Abstract
Biliary atresia (BA) is a progressive, inflammatory cholangiopathy that culminates in fibrosis of extrahepatic and intrahepatic bile ducts. A leading theory on the pathogenesis of BA is that the bile duct damage is initiated by a virus infection, followed by a bile duct-targeted autoimmune response. One mechanism of autoimmunity entails diminished number or function of regulatory T cells (Tregs). The aim of this study was to identify potential virus-specific liver T cells from infants with BA at the time of diagnosis, implicating the virus involved in early bile duct damage. A subaim was to determine if presence of virus infection was associated with quantitative changes in Tregs. Results: Liver T cells from BA and control patients were cultured with antigen presenting cells in the presence of a variety of viral or control proteins. 56% of BA patients had significant increases in IFN-γ-producing liver T cells in response to cytomegalovirus (CMV), compared to minimal BA responses to other viruses or the control group CMV response. In addition, a positive correlation between BA plasma CMV IgM and liver T cell CMV reactivity was identified. Investigation of peripheral blood Tregs revealed significant deficits in Tregs frequencies in BA compared to controls, with marked deficits in those BA patients who were positive for CMV. Conclusions: Liver T cell responses to CMV were identified in the majority of BA patients at diagnosis, suggesting perinatal CMV infection as a plausible initiator of bile duct damage. Deficiency of Tregs in BA implies decreased inhibition of inflammation and autoreactivity, potentially allowing for exaggerated bile duct injury.
Keywords: neonatal cholestasis, autoimmunity, cholangiotropic virus
Introduction
Biliary atresia (BA) is a progressive, inflammatory cholangiopathy that culminates in fibrosis of extrahepatic and intrahepatic bile ducts. The incidence of biliary atresia ranges from 1in 3,000 to 1 in 18,000 live births in different areas of the world (1–2). Approximately 85% of cases are the acquired, perinatal form while the other 15% are the embryonic form that is associated with congenital anomalies (1,3). Despite the Kasai portoenterostomy which is performed at the time of diagnosis, BA usually leads to biliary cirrhosis and is the most common indication for pediatric liver transplantation.
The etiology of this disease has yet to be elucidated. In 1974, Landing proposed that acquired BA could be caused by a virus infection (4). A leading theory of the pathogenesis of BA is that the bile duct damage is initiated by a virus infection followed by the release of altered “self” antigens that activate bile duct-specific autoreactive T cells, resulting in a chronic, inflammatory fibrosclerosing injury of the bile ducts (3,5). Pathogenic mechanisms of autoimmunity include this “bystander activation”, molecular mimicry and loss of inhibition of autoimmunity due to defects in regulatory T cells (Tregs) (6–9). Studies utilizing the rotavirus-induced mouse model of BA have established evidence for this virus-induced, autoimmune-mediated pathway of bile duct injury (10–12). Here, autoreactive T cells specific to bile duct epithelial proteins have been identified and contribute to bile duct injury (10,11). Furthermore, a role for humoral autoimmunity in mouse and human BA was identified based on detection of high levels of α-enolase autoantibodies (12).
BA patients at diagnosis have been tested for reovirus, rotavirus, cytomegalovirus (CMV), as well as other viruses, in an attempt to identify the inciting virus infection associated with disease onset. Thus far there have been conflicting results for all of these viruses. Studies on BA serum and liver tissue collected at the time of the Kasai portoenterostomy have identified increased incidences of reovirus (13–20), rotavirus (21), and CMV (15, 22–30), however other studies negate these findings (31–36). It is possible that the virus infection is short lived, the virus damages bile duct cells and is then cleared from the liver by the immune system, thus making it undetectable (3,5). In support of this theory, virus is cleared within the first two weeks in the rotavirus-induced mouse model of BA, despite progression of inflammation and bile duct obstruction (37–39).
We sought a different approach to answer the question of a possible perinatal virus infection associated with the onset of BA. If the neonate had a recent virus infection, then one would expect a liver T cell response encompassing resident virus-specific memory T cells. The memory response is long-lasting and would be present even in the setting of viral clearance. It has been previously reported that the periductal inflammation at the time of diagnosis of BA includes activated T cells (40,41). These T cells are oligoclonal in nature, suggesting antigen-specific T cell activation, however the inciting antigen(s) are not known (42). The aim of this study was to identify potential virus-specific liver T cells of infants with BA at the time of diagnosis, implicating the virus involved in early bile duct damage. Furthermore, virus infection is a proposed trigger to a subsequent autoimmune response. One mechanism of autoimmunity entails diminished number or function of regulatory T cells (Tregs). Thus, a subaim was to determine if virus infection was associated with quantitative changes in Tregs.
Methods
Study Population
Between 2006 and 2010, PBMCs and liver wedge biopsy samples were collected from 16 patients with the perinatal/acquired form of BA at the time of Kasai portoenterostomy and 8 age-matched control patients [5 TPN-related cholestasis, 3 INH]. For PBMC analysis an additional BA samples from infants (n=21) and 2 age-matched controls (A1AT deficiency, PFIC1) (n=10) were available for study. In addition, porta hepatis lymph nodes were obtained at the time of the surgery from 8 BA patients and 4 controls (2 donor livers, 1 choledochal cyst, 1 neonatal sclerosing cholangitis; age range 8 weeks-7 years). The majority of liver wedge biopsies were performed by a single surgeon with a consistent size of ~1×0.5×0.25 cm; one-half of the wedge was used for research. This study was approved by the Colorado Multiple Institutional Review Board, Children’s Hospital Colorado. This work is also part of an ancillary study within the Childhood Liver Disease Research and Education Network that approved the shared use of local patient samples.
Isolation and culture of immune cells from tissue
Liver was minced and cultured in a 48-well plate with RPMI media-10% FCS (Invitrogen, Carlsbad, CA) supplemented with 20 U/ml of rIL-2 (R&D Systems, Minneapolis, MN) for 2 weeks. T cells activated through TCR engagement become more responsive to IL-2, leading to their preferential expansion in culture (42). Cells were cryopreserved in RPMI-10% DMSO-10% FCS freezing media and maintained in liquid nitrogen. Fresh lymph node tissue was separated into a single cell suspension after filtering through a steel mesh filter and cryopreserved as described above.
PBMC Isolation
PBMCs were isolated by Ficoll density gradient (Amersham, Uppsala, Sweden) and cryopreserved. Isolation of macrophages and B cells (antigen presenting cells- APCs) for ELISPOT analysis was performed by staining PBMCs with mouse anti-human CD14 (61D3) and CD19 (HIB19) antibodies (eBioscience, SanDiego, CA), followed by goat anti-mouse IgG MicroBeads (Miltenyi Biotec, Auburn, CA). Cells were sorted by positive selection for CD14+CD19+ cells (APCs) using the AutoMACS cell sorter. The negative population contained the PBMC T cells that underwent subsequent Treg FACS analysis (see below).
Flow Cytometric Analysis
Liver immune cells were stained with CD3-FITC (UCHT1), CD4-PE (SK3) and CD8-APC (SK1) (eBioscience, San Diego, CA) or isotype controls. PBMC T cells purified by AutoMACS bead separation (negative selection) were analyzed for the Treg population using a human regulatory T cell staining kit (eBioscience, SanDiego) according to manufacturer's instructions. Cells were stained with CD4 (RPA-T4)/CD25 (BC96), fixed and permeabilized, blocked with rat serum and stained with Foxp3 (PCH101) or control rat IgG2a antibody. All samples were visualized with the FACSCaliber flow cytometer (Becton-Dickinson, Mountain View, CA) using CellQuest software for analysis.
ELISPOT
Plates were coated with IFN-γ capture antibody (BD Biosciences Pharmingen) and blocked with culture media (RPMI 1640–10% FCS). Liver T cells (1 × 105 cells/well) and APCs (~3 × 104 cells/well) were incubated for 48 hours in duplicate with either media alone (background control for peptides); 0.5 µg CMV-pp65 (Miltenyi Biotec, Auburn, CA), a pool of CMV peptides consisting of 15-mer sequences of 11 amino acid overlap covering the complete sequence of the pp65 protein of human CMV strain AD169; 0.5 µg EBV-BZLF1 (Miltenyi Biotec, Auburn, CA), a pool of EBV peptides consisting of 15-mer sequences of 11 amino acid overlap covering the complete sequence of the BZLF1 protein of human EBV strain B95-8; 25 µg of human CMV homogenate (sonicated; gift of Dr. Adriana Weinberg), 25 µg reovirus-T3Abney homogenate (sonicated; gift of Dr. Kenneth Tyler), 1.5×104 p.f.u. Rhesus group A rotavirus homogenate (sonicated), 25 µg human lung fibroblast homogenate (sonicated; gift of Dr. Adriana Weinberg- background control homogenate for CMV, reovirus), 25 µg kidney epithelial homogenate (sonicated; background control homogenate for rotavirus), 1 µg PHA (positive control). After 48 hours plates were incubated with IFN-γ detection antibody and spots were visualized by avidin-HRP and AEC substrate (BD Biosciences Pharmingen). ELISPOT plates were analyzed using a CTL Immunospot Analyzer (Cellular Technology Ltd., Cleveland, OH) where each spot-forming unit (SFU) represents one IFN-γ-producing T cell. The results are reported as the average SFU (from duplicate wells) minus background SFU from control wells. As a positive control to ensure that all viral preparations were capable of eliciting an IFN-γ T cell response, adult PBMCs (5×105 PBMC/well) were tested by ELISPOT. As shown in Supplementary Figure 1, reactivity to all viral preparations were displayed in various adult PBMCs.
Enzyme Linked Immunosorbent Assay (ELISA)
The Abnova CMV IgM ELISA kit was used to quantify plasma CMV IgM (Abnova, Taiwan) according to the manufacturer’s instructions. ELISA plate was coated with CMV antigen followed by incubation with diluted plasma samples (1:40) or reagent controls. Optical density readings were obtained at 450 nm on a kinetic microplate reader (Molecular Devices, Sunnyvale, CA).
Statistical Analysis
Data is shown as the mean±SEM and differences between groups (BA versus control) were analyzed by student’s t-test for unpaired samples, with Welch’s correction when data had unequal variance. Confirmation of determination of cutoff point for positivity in ELISPOT data was assessed by analysis with ROC curve. Pearson correlation coefficient was used to determine correlation between plasma CMV IgM and liver IFN-γ-producing T cells. For multiple group comparison of CMV IgM and Treg data involving 3 groups [BA CMV(+), BA CMV(−) and controls], differences between multiple groups were analyzed by one-way analysis of variance (ANOVA) and analysis between 2 groups by Tukey’s Multiple Comparison test. GraphPad Prism Software (San Diego, CA) was employed for statistical analysis and p<0.05 was considered statistically significant.
Results
Similar patient characteristics between groups
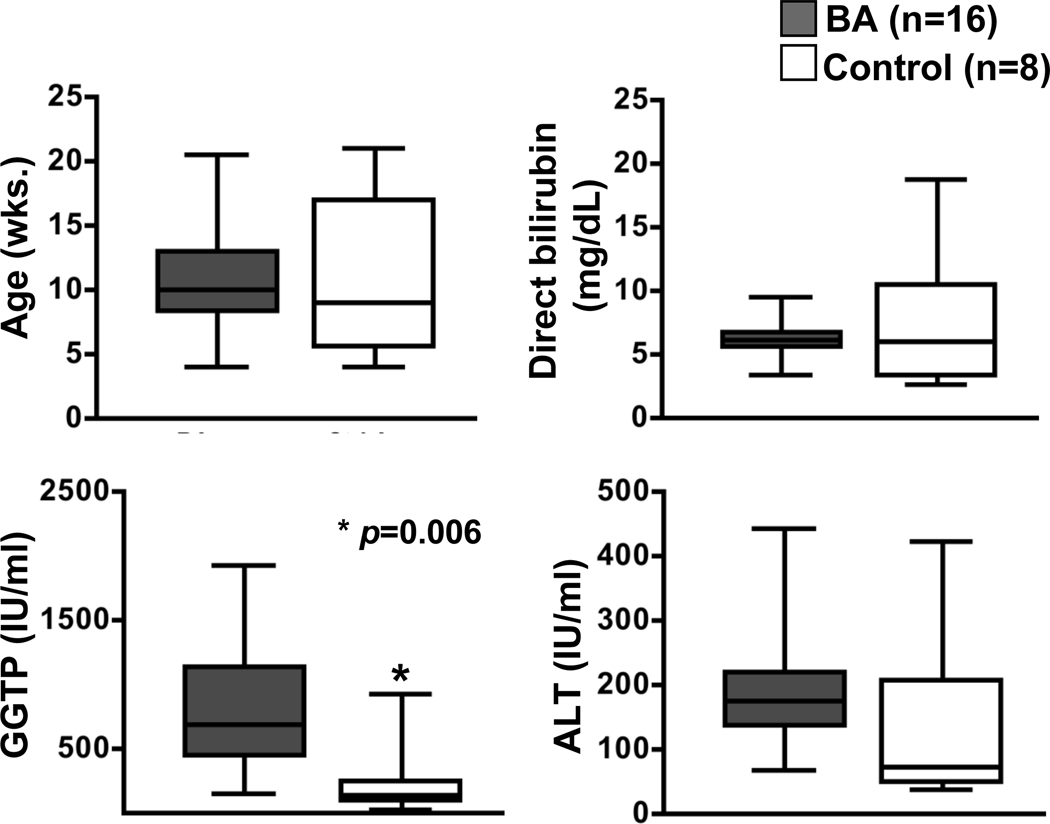
Biliary atresia and control patients were similar in age at the time of specimen collection (mean±S.D.: BA: 10.7±4.0 weeks, control: 10.9±6.2) (Figure 1). There was no significant difference in the female:male ratio (BA 10:6, control 4:4) (Fischer’s exact test, p>0.05). 62.5% of BA patients and 50% of control patients were born in the fall or winter months (September through March). Serum direct bilirubin, ALT and GGTP levels obtained within 24 hours of specimen collection were available from the medical records. The direct bilirubin (BA: 6.1±1.4 mg/dL, control: 7.4±5.2) and ALT (BA: 200.9±106.2 IU/ml, control: 131.9±128.1) levels were similar between groups and significantly lower GGTP levels were identified in the control group (BA: 811.6±484.3 IU/ml, control: 237.4±290.1; p=0.006). (Figure 1).
Figure 1. Patient characteristics.
Mean±SD of patients’ age and serum blood tests at the time of collection of blood and tissue samples.
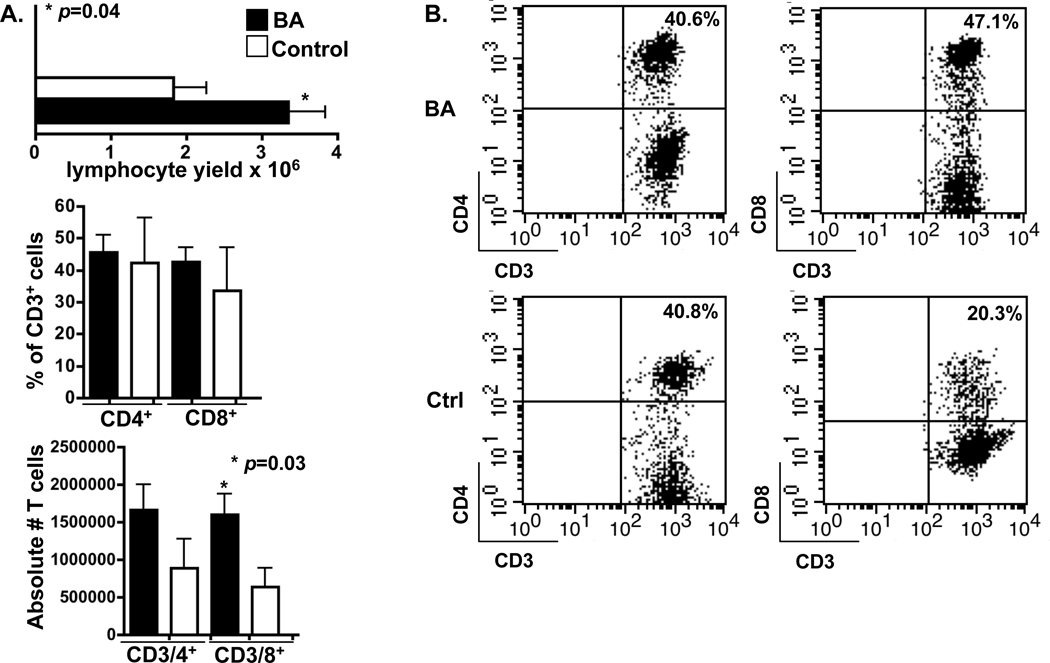
Marked T cell expansions from BA liver tissue compared to controls
Liver tissue T cells were expanded in culture with IL-2 over a 2 week time period. The yield of liver lymphocytes was higher from BA tissue (3.4±0.5 million cells) compared to control tissue (1.8±0.4; p=0.04) (Figure 2A). The FACS analysis forward and side scatter profile revealed a sub-population of lymphoblastic cells in BA samples that were not identified in control samples (data not shown). Similar percentages of CD4+ T cells and slightly increased percentages of CD8+ T cells were observed in BA livers compared to controls (CD4: BA: 45.5±5.4%, control: 42.4±14%; CD8: BA: 42.6±5.4%, control: 33.8±13.3%) (Figure 2A, 2B). However, analysis of absolute numbers of the T cell subsets from liver tissue revealed significantly increased numbers of CD8+ T cells within BA livers (CD8: BA: 1.6±0.3×106 cells, control: 0.64±0.26×106; p=0.03). While the number of CD4+ T cells was also increased in the BA liver compared to controls, the difference was not statistically significant (CD4: BA: 1.7±0.3×106 cells, control: 0.88±0.4×106) (Figure 2A). Consistent with our previous work (42), these findings suggest that the liver T cells in BA patients have been recently activated and proliferate upon IL-2 stimulation.
Figure 2. Profile of liver T cells.
A. Total liver lymphocyte yield and FACS analysis of percent and absolute number of liver T cell subsets (mean±SEM), gated on scatter density plot lymphocyte population and CD3+ histogram. B. Representative density plot of liver T cell subsets.
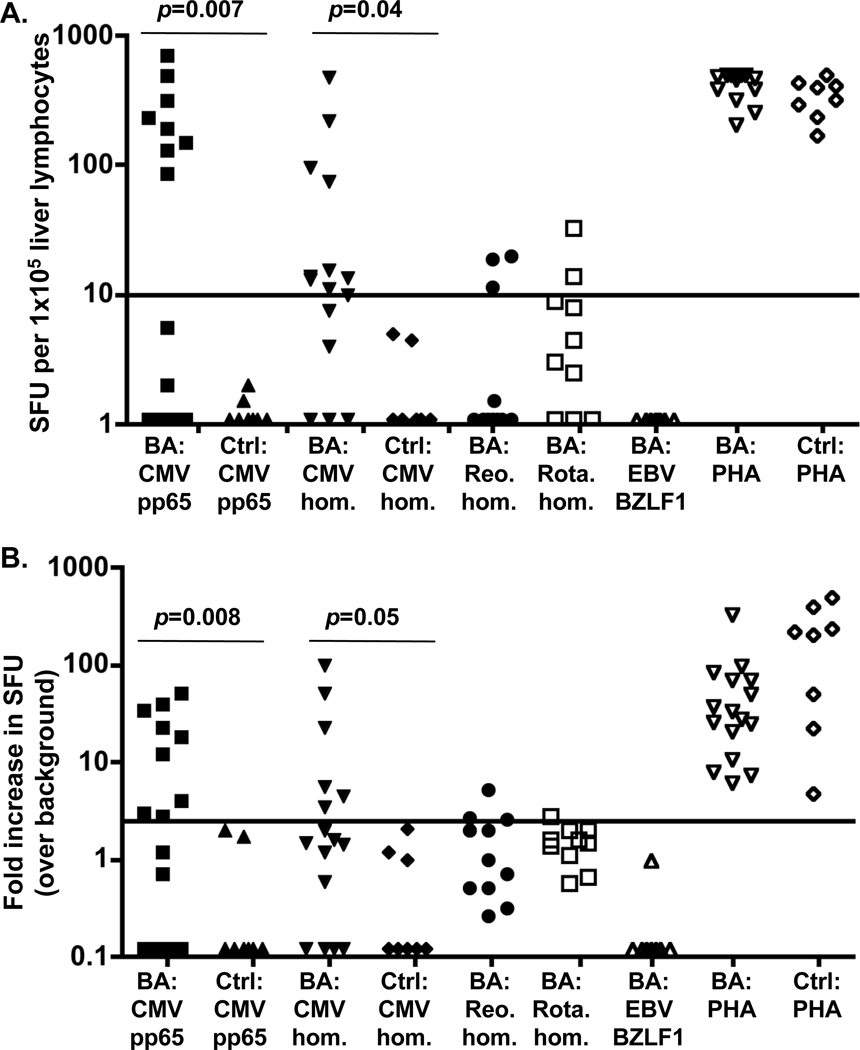
BA liver T cells produce IFN-γ in response to CMV proteins
Liver T cells from BA and control patients were cultured with autologous antigen presenting cells (APCs) in the presence of a variety of viral proteins (CMV peptides, CMV homogenate, reovirus homogenate, rotavirus homogenate, EBV peptides) or control proteins (media/FCS, lung fibroblast homogenate, kidney epithelial homogenate). A significant increase in IFN-γ-producing cells was defined as ≥10 SFU/well (candidate viral protein SFU- control protein SFU) and ≥2.5-fold increase in SFU from candidate viral protein over control protein (43–45). The data was also analyzed by ROC curve and the cutoff points provided 100% specificity and 56% sensitivity overall. Confirmation of the ability of the liver T cells to produce IFN-γ was demonstrated based on strong IFN-γ production from all patient samples in response to PHA (positive control T cell stimulator). Nine of the 16 (56%) BA patients had significant increases in IFN-γ-producing T cells in response to CMV peptides and/or CMV protein homogenate, compared to minimal BA responses to other viruses or the control group CMV response (Figure 3). Due to the limited amount of T cells available for study in the control group, only CMV-pp65 (peptide pool) and CMV protein homogenate reactivity was tested. The mean±SEM number of IFN-γ-producing T cells in response to specific viral proteins (minus background protein controls) was as follows: BA patient samples- CMVpp65: 143.5±51.0; CMV homogenate: 59.9±31.2; Reovirus: 5.4±2.3; Rotavirus: 7.7±3.1; EBV: 1.1 ±0.1; Control patient samples- CMVpp65: 1.3±0.1; CMV homogenate: 2.0±0.6. The fold-increase in IFN-γ-producing T cells in response to a specific virus over background control response was as follows: BA patient samples- CMVpp65: 11.8±4.1; CMV homogenate: 12.0±6.5; Reovirus: 1.6±0.5; Rotavirus: 1.5±0.2; EBV: 0.2 ±0.1; Control patient samples: CMVpp65: 0.55±0.3; CMV homogenate: 0.6±0.3. Three BA patients had a borderline positive response to reovirus; 2 of these 3 patients had strong reactivity to CMV proteins, suggesting possible weak cross-reactivity between the viral proteins. One BA patient was borderline positive for both reovirus and rotavirus.
Figure 3. Liver T cell IFN-γ production in response to virus.
ELISPOT analysis: Liver T cells and antigen presenting cells from BA and control (Ctrl) patients were cultured with viral proteins [CMV pp65 peptide pool, CMV homogenate (CMV hom.), reovirus homogenate (Reo. hom.), rotavirus homogenate (Rota. hom.), EBV BZLF1 peptide pool], background control proteins or phytohaemagglutinin (PHA)- positive control for T cell stimulation. A. Number of IFN-γ-producing T cells in response to virus minus IFN-γ-producing T cells in response to control proteins (media alone, fibroblast or epithelial protein homogenates- see Methods). Data are expressed as spot forming units (SFU)- each spot represents one IFN-γ-producing liver T cell. Each symbol represents the average of duplicate wells per patient sample. The solid line represents the cutoff point for a positive response. B. Fold increase in virus-specific SFU over background control protein SFU.
The liver memory T cell production of IFN-γ in response to CMV antigens suggests that the BA infant was exposed to CMV at some timepoint in the perinatal period (either late in the third trimester or at birth). In order to address the question as to if virus was still present in the liver, formalin-fixed liver tissue was available for immunohistochemistry detection studies of CMV antigens in 6 patients with CMV reactivity. The immunohistochemistry studies were performed within the clinical pathology department at Children’s Hospital Colorado and the results were read by a single pathologist. There was no detection of CMV antigens in the liver at the time of diagnosis, suggesting that actively replicating virus had been cleared at the time of diagnosis (data not shown).
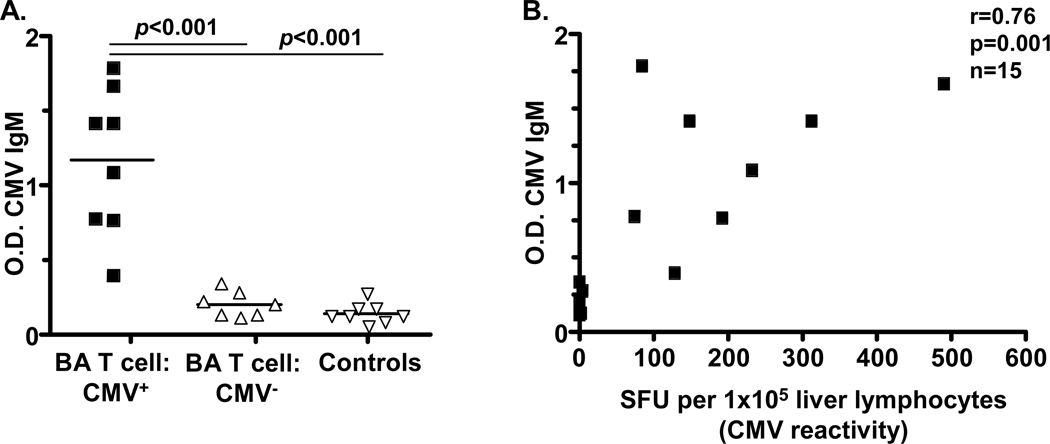
Detection of plasma CMV IgM correlates with CMV-specific liver T cell responses
Based on the findings of liver T cell reactivity to CMV in over half of the BA infants, we sought further evidence of recent CMV infection by detection of plasma CMV IgM (humoral response to virus). Plasma was available for 8 of the 9 patients who demonstrated T cell CMV reactivity. All 8 patients had significantly elevated CMV IgM compared to low/undetectable levels in the 7 BA patients with negative CMV T cell reactivity and in 8 control patients (p<0.0001; ANOVA) (Figure 4A). In addition, Pearson correlation analysis of all BA plasma CMV IgM values with liver T cell CMV reactivity identified a positive correlation (r=0.76; p=0.001) (Figure 4B).
Figure 4. Detection of plasma CMV-IgM and correlation with liver T cell response.
A. Plasma CMV-IgM levels: Each symbol reflects the average O.D. reading from duplicate wells per patient sample. The solid line is the average of all patient samples within the group. Groups include BA patients with CMV-specific liver T cell responses (BA T cell: CMV+), BA patients without CMV-specific liver T cell responses (BA T cell: CMV−), and control patients. B. Positive Pearson correlation between BA plasma CMV-IgM level and CMV-specific liver T cell response.
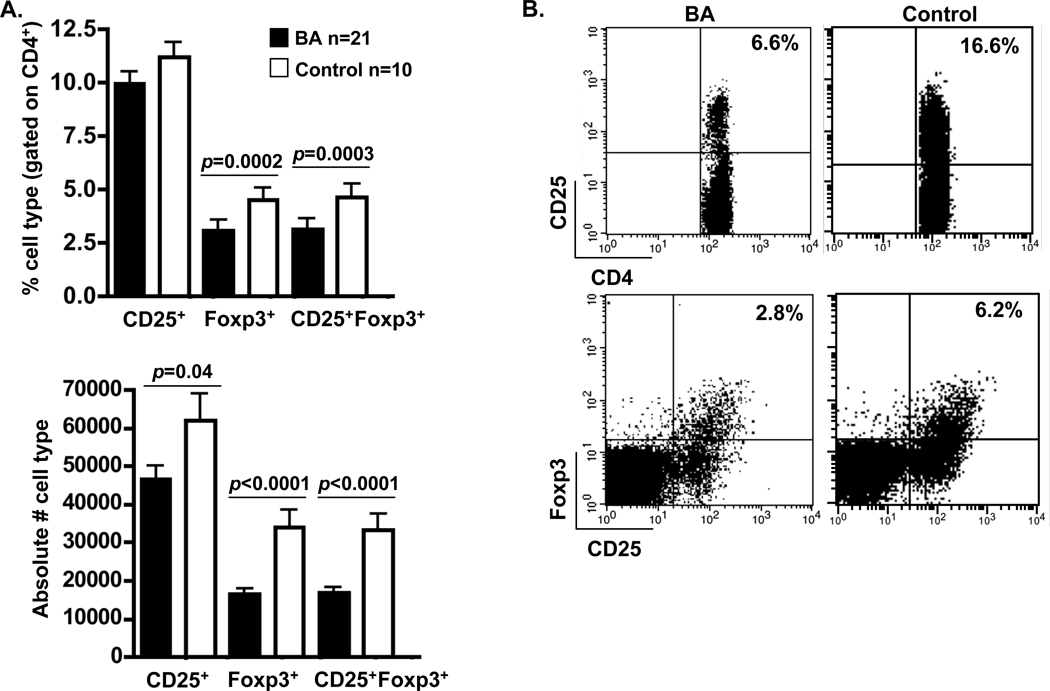
Deficiency in regulatory T cells (Treg) in BA patients is associated with CMV positivity
A leading theory of the pathogenesis of BA is that the bile duct damage is initiated by a virus, followed by an abnormal autoimmune response targeting bile duct epithelia (3). Regulatory T cells function to regulate inflammation in the setting of infection and inhibit expansion of autoreactive T cells, thus warding off autoimmunity (9). In BA, deficits in Tregs could result in an exaggerated inflammatory or autoimmune response in the setting of recent virus infection, leading to bile duct injury. To that end, we quantified the number of circulating Tregs in the peripheral blood from BA infants (n=21; age 10.2±3.8 wks.) and control patients (n=10; age 9.7±5.7 wks.) based on surface expression of CD4 and CD25 and intracellular expression of FoxP3 transcription factor. The gating strategy for FACS analysis is outlined in Supplementary Figure 2. Significantly decreased percentages and absolute numbers of CD4+CD25+FoxP3+ Tregs were identified in BA patients compared to controls (%: BA: 3.1±0.3, control: 5.4±0.5, p=0.0003; absolute number: BA: 1.6±0.1×104 cells, control: 3.3±0.4×104; p<0.0001) (Figure 5). It is plausible that the Treg deficit in peripheral blood is due to sequestration of Tregs within the liver or draining lymph nodes of BA patients. To assess this possibility, Treg analysis was performed on porta hepatis lymph nodes and compared to PBMC frequency from matched patient samples (n=8). No significant differences in Treg frequency were noted between BA PBMCs (CD4+CD25+FoxP3+: 3.1±0.5%) and BA lymph nodes (4.6±0.5) (p>0.05). Interestingly, significantly higher Treg frequencies were observed in the control lymph nodes (CD4+CD25+FoxP3+: 8.4±1.2%) compared to BA lymph nodes (4.6±0.5) (p=0.01). (Supplementary Figure 3).
Figure 5. Quantification of peripheral blood regulatory T cells (Tregs).
Purified peripheral blood T cells were incubated with antibodies to CD4, CD25 and FoxP3 and quantified by FACS analysis. A. FACS analysis of percent and absolute number of T cell populations (mean±SEM), gated on forward/side scatter density plot lymphocyte population and CD4+ histogram. B. Representative density plot of Treg populations.
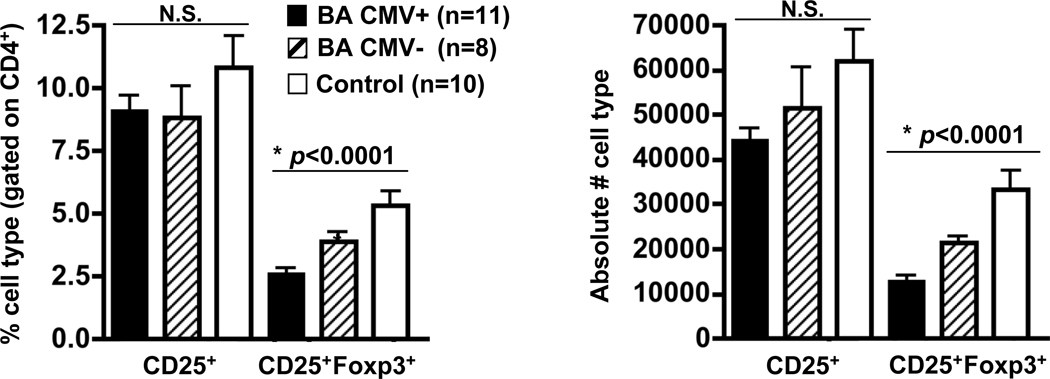
Further analysis was performed to determine if there were any differences in Tregs frequencies between BA patients that were CMV positive based on liver T cell reactivity or CMV IGM [BA:CMV(+)], compared to BA patients without CMV [BA:CMV(−)] and controls. Marked deficits in Tregs were associated with the BA:CMV(+) group compared to controls (%CD4+CD25+FoxP3+: BA:CMV(+): 2.6±0.3, BA:CMV(−): 3.9±0.3, control: 5.4±0.5; p<0.0001, ANOVA). Significant deficits in absolute numbers of circulating Tregs were also noted in both BA groups compared to controls, with striking deficits in the BA:CMV(+) group (absolute numbers: CD4+CD25+FoxP3+: BA:CMV(+): 1.3±0.15×104 cells, BA:CMV(−): 2.1±0.15×104 cells, control: 3.3±0.4×104) (Figure 6). In summary, deficits in circulating Tregs were identified in BA patients, with CMV-specific liver T cell reactivity being highly associated with marked Treg deficits.
Figure 6. Analysis of peripheral blood Treg quantities based on liver CMV response.
FACS analysis of percent and absolute number of T cell populations (mean±SEM), gated on forward/side scatter density plot lymphocyte population and CD4+ histogram. Groups include BA patients with CMV-specific liver T cell responses [BA CMV(+)], BA patients without CMV-specific liver T cell responses [BA CMV(−)], and control patients.
Discussion
Liver T cell responses to CMV were identified in a majority of BA patients at diagnosis, suggesting perinatal CMV infection as a plausible initiator of bile duct damage. CMV, a double stranded DNA virus from the Herpesviridae family, is known to infect and injure bile duct epithelia, as demonstrated by CMV inclusion bodies or positive CMV antigens within bile duct epithelia (46–49). Evidence for CMV infection at the time of diagnosis of BA has been described in the past (15, 22–30). A recent study from China identified positive CMV-IgM and CMV pp65 antigenemia in 48% and 37% of BA infants respectively (50). In our study, measurement of the virus-specific T cell response allows for a broader assessment of perinatal liver infection, compared to viral protein or DNA quantification from liver tissue. The virus may be quickly cleared from the liver, resulting in a negative CMV protein or DNA test, however the memory T cell response could last for many months or years (51).
The liver CMV-specific T cell response was present in 56% of cases; another 14% of cases had either reovirus or rotavirus-specific T cell activation. Both reovirus and rotavirus are also known to infect bile duct epithelia (52–54) and it is possible that more than one virus is capable of initiating the bile duct damage present in BA. There were no detectable virus-specific T cell responses in 29% of patients. Possible explanations for this include infection from a cholangiotropic virus that was not analyzed in this study or low numbers of resident memory T cells in the liver.
In BA, deficits in Treg quantity and/or function could result in an exaggerated inflammatory response in the setting of recent virus infection, leading to “bystander” bile duct injury. Furthermore, deficits in Tregs could increase the propensity for subsequent bile duct-targeted autoimmunity. Thus, the deficiency of circulating Tregs in BA may predispose to exaggerated inflammatory and/or autoimmune-mediated bile duct injury. Quantitative deficiencies in peripheral blood Tregs have been described in many autoimmune diseases, including rheumatoid arthritis and autoimmune hepatitis (55,56). Interestingly, these same diseases have been associated with increased numbers of Tregs in the joints and liver respectively (55,57). A limitation to this study is that fresh-frozen liver tissue was not available for quantification of Tregs, thus leaving the question of whether there is sequestration of Tregs in the liver of BA patients unanswered and warrants further investigation.
An important discovery in this study was that CMV infection was associated with the most significant decreases of Tregs in the peripheral blood of BA patients. Our findings of decreased Treg levels associated with CMV infection are consistent with recently published reports. Li et al. found that murine CMV infection led to a significantly decreased proportion of CD4+CD25+Foxp3+ Tregs in splenocytes during the first 30 days after CMV infection (58). In that study, the murine CMV infection was chronic and by 60 days the Treg quantities had recovered. Hayashi et al. described decreased Foxp3 expression associated with increased CMV-specific cytotoxic T cell responses in patients with intercurrent CMV infection and T-lymphotropic virus type 1-associated myelopathy (tropical spastic paraparesis) (59). Future studies in BA will investigate if Treg deficiencies are persistent over time and if Treg function is altered. In order to address the possible role of autoimmunity in bile duct injury, liver T cell reactivity studies in older children with BA will focus on identification of T cell responses to bile duct epithelial proteins.
Supplementary Material
Acknowledgments
Financial Support:
1. National Institutes of Health, NIDDK 1 R01 DK078195 2. National Institutes of Health, NIDDK 2 U01 DK062453; Childhood Liver Disease Research and Education Network
List of Abbreviations
- BA
Biliary Atresia
- CMV
Cytomegalovirus IL Interleukin
- EBV
Epstein-Barr Virus
- ELISA
Enzyme-Linked Immunosorbent Assay
- ELISPOT
Enzyme-Linked Immunosorbent Spot
- FACS
Fluorescence-Activated Cell Sorting
- FCS
Fetal Calf Serum
- Foxp3
Forkhead box P3
- IFN-γ
Interferon-Gamma
- INH
Idiopathic Neonatal Hepatitis
- PBMC
Peripheral Blood Mononuclear Cell
- PFU
Plaque Forming Unit
- RPMI
Roswell Park Memorial Instit. Media
- SFU
Spot Forming Unit
- TCR
T Cell Receptor
- TPN
Total Parenteral Nutrition
Contributor Information
Stephen M. Brindley, Email: stephen.brindley@ucdenver.edu.
Allison M. Lanham, Email: allison.lanham@ucdenver.edu.
Frederick M. Karrer, Email: fritz.karrer@childrenscolorado.org.
Rebecca M. Tucker, Email: rebecca.tucker@ucdenver.edu.
Andrew P. Fontenot, Email: andrew.fontenot@ucdenver.edu.
Cara L. Mack, Email: cara.mack@ucdenver.edu.
References
- 1.Sokol RJ, Mack C, Narkewicz MR, Karrer FM. Pathogenesis and outcome of biliary atresia: current concepts. J Pediatr Gastroenterol Nutr. 2003;37:4–21. doi: 10.1097/00005176-200307000-00003. [DOI] [PubMed] [Google Scholar]
- 2.Chen SM, Chang MH, Du JC, Lin CC, Chen AC, Lee HC, et al. Taiwan Infant Stool Color Card Study Group. Screening for biliary atresia by infant stool color card in Taiwan. Pediatr. 2006;117:1147–1154. doi: 10.1542/peds.2005-1267. [DOI] [PubMed] [Google Scholar]
- 3.Mack C. The pathogenesis of biliary atresia: evidence for a virus-induced autoimmune disease. Sem Liv Dis. 2007;27:233–242. doi: 10.1055/s-2007-985068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Landing BH. Considerations of the pathogenesis of neonatal hepatitis, biliary atresia and choledochal cyst- the concept of infantile obstructive cholangiopathy. Prog Pediatr Surg. 1974;6:113–139. [PubMed] [Google Scholar]
- 5.Kleinman R, Schreiber R. Genetics, immunology, and biliary atresia: An opening or a diversion. Jrl Pediatr Gastroenterol Nutr. 1993;16:111–113. doi: 10.1097/00005176-199302000-00001. [DOI] [PubMed] [Google Scholar]
- 6.Oldstone M. Molecular and cellular mechanisms, pathogenesis, and treatment of insulin-dependent diabetes obtained through study of a transgenic model of molecular mimicry. Curr Top Microbiol Immunol. 2005;296:65–87. doi: 10.1007/3-540-30791-5_5. [DOI] [PubMed] [Google Scholar]
- 7.Poole B, Scofield R, Harley J, James J. Epstein-Barr virus and molecular mimicry in systematic lupus erythematosus. Autoimmun. 2006;39:63–70. doi: 10.1080/08916930500484849. [DOI] [PubMed] [Google Scholar]
- 8.Sfriso P, Ghirardello A, Botsios C, Tonon M, Zen M, Bassi N, et al. Infections and autoimmunity: the multifaceted relationship. J Leukoc Biol. 2010;87(3):385–395. doi: 10.1189/jlb.0709517. [DOI] [PubMed] [Google Scholar]
- 9.Sakaguchi S. Regulatory T cells: history and perspective. Methods Mol Biol. 2011;707:3–17. doi: 10.1007/978-1-61737-979-6_1. [DOI] [PubMed] [Google Scholar]
- 10.Mack CL, Tucker RM, Lu BR, Sokol RJ, Fontenot AP, Ueno Y, et al. Cellular and humoral autoimmunity directed at bile duct epithelia in murine biliary atresia. Hepatol. 2006;44:1231–1239. doi: 10.1002/hep.21366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shivakumar P, Sabla G, Mohanty S, McNeal M, Ward R, Stringer K, et al. Effector role of neonatal hepatic CD8+ lymphocytes in epithelial injury and autoimmunity in experimental biliary atresia. Gastroenterol. 2007;133(1):268–277. doi: 10.1053/j.gastro.2007.04.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lu BR, Brindley SM, Tucker RM, Lambert CL, Mack CL. α-enolase autoantibodies cross-reactive to viral proteins in a mouse model of biliary atresia. Gastroenterol. 2010;139(5):1753–1761. doi: 10.1053/j.gastro.2010.07.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Morecki R, Glaser J, Cho S, Balistreri W, Horwitz M. Biliary atresia and reovirus type 3 infection. New Engl Jrl Med. 1982;307:481–483. doi: 10.1056/NEJM198208193070806. [DOI] [PubMed] [Google Scholar]
- 14.Tyler K, Sokol R, Oberhaus S, Le M, Karrer F, Narkewicz M, et al. Detection of reovirus RNA in hepatobiliary tissues from patients with extrahepatic biliary atresia and choledochal cysts. Hepatol. 1998;27:1475–1482. doi: 10.1002/hep.510270603. [DOI] [PubMed] [Google Scholar]
- 15.Rauschenfels S, Krassmann M, Al-Masri A, Verhagen W, Leonhardt J, Kuebler J, et al. Incidence of hepatotropic viruses in biliary atresia. Eur J Pediatr. 2009;168:469–476. doi: 10.1007/s00431-008-0774-2. [DOI] [PubMed] [Google Scholar]
- 16.Glacer J, Valistreri W, Morecki R. Role of reovirus type 3 in persistent infantile cholestasis. Jrl Pediatr. 1984;105(6):912–915. doi: 10.1016/s0022-3476(84)80076-1. [DOI] [PubMed] [Google Scholar]
- 17.Richardson S, Bishop R, Smith A. Reovirus serotype 3 infection in infants with extrahepatic biliary atresia or neonatal hepatitis. Jrl Gastroenterol Hepatol. 1994;9:264–268. doi: 10.1111/j.1440-1746.1994.tb01721.x. [DOI] [PubMed] [Google Scholar]
- 18.Glaser J, Morecki R. Reovirus type 3 and neonatal cholestasis. Sem Liv Dis. 1987;7(2):100–107. doi: 10.1055/s-2008-1040569. [DOI] [PubMed] [Google Scholar]
- 19.Morecki R, Glaser J, Johnson A, Kress Y. Detection of reovirus type 3 in the porta hepatic of an infant with extrahepatic biliary atresia: ultrastructural and immunocytochemical study. Hepatol. 1984;4(6):1137–1142. doi: 10.1002/hep.1840040608. [DOI] [PubMed] [Google Scholar]
- 20.Amer OT, Abd El-Rahma HA, Sherief LM, Hussein HF, Zeid AF, Abd El-Aziz AM. Role of some viral infections in neonatal cholestasis. Egypt J Immunol. 2004;11(2):149–155. [PubMed] [Google Scholar]
- 21.Riepenhoff-Talty M, Gouvea V, Evans MJ, Svensson L, Hoffenberg E, Sokol RJ, et al. Detection of group C rotavirus in infants with extrahepatic biliary atresia. Jrl Infect Dis. 1996;174(1):8–15. doi: 10.1093/infdis/174.1.8. [DOI] [PubMed] [Google Scholar]
- 22.Fischler B, Woxenius S, Nemeth A, Papadogiannakis N. Immunoglobulin deposits in liver tissue from infants with biliary atresia and the correlation to cytomegalovirus infection. Jrl Pediatr Surg. 2005;40:541–546. doi: 10.1016/j.jpedsurg.2004.11.035. [DOI] [PubMed] [Google Scholar]
- 23.DeTommaso A, Andrade P, Costa S, Escanhoela C, Hessel G. High frequency of human cytomegalovirus DNA in the liver of infants with extrahepatic neonatal cholestasis. BMC Infect Dis. 2005;5:108. doi: 10.1186/1471-2334-5-108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fischler B, Ehrnst A, Forsgren M, Orvell C, Nemeth A. The viral association of neonatal cholestasis in Sweden: A possible link between cytomegalovirus infection and extrahepatic biliary atresia. Jrl Pediatr Gastroenterol Nutr. 1998;27(1):57–64. doi: 10.1097/00005176-199807000-00010. [DOI] [PubMed] [Google Scholar]
- 25.Terr P, Haas J, Christie D. Biliary atresia, cytomegalovirus, and age at referral. Pediatr. 1996;97(6 Pt 1):828–831. [PubMed] [Google Scholar]
- 26.Chang M, Huang H, Huang E, Kao C, Hsu H, Lee C. Polymerase chain reaction to detect human cytomegalovirus in livers of infants with neonatal hepatitis. Gastroenterol. 1992;103(3):1022–1025. doi: 10.1016/0016-5085(92)90038-z. [DOI] [PubMed] [Google Scholar]
- 27.Domiati-Saad R, Dawson B, Margraf L, Finegold M, Weinberg A, Rogers B. Cytomegalovirus and human herpesvirus 6, but not human papillomavirus, are present in neonatal giant cell hepatitis and extrahepatic biliary atresia. Pediatr Devel Path. 2000;3:367–373. doi: 10.1007/s100240010045. [DOI] [PubMed] [Google Scholar]
- 28.Oliveira N, Kanawaty F, Costa S, Hessel G. Infection by cytomegalovirus in patients with neonatal cholestasis. Jrl Pediatr Gastroenterol Nutr. 2002;39(2):132–136. doi: 10.1590/s0004-28032002000200012. [DOI] [PubMed] [Google Scholar]
- 29.Fjaer R, Bruu A, Nordbo S. Extrahepatic bile duct atresia and viral involvement. Pediatr Transpl. 2005;9:68–73. doi: 10.1111/j.1399-3046.2005.00257.x. [DOI] [PubMed] [Google Scholar]
- 30.Soomro GB, Abbas Z, Hassan M, Luck N, Memon Y, Khan AW. Is there any association of extra hepatic biliary atresia with cytomegalovirus or other infections? J Pak Med Assoc. 2011;61(3):281–283. [PubMed] [Google Scholar]
- 31.Saito T, Shirasawa H, Matsunaga T, Ogawa T, Etoh T, Muramatsu T, et al. Lack of evidence for reovirus infection in tissues from patients with biliary atresia and congenital dilatation of the bile duct. Jrl Hepatol. 2004;40(2):203–211. doi: 10.1016/j.jhep.2003.10.025. [DOI] [PubMed] [Google Scholar]
- 32.Steele M, Marshall C, Lloyd R, Randolph V. Reovirus 3 not detected by reverse transcriptase-mediated polymerase chain reaction analysis of preserved tissue from infants with cholestatic liver disease. Hepatol. 1995;21(3):697–702. [PubMed] [Google Scholar]
- 33.Brown W, Sokol R, Levin M, Silverman A, Tamaru T, Lilly J, et al. Lack of correlation between infection with reovirus 3 and extrahepatic biliary atresia or neonatal hepatitis. Jrl Pediatr. 1988;113(4):670–676. doi: 10.1016/s0022-3476(88)80376-7. [DOI] [PubMed] [Google Scholar]
- 34.Bobo L, Ojeh C, Chiu D, Machado A, Colombani P, Schwarz K. Lack of evidence for rotavirus by polymerase chain reaction/enzyme immunoassay of hepatobiliary samples from children with biliary atresia. Pediatr Res. 1997;41(2):229–234. doi: 10.1203/00006450-199702000-00013. [DOI] [PubMed] [Google Scholar]
- 35.Yaghobi R, Didari M, Gramizadeh B, Rahsaz M, Heidari T, Banihashemi M, et al. Study of viral infections in infants with biliary atresia. Ind Jrl Pediatr. 2010 doi: 10.1007/s12098-010-0309-5. E-pub. [DOI] [PubMed] [Google Scholar]
- 36.Jevon G, Dimmick J. Biliary atresia and cytomegalovirus infection: a DNA study. Pediatr Devel Path. 1999;2:11–14. doi: 10.1007/s100249900083. [DOI] [PubMed] [Google Scholar]
- 37.Mack CL, Tucker RM, Sokol RJ, Kotzin BL. Armed CD4+ Th1 effector cells and activated macrophages participate in bile duct injury in murine biliary atresia. Clin Immunol. 2005;115(2):200–209. doi: 10.1016/j.clim.2005.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Petersen C, Biermanns D, Kuske M, Schakel K, Meyer-Junghanel L, Mildenberger H. New aspects in a murine model for extrahepatic biliary atresia. J Pediatr Surg. 1997;32:1190–1195. doi: 10.1016/s0022-3468(97)90680-1. [DOI] [PubMed] [Google Scholar]
- 39.Shivakumar P, Campbell KM, Sabla GE, Miethke A, Tiao G, McNeal MM, et al. Obstruction of extrahepatic bile ducts by lymphocytes is regulated by IFN-gamma in experimental biliary atresia. J Clin Invest. 2004;114:322–329. doi: 10.1172/JCI21153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mack CL, Tucker RM, Sokol RJ, Karrer FM, Kotzin BL, Whitington PF, et al. Biliary atresia is associated with CD4+ Th1 cell-mediated portal tract inflammation. Pediatr Res. 2004;56:79–87. doi: 10.1203/01.PDR.0000130480.51066.FB. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Davenport M, Gonde C, Redkar R, Koukoulis G, Tredger M, Mieli-Vergani G, et al. Immunohistochemistry of the liver and biliary tree in extrahepatic biliary atresia. J Pediatr Surg. 2001;36:1017–1025. doi: 10.1053/jpsu.2001.24730. [DOI] [PubMed] [Google Scholar]
- 42.Mack CL, Falta MT, Sullivan AK, Karrer F, Sokol RJ, Fontenot AP. Oligoclonal expansions of CD4+ and CD8+ T cells in the target organ of patients with biliary atresia. Gastroenterol. 2007;133(1):278–287. doi: 10.1053/j.gastro.2007.04.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Pott GB, Palmer BE, Sullivan AK, Silviera L, Maier LA, Newman LS, et al. Frequency of beryllium-specific, TH1-type cytokine-expressing CD4+ T cells in patients with beryllium-induced disease. J Allergy Clin Immunol. 2005;115(5):1036–1042. doi: 10.1016/j.jaci.2005.01.019. [DOI] [PubMed] [Google Scholar]
- 44.Moodie Z, Price L, Gouttefangeas C, Mander A, Janetzki S, Lower M, et al. Response definition criteria for ELISPOT assays revisited. Cancer Immunol Immunother. 2010;59:1489–1501. doi: 10.1007/s00262-010-0875-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Shirren CA, Jung MC, Gerlach JT, Worzfeld T, Baretton G, Mamin M, et al. Liver-derived hepatitis C virus-specific CD4 T cells recognize multiple epitopes and produce interferon gamma. Hepatology. 2000;32:597–603. doi: 10.1053/jhep.2000.9635. [DOI] [PubMed] [Google Scholar]
- 46.Evans PC, Coleman N, Wreghitt TG, Wight DG, Alexander GJ. Cytomegalovirus infection of bile duct epithelial cells, hepatic artery and portal venous endothelium in relation to chronic rejection of liver grafts. J Hepatol. 1999;31(5):913–920. doi: 10.1016/s0168-8278(99)80294-3. [DOI] [PubMed] [Google Scholar]
- 47.Oku T, Maeda M, Waga E, Wada Y, Nagamachi Y, Fujita M, et al. Cytomegalovirus cholangitis and pancreatitis in an immunocompetent patient. J Gastroenterol. 2005;40(10):987–992. doi: 10.1007/s00535-005-1683-z. [DOI] [PubMed] [Google Scholar]
- 48.Ko HM, Kim KS, Park JW, Lee YJ, Lee MY, Lee MC, et al. Congenital cytomegalovirus infection: three autopsy case reports. J Korean Med Sci. 2000;15:337–342. doi: 10.3346/jkms.2000.15.3.337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wang W, Zheng S, Shong Z, Zhao R. Development of a guinea pig model of perinatal cytomegalovirus-induced hepatobiliary injury. Fetal and Pediatric pathology. 2011:1–11. doi: 10.3109/15513815.2011.572959. early online. [DOI] [PubMed] [Google Scholar]
- 50.Shen C, Aheng S, Wang W, Xiao XM. Relationship between prognosis of biliary atresia and infection of cytomegalovirus. World J Pediatr. 2008;4(2):123–126. doi: 10.1007/s12519-008-0024-8. [DOI] [PubMed] [Google Scholar]
- 51.Bevan MJ. Memory T cells as an occupying force. Eur J Immunol. 2011;41(5):1192–1195. doi: 10.1002/eji.201041377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Papadimitriou JM. The biliary tract in acute murine reovirus 3 infection. Am J Pathol. 1968;53:595–611. [PMC free article] [PubMed] [Google Scholar]
- 53.Gilger MA, Matson DO, Conner ME, Rosenblatt HM, Finegold MJ, Estes MK. Extraintestinal rotavirus infections in children with immunodeficiency. J Pediatr. 1992;120:912–917. doi: 10.1016/s0022-3476(05)81959-6. [DOI] [PubMed] [Google Scholar]
- 54.Qiao H, Zhaori G, Jiang Z, Chen Y, Chen Y, Hou D. Detection of group C rotavirus antigen in bile duct and liver tissues of an infant with extrahepatic biliary atresia. Chin Med J. 1999;112:93–95. [PubMed] [Google Scholar]
- 55.Miyara M, Gorochov G, Ehrenstein M, Musset L, Sakaguchi S, Amoura Z. Human FoxP3 regulatory T cells in systemic autoimmune diseases. Autoimmun Rev. 2011;10:744–755. doi: 10.1016/j.autrev.2011.05.004. [DOI] [PubMed] [Google Scholar]
- 56.Longhi MS, Ma Y, Bogdanos DP, Cheeseman P, Mieli-Vergani G, Vergani D. Impairment of CD4+CD25+ regulatory T cells in autoimmune liver disease. J Hepatol. 2004;41:31–37. doi: 10.1016/j.jhep.2004.03.008. [DOI] [PubMed] [Google Scholar]
- 57.Sakaki M, Hiroishi K, Baba T, Ito T, Hirayama Y, Saito K, et al. Intrahepatic status of regulatory T cells in autoimmune liver diseases and chronic viral hepatitis. Hepatol Res. 2008;38:354–361. doi: 10.1111/j.1872-034X.2007.00284.x. [DOI] [PubMed] [Google Scholar]
- 58.Li YN, Zhou YF, Shu SN, Zhu DD, Yang ZF, Fang F. Effects of acute and chronic murine cytomegalovirus infections on the ratio of regulatory T cells and expression of Th1/Th2 transcription factors T-bet/GATA-3. Zhonghua Yi Xue Za Zhi. 2008;88(42):2999–3002. [PubMed] [Google Scholar]
- 59.Hayashi D, Kubota R, Takenouchi N, Tanaka Y, Hirano R, Takashima H, et al. Reduced Foxp3 expression with increased cytomegalovirus-specific CTL in HTLV-I-associated myelopathy. J Neuroimmunol. 2008;200(1–2):115–124. doi: 10.1016/j.jneuroim.2008.06.005. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.