Abstract
Primary objective
Given the major impact of traumatic brain injury (TBI) on society and the fact that effective therapies for common deficits in balance and gait are not known, the purpose of this review was to investigate the efficacy or effectiveness of non-aerobic exercise interventions to improve balance and gait in functionally mild to moderate individuals with TBI (those who demonstrate the ability or capacity to ambulate) and to provide evidence-based guidelines for clinical practice.
Methods
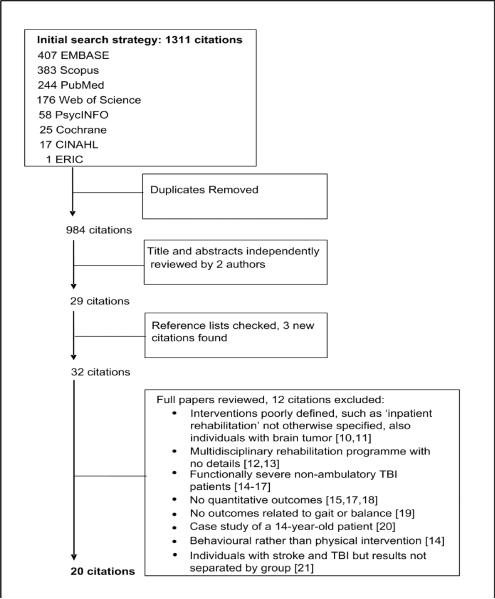
We searched eight databases (limits: January 1980 to December 2009) for papers including exercise interventions to improve gait and balance post TBI. Out of 984 unique citations, 20 fully met inclusion criteria. The methodological quality of studies was determined by the Physiotherapy Evidence Database (PEDro) scale and strength by Sackett's Levels of Evidence.
Results
We found limited evidence of the positive effects of balance, gait, or the combination of both interventions, in TBI rehabilitation. Most studies included small sample sizes with heterogeneous groups, and the interventions were variable and lacked standardization. The outcome measures were variable and low in quality. These limitations make it difficult to draw useful evidence-based recommendations for clinical practice.
Conclusions
The state of evidence for gait and balance interventions in patients with mild to moderate TBI is surprisingly poor. Greater consideration and conformity in the choice of outcome measures and attention in the design and standardization treatment approaches are essential in future research to advance practice.
Introduction
Traumatic brain injury (TBI), by definition, is any damage to the brain occurring after birth and unrelated to congenital disorders, developmental disabilities, or progressive processes [1]. TBI has become an important public health concern because it is one of the leading causes of death and long-term disability [1–3]. . The devastating personal consequences of TBI often include long-term disability in the areas of physical, cognitive, behavioural, or emotional functioning, possibly even from a TBI classified as `mild' [3, 4]. While impairments from TBI are broad, nearly 30% of patients report impaired balance [4], as well as limitations in motor function including gait problems [5]. Addressing gait and balance problems presents a significant challenge to the rehabilitation and recovery of patients with TBI because it is generally not known what therapies are effective. There is great variability in therapeutic methods used for treatment, although they often similarly involve a comprehensive interdisciplinary team, and the employment of techniques often differs by therapist or particular institution [6, 7].
Unfortunately, the state of research in gait and balance rehabilitation for patients with TBI lags behind that for patients with other neurologic impairments such as stroke and cerebral palsy [8]. To date, a few systematic reviews have been done to evaluate the effects of these treatments [1, 5–7], but all concluded that only limited conclusions could be drawn due to the low number and poor methodological quality of the available studies. Only two of these reviews focused on efficacy of specific interventions [1, 5]. The other two were more general, addressing whether the timing, intensity, or category of rehabilitation affected patient outcomes [6, 7], and suggested that rehabilitation in a general sense is beneficial for patients. In addition, those reviews included patients in the moderate to severe TBI category who do not show potential after rehabilitation to ambulate independently. None of the reviews so far have focused specifically on those in the mild to moderate category who are able to ambulate or are potentially ambulatory. In addition, most reviews evaluate various forms of motor intervention, whereas the intent of this review was to focus specifically on balance and gait interventions.
Thus, the purpose of our review is two-fold. First, we attempt to investigate the efficacy or effectiveness of non-aerobic exercise interventions to improve balance and gait in patients with TBI who possessed the ability or were assumed to have the potential to ambulate independently. Second, based on our findings, we aim to provide evidence-based guidelines for clinical practice.
Methods
Inclusion and Exclusion Criteria
The goal of the literature review was to evaluate the outcomes of all studies on physical therapy interventions aimed at improving gait and balance in ambulatory or potentially ambulatory adults with TBI. Studies on individuals with a variety of causes of TBI, such as motor vehicle accidents, sports-related concussions, or operation for a brain tumor, among others, were included. Some studies dealing with other populations (e.g. stroke) were only included if they also included individuals with TBI and reported outcome data on these individuals separately. Studies involving general kinesioterapy techniques, such as stretching and strength training, as well as studies involving aerobic exercise, were only included if they also involved specific gait or balance training programmes done in conjunction with these other interventions. Only studies reporting outcome measures related to gait or balance assessments were included. Because of differences in brain development and recovery at different ages, the population of interest for this review was adults, 18 years of age or older [9]. Studies that enrolled children were only included if they also enrolled adults and if the adults comprised the majority of the study sample. Furthermore if the brain injury occurred in childhood but the patient was evaluated for rehabilitation as an adult, the study was included. Time past injury was not a criteria for inclusion or exclusion in this review, so studies on both acute and chronic TBI were included.
Studies were excluded from this review if they met any of the following criteria: 1) investigation of exercise interventions aimed purely at increasing cardio-respiratory fitness or decreasing fatigue, 2) primary focus on functionally severe TBI, defined as those lacking either the ability to ambulate or a reasonable expectation that therapy could result in ambulation, 3) analysis of upper motor function only, or 4) use of purely subjective information as outcomes.
Search Strategy
A comprehensive systematic literature search was performed on the following databases: PubMed, EMBASE, CINAHL Plus (Cumulative Index to Nursing and Allied Health Literature), all databases within the Cochrane Library, Web of Science, Scopus, ERIC (Education Resources Information Center), and PsycINFO.
All records were limited to Humans, Adults (18 or 19+ depending on the database option), in English, and records added from January 1, 1980 to December 7, 2009, the date of search strategy finalization. The general search strategy, allowing for syntax differentiations between engines, for all databases was as follows:
gait
walking
balance
`postural stability'
vertigo
mobility
#1 OR #2 OR #3 OR #4 OR #5 OR #6
concussion
`head injury'
`traumatic brain injury'
#8 OR #9 OR #10
training
therapy
exercise
#12 OR #13 OR #14
#7 AND #11 AND #15
Figure 1 shows our search results. Our search generated a final list of 20 citations that fully met the inclusion criteria. Finally, Sackett's Levels of Evidence from I to V [22] (table 1) were used to determine the strength of the study in terms of the type of design used, and the PEDro (Physiotherapy Evidence Database) scale [23] (http://www.pedro.fhs.usyd.edu.au/scale_item.html#scale_1) was used to rate the scientific quality or rigor of these 20 studies. With the PEDro scale, quality of a study may be assessed by assigning a point for each positive criterion that is met with the exception of the first, specification of eligibility criteria, which does not count toward the total (see table 4 for a list of scores by criteria). For purposes of making conclusions, the findings of the review were summarized into the categories of strong, moderate, or limited evidence in accordance with the methods of previous systematic reviews on TBI [1, 5, 6]. Strong evidence is supported by the results of at least two fair quality (PEDro score of four or higher) RCTs. On the other hand, findings that are supported by a single, fair quality RCT represent only moderate evidence, and limited evidence consists of findings supported by at least one prospective cohort study (controlled or non-controlled) or case study. In addition, we have categorized outcome measures from each into the sub-categories of Body Structures and Functions or Activity and Participation as per the World Health Organization's International Classification of Functioning [24].
Figure 1.
Table 1.
Description of study design, participants, outcome measures, and results by study
| First Author, Year | Design | Sample size,Gender, Age mean (SD) | Diagnosis, Mobility level | Last injury mean (SD) | Assessment schedule, Outcome measures | Results |
|---|---|---|---|---|---|---|
| Blake, 2009 [26] | Small RCT |
Tai Chi: n=10 9M, 1F 44.5 (10.5) y Ctrl: n=10 6M.4F 46.2 (11.3) y |
TBI, not specified |
Tai Chi: 16 (9) y Ctrl: 14 (13) y |
0, 8 wks; training wks 1–8 | |
| PSDQ coordination | ↑ ctrl > Tai Chi, NS | |||||
| PSDQ flexibility | ↑ ctrl, ↓ Tai Chi, NS | |||||
| PSDQ physical activity | ↑ Tai Chi > ctrl, NS | |||||
| Bogataj, 1989 [27] | Case Study | n=1 1M 45 y |
Severe TBI, hemiplegia, ambulatory with moderate assistance from PT | Not specified | 0, 12 days + each FES; training days 1–12 | |
| Number of steps | ↑ 136 to 500 over daily FES sessions | |||||
| Mean stride time | ↑ 3.36 to 2.09 s over daily FES | |||||
| ↑ 5.24 to 3.58 s without FES | ||||||
| ↑ 5.24 to 2.3 s w/o FES pre vs. with FES post | ||||||
| Mean heel-on time | ↑ 40% over daily FES sessions | |||||
| Gait symmetry | ↑ 0.71 to 1.46 over daily FES sessions | |||||
| Mean velocity | ↑ 0.12 to 0.41 m/s over daily FES | |||||
| ↑ 0.08 to 0.15 m/s w/o FES | ||||||
| Mean stride length | ↑ 0.41 to 0.86 m over daily FES | |||||
| ↑ 0.43 to 0.57 m w/o FES | ||||||
| Stance time (impaired leg) | ↑ 45% to 65% of stride time w/o FES | |||||
| Load (on impaired leg) | ↑ 25% (w/o therapist assist) w/o FES | |||||
| Loading point | ↑ 80 to 70 mm from distal toes w/o FES | |||||
| Brown, 2005 [28] | Small RCT |
BWSTT: n=10 7M, 3F 38(11.8) y OGT: n=9 6M, 3F 42.6 (8.1) y |
Chronic TBI BWSTT: 9 wheelchair, 1 independent ambulator OGT: 5 wheelchair, 4 independent ambulators |
BWSTT: 15.1 (6.5) y OGT: 16.6 (4.9) y |
0, 3 mths (or within 2 wks); training mths 1–3 | |
| Gait velocity | BWSTT: ↑ post vs. pre, NS | |||||
| OGT: ↓ post vs. pre, NS | ||||||
| ↑ OGT > BWSTT, NS | ||||||
| Stride width | BWSTT: ↑ post vs. pre | |||||
| OGT: ↑ post vs. pre | ||||||
| ↑ OGT > BWSTT, NS | ||||||
| Step length asymmetry | BWSTT: ↓ post vs. pre, NS | |||||
| OGT: ↑ post vs. pre | ||||||
| ↑ OGT >BWSTT | ||||||
| FAC | BWSTT: no change, NS | |||||
| OGT: no change, NS | ||||||
| OGT = BWSTT, NS | ||||||
| Timed Up and Go | BWSTT: ↑ post vs. pre, NS | |||||
| OGT: ↑ post vs. pre, NS | ||||||
| ↑ OGT > BWSTT, NS | ||||||
| FRT | BWSTT: ↑ post vs. pre, NS | |||||
| OGT: ↑ post vs. pre, NS | ||||||
| ↑ BWSTT > OGT, NS | ||||||
| Dault, 2002 [29] | Prospective Cohort |
SST: n=5 3M, 2F 31.8 (13.8) y WT: n=3 3M 26 (5.6) y |
Mild to severe TBI, all independent ambulators |
SST: 62 (50.1) mths WT:15 (9.2) mths |
0, 12 wks; training wks 1–12 | |
| CTSIB | SST: ↑ post vs. pre | |||||
| WT: no change, NS | ||||||
| Degano, 2009 [30] | Case study | n=1 1 F 36 y |
TBI, severe with R hemiparesis (ambulation assistance not specified) | 5 mths | 0,1 mth; training 1 mth | |
| BBS | ↑ post vs. pre (17 vs. 21) | |||||
| LOS (reaction time) | ↑ post vs. pre | |||||
| SOT (equilibrium score) | ↑ post vs. pre | |||||
| ICARS (ataxia) | ↑ post vs. pre (41 vs. 21) | |||||
| OGA | ↑ post vs. pre | |||||
| Franckeviciute, 2008 [31] | Prospective Cohort | n=131 99M, 32F 18–44 y(n=83) 45–59 y (n=29) 60–74y(n=19) |
TBI, 28 moderate and 103 severe, mobility level not specified | Not specified | 0 and 2 mths | |
| COVS | ↑ group 18–44 > other age groups | |||||
| Gurr, 2001 [32] | Prospective Cohort | n=18 11M, 7F 46.9 y |
Mild to moderate TBI (dizziness and balance problems), excluded if hemiplegia | > 18y | 0,4,10,14 wks; training wks 4–10 | |
| Postural sway | pre vs. baseline, NS; ↑ post vs. pre | |||||
| Five point vertigo scale | pre vs. baseline, not analyzed; ↑ post vs. pre, ↑ follow-up vs. post | |||||
| VSS | pre vs. baseline, NS; ↑ post vs. pre | |||||
| VCQ | pre vs. baseline, NS; post vs. pre, NS | |||||
| VHQ | pre vs. baseline, NS; ↑ post vs. pre | |||||
| Herdman, 1990 [33] | Case study | n=1 1M 53 y |
TBI with dizziness, ambulation with cane | 2y | 0, 6 mths; exercises mths 1–6 | |
| SOT | ↑ post vs. pre (fell on fewer conditions; equilibrium scores of non-falls approached normal limits) | |||||
| Hurt, 1998 [34] | Prospective Cohort | n=5 3M, 2F 25.2 (5.4) y |
Moderate to severe TBI with persisting gait disorder, independent ambulation | 14.4 (6) mths | 0, 5 wks; training wks 1–5 | |
| Velocity | Normal pace: ↑ post vs. pre | |||||
| Fast: ↑ post vs. pre, NS | ||||||
| Cadence | Normal pace: ↑ post vs. pre | |||||
| Fast: ↑ post vs. pre, NS | ||||||
| Stride length | Normal pace: ↑ post vs. pre | |||||
| Fast: ↑ post vs. pre, NS | ||||||
| Symmetry | Normal pace: ↑ post vs. pre, NS | |||||
| Fast: ↑ post vs. pre, NS | ||||||
| Schalow, 2002 [10] | Prospective Cohort | n=6 (including kids) gender not specified 30 (range 13–47) y | Chronic TBI | Range 2–7 y | 0, 3 mths; training mths 1–3 | no statistics or numbers, information extrapolated from graphs |
| Walking time (fixed distance) | ↑ post vs. pre | |||||
| Number of jumps on springboard | ↑ post vs. pre | |||||
| Coordination dynamics | ↑ post vs. pre | |||||
| Scherer, 2007 [35] | Case Study | n=1 1M 36 y |
TBI, severe with L hemiparesis, initially required assistance from 2 therapists to walk | 9 wks | 0, 2, 3 wks; 9 sessions | |
| 6-minute walk test | ↑ 275%, wk1–wk2 | |||||
| maximum ambulated distance | ↑ 300%, wk1–wk3 | |||||
| Seif-Naraghi, 1999 [11] | Case study | n=2 2M 14 and 30 y |
TBI, both patients initially required maximum assistance to walk | Pt1 = 2 y Pt 2 = 4 mths |
0, 3–4 mths; training 3–4 mths | |
| Treatment progression | Pt1 ↑ (went from walking at 30% BWS at 0.7 mph for 10 min to 1.4 for 40 min) Pt2 ↑ (went from walking at 40% BWS at 0.2 mph for 10 min to 30% BWS at 0.5 mph for 40 min) |
|||||
| Subjective evaluation of ambulation ability | Pt1 ↑ (acquired independent ambulation with cane) Pt2 ↑ (acquired independent ambulation with front wheel walker) |
|||||
| Shepard, 1993 [36] | Prospective Cohort | n=152 balance disorders (26 TBI) 63M, 89F range 20–89 y |
Balance disorders including TBI, mobility not specified | Total group > 5 y | 0, 2–10 wks; training 2–10 wks | |
| Symptoms scores | ↑ in 62% patients | |||||
| DRS | ↑ in 53% patients | |||||
| Sveistrup, 2003 [37] | Small RCT | n=14 not specified |
TBI, mobility not specified | 6 mths | 0, 6 wks; training 6 wks | Note: results extrapolated from graphs; no numbers or statistics given |
| CB&MS | VR group: ↑ 19.5 points Control 1: ↑ 1 .4 points Control 2: ↑ 6 points |
|||||
| Thornton, 2005 [38] | Prospective Cohort |
VR: n=15 9M, 6F 42 y GBT: n=12 10M, 2F 37 y |
Moderate to severe, chronic TBI Able to stand for 2 min without aid VR: canes (4),walkers (2) GBT: cane (2), wheelchair + cane (2) |
> 6 mths | 0, 6 wks, 3 mths; training wks 1–6 | |
| ABC | ↑ post vs. pre, continued ↑ at follow-up, NS, in both groups | |||||
| LEFS | ↑ post vs. pre, continued ↑ at follow-up, NS, in both groups | |||||
| Vaz, 2008 [39] | Case Study | n=2 Pt1:M, 53 y Pt2:M, 25 y |
TBI with chronic ataxia, ability to walk >10m independently | Pt1: 5y | 0, 3, 7,10 wks; training wks 4–7 | |
| Gait speed | Pt1: ↑ post vs. pre, NS; ↓ at follow-up, NS Pt2: ↑ post vs. pre, NS; further ↑ at follow-up |
|||||
| Cadence | Pt1: ↑ post vs. pre; ↓ at follow-up, NS Pt2: ↑ post vs. pre, NS; further ↑ at follow-up |
|||||
| Step length | Pt1: ↑ post vs. pre; further ↑ at follow-up, NS Pt2: ↑ post vs. pre, NS; further ↑ at follow-up, NS |
|||||
| Timed Up and Go | Pt1: ↑ post vs. pre; further ↑ at follow-up, NS Pt2: ↑ post vs. pre; further ↑ at follow-up, NS |
|||||
| RVGA | Pt1: NS post vs. pre and at follow-up Pt2: NS post vs. pre; ↑ at follow-up |
|||||
| Alternate step touch | Pt1: ↑ post vs. pre but < than baseline; further ↑ at follow-up, NS Pt2: ↑ post vs. pre, NS; further ↑ at follow-up |
|||||
| Wade, 1997 [40] | Prospective Cohort | n=13 9M,4F 25 (8) y |
TBI, severe, able to stand independently for at least 10 sec | 47 (28) days | 0 and 6 weeks; training 6 wks | |
| Postural sway | ↑ post vs. pre | |||||
| Gait vel. and stride length | ↑ post vs. pre | |||||
| Stride symmetry ratio | ↑ post vs. pre, NS | |||||
| FIM (walking) | ↑ post vs. pre | |||||
| MAS (walking) | ↑ post vs. pre | |||||
| FRT | ↑ post vs. pre, NS | |||||
| Wilson, 2002 [42] | Case study | n=2 1M, 1F 21 and 39 y |
TBI, Pt 1= severe, Pt 2= moderate, both requiring assistance by therapist | Pt1= 6 mths Pt2= 5 y |
Weekly during training for 8 wks | |
| muscle tone (MoAS) | Pt1= ↑1 point; Pt2= no change | |||||
| strength (MGC) | Pt1= ↑1 point; Pt2= ↑ 1 point | |||||
| SBS | Pt1= ↑ 1 level; Pt2= ↑1 level | |||||
| FAC | Pt1= ↑ 1 level; Pt2= ↑ 1 level | |||||
| MAG | Pt1= ↑ 3 levels (ambulation with walker) Pt2= ↑ 1 level (did not reach independent ambulation) | |||||
| Wilson, 2006 [41] | Small RCT |
BWSTT: n=19 18M.1F 26 (8) y GBT: n= 19 17M, 2F 33 (14)y |
TBI, severe, ambulatory requiring assistance and non-ambulatory |
BWSTT: 4 (3) mths GBT: 3 (2) mths |
0, 8 wks | |
| SBS | BWSTT within ↑ post vs. pre GBT within ↑ post vs. pre ↑ BWSTT > GBT, NS |
|||||
| FAC | BWSTT within ↑ post vs. pre GBT within ↑ post vs. pre ↑ GBT > BWSTT, NS | |||||
| RMI | BWSTT within ↑ post vs. pre GBT within ↑ post vs. pre ↑ BWSTT > GBT, NS | |||||
| GMS | BWSTT within ↑ post vs. pre GBT within ↑ post vs. pre ↑ GBT > BWSTT, NS | |||||
| FIM | BWSTT within ↑ post vs. pre GBT within ↑ post vs. pre ↑ BWSTT > GBT, NS | |||||
| FAM | BWSTT within ↑ post vs. pre GBT within ↑ post vs. pre ↑ BWSTT > GBT, NS | |||||
| Yan, 2008 [43] | Case study | n=1 M 47 y |
TBI, postural instability and unable to ambulate | 4 wks | 0, 4 wks | |
| FIM | ↑ 80 to 110 | |||||
| BBS | ↑20 to 42 | |||||
| MMT | ↑4 to 5 | |||||
| Subjective evaluation of balance and mobility | Acquired independent bed mobility sitting and standing; improved postural stability |
Note: The listed papers reported several outcome measures on several domains, but only those related to gait and balance were captured in this table. Bold type indicates statistically significant results, NS = non-significant,
↑= improvement, y = year(s), mths = months, RCT = randomized controlled trial, PSDQ = Physical Self-description Questionnaire, FES = Functional Electrical Stimulation, BWSTT = Body-weight supported treadmill training, OGT = over-ground gait training, SST = Slide and Step Training, WT = Weight Training, CTSIB = Clinical Test for Sensory Interaction in Balance, BBS = Berg Balance Scale, LOS = Limits of Stability Test (Neurocom), SOT = Sensory Organization Test (Neurocom), ICARS = International Cooperative Ataxia Rating Scale, OGA = Observational Gait Analysis, COVS = Clinical Outcomes Variable Scale, VSS = Vertigo Symptom Scale, VCQ = Vertigo Copying Questionaire, VHQ = Vertigo Handicap Questionaire, DRS = Disability Rating Scores, CB&MS = Community Balance and Mobility Scale, ABC = activities-specific balance confidence scale, LEFS = Lower Extremity Functional Scale, RVGA = Rivermead Visual Gait Assessment, FIM=Functional Independence Measure, MAS=Motor Assessment Scale for Stroke, FRT=Functional Reach Test, MoAS = Modified Ashworth Scale, MGC = Muscle Grading Chart, SBS = Standing Balance Scale, FAC = Functional Ambulatory Category, MAG = Missouri Assisted Gait Scale, RMI = Rivermead Mobility Index , GMS = Gross Motor Subscale, FAM = Functional Assessment Measure, MMT = Manual Muscle Testing for strength
Results
The information in table 2 provides a general overview of the 20 studies in this systematic review [25–44], detailing the study design, number and characteristics of the participants, assessment schedule, outcome measures used, and summarized results. Our search identified four small RCTs [25, 27, 38, 42], eight prospective cohort studies [28, 30, 31, 33, 34, 37, 39, 41], and eight case studies [26, 29, 32, 35, 36, 40, 43, 44]. The sample size ranged from 14–38 subjects in the RCTs, and 5–152 in the prospective studies. Case studies involved one to two individuals. Most of the studies, 14 out of 20 [25, 27–31, 34, 35, 38–40, 42–44], were published in the last 10 years, and the four small RCTs were published within the last seven years. The majority of studies included patients who had suffered a severe TBI but had moderate functional deficits; four studies included independent ambulators [28, 33, 40, 41], eight studies included subjects who needed assistance to ambulate [26, 32, 35, 36, 39, 42–44], one study [27] included both independent and dependent ambulators, and seven studies did not specify functional level [25, 29–31, 34, 37, 38]. In regards to time elapsed since injury, six studies focused on individuals primarily in the acute phase (< six months) of TBI [29, 35, 38, 41, 42, 44], and ten were labeled as being in the chronic phase of TBI (> six months) [25, 27, 28, 31–34, 37, 39, 40]. Two others were not specified as to time since injury [26, 30], and two case studies included an acute and a chronic patient each [36, 43].
Table 2.
Description of Therapy Methods by Study
| First Author, Year | Setting | Main Intervention | Program frequency and duration | Control Group Interventions |
|---|---|---|---|---|
| Blake, 2009 [26] | Community day centre | Tai Chi | 1 hr/1 × per wk/8 wks | Social/leisure activities |
| Bogataj, 1989 [27] | Not specified | FES + CPT + meds | Individualized times daily/5 × per wk/12 days | None |
| Brown, 2005 [28] | Residential rehab facility | BWSTT + CPT | 15 min/2 × per wk/3 mths | OGT |
| Dault, 2002 [29] | Not specified | SST | 30 min/2 × per wk/12 wks | WT |
| Degano, 2009 [30] | OP/rehab center | APT + GBT | (1 hr APT/2 × wk + 1 hr GBT /1 × wk)/4 wks | None |
| Franckeviciute, 2008 [31] | IP/rehab unit | GBT + CPT | 40–50 min/78.7 ± 24.6 sessions/ 54 days. | None |
| Gurr, 2001 [32] | OP | Vest Rehab | 1 hr/1 × per wk/6 wks | None |
| Herdman, 1990 [33] | Not specified | Vest Rehab + med withdrawal | 6 mths | None |
| Hurt, 1998 [34] | OP/home | RAS | Individualized times daily/5 wks | None |
| Schalow, 2002 [10] | Not specified | CDT | At least 4 hrs per day/5.5 × per wk/3 mths | None |
| Scherer, 2007 [35] | IP/rehab unit | BWSTT | 9 sessions | None |
| Seif-Naraghi, 1999 [11] | IP/rehab | BWSTT | Patient 1: 3 to 40 min/3 × per wk/4 mths Patient 2: 5 to 40 min/3 × per wk/3 mths |
None |
| Shepard, 1993 [36] | Home | GBT + CPT | 2–10 weeks | None |
| Sveistrup, 2003 [37] | Not specified | VR | 1 hr/3 × per wk/ 6 wks | Control 1:GBT Control 2: no intervention |
| Thornton, 2005 [38] | OP/rehab center | Cohort1:VR Cohort2: GBT |
50 min/3 × per wk/6 wks | None |
| Vaz, 2008 [39] | OP/university rehab clinic | Treadmill | 20 min/3 × per wk/4 wks | None |
| Wade, 1997 [40] | IP/rehab unit | GBT + CPT | Individualized times | None |
| Wilson, 2002 [42] | IP/rehab unit | BWSTT + CPT | 1 hr/2× wk/8 wks | None |
| Wilson, 2006 [41] | IP/rehab hospital | BWSTT + CPT | (1 hr/3 × wk CPT + 1 hr 2× wk BWSTT)/ 8 wks | GBT+CPT + WT |
| Yan, 2008 [43] | IP/rehab unit | Balance + CPT + OT/ST | 4 wks | None |
Note: hr = hour, wk = week, mth = month, FES = functional electrical stimulation, CPT = conventional physical therapy, BWSTT = body weight-support treadmill training, OGT = over-ground gait training, SST = slide and step training, WT = weight training, GBT = gait & balance training, Vest Rehab = vestibular rehabilitation, RAS = rhythmic auditory stimulation, CDT = coordination dynamic therapy (walking, crawling, jumping),VR = virtual reality, APT = aquatic physical therapy, OT = occupational therapy, ST = speech therapy, OP = outpatient, IP = inpatient
A broad range of outcome measures was reported such that out of all 20 studies, approximately 50 different outcome measures were assessed. Eight studies used motor scales and/or questionnaires [25, 30, 37–39, 42–44], six used more quantitative instrumented measures (e.g. spatiotemporal gait parameters) [26, 28, 32–35], five used multiple types of outcomes [27, 29, 31, 40, 41], and one study used only subjective evaluation and treatment progression (e.g. changes in % of body weight support, walking time, walking speed) as outcome measures [36]. The outcome measures used for the most part tended to be specific to the type of intervention employed in the study. For example, there were seven gait intervention studies reporting gait outcomes only [26, 27, 33–36, 40], two balance intervention studies with only balance outcomes [31, 32], and six studies with both gait and balance interventions and outcomes [29, 30, 37–39, 41]. However, two of the gait intervention studies [42, 43] and two of the balance intervention studies [25, 44] evaluated effects on both gait and balance, while one study using both gait and balance interventions measured the effects on balance alone [28]. Validity and reliability of outcome measures were not reported in any studies. Based on the International Classification of Functioning [24], the outcome measures seemed to be evenly distributed between the Body Structures and Functions and Activity and Participation categories.
Overall results showed an improvement in the outcome measures but were limited by a lack of inferential statistical analysis (ten studies) [26, 29, 32, 34–38, 43, 44] or lack of improvement to a statistically significant level when analyses were performed on some of the outcome measures (nine studies) [25, 27, 28, 31, 33, 39–42]. The limited use of between-group statistical analyses was due largely to the paucity of RCTs and controlled cohort studies. The only study that used statistical analysis and demonstrated only positive significant findings was by Franckeviciute [30], who divided a cohort of individuals into age groups and reported the younger age group (18–44 years) improved significantly more in the Clinical Outcomes Variable Scale (COVS) than the older age groups (45–59 and 60–74 years). Among those trials with control/comparison groups [25, 27, 28, 38, 42], no intervention was shown to be significantly better than any other at improving outcomes, except in the study by Brown [27], which showed a greater decrease in step length asymmetry with over-ground gait training (OGT) than with body-weight supported treadmill training (BWSTT).
Table 3 provides a more in-depth description of the interventions including the setting, type of therapy, frequency and duration of treatment, any interventions that were provided concurrently or allowed to be continued along with the primary intervention, and control group interventions if applicable. Eight studies focused on individuals during inpatient hospital or rehabilitation center stays [27, 30, 35, 36, 41–44], another seven of those treated and assessed regularly as outpatients or at home [25, 29, 31, 33, 37, 39, 40], and the remaining five studies did not specify the setting [26, 28, 32, 34, 38]. The studies were also very heterogeneous in terms of treatment modality, the most common therapeutic technique employed being BWSTT in five studies [27, 35, 36, 42, 43]; another used treadmill training without support [40]. Three studies observed the effect of gait and balance training (GBT) in conjunction with conventional physical therapy (CPT) [30, 37, 41], while another combined the GBT with aquatic physical therapy (APT) [29]. Also, GBT alone was used for one of the cohorts in the study by Thornton [39]. The next most frequently observed interventions were only used in two studies each: virtual reality (VR) training [38, 39] and vestibular rehabilitation [31, 32]. In addition, subjects in the study by Herdman [32] were also withdrawn from the medications which had been treating their balance symptoms. A number of less common techniques received attention as well, eachc in a single study: Tai Chi [25], functional electrical stimulation (FES) [26], Slide and Step training [28], rhythmic auditory stimulation [33], and coordination dynamic therapy [34]. Furthermore, CPT was used in eight of the studies but always in addition to other treatments like FES and medications [26], BWSTT [27, 42, 43], GBT [30, 37, 41], and balance training plus speech and occupational therapy [44]. Though few studies incorporated control groups, the control interventions included social/leisure activities [25], OGT [27], weight training [28], GBT [38], and a combination of weight training, GBT, and CPT [42]. Only one study [38] utilized a `no intervention' control group in addition to the other control group receiving GBT.
There was also considerable variability in the frequency and duration of treatment programmes, many of which did not specify these parameters fully [26, 30, 32–37, 41, 44]. For example, the studies of GBT with CPT treated patients on an individual basis from two to ten weeks [30, 37, 41]. On the other hand, typical BWSTT programmes were one to two hours per week for four to eight weeks [35, 42, 43] or shorter sessions for a longer duration such as 30 minutes a week for three to four months [27, 36]. Both virtual reality training programmes were relatively similar, consisting of one-hour sessions, three times weekly for six weeks [38, 39]. In contrast, the vestibular rehabilitation programmes lasted six hours over six weeks and an unspecified amount over six months [31, 32]. Overall, the programmes incorporating concurrent CPT [26, 27, 30, 37, 41–44] used it according to the schedule of the primary intervention.
Table 4 summarizes the level and quality of evidence of the identified studies. No included studies reached the strength of level I evidence (large RCTs), but four [25, 27, 38, 42] did meet criteria for level II, which consists of small RCTs. However, the PEDro quality scores of these RCTs ranged from as low as 3 to a high of 8 out of 10. The two RCTs achieving quality scores of 8 were the highest quality studies found in our review, with points lost only for lack of blinding [25, 42]. Achieving a level of evidence rating of III or IV (depending on presence of a control group) were eight prospective cohort studies [28, 30, 31, 33, 34, 37, 39, 41]. Only one of these cohort studies included a control group, thus earning level III status [28]; this study, however, only scored 3 on the PEDro quality scale. The other seven prospective cohort studies were level IV evidence, and their quality scores ranged from 2 to 4. Finally, eight of the articles are only case studies [26, 29, 32, 35, 36, 40, 43, 44] which merit a level of evidence rating of V, the lowest, but most common, score in our review. All of these studies earned a quality score of 2, except for one 3 [40]; this was also the only reported case study that employed inferential statistical analysis. The authors utilized an ABA design and reported a time series analysis to identify trends in sequential measurements (celeration line) and a two-standard deviation band for analysis. In 14 studies, the quality ratings were so poor (2–3/10) [26, 28, 29, 32–40, 43, 44] that some reviews would consider them to be of inadequate quality to merit inclusion. As can be seen, certain trends existed among attainment of the quality items. All studies measured key outcomes from more than 85% of participants and treated all patients fully with intended therapy or claimed intention to treat analysis, gaining points for categories 8 and 9. On the other hand, virtually no studies earned points for items 3, 4, 5, 6, and 7, which address concealment of allocation, proof of baseline group similarity, and blinding of participants, therapists, and assessors, respectively.
When comparing gait versus balance interventions, we found that studies evaluating the use of balance training [25, 31, 32, 44] were fewer in number and very low in strength and quality of evidence, with the exception of one high quality RCT [25]. Of the four balance studies, there was one RCT, one prospective cohort study, and two case studies with quality scores from 2 to 8. The single balance-oriented RCT (PEDro score 8) [25], which compared Tai Chi to control group, did not show significantly better balance or gait outcomes from the intervention. Under PEDro classification, this leads to the conclusion that there is moderate evidence that practicing Tai Chi does not improve gait and balance better than a `no exercise' condition. On the other hand, while the case studies noted improvements after balance therapies and the cohort study suggested statistically significant improvements, according to PEDro classification these studies indicate only limited evidence of positive effects from balance interventions.
Despite the fact that the highest number, level, and quality of studies dealt with gait training alone [26, 27, 33–36, 40, 42, 43], only two were RCTs [27, 42]. These showed no significantly different levels of improvement in gait or balance outcomes after therapy with BWSTT and CPT compared to OGT in one study [27] and compared to combination therapy of CPT, GBT, and weight training in the other [42], although both intervention groups did improve as a result of therapy in each case. This allows us to conclude that there is strong evidence that BWSTT is no better at improving gait and balance than other exercise programmes in this population (i.e. OGT or GBT with weight training). The other gait studies were two prospective cohort studies and five case studies with quality scores ranging from 2 to 8. Every one of these studies showed improvements post therapy, though not all results were significant. Together, evidence is both limited and inconsistent that various types of gait training have positive effects on gait and balance outcomes in accordance with the PEDro classification.
The lowest level of evidence and quality group was that of the seven studies involving both gait and balance training [28–30, 37–39, 41], consisting of one RCT, one controlled and four non-controlled prospective cohort studies, and one case study with quality scores from 2 to 4. The single RCT investigating the combination of gait and balance training [38] was very low quality, PEDro score 3, partly because it did not report means and standard deviations and it did not report statistical analyses, leaving the reader to extrapolate results from graphs. Nevertheless, it reported that gait and balance training in a VR environment improved patients' balance and mobility, while groups with conventional GBT and no intervention improved to a lesser extent. The other controlled trial, a prospective cohort study [28], showed that Slide & Step training, which led to statistically significant improvements, was superior to weight training, which yielded no change in balance outcomes. Of the remaining observational cohort and case studies, all listed improvements from various gait and balance interventions, but only one [41] showed statistically significant improvements on gait and balance outcomes. Therefore, only limited evidence supports that the combination of gait and balance therapies can improve patient outcomes because the single RCT in this group was less than fair quality.
Discussion
The primary goal of this literature review was to evaluate the evidence for the efficacy or effectiveness of gait and balance interventions in treating residual functional problems in individuals who have suffered a TBI. This review found limited evidence that physical therapy interventions aimed at improving balance, gait, or both, regardless of type, were effective as a rehabilitation strategy in the TBI population. These findings are consistent with prior systematic reviews on the subject of brain injury rehabilitation [1, 5]. Teasell et al. [1] investigated the effects of any rehabilitation intervention (i.e. multidisciplinary rehabilitation, pharmacologic treatment, exercise/aerobic training, etc.) and found primarily limited evidence of positive effects of any interventions due to poor methodological quality of the studies and the fact that a minority were RCTs. Marshall et al. [5] restricted the literature review to treatments affecting motor impairments, and though there was a broad range of pharmacologic, non-pharmacologic, and exercise interventions, one conclusion was that BWSTT was not superior to conventional gait training, a finding corroborated by our review. As such, ours is the first systematic review to focus specifically on gait and balance training.
The secondary goal of this review was to provide evidence-based guidelines for clinical practice. Results on intensity, frequency and duration of therapy were variable and not fully specified by many articles, but in general therapy sessions that were evaluated lasted 30 minutes to 1 hour, were as frequent as 1 to 3 times per week, for 2 weeks minimum to 6 months maximum. Our ability to make further recommendations has been limited by several factors. The most important factors are that not only is the number of RCTs in this specific area limited, but many also were of low to fair quality. There were only two small RCTs of fair quality to support the effects of gait training, one for balance training, and none for the combination of both. A much larger portion of the studies identified by this review were non-controlled prospective cohort and single case studies, which generally scored poorly on the quality scale. Partly responsible for the low quality ratings of these studies is the fact that the Pedro scale used to calculate these values apply primarily to RCTs. Hence, studies representing lower levels of evidence necessarily receive lower quality scores. For example, only RCTs could receive points for items 2 (random allocation) and 10 (between-group statistical analysis). Overall our findings suggest a lack of methodological quality with regards to the following aspects: 1) group size and homogeneity, 2) intervention quality, and 3) outcome quality.
1) Small sample sizes and heterogeneous groups were a common observation in this review
Most studies had no more than 20 subjects, and the largest RCT [42] had 38 subjects divided into two groups. Variability in the samples across studies was a major issue, even causing difficulty structuring the review, with differences noted in the following areas: TBI classification, time since injury (acute vs. chronic), and inpatient vs. outpatient rehabilitation. In fact, many of the studies did not clearly state how individuals were classified in terms of their injury, possibly because there was often a mixture of severity within groups. However, those who did employ their own subjective TBI classification (mild, moderate, severe) still included individuals with diverse functional levels, and rarely was it specified how these individuals were distributed between groups.
Group heterogeneity and small samples in an RCT may lead to non-equivalence between groups with respect to baseline function and other characteristics, causing an intervention to appear less effective on a group that has less ambulatory potential. Unfortunately, heterogeneity is inherent to TBI, and the traditional TBI classification system has failed to provide a homogeneous means of classifying TBI groups. Studies have shown that the categories mild, moderate, and severe are not only too broad, but also ineffective to predict adequately long-term prognosis of outcomes like return to functional independence [45]. A more useful alternative to the traditional classification would be a functional classification representing the current status of patients, and therefore this is the approach taken in our review.
Another common finding in our review was that the time since TBI differed greatly. There were different numbers of acute vs. chronic patients, as well as chronic patients with variable times between injury and start of rehabilitation. Finally, heterogeneity was also found in the number of studies that evaluated inpatient vs. outpatient treatment programmes. Many of the studies seem to have used convenience samples. The issue of small and variable samples further adversely affects power to detect significant differences in therapies.
2) The interventions investigated were variable and lacked control
Not only were 18 distinct interventions utilized in the 20 studies, but the frequency and duration of treatment varied as well. This creates difficulty comparing results across studies in a literature review, making it difficult even to group the interventions. With such variability, there is not enough information to recommend to clinicians precisely which therapy is best and how long and how often it should be performed. In addition, the intervention in some cases may not have been done long enough to show an effect.
Another problem found in many studies was that patients received more than one intervention type concurrently (i.e. BWSTT with CPT or virtual reality training with medication withdrawal). Conducting multiple therapies simultaneously clouds the results, making it impossible to determine which treatment resulted in improvement. The use of comparison interventions rather than no intervention to establish a pure control for comparison was also very common. This makes it difficult to find superior effects of the principal intervention since both groups ought to improve when compared against another intervention. Another issue was the lack of blinding of therapists treating patients, or the lack of report on that, by many studies. This is a problem because if the therapist treating patients is the same investigating the effects of therapy, collecting the data, and analyzing it, that individual will probably be biased to report positive results, especially when using measures like rating scales.
3) Outcome measures were variable and lacked quality
As mentioned in the results, approximately 50 different measures were identified. Having a variety of measures creates difficulty in comparing results across studies and drawing useful conclusions on treatment effects. Many studies failed to blind the tester, or if they did, it was not reported. Lack of tester blinding may increase investigator bias [46]. Another finding was that most studies failed to report about sensitivity, validity, and reliability of the outcome measures. This can be a problem because if the tool is not sensitive, small changes occurring due to the intervention may go undetected; if it is not valid, the results may be meaningless for that population; and if it is not reliable, results cannot be reproduced in other studies [47].
Conclusion and Future Studies
The limitations found in the reviewed studies make it difficult to draw useful evidence-based recommendations for clinical practice. Nevertheless, several recommendations can be drawn for future studies. First, larger and higher quality RCTs are needed to evaluate the effects of specific gait and balance interventions for TBI rehabilitation. Samples should be larger and more homogeneous to enhance statistical power. Not only will groups with more baseline similarity produce less convoluted results, but also more direct recommendations will result about which groups (i.e. acute vs. chronic, inpatient vs. outpatient, ambulatory vs. non-ambulatory) may benefit most from a particular intervention. Grouping individuals by functional severity and not solely severity of injury would be one solution to produce more homogeneous samples. When homogeneity of groups is not achieved, the study should correct for that statistically (e.g. ANCOVA).
Multiple, concurrent interventions should be avoided, and instead single therapies should be addressed to allow for a clear determination on the efficacy of a specific therapy. Given the wide heterogeneity across subjects, control groups should be more carefully considered and as one possible alternative could include a delayed entrance crossover design where subjects serve as their own controls. Even though double blinding is not feasible with exercise interventions, studies should be blinded at least to the assessors to reduce measurement bias. Also, the intensity, frequency, and duration of interventions must be standardized to draw meaningful conclusions. Future studies must further address the optimal intensity, frequency, and duration of treatment for this type of standardization to be possible, a process exemplified by Teasell et al. [1] with their strong evidence that more intense therapy leads to earlier and better functional outcomes. Finally, care should be taken in choosing outcome measures that are sensitive, valid, and reliable. Ideally, the field of TBI rehabilitation would benefit from standardized, well-established measures, allowing studies to be compared against each other.
In conclusion, the state of the evidence for TBI rehabilitation, specifically in regards to gait and balance interventions, is surprising given the prevalence of TBI and the fact that these are common residual deficits. Despite the fact that no general conclusion can yet be made about which intervention is most effective in this population and how best to employ it, a few results can be helpful for clinical practice beyond advice for designing and conducting more research. Although it is a commonly employed technique, the evidence is strong that BWSTT is no better at improving gait and balance outcomes (e.g. spatiotemporal parameters, functional gait and balance scales) in individuals with TBI than conventional OGT [27] or GBT [42]. Moderate evidence supports that Tai Chi is also equivalent to social activities performed in a community day centre in improving individuals' self-description of coordination, flexibility and physical activity [25]. Balance and gait interventions in combination only share limited evidence of positive effects on balance and mobility outcomes. When comparing the two types of intervention, neither balance or gait intervention alone has emerged as more effective than the other. With this in mind, future research must be better designed to include larger and more homogeneous groups of subjects, to apply more standardized and controlled treatment approaches, and to choose good-quality outcome measures. In addition, research in this area would benefit frominvestigating cutting edge promising therapies involving technology like robotics and virtual reality.
Acknowledgements
This work was funded in part by the NIH Clinical Research Training Program, the NIH Clinical Center intramural research program and the Center for Neuroscience and Regenerative Medicine.
References
- 1.Teasell R, Bayona N, Marshall S, et al. A systematic review of the rehabilitation of moderate to severe acquired brain injuries. Brain Inj. 2007;21(2):107–112. doi: 10.1080/02699050701201524. [DOI] [PubMed] [Google Scholar]
- 2.Langlois JA, Rutland-Brown W, Wald MM. The epidemiology and impact of traumatic brain injury: a brief overview. J Head Trauma Rehabil. 2006;21(5):375–378. doi: 10.1097/00001199-200609000-00001. [DOI] [PubMed] [Google Scholar]
- 3.Powell JM, Temkin NR, Machamer JE, Dikmen SS. Nonrandomized studies of rehabilitation for traumatic brain injury: can they determine effectiveness? Arch Phys Med Rehabil. 2002;83(9):1235–1244. doi: 10.1053/apmr.2002.34556. [DOI] [PubMed] [Google Scholar]
- 4.Basford JR, Chou LS, Kaufman KR, et al. An assessment of gait and balance deficits after traumatic brain injury. Arch Phys Med Rehabil. 2003;84(3):343–349. doi: 10.1053/apmr.2003.50034. [DOI] [PubMed] [Google Scholar]
- 5.Marshall S, Teasell R, Bayona N, et al. Motor impairment rehabilitation post acquired brain injury. Brain Inj. 2007;21(2):133–160. doi: 10.1080/02699050701201383. [DOI] [PubMed] [Google Scholar]
- 6.Cullen N, Chundamala J, Bayley M, Jutai J. The efficacy of acquired brain injury rehabilitation. Brain Inj. 2007;21(2):113–132. doi: 10.1080/02699050701201540. [DOI] [PubMed] [Google Scholar]
- 7.Hellweg S, Johannes S. Physiotherapy after traumatic brain injury: a systematic review of the literature. Brain Inj. 2008;22(5):365–373. doi: 10.1080/02699050801998250. [DOI] [PubMed] [Google Scholar]
- 8.McFadyen BJ, Cantin JF, Swaine B, et al. Modality-specific, multitask locomotor deficits persist despite good recovery after a traumatic brain injury. Arch Phys Med Rehabil. 2009;90(9):1596–1606. doi: 10.1016/j.apmr.2009.03.010. [DOI] [PubMed] [Google Scholar]
- 9.Kolb B, Teskey GC. Age, Experience, Injury, and the Changing Brain. [Accessed 2011 Mar 3];Developmental Psychobiology. 2010 doi: 10.1002/dev.20515. http://www.ncbi.nlm.nih.gov/pubmed/21108243. [DOI] [PubMed]
- 10.Huang ME, Cifu DX, Keyser-Marcus L. Functional outcomes in patients with brain tumor after inpatient rehabilitation: Comparison with traumatic brain injury. American Journal of Physical Medicine and Rehabilitation. 2000;79(4):327–335. doi: 10.1097/00002060-200007000-00003. [DOI] [PubMed] [Google Scholar]
- 11.O'Dell MW, Barr K, Spanier D, Warnick RE. Functional outcome of inpatient rehabilitation in persons with brain tumors. Arch Phys Med Rehabil. 1998;79(12):1530–1534. doi: 10.1016/s0003-9993(98)90414-2. [DOI] [PubMed] [Google Scholar]
- 12.Powell J, Heslin J, Greenwood R. Community based rehabilitation after severe traumatic brain injury: a randomised controlled trial. J Neurol Neurosurg Psychiatry. 2002;72(2):193–202. doi: 10.1136/jnnp.72.2.193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sahgal V, Heinemann A. Recovery of function during inpatient rehabilitation for moderate traumatic brain injury. Scand J Rehabil Med. 1989;21(2):71–79. [PubMed] [Google Scholar]
- 14.Alderman N, Shepherd J, Youngson H. Increasing standing tolerance and posture quality following severe brain injury using a behaviour modification approach. Physiotherapy. 1992;78(5):335–343. [Google Scholar]
- 15.Betker AL, Szturm T, Moussavi ZK, Nett C. Video Game-Based Exercises for Balance Rehabilitation: A Single-Subject Design. Arch Phys Med Rehabil. 2006;87(8):1141–1149. doi: 10.1016/j.apmr.2006.04.010. [DOI] [PubMed] [Google Scholar]
- 16.Freivogel S, Mehrholz J, Husak-Sotomayor T, Schmalohr D. Gait training with the newly developed `LokoHelp'-system is feasible for non-ambulatory patients after stroke, spinal cord and brain injury. A feasibility study. Brain Inj. 2008;22(7–8):625–632. doi: 10.1080/02699050801941771. [DOI] [PubMed] [Google Scholar]
- 17.Shapira MY, Chelouche M, Yanai R, Kaner C, Szold A. Tai Chi Chuan practice as a tool for rehabilitation of severe head trauma: 3 case reports. Arch Phys Med Rehabil. 2001;82(9):1283–1285. doi: 10.1053/apmr.2001.25152. [DOI] [PubMed] [Google Scholar]
- 18.Berrol C. Dance/movement therapy in head injury rehabilitation. Brain Inj. 1990;4(3):257–265. doi: 10.3109/02699059009026175. [DOI] [PubMed] [Google Scholar]
- 19.Zhu XL, Poon WS, Chan CC, Chan SS. Does intensive rehabilitation improve the functional outcome of patients with traumatic brain injury (TBI)? A randomized controlled trial. Brain Inj. 2007;21(7):681–690. doi: 10.1080/02699050701468941. [DOI] [PubMed] [Google Scholar]
- 20.Bohannon RW, Gibson DF. Effectiveness of a rolling board treatment for improving gait. A case report. Phys Ther. 1986;66(3):349–350. doi: 10.1093/ptj/66.3.349. [DOI] [PubMed] [Google Scholar]
- 21.Wieler M, Stein RB, Ladouceur M, et al. Multicenter evaluation of electrical stimulation systems for walking. Arch Phys Med Rehabil. 1999;80(5):495–500. doi: 10.1016/s0003-9993(99)90188-0. [DOI] [PubMed] [Google Scholar]
- 22.Sackett DL, Straus SE, Richardson WS, et al. Evidence-Based Medicine: How to Practice and Teach EBM. Churchill Livingstone; Toronto, ON: 2000. [Google Scholar]
- 23.Maher CG, Sherrington C, Herbert RD, Moseley AM, Elkins M. Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys Ther. 2003;83(8):713–721. [PubMed] [Google Scholar]
- 24.World Health Organization [Accessed 2011 Mar 4];International Classification of Functioning, Disability and Health. http://apps.who.int/classifications/icfbrowser.
- 25.Blake H, Batson M. Exercise intervention in brain injury: A pilot randomized study of Tai Chi Qigong. Clinical Rehabilitation. 2009;23(7):589–598. doi: 10.1177/0269215508101736. [DOI] [PubMed] [Google Scholar]
- 26.Bogataj U, Gros N, Malezic M, Kelih B, Kljajic M, Acimovic R. Restoration of gait during two to three weeks of therapy with multichannel electrical stimulation. Phys Ther. 1989;69(5):319–327. doi: 10.1093/ptj/69.5.319. [DOI] [PubMed] [Google Scholar]
- 27.Brown TH, Mount J, Rouland BL, Kautz KA, Barnes RM, Kim J. Body weight-supported treadmill training versus conventional gait training for people with chronic traumatic brain injury. J Head Trauma Rehabil. 2005;20(5):402–415. doi: 10.1097/00001199-200509000-00002. [DOI] [PubMed] [Google Scholar]
- 28.Dault MC, Dugas C. Evaluation of a specific balance and coordination programme for individuals with a traumatic brain injury. Brain Inj. 2002;16(3):231–244. doi: 10.1080/02699050110103300. [DOI] [PubMed] [Google Scholar]
- 29.Degano AC, Geigle PR. Use of aquatic physical therapy in the treatment of balance and gait impairments following traumatic brain injury: a case report. Journal of Aquatic Physical Therapy. 2009;17(1):16–21. [Google Scholar]
- 30.Franckeviciute EV, Krisciunas AJ. Motor recover during the acute period of craniocerebral trauma using kinetotherapy. Neuroscience and Behavioral Physiology. 2008;38(8):877–881. doi: 10.1007/s11055-008-9050-1. [DOI] [PubMed] [Google Scholar]
- 31.Gurr B, Moffat N. Psychological consequences of vertigo and the effectiveness of vestibular rehabilitation for brain injury patients. Brain Inj. 2001;15(5):387–400. doi: 10.1080/02699050010005904. [DOI] [PubMed] [Google Scholar]
- 32.Herdman SJ. Treatment of vestibular disorders in traumatically brain-injured patients. J Head Trauma Rehabil. 1990;5(4):63–76. [Google Scholar]
- 33.Hurt CP, Rice RR, McIntosh GC, Thaut MH. Rhythmic Auditory Stimulation in Gait Training for Patients with Traumatic Brain Injury. Journal of Music Therapy. 1998;35(4):228–241. doi: 10.1093/jmt/35.4.228. [DOI] [PubMed] [Google Scholar]
- 34.Schalow G. Improvement after traumatic brain injury achieved by coordination dynamic therapy. Electromyography and Clinical Neurophysiology. 2002;42(4):195–203. [PubMed] [Google Scholar]
- 35.Scherer M. Gait rehabilitation with body weight-supported treadmill training for a blast injury survivor with traumatic brain injury. Brain Inj. 2007;21(1):93–100. doi: 10.1080/02699050601149104. [DOI] [PubMed] [Google Scholar]
- 36.Seif-Naraghi AH, Herman RM. A novel method for locomotion training. J Head Trauma Rehabil. 1999;14(2):146–162. doi: 10.1097/00001199-199904000-00005. [DOI] [PubMed] [Google Scholar]
- 37.Shepard NT, Smith-Wheelock M, Telian SA, Raj A. Vestibular and balance rehabilitation therapy. Annals of Otology, Rhinology and Laryngology. 1993;102(3 I):198–205. doi: 10.1177/000348949310200306. [DOI] [PubMed] [Google Scholar]
- 38.Sveistrup H, McComas J, Thornton M, et al. Experimental Studies of Virtual Reality-Delivered Compared to Conventional Exercise Programs for Rehabilitation. CyberPsychology & Behavior. 2003;6(3):245–249. doi: 10.1089/109493103322011524. [DOI] [PubMed] [Google Scholar]
- 39.Thornton M, Marshall S, McComas J, Finestone H, McCormick A, Sveistrup H. Benefits of activity and virtual reality based balance exercise programmes for adults with traumatic brain injury: Perceptions of participants and their caregivers. Brain Inj. 2005;19(12):989–1000. doi: 10.1080/02699050500109944. [DOI] [PubMed] [Google Scholar]
- 40.Vaz DV, Schottino RdC, De Castro TRR, Teixeira VR, Furtado SRC, De Mello Figueiredo E. Treadmill training for ataxic patients: A single-subject experimental design. Clinical Rehabilitation. 2008;22(3):234–241. doi: 10.1177/0269215507081578. [DOI] [PubMed] [Google Scholar]
- 41.Wade LD, Canning CG, Fowler V, Felmingham KL, Baguley IJ. Changes in postural sway and performance of functional tasks during rehabilitation after traumatic brain injury. Arch Phys Med Rehabil. 1997;78(10):1107–1111. doi: 10.1016/s0003-9993(97)90136-2. [DOI] [PubMed] [Google Scholar]
- 42.Wilson DJ, Powell M, Gorham JL, Childers MK. Ambulation training with and without partial weight bearing after traumatic brain injury: Results of a randomized, controlled trial. American Journal of Physical Medicine and Rehabilitation. 2006;85(1):68–74. doi: 10.1097/01.phm.0000193507.28759.37. [DOI] [PubMed] [Google Scholar]
- 43.Wilson DJ, Swaboda JL. Partial weight-bearing gait retraining for persons following traumatic brain injury: Preliminary report and proposed assessment scale. Brain Inj. 2002;16(3):259–268. doi: 10.1080/02699050110103922. [DOI] [PubMed] [Google Scholar]
- 44.Yan CC. Optimizing postural control after traumatic brain injury: A task-oriented approach to examination and intervention. Physiotherapy Singapore. 2008;11(1):6–13. [Google Scholar]
- 45.Green RE, Colella B, Hebert DA, et al. Prediction of return to productivity after severe traumatic brain injury: investigations of optimal neuropsychological tests and timing of assessment. Arch Phys Med Rehabil. 2008;89(12 Suppl):S51–60. doi: 10.1016/j.apmr.2008.09.552. [DOI] [PubMed] [Google Scholar]
- 46.Portney LG, Watkins MP. Experimental Control. In: Portney LG, Watkins MP, editors. Foundations of clinical research: applications to practice. 2nd ed. Prentice-Hall, Inc.; Upper Saddle River, New Jersey: 2000. [Google Scholar]
- 47.Portney LG, Watkins MP. Validity of Measurements. In: Portney LG, Watkins MP, editors. Foundations of clinical research: applications to practice. 2nd ed. Prentice-Hall, Inc.; Upper Saddle River, New Jersey: 2000. [Google Scholar]