Abstract
Background
The reasons for racial/ethnic disparities in hypertension prevalence in the U.S are poorly understood.
Methods
Using data from the Multi-Ethnic Study of Atherosclerosis (MESA), we investigated whether individual and neighborhood-level chronic stressors contribute to these disparities in cross-sectional analyses. The sample consisted of 2679 MESA participants (45–84yrs) residing in Baltimore, New York, and North Carolina. Hypertension was defined as systolic or diastolic blood pressure ≥140 or 90mmHg, or taking anti-hypertensive medications. Individual-level chronic stress was measured by self-reported chronic burden and perceived major and everyday discrimination. A measure of neighborhood (census tract) chronic stressors (i.e. physical disorder, violence) was developed using data from a telephone survey conducted with other residents of MESA neighborhoods. Binomial regression was used to estimate associations between hypertension and race/ethnicity before and after adjustment for individual and neighborhood stressors.
Results
The prevalence of hypertension was 59.5% in African Americans (AA), 43.9% in Hispanics, and 42.0% in whites. Age and sex adjusted relative prevalences of hypertension (compared to whites) were 1.30 [95% Confidence Interval (CI): 1.22–1.38] for AA and 1.16 [95% CI: 1.04–1.31] for Hispanics. Adjustment for neighborhood stressors reduced these to 1.17 [95% CI: 1.11–1.22] and 1.09 [95% CI: 1.00–1.18] respectively. Additional adjustment for individual-level stressors, acculturation, income, education, and other neighborhood features only slightly reduced these associations.
Conclusion
Neighborhood chronic stressors may contribute to race/ethnic differences in hypertension prevalence in the U.S.
Keywords: neighborhoods, race, ethnicity, chronic stress, discrimination
Introduction
Despite a large body of literature documenting a greater prevalence of hypertension (HTN) and hypertension related morbidity and mortality among African Americans compared to whites, such differences remain poorly understood. (1, 2) Research on disparities in hypertension has focused on biological differences, (3–5) socioeconomic position, (6) and health behaviors (diet, physical inactivity) (7–9) as potential explanations. However many argue that an examination of psychosocial stressors and potentially stress-generating structural/contextual factors is necessary for a full understanding of racial/ethnic disparities in health in general and in hypertension in particular. (10–12)
Psychosocial stressors previously associated with hypertension include stressful life events, perceived discrimination, and job strain. (13–16) However, few studies have examined the contribution of psychosocial stressors to race/ethnic differences in hypertension or other blood-pressure related outcomes.(16–18) When examined, generally, only one type of stressor is considered and rarely are stressors defined at multiple levels considered. Stress is multidimensional in nature and multiple sources of stress may cluster in individuals.(19) For example, in addition to stressful life events neighborhoods may also serve as stressors via neighborhood problems (e.g. vandalism, violence, overcrowding, noise) or disorder (physical and social)(19–21). Exposure to these stressors may cause individuals to perceive their environment as threatening and cause a direct physiologic stress response that may induce hypertension or affect hypertension by hindering physical activity. The lack of resources in neighborhoods may also limit resident's ability to cope with other sources of stress in their lives.(20, 21)
The few studies that have investigated associations between neighborhood stressors and hypertension or hypertension-related mortality, use census derived indicators of socioeconomic position (SEP) as proxies for specific features of neighborhood environments that may be chronic stressors. (22, 23) These measures of neighborhood SEP may be poor proxies for the potentially stress-inducing features of residential environments. (20) To more precisely examine the contribution of neighborhood-level stressors on racial/ethnic differences in hypertension prevalence we used direct measures of neighborhood stressors. Based on prior work (24), we hypothesized that multiple neighborhood-level stressors including neighborhood safety and social cohesion among others would be associated with hypertension. Further, we anticipate that the association between race/ethnicity and hypertension would be reduced after adjusting for neighborhood and individual-level chronic stressors.
Materials and Methods
Study Population
The Multi-Ethnic Study of Atherosclerosis (MESA) is prospective study of 6814 men and women age 45 to 84 years recruited from six study sites within the U.S. (Baltimore, MD; Chicago, IL; Forsyth County, NC; Los Angeles, CA; northern, New York City, NY; and St. Paul, MN). Participants free from clinical cardiovascular disease (CVD) at baseline were recruited between August 1, 2000 and July 30, 2002. Participation rates among those screened and deemed eligible was 59.8%. Detailed sampling and recruitment procedures have been previously described. (25) The institutional review boards at all participating centers approved the study, and all participants gave informed consent.
In this study, we use a subsample of MESA participants restricted to three of the six study sites for which enriched neighborhood information was available (New York, Maryland, North Carolina, N=3265) as part of the MESA ancillary Neighborhood Study. Additionally, we restricted analyses to those with baseline addresses that were successfully geocoded and with complete information on study covariates (N=2679, 82% of MESA subsample).
Outcome variable
Resting seated blood pressure was measured three times using an automated oscillometric sphygmomanometer, and the average of the last two measurements was used for analysis (called “clinic blood pressure”). Hypertension was defined as systolic or diastolic blood pressure ≥ 140 or 90 mmHg respectively, or taking anti-hypertensive medications. (26)
Individual chronic stressors
Three domains of chronic stressors were assessed at the individual level: chronic burden, perceived major discrimination, and everyday discrimination.
Chronic burden was measured using the chronic burden scale. (27) Respondents were asked to indicate whether they had experienced any ongoing problems in five domains [health (self), health (loved one), job, relationship, and financial problems and if any ongoing problems lasted 6 or more months]. Respondents rated how stressful each problem was. Respondents were classified as having chronic burden for each of the five domains if they had experienced the circumstance for at least six months and it was moderately or very stressful. We summed the number of domains in which chronic burden was experienced (0, 1, 2 or more) to estimate overall chronic burden.
A 6 item perceived discrimination scale was adapted from the Detroit Area Study. (28) Respondents were asked to indicate whether they had ever been denied employment or education, unfairly fired, threatened by the police, or prevented from moving into a neighborhood over the lifetime. Respondents were also asked the source of the unfair treatment (race/ethnicity, gender, etc). We use the number of areas in which a person reported experiencing unfair treatment (0, 1, 2 or more), irrespective of the source, to characterize each person's perceived discrimination.
Items for the everyday discrimination scale (9 items) were adapted from The Detroit Area Study. (28) This measure captures the day-to-day minor incidents of unfair treatment. Respondents were asked to indicate the frequency of encounters in which they perceived that they were treated unfairly (i.e. harassed and called names, treated as if you are dishonest, of less value, harmful, or unintelligent) on a day to day basis. Responses for the everyday discrimination scale range from 1 to 6 (1=almost every day to 6=never) and a summary measure of everyday discrimination was created by summing across the nine items. Higher scores indicate more daily discrimination.
Neighborhood-level stressors
Information on neighborhoods was obtained as part of an ancillary study to MESA, the MESA Neighborhood study, designed to assess neighborhood conditions potentially relevant to CVD. A separate sample of 5,988 individuals (recruited between January and August 2004) residing in the same neighborhoods (census tracts) as MESA study participants were asked to rate their neighborhood via a telephone survey. Data from an independent sample was used to: 1) reduce the potential for same source bias, 2) increase the within neighborhood sample size, and 3) obtain a more valid measure of the features of interest by aggregating perceptions. We recruited a median of 8 individuals per neighborhood (range 1–62). Census tracts were used as proxies for neighborhoods in all analyses based on prior work indicating good agreement across individuals residing within the same tract in relation to neighborhood stressors [intraneighborhood agreement (ICC)=0.51; neighborhood reliability=0.82]. Additional details on the community survey and measurement properties of the neighborhood scales are provided elsewhere. (29)
Thirteen items (see appendix) were used to characterize neighborhood-level sources of chronic stress in these analyses based on face validity and previous research when possible. (20, 30) A summary neighborhood stressors scale constructed by summing responses for these items had good internal consistency (Cronbachs alpha=0.88) and test retest reliabilities (ICC=0.78). We also considered a measure of neighborhood walkability and availability of healthy foods based on prior associations between these measures and HTN. (24) All neighborhood measures were constructed using Empirical Bayes estimation techniques described elsewhere. (24)
Additional covariates
Additional variables obtained from study questionnaire included study site, age, gender, race/ethnicity, education, income, time lived in neighborhood, acculturation, physical activity, diet, and alcohol consumption. An overall acculturation score (ranging from 0=least acculturated to 5=most acculturated) was created by aggregating information on nativity, years lived in the U.S., and language spoken at home based on previous methods. (31) Physical activity was measured as total light, moderate, and vigorous activity in metabolic equivalent (MET)-minutes per week. Diet was measured using a summary score of dash diet accordance (ranging from 0–7) based on thresholds defined in DASH trials for eight nutrients (total fat, saturated fat, protein, cholesterol, fiber, potassium, magnesium, and calcium). (32). Higher scores indicate more physical activity and better dash diet accordance. Weight and height measurements were obtained during the MESA baseline examination and body mass index was calculated as weight (kg)/height (m)2.
Statistical Analysis
We first compared the distribution of sociodemographic characteristics and chronic stressors across racial/ethnic categories using chi-square tests. We then used logistic regression models to calculate the adjusted probability of hypertension across levels of individual and neighborhood-level chronic stressors, after adjusting for age and gender. We tested for a linear trend across ordered categories by including each stressor as an ordinal measure in regression models.
Binomial regression was used to estimate prevalence ratios of hypertension associated with individual and neighborhood-level stressors before and after adjustment for individual level covariates. Binomial regression was used because of the limitations of reporting odds ratios in cases of common outcomes. (33) We used a series of sequential models to investigate the contribution of chronic stressors to race/ethnic differences in hypertension. We estimated the prevalence ratios of hypertension by race/ethnicity controlling for site, age, and gender in Model 1. We then added individual-level chronic stressors (Model 2), neighborhood level stressors (Model 3), all stressors (Model 4), and all stressors plus individual and neighborhood-level confounders (individual-level SEP, acculturation, time lived in neighborhood, neighborhood walkability and availability of health foods) (Model 5). In Model 6 we also added traditional risk factors for hypertension including BMI, physical activity, diet, and alcohol consumption. These risk factors were added to the final models because they could partly mediate the effects of stressors on hypertension.
We tested two-way interactions between race/ethnicity and chronic stressors (neighborhood and individual-level) as well as between neighborhood stressors and sociodemographic factors (age, gender, site, individual SEP, acculturation, individual chronic stressors, and time lived in neighborhood). Following prior work, interactions were considered statistically significant if p<0.10.
Results
Table 1 shows the distribution of study site, age, gender, education, income, and hypertension overall and by race/ethnicity. The mean age was 62.3 (SD=9.9), 49.9% were hypertensive, and 41.3%, 43.3%, and 15.5% were white, African American, and Hispanic respectively. Only 8.4% of Hispanics were born in the US compared to over 90% of whites and African Americans, Among foreign born Hispanics (63.6%) the Caribbean Islands were the most common place of origin (67.8%, not shown in Table 1).
Table 1.
Selected characteristics of MESA participants at baseline (2000–2002) overall and by race/ethnicity
| Overall (n=2679) | White (n=1105) | African American (n=1159) | Hispanic (n=415) | p-value | |
|---|---|---|---|---|---|
| N | % | % | % | ||
| Study site | |||||
| Baltimore | 850 | 37.5 | 37.6 | 0.0 | <0.001 |
| New York | 913 | 16.8 | 27.1 | 99.6 | |
| North Carolina | 916 | 45.7 | 35.3 | 0.4 | |
| Age, years | 2679 | 63.3 (9.8) | 61.7 (9.8) | 61.3 (10.4) | <0.001 |
| Categorized Age, years | |||||
| 45–55 | 748 | 24.2 | 29.8 | 32.8 | <0.001 |
| 55–65 | 746 | 27.7 | 27.9 | 28.2 | |
| 65–75 | 834 | 33.9 | 31.1 | 23.9 | |
| 75+ | 351 | 14.2 | 11.3 | 15.2 | |
| Gender | |||||
| Male | 1236 | 48.7 | 43.8 | 45.8 | 0.067 |
| Female | 1443 | 51.3 | 56.2 | 54.2 | |
| Education | |||||
| <H.S diploma | 374 | 5.6 | 12.2 | 41.0 | <0.001 |
| H.S diploma | 551 | 19.7 | 20.7 | 22.6 | |
| Some college | 785 | 26.4 | 34.0 | 23.9 | |
| College graduate+ | 969 | 48.3 | 33.1 | 12.5 | |
| Income | |||||
| <$24,999 | 664 | 14.8 | 26.7 | 46.0 | <0.001 |
| $25,000–$49,999 | 805 | 27.9 | 30.1 | 35.7 | |
| $50,000–$74,999 | 517 | 21.5 | 19.5 | 12.8 | |
| >=$75,000 | 563 | 33.5 | 14.9 | 4.8 | |
| Unknown | 130 | 2.3 | 8.8 | 0.7 | |
| Acculturation † | 2551 | 4.9 (0.3) | 4.9 (0.4) | 2.4 (1.1) | <0.001 |
| Alcohol use | |||||
| Never | 469 | 65.9 | 45.9 | 48.4 | <0.001 |
| Former | 744 | 19.9 | 36.1 | 26.5 | |
| Current | 1453 | 14.3 | 18.0 | 25.1 | |
| Dash diet accordance † | 2332 | 1.5 (1.4) | 1.4 (1.3) | 1.8 (1.2) | <0.001 |
| Total physical activity, MET‡ minutes/week † | 2678 | 3.2 (3.6) | 4.9 (5.0) | 3.4 (3.7) | <0.001 |
| Body mass index | 2679 | 27.7 (5.0) | 30.4 (5.8) | 28.9 (5.0) | <0.001 |
| Hypertension | |||||
| Yes | 1336 | 42.0 | 59.3 | 43.9 | <.0001 |
| No | 1343 | 58.0 | 40.7 | 56.1 | |
| Time lived in neighborhood | |||||
| Yes | 1114 | 39.9 | 44.9 | 58.2 | <0.001 |
| No | 1373 | 60.1 | 55.1 | 41.9 | |
| Neighborhood walkability † | 3.8 (0.3) | 3.6 (0.3) | 3.7(0.3) | <0.001 | |
| Neighborhood availability of healthy foods † | 3.3 (0.4) | 3.1 (0.3) | 3.2 (0.3) | <0.001 | |
p-values correspond to chi-square tests for differences across race/ethnic group
Mean (standard deviation); MET=metabolic equivalent
All sociodemographic characteristics except gender were associated with race/ethnicity (p-value for all <0.001) (Table 1). Whites were slightly older and had higher levels of education and income than African Americans and Hispanics. African Americans had the highest prevalence of hypertension (59.3%) followed by Hispanics (43.6%) and whites (42.0%) (p<0.001). Hypertension prevalence for Hispanics only slightly differed by country of origin with those born in Central America and the Caribbean Islands having higher prevalence (48.6% and 47.8% respectively) than those born in the US and Puerto Rico (42.9% and 39.7% respectively) (not shown in Table 1). These differences were not statistically significant (p=0.490).
Table 2 shows the distribution of individual and neighborhood level stressors overall and by race/ethnicity. All stressors were strongly patterned by race/ethnicity (p<0.001). African Americans reported higher levels of perceived major and everyday discrimination than Hispanics or whites, and lived in neighborhoods with more chronic stressors than whites. Hispanics lived in neighborhoods with more chronic stressors than African Americans or whites, but reported levels of major and everyday discrimination similar to whites. Both African American and Hispanics were more likely to experience medium or high levels of atleast one individual and neighborhood-level stressor as compared to whites.
Table 2.
Individual and neighborhood stressors by race/ethnicity
| N=2679 | White (n=1105) | African American (n=1159) | Hispanic (n=415) | p-trend | |
|---|---|---|---|---|---|
| % | % | % | % | ||
| Chronic burden | |||||
| 0 | 46.0 | 42.2 | 48.1 | 50.1 | <0.001 |
| 1 | 29.2 | 33.8 | 25.5 | 27.2 | |
| 2+ | 24.8 | 24.0 | 26.4 | 22.7 | |
| Perceived major discrimination | |||||
| 0 | 54.4 | 64.4 | 41.7 | 62.9 | <0.001 |
| 1 | 24.3 | 22.4 | 27.3 | 20.7 | |
| 2+ | 21.3 | 13.1 | 31.0 | 16.4 | |
| Everyday discrimination | |||||
| Low | 29.5 | 33.5 | 21.1 | 42.4 | <0.001 |
| Medium | 33.1 | 35.9 | 30.7 | 32.1 | |
| High | 37.4 | 30.6 | 48.2 | 25.5 | |
| Neighborhood stressors | |||||
| Low | 33.4 | 52.7 | 26.9 | 1.0 | <0.001 |
| Medium | 33.5 | 35.3 | 36.9 | 19.3 | |
| High | 32.9 | 12.0 | 36.2 | 79.8 | |
| One individual/neighborhood-level stressors | |||||
| Yes | 50.9 | 35.3 | 61.1 | 64.1 | <0.001 |
| No | 49.1 | 64.7 | 38.9 | 35.9 | |
p-trends correspond to chi-square test for differences by race/ethnicity
Yes presents individuals who are individuals who reported medium or high levels of atleast one individual-level stressor and the neighborhood-level stressor.
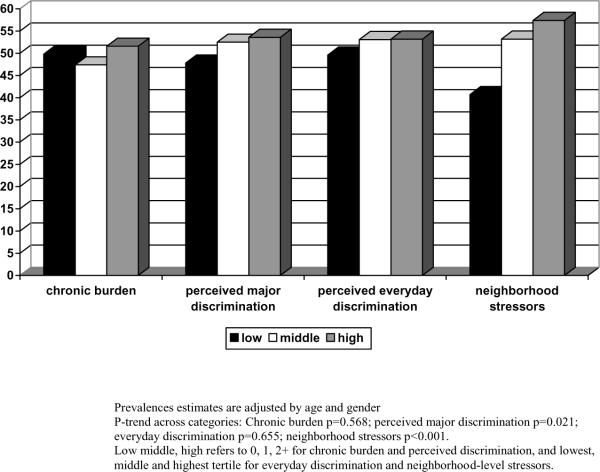
Figure 1 shows the adjusted prevalence of hypertension by categories of individual and neighborhood-level stressors. Higher levels of perceived major discrimination and neighborhood level stressors were positively associated with hypertension (p=0.021, <0.001, respectively), after adjusting for age and gender. No clear pattern was present for chronic burden and everyday discrimination.
Figure 1.
Age and gender adjusted percent hypertension by levels and sources of chronic stressors
Table 3 shows prevalence ratios of hypertension by categories of race/ethnicity and individual and neighborhood-level stressors before and after sequential adjustment for individual- level and neighborhood-level factors. Age and sex adjusted relative prevalences of hypertension (compared to whites) were 1.30 [95% CI: 1.22–1.38] for African Americans and 1.16 [95% CI: 1.04–1.31] for Hispanics as compared to whites (Model 1). The relative prevalence was only slightly reduced with the inclusion of individual-level stressors (Model 2) but significantly reduced with the inclusion of neighborhood-level stressors (Model 3). Specifically, when neighborhood stressors were included in the models (Model 3), the relative prevalence of hypertension (compared to whites) were reduced from 1.30 to 1.17 [95% CI: 1.11–1.22] for African Americans and from 1.16 to 1.09 [95% CI: 1.00–1.18] for Hispanics. Additional adjustment for income, education, acculturation, neighborhood walkability, availability of health foods, and time lived in neighborhood did not significantly modify these results (Model 5), nor did the inclusion of hypertension risk factors (Model 6). There were no statistically significant interactions between race/ethnicity, chronic stressors (individual and neighborhood), and sociodemographic factors (p>0.100 for all 14 interactions tested).
Table 3.
Relative prevalence of hypertension by race/ethnicity and sources of chronic stressors
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | Model 6 | |
|---|---|---|---|---|---|---|
| Race | ||||||
| White (referent) | -- | -- | -- | -- | -- | -- |
| Black | 1.30 [1.22–1.38] | 1.24 [1.17–1.30] | 1.17 [1.11–1.22] | 1.16 [1.11–1.21] | 1.17 [1.11–1.24] | 1.15 [1.08–1.23] |
| Hispanic | 1.16 [1.04–1.31] | 1.13 [1.02–1.24] | 1.09 [1.00–1.18] | 1.08 [1.00–1.17] | 1.10 [0.95–1.28] | 1.09 [0.93–1.28] |
| χ 2 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
| Chronic burden | ||||||
| 0 (referent) | -- | -- | -- | -- | ||
| 1 | 1.00 [0.95–1.05] | 1.00 [0.96–1.05] | 1.00 [0.95–1.06] | 1.00 [0.94–1.06] | ||
| 2 + | 1.02 [0.97–1.08] | 1.02 [0.97–1.07] | 1.03 [0.97–1.09] | 1.01 [0.95–1.08] | ||
| χ 2 | 0.698 | 0.735 | 0.555 | 0.958 | ||
| Major discrimination | ||||||
| 0 (referent) | -- | -- | -- | -- | ||
| 1 | 1.00 [0.95–1.06] | 1.00 [0.95–1.05] | 1.00 [0.95–1.06] | 1.02 [0.95–1.09] | ||
| 2+ | 1.01 [0.95–1.08] | 1.01 [0.96–1.07] | 1.01 [0.95–1.08] | 1.02 [0.96–1.08] | ||
| χ 2 | 0.923 | 0.945 | 0.950 | 0.823 | ||
| Everyday discrimination | ||||||
| Low (referent) | -- | -- | -- | -- | ||
| Medium | 1.02 [0.97–1.08] | 1.01 [0.96–1.06] | 1.02 [0.97–1.08] | 1.03 [0.96–1.10] | ||
| High | 0.95 [0.89–1.02] | 0.96 [0.91–1.02] | 0.96 [0.90–1.03] | 0.96 [0.90–1.04] | ||
| χ 2 | 0.076 | 0.167 | 0.189 | 0.168 | ||
| Neighborhood stressors | ||||||
| Low (referent) | -- | -- | -- | -- | ||
| Medium | 1.05 [1.00–1.10] | 1.04 [0.99–1.09] | 1.04 [0.98–1.11] | 1.04 [0.98–1.12] | ||
| High | 1.06 [0.99–1.13] | 1.05 [0.99–1.12] | 1.04 [0.95–1.13] | 1.02 [0.93–1.13] | ||
| χ 2 | 0.129 | 0.179 | 0.360 | 0.457 |
Model 1: study site, age, gender, race/ethnicity;
Model 2: Model 1+ individual-level stressors;
Model 3: Model 1 + neighborhood-level stressors;
Model 4: Model 1+individual+neighborhood stressors;
Model 5: Model 4 + education, income, acculturation, neighborhood walkability, availability of healthy foods, time lived in neighborhood
Model 6: Model 5 + body mass index, alcohol consumption, physical activity, diet
Neighborhood walkability and availability of healthy foods were included as continuous variables
Discussion
The overall goal of our study was to investigate individual-level and neighborhood-level chronic stressors as potential mechanisms contributing to race/ethnic differences in blood pressure. Racial/ethnic disparities in hypertension prevalence have been previously reported in the MESA cohort with African Americans having a higher prevalence of hypertension than whites or Hispanics in the full MESA sample.(34) However, in this subsample restricted to three of the MESA sites (including NY were Hispanics were predominately Caribbean-origin) we also found that the prevalence of hypertension was higher in Hispanics as compared to whites. This is contrary to nationally representative data sources such as the National Health and Nutrition Examination Survey, (35, 36) that include Hispanics of predominately Mexican origin.
We found that African Americans reported more perceived major and everyday discrimination than whites and Hispanics. In addition, African Americans and Hispanics lived in more stressful neighborhoods than whites and higher levels of neighborhood stressors in turn were associated with a higher prevalence of hypertension, independent of site, age, and gender. We also documented a substantial reduction in the association between race/ethnicity and hypertension after adjustment for neighborhood-level stressors.
This study is novel in extending the study of psychosocial stressors and hypertension to the neighborhood level. This is one of the first studies to measure associations between neighborhood stressors and blood pressure by moving beyond census derived indicators of neighborhood socioeconomic position to the direct measurement of neighborhood conditions. We previously examined a range of physical (walkability, availability of healthy foods) and social features (safety, social cohesion), of neighborhood environments in relation to hypertension and documented associations between these features and HTN, independent of some individual-level factors (age, gender, education, income). In current analyses we found that neighborhood stressors were also associated with hypertension, although possibly due to the strong patterning of neighborhood characteristics by race/ethnicity, these associations were not statistically significant after adjusting for race/ethnicity. However, our trend of positive associations between neighborhood stressors and the prevalence of hypertension, is consistent with prior work showing significantly higher systolic and diastolic blood pressure for black men and women living in high stress areas (as characterized by census measures) compared to black men and women in low stress areas, after adjustment for a series of individual-level variables (such as age and socioeconomic position). (23)
Our study is also one of few that attempt to examine the contribution of stressors to race/ethnic disparities in hypertension and related outcomes (16–18). The fact that race/ethnic differences in hypertension were reduced after adjusting for neighborhood stressors is compatible with (although it does not categorically demonstrate) a causal role of neighborhood stressors in creating the observed disparities in hypertension prevalence. (37) The proportion of race/ethnic differences in hypertension prevalence that is statistically explained by neighborhood stressors may differ from sample to sample depending on the degree of residential segregation and the strength of associations between neighborhood characteristics and hypertension; hence we do not draw inferences regarding the percent of the difference “explained”. In addition, because of the potential for many unobserved social and biologic differences between race/ethnic groups which are not accounted for by the variables we included, we make no attempt to interpret the determinants of the race/ethnic difference that persists after adjustment.(38)
Although, we provide a more complete assessment of chronic stressors operating at different levels than prior work, we have not considered the full spectrum of stressors that individuals are exposed to throughout the lifecourse. For example, we did not examine job stressors (which have been linked to hypertension (13) because of the large representation of retirees (34%) in this sample. Additionally, the stressors we did include are subject to measurement error. Defensiveness or denial may cause an under-reporting of discriminatory acts whereas anger and hostility may lead to over-reporting. (39, 40) Our measure of neighborhood stressors was based on prior work, however we did not have all items that comprised previously validated scales of neighborhood disorder. (20) Despite this exclusion, we found that our measure had good internal consistency and test-retest reliability. Limitations of our measures of stress (in both type and measurement) may have contributed to our inability to detect an association between stressors and hypertension in adjusted models.
As an additional concern, neighborhood chronic stressors may cluster with other features of neighborhood infrastructure. This creates difficulty in teasing out whether it is the stressors or the physical features of neighborhoods associated with them, which contribute to hypertension. In our data, the neighborhood stressors scale was moderately correlated with neighborhood measures of walkability (r=−0.45) and availability of healthy foods (r=−0.33). Additional adjustment for these factors did not further reduce race/ethnic differences although this may be because the neighborhood stressor scale was already capturing these other neighborhood attributes.
Other limitations include limited overlap in the neighborhood stressors by race/ethnicity. For example, 79.8% of Hispanics lived in neighborhoods with the highest tertile of neighborhood stressors as compared to only 12.0% of whites. Regression results are therefore based on extrapolations to areas of sparse data, but we believe these extrapolations are reasonable. Another limitation is the inability to fully capture the accumulation of chronic stressors (at the neighborhood level) to impact a chronic condition like HTN that develops over the lifecourse. In our sample, 44.1% of respondents have resided in the current neighborhood for 20 or more years. We did not find any statistically significant interactions between time lived in neighborhood and neighborhood stressors in relation to hypertension prevalence. The absence of effect modification by time lived in neighborhood could have resulted from individuals being exposed to similar conditions in previous neighborhoods. However, we had limited statistical power to detect significant interactions.
In summary, in this ethnically diverse sample we found that cross-sectional associations between race/ethnicity and hypertension were reduced after accounting for chronic stressors at the neighborhood level. Although these results need to be confirmed in longitudinal and lifecourse designs, they suggest that multilevel sources of stress may contribute to race/ethnic disparities in hypertension. Future work also needs to examine the behavioral and biologic mechanisms though which stressors may be related to hypertension. Our findings suggest that efforts to reduce race/ethnic disparities in high blood pressure may benefit from consideration of possible stress inducing features of neighborhoods.
Acknowledgments
The authors thank the Robert Wood Johnson Foundation Health & Society Scholars program for its financial support. The authors also thank other investigators, the staff, and the participants of the Multi-Ethnic Study of Atherosclerosis (MESA) for their valuable contributions.
This research was supported by the Michigan Center for Integrative Approaches to Health Disparities P60 MD002249 (Diez Roux PI). MESA is supported by contracts N01-HC-95159 through N01-HC-95165, N01-HC-95169 and R01 HL071759 from the National Heart, Lung, and Blood Institute., The authors thank the other investigators, the staff, and the participants of the MESA study for their valuable contributions. A full list of participating MESA investigators and institutions can be found at http://www.mesa-nhlbi.org.
Footnotes
Disclosures: None
References
- 1.Flack JM, Ferdinand KC, Nasser SA. Epidemiology of hypertension and cardiovascular disease in African Americans. J Clin Hypertens (Greenwich) 2003 Jan-Feb;5(1 Suppl 1):5–11. doi: 10.1111/j.1524-6175.2003.02152.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gillum RF. The epidemiology of cardiovascular disease in black Americans. N Engl J Med. 1996 Nov 21;335(21):1597–9. doi: 10.1056/NEJM199611213352110. [DOI] [PubMed] [Google Scholar]
- 3.Isezuo SA. Systemic hypertension in blacks: an overview of current concepts of pathogenesis and management. Niger Postgrad Med J. 2003 Sep;10(3):144–53. [PubMed] [Google Scholar]
- 4.Kaufman JS, Hall SA. The slavery hypertension hypothesis: dissemination and appeal of a modern race theory. Epidemiology. 2003 Jan;14(1):111–8. doi: 10.1097/00001648-200301000-00027. [DOI] [PubMed] [Google Scholar]
- 5.Sowers JR, Ferdinand KC, Bakris GL, Douglas JG. Hypertension-related disease in African Americans. Factors underlying disparities in illness and its outcome. Postgrad Med. 2002 Oct;112(4):24–6. 9–30, 3–4. doi: 10.3810/pgm.2002.10.1331. passim. [DOI] [PubMed] [Google Scholar]
- 6.Colhoun HM, Hemingway H, Poulter NR. Socio-economic status and blood pressure: an overview analysis. J Hum Hypertens. 1998 Feb;12(2):91–110. doi: 10.1038/sj.jhh.1000558. [DOI] [PubMed] [Google Scholar]
- 7.Bassett DR, Jr., Fitzhugh EC, Crespo CJ, King GA, McLaughlin JE. Physical activity and ethnic differences in hypertension prevalence in the United States. Prev Med. 2002 Feb;34(2):179–86. doi: 10.1006/pmed.2001.0969. [DOI] [PubMed] [Google Scholar]
- 8.Dyer AR, Liu K, Walsh M, Kiefe C, Jacobs DR, Jr., Bild DE. Ten-year incidence of elevated blood pressure and its predictors: the CARDIA study. Coronary Artery Risk Development in (Young) Adults. J Hum Hypertens. 1999 Jan;13(1):13–21. doi: 10.1038/sj.jhh.1000740. [DOI] [PubMed] [Google Scholar]
- 9.Liu K, Ballew C, Jacobs DR, Jr., Sidney S, Savage PJ, Dyer A, et al. Ethnic differences in blood pressure, pulse rate, and related characteristics in young adults. The CARDIA study. Hypertension. 1989 Aug;14(2):218–26. doi: 10.1161/01.hyp.14.2.218. [DOI] [PubMed] [Google Scholar]
- 10.Dressler WW, Oths KS, Gravlee CC. RACE AND ETHNICITY IN PUBLIC HEALTH RESEARCH: Models to Explain Health Disparities. Annual Review of Anthropology. 2005;34(1):231–52. [Google Scholar]
- 11.Schnittker J, McLeod JD. THE SOCIAL PSYCHOLOGY OF HEALTH DISPARITIES. Annual Review of Sociology. 2005;31(1):75–103. [Google Scholar]
- 12.Williams DR, Collins C. Racial residential segregation: a fundamental cause of racial disparities in health. Public Health Rep. 2001 Sep-Oct;116(5):404–16. doi: 10.1093/phr/116.5.404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Markovitz JH, Matthews KA, Whooley M, Lewis CE, Greenlund KJ. Increases in job strain are associated with incident hypertension in the CARDIA Study. Ann Behav Med. 2004 Aug;28(1):4–9. doi: 10.1207/s15324796abm2801_2. [DOI] [PubMed] [Google Scholar]
- 14.Kaplan MS, Nunes A. The psychosocial determinants of hypertension. Nutr Metab Cardiovasc Dis. 2003 Feb;13(1):52–9. doi: 10.1016/s0939-4753(03)80168-0. [DOI] [PubMed] [Google Scholar]
- 15.Brondolo E, Rieppi R, Kelly KP, Gerin W. Perceived racism and blood pressure: a review of the literature and conceptual and methodological critique. Ann Behav Med. 2003 Winter;25(1):55–65. doi: 10.1207/S15324796ABM2501_08. [DOI] [PubMed] [Google Scholar]
- 16.Krieger N, Sidney S. Racial discrimination and blood pressure: the CARDIA Study of young black and white adults. Am J Public Health. 1996 Oct;86(10):1370–8. doi: 10.2105/ajph.86.10.1370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bell CN, Thorpe RJ, Jr., Laveist TA. Race/Ethnicity and hypertension: the role of social support. Am J Hypertens. May;23(5):534–40. doi: 10.1038/ajh.2010.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Spruill TM, Gerin W, Ogedegbe G, Burg M, Schwartz JE, Pickering TG. Socioeconomic and psychosocial factors mediate race differences in nocturnal blood pressure dipping. Am J Hypertens. 2009 Jun;22(6):637–42. doi: 10.1038/ajh.2009.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wheaton B. In: The nature of stressors. Horwitz AV, Scheid TL, editors. Cambridge University Press; New York: 1999. [Google Scholar]
- 20.Ross CE, Mirowsky J. Neighborhood disadvantage, disorder, and health. J Health Soc Behav. 2001 Sep;42(3):258–76. [PubMed] [Google Scholar]
- 21.Elliott M. The stress process in neighborhood context. Health Place. 2000 Dec;6(4):287–99. doi: 10.1016/s1353-8292(00)00010-1. [DOI] [PubMed] [Google Scholar]
- 22.James SA, Kleinbaum DG. Socioecologic stress and hypertension related mortality rates in North Carolina. Am J Public Health. 1976 Apr;66(4):354–8. doi: 10.2105/ajph.66.4.354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Harburg E, Erfurt JC, Chape C, Hauenstein LS, Schull WJ, Schork MA. Socioecological stressor areas and black-white blood pressure: Detroit. J Chronic Dis. 1973 Sep;26(9):595–611. doi: 10.1016/0021-9681(73)90064-7. [DOI] [PubMed] [Google Scholar]
- 24.Mujahid MS, Diez Roux AV, Morenoff JD, Raghunathan TE, Cooper RS, Ni H, et al. Neighborhood characteristics and hypertension. Epidemiology. 2008 Jul;19(4):590–8. doi: 10.1097/EDE.0b013e3181772cb2. [DOI] [PubMed] [Google Scholar]
- 25.Bild DE, Bluemke DA, Burke GL, Detrano R, Diez Roux AV, Folsom AR, et al. Multi-ethnic study of atherosclerosis: objectives and design. Am J Epidemiol. 2002 Nov 1;156(9):871–81. doi: 10.1093/aje/kwf113. [DOI] [PubMed] [Google Scholar]
- 26.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr., et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. Jama. 2003 May 21;289(19):2560–72. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 27.Pilkonis PA, Imber SD, Rubinsky P. Dimensions of life stress in psychiatric patients. J Human Stress. 1985 Spring;11(1):5–10. doi: 10.1080/0097840X.1985.9936732. [DOI] [PubMed] [Google Scholar]
- 28.Williams DR, Yan Y, Jackson JS, Anderson NB. Racial Differences in Physical and Mental Health: Socio-economic Status, Stress and Discrimination. J Health Psychol. 1997 July 1;2(3):335–51. doi: 10.1177/135910539700200305. 1997. [DOI] [PubMed] [Google Scholar]
- 29.Mujahid MS, Diez Roux AV, Morenoff JD, Raghunathan T. Assessing the Measurement Properties of Neighborhood Scales: From Psychometrics to Ecometrics. Am J Epidemiol. 2007 Feb 28; doi: 10.1093/aje/kwm040. [DOI] [PubMed] [Google Scholar]
- 30.Steptoe A, Feldman PJ. Neighborhood Problems as Sources of Chronic Stress: Development of a Measure of Neighborhood Problems, and Associations With Socioeconomic Status and Health. Annals of Behavioral Medicine. 2001;23(3):177–85. doi: 10.1207/S15324796ABM2303_5. [DOI] [PubMed] [Google Scholar]
- 31.Kandula NR, Diez-Roux AV, Chan C, Daviglus ML, Jackson SA, Ni H, et al. Association of acculturation levels and prevalence of diabetes in the multi-ethnic study of atherosclerosis (MESA) Diabetes Care. 2008 Aug;31(8):1621–8. doi: 10.2337/dc07-2182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gao SK, Fitzpatrick AL, Psaty B, Jiang R, Post W, Cutler J, et al. Suboptimal nutritional intake for hypertension control in 4 ethnic groups. Arch Intern Med. 2009 Apr 13;169(7):702–7. doi: 10.1001/archinternmed.2009.17. [DOI] [PubMed] [Google Scholar]
- 33.Spiegelman D, Hertzmark E. Easy SAS Calculations for Risk or Prevalence Ratios and Differences. Am J Epidemiol. 2005 August 1;162(3):199–200. doi: 10.1093/aje/kwi188. 2005. [DOI] [PubMed] [Google Scholar]
- 34.Kramer H, Han C, Post W, Goff D, Diez-Roux A, Cooper R, et al. Racial/ethnic differences in hypertension and hypertension treatment and control in the multi-ethnic study of atherosclerosis (MESA) Am J Hypertens. 2004 Oct;17(10):963–70. doi: 10.1016/j.amjhyper.2004.06.001. [DOI] [PubMed] [Google Scholar]
- 35.Hertz RP, Unger AN, Cornell JA, Saunders E. Racial Disparities in Hypertension Prevalence, Awareness, and Management. Arch Intern Med. 2005 October 10;165(18):2098–104. doi: 10.1001/archinte.165.18.2098. 2005. [DOI] [PubMed] [Google Scholar]
- 36.Hajjar I, Kotchen TA. Trends in Prevalence, Awareness, Treatment, and Control of Hypertension in the United States, 1988–2000. JAMA. 2003 July 9;290(2):199–206. doi: 10.1001/jama.290.2.199. 2003. [DOI] [PubMed] [Google Scholar]
- 37.Cole SR, Hernan MA. Fallibility in estimating direct effects. Int J Epidemiol. 2002 Feb;31(1):163–5. doi: 10.1093/ije/31.1.163. [DOI] [PubMed] [Google Scholar]
- 38.Kaufman JS, Cooper RS. Commentary: considerations for use of racial/ethnic classification in etiologic research. Am J Epidemiol. 2001 Aug 15;154(4):291–8. doi: 10.1093/aje/154.4.291. [DOI] [PubMed] [Google Scholar]
- 39.Nyklicek I, Vingerhoets AJ, Van Heck GL, Van Limpt MC. Defensive coping in relation to casual blood pressure and self-reported daily hassles and life events. J Behav Med. 1998 Apr;21(2):145–61. doi: 10.1023/a:1018775807593. [DOI] [PubMed] [Google Scholar]
- 40.Watson D, Pennebaker JW. Health complaints, stress, and distress: exploring the central role of negative affectivity. Psychol Rev. 1989 Apr;96(2):234–54. doi: 10.1037/0033-295x.96.2.234. [DOI] [PubMed] [Google Scholar]