Abstract
Purpose
To compare echocardiography use among urban and rural veterans and whether differences could be accounted for by distance.
Methods
We used Veterans Administration (VA) administrative data from 1999 to 2007 to identify regular users of the VA Healthcare System (VA users) who did and did not receive echocardiography. Each veteran was categorized as residing in urban, rural or highly rural areas using RUCA codes. Poisson regression was used to compare echocardiography utilization rates among veterans residing in each area after adjusting for demographics, comorbidities, clustering of patients within VA networks and distance to the nearest VA medical center offering echocardiography.
Findings
Our study included 22.7 million veterans of whom 1.3 million (5.7%) received at least one echocardiogram. Of echocardiography recipients, 69.2% lived in urban, 22.0% in rural and 8.8% in highly rural areas. In analyses adjusting for patient demographics, comorbidities, and clustering, utilization of echocardiography was modestly lower for highly rural and rural veterans compared with urban veterans (42.0 vs 40.1 vs 43.1 echocardiograms per 1,000 VA users per year for highly rural, rural and urban, respectively; P < .001). After further adjusting for distance, echocardiography utilization was somewhat higher for veterans in highly rural and rural areas than it was for urban areas (44.9 vs 41.8 vs 40.8 for highly rural, rural and urban, respectively; P < .001).
Conclusions
Echocardiography utilization among rural and highly rural veterans was marginally lower than for urban veterans, but these differences can be accounted for by the greater distance of more rural veterans from facilities offering echocardiograms.
Keywords: echocardiography, rural, urban, utilization, veterans
An estimated 60 million Americans representing more than 21% of the population reside in rural areas.1,2 Because physicians and hospitals are typically located in urban centers, there has been ongoing concern that rural residents might lack access to high-quality medical care.3,4 Indeed, the federal government has implemented a number of programs designed to enhance health care access for rural Americans.5,6
Studies evaluating whether rural Americans receive less care or experience worse health outcomes than their urban counterparts have often reached conflicting conclusions.7–12 For example, while Axelrod et al7 found that rural Americans have relatively lower rates of heart, liver and kidney transplant, Doescher et al11 and Abrams et al12 found no difference in the use of preventive health services or outcomes after acute myocardial infarction in urban and rural populations. There is a particular concern that a lack of specialists in rural areas may limit patient access to important new technologies. At the same time, comparisons of the care received by urban and rural Americans are complicated by underlying differences in urban and rural populations and the prevalence of disease among these populations. For example, prior studies have found that rural Americans are more likely to be uninsured and are older, less racially diverse and have worse baseline health status than their urban counterparts, all of which may contribute to variations in care between urban and rural populations.13–17
The Veterans Administration (VA) Healthcare System is the largest integrated delivery system in the United States (US) providing comprehensive health care services to roughly 8 million veterans, 40% of whom reside in rural areas.18 Eligible veterans who enroll in the VA Healthcare System generally have identical health benefits irrespective of rural or urban residence and have similar access to specialist medical care offered by the VA.
Echocardiography is the most common imaging procedure used in cardiovascular medicine and has become the mainstay for assessing the structure and function of the heart. Its use allows physicians to visualize cardiac structures, as well as evaluate regional wall motion at rest and during stress.19 It has proven utility in the diagnosis, guidance of therapy and assessment of prognosis for several cardiac diseases including heart failure, ischemic heart disease and valvular heart disease. The use of echocardiography in the assessment of specific cardiovascular disorders is supported by recent guidelines.20,21 Whether rural patients have reduced access to and receipt of echocardiography relative to their urban counterparts remain an open question.
The objective of this study was to examine the utilization of echocardiography at VA facilities by veterans residing in urban and rural areas and to ascertain whether any differences that were observed might be explained by differences in patient comorbidity or travel distance to VA facilities offering echocardiography.
METHODS
Data Sources
We used VA administrative data from the Patient Treatment Files (PTF) and Outpatient Care Files (OPC) from fiscal years 1999 to 2007. The PTF contains discharge abstract data for all patients hospitalized in VA medical centers. Key data elements include patient demographics, admission dates, residential zip codes, primary and secondary diagnoses and procedures performed during hospitalization (eg, echocardiography) as defined by International Classification of Diseases Ninth Clinical Modification (ICD-9-CM) codes. The OPC contains administrative data on all outpatient encounters at VA facilities. Data elements include dates of visits, type of clinics (eg, primary care, mental health), residential zip codes, diagnoses defined by ICD-9-CM codes, and procedures performed at each encounter defined by Current Procedural Terminology (CPT) codes. All encounters include patient unique identifiers that allow merging of information across the databases.
Identification of Echocardiography Recipients
For purposes of this analysis it was first necessary to identify all echocardiograms performed on veterans during the study period, as this constituted the numerator in subsequent calculations of utilization described below. We identified all echocardiograms performed in the inpatient setting using ICD-9-CM code 88.72; echocardiograms performed in the outpatient setting were identified using CPT codes 93307 (transthoracic echocardiogram complete without Doppler and color flow), 93320 (Doppler add-on), 93325 (color flow add-on), and 93308 (transthoracic echocardiogram follow-up or limited study). Stress and transesophageal echocardiography were excluded due to the specialized indications for these procedures.
Identification of VA Users
In order to calculate echocardiography utilization (ie, number of echocardiograms performed per 1,000 eligible patients), it was also necessary for us to identify the number of patients receiving regular medical care from VA (aka “VA users”)—these individuals would represent the denominator population of individuals eligible to receive an echocardiogram during a given year. For purposes of this study we defined VA users as patients having 2 or more primary care clinic visits during the year. Patients with fewer than 2 primary care clinic visits in a fiscal year were not considered VA users for that year because such patients are unlikely to receive consistent care from VA, likely have other sources for medical care outside the VA, and thus would have a high probability of receiving an echocardiography from a private sector source if one was required. This approach is supported by prior studies demonstrating that most patients with infrequent VA use (eg, fewer than 2 visits per year) seek care from the VA primarily for pharmacy services,22 and they receive the majority of their ongoing medical care from the private sector.23 Thus, inclusion of patients who visit the VA only sporadically could erroneously inflate the denominator in our study and consequently artificially reduce estimates of echocardiography utilization rates.
Defining Rurality
Defining rurality is complex and a number of different methods have been used.24–27 For the purpose of this study, we used the Rural-Urban Commuting Area (RUCA) taxonomy developed by the Health Resources and Services Administration’s Office of Rural Health Policy (ORHP), the Department of Agriculture’s Economic Research Service (ERS), and the WWAMI Rural Health Research Center (RHRC) at the University of Washington School of Medicine.27 RUCA codes use US Census Bureau information on population density and urbanization together with commuting patterns to differentiate geographic regions based on their city or town size and functional relationship to larger cities and towns.28 A zip code approximation of the census tract-based RUCA codes allows individual residential zip codes to be assigned specific RUCA codes.29 Based on each veteran’s residential zip code and corresponding RUCA code, we classified each patient as residing in either an urban (RUCA codes 1.0, 1.1, 2.0, 2.1, 3.0, 4.1, 5.1, 7.1, 8.1, 10.1), rural (RUCA codes 4.0, 4.2, 5.0, 5.2, 6.0, 6.1) or highly rural (RUCA codes 7.0, 7.2, 7.3, 7.4, 8.0, 8.2, 8.3, 8.4, 9.0, 9.1, 9.2, 10.0, 10.2, 10.3, 10.4, 10.5, 10.6) area. We collapsed the standard RUCA categories into these 3 rural categories to allow for more meaningful comparisons in the VA.
Data Analysis
We first compared demographic characteristics and comorbid conditions of all urban, rural and highly rural VA users using the chi-square test of independence for categorical variables and one-way ANOVA for continuous variables; similar tests were used to compare the characteristics of urban, rural and highly rural echocardiogram recipients. These analyses allowed us to examine whether patients residing in more (or less) rural areas possibly had demographic characteristics or comorbidity that might contribute to greater echocardiogram use (see below). Comorbid conditions were defined based on algorithms developed by Elixhauser et al and updated by Quan et al,30,31 and they were identified based on diagnoses present on all VA encounters within the 12 months preceding the date of receipt of the patient’s first echocardiogram. To estimate the total burden of comorbidity for each patient, we summed the total number of individual comorbid conditions identified for each patient and then compared the mean number of comorbid conditions among VA users living in urban, rural and highly rural areas. Similar analyses were performed for echocardiogram recipients.
Second, for every VA user, we calculated the distance between his or her residential zip code and the nearest VA medical center (VAMC). While the VA has dramatically expanded health care access through the opening of Community-Based Outpatient Clinics (CBOCs), echocardiograms are offered only at VAMCs. Distance to the nearest VAMC therefore serves as the distance to the nearest VA echocardiogram facility. Distance was measured in miles as a straight line between the location of the health care facility and the centroid of the zip code of the patient’s residence. We compared the median distance to the nearest VAMC for VA users living in urban, rural and highly rural areas, and similarly, we compared distance to the nearest VAMC for echocardiogram recipients.
Third, we examined trends in unadjusted echocardiogram utilization rates (echocardiograms per 1,000 VA users per year) over time for veterans living in each of the 3 geographic categories. Yearly utilization rates were calculated using the individual number of echocardiograms in a given year divided by the number of VA users in that year. This analysis allowed us to examine changes in utilization of echocardiography while accounting for changes in the number of VA users in the different geographic categories over time. Changes in utilization rates over adjacent years were evaluated using the Mantel-Haenszel chi-square test for trend.
Fourth, we used Poisson regression models to examine unadjusted and adjusted echocardiography utilization rates among VA users residing in urban, rural and highly rural areas. Initial models adjusted for patient demographics, the prevalence of comorbid conditions that might be expected to influence echocardiography use, VA eligibility criteria, and clustering of patients within regional health care networks (ie, Veterans Integrated Service Network, VISNs). Specific comorbid conditions included congestive heart failure (CHF), cardiac arrhythmias, valvular heart disease, acute myocardial infarction (AMI), cerebrovascular disease or stroke (CVD), chronic obstructive pulmonary disease (COPD), diabetes, and hypertension, and they were chosen based on clinical significance. Subsequent models adjusted for all of the factors described above plus the distance each patient lived from the nearest VAMC: inclusion of distance in these final models allowed us to examine whether differences in echocardiography utilization between urban, rural and highly rural patients might be related primarily to the greater distance of patients in more rural areas from facilities offering echocardiography. We also calculated unadjusted echocardiography utilization rates for rural and highly rural veterans living at specific distance cut points to provide a general overview of the relationship between distance and echocardiography utilization.
Fifth, we investigated the frequency of repeated testing among echocardiography recipients by examining the proportion of veterans receiving multiple echocardiograms in a given year and whether this varied by rural-urban category.
Finally, we performed sensitivity analyses in which we used alternative definitions for identifying VA users. In particular, we repeated our analyses described above while defining VA users as patients with at least 1 primary care visit per year, as well as patients with no restriction on the number of primary care visits per year (ie, including patients who had no primary care visit in a particular year).
All analyses were conducted using SAS statistical software version 9.2 (SAS Institute, Cary, North Carolina). The study was approved by both the University of Iowa Institutional Review Board and the Research and Development Committee at the Iowa City VA Medical Center.
RESULTS
Patient Characteristics
Our study population included 22.7 million VA users between 1999 and 2007 of whom 1,295,658 (5.7%) received at least one echocardiogram at a VA facility. Of the VA users, 68.0% lived in urban areas, 23.3% lived in rural areas and 8.7% lived in highly rural areas (Table 1). By comparison, 896,382 (69.2%) of echocardiogram recipients lived in urban areas, 285,066 (22.0%) lived in rural areas and 114,210 (8.8%) lived in highly rural areas (Table 2). VA users living in highly rural areas (Table 1) were older (mean age 65.5 years compared with 64.9 years for rural and 63.7 years for urban VA users) and more likely to be white than their urban counterparts (64.9% compared with 61.8% for rural and 50.2% for urban VA users). Black veterans were more likely to be living in urban areas. More than 94.0% of all VA users were men. Due to the large sample size, statistically significant differences were observed in the prevalence of most of the comorbid characteristics across geographic regions. Highly rural VA users had a higher prevalence of most conditions, but the absolute difference in prevalence was generally small (Table 1). Not surprisingly, VA users living in highly rural areas lived farther from the nearest VAMC than rural and urban users (median distance 58.1 miles vs 52.2 miles for rural and 16.0 miles for urban VA users) (Table 1). Similar differences were observed in analyses of echocardiogram recipients (Table 2), with highly rural veterans being slightly older, more likely to be white, and living farther from the nearest VAMC.
Table 1.
Characteristics of VA users between 1999 and 2007 by rural categorya
| Urban (%) |
Rural (%) |
Highly Rural (%) |
|
|---|---|---|---|
| n= 15,464,725 (68.0) |
n= 5,290,865 (23.3) |
n= 1,975,028 (8.7) |
|
| Age, mean (SD), y | 63.7 (14.1) | 64.9 (12.9) | 65.5 (12.3) |
| Sex (%) | |||
| Male | 94.0 | 95.6 | 96.2 |
| Female | 6.0 | 4.4 | 3.8 |
| Race (%) | |||
| White | 50.2 | 61.8 | 64.9 |
| Black | 13.6 | 5.7 | 3.6 |
| Otherb | 36.2 | 32.5 | 31.5 |
| Comorbid Conditions (%) | |||
| Congestive Heart Failure | 6.6 | 6.9 | 7.1 |
| Valvular Heart Disease | 3.1 | 3.0 | 3.2 |
| Cerebrovascular Disease | 6.8 | 7.1 | 7.1 |
| Hypertension | 62.1 | 64.1 | 64.3 |
| Diabetes | 26.3 | 26.8 | 26.3 |
| Cardiac Arrhythmias | 10.6 | 11.0 | 11.7 |
| Myocardial Infarction | 2.6 | 2.8 | 3.0 |
| COPD | 16.8 | 19.7 | 20.4 |
| Mean number of Comorbid Conditions, mean (SD) | 2.7 (2.1) | 2.6 (2.0) | 2.6 (2.0) |
| Distance to nearest Medical Center, median (IQR), miles | 16.0 (32.6) | 52.2 (44.5) | 58.1 (42.0) |
P < .001 for all comparisons between urban, rural and highly rural VA users.
Other race includes Hispanics, other nonwhite and missing race.
Table 2.
Characteristics of VA users receiving echocardiographs between 1999 and 2007 by rural category
| Urban (%) |
Rural (%) |
Highly Rural (%) |
P Value | |
|---|---|---|---|---|
| n= 896,382 (69.2) |
n= 285,066 (22.0) |
n= 114,210 (8.8) |
||
| Age, mean (SD), y | 66.6 (12.2) | 66.7 (11.4) | 67.3 (10.9) | < .001 |
| Sex (%) | < .001 | |||
| Male | 95.6 | 96.6 | 97.2 | |
| Female | 4.4 | 3.4 | 2.8 | |
| Race (%) | < .001 | |||
| White | 59.4 | 73.6 | 76.5 | |
| Black | 17.2 | 6.2 | 3.9 | |
| Othera | 23.4 | 20.2 | 19.6 | |
| Comorbid Conditions (%) | ||||
| Congestive Heart Failure | 30.6 | 29.4 | 29.3 | < .001 |
| Valvular Heart Disease | 22.2 | 20.8 | 22.7 | < .001 |
| Cerebrovascular Disease | 16.5 | 16.5 | 16.5 | .90 |
| Hypertension | 77.9 | 77.6 | 77.4 | < .001 |
| Diabetes | 35.8 | 35.4 | 34.6 | < .001 |
| Cardiac Arrhythmias | 32.0 | 32.0 | 33.5 | < .001 |
| Myocardial Infarction | 10.8 | 11.0 | 11.1 | < .001 |
| COPD | 30.8 | 34.1 | 34.8 | < .001 |
| Mean number of Comorbid Conditions, mean (SD) | 4.8 (2.8) | 4.6 (2.7) | 4.5 (2.7) | < .001 |
| Distance to nearest Medical Center, median (IQR), miles | 11.4 (20.7) | 46.7 (40.1) | 54.0 (38.4) | < .001 |
Other race includes Hispanics, other nonwhite and missing race.
Echocardiography Utilization
Between 1999 and 2007, a total of 1,429,898 individual echocardiograms were performed: 991,435 (69.3%) on VA users living in urban areas, 312,741 (21.9%) on VA users living in rural areas and 125,722(8.8%) on VA users living in highly rural areas.
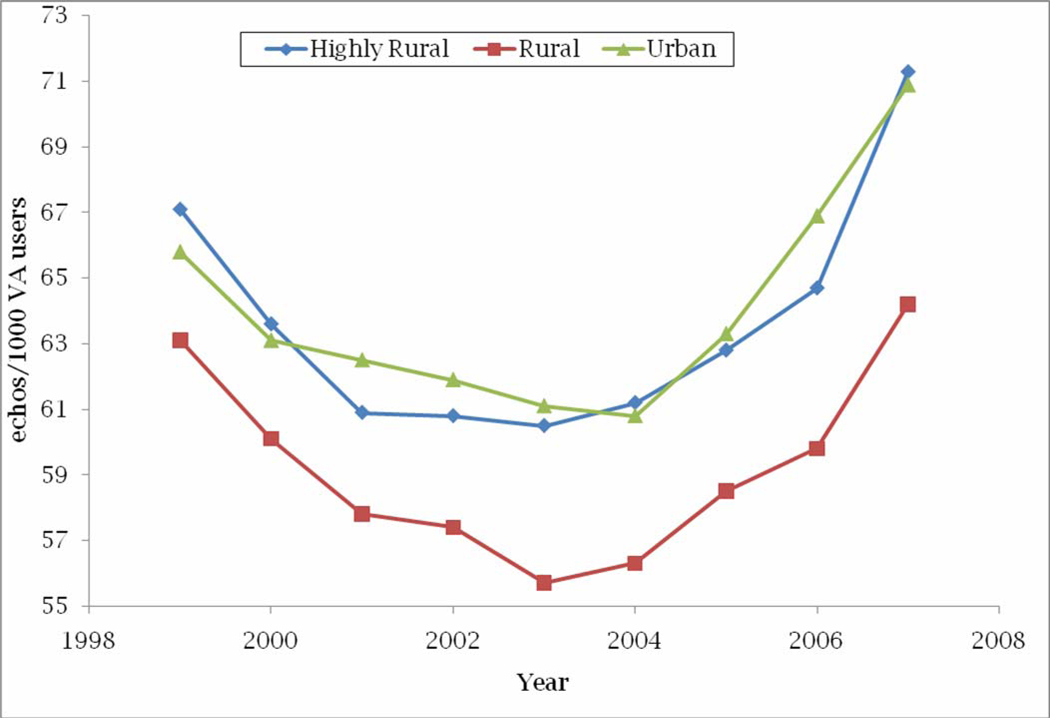
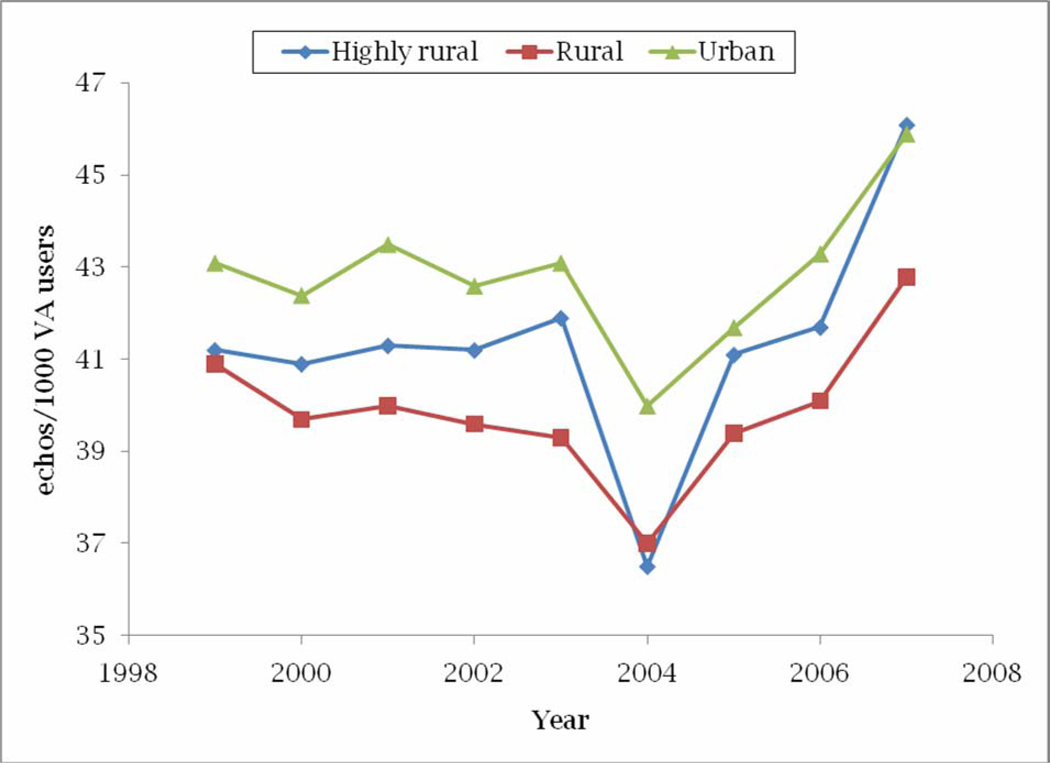
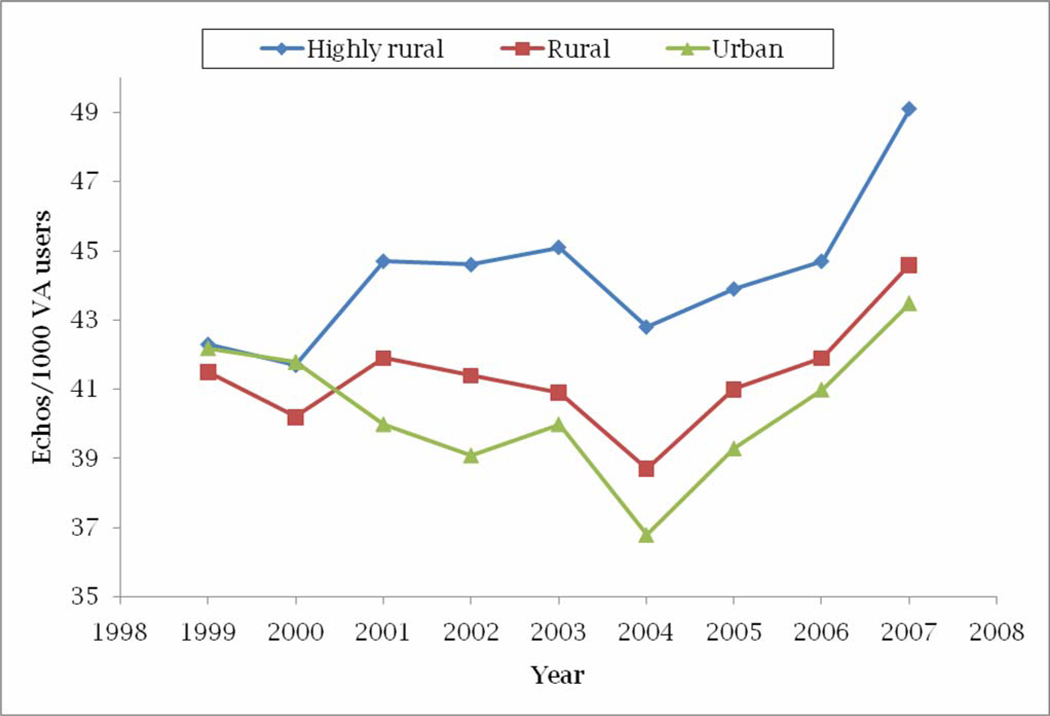
Echocardiography utilization in all 3 geographic regions declined between 1999 and 2003 and increased thereafter (Figure 1). In aggregate, between 1999 and 2007, unadjusted echocardiography utilization rates increased by 7.7% for veterans residing in urban areas, 1.7% for veterans residing in rural areas, and 6.2% for veterans in highly rural areas. Unadjusted echocardiography utilization was significantly lower for VA users living in rural and highly rural areas compared with VA users living in urban areas (59.1 echocardiograms per 1,000 VA users for rural vs 64.1 per 1,000 VA users for urban, RR 0.922, P < .0001; and 63.7 per 1,000 VA users for highly rural vs 64.1 per 1,000 VA users for urban, RR 0.993, P = .02). In analyses adjusting for patient demographics, comorbidity, and accounting for the clustering of patients within hospital networks, echocardiography utilization rates remained significantly lower for VA users living in rural and highly rural areas compared with VA users living in urban areas (40.1 for rural vs 43.1 for urban, RR 0.932, P < .0001; and 42.0 for highly rural vs 43.1 for urban, RR 0.976, P < .0001) (Table 3 and Figure 2). After additional adjustment for the distance to the nearest VAMC, echocardiography utilization rates were actually significantly higher for VA users living in rural and highly rural areas compared with VA users living in urban areas (Table 3 and Figure 3).
Figure 1.
Trends in unadjusted echocardiography utilization rates for VA users residing in urban, rural and highly rural areas from 1999 to 2007
Table 3.
Unadjusted and adjusted echocardiography utilization rates and rate ratios for urban, rural and highly rural VA users from 1999 to 2007
| Urban | Rural | Highly rural | ||||||
|---|---|---|---|---|---|---|---|---|
| Echo Ratea |
RR (95% CI) |
Echo rate* |
RR (95% CI) |
P Value (vs urban) |
Echo rate* |
RR (95% CI) |
P Value (vs urban) |
|
| Unadjusted | 64.1 | 1 (Ref) | 59.1 | 0.92 (0.92–0.93) | < .001 | 63.7 | 0.99 (0.99–1.00) | .02 |
| Adjustedb | 43.1 | 1 (Ref) | 40.1 | 0.93 (0.93–0.94) | < .001 | 42.0 | 0.98 (0.97–0.98) | < .001 |
| Adjustedc | 40.8 | 1 (Ref) | 41.8 | 1.03 (1.02–1.03) | < .001 | 44.9 | 1.10 (1.09–1.11) | < .001 |
Echocardiographs per 1,000 VA users per year.
Adjusted rate ratios derived using Poisson regression controlling for patient demographics (age, sex and race), VISN, VA priority and comorbid conditions (CHF, myocardial infarction, valvular heart disease, stroke, COPD, cardiac arrhythmias, diabetes, hypertension).
Adjusted rate ratios derived using Poisson regression controlling for patient demographics (age, sex and race), VISN, VA priority, comorbid conditions (CHF, myocardial infarction, valvular heart disease, stroke, COPD, cardiac arrhythmias, diabetes, hypertension) and distance to the nearest VAMC.
Figure 2.
Trends in adjusted* echocardiography utilization rates for VA users residing in urban, rural and highly rural areas from 1999 to 2007.
*Model adjusted for age, race, sex, VISN and comorbid conditions
Figure 3.
Trends in adjusted* echocardiography utilization rates for VA users residing in urban, rural and highly rural areas from 1999 to 2007.
*Model adjusted for age, race, sex, VISN, comorbid conditions and distance to nearest VAMC
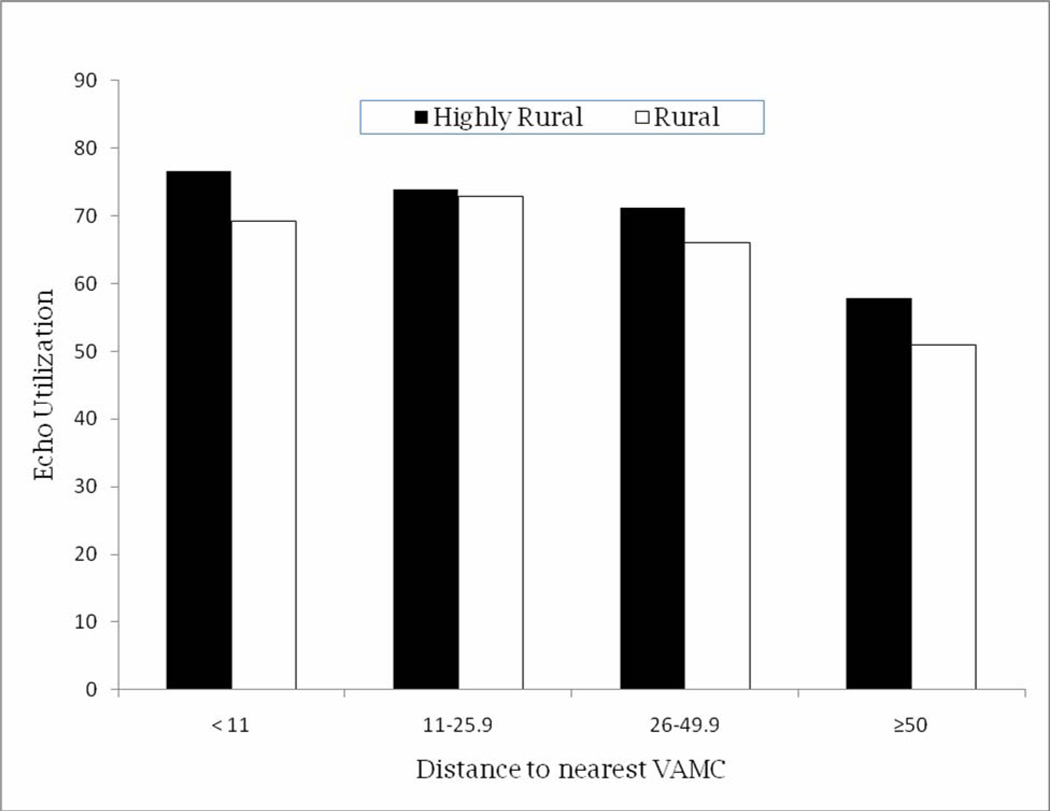
In analysis comparing unadjusted echocardiography utilization for highly rural and rural veterans residing at specific distance cut points from the nearest VAMC, we found echocardiography utilization among highly rural veterans decreasing linearly with increasing distance from the nearest VAMC until about 50 miles from the nearest VAMC. This was less true for rural veterans whose echocardiography utilization remained relatively constant. After distances greater than 50 miles from the nearest VAMC, however, echocardiography utilization drops suddenly compared to utilization at the preceding distance range (26–49.9 miles) for both highly rural and rural VA users (18.7% for highly rural VA users and 22.8% for rural VA users) (Figure 4).
Figure 4.
Echocardiography utilization for rural and highly rural veterans living at different distances from nearest VAMC.
Repeated testing was relatively low among VA users, with more than 90% of VA echocardiography recipients receiving one echocardiograph in a 12-month period. Among echocardiography recipients living in urban areas, an average of 91.2% received one echocardiogram over a 12-month period, 7.5% received 2 echocardiograms and 1.3% received 3 or more echocardiograms over a 12-month period. For recipients living in rural areas, 91.9% received one echocardiogram, while 6.9% received 2 echocardiograms and 1.2% received 3 or more echocardiograms over a 12-month period. Among echocardiogram recipients living in highly rural areas, 91.6% received one echocardiogram, 7.1% received 2 echocardiograms and 1.3% received 3 or more echocardiograms over a 12-month period.
In sensitivity analyses using more liberal criteria to identify VA users, results were similar.
DISCUSSION
In our analysis of national VA administrative data, we found that veterans residing in rural or highly rural areas had between 1.0% and 8.0% lower echocardiography utilization rates at VA facilities compared with their urban dwelling counterparts. These differences persisted after adjusting for patient demographics and comorbidity but were eliminated by additional adjustment for the distances patients lived from VAMCs. In aggregate, these results suggest that rural veterans receive fewer echocardiograms than their more urban counterparts and that the lower rate of echocardiography can be accounted for largely by the distance that rural patients live from VA medical centers which perform echocardiograms.
Our findings should be considered in the context of prior literature exploring health care access for rural and urban populations. Prior studies have found that rural patients have reduced access to an array of services including cancer screening, organ transplant, and other preventive services both in the private sector7–11,14,32,33 and the VA.34,35 Our findings, that after controlling for distance to the nearest facility performing echocardiograms, rural and highly rural veterans actually had higher echocardiography utilization rates than their urban counterparts, is important to consider. In particular, our results could be interpreted as showing that, aside from the distance that more rural veterans must travel, there are no particular patient factors (eg, reduced preference for diagnostic testing) or provider factors (eg, discrimination) underlying reduced echocardiogram use in rural veterans. Why might highly rural veterans actually have higher echocardiography utilization once distance is taken into account? One possible explanation is that highly rural veterans may have a higher “willingness to travel” to receive medical services relative to their urban counterparts since they are more accustomed to travelling long distances as part of their daily living.
Of note is the interesting finding that highly rural veterans have higher echocardiography utilization rates than their rural counterparts both before and after adjusting for distance. One possible explanation is as mentioned above, “willingness to travel.” Highly rural veterans may be more willing or more accustomed to travelling long distances to receive health care services compared to their rural counterparts. Another potential explanation is that VA outreach efforts targeting rural populations may improve access for highly rural veterans more effectively than rural veterans. In particular, it is possible that VA carpooling and van ridership programs effectively reach highly rural areas while bypassing rural areas. A third hypothesis is that rural veterans have greater access to non-VA services and thus may receive more of their echocardiography services from these sources compared with their counterparts from highly rural areas who may have limited choices for care outside of the VA system.
It is important to think more generally about the potential causes for reduced echocardiography utilization among rural residents. In their study examining utilization of colorectal cancer screening among rural and urban Americans, Coughlin et al14 argued that physician shortage in rural areas may partly explain the lower rates of screening in rural patients. Other studies have suggested differences in physician practice patterns,36 lower patient income,8 inadequate insurance coverage,37,38 and different patient demographics as contributing factors for rural-urban disparities in utilization of health services. Among veterans, factors such as lack of insurance are eliminated since eligible veterans receive care without regard for their health insurance. However, due to the regionalization of care delivery in the VA, there is a tendency for rural veterans to live at considerable distances from the nearest VAMC. Our current study therefore utilizes multivariate regression methods to control for some of these inherent differences between rural and urban veterans. In addition, our use of VA data controls for differences in insurance coverage between rural and urban veterans. Thus, our findings of higher echocardiography utilization in rural and highly rural veterans only in the analyses adjusting for distance to the nearest VAMC adds to the debate that increased travel distance reduces access and utilization of health care services.
This study provides a nationwide perspective of rural-urban echocardiography utilization by using nationally representative data, thus building on other studies of health services utilization that have concentrated on single regions or states.9,34,37,39–43 In addition, we used the RUCA taxonomy that provides a more nuanced definition of rurality and a stronger differentiation of rural areas according to their economic integration with urban and other rural areas, which ultimately has significant policy implications.
Finally, it is important to consider whether the differences in echocardiography utilization we observed represent overuse in urban populations or underuse in rural populations. There is growing concern that at a population level overuse of many diagnostic testing and imaging modalities is a greater problem than underuse.44 At the same time, it is well recognized that underuse and overuse can exist simultaneously.45 Further research in rural-urban disparities should attempt to better elucidate which of these factors is at play and whether underuse of particular diagnostic tests such as echocardiography has measureable adverse health consequences.
Our study has a number of limitations that are important to note. First, we relied on administrative data, thus limiting our ability to identify echocardiograms that were performed but not coded. Likewise, our reliance on administrative data limits our ability to identify the indications and/or appropriateness of echocardiograms, thereby limiting our ability to determine whether echocardiography utilization rates represent overuse in one rural category versus underuse in another. Second, echocardiograms performed outside the VA on VA users were not included in our analysis and thus we may underestimate echocardiography utilization to some degree for our entire population. Third, we lack data on differential utilization of VA services by eligible veterans in rural and urban areas. Our results could therefore potentially be biased one way or the other by differences in utilization of VA services by veterans without indication for echocardiography. Fourth, our study was conducted in the VA and generalizing our findings to the private sector should be done with caution. Finally, it is important to acknowledge that we measured distance using straight-line distance as opposed to actual driving distance. That said, prior research suggests that straight-line distance provides a reasonable approximation for most applications.46
In conclusion, we found that between 1999 and 2007, echocardiography utilization among rural VA users was slightly lower than among urban VA users. However, after accounting for distance, there was no longer any evidence of lower echocardiogram use among rural veterans, suggesting that the reduced utilization seen in rural veterans could be largely accounted for by distance and not other factors. These results underscore the need for policy makers to strategically position certain key diagnostic services, such as echocardiography, so that they are at reasonable distances from rural communities. In some cases, this might require providing echocardiography services at CBOCs or subcontracting to other local facilities. In addition, VA carpooling and van ridership programs should be targeting more rural areas.
Acknowledgments
Dr. Okrah received fellowship stipend and tuition support from the Cardiovascular Interdisciplinary Research Training Grant, Iowa Cardiovascular Center, University of Iowa Carver College of Medicine. Dr. Cram has an appointment in the Center for Comprehensive Access and Delivery Research and Evaluation (CADRE) at the Iowa City VA Medical Center, which is funded through the Department of Veterans Affairs, Veterans Health Administration, Health Services Research and Development Service. Dr. Cram is supported by a K23 career development award (RR01997201) from the NCRR at the NIH and the Robert Wood Johnson Physician Faculty Scholars Program. Dr. Kaboli has an appointment in the VA Office of Rural Health (ORH), Veterans Rural Health Resource Center-Central Region at the Iowa City VA Medical Center, which is funded through the Department of Veterans Affairs, Veterans Health Administration, Office of Rural Health.
REFERENCES
- 1.U.S. Department of Transportation. [Accessed May 6, 2010];Census 2000 Population Statistics: U.S. Population Living in Urban vs. Rural Areas. Available at: http://www.fhwa.dot.gov/planning/census/cps2k.htm.
- 2.U.S. Census Bureau. [Accessed May 6, 2010];Urban/Rural and Metropolitan/Nonmetropilitan Population. 2000 Available at: http://factfinder.census.gov/servlet/GCTTable?.
- 3.Pearson TA, Lewis C. Rural epidemiology: insights from a rural population laboratory. Am J Epidemiol. 1998;148:949–957. doi: 10.1093/oxfordjournals.aje.a009571. [DOI] [PubMed] [Google Scholar]
- 4.Ruland S, Gorelick PB, Schneck M, Kim D, Moore CG, Leurgans S. Acute stroke care in Illinois: a statewide assessment of diagnostic and treatment capabilities. Stroke. 2002;33:1334–1339. doi: 10.1161/01.str.0000014609.44258.ad. [DOI] [PubMed] [Google Scholar]
- 5.Federal Register. Medicare rural hospital flexibility program regulations. Washington, DC: U S Government Printing Office; 1997. [Google Scholar]
- 6.National Health Service Corps. [Accessed May 7, 2010]; Available at: http://nhsc.bhpr.hrsa.gov/loanrepayment/.
- 7.Axelrod DA, Guidinger MK, Finlayson S, et al. Rates of solid-organ wait-listing, transplantation, and survival among residents of rural and urban areas. JAMA. 2008;299:202–207. doi: 10.1001/jama.2007.50. [DOI] [PubMed] [Google Scholar]
- 8.Larson S, Correa-de-Araujo R. Preventive health examinations: a comparison along the rural-urban continuum. Womens Health Issues. 2006;16:80–88. doi: 10.1016/j.whi.2006.03.001. [DOI] [PubMed] [Google Scholar]
- 9.Gessert CE, Haller IV, Kane RL, Degenholtz H. Rural-urban differences in medical care for nursing home residents with severe dementia at the end of life. J Am Geriatr Soc. 2006;54:1199–1205. doi: 10.1111/j.1532-5415.2006.00824.x. [DOI] [PubMed] [Google Scholar]
- 10.Larson SL, Fleishman JA. Rural-urban differences in usual source of care and ambulatory service use: analyses of national data using Urban Influence Codes. Med Care. 2003;41:III65–III74. doi: 10.1097/01.MLR.0000076053.28108.F2. [DOI] [PubMed] [Google Scholar]
- 11.Doescher MP, Jackson JE. Trends in cervical and breast cancer screening practices among women in rural and urban areas of the United States. J Public Health Manag Pract. 2009;15:200–209. doi: 10.1097/PHH.0b013e3181a117da. [DOI] [PubMed] [Google Scholar]
- 12.Abrams TE, Vaughan-Sarrazin M, Kaboli PJ. Mortality and Revascularization Following Admission for Acute Myocardial Infarction: Implication for Rural Veterans. J Rural Health. 2010;26:310–317. doi: 10.1111/j.1748-0361.2010.00318.x. [DOI] [PubMed] [Google Scholar]
- 13.Rhoades JA, Brown EJ, Vistnes JP. Research Findings #11: Health Insurance Status of the Civilian Noninstitutionalized Population, 1998. Rockville, MD: AHRQ; 2000. Apr, [Accessed May 26, 2010]. Available at: http://www.meps.ahrq.gov/data_files/publications/rf11/rf11.shtml. [Google Scholar]
- 14.Coughlin SS, Thompson TD. Colorectal cancer screening practices among men and women in rural and nonrural areas of the United States, 1999. J Rural Health. 2004;20:118–124. doi: 10.1111/j.1748-0361.2004.tb00017.x. [DOI] [PubMed] [Google Scholar]
- 15.Larson SL, Hill SC. Rural-urban differences in employment-related health insurance. J Rural Health. 2005;21:21–30. doi: 10.1111/j.1748-0361.2005.tb00058.x. [DOI] [PubMed] [Google Scholar]
- 16.Lu N, Samuels ME, Kletke PR, Whitler ET. Rural-urban differences in health insurance coverage and patterns among working-age adults in Kentucky. J Rural Health. 2010;26:129–138. doi: 10.1111/j.1748-0361.2010.00274.x. [DOI] [PubMed] [Google Scholar]
- 17.Rabinowitz HK, Diamond JJ, Markham FW, Paynter NP. Critical factors for designing programs to increase the supply and retention of rural primary care physicians. JAMA. 2001;286:1041–1048. doi: 10.1001/jama.286.9.1041. [DOI] [PubMed] [Google Scholar]
- 18.Department of Veterans Affairs. Veterans Health Administration. Office of Rural Health. Strategic Plan, 2010–2014. Washington, DC: Department of Veterans Affairs; 2010. [Accessed April 1, 2011]. Available at: http://www.ruralhealth.va.gov/docs/VHA_ORH_StrategicPlan2010_2014.pdf. [Google Scholar]
- 19.Krishnamoorthy VK, Sengupta PP, Gentile F, Khandheria BK. History of echocardiography and its future applications in medicine. Crit Care Med. 2007;35:S309–S313. doi: 10.1097/01.CCM.0000270240.97375.DE. [DOI] [PubMed] [Google Scholar]
- 20.Cheitlin MD, Armstrong WF, Aurigemma GP, et al. ACC/AHA/ASE 2003 Guideline Update for the Clinical Application of Echocardiography: summary article. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (ACC/AHA/ASE Committee to Update the 1997 Guidelines for the Clinical Application of Echocardiography) J Am Soc Echocardiogr. 2003;16:1091–1110. doi: 10.1016/S0894-7317(03)00685-0. [DOI] [PubMed] [Google Scholar]
- 21. [Accessed May 24, 2010];Joint Commission for Accreditation of Healthcare Organizations— Performance Measures. Available at: http://www.jcaho.org/pms/core+measures/cr_hos_cm.htm.
- 22.Zhu SC, Gardner JA, Hendricks A. Heath Care Financing and Economics Data Brief #2004–10. 2004. Boston, MA: VA Boston Health Care System Research and Development; 2004. How many enrollees come to VA just for pharmacy? [Google Scholar]
- 23.Wright SM, Petersen LA, Lamkin RP, Daley J. Increasing use of Medicare services by veterans with acute myocardial infarction. Med Care. 1999;37:529–537. doi: 10.1097/00005650-199906000-00002. [DOI] [PubMed] [Google Scholar]
- 24.Hall SA, Kaufman JS, Ricketts TC. Defining urban and rural areas in U.S. epidemiologic studies. J Urban Health. 2006;83:162–175. doi: 10.1007/s11524-005-9016-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Economic Research Service USDA. [Accessed May 27, 2010];ERS/USDA Briefing Room-Measuring Rurality: Urban Influence Codes. Available at: http://www.census.gov/geo/www/ua/ua_2k.html.
- 26.U.S. Department of Agriculture, Economic Research Service. [Accessed May 27, 2010];ERS/USDA Briefing Room: Measuring Rurality: Rural-Urban Commuting Area Codes. Available at: http://www.ers.usda.gov/briefing/Rurality/RuralUrbanCommutingAreas/
- 27.WWAMI Rural Health Research Center. [Accessed February 1, 2010];Rural-Urban Commuting Area Codes, Version 2.0. Available at: http://depts.washington.edu/uwruca/ruca-codes.php.
- 28.Baldwin LM, Cai Y, Larson EH, et al. Access to cancer services for rural colorectal cancer patients. J Rural Health. 2008;24:390–399. doi: 10.1111/j.1748-0361.2008.00186.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.WWAMI Rural Health Research Center. [Accessed February 1, 2010];Zip Code RUCA Approximation. Available at: http://depts.washington.edu/uwruca/ruca-approx.php.
- 30.Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43:1130–1139. doi: 10.1097/01.mlr.0000182534.19832.83. [DOI] [PubMed] [Google Scholar]
- 31.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36:8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 32.Baldwin LM, MacLehose RF, Hart LG, Beaver SK, Every N, Chan L. Quality of care for acute myocardial infarction in rural and urban US hospitals. J Rural Health. 2004;20:99–108. doi: 10.1111/j.1748-0361.2004.tb00015.x. [DOI] [PubMed] [Google Scholar]
- 33.Casey MM, Thiede Call K, Klingner JM. Are rural residents less likely to obtain recommended preventive healthcare services? Am J Prev Med. 2001;21:182–188. doi: 10.1016/s0749-3797(01)00349-x. [DOI] [PubMed] [Google Scholar]
- 34.Weeks WB, Bott DM, Lamkin RP, Wright SM. Veterans Health Administration and Medicare outpatient health care utilization by older rural and urban New England veterans. J Rural Health. 2005;21:167–171. doi: 10.1111/j.1748-0361.2005.tb00077.x. [DOI] [PubMed] [Google Scholar]
- 35.Weeks WB, Mahar PJ, Wright SM. Utilization of VA and Medicare services by Medicare-eligible veterans: the impact of additional access points in a rural setting. J Healthc Manag. 2005;50:95–106. discussion 106–107. [PubMed] [Google Scholar]
- 36.Carr WP, Maldonado G, Leonard PR, et al. Mammogram utilization among farm women. J Rural Health. 1996;12:278–290. doi: 10.1111/j.1748-0361.1996.tb00817.x. [DOI] [PubMed] [Google Scholar]
- 37.Borders TF, Rohrer JE, Hilsenrath PE, Ward MM. Why rural residents migrate for family physician care. J Rural Health. 2000;16:337–348. doi: 10.1111/j.1748-0361.2000.tb00484.x. [DOI] [PubMed] [Google Scholar]
- 38.Frenzen PD. Health insurance coverage in U.S. urban and rural areas. J Rural Health. 1993;9:204–214. doi: 10.1111/j.1748-0361.1993.tb00514.x. [DOI] [PubMed] [Google Scholar]
- 39.Chan L, Hart LG, Goodman DC. Geographic access to health care for rural Medicare beneficiaries. J Rural Health. 2006;22:140–146. doi: 10.1111/j.1748-0361.2006.00022.x. [DOI] [PubMed] [Google Scholar]
- 40.Nemet GF, Bailey AJ. Distance and health care utilization among the rural elderly. Soc Sci Med. 2000;50:1197–1208. doi: 10.1016/s0277-9536(99)00365-2. [DOI] [PubMed] [Google Scholar]
- 41.Liff JM, Chow WH, Greenberg RS. Rural-urban differences in stage at diagnosis. Possible relationship to cancer screening. Cancer. 1991;67:1454–1459. doi: 10.1002/1097-0142(19910301)67:5<1454::aid-cncr2820670533>3.0.co;2-k. [DOI] [PubMed] [Google Scholar]
- 42.Flynn BS, Gavin P, Worden JK, Ashikaga T, Gautam S, Carpenter J. Community education programs to promote mammography participation in rural New York State. Prev Med. 1997;26:102–108. doi: 10.1006/pmed.1997.0110. [DOI] [PubMed] [Google Scholar]
- 43.Jonk YC, Call KT, Cutting AH, O'Connor H, Bansiya V, Harrison K. Health care coverage and access to care: the status of Minnesota's veterans. Med Care. 2005;43:769–774. doi: 10.1097/01.mlr.0000170403.97264.39. [DOI] [PubMed] [Google Scholar]
- 44.Smith-Bindman R, Miglioretti DL, Larson EB. Rising use of diagnostic medical imaging in a large integrated health system. Health Aff (Millwood) 2008;27:1491–1502. doi: 10.1377/hlthaff.27.6.1491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Institute of Medicine. [Accessed June 21, 2010];Crossing the Quality Chasm: A New Health System for the 21st Century. Available at: http://www.nap.edu/html/quality_chasm/reportbrief.pdf.
- 46.Phibbs CS, Luft HS. Correlation of travel time on roads versus straight line distance. Med Care Res Rev. 1995;52:532–542. doi: 10.1177/107755879505200406. [DOI] [PubMed] [Google Scholar]