Abstract
Objective
The term "teachable moment" (TM) has been used to describe a life transition or event which motivates an individual to change a behavior or presents an opportunity to intervene to prompt behavior change. We examined whether receipt of a false positive ovarian cancer (OC) screening result may represent a TM.
Methods
403 women participating in an OC screening program completed questionnaires assessing demographic, clinical, behavioral, and psychosocial information. The TM was operationalized as expressed interest in receiving health-related information. We hypothesized that among women receiving a false positive screening test result, those women who had experienced greater personal perceived risk for OC as well as distress would be more interested in receiving health-related information than women receiving a normal result.
Results
Analyses revealed that women receiving a false positive screening result were less interested in receiving health-related information than women receiving a normal screening result. For women receiving a false positive result, expressed interest in receipt of health-related information was only modestly related to distress and related even less to perceptions of OC risk.
Conclusions
Our data do not support viewing a false positive OC screening result as a TM. Potential explanations for the current findings as well as recommendations for future research investigating the TM are discussed.
Keywords: teachable moment, ovarian cancer screening, normal/false positive cancer screening result, cancer risk
Introduction
The term "teachable moment" has been used to describe naturally occurring life transitions or health events that have the potential to motivate individuals to adopt risk-reducing or health protective behaviors (Ganz, 2005; McBride, Emmons, & Lipkus, 2003). The concept of the teachable moment has been applied most frequently in the health literature where it has often been used to explain or understand health behavior change in response to an illness or other significant health event. For example, experience of myocardial infarction, pregnancy, or cancer diagnosis have all been considered teachable moments that could increase the likelihood of smoking quit attempts and ultimately smoking cessation (Freund, D'Agostino, Belanger, Kannel, & Stokes, 1992; Gritz et al., 2006; Gritz, Nisenbaum, Elashoff, & Holmes, 1991; Haug, Fugelli, Aaro, & Foss, 1994; McBride, Pirie, & Curry, 1992). Participation in lung and cervical cancer screening have also been considered teachable moments that might encourage smoking cessation (Loss, Hall, & Speers, 1979; McBride et al., 2008; McBride et al., 1999; Taylor et al., 2007). Baker and Wardle (2002) in their randomized controlled trial among adults participating in colorectal cancer screening demonstrated that a brief tailored intervention to increase fruit and vegetable intake led to significant increases in fruit and vegetable servings in the intervention group compared to the control group. Medical triggers, such as disease diagnosis and physician prompts, have also been suggested as potential teachable moments that may foster greater weight control efforts (Gorin, Phelan, Hill, & Wing, 2004) while presentation at a trauma center due to an alcohol-related injury may represent a teachable moment to foster lower alcohol intake and reduce future alcohol-related injuries (Marks & Williams, 2007). Geller and colleagues (2006) found siblings of patients recently diagnosed with melanoma engaged in more skin cancer risk-reduction strategies over time, suggesting a sibling's cancer diagnosis may prompt health behavior changes in their siblings and thus may represent a teachable moment. Finally, Humpel and colleagues (2007) found cancer survivors and their family members reported increased physical activity, dietary improvements, and smoking cessation following a cancer diagnosis, suggesting the power of a cancer diagnosis as a teachable moment.
While the concept of the teachable moment has been widely invoked to account for health behavior change following a significant health event, the research literature relevant to the concept of the teachable moment has been largely descriptive (Lawson & Flocke, 2008). In fact, there has been very little hypothesis-driven research focusing on the teachable moment. In large part, this is likely due to the lack of a suitable conceptual and theoretical framework surrounding the concept of the teachable moment. Recently, however, McBride and colleagues (2003; 2008) have proposed three key characteristics which could be used to determine whether an event might motivate health behavior change and thus might be considered a teachable moment. These include the extent to which the event: 1) affects perceived personal risk, 2) prompts emotional responses, such as worry, and 3) challenges self-concept or social role (McBride et al., 2003; McBride et al., 2008). Consistent with this conceptual framework, among individuals diagnosed with pre-cancerous colon polyps randomized to a behavioral intervention to lower their risk of cancer, those reporting the most worry regarding development of cancer engaged the most in the intervention (McBride et al., 2008). This suggested diagnosis of pre-cancerous colon polyps might represent a teachable moment.
The purpose of the present study was to examine the potential of receipt of a false positive ovarian cancer (OC) screening test result to serve as a teachable moment. Receipt of a false positive screening test result first involves receipt of an abnormal screening result which is followed by a repeat test yielding a normal result. It seems reasonable to believe receipt of an abnormal OC screening result could increase perceptions of personal risk for OC. Furthermore, receipt of an abnormal OC screening test result has been linked to increased distress (Andrykowski, Boerner, Salsman, & Pavlik, 2004; Gaugler, Pavlik, Salsman, & Andrykowski, 2006 17; F. J. Wardle et al., 1993). Thus, receipt of an abnormal OC screening test result would appear to possess at least two of the three proposed key characteristics of a teachable moment (McBride et al., 2008). Consequently, we hypothesized that interest in obtaining information about a variety of health information topics would be greater in women who had previously received an abnormal test result and were subsequently informed that this was a false positive relative to women receiving a normal OC screening test result. Furthermore, based on McBride's conceptualization of the teachable moment (McBride et al., 2008), we hypothesized that among women who had previously received an abnormal test result and were subsequently informed that it was a false positive result, greater perceived personal risk for OC and greater OC-specific distress would be associated with greater interest in receiving health-related information.
Methods
Sample
The study sample consisted of participants in an OC screening program offered by the University of Kentucky Markey Cancer Center (DePriest & DeSimone, 2003; van Nagell et al., 2000). This program offers free, annual transvaginal sonographic (TVS) screening to asymptomatic women ≥ 50 years of age as well as asymptomatic women 30 to 50 years of age who are postmenopausal or who possess a family history of OC (van Nagell et al., 2000). The proportion of women receiving an abnormal screening test result in the course of routine screening in the University of Kentucky screening program is approximately 5–7% (DePriest & Desimone, 2003). A Routine Screening (RS) Group (n=124) consisted of women who had recently undergone a routine TVS screening test, had received a "normal" TVS test result, and were advised to return for additional routine screening in one year. A False Positive Screening (FP) Group (n=279) consisted of women who had recently undergone a routine TVS screening test, had received an "abnormal" TVS test result, and subsequently returned for a repeat TVS screening test 4–16 weeks later which was clear and thus indicated that their previous abnormal TVS test result was a false positive result.
Procedure
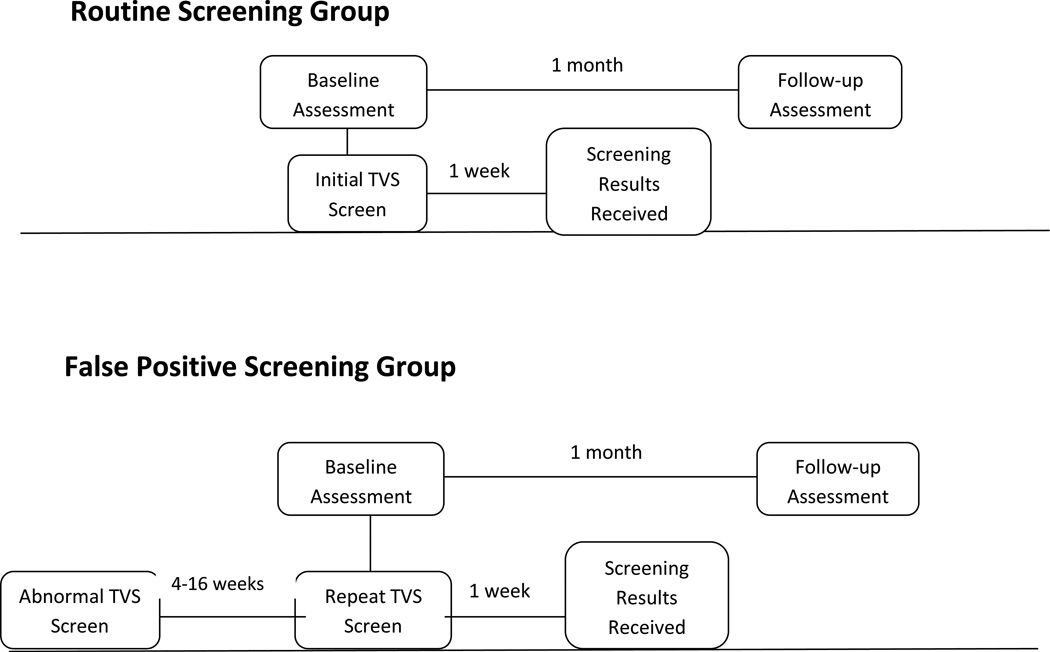
The data reported here were collected as part of a broader study of psychological and behavioral response to an abnormal OC screening test result. Institutional Review Board approval was obtained. Data collection for this broader, parent study occurred between May, 2004 and December, 2007. As reported earlier (Andrykowski & Pavlik, in press), less than 5% of study eligible women offered study participation declined. Potential study participants were approached by research staff in the clinic waiting area of the University of Kentucky OC screening program. Information about study procedures was provided and written, informed consent was obtained. All enrolled women completed a baseline assessment. For women in the RS group, the Baseline assessment occurred immediately prior to a routine TVS screening test. For women in the FP group, the Baseline assessment occurred immediately prior to a repeat TVS screening test needed to clarify the results of an abnormal TVS test result received 4–16 weeks earlier in the course of routine TVS screening. All women then completed a follow-up assessment one month following the Baseline assessment. The 1 Month Follow-up assessment was conducted by telephone. All women in the FP group were notified of the result of their repeat TVS screening test within one week of the Baseline assessment. For all women in the FP group, their repeat TVS test indicated no malignancy was present; therefore their previous abnormal OC screening result had been a false positive result. Figure 1 is an illustration portraying the study design and flow of participants through the study. The two groups are identical in all respects at the time of the 1 month follow-up, except for the prior screening test in the FP group that was abnormal, thus triggering a follow-up screening test. Both the Baseline and 1 Month Follow-up assessments consisted of completion of a set of questionnaires assessing a variety of demographic, clinical, behavioral, and psychosocial information. For all women, information regarding prior history of TVS screening, including the number of previous routine TVS screening tests and whether she had a prior history of receiving an abnormal TVS test result was obtained from computerized clinic records.
Figure 1.
Study design and flow of participants through study
Study Measures
Information obtained at the Baseline assessment included age, race, marital status, education, and history of OC in a first degree relative (FDR). At the 1 Month Follow-up assessment, all women were asked about their interest in receiving information about a variety of health-related topics. Specifically, women were asked "What type of additional information would be helpful to you or would you be interested in at this time?" Women were then presented with a list of ten options (See Table II) and asked to indicate which, if any, of these health information topics she was interested in. Women could indicate interest in as many of the ten topics as they desired. The health information list was developed for use in the present research. The 10 information topics were chosen based on consultation with experts in the field of ovarian screening to represent a range of health information interests likely to be expressed by women in this age group undergoing OC screening ranging from OC-specific (e.g., my risk for OC), through cancer in general (e.g., how I can prevent cancer), and to general health interests (e.g., how I can change my health habits to live a healthier life).
Table II.
Proportion of FP (n=279) and RS (n=124) Groups Expressing Interest in Obtaining Information About Specific Health Information Topics.
| Information Topic | FP Group | RS Group | p-Value |
|---|---|---|---|
| My risk for ovarian cancer | 69% | 63% | 0.251 |
| My risk for breast cancer | 44% | 55% | 0.036 |
| My risk for colorectal cancer | 44% | 57% | 0.026 |
| My husband or partner’s risk for cancer | 28% | 34% | 0.231 |
| Risk for cancer in other members of my family | 41% | 42% | 0.787 |
| How I can change my health habits to live a healthier life | 57% | 66% | 0.084 |
| How I can prevent cancer | 58% | 72% | 0.009 |
| What screening tests for cancer I should receive | 65% | 63% | 0.756 |
| Cancers that are inherited or run in families | 58% | 68% | 0.057 |
| Tests I could receive to determine whether I am at risk for developing a cancer that is inherited | 57% | 56% | 0.854 |
Note. p-values shown are for chi square test with 1 df, 2-tailed test
Women in both the FP and RS groups completed the 15-item Impact of Events Scale (IES; (Horowitz, Wilner, & Alvarez, 1979) at the Baseline assessment. The IES is a measure of intrusive and avoidant cognition and behavior related to a specific stressor - in this study "the possibility that you might get ovarian cancer someday." As such, the IES might be considered a measure of OC-specific distress. The IES yields a Total score as well as Intrusion and Avoidance subscale scores.
Several estimates of lifetime OC risk were obtained from women in the FP and RS groups at the baseline assessment. Participants estimated Personal OC Risk by providing a percentage between 0 and 100% in response to the question "What are the chances you will develop OC some day?" (Andrykowski et al., 2004). Participants estimated Typical OC risk by providing a percentage between 0 and 100% in response to the question "What are the chances the average woman your age will develop OC some day?" (Andrykowski et al., 2004). These two risk items were combined to form a Comparative OC Risk index by subtracting Typical OC Risk from Personal OC Risk estimates for each woman. A negative Comparative OC Risk score thus indicated a woman' perception that her personal risk for OC was less than a typical woman's risk for OC.
Data Analysis
For each of the ten health information topics, the proportion of respondents in the RS and FP groups indicating interest in that topic was compared using chi square test. The number of health information topics a woman indicated interest in was summed to create an index of Total Health Information Interest (range from 0 to 10). Standard procedures were used to calculate IES total and subscale scores. A probability value of .05 was used as the criterion for statistical significance.
Results
Table I shows descriptive information for both the RS and FP groups with regard to clinical and demographic variables, IES scores, and OC risk estimates. Comparison of the RS and FP groups revealed no significant differences with regard to age, education, number of days between the Baseline and 1 Month Follow-up assessments, number of previous routine TVS screening tests, history of OC in an FDR, history of a previous abnormal TVS test result, or minority status (all p's > .05). The RS and FP groups did significantly differ with regard to IES total scores at the Baseline assessment (t (277) = 3.61; p< .001). Specifically, as would be expected given their recent receipt of an abnormal screening test result (Andrykowski et al., 2004; Gaugler et al., 2006), the FP group reported higher IES- Total scores at the Baseline assessment. In addition, the RS and FP groups differed significantly with regard to Comparative OC Risk (t (390) = 2.14; p < .05). While both the RS and FP groups reported they believed their personal risk for OC was less than the risk for OC of a typical woman their age (i.e., mean values for Comparative OC Risk were negative), the FP group reported greater perceived personal risk for OC as their estimate of personal risk for OC was more similar to a typical woman their age (Mean = 1.8% lower) than women in the RS group (mean = 6.7% lower). No group differences were found in estimates of Personal or Typical OC Risk.
Table I.
Comparison of FP (n=279) and RS (n=124) Groups With Regard to Demographic, Psychosocial, and Clinical Variables.
| Variable | FP Group | RS Group | p-value |
|---|---|---|---|
| Age in years | 56.6 (11.9) | 58.0 (11.6) | 0.267 |
| Education in years | 14.0 (2.8) | 14.1 (3.0) | 0.704 |
| Prior # routine TVS tests | 4.00 (4.7) | 3.8 (4.4) | 0.637 |
| Days between Baseline and 1 Month Follow-up | 32.9 (7.0) | 34.5 (9.0) | 0.052 |
| IES-Total at Baseline | 14.7 (14.2) | 8.4 (12.1) | 0.000 |
| Personal OC Risk at Baseline | 26.9 (21.6) | 25.4 (24.6) | 0.554 |
| Typical OC Risk at Baseline | 28.7 (18.6) | 32.1 (16.7) | 0.084 |
| Comparative OC Risk at Baseline | −1.8 (20.7) | −6.7 (21.6) | 0.033 |
| % Previous abnormal TVS tests | 24% | 30% | 0.160 |
| % OC in FDR | 19% | 14% | 0.175 |
| % Breast Cancer in FDR | 24% | 21% | 0.409 |
| % Colorectal Cancer in FDR | 11% | 12% | 0.925 |
| % Minority | 3% | 2% | 0.445 |
Note. Means and standard deviation (in parentheses) shown for age, education, # prior TVS tests, days between Baseline and 1 Month Follow-Up assessments, IES scores, and Comparative OC Risk estimates. Negative values for Comparative OC Risk indicates perceived personal OC risk is less than perceived OC risk of typical woman
Scores on the Total Health Information Interest index for the RS and FP groups were compared using t-test analysis. Women in the RS group expressed interest in a mean of 5.8 (SD=3.1) health information topics compared to a mean of 5.2 (SD=3.0) in the FP group (t (400) = 1.79; p = .075). Table II shows the proportion of women in the FP and RS groups expressing interest in each of the ten health information topics. Significant differences between the FP and RS groups were evident in the proportion of women expressing interest in "information about my risk for breast cancer" (FP Group = 44% vs. RS Group = 55%; χ2 = 4.41; p < .05), "information about my risk for colorectal cancer" (FP Group = 44% vs. RS Group = 57%; χ2 = 4.96; p < .05), and "information about how I can prevent cancer" (FP Group = 58% vs. RS Group = 72%; χ2 = 6.87; p < .01). In addition, differences between the FP and RS group approached our .05 criterion for statistical significance for "information about cancers that are inherited or run in families" (FP Group = 58% vs. RS Group = 68%; χ2 = 3.63; p = .057) and "information about how I can change my health habits to lead a healthier life" (FP Group = 57% vs. RS Group 66%; χ2 = 2.98; p = .084). For all five of these health information topics, the proportion of women in the RS group indicating interest in that specific health information topic exceeded the proportion in the FP group.
To examine whether interest in health information topics within the FP group was associated with the either the magnitude of OC-specific distress or perceived risk for OC, a set of point-biserial correlations were calculated. Correlations were calculated between interest in each of the 10 health information topics and the Total Health Information Index and IES-Total and IES-Intrusion scores and Personal and Comparative OC Risk estimates at the Baseline assessment (see Table III). The pattern of correlations between health information interests and IES-Avoidance scores are not shown but were very similar. IES-Total scores at Baseline were significantly correlated with interest in 6 of the 10 health information topics. Correlations for these 6 topics ranged from .13 to .22. IES- Intrusion scores at Baseline were also significantly correlated with interest in 6 of the 10 health information topics. Correlations for these 6 topics ranged from .12 to .24. In all instances, higher IES scores were associated with greater interest in receiving information about a health information topic. Personal OC Risk estimates were significantly correlated with interest in 5 of the ten health information topics. Comparative OC Risk was significantly correlated only with interest in information regarding tests for hereditary cancer (r = .15; p < .01). In all instances, interest in a health information topic was associated with greater perceptions of OC risk. Finally, the Total Health Information Index was significantly correlated with IES-Total scores (r = .19; p < .001), IES-Intrusion scores (r = .22; p < .001), and Personal OC Risk estimates (r = .18; p < .01). As with individual health interest items, greater interest in health information topics, in total, was associated with higher IES scores and perceptions of OC risk.
Table III.
Point Biserial Correlations Between Interest in Health Information Topics and IES-Total, IES-Intrusion Scores, Personal OC Risk, and Comparative OC Risk at the Baseline Assessment for the FP group (n=279).
| Information Topic | IES-Total | IES-Intrusion | Personal OC Risk |
Comparative OC Risk |
|---|---|---|---|---|
| My risk for ovarian cancer | .21 *** | .21 *** | .09 | .06 |
| My risk for breast cancer | .03 | .06 | .05 | .02 |
| My risk for colorectal cancer | .10 | .13 * | .07 | .01 |
| My husband or partner’s risk for cancer | .00 | .04 | .10 * | .08 |
| Risk for cancer in other members of my family | .13 * | .19 ** | .18 *** | .04 |
| How I can change my health habits to live a healthier life | .13 * | .10 | .06 | −.01 |
| How I can prevent cancer | .14 * | .12 * | .09 | .08 |
| What screening tests for cancer I should receive | .15 * | .15 * | .11 * | .03 |
| Cancers that are inherited or run in families | .06 | .10 | .14 ** | .09 |
| Tests I could receive to determine whether I am at risk for Developing a cancer that is inherited | .22*** | .24 *** | .17 ** | .15 ** |
| Total Health Information Interest Index | .19*** | .22*** | .18** | .05 |
Note: Interest in information topics coded as 0=no and 1=yes
p < .001;
p < .01;
p < .05
Discussion
Contrary to our primary hypothesis, women receiving a false positive OC screening result (i.e., FP group) were not more interested in receiving additional health-related information than women receiving a normal OC screening result (i.e., RS group). In fact, the evidence suggested women in the FP group generally reported less interest in receiving additional health-related information than women in the RS group. Furthermore, we obtained only weak support for our secondary hypotheses. For women in the FP group, expressed interest in receipt of additional health-related information was only modestly related to IES distress scores and related even less to perceptions of OC risk. Even when significant correlations were evident, the size of these correlations was small (Table III). Thus, contrary to our expectation, our data do not support viewing receipt of a false positive screening test result during routine OC screening as a “teachable moment.”
There are several possible explanations for our findings. First, receipt of a false positive OC screening test result during the course of routine screening for OC may simply not represent a teachable moment. If so, this would seem inconsistent with prior research suggesting discovery of pre-cancerous polyps during routine colon cancer screening might be considered a teachable moment (McBride et al., 2008). However, not all cancer screening tests are alike. It may be the case that the OC screening setting was not a suitable situation in which to test for a teachable moment. It is also important to note that many of the women had previously undergone OC screening and received false positive results, so this also may have influenced the present findings.
On the other hand, it appeared receipt of an abnormal OC screening test result during the course of a false positive screening experience increased perceptions of personal risk and prompted an emotional response, two of McBride et al.’s (McBride et al., 2008) three suggested criteria for a teachable moment. However, it is possible that while receipt of an abnormal OC screening test result did impact risk perceptions and did engender an emotional response, the magnitude of this impact was not sufficient to trigger the teachable moment phenomenon. By the same token, it could be there is a ceiling level of psychological impact which an event must not exceed in order to trigger the teachable moment response. This seems to be an unlikely explanation for results in the current study as the magnitude of differences between the FP and RS groups with regard to distress and OC risk perceptions, while statistically significant, were not overly large. Another possibility is while the abnormal screening result may have set the stage for the teachable moment (i.e., distress and risk perceptions were present) the intervening variable of notification that the abnormal result was a false positive may have led these women to experience relief and the desire to avoid thinking about issues relevant to their screening experience (i.e., receiving additional health related information). Finally, we did not assess McBride et al.’s (McBride et al., 2008) third criteria for defining a teachable moment, that an event challenge self concept or social role, and this may contribute to the present findings. Alternatively, it is possible that receipt of a false positive OC screening test result is indeed a potential teachable moment; however, our study methods were not capable of adequately documenting this. We used expressed interest in receipt of additional health-related information as our index of whether receipt of a false positive OC screening test result represented a “teachable moment.” While this is similar to previous research (Ostbye et al., 2003), other research has used other indices such as “engagement” in an intervention (McBride et al., 2008) or actual behavior change (Geller et al., 2006; Gritz et al., 1991; McBride et al., 1999) to define a teachable moment. So there is a lack of consensus in the literature regarding what indices might best document the teachable moment. In addition, the timing of our assessment of interest in receiving additional health-related information could have been suboptimal. It may be the teachable moment, the period of time when an individual is most motivated to change behavior, occurred earlier or perhaps even later than the 1 Month Follow-up Assessment when we assessed interest in receiving additional health information. For some events, the period of time when motivation to change behavior is increased (i.e., the teachable moment) might occur rather quickly after an event. For other events, the teachable moment might occur later, perhaps after an individual has time to sufficiently process and resolve the threat posed by that event. In addition, the size of the teachable moment, the temporal window of opportunity when motivation to change behavior is elevated, may differ across events and individuals. These are all issues which remain to be addressed by future research.
As interest in health-related information was assessed at only a single point in time, we do not know not whether interest decreased in the FP group as a result of their abnormal screening test or if interest increased in the RS group following their normal test result – or both. Future research could resolve this question by including longitudinal measures of information interest as well as measures of positive and negative affect. Longitudinal assessment would enable determination of whether interests go up or down over time in the two groups and whether these ups or downs are linked to changes in affect over time. Resolving this question has important theoretical and practical implications. Some evidence suggests participation in routine cancer screening and receipt of a normal test result can enhance feelings of well-being and positive affect (Gaugler et al., 2006; J. Wardle et al., 2003). Consistent with Frederickson’s Broaden-and-Build theory (Fredrickson, 2001) this may have increased interest in receiving additional health-related information in the RS group. According to this theory, the experience of well-being and positive emotion can broaden one's perspective while the experience of distress narrows it. Thus the greater interest in receipt of health-related information evident in the RS group may reflect an increase in openness and exploration attributable to a boost in well-being and positive affect after their successful participation in routine OC screening. In contrast, the distress experienced by the FP group after receipt of an abnormal OC screening test result may have narrowed their focus to the problem at hand and limited their ability to accommodate additional health-related information (Fredrickson, 2001; Fredrickson & Losada, 2005). Consistent with this view, IES distress levels in the FP group were most strongly correlated with interest in receiving additional information about OC cancer risk.
The possibility that interest in health-related information was enhanced in the RS group suggests that participation in routine cancer screening and receipt of a normal screening test result might represent a kind of teachable moment as well. In this case, positive affect and well-being engendered by their positive cancer screening experience may make these women more receptive to health information and behavior change interventions. To date, very little research has investigated whether positive affect increases motivation for health behavior change (Charlson et al., 2007; Folkman & Moskowitz, 2000; Kelsey et al., 2006). However, future research might benefit from an increased focus on the psychological impact of successful participation in routine cancer screening and the possibility that any well-being and positive affect that might result could be used to enhance positive health behavior change.
In summary, the concept of the teachable moment has broad clinical appeal as its motivational power could potentially be harnessed to foster health behavior changes that could serve to prevent health problems and enhance prognosis associated with existing health conditions (Demark-Wahnefried, Aziz, Rowland, & Pinto, 2005). In addition, the concept of the teachable moment has important theoretical implications for our understanding of factors that enhance or impede successful health behavior change. However, the concept of the “teachable moment” has largely been used descriptively and rather indiscriminately in the literature to date. Only recently has a characterization of the teachable moment been proposed (McBride et al., 2008) and there is a distinct paucity of hypothesis-driven research examining the teachable moment phenomenon. Lawson and Flocke (2008) have also recently published a mini review and concept analysis of the teachable moment. However, research is needed to further characterize the teachable moment and understand its limitations and potential. Specifically, our data suggest a need for a more precise and careful consideration of what types of events may or may not represent a teachable moment. Furthermore, more work needs to be done to identify the size and timing (relative to a triggering event) of the window of opportunity that represents the teachable moment.
Acknowledgments
This research was supported by grants CA084036 and CA096558 from the National Institutes of Health.
References
- Andrykowski MA, Boerner LM, Salsman JM, Pavlik E. Psychological response to test results in an ovarian cancer screening program: a prospective, longitudinal study. Health Psychol. 2004;23(6):622–630. doi: 10.1037/0278-6133.23.6.622. [DOI] [PubMed] [Google Scholar]
- Andrykowski MA, Pavlik EJ. Response to an abnormal ovarian cancer-screening test result: Test of the social cognitive processing and cognitive social health information processing models. Psychol Health. doi: 10.1080/08870440903437034. (in press). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker AH, Wardle J. Increasing fruit and vegetable intake among adults attending colorectal cancer screening: the efficacy of a brief tailored intervention. Cancer Epidemiol Biomarkers Prev. 2002;11(2):203–206. [PubMed] [Google Scholar]
- Charlson ME, Boutin-Foster C, Mancuso CA, Peterson JC, Ogedegbe G, Briggs WM, et al. Randomized controlled trials of positive affect and self-affirmation to facilitate healthy behaviors in patients with cardiopulmonary diseases: rationale, trial design, and methods. Contemp Clin Trials. 2007;28(6):748–762. doi: 10.1016/j.cct.2007.03.002. [DOI] [PubMed] [Google Scholar]
- Demark-Wahnefried W, Aziz NM, Rowland JH, Pinto BM. Riding the crest of the teachable moment: promoting long-term health after the diagnosis of cancer. J Clin Oncol. 2005;23(24):5814–5830. doi: 10.1200/JCO.2005.01.230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DePriest PD, DeSimone CP. Ultrasound screening for the early detection of ovarian cancer. J Clin Oncol. 2003;21(10 Suppl):194s–199s. doi: 10.1200/JCO.2003.02.054. [DOI] [PubMed] [Google Scholar]
- Folkman S, Moskowitz JT. Positive affect and the other side of coping. Am Psychol. 2000;55(6):647–654. doi: 10.1037//0003-066x.55.6.647. [DOI] [PubMed] [Google Scholar]
- Fredrickson BL. The role of positive emotions in positive psychology. The broaden-and-build theory of positive emotions. Am Psychol. 2001;56(3):218–226. doi: 10.1037//0003-066x.56.3.218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredrickson BL, Losada MF. Positive affect and the complex dynamics of human flourishing. Am Psychol. 2005;60(7):678–686. doi: 10.1037/0003-066X.60.7.678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freund KM, D'Agostino RB, Belanger AJ, Kannel WB, Stokes J., 3rd Predictors of smoking cessation: the Framingham Study. Am J Epidemiol. 1992;135(9):957–964. doi: 10.1093/oxfordjournals.aje.a116407. [DOI] [PubMed] [Google Scholar]
- Ganz PA. A teachable moment for oncologists: cancer survivors, 10 million strong and growing! J Clin Oncol. 2005;23(24):5458–5460. doi: 10.1200/JCO.2005.04.916. [DOI] [PubMed] [Google Scholar]
- Gaugler JE, Pavlik E, Salsman JM, Andrykowski MA. Psychological and behavioral impact of receipt of a "normal" ovarian cancer screening test. Prev Med. 2006;42(6):463–470. doi: 10.1016/j.ypmed.2006.02.004. [DOI] [PubMed] [Google Scholar]
- Geller AC, Emmons KM, Brooks DR, Powers C, Zhang Z, Koh HK, et al. A randomized trial to improve early detection and prevention practices among siblings of melanoma patients. Cancer. 2006;107(4):806–814. doi: 10.1002/cncr.22050. [DOI] [PubMed] [Google Scholar]
- Gorin AA, Phelan S, Hill JO, Wing RR. Medical triggers are associated with better short- and long-term weight loss outcomes. Prev Med. 2004;39(3):612–616. doi: 10.1016/j.ypmed.2004.02.026. [DOI] [PubMed] [Google Scholar]
- Gritz ER, Fingeret MC, Vidrine DJ, Lazev AB, Mehta NV, Reece GP. Successes and failures of the teachable moment: smoking cessation in cancer patients. Cancer. 2006;106(1):17–27. doi: 10.1002/cncr.21598. [DOI] [PubMed] [Google Scholar]
- Gritz ER, Nisenbaum R, Elashoff RE, Holmes EC. Smoking behavior following diagnosis in patients with stage I non-small cell lung cancer. Cancer Causes Control. 1991;2(2):105–112. doi: 10.1007/BF00053129. [DOI] [PubMed] [Google Scholar]
- Haug K, Fugelli P, Aaro LE, Foss OP. Is smoking intervention in general practice more successful among pregnant than non-pregnant women? Fam Pract. 1994;11(2):111–116. doi: 10.1093/fampra/11.2.111. [DOI] [PubMed] [Google Scholar]
- Horowitz M, Wilner N, Alvarez W. Impact of Event Scale: a measure of subjective stress. Psychosom Med. 1979;41(3):209–218. doi: 10.1097/00006842-197905000-00004. [DOI] [PubMed] [Google Scholar]
- Humpel N, Magee C, Jones SC. The impact of a cancer diagnosis on the health behaviors of cancer survivors and their family and friends. Supportive Care in Cancer. 2007;15(6):621–630. doi: 10.1007/s00520-006-0207-6. [DOI] [PubMed] [Google Scholar]
- Kelsey KS, DeVellis BM, Begum M, Belton L, Hooten EG, Campbell MK. Positive affect, exercise and self-reported health in blue-collar women. Am J Health Behav. 2006;30(2):199–207. doi: 10.5555/ajhb.2006.30.2.199. [DOI] [PubMed] [Google Scholar]
- Lawson PJ, Flocke SA. Teachable moments for health behavior change: A concept analysis. Patient Educ Couns. 2009;76(1):25–30. doi: 10.1016/j.pec.2008.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loss RW, Hall WJ, Speers DM. Evaluation of early airway disease in smokers: cost effectiveness of pulmonary function testing. Am J Med Sci. 1979;278(1):27–37. doi: 10.1097/00000441-197907000-00004. [DOI] [PubMed] [Google Scholar]
- Marks P, Williams R. Alcohol-related road traffic accidents: promoting a lower alcohol strategy. Clin Med. 2007;7(4):348–350. doi: 10.7861/clinmedicine.7-4-348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McBride CM, Emmons KM, Lipkus IM. Understanding the potential of teachable moments: the case of smoking cessation. Health Educ Res. 2003;18(2):156–170. doi: 10.1093/her/18.2.156. [DOI] [PubMed] [Google Scholar]
- McBride CM, Pirie PL, Curry SJ. Postpartum relapse to smoking: a prospective study. Health Educ Res. 1992;7(3):381–390. doi: 10.1093/her/7.3.381. [DOI] [PubMed] [Google Scholar]
- McBride CM, Puleo E, Pollak KI, Clipp EC, Woolford S, Emmons KM. Understanding the role of cancer worry in creating a "teachable moment" for multiple risk factor reduction. Soc Sci Med. 2008;66(3):790–800. doi: 10.1016/j.socscimed.2007.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McBride CM, Scholes D, Grothaus LC, Curry SJ, Ludman E, Albright J. Evaluation of a minimal self-help smoking cessation intervention following cervical cancer screening. Prev Med. 1999;29(2):133–138. doi: 10.1006/pmed.1999.0514. [DOI] [PubMed] [Google Scholar]
- Ostbye T, McBride C, Demark-Wahnefried W, Bastian L, Morey M, Krause KM, et al. Interest in healthy diet and physical activity interventions peripartum among female partners of active duty military. Mil Med. 2003;168(4):320–325. [PubMed] [Google Scholar]
- Taylor KL, Cox LS, Zincke N, Mehta L, McGuire C, Gelmann E. Lung cancer screening as a teachable moment for smoking cessation. Lung Cancer. 2007;56(1):125–134. doi: 10.1016/j.lungcan.2006.11.015. [DOI] [PubMed] [Google Scholar]
- van Nagell JR, Jr, DePriest PD, Reedy MB, Gallion HH, Ueland FR, Pavlik EJ, et al. The efficacy of transvaginal sonographic screening in asymptomatic women at risk for ovarian cancer. Gynecol Oncol. 2000;77(3):350–356. doi: 10.1006/gyno.2000.5816. [DOI] [PubMed] [Google Scholar]
- Wardle FJ, Collins W, Pernet AL, Whitehead MI, Bourne TH, Campbell S. Psychological impact of screening for familial ovarian cancer. J Natl Cancer Inst. 1993;85(8):653–657. doi: 10.1093/jnci/85.8.653. [DOI] [PubMed] [Google Scholar]
- Wardle J, Williamson S, Sutton S, Biran A, McCaffery K, Cuzick J, et al. Psychological impact of colorectal cancer screening. Health Psychol. 2003;22(1):54–59. doi: 10.1037//0278-6133.22.1.54. [DOI] [PubMed] [Google Scholar]