Abstract
Parents’ concerns about their children’s development were examined prospectively at 14, 24, and 36 months for 89 younger siblings of a child with autism. Parent reported concern was high at all ages (40–75%) and was higher at 24 and 36 months in children with ASD than non-ASD outcomes (p < .05). Communication concerns were reported most frequently. Parent concern compared to impairment classification based on concurrent standardized tests provided better specificity than sensitivity, and was better for communication than social functioning. Parent communication concern (but not social concern) at 24 months and 36 months predicted ASD versus non-ASD outcome; however, children’s impairment on standardized tests yielded greater predictive value at all ages (p < .001). Close monitoring of this at risk group is warranted.
Keywords: Autism, Parent concern, Communication, Social, Screening, Standardized assessment
Introduction
The importance of early detection of autism spectrum disorders (ASD) is widely recognized (e.g., Johnson and Myers 2007), largely due to advances in the neurosciences pertaining to neuroplasticity, revealing the importance of early experience in brain development. Early detection of ASD facilitates enrollment into early intervention, likely improving outcome (Dawson et al. 2010; Landa et al. 2011; Sallows and Graupner 2005). In order to detect ASD early, professionals rely heavily on parents’ report of concerns about their young child’s development. For developmental problems in general, parent concern has been considered an effective screening mechanism (Glascoe 1997, 1999). Only two studies have examined parent concerns prospectively prior to the time of diagnosis with a specific focus on ASD (Wetherby et al. 2008; Ozonoff et al. 2009). In the present study, we add to this literature by examining the implications of parent concern, or lack thereof, about toddlers at high genetic risk for ASD within a prospective, longitudinal study.
Most published reports of parent concerns about children with ASD are retrospective, acquiring such information usually well after the diagnosis had been given. Those studies identify the average age of first concern as being about 18 months of age (Howlin and Asgharian 1999), with parents first reporting concern to professionals between 18 and 26 months (e.g., Young et al. 2003; De Giacomo and Fombonne 1998), but diagnosis of ASD occurring after age 3 years (Mandell et al. 2006). In a study of young children recruited through a clinic sample referred due to concerns of ASD, parent concern was reported as early as 14 months (Chawarska et al. 2007). That study identified a relation between age of first concern and severity of ASD with first concerns arising at or before age 10 months being associated with a diagnosis of autism more often than Pervasive Developmental Disorder-Not Otherwise Specified (PDD-NOS) at age 4 years. When first concerns arose between 11 and 18 months, later diagnosis of autism or PDD-NOS were equally likely (Chawarska et al. 2007). While the nature of parents’ first concerns vary from child to child, the most commonly reported concerns involve communication development, followed by social difficulties for children later diagnosed with autism (Chawarska et al. 2007; De Giacomo and Fombonne 1998; Young et al. 2003). However, the nature of developmental concerns reported by parents has not consistently distinguished ASD from non-ASD (Trillingsgaard et al. 2005).
Most pediatric practices do not routinely screen for ASD (Dosreis et al. 2006; Gillis 2009). However, pediatricians often ask open-ended questions regarding parents’ development concerns about their children. It is important to empirically determine how effective this practice is in identifying developmental impairment as well as autism spectrum disorders. In a study of a general pediatric population that focused on parent concerns about communication, parents were asked about any concerns they had, then all children were evaluated using a standardized communication assessment (Wetherby et al. 2008). In the youngest children (under 20 months of age), parents often failed to identify a communication concern when communication skills were documented as delayed on the standardized assessment. In slightly older children (ages 21–24 months), parents frequently expressed concern about communication delay despite children’s age-appropriate scores on the standardized assessment. This was true for the general pediatric population as a whole, as well as for the ASD subgroup.
Routine screening for developmental delays and for ASD is particularly important with regard to young children whose parents already have an older child with ASD given the younger child’s genetic risk for ASD and milder impairments. A study by McMahon et al. (2007) found that parents who had an older child with ASD were more likely to report developmental concerns regarding a younger sibling aged 12–24 months compared to parents with age-matched children having no family history of ASD. Additionally, they reported higher levels of parent concern being associated with lower performance on cognitive and language measures. McMahon et al. (2007) examined this relation at one point in time, so it was not clear how parent concern may change in this at-risk sample over time. Only one study has used a prospective, longitudinal design to examine this issue in later-born siblings of children with ASD. In that study, Ozonoff et al. (2009) compared parent concern about children at ages 6, 12, and 18 months of age who did and did not have an older sibling with ASD. They found that parents who already had one child with ASD reported more concerns about autism symptom-related behaviors (e.g., communication, social, stereotyped behavior), assessed using an open-ended query, at ages 12 and 18 months in their later-born children who developed ASD than about those who did not develop ASD, and compared to parents having no children with ASD. When parents of children with ASD reported first concerns about their later-born children at 6 months of age, the concerns were most often about social development. When first concerns were reported at 12 or 18 months, the concern was most often about communication skills. However, parents’ concerns about ASD-related behaviors from 6 to 18 months were of limited utility in predicting 36-month ASD diagnosis in younger siblings of children with ASD as shown by high specificity but low sensitivity at most ages.
A question not addressed by Ozonoff et al. (2009) regards whether parent concern about later-born siblings of children with ASD has predictive validity for ASD after 18 months of age. Predictive validity of parent concern for ASD may increase with child age. Ozonoff et al. (2009) queried parents of 6- to 18–month-olds regarding concerns, then provided diagnostic assessments to generate diagnostic outcome classification at 36 months of age. They examined concurrent validity of number of ASD-concerns in relation to children’s ADOS total scores and Mullen Early Learning Composite scores as well as how parent concerns from the earlier queries (at child age 6–18 months) predicted 36-month outcome classification. In our prospective, longitudinal study of younger siblings of children with autism, we examined, concurrently and prospectively, parent concerns of children aged 14–36 months in relation to the children’s concurrent standardized test performance and 36-month diagnostic outcome classification as ASD or non-ASD. We specifically examined how parent social and communication concerns related to similar domains on the ADOS and Mullen Scales of Early Learning. This design provides essential information about the accuracy and validity of parent concerns regarding development in children at high risk for ASD and milder disorders (Folstein and Rutter 1977; Fombonne 2003), eliminating biases that exist in retrospective parent report studies when there are time lapses between the first concern and interview, and eliminating biases related to parents’ recall once their child is diagnosed with autism (Lord, Shulman, et al. 2004). We addressed three questions. (a) Are parents of children with autism concerned about their younger child’s development, and if so, what is the nature of the concerns? (b) How do parent concerns about communication and social functioning (core autism deficits) at each age relate to later ASD diagnosis? (c) What is the relation between parent concerns and child performance on standardized measures of communication and social functioning?
Method
This study was approved by the Johns Hopkins Medical Institutional Review Board; all families gave written informed consent for participation.
Participants
Participants were younger siblings (N = 89; 47 males) of a proband with idiopathic autism. These siblings were part of a federally funded research project focused on understanding early markers for, and developmental trajectory associated with, ASD. Parents identified race and ethnicity of the children as 86.52% Caucasian, 1.2% African-American, 1.2% Latino, 8.99% multi-racial, and 2% unspecified. Socio-economic status (SES; Hollingshead 1975) ranged from 30 to 66 (M = 57.36, SD = 8.97) with higher scores indicating higher SES.
Probands with autism met diagnostic criteria for autism on the Autism Diagnostic Observation Schedule (ADOS; Lord et al. 2002), Autism Diagnostic Interview-Revised (ADI-R; Lord et al. 1994), and clinical judgment (except two cases whose ADOS classification was ASD). Exclusion criteria for younger siblings were: primary language exposure other than English, birth weight <2,500 g, gestational age <35 weeks, severe birth trauma, head injury, prenatal illicit drug or excessive alcohol exposure, known genetic disorder that would confer increased risk for autism (e.g., fragile X), and severe birth defects.
At 36 months of age, children received outcome classification of ASD (n = 24) or Non-ASD (n = 65) by raters who were unaware of parent reported concerns about the child. Children in the ASD group (n = 24) met ADOS algorithm criteria for autism or ASD, and clinical judgment for autism or PDD-NOS.
Procedure
Children received developmental assessments at 14 (M = 14.22; SD = .48), 24 (M = 24.28; SD = .68), and 36 months of age (M = 36.47; SD = .62). Assessments were conducted at the Kennedy Krieger Institute or Spaulding Rehabilitation Center’s LADDERS program by a master’s or Ph.D. level professional who had experience with young children with autism. We attempted to keep examiners unaware of the child’s group status by asking parents not to reveal whether the child was a baby sibling of a child with autism or a low-risk control child with no family history of autism (given that the larger study included both groups). In most cases, examiners were indeed unaware of the child’s group status. Parents completed questionnaires about whether they had concern regarding their child’s development at each assessment. Some parents did not complete the questionnaire at one or two datapoints, yielding an n of 75, 73, and 63 at 14, 24, and 36 months, respectively.
Measures
Measures administered at each age (unless noted) that are relevant to this report are described below.
Parental perceptions about children’s developmental difficulties were assessed through three brief paper-and-pencil questionnaires, each containing an open-ended question requesting that parents specify current concerns about their children. The first questionnaire was an intake form asking parents if they presently had concerns about their child. Permissible responses were “Yes” or “No”. If “Yes”, parents were requested to list their concerns. The second questionnaire was the Communication and Symbolic Behavior Scale Developmental Profile-Caregiver Questionnaire (Wetherby and Prizant 2002), which presented four open-ended questions regarding children’s (a) communication changes, (b) strengths/assets, (c) concerns about development, and (d) anything else regarding the child’s development that parents wished to share. The third questionnaire was the Sensory Profile (Dunn 1999), which had two open-ended questions regarding children’s strengths and parental concerns.
Parent responses regarding concerns about their children on all three questionnaires were tallied and categorized with no attempt to prioritize concerns. This information was collected prior to the start of the child’s evaluation and prior to any feedback given by the clinician regarding the child’s performance. Responses were categorized into the following domains: communication (including speech, language, communication, and social communication), motor (including fine and gross), social, behavior/temperament (including stereotyped/repetitive behaviors and interests; challenging behaviors such as aggression or negativity; temperamental characteristics such as strong-willed or stubborn), sensory (including sensory defensiveness or sensory seeking), other (including anxiety, adaptive skills, somatic or medical issues, etc.) or “No Response” by coders who were unaware of the child’s diagnostic status. Examples of parent reported concerns included, “doesn’t say words” (communication), “not pointing” (communication), “flaps hands when excited” (behavior/temperament), “behavior can be very difficult, gets very upset, does not back down” (behavior/temperament), “clumsy gross motor coordination” (motor), “low muscle tone” (motor), “ongoing sensory integration issues” (sensory), “licking metal objects” (sensory), “doesn’t seek peers” (social), “joint attention” (social), “food allergies” (other), and “seizures” (other). For each category, responses were dichotomized to represent Concern versus No Concern. If the concerns section was left blank but all other sections were completed, or if parents indicated “None” or “N/A”, this was coded as “No Concern.” If a parent reported the same or similar concern on more than one form, it was counted as one concern and placed in the appropriate category. If the parent reported a different concern on each form, each was counted as separate concern and placed in the appropriate category. For coding reliability, two raters coded 25% of parent concern forms, and intraclass correlation coefficients were calculated. Intraclass correlation coefficients were acceptable for all seven codes and ranged from .61 for Behavior/Temperament to .85 for Communication with mean intraclass correlation coefficient of .75 across the seven categories (all p < .001).
The Receptive and Expressive Language scales of the Mullen Scales of Early Learning (MSEL; Mullen, 1995) were used as the criterion standard to document language delay (Mean T-score = 50; SD = 10). The criterion for language delay was defined as a T score greater than 1.5 standard deviations below the mean (≤34) on either of these scales.
The ADOS (Lord et al. 2002) was used to document the presence of autism symptoms in social interaction, communication, play, and repetitive behaviors. This semi-structured play-based assessment has standardized administration and scoring schema (no age norms). Children completed Module 1 (minimal to no language) or Module 2 (non-echoed phrase speech). The algorithm provides ASD or autism cut-off scores for the Reciprocal Social Interaction and Communication domains, and a separate diagnostic classification cut off for ASD or autism based on combined scores from these two domains. Criteria for social and communication impairments on the ADOS were defined as meeting algorithm criteria for ASD or autism on the Reciprocal Social Interaction or Communication domain.
Statistical Procedures
All data are presented cross-sectionally by age. We calculated descriptive statistics to address the first question, regarding presence and nature of parent concerns. We conducted Fisher exact tests (2 × 2) to test for differences in number of parent-reported concern categories (single concern category vs. no concern; multiple concern categories vs. no concern) by diagnostic outcome group (ASD vs. non-ASD).
To address the second question regarding predictive validity, we conducted logistic regression analyses to determine how well parent concerns about children’s developmental difficulties at 14 and 24 months predicted outcome classification of ASD versus non-ASD at 36 months. Regarding concurrent validity, we conducted logistic regression analyses to determine how well parent concerns about children’s developmental difficulties at 36 months related to outcome classification of ASD versus non-ASD at 36 months.
To address the third question, regarding the concurrent relation between parents’ concerns and children’s standardized test performance on measures of communication and social functioning at each age, we calculated sensitivity and specificity rates. Parent perceptions of developmental difficulties represented the screening test and child performance on the MSEL and ADOS served as criterion measures for communication and social functioning. Sensitivity refers to the proportion of children who have impairment and are correctly identified as having impairment by the screening test (“true positives”; Aylward 1994). Specificity is the proportion of children who do not have impairment and are correctly identified as not having impairment by the screening test (“true negatives”; Aylward 1994). In addition, we provided descriptive comparisons for rates of parent reported concern as well as rates of impairment per standardized assessments.
Results
Parent Concern Regarding Any Developmental Domain
Most parents of children with ASD outcomes (about 75%) listed a concern in at least one developmental domain at all three ages. Fewer parents of children with non-ASD outcomes, but still over half (58.2%), listed concern in at least one domain at 14 months, dropping to 41.5 and 40.9% at 24 and 36 months, respectively (Table 1).
Table 1.
Percentage of parents reporting developmental concerns by child age and outcome classification
| Concerns | 14 months | 24 months | 36 months |
|---|---|---|---|
| ASD group | |||
| 1 concern category | 75.0 | 70.0 | 78.9 |
| ≥2 concern categories | 60.0 | 65.0 | 52.6 |
| Non-ASD group | |||
| 1 concern category | 58.2 | 41.5 | 40.9 |
| ≥2 concern categories | 40.0 | 20.8 | 27.3 |
At 14 months, the presence of any type of parent concern, regardless of the number of developmental domains listed, was unrelated to presence or absence of ASD diagnosis at age three (p = .28 and .19, respectively) when examining predictive validity of parent concern early in the child’s life. However, when examining predictive validity at 24 months, the presence of single or multiple concern categories was significantly associated with an ASD outcome at age three (Phi = .42 p <.001 for concern regarding a single domain; Phi = −.25, p = .038 for concern regarding multiple domains). In terms of concurrent validity, at 36 months, parents with concerns in multiple categories were significantly more likely to have a child with an ASD outcome as opposed to a non-ASD outcome (Phi = −.24, p <. 001).
The most frequently reported concern at all ages involved communication development, with 48, 28.8, and 27.0% of parents from the overall sample specifying such concerns at 14, 24, and 36 months, respectively (Table 2). This phenomenon held true for both the ASD and non-ASD groups at 14 months, but at 24 and 36 months, the most commonly reported concern in the ASD group was communication; in the non-ASD group, the most commonly reported concern regarded behavior/temperament. For the overall sample, the second most frequently reported concern involved behavior/temperament at 14 months (20.0%) and 24 months (24.7%), and both social development and behavior/temperament at 36 months (both 20.6%). Because communication and social impairment are diagnostic criteria for autism, the remainder of the analyses focused on parent concern about these aspects of development.
Table 2.
Percentage of parents reporting concerns by developmental domain and child age
| Developmental Domain | 14 months (N = 75) |
24 months (N = 73) |
36 months (N = 63) |
|---|---|---|---|
| Communication | 48.0 | 28.8 | 27.0 |
| Social | 13.3 | 8.2 | 20.6 |
| Motor | 18.7 | 8.2 | 7.9 |
| Behavior/temperament | 20.0 | 24.7 | 20.6 |
| Sensory | 10.7 | 9.6 | 7.9 |
| Other (e.g., adaptive, medical, somatic) | 16.0 | 12.2 | 17.5 |
Since some parents described multiple types of concerns about their child, the percentages in this table do not equal 100%
Parent Concerns About Communication and Social Functioning in Predicting Outcome Classification
Logistic regression analyses were conducted to assess whether parent concerns about communication or social functioning at each age were related to ASD outcome when examining predictive validity (14- and 24- month parent concerns in relation to 36-month ASD outcome) and concurrent validity (36-month parent concerns in relation to 36- month ASD outcome). Results showed that parent communication concerns at 24 months (X2(1, N = 73) = 12.40, p <.001; B = 1.99, SE = .59) and 36 months (X2(1, N = 63) = 12.57, p <.001; B = 2.16, SE = .64), but not 14 months, were significantly related to ASD outcome at 36 months; models that included parent social concerns either alone or in addition to communication concerns did not add predictive value. For 24-month-olds, the model with parent communication concerns explained 23.7% (Nagelkerke R-square) of the variance in ASD versus non-ASD outcome, correctly classifying 76.7% of cases (83% non-ASD cases, 60% ASD cases; c-statistic = .72, p = .005). For 36-month-olds, the model explained 25.6% (Nagelkerke R-Square) of the variance in ASD versus non-ASD outcome, correctly classifying 77% of cases (86.4% non-ASD cases, 57.9% ASD cases; c-statistic = .71, p = .006). These results indicate that the discriminative power of the logistic regression models at 24 and 36 months was significantly better than chance.
Children’s Standardized Test Performance in Predicting Outcome Classification
Logistic regression analyses using MSEL, ADOS Communication, and ADOS Reciprocal Social Interaction impairment (together in one model) were significantly related to 36-month ASD versus non-ASD outcome when using children’s performance scores on the standardized measures at 14 months (X2(3, N = 89) = 23.74, p <.001), 24 months (X2(3, N = 70) = 33.62, p <.001), and 36 months (X2(3, N = 89) = 75.08, p <.001). At 14, 24, and 36 months, the model explained 34.0%, 53.1%, and 82.8% of the variance (Nagelkerke R-Squares) in ASD versus non-ASD outcome, respectively. The model correctly classified 82% of cases (90.8% non-ASD cases, 58.3% ASD cases; c-statistic = .81, p < .001) for 14-month-olds, 84.3% of cases (95.7% non-ASD cases, 60.9% ASD cases; c-statistic = .87, p < .001) for 24-month-olds, and 89.9% of cases (100% non-ASD cases, 62.5% ASD cases; c-statistic = .97, p < .001) for 36-month olds. These results indicate that the discriminative power of the logistic regression models at 14, 24, and 36 months was significantly better than chance.
Parent Communication and Social Concern Compared to Children’s Test Performance
Sensitivity and Specificity
Sensitivity and specificity was calculated using presence of parental concern for the entire sample as the screening test and using standardized test results as the “gold standard” to examine concurrent relations at each time point. We combined the ASD and non-ASD groups to examine sensitivity and specificity issues for ecological validity purposes, as parents expressing first concerns to health care providers do not yet know whether their child will be diagnosed with ASD (Table 3). Sensitivity rates were below 70% across all measures of communication and social functioning and across ages, indicating that parents were infrequently concerned about children who met standardized test criteria for impairment. Although modest, the best sensitivity rates at all ages involved the relation between parent communication concerns and children’s impairment classification based on MSEL communication composite (61.54–63.64%). Specificity rates were higher than sensitivity rates at 24 and 36 months, ranging from 78 to 92% for all comparisons. Comparisons involving 14-month data revealed high specificity (>90%) for social functioning, but low specificity (56–61%) for communication functioning, regardless of whether the “gold standard” was MSEL or ADOS scores.
Table 3.
Relation of parents’ concerns about communication and social functioning with children’s communication and social performance on the MSEL and ADOS
| Age of child | Sensitivity (%) | Specificity (%) | False positive (%) | False negative (%) |
|---|---|---|---|---|
| 14 months | ||||
| Communication MSEL (N = 75) | 62.07 | 60.87 | 39.13 | 37.93 |
| Communication ADOS (N = 75) | 58.33 | 56.86 | 43.13 | 41.67 |
| Social ADOS (N = 75) | 16.28 | 90.63 | 9.38 | 83.72 |
| 24 months | ||||
| Communication MSEL (N = 73) | 61.54 | 78.33 | 21.67 | 38.46 |
| Communication ADOS (N = 59) | 50.00 | 79.49 | 20.51 | 50.00 |
| Social ADOS (N = 59) | 12.12 | 92.31 | 7.70 | 87.88 |
| 36 months | ||||
| Communication MSEL (N = 63) | 63.64 | 80.77 | 19.23 | 36.36 |
| Communication ADOS (N = 63) | 40.00 | 89.29 | 10.71 | 60.00 |
| Social ADOS (N = 63) | 24.14 | 82.35 | 17.65 | 75.86 |
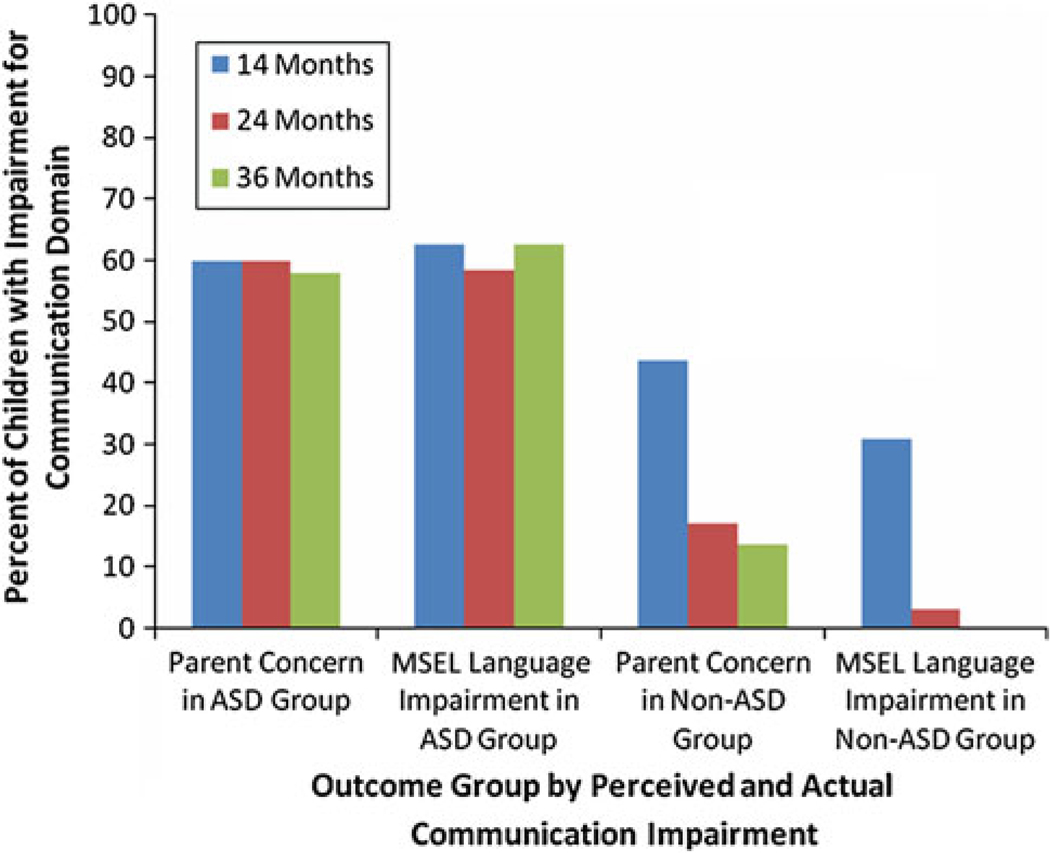
Disagreements Involving Communication Development Measured by MSEL
Disagreements involving the absence of parent report of communication concerns despite below age-level MSEL performance (false negatives) were similar across ages (37.93, 38.46, and 36.36%, respectively; Table 3). Disagreements involving parent concern despite age-appropriate MSEL performance (false positives) were high at 14 months of age (39.13%), but decreased thereafter (21.67, and 19.23% at 24 and 36 months, respectively). This type of disagreement involved 18, 13, and 10 children at 14, 24, and 36 months of age, respectively (representing 35 different children). Nine of these children were later diagnosed with ASD. Examination within the ASD group revealed that agreement between parent communication concern and MSEL impairment classification was high and stable over time (Fig. 1). However, within the non-ASD group, rates of parent communication concern were higher than rates of MSEL classification of communication impairment at all ages (Fig. 1).
Fig. 1.
Percentage of parents with concerns about children’s communication functioning and percent of children meeting criteria for impairment based on MSEL receptive and/or expressive language scale scores at 14, 24, and 36 months by ASD versus non-ASD outcome grouping
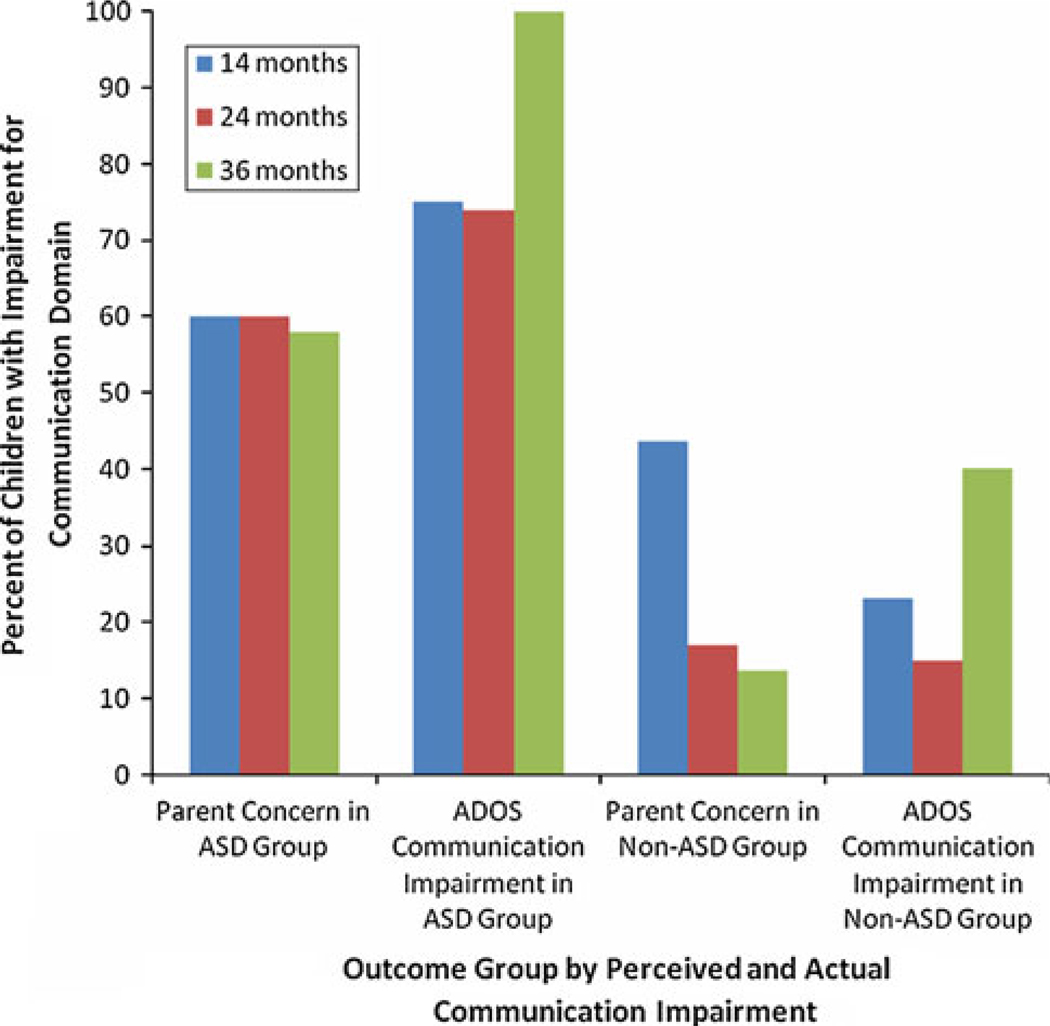
Disagreements Involving Communication and Social Functioning Measured by ADOS
Disagreement involving absence of parent report of communication concern despite abnormal ADOS algorithm Communication domain score (false negatives) were common, and increased with age: 41.67, 50.00, and 60.00% at 14, 24, and 36 months, respectively (Table 3). Figure 2 reveals that this disagreement was characteristic of the ASD group at all ages, but was true of the non-ASD group only at 36 months.
Fig. 2.
Percentage of parents with concerns about children’s communication functioning and percent of children meeting ASD or autism cutoff for ADOS communication domain at 14, 24, and 36 months by ASD versus non-ASD outcome grouping
In contrast, false positives occurred primarily at 14 months within the non-ASD group where parents more often expressed communication concern when children’s ADOS Communication domain score was within the non-ASD range (Table 3; Fig. 2). False positives were noted for 22, eight, and three children at 14, 24, and 36 months of age, respectively (representing 26 different children). Three of the 14-month-olds, and one additional 24-month-old were later diagnosed with ASD.
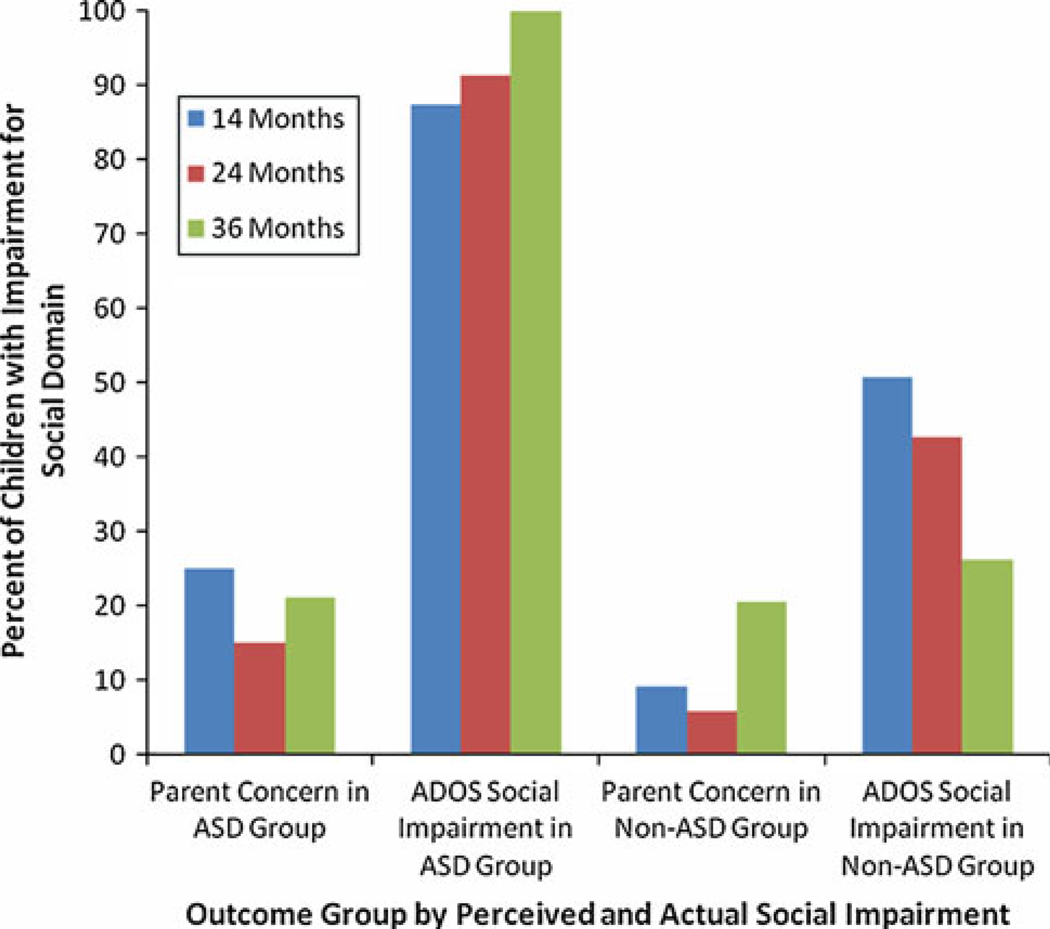
Disagreements between parent report of concerns about social functioning and ADOS Reciprocal Social Interaction algorithm classification were high at all ages in both groups (Fig. 3). The disagreements usually involved absence of parent concern when children met ADOS criteria for ASD or autism (false negatives), occurring in more than 75% of children at each age (Table 3). False positives were observed much less often, involving parents expressing concern about social functioning when children scored in the non-ASD range on the ADOS Reciprocal Social domain (see Table 3). This involved 3, 2, and 6 children at 14, 24, and 36 months of age, respectively (10 different children). Only one of these children, a 24-month-old, was later diagnosed with ASD.
Fig. 3.
Percentage of parents with concerns about children’s social functioning and percent of children meeting ASD or autism cutoff for ADOS reciprocal social interaction domain at 14, 24, and 36 months by ASD versus non-ASD outcome grouping
Discussion
This prospective, longitudinal study, involving younger siblings of children with autism aged 14–36 months, examined parent concern regarding their children’s development. Using open-ended questions, parents were asked to report concerns about their child’s development, a system similar to that used by pediatricians at well-visits. As early as 14 months of age, the majority of parents listed a concern in at least one developmental domain, and nearly half listed concerns representing multiple developmental domains. This is earlier than the average age of parent concern reported to professionals, which is 18–26 months (Young et al. 2003, De Giacomo and Fombonne 1998). With increasing age, fewer parents expressed concerns, and these concerns involved fewer domains of development. Parents of children with an ASD outcome reported concern more frequently than parents of children with non-ASD outcomes at all ages.
Consistent with the literature (De Giacomo and Fombonne 1998; Young et al. 2003; Chawarska et al. 2007; Ozonoff et al. 2009), the most frequently reported concern by parents in the present study involved communication. The second most frequently listed concerns involved behavior/temperament at 14 and 24 months, and both behavior/temperament and social development at 36 months of age. Few parents reported concern about social functioning until 36 months of age. Parents may have more difficulty identifying social impairment related to ASD at early ages. Perhaps social difficulties are less apparent to parents of toddlers because exposure to peers is as yet limited, thus limiting opportunities for comparison to typical development. It is possible that even if the younger sibling of a child with autism exhibits social impairment, the child may be less affected than the older sibling with ASD, leading to diminished parent concern.
Communication and social functioning are core deficits of autism, and thus, we focused on these developmental areas when examining predictive value of parent concern. Specificity of parent concern reached acceptable levels (American Academy of Pediatrics, Council On Children with Disabilities 2001), with parents usually expressing no concern given children’s typical performance on standardized assessments. However, sensitivity was below acceptable levels, with parents often failing to identify impairment when children scored in the impaired range on standardized measures. Agreement between parent concern and standardized test results for social functioning was lower than such agreement for communication functioning at all ages. Yet developmental impairment in communication and social development is detectable by trained clinicians in children with autism by 14 months (Landa et al. 2007).
Disagreement involving presence of parent reported concern and non-impaired standardized assessment scores (i.e., false positives) was noted for nine children with ASD outcome. One reason for such disagreement involved impairment being detected by one communication measure but not the other (i.e., child met criteria for impairment on MSEL but not ADOS or vice versa). For instance, parent concern about echolalia should be detected on the ADOS Communication domain, but not the MSEL since the latter measures language (e.g., vocabulary use and understanding) but not broader aspects of communication (gesture, echolalia/repetitive language usage, pragmatics). Another reason involved children demonstrating a mild impairment compared to peer group (1–1.5 standard deviations below the MSEL mean), but not meeting our clinical cut-off of greater than 1.5 standard deviations below the mean. The third reason was that the standardized tests were not designed to measure some aspects of development about which parents were concerned, such as articulation difficulties or social behavior with peers. This emphasizes the importance of using multiple measures to detect developmental impairment including assessments of milestones or acquired skills and assessments of qualitative social and communication behavior. It also obviates the need to establish an evidence base for setting thresholds for classification of impairment.
At each visit, clinicians completed a clinical judgment checklist to document concerns about the child in various domains (e.g., Speech or Articulation, Language, Social Communication, Social, Temperament, Behavior, Repetitive Interests, etc.). For all nine children with ASD whose parents’ concerns were not supported by direct assessment, clinicians had documented concerns involving at least the same domain(s) as listed by the parent (and unaware of parent report of concern in most cases). This highlights the importance of clinical expertise in assessing young children with autism, and the need to prioritize clinical judgment over standardized test scores, which may fail to detect subtle abnormal behaviors associated with early manifestation of ASD. As parents may recognize qualitative or subtle signs of developmental impairment in toddlers that are not detectable by existing standardized measures, the presence of parent concern, particularly in high risk children, should motivate frequent and close developmental surveillance or referral to experts in infant-toddler developmental disorders.
Disagreement involving absence of parent reported concern and impaired standardized assessment scores (i.e., false negatives) was higher than expected. In this genetic risk sample, some parents missed signs of developmental impairment, and parents had more difficulty identifying social impairments than communication impairments. These findings emphasize the importance of routine developmental screening, including ASD-specific screening, as recommended by the AAP (2007) for all children, with close monitoring of this genetic risk group.
Parent-reported communication concern at 24 months predicted ASD outcome at age three, indicating adequate predictive validity of the parent concern measure for this age, but not at 14 months, and not for parent reported social concern at either age. Similarly, concurrent validity of parent-reported communication concern, but not social concern, at 36 months in relation to ASD outcome was adequate. However, children’s standardized test performance for communication and social functioning at 14 and 24 months explained more variance in children’s ASD outcome at age 3 compared to parent concern suggesting better predictive validity for the standardized measures. Similarly, standardized test performance at 36 months had stronger concurrent relation to ASD outcome compared to parent concern in these domains.
Our findings suggest that eliciting parent concern in an open-ended manner should be considered a pre-screening measure given its low sensitivity and lower predictive value in relation to standardized assessments in predicting presence or absence of ASD outcome. Use of standardized questionnaires, such as the Parents’ Evaluation of Developmental Status (PEDS; Glascoe 1997, 1999) which provides both open-ended questions and specific probes regarding concerns in various domains, has documented validity and reliability as a universal developmental screener. It is also necessary to supplement universal screeners with autism-specific screeners, such as the Modified Checklist for Autism in Toddlers (M-CHAT; Robins et al. 1999) paired with the M-CHAT follow-up questionnaire to reduce false positives (Robins 2008; Kleinman et al. 2008). We recommend a call to action for pediatricians to listen closely to early parent concerns and to refer children for further assessment when concerns are identified on a screener or through parent report rather than taking a wait-and-see approach. Additionally, we recommend more widespread utilization of valid and reliable screening instruments by pediatricians as part of routine well-child visits. The AAP recommends universal screening for developmental impairments and autism with standardized tools (Johnson and Myers 2007) as these are effective in identifying developmental delays and autism (e.g., Wetherby et al. 2008; Kleinman et al. 2008). With earlier identification, children will have earlier entry into intervention services to best foster more positive outcomes. Continued research regarding efficacious interventions and best practices, utilizing models that incorporate parent training as part of the programs, is necessary to best serve children with developmental impairments.
Limitations
Our sample size at 36 months was lower than at younger ages since fewer parents answered the questions regarding developmental concerns at that age. Our study lacked a comparison group of low-risk children with no family history of ASD.
Conclusion
Younger siblings of children with autism are at increased risk for autism and milder developmental impairments. Screening and close monitoring of these children is recommended given the low sensitivity of parent concern and high rates of developmental impairment in this genetic risk group. It is important to keep in mind that the sensitivity of a screening tool as a whole, as well as sensitivity of specific items, varies with the age of the child and the characteristics of the sample being assessed (e.g., cognitive and adaptive level; whether recruited from a primary or tertiary care setting; see Snow and Lecavalier 2008). Parents should be educated at pediatric visits about ASD red flags and how behaviors may change at different developmental ages to help parents accurately identify and report concerning behaviors to professionals.
Acknowledgments
This research was supported in part by grants from the National Institute of Health MH59630 and 154MH066417, Pathfinders for Autism, National Alliance for Autism Research, Cure Autism Now, Autism Speaks, and Coalition for Autism, awarded to Rebecca Landa (Principal Investigator). We thank the families for their generous participation in this research. Sincere appreciation is expressed to Dr. Landa’s staff and to Dr. Margaret Bauman and her staff in the LADDERS program of Massachusetts General Hospital, who contributed to the data collection for this study.
Contributor Information
Christine Reiner Hess, Center for Autism and Related Disorders, Kennedy Krieger, Institute, 3901 Greenspring Avenue, Baltimore, MD 21211, USA.
Rebecca J. Landa, Email: landa@kennedykrieger.org, Center for Autism and Related Disorders, Kennedy Krieger, Institute, 3901 Greenspring Avenue, Baltimore, MD 21211, USA; Johns Hopkins University School of Medicine, Baltimore, MD, USA.
References
- American Academy of Pediatrics. Developmental surveillance and screening of infants and young children. Pediatrics. 2001;108(1):192–195. doi: 10.1542/peds.108.1.192. [DOI] [PubMed] [Google Scholar]
- Aylward G. Practioner’s guide to developmental and psychological testing. New York: Plenum Medical Book Company; 1994. [Google Scholar]
- Chawarska K, Paul R, Klin A, Hannigen S, Dichtel LE, Volkmar F. Parental recognition of developmental problems in toddlers with autism spectrum disorders. Journal of Autism and Developmental Disorders. 2007;37(1):62–72. doi: 10.1007/s10803-006-0330-8. [DOI] [PubMed] [Google Scholar]
- Dawson G, Rogers S, Munson J, Smith M, Winter J, Greenson J, Donaldson A, Varley J. Randomized, controlled trial of an intervention for toddlers with autism: The early start denver model. Pediatrics. 2010;125(1):e17–e23. doi: 10.1542/peds.2009-0958. Epub 2009 Nov 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Giacomo A, Fombonne E. Parental recognition of developmental abnormalities in autism. European Child and Adolescent Psychiatry. 1998;7:131–136. doi: 10.1007/s007870050058. [DOI] [PubMed] [Google Scholar]
- Dosreis S, Weiner CL, Johnson L, Newschaffer CJ. Autism spectrum disorder screening and management practices among general pediatric providers. Journal of Developmental and Behavioral Pediatrics. 2006;27(2 Supplement):S88–S94. doi: 10.1097/00004703-200604002-00006. [DOI] [PubMed] [Google Scholar]
- Dunn W. Sensory profile. San Antonio, TX: The Psychological Corporation; 1999. [Google Scholar]
- Folstein S, Rutter M. Infantile autism: A genetic study of 21 twin pairs. Journal of Child Psychology and Psychiatry. 1977;18(4):297–321. doi: 10.1111/j.1469-7610.1977.tb00443.x. [DOI] [PubMed] [Google Scholar]
- Fombonne E. Epidemiological surveys of autism and pervasive developmental disorders: An update. Journal of Autism and Developmental Disorders. 2003;33:365–382. doi: 10.1023/a:1025054610557. [DOI] [PubMed] [Google Scholar]
- Gillis JM. Screening practices of family physicians and pediatricians in 2 Southern states. Infants and Young Children. 2009;22(4):321–331. [Google Scholar]
- Glascoe FP. Parents’ concerns about children’s development: Prescreening technique or screening test? Pediatrics. 1997;99:522–528. doi: 10.1542/peds.99.4.522. [DOI] [PubMed] [Google Scholar]
- Glascoe FP. Using parents’ concerns to detect and address developmental and behavioral problems. Journal of the Society of Pediatric Nurses. 1999;4(1):24–35. doi: 10.1111/j.1744-6155.1999.tb00077.x. [DOI] [PubMed] [Google Scholar]
- Hollingshead AB. Four-factor index of social status. New Haven, CT: Yale University; 1975. Unpublished manuscript. [Google Scholar]
- Howlin P, Asgharian A. The diagnosis of autism and Asperger syndrome: findings from a survey of 770 families. Developmental Medicine and Child Neurology. 1999;41(12):834–839. doi: 10.1017/s0012162299001656. [DOI] [PubMed] [Google Scholar]
- Johnson CP, Myers SM. Identification and evaluation of children with autism spectrum disorders. Pediatrics. 2007;120(5):1183–1215. doi: 10.1542/peds.2007-2361. [DOI] [PubMed] [Google Scholar]
- Kleinman JM, Robins DL, Ventola PE, Pandey J, Boorstein HC, Esser E, et al. The modified checklist for autism in toddlers: A follow-up study investigating the early detection of autism spectrum disorders. Journal of Autism and Developmental Disorders. 2008;38:827–839. doi: 10.1007/s10803-007-0450-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landa RJ, Holman KC, Garrett-Mayer E. Social and communication development in toddlers with early and later diagnosis of autism spectrum disorders. Archives of General Psychiatry. 2007;64(7):853–864. doi: 10.1001/archpsyc.64.7.853. [DOI] [PubMed] [Google Scholar]
- Landa RJ, Holman KC, O’Neill AH, Stuart E. Intervention targeting development of socially synchronous engagement in toddlers with autism spectrum disorder: A randomized controlled trial. Journal of Child Psychology and Psychiatry. 2011;52(1):13–21. doi: 10.1111/j.1469-7610.2010.02288.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lord C, Rutter M, DiLavore PC, Risi S WPS. Autism diagnostic observation schedule. Los Angeles: Western Psychological Services; 2002. [Google Scholar]
- Lord C, Rutter M, LeCouteur A. Autism diagnostic interview—revised: A revised version of a diagnostic interview for caregivers of individuals with possible pervasive developmental disorders. Journal of Autism and Developmental Disorders. 1994;24:659–685. doi: 10.1007/BF02172145. [DOI] [PubMed] [Google Scholar]
- Lord C, Shulman C, DiLavore P. Regression and word loss in autism spectrum disorders. Journal of Child Psychology and Psychiatry. 2004;45(5):936–955. doi: 10.1111/j.1469-7610.2004.t01-1-00287.x. [DOI] [PubMed] [Google Scholar]
- Mandell DS, Novak MM, Zubritsky CD. Factors associated with age of diagnosis among children with autism spectrum disorders. Journal of the American Academy of Child and Adolescent Psychiatry. 2006;45(6):657–659. [Google Scholar]
- McMahon CR, Malesa EE, Yoder PJ, Stone WL. Parents of children with autism spectrum disorders have merited concerns about their later-born infants. Research and Practice for Persons with Severe Disabilities. 2007;32(2):154–160. [Google Scholar]
- Mullen EM AGS. Mullen scales of early learning. Circle Pines, MN: American Guideline Service; 1995. [Google Scholar]
- Ozonoff S, Young GS, Steinfield MB, Hill MM, Cook I, Hutman T, et al. How early do parent concerns predict later autism diagnosis? Journal of Developmental and Behavioral Pediatrics. 2009;30:367–375. doi: 10.1097/dbp.0b013e3181ba0fcf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robins DL. Screening for autism spectrum disorders in primary care settings. Autism. 2008;12:537–556. doi: 10.1177/1362361308094502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robins DL, Fein D, Barton ML. Modified checklist for autism in toddlers (M-CHAT) 1999 Self-published. [Google Scholar]
- Sallows GO, Graupner TD. Intensive behavioral treatment for children with autism: Four-year outcome and predictors. American Journal on Mental Retardation. 2005;110(6):417–438. doi: 10.1352/0895-8017(2005)110[417:IBTFCW]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Snow AV, Lecavalier L. Sensitivity and specificity of the modified checklist for autism in toddlers and the social communication questionnaire in preschoolers suspected of having pervasive developmental disorders. Autism. 2008;12(6):627–644. doi: 10.1177/1362361308097116. [DOI] [PubMed] [Google Scholar]
- Trillingsgaard A, Sorenson EU, Nemec G, Jorgensen M. What distinguishes autism spectrum disorders from other developmental disorders before the age of 4 years? European Journal of Child and Adolescent Psychiatry. 2005;14:65–72. doi: 10.1007/s00787-005-0433-3. [DOI] [PubMed] [Google Scholar]
- Wetherby AM, Brosnan-Maddox S, Peace V, Newton L. Validation of the Infant-Toddler Checklist as a broadband screener for autism spectrum disorders from 9 to 24 months of age. Autism. 2008;12(5):487–511. doi: 10.1177/1362361308094501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wetherby AM, Prizant BM. Communication and symbolic behavior scales. Baltimore, MD: Brookes Publishing Co; 2002. [Google Scholar]
- Young RL, Brewer N, Pattison C. Parental identification of early behavioral abnormalities in children with autistic disorder. Autism. 2003;7(2):125–143. doi: 10.1177/1362361303007002002. [DOI] [PubMed] [Google Scholar]