Abstract
A US national sample of 20,962 participants (57% women, 44% blacks) from the Reasons for Geographic and Racial Differences in Stroke (REGARDS) study provided general population estimates for ECG abnormalities among black and white men and women. Participants were recruited during 2003–2007 by random selection from a commercially available nationwide list, with oversampling of blacks and persons from the stroke belt for a cooperation rate of 49%. Measurement of risk factors and 12-lead ECGs (centrally coded using Minnesota Code criteria) showed 28% had at least one major ECG abnormality. Prevalence of abnormalities was higher (35%+) for those 65 years and older with no differences between blacks and whites. However, among men less than 65 years, blacks had more major abnormalities than whites, most notably for atrial fibrillation, major Q waves and left ventricular hypertrophy (LVH). Men generally had more ECG abnormalities than women. The most common ECG abnormalities were T-wave abnormalities. Average heart rate corrected QT interval was longer in women than men, similar in whites and blacks and increased with age, whereas the average heart rate was higher in women than men and in blacks than whites and decreased with age. The prevalence of ECG abnormalities was related to hypertension, diabetes, blood pressure level and age. In conclusion, black men and women in the US have a significantly higher prevalence of ECG abnormalities than whites at ages 45–64 but these proportions, although larger, tend to equalize or reverse after age 65.
Keywords: ECG abnormalities, prevalence, black/white
INTRODUCTION
No published data exist of the prevalence of ECG abnormalities from national samples of black and white Americans beyond The National Health and Nutrition Examination Survey (NHANES) reports. The first of these was a sample of 25 to 74 year old Americans from the 1971–1975 Health and Nutrition Study (HANES I) survey 1 of 6,913 persons with recorded ECGs. Only simple frequencies of ECG abnormalities are given without age, race or sex stratification. Some continuous measurements are given without heart rate correction and the abnormalities listed do not have precise definitions as in the Minnesota Code which is the primary ECG classification system for electrocardiographic findings and abnormalities in clinical trials and epidemiologic studies 2. The only other ECG recordings on a national sample of the US was made for NHANES III (1988–1994) and was only for 6,286 white and 2,041 black persons 40 years of age and over. The totality of these data has not been published but is available in reports of the US Department of Health and Human Services 3. Only the white prevalences, unstratified, by race and sex, have been published in a recent paper comparing US white and Taiwanese Chinese populations 4. These reports of ECG abnormalities lack subgroup specificity and associations with relevant demographic and clinical variables. Here we characterize the full range of ECG findings and abnormalities among a national sample of 20,962 black and white men and women from The Reasons For Geographic and Racial Differences In Stroke (REGARDS) study and assess the impact of adjustment for confounding clinical and demographic modifiers on observed differences.
METHODS
The REGARDS study is a national, population-based longitudinal study evaluating causes of racial and regional differences in stroke mortality. The objectives and methods of the study have been published elsewhere.5 Briefly, between January 2003 and October 2007 30,239 black and white men and women aged ≥45 years were recruited by random selection of names/addresses from a commercially available nationwide list (Genesys Inc., Daly City, CA), with a 49% cooperation rate.6 The final sample comprised 21% from the stroke buckle (coastal plain of North Carolina, South Carolina, and Georgia), 35% from rest of the stroke belt area (the remainder of North Carolina, South Carolina, and Georgia, and Tennessee, Mississippi, Alabama, Louisiana, and Arkansas, 44% from the other 40 contiguous states, and 42% black, 55% women. Demographic information and medical history were obtained by telephone interview. A brief physical examination was conducted 3 to 4 weeks after the telephone interview, including standardized measurements of risk factors, collection of blood and urine, and recording of resting ECG
The ECG recording in REGARDS was initially incorporated only to diagnose atrial fibrillation, one of the major risk factors for stroke. Hence, the first 8,432 REGARDS participants underwent 7-lead ECG recording acquired by applying the standard 4 limb electrodes and a mid-sternal electrode. However, during the course of the study, it was determined that a 12-lead ECG should (and could) be recorded. Therefore, the remaining REGARDS participants (n = 21,071) underwent a standard 12-lead-ECG recording. The change in the ECG protocol and the broadening of the age eligibility to include those aged 45 to 54 occurred at approximately the same time. All ECGs were read centrally at the EPICARE center located at Wake Forest School of Medicine, where the ECGs were coded by trained MD electrocardiographers and all abnormalities over-read by a second MD electrocardiographer. For the purpose of this analysis we excluded all participants without a 12-lead ECG and those without readable ECGs. This left 20,962 ECGs for the present analysis. The ECG variables include all ECG Minnesota codes (MC) with codes 1 through 9 7 and continuous ECG variables: heart rate, QRS duration, QT duration (and QTI: ([QT]/656 * ([HR] + 100), RaVL, SV1 and SV3. Major abnormalities (Appendix table 2) include: ventricular conduction defects (MC 7.1.7.2, 7.4, 7.8), major Q waves (MC1.1, 1.2: all at least ≥.03 sec duration), minor Q waves plus STT abnormalities (MC 1.3 + 4.1 or 4.2 or 5.1 or 5.2), major isolated STT abnormalities (MC 4.1 or 4.2 all with STJ at least 0.5 mm depressed with a horizontal or downward sloping ST segment; or 5.1 or 5.2: at least 1 mm T wave inversion)), left ventricular hypertrophy plus major STT abnormalities (MC 3.1 + 4.1 or 4.2 or 5.1 or 5.2), atrial fibrillation or flutter (MC 8.3), major AV conduction abnormalities (MC 6.1, 6.2, 6.4), other major arrhythmias (MC 8.2,8.4), artificial pacemaker (MC 6.8), and major QT prolongation (QTI≥116).
For national prevalence estimates reflecting the sampling design of REGARDS, SAS-callable SUDAAN 8 was used to perform all statistical analyses with sampling weights. The sampling weights were obtained using a post-stratification method. There were 108 strata based on region, race, sex, and age groups. The national population was based on the 2000 census and obtained through the Centers for Disease Control and Prevention (CDC) Wonder website. National population estimates by strata and REGARDS population by strata were obtained to create selection probabilities. Sampling weights were then obtained by taking the inverse of the selection probability.
Population weighted means and proportions were obtained to describe the distributions of continuous ECG variables and categorical variables, respectively. Logistic regressions were used to assess associations between risk factors and demographic traits with the outcome. Simple models were adjusted for demographic factors such as age, race and sex. Full models took into account major risk factors as well as socioeconomic factors. After producing the weights, we were able to recreate the national population estimates using these weights.
RESULTS
The national weighted mean age of the study sample was 59 years (56 years for black men [BM], 58 for black women [BW], 61 for white women [WW] and 58 for white men [WM]). Clinical measurements of blood pressure, body mass index (BMI) and serum lipid levels together with histories of diabetes, hypertension and treatment for hyperlipidemia are given in Table 1. Smoking rates and blood levels of LDL, and HDL cholesterol and triglycerides differed between groups as did treatment for hyperlipidemia and hypertension.
Table 1.
Demographic and clinical risk factors of the participants
| Total (N=20,962) | White Men (n=5052) | Black Men (n=2760) | White Women (n=7317) | Black Women (n=5833) |
|---|---|---|---|---|
| Age (years*) | 57.7 (0.04) | 55.7(0.05) | 61.0(0.03) | 58.1(0.03) |
| Systolic blood pressure, (mm Hg) | 123.6(0.40) | 129.5(0.56) | 120.9(0.33) | 127.2(0.35) |
| Body mass index (kg/m2) | 28.5(0.16) | 29.2(0.19) | 28.2(0.13) | 32.0(0.16) |
| Low density lipoprotein-cholesterol (mg/dL) | 113.6 (0.97) | 114.5(1.26) | 114.9(0.68) | 118.0(0.73) |
| High density lipoprotein-cholesterol (,mg/dL) | 45.0(0.37) | 48.8(0.52) | 58.0(0.33) | 56.5(0.31) |
| Triglycerides (mg/dL) | 148.7(3.60) | 119.1(2.36) | 134.2(1.77) | 105.6(1.21) |
| Diabetes mellitus | 885(13.3%) | 795(24.0%) | 904(9.8%) | 1669(23.9%) |
| Current Smoker | 641(13.7%) | 574(26.9%) | 943(13.5%) | 901(19.8%) |
| Treated for Hypertension† | 2690(36.9%) | 1748(50.4%) | 3620(40.7%) | 3978(59.1%) |
| Treated for Hyperlipidemia‡ | 1968(27.2%) | 817(22.2%) | 2052(22.7%) | 1680(22.1%) |
Weighted Means (standard error) unless otherwise indicated
Any lipid lowering medication
Any antihypertensive medication (diuretic, ace-inhibitor, beta-blocker, calcium-channel blocker, angiotensin converting enzyme inhibitor, alpha-blocker)
In Table 2 weighted means and standard errors are given for selected continuous measures of ECG variables with independent prognostic value. Each of the 4 race/sex groups are divided into age groups above and below 65 years. QRS duration increases with age and is longer in men than women and in whites than blacks. QTc and QTI, both heart rate-corrected measures of QT interval, increase with age and are longer in women than men and are similar in blacks and whites. Heart rate is also higher in women than men but decreases with age and is higher in blacks than whites.
Table 2.
Continuous ECG characteristics for the study cohort†.
| White | Black | |||||||
|---|---|---|---|---|---|---|---|---|
| Male < 65 yr 2394 |
Male≥65 yr 2658 |
Female<65yr 3909 |
Female≥65yr 3408 |
Male < 65 yr 1592 |
Male≥65 yr 1168 |
Female<65yr 3361 |
Female≥65yr 2472 |
|
| QRS duration | 88.7(0.5) | 96.2(0.6) | 84.0(0.3) | 87.1(0.5) | 86.7(0.51) | 91.1(0.7) | 82.5(0.2) | 86.4(0.4) |
| QTC | 406.0(0.8) | 414.7(0.8) | 415.4(0.6) | 418.3(0.8) | 409.0(1.1) | 413.4(1.00) | 417(0.6) | 418.5(0.7) |
| QTI | 98.7(0.2) | 101.0(0.2) | 100.4(0.1) | 101.3(0.2) | 98.8(0.2) | 100.2(0.2) | 100.6(0.1) | 101.1(0.2) |
| Heart Rate | 64.2(0.4) | 63.1(0.3) | 67.0(0.3) | 65.9(0.3) | 68.1(0.5) | 66.2(0.4) | 69.7(0.3) | 68.0(0.3) |
Weighted mean (standard error)
The prevalence of extant ECG abnormalities, are displayed in Table 3 and the significant age/race/sex associations of each of the abnormalities is given in Appendix table 1). Of the total population 28.2% had at least one major ECG abnormality, the prevalence of which was greater in those over 65 (p<0.0001) (37% in black and white men; 35.7% in WW and 34.9% in BW). Among those less than 65 years women had more abnormalities than men among whites (25.4% vs. 23.2%) and these were greater among blacks where the sex proportions were more nearly equal for women and men (28.4% vs. 28.8% respectively). Major Q waves were present in 11.2 % of the population with the highest proportion (20.4%) among WM over the age of 65 years p<0.0001); and major Q waves more common in blacks than whites under the age of 65 years. The most common abnormalities overall were minor T wave abnormalities (20.4%) and the most common major abnormality also was T wave abnormalities (19.1%). Left ventricular hypertrophy (LVH), by Cornell voltage, was 7.4% overall and was more common in women than men (p<0.0001) and much more in blacks than whites (p<0.0001), reaching 19.9% in BW. Bundle branch block (BBB) was most common in white men older than 65 years (p<0.0001): 17.1% (any MC 7 code). More persons had right BBB (2.7%) than had left BBB (1.2%). Atrial fibrillation (AF) was present in 1.2% of the population with increased levels above age 65 and the highest proportion in men over the age of 65 years; blacks had lower prevalence than whites except for BM less than 65 years (1.0%) who were twice as likely to have AF as white men under 65 years (0.4%). Atrial premature beats were more common in blacks than whites and more common in men than women. Overall, atrial premature beats were more common than were ventricular premature beats (5.8% vs. 3.5%).
Table 3.
Weighted* analysis of ECG abnormalities: Percentage of US population with specific abnormalities by race, sex and age group.
| % | White (12,369, 59%) | Black (8,593, 41%) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | 20962 | Male<65yr 2394 |
Male≥65yr 2658 |
Female<65yr 3909 |
Female≥65yr 3408 |
Male<65yr 1592 |
Male≥65yr 1168 |
Female<65yr 3361 |
Female≥65yr 2472 |
||
| Major Q Wave abnormalities (MC∫1.1,1.2) | 2738 | 11.2 | 11.6 | 20.4 | 6.9 | 14.4 | 12.1 | 17.6 | 7.8 | 13.8 | |
| Minor Q Wave abnormalities (MC 1.3) | 873 | 4.1 | 3.0 | 3.9 | 3.3 | 7.1 | 4.8 | 5.6 | 4.2 | 8.5 | |
| Major ST segment depression (MC 4.1, 4.2) | 1952 | 6.8 | 4.9 | 9.6 | 4.7 | 10.6 | 9.3 | 16.5 | 7.0 | 15.0 | |
| Minor ST segment depression (MC 4.2,4.4) | 2173 | 8.0 | 5.7 | 10.4 | 6.1 | 12.0 | 9.7 | 16.7 | 8.6 | 16.2 | |
| Major T Wave abnormalities (MC 5.1,5.2) | 5234 | 19.1 | 11.3 | 24.3 | 16.8 | 29.7 | 21.4 | 33.5 | 21.4 | 34.4 | |
| Minor T Wave abnormalities (MC 5.3,5.4) | 5571 | 20.4 | 11.4 | 25.3 | 18.6 | 32.4 | 21.2 | 34.0 | 22.9 | 36.1 | |
| ANY Q waves | 3611 | 14.9 | 14.3 | 23.4 | 9.9 | 20.5 | 16.3 | 22.2 | 11.6 | 21.1 | |
| ANY ST Segment depression | 2192 | 8.1 | 5.8 | 10.6 | 6.2 | 12.2 | 9.7 | 16.7 | 8.6 | 16.3 | |
| ANY T Wave abnormalities | 5771 | 22.6 | 12.0 | 25.6 | 20.6 | 33.3 | 21.7 | 34.2 | 24.5 | 37.5 | |
| ST Segment elevation in inferior leads (MC 9.2) | 15 | 0.02 | 0 | 0.07 | 0.01 | 0 | 0.07 | 0.12 | 0.19 | 0.05 | |
| ST Segment elevation in lateral leads (MC 9.2) | 16 | 0.08 | 0.18 | 0 | 0 | 0 | 0.57 | 0.17 | 0 | 0.01 | |
| ST segment elevation in anterior leads (MC 9.2) | 161 | 0.72 | 1.3 | 0.4 | 0.01 | 0.05 | 6.3 | 1.9 | 0.5 | 0.3 | |
| LVH** | 2197 | 7.4 | 3.5 | 10.7 | 4.7 | 14.7 | 9.0 | 14.9 | 9.2 | 19.9 | |
| Tall R waves | MC 3.1 or 3.3 | 1665 | 5.2 | 4.9 | 4.5 | 3.3 | 4.8 | 15.6 | 11.4 | 10.0 | 13.7 |
| MC3.1 | 1324 | 4.1 | 3.6 | 4.1 | 2.6 | 4.1 | 10.7 | 9.7 | 7.3 | 11.1 | |
| MC3.3 | 341 | 1.2 | 1.2 | 0.4 | 0.8 | 0.7 | 4.8 | 1.8 | 2.7 | 2.6 | |
| A-V Conduction Abnormalities | 998 | 3.9 | 2.6 | 14.9 | 1.0 | 5.8 | 3.6 | 12.2 | 1.6 | 4.4 | |
| Any Bundle Branch Block (MC 7.) | 1667 | 7.4 | 6.9 | 17.1 | 4.4 | 10.1 | 6.6 | 11.0 | 2.6 | 8.4 | |
| Complete Left Bundle Branch Block (MC 7.1) | 293 | 1.2 | 0.3 | 2.7 | 0.6 | 3.1 | 0.4 | 1.1 | 0.3 | 2.4 | |
| Complete Right BBB (MC 7.2) | 726 | 2.7 | 2.8 | 9.4 | 0.6 | 3.8 | 1.8 | 7.4 | 0.7 | 4.4 | |
| Incomplete Right Bundle Branch Block (MC 7.3) | 508 | 2.8 | 3.2 | 2.7 | 3.1 | 2.3 | 4.0 | 1.1 | 1.5 | 1.3 | |
| Non-Specific Intraventricular BBB(MC 7.4) | 140 | 0.6 | 0.6 | 2.3 | 0.1 | 0.9 | 0.5 | 1.3 | 0.1 | 0.4 | |
| Atrial and Ventricular Premature Beats (MC 8.1) | 2633 | 10.2 | 7.4 | 19.7 | 6.7 | 16.2 | 9.4 | 22.1 | 8.1 | 18.1 | |
| Atrial or Junctional Premature Beats (MC 8.1.1) | 1449 | 5.8 | 4.6 | 10.2 | 3.8 | 9.2 | 5.7 | 12.9 | 4.1 | 9.7 | |
| Ventricular Premature Beats (MC 8.1.2) | 922 | 3.5 | 2.3 | 7.0 | 2.5 | 5.5 | 2.7 | 5.9 | 3.5 | 6.1 | |
| Both atrial and ventricular Premature beats (MC 8.1.3) | 252 | 0.9 | 0.5 | 2.4 | 0.5 | 1.4 | 1.0 | 3.3 | 0.5 | 2.3 | |
| Atrial Fibrillation (MC 8.3) | 277 | 1.2 | 0.4 | 5.2 | 0.2 | 2.6 | 1.0 | 1.8 | 0.02 | 1.0 | |
| Supraventricular rhythm (MC 8.4) | 116 | 0.4 | 0.2 | 0.9 | 0.2 | 0.7 | 0.2 | 0.7 | 0.4 | 0.7 | |
| Low Voltage QRS (MC 9.1) | 1401 | 7.3 | 3.8 | 4.0 | 11.6 | 8.1 | 2.2 | 2.5 | 6.7 | 6.2 | |
| Tall P Waves (MC 9.3) | 89 | 0.4 | 0.3 | 0.2 | 0.5 | 0.3 | 1.1 | 0.6 | 0.9 | 0.5 | |
| Total Major Abnormalities† | 6790 | 28.2 | 23.2 | 37.1 | 25.4 | 35.7 | 28.8 | 37.4 | 28.4 | 34.9 | |
Weighted to reflect the national population using SUDAAN 15
MC = Minnesota Code
LVH, left ventricular hypertrophy) is by Cornell Voltage (Ravl+SV3) >2800μV for men and >2200μV for women.
Major abnormalities include: ventricular conduction defects (MC 7.1.7.2, 7.4, 7.8); major Q waves (MC1.1, 1.2); minor Q waves plus STT abnormalities (MC 1.3 + 4.1 or 4.2 or 5.1 or 5.2);major isolated STT abnormalities (MC 4.1 or 4.2 or 5.1 or 5.2); left ventricular hypertrophy plus major STT abnormalities (MC 3.1 + 4.1 or 4.2 or 5.1 or 5.2); atrial fibrillation or flutter (MC 8.3); major AV conduction abnormalities (MC 6.1, 6.2, 6.4, 6.8,); Mother major arrhythmias (MC 8.2,8.4); artificial pacemaker (MC 6.8); Major QT prolongation (QTI≥116).
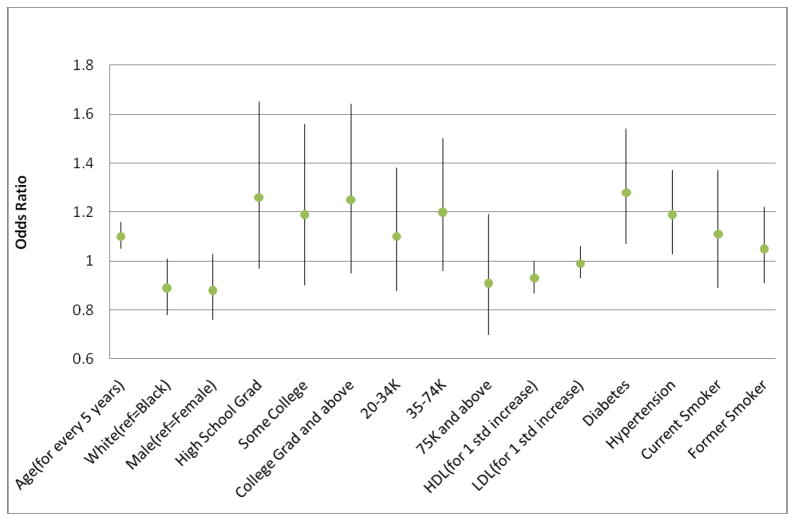
Demographic and clinical variable associations with the presence of major ECG abnormalities are shown in the forest plot of figure 1: Significant independent increased odds ratios (OR) are shown for each 5 year increase in age (OR 1.22, 95% confidence interval [CI] 1.16, 1.28), presence of hypertension (OR 1.35, 95% CI 1.18,1.55) and diabetes (OR 1.52, 95% CI 1.28,1.82). Raised HDL cholesterol significantly reduced the risk (OR 0.91, 95% CI 0.85,0.98) and systolic BP increased the risk (Appendix Table 3).
Figure 1.
Independent associations (odds ratios) of demographic and clinical variables with prevalence of major ECG abnormalities:
DISCUSSION
This study provides prevalence estimates for major and minor ECG abnormalities for blacks and whites in the US by ages above and below 65 years for men and women separately. The presence of ECG abnormalities is high in US middle aged and older adults. Black men and women in the US have significantly higher prevalence of ECG abnormalities than whites at ages 45 to 64 but these proportions, although larger, tend to equalize or reverse in relation to whites over the age of 65. The race and sex differences for the presence of major ECG abnormalities were removed after adjustment for systolic blood pressure, history of hypertension and diabetes, age and HDL cholesterol.
Descriptions of the differences in the prevalence of specific ECG findings between US blacks and whites began with limited and regional studies in Evans County Georgia 9, where 53% of 308 blacks and 31 % of 511 whites were found to have any ECG abnormalities. And later, in Charleston In 1960 in South Carolina 10 1,394 white and 787 black men and women were examined with only 8-lead ECG recordings. Minnesota coding was performed at a later date for the men only and revealed almost double the proportion of minor and major ECG abnormalities in black than white men. Another study of a southern urban population showed differences in black and white ECG abnormalities also 11.
Later, more descriptions with detailed Minnesota coding of ECG findings appeared for more than 10,000 black and white men and women in the Hypertension Detection and Follow-up Program 12 with specific abnormalities tabulated by age race and sex and showed generally that black men had the greatest proportion of abnormalities present. This was a cohort of hypertensive persons of whom 79% had an ECG abnormality.
Among healthy biracial cohorts of US populations, reports of specific ECG variables and Minnesota codes began to appear for larger numbers of men and women from particular regional epidemiologic cohort studies of cardiovascular disease where standard 12 lead ECGs had been recorded. Specifically, in the Atherosclerosis Risk in Communities study (ARIC) for a cohort of average age 51 years, comprising 493 black and 2,193 white men and women free of cardiovascular disease, among men 46 % of African Americans men but only 24 % of whites had minor ECG abnormalities and in women the prevalence among blacks was 32% vs. 23 % 13. However, in this study the majority of the African Americans were from only one of the four clinical centers of the study (Jackson Mississippi), and as such it is not clear whether racial differences are confounded by the geographic location of study participants. Later, for selected ECG abnormalities prevalence values were published for the whole ARIC cohort of 12,987 black and white men and women aged 45–64 years 14, recorded at the baseline examination in 1987–1989. More recently the results of 12-lead ECG recordings for the 20 year examination for the Coronary Artery Risk Development in Young Adults (CARDIA) study from examination in 2005–2006 with identical recording and Minnesota code analysis as in the ARIC study among 2,585 black and white men and women showed smaller differences in black and white prevalent ECG abnormalities than those in the ARIC study of almost a decade earlier 15. By design, CARDIA recruited from each of four clinical centers, and as such the black-to-white distribution is also confounded with geography. There are also published data for standards of continuous measurement of durations and voltages on more than 79,000 participants in pharmaceutical clinical trials 16.
Limitations of our study include a complex sampling scheme and the fact that the ECGs are paper copy only, recorded on multiple electrocardiograph models, which in fact mirrors the state of US physician offices. In addition, because the focus of the REGARDS was on black-to-white disparities and on the distribution of geographic disparities, by design REGARDS did not recruit study participants from either Hawaii or Alaska. It was felt that these states included relative few African Americans and they were geographically “detached” from the continental US, making smoothing of incidence rates to describe geographic disparities problematic. Finally, since the focus of REGARDS was on stroke incidence, the age of the population was restricted to ages 45 and over, not permitting us to report ECG abnormalities in the younger ages. The strengths are the large biracial sample size and quality controlled standardized coding of the ECGs, together with clinical and demographic data available for subgroup categorization.
Supplementary Material
Acknowledgments
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Neurological Disorders and Stroke or the National Institutes of Health. There are no conflicts of interests for any of the authors. This work was supported by a cooperative agreement U01 NS041588 from the National Institute of Neurological Disorders and Stroke, National Institutes of Health, Department of Health and Human Services. Representatives of the funding institute have been involved in the review of the manuscript but were not directly involved in the collection, management, analysis or interpretation of the data. The authors thank the other investigators, the staff, and the participants of the REGARDS study for their valuable contributions. A full list of participating REGARDS investigators and institutions can be found at http://www.regardsstudy.org. George Howard Dr. PH, study PI, had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Public Use Data Tape Documentation: computer measurements and interpretations of electrocardiograms ages 25–74 Tape number 4140 National Health and Nutrition Examination Survey, 1971–1975.
- 2.Prineas RJ, Crow RS, Blackburn H. The Minnesota Code Manual of Electrocardiographic Findings. Boston: John Wright PSB; 1982. p. 229. [Google Scholar]
- 3.US department of Health and Human Services (DHHS), National Center for Health Statistics. The third National Health and Nutrition Examination Survey, 1988–94. Reference Manuals and Reports. Hyattsville MD: Center for Disease Control Prevention; ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/nhanes/nhanes3/2A/NH3ECG-acc.pdf. [Google Scholar]
- 4.Wu CC, Yeh WT, Crow RS, Bai CH, Pan WH. Comparison of electrocardiographic findings and associated risk factors between Taiwan Chinese and US White adults. Int J Cardiol. 2008;128:224–231. doi: 10.1016/j.ijcard.2007.05.038. [DOI] [PubMed] [Google Scholar]
- 5.Howard VJ, Cushman M, Pulley L, Gomez CR, Go RC, Prineas RJ, Graham A, Moy CS, Howard G. The reasons for geographic and racial differences in stroke study: objectives and design. Neuroepidemiology. 2005;25:135–143. doi: 10.1159/000086678. [DOI] [PubMed] [Google Scholar]
- 6.Morton LM, Cahill J, Hartge P. Reporting participation in epidemiologic studies: a survey of practice. Am J Epidemiol. 2006;163:197–203. doi: 10.1093/aje/kwj036. [DOI] [PubMed] [Google Scholar]
- 7.Prineas RJ, Crow RS, Zhang ZM. The Minnesota Code Manual of Electrocardiographic Findings (including measurement and comparison with the Novacode: Standards and procedures for measurement in epidemiologic and clinical trials. 2. Springer; London, New York: 2010. p. 328. new and enlarged. [Google Scholar]
- 8.Shah BV, Barnwell BG, Bieler GS. SUDAAN User’s Manual. 5. Research Triangle Park, N.C: Research Triangle Institute; 1997. Release 7. [Google Scholar]
- 9.Strogatz DS, Tyroler HA, Watkins LO, Hames CG. Electrocardiographic abnormalities and mortality among middle-aged black men and white men of Evans County, Georgia. J Chron Dis. 1987;40:149–155. doi: 10.1016/0021-9681(87)90066-x. [DOI] [PubMed] [Google Scholar]
- 10.Sutherland SE, Gazes PC, Keil JE, Gilbert GE, Knapp RG. Electrocardiographic abnormalities and 30-year mortality among white and black men of the Charleston Heart study. Circulation. 1993;88:2685–2692. doi: 10.1161/01.cir.88.6.2685. [DOI] [PubMed] [Google Scholar]
- 11.Riley CP, Oberman A, Hurst DC, Peacock PB. Electrocardiographic findings in a biracial, urban population. The Birmingham Stroke Study. Ala J Med Sci. 1973;10:160–170. [PubMed] [Google Scholar]
- 12.Prineas RJ, Castle CH, Curb JD, Harrist R, Lewin A, Stamler J with Hypertension Detection and Follow-Up Program Cooperative Group. Baseline electrocardiographic characteristics of the hypertension participants. Hypertension. 1983;5(6 Pt 2):IV160–IV189. doi: 10.1161/01.hyp.5.6_pt_2.iv160. [DOI] [PubMed] [Google Scholar]
- 13.Vitelli LL, Crow RS, Shahar E, Hutchinson RG, Rautaharju PM, Folsom AR. Electrocardiographic findings in a healthy biracial population. Atherosclerosis Risk in Communities (ARIC) Study Investigators. Am J Cardiol. 1998;81:453–459. doi: 10.1016/s0002-9149(97)00937-5. [DOI] [PubMed] [Google Scholar]
- 14.Machado DB, Crow RS, Boland LL, Hannan PJ, Taylor HA, Folsom AR. Electrocardiographic Findings and incident coronary heart disease among participants in the Atherosclerosis Risk in Communities (ARIC) Study. Am J Cardiol. 2006;97:1176–1181. doi: 10.1016/j.amjcard.2005.11.036. [DOI] [PubMed] [Google Scholar]
- 15.Walsh JA, Prineas R, Daviglus ML, Ning H, Liu K, Lewis CE, Sidney S, Schreiner PJ, Irribarren C, Lloyd-Jones DM. Prevalence of electrocardiographic abnormalities in a middle-aged, biracial population: Coronary Artery Risk Development in Young Adults (CARDIA) Study. J Electrocardiol. 2010;43:385.e1–9. doi: 10.1016/j.jelectrocard.2010.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mason JW, Ramseth DJ, Chanter DO, Moon TE, Goodman DB, Mendzelevski B. J Electrocardiographic reference ranges derived from 79,743 ambulatory subjects. J Electrocardiol. 2007;40:228–234. doi: 10.1016/j.jelectrocard.2006.09.003. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.