlargement in schizophrenics relative to controls was reported in 66% of articles included in our meta-analysis. The mean VBR of schizophrenics taken across studies was also significantly greater than the mean of the control samples. Indeed, there appears to be an undeniable enlargement of the lateral cerebral ventricles in schizophrenia which is likely a hallmark of the disease process. The size of the reported effects, however, appear to be heavily dependent on study-based, as opposed to sample-based, factors.
4.2 Diagnostic Criteria Effects
That studies differ in the reported VBRs on the basis of diagnostic criteria suggests that subtle factors between means of assessing schizophrenia have important influences on how large the VBRs of those patients will be. For instance, in Table 3 there is a steady reduction in the size of the schizophrenic VBR with each successive revision of the Diagnostic and Statistical Manual (DSM). Moreover, combining criteria, such as the DSM and the Research Diagnostic Criteria (RDC; Endicott and Spitzer 1978; Spitzer, Endicott et al. 1978), intended to serve as a more strict screening for defining schizophrenia than using each criterion separately, results in a lower VBR in patients than either of these criteria when applied alone. This suggests that subtleties in the underlying diagnostic factors that have been subject to refinement over the years (e.g. Axis I) may, in fact, be sensitive to ventricular size. This appears particularly true in the case between DSM revisions, though more examples would be needed to determine the reliability of this finding. If true, this implies that patients diagnosed with schizophrenia under one edition of the DSM and also having larger ventricles might not have been given a schizophrenia diagnosis under a newer DSM revision. When no diagnostic criterion is reported, the mean VBR difference between schizophrenic and control samples appears largest though this is only representative of a few studies.
Table 3.
Unweighted descriptive statistics for the independent variables and for VBR in schizophrenics and controls by diagnostic group
| Schizophrenics | Controls | |||||
|---|---|---|---|---|---|---|
| Mean | SD | n | Mean | SD | n | |
| Age | 31.79 | 9.57 | 72 | 32.11 | 8.92 | 72 |
| Age at Onset of Illness | 25.25 | 12.2 | 43 | - | - | - |
| Duration of Illness | 8.04 | 4.09 | 43 | - | - | - |
| Percentage of males in sample | 0.69 | 0.21 | 60 | 0.64 | 0.23 | 55 |
| Year of Study | 1990.46 | 6.37 | 72 | - | - | - |
| Mean VBR by diagnostic group | ||||||
| DSM–III | 6.83 | 1.96 | 27 | 4.94 | 2.0 | 27 |
| DSM-III-R | 6.66 | 2.5 | 19 | 5.06 | 2.26 | 19 |
| DSM–IV | 3.14 | 3.48 | 4 | 2.32 | 2.51 | 4 |
| RDC | 6.45 | 2.14 | 8 | 5.65 | 2.77 | 8 |
| Multiple Criteria Used | 6.32 | 1.75 | 11 | 4.92 | 1.73 | 11 |
| None Given | 4.25 | 3.76 | 3 | 1.87 | 1.74 | 3 |
Additionally, if the patient population was diagnosed as having acute schizophrenia (as opposed to first episode schizophrenia, chronic schizophrenia, late-onset-schizophrenia, or a mixed diagnosis in the patient group) then the VBR was lower than other diagnoses. The reason for this is unclear, but the diagnosis of acute schizophrenia had the most subjects, n=27, so it was the highest powered group in our meta-analysis. As in our original regression, the SD. of the VBR of schizophrenics was once again significant, with the SD increasing with the mean VBR of the schizophrenic group.
Nevertheless, these results suggest that differences in diagnostic factors are important contributors to reported VBR-related effects. It might be of interest to examine the historical changes to these diagnostic criteria over time to identify those changes which might have been most selective to factors related to ventricular size. Since a better (endo-)phenotypic characterization of schizophrenia has been a central point of diagnostic criterion research over the years (Regier, Narrow et al. 2009) (Esterberg and Compton 2009; Linscott and van Os 2010), such results may not be surprising or unwanted. It might also indicate that ventricular enlargement in schizophrenia is an epiphenomenon of other non-disease-related factors (e.g. medication, drug use, viral infection, etc).
4.3 Illness Duration and Age of Onset
Given discussion in the literature on the extent of progressive structural abnormalities in schizophrenia and their association with clinical outcome and duration of disease (Ho, Andreasen et al. 2003; van Haren, Cahn et al. 2008), we regret not having sufficient data concerning age of onset and illness duration to adequately incorporate these potentially important predictor variables into our regression analyses. This potential limitation is emphasized by the results of our meta-analysis itself in which we noted that “acute patients” had the lowest VBR values among the coded patient sub-types. However, for the n=43 studies (~60% of studies) that did report duration of illness for their patient sample, raw mean VBR did not correlate with the length of illness (R2 = 0.012, p = ns), nor did the effect size (Cohen’s d) between the patients and control sample (R2 = 0.02, p = ns). Factors not reliably present in this collection of VBR studies that might further shed light on progressive structural abnormalities would include medication effects and the potential for gene-by-environment interactions which would likely necessitate large-scale multi-site twin studies to examine in detail.
4.3 Year of Publication
Van Horn and McManus (1992) noted in their meta-analysis that the size of the difference between schizophrenics and control VBR was negatively correlated with the year of study publication. This was not due to changes in the mean schizophrenic VBR getting smaller over time but in the control sample mean VBR getting larger. These authors surmised that the earliest studies may have used criteria for the inclusion of control subjects that could have inflated the size of the between-group differences. Many early studies asked a neurologist to examine the CT and MRI scans of the control subjects to assess them as indeed being “normal subjects”. If the ventricles appeared “too large” then the subjects were suspected of having a neurological issue that meant they were not normal and they were excluded from further study. However, the distribution of the VBR in the normal population is substantially skewed with a positive tail. Thus, even normal subjects can have relatively large ventricles and the practice of artificially culling the upper tail of the natural VBR distribution – thereby lowering the mean VBR and reducing the variance of the VBR distribution - was one likely factor in the larger reported between group effects in these earlier studies. Additionally, a similar culling of the schizophrenic sample was not performed with no schizophrenic ventricles being deemed too small with subsequent effects on their distributional properties (e.g. increased mean and reduced variance) or too large. As the natural variability in the distribution of the control VBR was recognized and other experimental controls were introduced for the inclusion of subjects, the differences between groups was reduced over time. Van Horn and McManus had predicted that this effect would eventually stabilize and that the year of publication effect would eventually disappear after several years when the weight of additional, better controlled, studies made their effects on a meta-analysis felt. This appears to have happened as there was no significant year of study effect present when all N=72 studies were examined. Nevertheless, other meta-analyses on clinical samples using neuroimaging data may wish to examine year of study publication as one potential predictor of effect size, especially during the earliest studies being examined.
4.4 Effects Due to the Control Subjects
The effects of the control sample seemed to be an important factor on whether or not a study reported their findings to be significantly different or not. Often, it was only the control VBR that predicted the between group effects and not the VBR of the schizophrenics. Therefore, the reported significance differences might be due to how rigorously control subjects were screened and age/gender matched to their patient counterpart. Additionally, in scrutinizing the standard deviation of the VBR in schizophrenic subjects we noted that studies with higher schizophrenic VBR SDs had generally lower control subject VBRs.
However, we also classified the control samples into those who were volunteers recruited to take part in the study (n=42) versus those who were themselves patients being scanned to rule out neurological issues associated with headache or other symptoms (n=30). Comparing mean VBRs between controls in those studies with volunteers (mean VBR±SD = 4.48±2.42) against those with patients (mean VBR±SD = 5.19±1.99) showed no appreciable difference (p = 0.194). On the other hand, studies that used patient control subjects had significantly higher VBR standard deviations (mean VBR_SD±SD = 2.47±0.78) than did volunteer controls (mean VBR_SD±SD = 1.88±1.09; t(70) = 2.57, p=0.0124). This implies that patient controls are, in and of themselves, inherently more variable in their ventricular size as compared to volunteer subjects despite these two groups not differing in their overall mean VBRs. Thus, use of otherwise “normal” patient control groups may not be the ideal control sample since, for instance, chronic migraine might be associated with subtle but variable brain morphology changes.
Also, studies conducted in Europe tended to have lower standard deviations of the VBR in controls suggesting either (1) that normal Europeans are less variable in ventricular size, or more likely, (2) that European studies have different inclusion criteria concerning normal subjects. Taken together, these results strongly suggest that the true population difference between control and schizophrenic VBR distributions is likely to depend highly on the clinical definition for what constitutes a control subject.
4.5 Number of Study Authors
A surprising and interesting observation concerns the number of study co-authors. There tended to be a higher number of study authors in our more recent survey of the VBR literature than were present in the original Van Horn and McManus analysis. Overall, there was a significant correlation between the number of authors and the year of article publication in our collection of VBR studies (r = 0.33, p= 0.0047). This agrees with the general trend in the biomedical sciences for the number of multi-author studies to have steadily increased over time (see http://www.nlm.nih.gov/bsd/authors1.html). This may be due to an increase in the number of multi-center collaborations made possible through the increasing availability of the internet beginning in the early 1990’s. The number of co-authors was not, however, related to number of total subjects (R2=0.002, p = ns) meaning that larger studies did not possess a greater number of authors. Being able to share data, resources, and expertise using the internet has given rise to increased interest in broad multi-institutional partnerships notably in the case of neuroimaging (Van Horn and Toga 2009). As a result, research articles published by multi-center programs frequently involve more researchers than any single participating institution might ordinarily. Despite apparent stochastic properties that may govern such trends (Hsu and Huang 2009), the fact that greater ease of collaboration has played a role in carrying out studies of neuropathologies in schizophrenia is not necessarily astonishing.
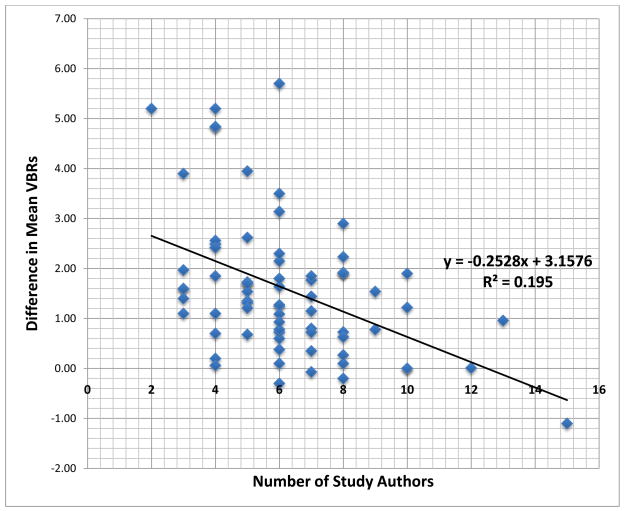
What is of particular interest is the observation that as the number of study authors increases the between group difference in mean VBRs is reduced. Examination of Figure 2 indicates this relationship and it is noteworthy as it is not driven by one or two outliers but a legitimate effect present in this collection of rigorously identified studies. This is clearly a unique observation and one whose origin is difficult to surmise with accuracy. For instance, due to lack of detail in the studies, we were not able to reliably ascertain the academic degrees or overall qualifications for all authors which might explain smaller effect sizes in some studies versus others. One potential interpretation of this finding, however, is that increases in the number of study authors helps to strengthen the overall experimental, analytical, and interpretive rigor which a study might have. Studies having fewer authors may be modestly easier to publish simply because there are fewer co-author opinions to balance out and incorporate into the submitted manuscript. Yet such studies may be more subject to biases associated with pressures to publish and the push to rapidly disseminate findings (Song, Parekh et al. 2010). Conversely, a greater number of study contributors may help to mitigate the enthusiasm for certain statistical effects which others might rush to publish results too soon. Coupled with an increase in multi-center collaborations, this may imply that the trend for large-scale research partnerships in recent years has been beneficial to the literature by producing relatively more rigorous and representative results concerning findings of ventricular enlargement.
Figure 2.
The number of co-authors effect on the difference between schizophrenic and control sample mean VBRs. The correlation between the number of study authors and the VBR difference was r = 0.442, p<0.001).
4.6 Journal Impact Factor
We had anticipated that there might have been some relationship between the relative impact factor of the journal in which the article appeared and reported VBR differences. This was based on the reasoning that if a particularly large effect existed between patients and controls, then authors might believe their results to be of particular novelty and, hence, worthy of publication in a high impact factor journal. Indeed, journal impact has been shown to be a helpful predictor variable for meta-analytic treatments of psychiatric research themselves (Ipser and Stein 2009). We utilized Hirsch’s h-index since it is easily computable given available citation data unlike traditional impact factors which are formally computed relatively infrequently or require a paid subscription to obtain (e.g. http://isiwebofknowledge.com/). However, we failed to note a significant relationship between the VBRs of patients, controls, or their difference related to journal h-index. This suggests that authors were just as likely to publish large-effects in relatively low-impact journals as they were in higher-impact publications. The choice of journal in which to publish any particular study findings is clearly a multifaceted choice, involving the authors – views on the audience best suited to interpret and utilize the study findings, the perceived importance of the hypotheses under examination, and the relative novelty of the obtained results. Given these decisions that researchers of complex disease processes like schizophrenia must make concerning their published articles it is, therefore, not surprising that the magnitude of reported VBR effects are not overly dependent upon the impact of the journal in which they appear, per se.
4.7 The Potential for Publication Bias
What can be especially difficult to assess in meta-analyses are the concerns that results are taken from across a set of published articles which only report statistically significant outcomes. Such publication biases arise from this tendency for researchers, editors, and pharmaceutical companies, due to pressures to continually produce publishable work (Fanelli 2010), to encourage the reporting of experimental results that are positive (i.e. they show a significant effect) differently from results that are negative (i.e. supporting the null hypothesis) or inconclusive. That is, the significant results tend to get published, especially when they concur with the hypotheses of the authors or with the conventional expectations in the field. This gives rise to the so-called “file drawer problem”, where studies that fail to meet statistical significance are not published and are tucked away into file drawers, instead. What this means, is that what a literature may contain are only the 5% of research studies which obtained a p<0.05 result by chance alone – the remaining 95% of non-significant studies are unknown or unavailable for meta-analytic consideration. On the other hand, publication bias occurs when authors publish statistically significant results despite having relatively low sample sizes.
It is possible to estimate the minimum number of non-significant unpublished studies above which the overall effect detected by our meta-analysis would be overturned (Rosenthal 1979). This estimated number, called the “fail-safe file drawer” (FSFD) estimate, is thus required to be very large: that is, when it is unlikely that there are so many unpublished studies left in researcher’s file drawers. In practice, the real number of unpublished studies can only be guessed at from one's knowledge of the field in question (for instance, from the number of research teams and duration of the research). However, the fail-safe sample size has been strongly criticized (Scargle 2000). More sophisticated tests have been designed specifically to test for the presence of publication bias related to statistical significance (Begg and Mazumdar 1994). Such tests rely on the fact that publication bias would generate a correlation between the observed magnitude of the effect and sample size because studies with small samples (low power) will be published only if the observed effect is extreme (causing the test to be significant). To our knowledge, such tests have only been sparingly applied to biological studies though have been widely applied to meta-analyses of studies examining cancer causing agents (Vandenbroucke 1988; Morris 1994). Thus, while quantitative analyses of publication bias are becoming more available (Sugita, Kanamori et al. 1992; Ioannidis and Trikalinos 2007; Schwarzer, Antes et al. 2007; Copas and Malley 2008) some of these methods may still be in their infancy.
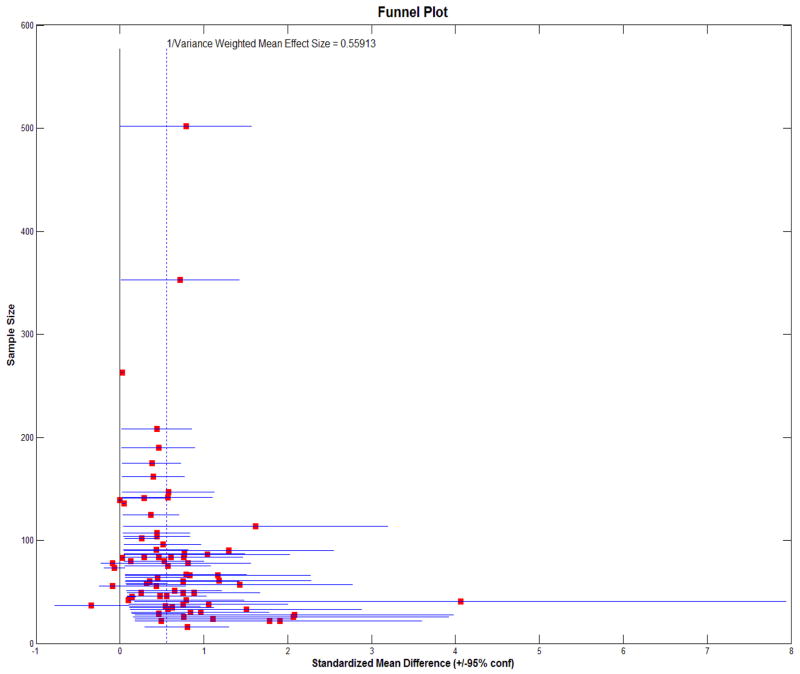
To assess the possibility of publication bias, we employed several different techniques for examining such effects in our meta-analysis including funnel plot regression, the Begg rank correlation approach (using both the variance of the effect size and the sample size as bias predictors), the Egger Regression, the Funnel Plot regression, and the Trim and Fill method (Rendina-Gobioff and Kromrey 2006) (Table 6). Figure 3 illustrates a plot of VBR study effect sizes (+/− 95% confidence intervals) versus study sample size showing considerable variance between published studies. Gaining insight into the factors that give rise to such variance was a principle motivation for further meta-analysis. The collection of study effect sizes were considered homogeneous via the Q-statistic (Figure 3, caption) while no amount of random effects variance was apparent in these effect sizes. Incidentally, the median power for all studies was 0.743 while the mean power was 0.654 – reflective of only modest potential study reproducibility. Unsurprisingly, the mean power for non-significant results was much smaller (0.25, n=24) than that of significant results (0.86, n=47; p-value <0.0001). This indicates that many studies indicating large statistical effects are published with relatively small sample sizes - a hallmark of publication bias. Such small studies may be limited in their accuracy and statistical power. We, nevertheless, remain confident in the findings from our meta-analytic regression results as reflective of study and sample factors giving rise to such effects.
Table 6.
Meta Analysis: Tests of Publication Bias
| p-value | Publication bias present? | |
|---|---|---|
| Egger Regression | 0.0738 | No |
| Begg Rank Correlation (V)* | 0.0036 | Yes |
| Begg Rank Correlation (N)* | 0.0020 | Yes |
| Funnel Plot Regression | <0.0001 | Yes |
| Trim and Fill | ||
| Right Tail (144) | Yes | |
| Left Tail (10) | Yes | |
| Both | Yes |
(V) uses the variance of the effect size as a predictor while (N) uses the total sample size (e.g. the number of patients plus controls) as the predictor
Figure 3.
A funnel plot of VBR study effect size (+/− 95% confidence intervals) against study sample size. The vertical dashed line represents the weighted mean effect size across studies. Assessment of study VBR effect size variability was obtained using the Q-statistic (Higgins and Thompson 2002); Q = 231.46, df = 71, p< 0.0001.
Since we focused our analysis on variables such as the diagnostic criterion, patient diagnosis, gender, number of authors, and the time period of the study as predictors of the outcome measure, we are somewhat less concerned with the “file-drawer” effect and the potential for it to bias results. For instance, it is unclear how the effects of the number of authors on VBR might be a result of publication bias when there exist other studies that, in fact, have never been published and, hence, have no authors. However, there is additional evidence that publication bias exists since the literature as a whole shows results which are dependent on the control VBR, which, in principle, should not be expected to vary more than the VBR of the patient population. So while there seems to be an undeniable difference between the VBR of schizophrenics and controls, this overall effect may not be as large as the mean effect size suggests due to some publication bias. Yet, our sample included many studies that were non-significant (24/72 = 33.3% of studies examined had a p-value>0.05) and so it was not the case that all included studies reported only significant findings. Finally, we note that great pains were taken to specifically select VBR studies that met very particular criteria for inclusion in this meta-analysis, were likely of higher experimental quality, and thus suitably appropriate for such meta-analytic consideration.
4.8 Potential Limitations of this Meta-Analysis
The interpretation of results was restricted partly due to the often poor amount of information that could be extracted from this collection of published articles related to levels/types of medication, durations of illness, handedness, ages of onset, years of education, handedness, etc. in the patient and, where appropriate, the control samples. These variables have been shown to be relevant to ventricular size differences in a variety of psychiatric patient sub-types. Their availability here would have been of particular interest and value for assessing their role on average ventricular size in schizophrenia relative to control subjects. We also could not be more precise concerning the presence of “first episode” patients in studies that listed their sample as being comprised of “acute” patients. As newer studies are undertaken using the VBR or other brain morphometric variables in healthy or patient samples, we encourage authors to report these and related variables whenever possible to facilitate future quantitative review and meta-analysis.
4.9 The Future of Ventricular Enlargement Studies in Schizophrenia
Despite its ongoing use in the study of traumatic brain injury (Ghosh, Wilde et al. 2009), hydrocephalus (Chatzidakis, Barlas et al. 2008), dementia (Carmichael, Kuller et al. 2007), and a variety of diseases, the assessment of ventricular size using the ventricle-to-brain ratio is not likely to be as prominent in future investigations of neuropathology in schizophrenia as it has been historically. Morphological measurement using relatively-simple metrics such as the VBR is likely to be considered outmoded given the emergence of 3D surface and shape modeling approaches (Narr, Thompson et al. 2001; Narr, Thompson et al. 2001; Narr, Sharma et al. 2003; Anticevic, Dierker et al. 2008). For instance, in a study of plasma Na(+) level/osmolality in first-episode schizophrenics, Gunduz-Bruce and colleagues (2007) fit 3D surface mesh models to the ventricular system and noted no general differences between the patient and healthy control groups in ventricular size. However, a mixed model procedure indicated a significant group effect and a significant osmolality-by-group interaction in measures made on the ventricular surfaces. The healthy control group showed a significant relationship between osmolality and ventricle measures while this relationship was absent in the patients. These results suggested that plasma Na(+) concentration may be related to ventricle size in healthy volunteers and may be impaired in patients with first episode schizophrenia. While some studies have sought to sub-divide the lateral ventricles into sub-sections (e.g. Shiraishi, Koizumi et al. 1990), modeling of the entire surface of the ventricular system is better suited to identifying more regionally-specific effects based on surface deformations in patients relative to control subjects (Narr, Bilder et al. 2006). Yet, the scaling of ventricular measurements with respect to overall brain size is an important innovation present in the use of the VBR which has inherent validity for adjusting for scalar effects of brain size and making such metrics comparable across subjects.
Nevertheless, the lessons learned from a retrospective, quantitative meta-analysis of published VBR results obtained from its application are important to consider even after more sophisticated methods have been introduced to the field. As researchers further consider the etiological factors that underlie schizophrenia, it will be essential to make sure that proper experimental controls are utilized, that consistent definitions for patient as well as control samples are employed, and that control samples are constructed so as not to drive the magnitude of reported effects. Larger research collaborative have many advantages for such investigations, not the least of which may be a more conservative approach to quantifying between group differences. While finally, that morphometric neuroimaging findings of overall or regionally-localized ventricular enlargement (or other structural abnormality) in schizophrenia are best not over-interpreted without a robust convergence of other corroborating evidence.
5. CONCLUSIONS
In this 20 year follow-up meta-analysis, building on that of Van Horn and McManus (1992), comprising 72 studies of ventricular size in schizophrenia versus normal control subjects – representing over 30 years of schizophrenia ventricular size research – schizophrenic samples, with few exceptions, showed increased ventricular size relative to controls. The majority of studies meeting strict criteria for inclusion reported these differences to be statistically significant. However, certain study factors were influential in the size of these reported VBR differences. These included the diagnostic criteria used for determining schizophrenia as well as the number of co-authors contributing to the research article. In several instances the differences were noted to be due to the ventricular size of the control samples. While there appears to be an undeniable enlargement of the lateral cerebral ventricles in schizophrenia which is likely a hallmark of the disease process, the size of the reported effects may be heavily dependent on these study-based, as opposed to sample-based, factors. Publication bias was unlikely to have contributed to such effects since they were specifically based on factors associated with the published articles themselves. Ventricular enlargement remains one of the most prominent and oft reported neurological biomarkers for the disease. We encourage the careful consideration of the various factors described in this article in future studies of ventricular size as a major biological index for severe mental illness in schizophrenia and other syndromes.
Supplementary Material
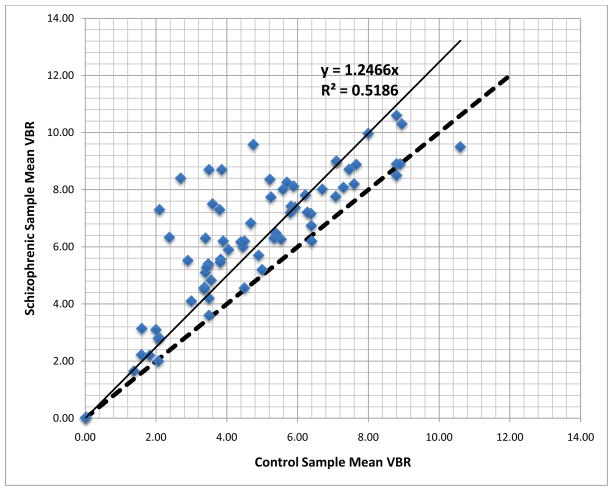
Figure 1.
This figure shows a graph similar to Fig. 1 in the original Van Horn and McManus (1992) article in which the schizophrenic mean VBR in each study is plotted against the VBR of controls for the same study. The regression line is presented, in this instance with the y-intercept set to equal exactly zero (r = 0.72, p<0.0001). The thick dashed line represents the line of equality upon which points would fall if the schizophrenic and control VBRs were equal in any given study. The majority of points are situated above the line of equality indicating the general tendency to identify greater ventricular size in schizophrenic patients.
Table 4.
Number of Authors in Studies Reporting Significant vs. Non-Significant VBR Differences (unweighted)
| Number of Authors | Schizophrenic VBR | Control VBR | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | n | Mean | SD | n | Mean | SD | n | |
| Significant (p≤0.05) | 5.66 | 2.25 | 48 | 6.31 | 2.23 | 48 | 4.23 | 1.84 | 48 |
| Non- significant (p>0.05) | 7.42 | 2.36 | 24 | 6.45 | 2.69 | 24 | 5.85 | 2.65 | 24 |
Table 5.
Number of Authors by Publication Time Period
| Number of Authors | |||
|---|---|---|---|
| Mean | SD | n | |
| Pre-1991 | 5.51 | 2.22 | 39 |
| Post-1991 | 7.12 | 2.38 | 33 |
RESEARCH HIGHLIGHTS.
A meta-analysis of studies using the VBR comparing schizophrenic subjects to normals
This was a 20-year follow-up to a similar meta-analysis published in 1992
N=72 total studies were identified from the peer reviewed literature from 1979 to 2010
Characteristics from schizophrenics and controls were coded for use as predictor variables
Study factors on how studies were conducted and reported were also coded
Results showed significant between group differences in ventricular size
But also the effects of diagnostic criteria on the magnitude of the reported VBR
An inverse relationship between VBR difference and the number of study authors
Acknowledgments
The authors wish to acknowledge Dr. Arthur W. Toga and the staff of the Laboratory of Neuro Imaging (LONI) in the Department of Neurology at the David Geffen School of Medicine at the University of California Los Angeles. We are particularly indebted to Dr. Katherine Narr and to two anonymous reviewers for carefully critiquing an earlier version our manuscript. JVH had full access to all of the study data analyzed as part of this article and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Abi-Dargham A. Do we still believe in the dopamine hypothesis? New data bring new evidence. Int J Neuropsychopharmacol. 2004;7(Suppl 1):S1–5. doi: 10.1017/S1461145704004110. [DOI] [PubMed] [Google Scholar]
- Alasbali T, Smith M, Geffen N, Trope GE, Flanagan JG, Jin Y, Buys YM. Discrepancy between results and abstract conclusions in industry- vs nonindustry-funded studies comparing topical prostaglandins. Am J Ophthalmol. 2009;147(1):33–38. e32. doi: 10.1016/j.ajo.2008.07.005. [DOI] [PubMed] [Google Scholar]
- Andreasen NC, Olsen S. Negative v positive schizophrenia. Definition and validation. Arch Gen Psychiatry. 1982;39(7):789–794. doi: 10.1001/archpsyc.1982.04290070025006. [DOI] [PubMed] [Google Scholar]
- Anticevic A, Dierker DL, Gillespie SK, Repovs G, Csernansky JG, Van Essen DC, Barch DM. Comparing surface-based and volume-based analyses of functional neuroimaging data in patients with schizophrenia. Neuroimage. 2008;41(3):835–848. doi: 10.1016/j.neuroimage.2008.02.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arnone D, Cavanagh J, Gerber D, Lawrie SM, Ebmeier KP, McIntosh AM. Magnetic resonance imaging studies in bipolar disorder and schizophrenia: meta-analysis. Br J Psychiatry. 2009;195(3):194–201. doi: 10.1192/bjp.bp.108.059717. [DOI] [PubMed] [Google Scholar]
- Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50(4):1088–1101. [PubMed] [Google Scholar]
- Carmichael OT, Kuller LH, Lopez OL, Thompson PM, Dutton RA, Lu A, Lee SE, Lee JY, Aizenstein HJ, Meltzer CC, Liu Y, Toga AW, Becker JT. Cerebral ventricular changes associated with transitions between normal cognitive function, mild cognitive impairment, and dementia. Alzheimer Dis Assoc Disord. 2007;21(1):14–24. doi: 10.1097/WAD.0b013e318032d2b1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chatzidakis EM, Barlas G, Condilis N, Bouramas D, Anagnostopoulos D, Volikas Z, Simopoulos K. Brain CT scan indexes in the normal pressure hydrocephalus: predictive value in the outcome of patients and correlation to the clinical symptoms. Ann Ital Chir. 2008;79(5):353–362. [PubMed] [Google Scholar]
- Copas JB, Malley PF. A robust P-value for treatment effect in meta-analysis with publication bias. Stat Med. 2008;27(21):4267–4278. doi: 10.1002/sim.3284. [DOI] [PubMed] [Google Scholar]
- Egger M, Smith GD, Altman DG. Systematic Reviews in Health Care: Meta-Analysis in Context. London: British Medical Journal Books; 2001. [Google Scholar]
- Endicott J, Spitzer RL. A diagnostic interview: the schedule for affective disorders and schizophrenia. Archives of General Psychiatry. 1978;35(7):837–844. doi: 10.1001/archpsyc.1978.01770310043002. [DOI] [PubMed] [Google Scholar]
- Esterberg ML, Compton MT. The psychosis continuum and categorical versus dimensional diagnostic approaches. Curr Psychiatry Rep. 2009;11(3):179–184. doi: 10.1007/s11920-009-0028-7. [DOI] [PubMed] [Google Scholar]
- Fanelli D. Do Pressures to Publish Increase Scientists' Bias? An Empirical Support from US States Data. PLoS ONE. 2010;5(4):e10271. doi: 10.1371/journal.pone.0010271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghosh A, Wilde EA, Hunter JV, Bigler ED, Chu Z, Li X, Vasquez AC, Menefee D, Yallampalli R, Levin HS. The relation between Glasgow Coma Scale score and later cerebral atrophy in paediatric traumatic brain injury. Brain Inj. 2009;23(3):228–233. doi: 10.1080/02699050802672789. [DOI] [PubMed] [Google Scholar]
- Glass GV, McGaw B, Smith ML. Meta-analysis in social research. Beverly Hills: Sage Publications; 1981. [Google Scholar]
- Gunduz-Bruce H, Narr KL, Gueorguieva R, Toga AW, Szeszko PR, Ashtari M, Robinson DG, Sevy S, Kane JM, Bilder RM. CSF sub-compartments in relation to plasma osmolality in healthy controls and in patients with first episode schizophrenia. Psychiatry Res. 2007;155(1):57–66. doi: 10.1016/j.pscychresns.2006.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hedges LV, Olkin I. Statistical Methods for Meta-Analysis. London: Academic Press; 1985. [Google Scholar]
- Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- Ho BC, Andreasen NC, Nopoulos P, Arndt S, Magnotta V, Flaum M. Progressive structural brain abnormalities and their relationship to clinical outcome: a longitudinal magnetic resonance imaging study early in schizophrenia. Arch Gen Psychiatry. 2003;60(6):585–594. doi: 10.1001/archpsyc.60.6.585. [DOI] [PubMed] [Google Scholar]
- Hsu J-w, Huang D-w. Distribution for the number of coauthors. Physical Review E. 2009;80(5):057101. doi: 10.1103/PhysRevE.80.057101. [DOI] [PubMed] [Google Scholar]
- Insel TR. Disruptive insights in psychiatry: transforming a clinical discipline. The Journal of Clinical Investigation. 2009;119(4):700–705. doi: 10.1172/JCI38832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ioannidis JP, Trikalinos TA. An exploratory test for an excess of significant findings. Clin Trials. 2007;4(3):245–253. doi: 10.1177/1740774507079441. [DOI] [PubMed] [Google Scholar]
- Ipser JC, Stein DJ. A systematic review of the quality and impact of anxiety disorder meta-analyses. Curr Psychiatry Rep. 2009;11(4):302–309. doi: 10.1007/s11920-009-0044-7. [DOI] [PubMed] [Google Scholar]
- Johnstone EC, Crow TJ, Frith CD. Cerebral ventricle size and cognitive impairment in chronic schizophrenia. Lancet. 1976;2:924–926. doi: 10.1016/s0140-6736(76)90890-4. [DOI] [PubMed] [Google Scholar]
- Linscott RJ, van Os J. Systematic reviews of categorical versus continuum models in psychosis: evidence for discontinuous subpopulations underlying a psychometric continuum. Implications for DSM-V, DSM-VI, and DSM-VII. Annu Rev Clin Psychol. 2010;6:391–419. doi: 10.1146/annurev.clinpsy.032408.153506. [DOI] [PubMed] [Google Scholar]
- Meyer-Lindenberg A. From maps to mechanisms through neuroimaging of schizophrenia. Nature. 2010;468(7321):194–202. doi: 10.1038/nature09569. [DOI] [PubMed] [Google Scholar]
- Morris RD. Meta-analysis in cancer epidemiology. Environ Health Perspect. 1994;102(Suppl 8):61–66. doi: 10.1289/ehp.94102s861. '1566544:' 1566544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Narr KL, Bilder RM, Woods RP, Thompson PM, Szeszko P, Robinson D, Ballmaier M, Messenger B, Wang Y, Toga AW. Regional specificity of cerebrospinal fluid abnormalities in first episode schizophrenia. Psychiatry Res. 2006;146(1):21–33. doi: 10.1016/j.pscychresns.2005.10.005. [DOI] [PubMed] [Google Scholar]
- Narr KL, Sharma T, Woods RP, Thompson PM, Sowell ER, Rex D, Kim S, Asuncion D, Jang S, Mazziotta J, Toga AW. Increases in regional subarachnoid CSF without apparent cortical gray matter deficits in schizophrenia: modulating effects of sex and age. Am J Psychiatry. 2003;160(12):2169–2180. doi: 10.1176/appi.ajp.160.12.2169. [DOI] [PubMed] [Google Scholar]
- Narr KL, Thompson PM, Sharma T, Moussai J, Blanton R, Anvar B, Edris A, Krupp R, Rayman J, Khaledy M, Toga AW. Three-dimensional mapping of temporo-limbic regions and the lateral ventricles in schizophrenia: gender effects. Biol Psychiatry. 2001;50(2):84–97. doi: 10.1016/s0006-3223(00)01120-3. [DOI] [PubMed] [Google Scholar]
- Narr KL, Thompson PM, Sharma T, Moussai J, Zoumalan C, Rayman J, Toga AW. Three-dimensional mapping of gyral shape and cortical surface asymmetries in schizophrenia: Gender effects. American Journal of Psychiatry. 2001;V158(N2):244–255. doi: 10.1176/appi.ajp.158.2.244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noordin S, Wright JG, Howard A. Relationship between declared funding support and level of evidence. J Bone Joint Surg Am. 2010;92(7):1647–1651. doi: 10.2106/JBJS.I.00224. [DOI] [PubMed] [Google Scholar]
- Regier DA, Narrow WE, Kuhl EA, Kupfer DJ. The conceptual development of DSM-V. Am J Psychiatry. 2009;166(6):645–650. doi: 10.1176/appi.ajp.2009.09020279. [DOI] [PubMed] [Google Scholar]
- Reite M, Reite E, Collins D, Teale P, Rojas DC, Sandberg E. Brain size and brain/intracranial volume ratio in major mental illness. BMC Psychiatry. 2010;10:79. doi: 10.1186/1471-244X-10-79. '2958994:' 2958994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rendina-Gobioff G, Kromrey JD. PUB_BIAS: A SAS Macro for Detecting Publication Bias in Meta-Analysis. 14th Annual SouthEast SAS Users Group (SESUG) Conference; Atlanta, GA: SouthEast SAS Users Group (SESUG); 2006. [Google Scholar]
- Rosenthal R. Meta-Analytic Procedures for Social Research. Sage; Beverly Hills: 1984. [Google Scholar]
- Scargle JD. Publication Bias: The “File Drawer” Problem in Scientific Inference. Journal of Scientific Exploration. 2000;14(1):91–106. [Google Scholar]
- Schwarzer G, Antes G, Schumacher M. A test for publication bias in meta-analysis with sparse binary data. Stat Med. 2007;26(4):721–733. doi: 10.1002/sim.2588. [DOI] [PubMed] [Google Scholar]
- Shiraishi H, Koizumi J, Ofuku K, Suzuki T, Saito K, Hori T, Ikuta T, Kase K, Hori M. Enlargement of the anterior horn of the lateral ventricle in schizophrenic patients: chronological and morphometrical studies. Jpn J Psychiatry Neurol. 1990;44(4):693–702. doi: 10.1111/j.1440-1819.1990.tb01646.x. [DOI] [PubMed] [Google Scholar]
- Shuster JJ. Empirical vs natural weighting in random effects meta-analysis. Statistics in Medicine. 2010;29(12):1259–1265. doi: 10.1002/sim.3607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song F, Parekh S, Hooper L, Loke YK, Ryder J, Sutton AJ, Hing C, Kwok CS, Pang C, Harvey I. Dissemination and publication of research findings: an updated review of related biases. Health Technol Assess. 2010;14(8):iii, ix–xi, 1–193. doi: 10.3310/hta14080. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Endicott J, Robins E. Research diagnostic criteria: rationale and reliability. Arch Gen Psychiatry. 1978;35(6):773–782. doi: 10.1001/archpsyc.1978.01770300115013. [DOI] [PubMed] [Google Scholar]
- Sugita M, Kanamori M, Izuno T, Miyakawa M. Estimating a summarized odds ratio whilst eliminating publication bias in meta-analysis. Jpn J Clin Oncol. 1992;22(5):354–358. [PubMed] [Google Scholar]
- van Haren NE, Cahn W, Hulshoff Pol HE, Kahn RS. Schizophrenia as a progressive brain disease. Eur Psychiatry. 2008;23(4):245–254. doi: 10.1016/j.eurpsy.2007.10.013. [DOI] [PubMed] [Google Scholar]
- Van Horn JD, McManus IC. Ventricular enlargement in schizophrenia. A meta-analysis of studies of the ventricle:brain ratio (VBR) Br J Psychiatry. 1992;160:687–697. doi: 10.1192/bjp.160.5.687. [DOI] [PubMed] [Google Scholar]
- Van Horn JD, Toga AW. Multisite neuroimaging trials. Curr Opin Neurol. 2009 doi: 10.1097/WCO.0b013e32832d92de. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vandenbroucke JP. Passive smoking and lung cancer: a publication bias? Br Med J (Clin Res Ed) 1988;296(6619):391–392. doi: 10.1136/bmj.296.6619.391. '2544973:' 2544973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright IC, Rabe-Hesketh S, Woodruff PW, David AS, Murray RM, Bullmore ET. Meta-analysis of regional brain volumes in schizophrenia. Am J Psychiatry. 2000;157(1):16–25. doi: 10.1176/ajp.157.1.16. [DOI] [PubMed] [Google Scholar]
CITATIONS FOR ARTICLES INCLUDED IN THE META-ANALYSIS
- Andreasen N, Smith M, Jacoby C, Dennert J, Olsen S. Ventricular enlargement in schizophrenia: definition and prevalence. Am J Psychiatry. 1982;139(3):292–296. doi: 10.1176/ajp.139.3.292. [DOI] [PubMed] [Google Scholar]
- Barta PE, Powers RE, Aylward EH, Chase GA, Harris GJ, Rabins PV, Tune LE, Pearlson GD. Quantitative MRI volume changes in late onset schizophrenia and Alzheimer's disease compared to normal controls. Psychiatry Res. 1997;68(2–3):65–75. doi: 10.1016/s0925-4927(96)02751-5. [DOI] [PubMed] [Google Scholar]
- Benes F, Sunderland P, Jones BD, LeMay M, Cohen BM, Lipinski JF. Normal ventricles in young schizophrenics. Br J Psychiatry. 1982;141:90–93. doi: 10.1192/bjp.141.1.90. [DOI] [PubMed] [Google Scholar]
- Bishop RJ, Golden CJ, MacInnes WD, Chu CC, Ruedrich SL, Wilson J. The BPRS in assessing symptom correlates of cerebral ventricular enlargement in acute and chronic schizophrenia. Psychiatry Res. 1983;9(3):225–231. doi: 10.1016/0165-1781(83)90047-1. [DOI] [PubMed] [Google Scholar]
- Boronow J, Pickar D, Ninan PT, Roy A, Hommer D, Linnoila M, Paul SM. Atrophy limited to the third ventricle in chronic schizophrenic patients. Report of a controlled series. Arch Gen Psychiatry. 1985;42(3):266–271. doi: 10.1001/archpsyc.1985.01790260060007. [DOI] [PubMed] [Google Scholar]
- Buckman TD, Kling AS, Eiduson S, Sutphin MS, Steinberg A. Glutathione peroxidase and CT scan abnormalities in schizophrenia. Biol Psychiatry. 1987;22(11):1349–1356. doi: 10.1016/0006-3223(87)90069-2. [DOI] [PubMed] [Google Scholar]
- d'Amato T, Rochet T, Dalery J, Chauchat JH, Martin JP, Marie-Cardine M. Seasonality of birth and ventricular enlargement in chronic schizophrenia. Psychiatry Res. 1994;55(2):65–73. doi: 10.1016/0925-4927(94)90001-9. [DOI] [PubMed] [Google Scholar]
- DeLisi LE, Goldin LR, Hamovit JR, Maxwell ME, Kurtz D, Gershon ES. A family study of the association of increased ventricular size with schizophrenia. Arch Gen Psychiatry. 1986;43(2):148–153. doi: 10.1001/archpsyc.1986.01800020058007. [DOI] [PubMed] [Google Scholar]
- Dewan MJ, Pandurangi AK, Lee SH, Ramachandran T, Levy B, Boucher M, Yozawitz A, Major L. A comprehensive study of chronic schizophrenic patients. I. Quantitative computed tomography: cerebral density, ventricle and sulcal measures. Acta Psychiatr Scand. 1986;73(2):152–160. doi: 10.1111/j.1600-0447.1986.tb10581.x. [DOI] [PubMed] [Google Scholar]
- Elkis H, Friedman L, Buckley PF, Lee HS, Lys C, Kaufman B, Meltzer HY. Increased prefrontal sulcal prominence in relatively young patients with unipolar major depression. Psychiatry Res. 1996;67(2):123–134. doi: 10.1016/0925-4927(96)02744-8. [DOI] [PubMed] [Google Scholar]
- Falkai P, Schneider-Axmann T, Honer WG, Vogeley K, Schonell H, Pfeiffer U, Scherk H, Block W, Traber F, Schild HH, Maier W, Tepest R. Influence of genetic loading, obstetric complications and premorbid adjustment on brain morphology in schizophrenia: a MRI study. Eur Arch Psychiatry Clin Neurosci. 2003;253(2):92–99. doi: 10.1007/s00406-003-0414-9. [DOI] [PubMed] [Google Scholar]
- Ferrari MC, Kimura L, Nita LM, Elkis H. Structural brain abnormalities in early-onset schizophrenia. Arq Neuropsiquiatr. 2006;64(3B):741–746. doi: 10.1590/s0004-282x2006000500008. [DOI] [PubMed] [Google Scholar]
- Gur RE, Mozley PD, Shtasel DL, Cannon TD, Gallacher F, Turetsky B, Grossman R, Gur RC. Clinical subtypes of schizophrenia: differences in brain and CSF volume. Am J Psychiatry. 1994;151(3):343–350. doi: 10.1176/ajp.151.3.343. [DOI] [PubMed] [Google Scholar]
- Harvey I, Williams M, Toone BK, Lewis SW, Turner SW, McGuffin P. The ventricular-brain ratio (VBR) in functional psychoses: the relationship of lateral ventricular and total intracranial area. Psychol Med. 1990;20(1):55–62. doi: 10.1017/s0033291700013222. [DOI] [PubMed] [Google Scholar]
- Hayashi T, Watanabe T, Kitoh H, Sekine T. Multivariate analyses of CT findings in typical schizophrenia and atypical psychosis. Jpn J Psychiatry Neurol. 1992;46(3):699–709. doi: 10.1111/j.1440-1819.1992.tb00545.x. [DOI] [PubMed] [Google Scholar]
- Hoffler J, Braunig P, Kruger S, Ludvik M. Morphology according to cranial computed tomography of first-episode cycloid psychosis and its long-term-course: differences compared to schizophrenia. Acta Psychiatr Scand. 1997;96(3):184–187. doi: 10.1111/j.1600-0447.1997.tb10149.x. [DOI] [PubMed] [Google Scholar]
- Holsenbeck LS, 3rd, Davidson LM, Hostetter RE, Casanova MF, Taylor DO, Kelley CT, Perrotta C, Jr, Borison RL, Diamond B. Ventricle-to-brain ratio and symptoms at the onset of first-break schizophrenia. Schizophr Bull. 1992;18(3):427–435. doi: 10.1093/schbul/18.3.427. [DOI] [PubMed] [Google Scholar]
- Iacono WG, Smith GN, Moreau M, Beiser M, Fleming JA, Lin TY, Flak B. Ventricular and sulcal size at the onset of psychosis. Am J Psychiatry. 1988;145(7):820–824. doi: 10.1176/ajp.145.7.820. [DOI] [PubMed] [Google Scholar]
- Jernigan TL, Zatz LM, Moses JA, Jr, Berger PA. Computed tomography in schizophrenics and normal volunteers. I. Fluid volume. Arch Gen Psychiatry. 1982;39(7):765–770. doi: 10.1001/archpsyc.1982.04290070001001. [DOI] [PubMed] [Google Scholar]
- Kaiya H, Uematsu M, Ofuji M, Nishida A, Morikiyo M, Adachi S. Computerised tomography in schizophrenia. Familial versus non-familial forms of illness. Br J Psychiatry. 1989;155:444–450. doi: 10.1192/bjp.155.4.444. [DOI] [PubMed] [Google Scholar]
- Kelsoe JR, Jr, Cadet JL, Pickar D, Weinberger DR. Quantitative neuroanatomy in schizophrenia. A controlled magnetic resonance imaging study. Arch Gen Psychiatry. 1988;45:533–541. doi: 10.1001/archpsyc.1988.01800300029003. [DOI] [PubMed] [Google Scholar]
- Kemali D, Maj M, Galderisi S, Salvati A, Starace F, Valente A, Pirozzi R. Clinical, biological, and neuropsychological features associated with lateral ventricular enlargement in DSM-III schizophrenic disorder. Psychiatry Res. 1987;21(2):137–149. doi: 10.1016/0165-1781(87)90071-0. [DOI] [PubMed] [Google Scholar]
- Kim DK, Shin YM, Kim CE, Cho HS, Kim YS. Electrodermal responsiveness, clinical variables, and brain imaging in male chronic schizophrenics. Biol Psychiatry. 1993;33(11–12):786–793. doi: 10.1016/0006-3223(93)90019-a. [DOI] [PubMed] [Google Scholar]
- Klausner JD, Sweeney JA, Deck MD, Haas GL, Kelly AB. Clinical correlates of cerebral ventricular enlargement in schizophrenia. Further evidence for frontal lobe disease. J Nerv Ment Dis. 1992;180(7):407–412. doi: 10.1097/00005053-199207000-00001. [DOI] [PubMed] [Google Scholar]
- Kling AS, Metter EJ, Riege WH, Kuhl DE. Comparison of PET measurement of local brain glucose metabolism and CAT measurement of brain atrophy in chronic schizophrenia and depression. Am J Psychiatry. 1986;143(2):175–180. doi: 10.1176/ajp.143.2.175. [DOI] [PubMed] [Google Scholar]
- Kurokawa K, Nakamura K, Sumiyoshi T, Hagino H, Yotsutsuji T, Yamashita I, Suzuki M, Matsui M, Kurachi M. Ventricular enlargement in schizophrenia spectrum patients with prodromal symptoms of obsessive-compulsive disorder. Psychiatry Res. 2000;99(2):83–91. doi: 10.1016/s0925-4927(00)00058-5. [DOI] [PubMed] [Google Scholar]
- Lauer CJ, Schreiber W, Pollmacher T, Holsboer F, Krieg JC. Sleep in schizophrenia: a polysomnographic study on drug-naive patients. Neuropsychopharmacology. 1997;16(1):51–60. doi: 10.1016/S0893-133X(96)00159-5. [DOI] [PubMed] [Google Scholar]
- Lewine RR, Risch SC, Risby E, Stipetic M, Jewart RD, Eccard M, Caudle J, Pollard W. Lateral ventricle-brain ratio and balance between CSF HVA and 5-HIAA in schizophrenia. Am J Psychiatry. 1991;148(9):1189–1194. doi: 10.1176/ajp.148.9.1189. [DOI] [PubMed] [Google Scholar]
- Losonczy MF, I, Song S, Mohs RC, Small NA, Davidson M, Johns CA, Davis KL. Correlates of lateral ventricular size in chronic schizophrenia, I: Behavioral and treatment response measures. Am J Psychiatry. 1986;143(8):976–981. doi: 10.1176/ajp.143.8.976. [DOI] [PubMed] [Google Scholar]
- Luchins DJ, Lewine RR, Meltzer HY. Lateral ventricular size, psychopathology, and medication response in the psychoses. Biol Psychiatry. 1984;19(1):29–44. [PubMed] [Google Scholar]
- Luchins DJ, Meltzer HY. A comparison of CT findings in acute and chronic schizophrenia. Psychiatry Res. 1986;17:7–14. doi: 10.1016/0165-1781(86)90036-3. [DOI] [PubMed] [Google Scholar]
- Miller R. Computerised tomography in schizophrenia. Br J Psychiatry. 1991;158:863. doi: 10.1192/bjp.158.6.863a. [DOI] [PubMed] [Google Scholar]
- Moscarelli M, Cesana BM, Ciussani S, Novati NC, Cazzullo CL. Ventricle-brain ratio and alogia in 19 young patients with chronic negative and positive schizophrenia. Am J Psychiatry. 1989;146(2):257–258. doi: 10.1176/ajp.146.2.257. [DOI] [PubMed] [Google Scholar]
- Nasrallah HA, Schwarzkopf SB, Olson SC, Coffman JA. Gender differences in schizophrenia on MRI brain scans. Schizophr Bull. 1990;16(2):205–210. doi: 10.1093/schbul/16.2.205. [DOI] [PubMed] [Google Scholar]
- Nasrallah HA, Jacoby CG, McCalley-Whitters M, Kuperman S. Cerebral ventricular enlargement in subtypes of chronic schizophrenia. Arch Gen Psychiatry. 1982;39(7):774–777. doi: 10.1001/archpsyc.1982.04290070010003. [DOI] [PubMed] [Google Scholar]
- Northoff G, Waters H, Mooren I, Schluter U, Diekmann S, Falkai P, Bogerts B. Cortical sulcal enlargement in catatonic schizophrenia: a planimetric CT study. Psychiatry Res. 1999;91(1):45–54. doi: 10.1016/s0925-4927(99)00024-4. [DOI] [PubMed] [Google Scholar]
- Obiols JE, Marcos T, Salamero M. Ventricular enlargement and neuropsychological testing in schizophrenia. Acta Psychiatr Scand. 1987;76(2):199–202. doi: 10.1111/j.1600-0447.1987.tb02884.x. [DOI] [PubMed] [Google Scholar]
- Obiols Llandrich JE, Ruscalleda J, Masferrer M. Ventricular enlargement in young chronic schizophrenics. Acta Psychiatr Scand. 1986;73(1):42–44. doi: 10.1111/j.1600-0447.1986.tb02664.x. [DOI] [PubMed] [Google Scholar]
- Ohaeri JU, Adeyinka AO, Enyidah SN, Osuntokun BO. Schizophrenic and manic brains in Nigerians. Computerised tomography findings. Br J Psychiatry. 1995;166(4):496–500. doi: 10.1192/bjp.166.4.496. [DOI] [PubMed] [Google Scholar]
- Ohara K, Xu HD, Matsunaga T, Xu DS, Huang XQ, Gu GF, Ohara K, Wang ZC. Cerebral ventricle-brain ratio in monozygotic twins discordant and concordant for schizophrenia. Prog Neuropsychopharmacol Biol Psychiatry. 1998;22(6):1043–1050. doi: 10.1016/s0278-5846(98)00048-7. [DOI] [PubMed] [Google Scholar]
- Owen MJ, Lewis SW, Murray RM. Family history and cerebral ventricular enlargement in schizophrenia. A case control study. Br J Psychiatry. 1989;154:629–634. doi: 10.1192/bjp.154.5.629. [DOI] [PubMed] [Google Scholar]
- Pandurangi AK, Dewan MJ, Lee SH, Ramachandran T, Levy BF, Boucher M, Yozawitz A, Major L. The ventricular system in chronic schizophrenic patients. A controlled computed tomography study. Br J Psychiatry. 1984;144:172–176. doi: 10.1192/bjp.144.2.172. [DOI] [PubMed] [Google Scholar]
- Pearlson GD, Veroff AE, McHugh PR. The use of computed tomography in psychiatry: recent applications to schizophrenia, manic-depressive illness and dementia syndromes. Johns Hopkins Med J. 1981;149(5):194–202. [PubMed] [Google Scholar]
- Pearlson GD, Tune LE, Wong DF, Aylward EH, Barta PE, Powers RE, Tien AY, Chase GA, Harris GJ, Rabins PV. Quantitative D2 dopamine receptor PET and structural MRI changes in late-onset schizophrenia. Schizophr Bull. 1993;19(4):783–795. doi: 10.1093/schbul/19.4.783. [DOI] [PubMed] [Google Scholar]
- Pearlson GD, Garbacz DJ, Breakey WR, Ahn HS, DePaulo JR. Lateral ventricular enlargement associated with persistent unemployment and negative symptoms in both schizophrenia and bipolar disorder. Psychiatry Res. 1984;12(1):1–9. doi: 10.1016/0165-1781(84)90133-1. [DOI] [PubMed] [Google Scholar]
- Puri BK, Hutton SB, Saeed N, Oatridge A, Hajnal JV, Duncan L, Chapman MJ, Barnes TR, Bydder GM, Joyce EM. A serial longitudinal quantitative MRI study of cerebral changes in first-episode schizophrenia using image segmentation and subvoxel registration. Psychiatry Res. 2001;106(2):141–150. doi: 10.1016/s0925-4927(01)00072-5. [DOI] [PubMed] [Google Scholar]
- Reite M, Reite E, Collins D, Teale P, Rojas DC, Sandberg E. Brain size and brain/intracranial volume ratio in major mental illness. BMC Psychiatry. 2010;10:79. doi: 10.1186/1471-244X-10-79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Risch SC, Lewine RJ, Kalin NH, Jewart RD, Risby ED, Caudle JM, Stipetic M, Turner J, Eccard MB, Pollard WE. Limbic-hypothalamic-pituitary-adrenal axis activity and ventricular-to-brain ratio studies in affective illness and schizophrenia. Neuropsychopharmacology. 1992;6(2):95–100. [PubMed] [Google Scholar]
- Rossi A, Stratta P, Gallucci M, Passariello R, Casacchia M. Quantification of corpus callosum and ventricles in schizophrenia with nuclear magnetic resonance imaging: a pilot study. Am J Psychiatry. 1989;146(1):99–101. doi: 10.1176/ajp.146.1.99. [DOI] [PubMed] [Google Scholar]
- Rossi A, Stratta P, Mancini F, Gallucci M, Mattei P, Core L, Di Michele V, Casacchia M. Magnetic resonance imaging findings of amygdala-anterior hippocampus shrinkage in male patients with schizophrenia. Psychiatry Res. 1994;52(1):43–53. doi: 10.1016/0165-1781(94)90119-8. [DOI] [PubMed] [Google Scholar]
- Rossi A, Stratta P, Casacchia M, D'Albenzio L, Schiazza G, De Donatis M. Age and duration of illness as predictors of ventricular brain ratio (VBR) size in chronic schizophrenic patients. A stepwise regression analysis study. Acta Psychiatr Scand. 1987;76(3):256–260. doi: 10.1111/j.1600-0447.1987.tb02893.x. [DOI] [PubMed] [Google Scholar]
- Rossi A, Stratta P, Gallucci M, Passariello R, Casacchia M. Brain morphology in schizophrenia by magnetic resonance imaging (MRI) Acta Psychiatr Scand. 1988;77(6):741–745. doi: 10.1111/j.1600-0447.1988.tb05197.x. [DOI] [PubMed] [Google Scholar]
- Rubin P, Karle A, Moller-Madsen S, Hertel C, Povlsen UJ, Noring U, Hemmingsen R. Computerised tomography in newly diagnosed schizophrenia and schizophreniform disorder. A controlled blind study. Br J Psychiatry. 1993;163:604–612. doi: 10.1192/bjp.163.5.604. [DOI] [PubMed] [Google Scholar]
- Sacchetti E, Calzeroni A, Vita A, Terzi A, Pollastro F, Cazzullo CL. The brain damage hypothesis of the seasonality of births in schizophrenia and major affective disorders: evidence from computerised tomography. Br J Psychiatry. 1992;160:390–397. doi: 10.1192/bjp.160.3.390. [DOI] [PubMed] [Google Scholar]
- Sallet PC, Elkis H, Alves TM, Oliveira JR, Sassi E, de Castro CC, Busatto GF, Gattaz WF. Rightward cerebral asymmetry in subtypes of schizophrenia according to Leonhard's classification and to DSM-IV: a structural MRI study. Psychiatry Res. 2003;123(1):65–79. doi: 10.1016/s0925-4927(03)00020-9. [DOI] [PubMed] [Google Scholar]
- Scottish Schizophrenia Research Group. Mac Donald HL, West JJ. The Scottish first episode schizophrenia study: VI computerized tomography brain scans in patients and controls. British Journal of Psychiatry. 1989;154:492–498. doi: 10.1192/bjp.154.4.492. [DOI] [PubMed] [Google Scholar]
- Schulz SC, Koller MM, Kishore PR, Hamer RM, Gehl JJ, Friedel RO. Ventricular enlargement in teenage patients with schizophrenia spectrum disorder. Am J Psychiatry. 1983;140(12):1592–1595. doi: 10.1176/ajp.140.12.1592. [DOI] [PubMed] [Google Scholar]
- Shelton RC, Karson CN, Doran AR, Pickar D, Bigelow LB, Weinberger DR. Cerebral structural pathology in schizophrenia: evidence for a selective prefrontal cortical defect. Am J Psychiatry. 1988;145(2):154–163. doi: 10.1176/ajp.145.2.154. [DOI] [PubMed] [Google Scholar]
- Shima S, Kanba S, Masuda Y, Tsukumo T, Kitamura T, Asai M. Normal ventricles in chronic schizophrenics. Acta Psychiatr Scand. 1985;71(1):25–29. doi: 10.1111/j.1600-0447.1985.tb05047.x. [DOI] [PubMed] [Google Scholar]
- Siever LJ, Rotter M, Losonczy M, Guo SL, Mitropoulou V, Trestman R, Apter S, Zemishlany Z, Silverman J, Horvath TB. Lateral ventricular enlargement in schizotypal personality disorder. Psychiatry Res. 1995;57(2):109–118. doi: 10.1016/0165-1781(95)02645-d. [DOI] [PubMed] [Google Scholar]
- Silverman JM, Smith CJ, Guo SL, Mohs RC, Siever LJ, Davis KL. Lateral ventricular enlargement in schizophrenic probands and their siblings with schizophrenia-related disorders. Biol Psychiatry. 1998;43(2):97–106. doi: 10.1016/s0006-3223(97)00247-3. [DOI] [PubMed] [Google Scholar]
- Smeraldi E, Gambini O, Bellodi L, Sacchetti E, Vita A, di Rosa M, Macciardi F, Cazzullo CL. Combined measure of smooth pursuit eye movements and ventricle-brain ratio in schizophrenic disorders. Psychiatry Res. 1987;21(4):293–301. doi: 10.1016/0165-1781(87)90012-6. [DOI] [PubMed] [Google Scholar]
- Smith GN, Iacono WG. Ventricular size in schizophrenia: importance of choice of control subjects. Psychiatry Res. 1988;26(2):241–243. doi: 10.1016/0165-1781(88)90078-9. [DOI] [PubMed] [Google Scholar]
- Smith RC, Baumgartner R, Ravichandran GK, Mauldin M, Burd A, Vroulis G, Gordon J, Calderon M. Lateral ventricular enlargement and clinical response in schizophrenia. Psychiatry Res. 1985;14(3):241–253. doi: 10.1016/0165-1781(85)90019-8. [DOI] [PubMed] [Google Scholar]
- Sponheim SR, Iacono WG, Beiser M. Stability of ventricular size after the onset of psychosis in schizophrenia. Psychiatry Res. 1991;40(1):21–29. doi: 10.1016/0925-4927(91)90026-m. [DOI] [PubMed] [Google Scholar]
- Vazquez-Barquero JL, Cuesta Nunez MJ, Quintana Pando F, de la Varga M, Herrera Castanedo S, Dunn G. Structural abnormalities of the brain in schizophrenia: sex differences in the Cantabria First Episode of Schizophrenia Study. Psychol Med. 1995;25(6):1247–1257. doi: 10.1017/s0033291700033213. [DOI] [PubMed] [Google Scholar]
- Vita A, Dieci M, Giobbio GM, Garbarini M, Morganti C, Braga M, Invernizzi G. A reconsideration of the relationship between cerebral structural abnormalities and family history of schizophrenia. Psychiatry Res. 1994;53(1):41–55. doi: 10.1016/0165-1781(94)90094-9. [DOI] [PubMed] [Google Scholar]
- Vita A, Dieci M, Silenzi C, Tenconi F, Giobbio GM, Invernizzi G. Cerebral ventricular enlargement as a generalized feature of schizophrenia: a distribution analysis on 502 subjects. Schizophr Res. 2000;44(1):25–34. doi: 10.1016/s0920-9964(99)00134-6. [DOI] [PubMed] [Google Scholar]
- Weinberger DR, Torrey EF, Neophytides AN, Wyatt RJ. Lateral cerebral ventricular enlargement in chronic schizophrenia. Arch Gen Psychiatry. 1979;36:735–739. doi: 10.1001/archpsyc.1979.01780070013001. [DOI] [PubMed] [Google Scholar]
- Weinberger DR, DeLisi LE, Perman GP, Targum S, Wyatt RJ. Computed tomography in schizophreniform disorder and other acute psychiatric disorders. Arch Gen Psychiatry. 1982;39(7):778–783. doi: 10.1001/archpsyc.1982.04290070014004. [DOI] [PubMed] [Google Scholar]
- Williams AO, Reveley MA, Kolakowska T, Ardern M, Mandelbrote BM. Schizophrenia with good and poor outcome. II: Cerebral ventricular size and its clinical significance. Br J Psychiatry. 1985;146:239–246. doi: 10.1192/bjp.146.3.239. [DOI] [PubMed] [Google Scholar]
- Wilms G, Van Ongeval C, Baert AL, Claus A, Bollen J, De Cuyper H, Eneman M, Malfroid M, Peuskens J, Heylen S. Ventricular enlargement, clinical correlates and treatment outcome in chronic schizophrenic inpatients. Acta Psychiatr Scand. 1992;85(4):306–312. doi: 10.1111/j.1600-0447.1992.tb01474.x. [DOI] [PubMed] [Google Scholar]
CITATIONS FOR ARTICLES NOT INCLUDED THE META-ANALYSIS
- Aso M, Kurachi M, Suzuki M, Yuasa S, Matsui M, Saitoh O. Asymmetry of the ventricle and age at the onset of schizophrenia. Eur Arch Psychiatry Clin Neurosci. 1995;245(3):142–144. doi: 10.1007/BF02193086. [DOI] [PubMed] [Google Scholar]
- Barak Y, Aizenberg D, Mirecki I, Mazeh D, Achiron A. Very late-onset schizophrenia-like psychosis: clinical and imaging characteristics in comparison with elderly patients with schizophrenia. J Nerv Ment Dis. 2002;190(11):733–736. doi: 10.1097/00005053-200211000-00002. [DOI] [PubMed] [Google Scholar]
- Benson KL, Sullivan EV, Lim KO, Lauriello J, Zarcone VP, Jr, Pfefferbaum A. Slow wave sleep and computed tomographic measures of brain morphology in schizophrenia. Psychiatry Res. 1996;60(2–3):125–134. doi: 10.1016/0165-1781(96)02705-9. [DOI] [PubMed] [Google Scholar]
- Bornstein RA, Schwarzkopf SB, Olson SC, Nasrallah HA. Third-ventricle enlargement and neuropsychological deficit in schizophrenia. Biol Psychiatry. 1992;31(9):954–961. doi: 10.1016/0006-3223(92)90121-f. [DOI] [PubMed] [Google Scholar]
- Caputo A, Ghiringhelli L, Dieci M, Giobbio GM, Tenconi F, Ferrari L, Gimosti E, Prato K, Vita A. Epithalamus calcifications in schizophrenia. Eur Arch Psychiatry Clin Neurosci. 1998;248(6):272–276. doi: 10.1007/s004060050049. [DOI] [PubMed] [Google Scholar]
- Chang K, Barnea-Goraly N, Karchemskiy A, Simeonova DI, Barnes P, Ketter T, Reiss AL. Cortical magnetic resonance imaging findings in familial pediatric bipolar disorder. Biol Psychiatry. 2005;58(3):197–203. doi: 10.1016/j.biopsych.2005.03.039. [DOI] [PubMed] [Google Scholar]
- Curtis CE, Iacono WG, Beiser M. Relationship between nailfold plexus visibility and clinical, neuropsychological, and brain structural measures in schizophrenia. Biol Psychiatry. 1999;46(1):102–109. doi: 10.1016/s0006-3223(98)00363-1. [DOI] [PubMed] [Google Scholar]
- Davis KL, Buchsbaum MS, Shihabuddin L, Spiegel-Cohen J, Metzger M, Frecska E, Keefe RS, Powchik P. Ventricular enlargement in poor-outcome schizophrenia. Biol Psychiatry. 1998;43(11):783–793. doi: 10.1016/s0006-3223(97)00553-2. [DOI] [PubMed] [Google Scholar]
- DeQuardo JR, Goldman M, Tandon R. VBR in schizophrenia: relationship to family history of psychosis and season of birth. Schizophr Res. 1996;20(3):275–285. doi: 10.1016/0920-9964(95)00003-8. [DOI] [PubMed] [Google Scholar]
- DeQuardo JR, Tandon R, Goldman R, Meador-Woodruff JH, McGrath-Giroux M, Brunberg JA, Kim L. Ventricular enlargement, neuropsychological status, and premorbid function in schizophrenia. Biol Psychiatry. 1994;35(8):517–524. doi: 10.1016/0006-3223(94)90098-1. [DOI] [PubMed] [Google Scholar]
- Dequardo JR, Tomori O, Brunberg JA, Tandon R. Does neuroanatomy predict ECT response? Prog Neuropsychopharmacol Biol Psychiatry. 1997;21(8):1339–1352. doi: 10.1016/s0278-5846(97)00168-1. [DOI] [PubMed] [Google Scholar]
- Emsley R, Roberts M, Smith R, Spangenberg J, Chalton D. Disordered water homeostasis in schizophrenia and cerebral ventricular size. Br J Psychiatry. 1995;166(4):501–506. doi: 10.1192/bjp.166.4.501. [DOI] [PubMed] [Google Scholar]
- Farmer RL, Pandurangi AK. Diversity in schizophrenia: toward a richer biopsychosocial understanding for social work practice. Health Soc Work. 1997;22(2):109–116. doi: 10.1093/hsw/22.2.109. [DOI] [PubMed] [Google Scholar]
- Ford RA, Lewis SW, Syed GM, Reveley A, Toone BK. Ventricular size and regional cerebral blood flow in schizophrenia: an attempted replication. Psychiatry Res. 1992;45(4):209–213. [PubMed] [Google Scholar]
- Friedman L, Knutson L, Shurell M, Meltzer HY. Prefrontal sulcal prominence is inversely related to response to clozapine in schizophrenia. Biol Psychiatry. 1991;29(9):865–877. doi: 10.1016/0006-3223(91)90053-o. [DOI] [PubMed] [Google Scholar]
- Gaser C, Nenadic I, Buchsbaum BR, Hazlett EA, Buchsbaum MS. Ventricular enlargement in schizophrenia related to volume reduction of the thalamus, striatum, and superior temporal cortex. Am J Psychiatry. 2004;161(1):154–156. doi: 10.1176/appi.ajp.161.1.154. [DOI] [PubMed] [Google Scholar]
- Goldberg TE, Bigelow LB, Weinberger DR, Daniel DG, Kleinman JE. Cognitive and behavioral effects of the coadministration of dextroamphetamine and haloperidol in schizophrenia. Am J Psychiatry. 1991;148(1):78–84. doi: 10.1176/ajp.148.1.78. [DOI] [PubMed] [Google Scholar]
- Goldman M, Tandon R, DeQuardo JR, Taylor SF, Goodson J, McGrath M. Biological predictors of 1-year outcome in schizophrenia in males and females. Schizophr Res. 1996;21(2):65–73. doi: 10.1016/0920-9964(96)00021-7. [DOI] [PubMed] [Google Scholar]
- Hata K, Iida J, Iwasaka H, Negoro H, Kishimoto T. Association between minor physical anomalies and lateral ventricular enlargement in childhood and adolescent onset schizophrenia. Acta Psychiatr Scand. 2003;108(2):147–151. doi: 10.1034/j.1600-0447.2003.00116.x. [DOI] [PubMed] [Google Scholar]
- Hoffman WF, Ballard L, Turner EH, Casey DE. Three-year follow-up of older schizophrenics: extrapyramidal syndromes, psychiatric symptoms, and ventricular brain ratio. Biol Psychiatry. 1991;30(9):913–926. doi: 10.1016/0006-3223(91)90005-7. [DOI] [PubMed] [Google Scholar]
- Juckel G, Reischies FM, Muller-Schubert A, Vogel AC, Gaebel W, Hegerl U. Ventricle size and P300 in schizophrenia. Eur Arch Psychiatry Clin Neurosci. 1994;243(6):352–354. doi: 10.1007/BF02195730. [DOI] [PubMed] [Google Scholar]
- Keshavan MS, Reynolds CF, 3rd, Ganguli R, Brar J, Houck P. Electroencephalographic sleep and cerebral morphology in functional psychoses: a preliminary study with computed tomography. Psychiatry Res. 1991;39(3):293–301. doi: 10.1016/0165-1781(91)90095-7. [DOI] [PubMed] [Google Scholar]
- King DJ, Wilson A, Cooper SJ, Waddington JL. The clinical correlates of neurological soft signs in chronic schizophrenia. Br J Psychiatry. 1991;158:770–775. doi: 10.1192/bjp.158.6.770. [DOI] [PubMed] [Google Scholar]
- Kirch DG, Alexander RC, Suddath RL, Papadopoulos NM, Kaufmann CA, Daniel DG, Wyatt RJ. Blood-CSF barrier permeability and central nervous system immunoglobulin G in schizophrenia. J Neural Transm Gen Sect. 1992;89(3):219–232. doi: 10.1007/BF01250674. [DOI] [PubMed] [Google Scholar]
- Lauer CJ, Krieg JC. Slow-wave sleep and ventricular size: a comparative study in schizophrenia and major depression. Biol Psychiatry. 1998;44(2):121–128. doi: 10.1016/s0006-3223(97)00342-9. [DOI] [PubMed] [Google Scholar]
- Leadbetter RA, Shutty MS, Jr, Elkashef AM, Kirch DG, Spraggins T, Cail WS, Wu H, Bilder RM, Lieberman JA, Wyatt RJ. MRI changes during water loading in patients with polydipsia and intermittent hyponatremia. Am J Psychiatry. 1999;156(6):958–960. doi: 10.1176/ajp.156.6.958. [DOI] [PubMed] [Google Scholar]
- Lesser IM, Miller BL, Swartz JR, Boone KB, Mehringer CM, Mena I. Brain imaging in late-life schizophrenia and related psychoses. Schizophr Bull. 1993;19(4):773–782. doi: 10.1093/schbul/19.4.773. [DOI] [PubMed] [Google Scholar]
- Levitt JJ, Shenton ME, McCarley RW, Faux SF, Ludwig AS. Premorbid adjustment in schizophrenia: implications for psychosocial and ventricular pathology. Schizophr Res. 1994;12(2):159–168. doi: 10.1016/0920-9964(94)90073-6. [DOI] [PubMed] [Google Scholar]
- Mauri MC, Vita A, Giobbio GM, Ferrara A, Dieci M, Bitetto A, Altamura AC. Prediction of response to haloperidol in schizophrenia: neuroendocrine, neuromorphological and clinical variables. Int Clin Psychopharmacol. 1994;9(1):3–7. doi: 10.1097/00004850-199400910-00001. [DOI] [PubMed] [Google Scholar]
- McCreadie RG, Thara R, Padmavati R, Srinivasan TN, Jaipurkar SD. Structural brain differences between never-treated patients with schizophrenia, with and without dyskinesia, and normal control subjects: a magnetic resonance imaging study. Arch Gen Psychiatry. 2002;59(4):332–336. doi: 10.1001/archpsyc.59.4.332. [DOI] [PubMed] [Google Scholar]
- Ohara K, Sato Y, Tanabu S, Yoshida K, Shibuya H. Magnetic resonance imaging study of the ventricle-brain ratio in parents of schizophrenia subjects. Prog Neuropsychopharmacol Biol Psychiatry. 2006;30(1):89–92. doi: 10.1016/j.pnpbp.2005.06.007. [DOI] [PubMed] [Google Scholar]
- Ohrmann P, Siegmund A, Suslow T, Spitzberg K, Kersting A, Arolt V, Heindel W, Pfleiderer B. Evidence for glutamatergic neuronal dysfunction in the prefrontal cortex in chronic but not in first-episode patients with schizophrenia: a proton magnetic resonance spectroscopy study. Schizophr Res. 2005;73(2–3):153–157. doi: 10.1016/j.schres.2004.08.021. [DOI] [PubMed] [Google Scholar]
- Pandurangi AK, Pelonero AL, Nadel L, Calabrese VP. Brain structure changes in schizophrenics with high serum titers of antibodies to herpes virus. Schizophr Res. 1994;11(3):245–250. doi: 10.1016/0920-9964(94)90018-3. [DOI] [PubMed] [Google Scholar]
- Puri BK, Richardson AJ, Oatridge A, Hajnal JV, Saeed N. Cerebral ventricular asymmetry in schizophrenia: a high resolution 3D magnetic resonance imaging study. Int J Psychophysiol. 1999;34(3):207–211. doi: 10.1016/s0167-8760(99)00078-1. [DOI] [PubMed] [Google Scholar]
- Puri BK, Saeed N, Richardson AJ, Oatridge A, Hajnal JV, Bydder GM. Schizophrenia syndromes associated with changes in ventricle-to-brain ratios: a serial high-resolution three-dimensional magnetic resonance imaging study in first-episode schizophrenia patients using subvoxel registration and semiautomated quantification. Int J Clin Pract. 2005;59(4):399–402. doi: 10.1111/j.1368-5031.2005.00501.x. [DOI] [PubMed] [Google Scholar]
- Sandyk R. Pineal and habenula calcification in schizophrenia. Int J Neurosci. 1992;67(1–4):19–30. doi: 10.3109/00207459208994773. [DOI] [PubMed] [Google Scholar]
- Sandyk R. The relationship of thought disorder to third ventricle width and calcification of the pineal gland in chronic schizophrenia. Int J Neurosci. 1993;68(1–2):53–59. doi: 10.3109/00207459308994259. [DOI] [PubMed] [Google Scholar]
- Sandyk R, Kay SR. The relationship of pineal calcification to cortical atrophy in schizophrenia. Int J Neurosci. 1991;57(3–4):179–191. doi: 10.3109/00207459109150692. [DOI] [PubMed] [Google Scholar]
- Schroder J, Buchsbaum MS, Siegel BV, Geider FJ, Niethammer R. Structural and functional correlates of subsyndromes in chronic schizophrenia. Psychopathology. 1995;28(1):38–45. doi: 10.1159/000284898. [DOI] [PubMed] [Google Scholar]
- Schroder J, Geider FJ, Binkert M, Reitz C, Jauss M, Sauer H. Subsyndromes in chronic schizophrenia: do their psychopathological characteristics correspond to cerebral alterations? Psychiatry Res. 1992;42(3):209–220. doi: 10.1016/0165-1781(92)90113-h. [DOI] [PubMed] [Google Scholar]
- Shioiri T, Hamakawa H, Kato T, Fujii K, Murashita J, Inubushi T, Someya T. Frontal lobe membrane phospholipid metabolism and ventricle to brain ratio in schizophrenia: preliminary 31P-MRS and CT studies. Eur Arch Psychiatry Clin Neurosci. 2000;250(4):169–174. doi: 10.1007/s004060070021. [DOI] [PubMed] [Google Scholar]
- Shiraishi H, Koizumi J, Ofuku K, Suzuki T, Saito K, Hori T, Ikuta T, Kase K, Hori M. Enlargement of the anterior horn of the lateral ventricle in schizophrenic patients: chronological and morphometrical studies. Jpn J Psychiatry Neurol. 1990;44(4):693–702. doi: 10.1111/j.1440-1819.1990.tb01646.x. [DOI] [PubMed] [Google Scholar]
- Tabarés-Seisdedos R, Balanza-Martinez V, Pallardo Y, Salazar-Fraile J, Selva G, Vilela C, Vallet M, Leal C, Gomez-Beneyto M. Similar effect of family history of psychosis on Sylvian fissure size and auditory P200 amplitude in schizophrenic and bipolar subjects. Psychiatry Res. 2001;108(1):29–38. doi: 10.1016/s0925-4927(01)00113-5. [DOI] [PubMed] [Google Scholar]
- Tandon R, DeQuardo JR, Taylor SF, McGrath M, Jibson M, Eiser A, Goldman M. Phasic and enduring negative symptoms in schizophrenia: biological markers and relationship to outcome. Schizophr Res. 2000;45(3):191–201. doi: 10.1016/s0920-9964(99)00163-2. [DOI] [PubMed] [Google Scholar]
- Tandon R, Greden JF. Negative symptoms of schizophrenia: the need for conceptual clarity. Biol Psychiatry. 1991;30(4):321–325. doi: 10.1016/0006-3223(91)90287-v. [DOI] [PubMed] [Google Scholar]
- Tandon R, Mazzara C, DeQuardo J, Craig KA, Meador-Woodruff JH, Goldman R, Greden JF. Dexamethasone suppression test in schizophrenia: relationship to symptomatology, ventricular enlargement, and outcome. Biol Psychiatry. 1991;29(10):953–964. doi: 10.1016/0006-3223(91)90353-n. [DOI] [PubMed] [Google Scholar]
- Tsai G, van Kammen DP, Chen S, Kelley ME, Grier A, Coyle JT. Glutamatergic neurotransmission involves structural and clinical deficits of schizophrenia. Biol Psychiatry. 1998;44(8):667–674. doi: 10.1016/s0006-3223(98)00151-6. [DOI] [PubMed] [Google Scholar]
- van Kammen DP, Kelley ME, Gilbertson MW, Gurklis J, O'Connor DT. CSF dopamine beta-hydroxylase in schizophrenia: associations with premorbid functioning and brain computerized tomography scan measures. Am J Psychiatry. 1994;151(3):372–378. doi: 10.1176/ajp.151.3.372. [DOI] [PubMed] [Google Scholar]
- van Kammen DP, Petty F, Kelley ME, Kramer GL, Barry EJ, Yao JK, Gurklis JA, Peters JL. GABA and brain abnormalities in schizophrenia. Psychiatry Res. 1998;82(1):25–35. doi: 10.1016/s0925-4927(98)00006-7. [DOI] [PubMed] [Google Scholar]
- Vita A. Cerebral ventricular abnormalities in schizophrenia: evidence of their early origin and stability over time. Schizophr Res. 1991;5(3):189–190. doi: 10.1016/0920-9964(91)90065-y. [DOI] [PubMed] [Google Scholar]
- Vita A, Dieci M, Giobbio GM, Azzone P, Garbarini M, Sacchetti E, Cesana BM, Cazzullo CL. CT scan abnormalities and outcome of chronic schizophrenia. Am J Psychiatry. 1991;148(11):1577–1579. doi: 10.1176/ajp.148.11.1577. [DOI] [PubMed] [Google Scholar]
- Walker EF, Lewine RR, Neumann C. Childhood behavioral characteristics and adult brain morphology in schizophrenia. Schizophr Res. 1996;22(2):93–101. doi: 10.1016/s0920-9964(96)00070-9. [DOI] [PubMed] [Google Scholar]
- Young AH, Blackwood DH, Roxborough H, McQueen JK, Martin MJ, Kean D. A magnetic resonance imaging study of schizophrenia: brain structure and clinical symptoms. Br J Psychiatry. 1991;158:158–164. doi: 10.1192/bjp.158.2.158. [DOI] [PubMed] [Google Scholar]
- Zorrilla LT, Cannon TD, Kronenberg S, Mednick SA, Schulsinger F, Parnas J, Praestholm J, Vestergaard A. Structural brain abnormalities in schizophrenia: a family study. Biol Psychiatry. 1997;42(12):1080–1086. doi: 10.1016/s0006-3223(97)00006-1. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.