Abstract
There are few studies that have assessed factors influencing infection control practices among health care workers (HCW) in nursing homes. We conducted a cross-sectional survey of HCWs (N = 392) in 4 nursing homes to assess whether knowledge, beliefs, and perceptions influence reported hand hygiene habits. Positive perceptions and beliefs regarding effectiveness of infection control in nursing homes were associated with reported appropriate glove use and fingernail characteristics, respectively, among HCWs. Further research on hand hygiene interventions, including targeted educational in-services should be conducted in the nursing home setting.
The potent mix of functionally dependent individuals and institutional environment of nursing homes creates a favorable setting for acquisition and transmission of infectious pathogens. Although several studies have addressed hand hygiene in hospital settings, few studies have examined hand hygiene in nursing homes.1-3 The purpose of this study was to examine the influence of knowledge, beliefs, and hand hygiene perception on infection control practices, including hand hygiene habits, gloving, and fingernail characteristics, among nursing home health care workers (HCWs).
Methods
Study design
A cross-sectional survey of nursing staff in nursing homes was utilized to assess knowledge, beliefs, perceptions and practices of hand hygiene-related infection control practices. The survey was conducted in February 2005 among 4 nursing homes in southeastern Michigan. An invitation to participate in infection control research was sent to 105 nursing homes: 22 reported interest and 13 homes agreed to participate. Nursing homes were approached based on proximity to the University of Michigan. The first 4 homes approached agreed to participate, providing sufficient sample size for the proposed analysis. The study was approved by the University of Michigan Medical Institutional Review Board.
Questionnaire
Data was collected via self-administered survey in each facility from registered nurses (RNs), nurse practitioners (NPs), licensed practicing nurses (LPN), and certified nursing assistants (CNAs). Full-time or part-time HCWs from all shifts were invited to participate. Three hundred ninety-two HCWs were eligible to take the survey and 330 had data available for analyses.
The survey instrument used in this study was based on earlier surveys described by Pittet et al4 and Kennedy et al.5 Questions included demographics and responses to the following content areas: hand hygiene, alcohol rub use, fingernails, glove use, and Centers for Disease Control and Prevention (CDC) hand hygiene guidelines. Summary variables were created to measure knowledge, beliefs about hand hygiene, beliefs about fingernails, perception of potential barriers to good hand hygiene, and hand hygiene practice. Frequency of handwashing was derived from reported number of times hands were washed during the shift divided by hours on shift.
Statistical methods
Participant characteristics were compared across facilities using χ2 tests and analysis of variance. The odds of better gloving and fingernail practices by occupational title were estimated using logistic regression with generalized estimating equations (GEE) to account for correlations among staff working in the same facility. The relationships among knowledge, beliefs, perception measures, and hand hygiene practices were assessed using linear and logistic regression with GEE, adjusted for occupational title and patients per shift hour. All analyses were conducted using SAS (V.9; SAS Institute, Cary, NC)
Results
A total of 343 of 392 questionnaires were returned, providing a response rate of 87.5%. Of the 343 participants, 330 responded to all questions of interest, and their characteristics are shown in Table 1. Figure 1 shows the proportion of subjects responding positively to hand hygiene practices. More than 80% of the participants believed that hand hygiene is useful, that gloves were useful for preventing infections, and that artificial nails are associated with higher counts of gram-negative bacteria. In contrast, only 39.5% of the participants were able to identify the correct (eg, 30 seconds) recommended duration of washing.
Table 1. Characteristics of the 330 participants overall and by facility.
| Overall | Facility 1 | Facility 2 | Facility 3 | Facility 4 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Characteristic | (536 beds) | (103 beds) | (230 beds) | (43 beds) | (160 beds) | P value* | |||||
| Total N | 330 | 71 | 115 | 42 | 102 | ||||||
| Occupation, % (n) | .31 | ||||||||||
| Nurse practitioner | 1.21 | (4) | 0 | (0) | 1.71 | (2) | 2.38 | (1) | 0.98 | (1) | |
| Registered nurse | 13.0 | (43) | 9.86 | (7) | 9.57 | (11) | 14.3 | (6) | 18.6 | (19) | |
| Licensed practicing nurse | 28.8 | (95) | 28.2 | (20) | 31.3 | (36) | 16.7 | (7) | 31.4 | (32) | |
| Certified nursing assistant | 57.0 | (188) | 62.0 | (44) | 57.4 | (66) | 66.7 | (28) | 49.0 | (50) | |
| Sex, % (n) | .45 | ||||||||||
| Female | 96.4 | (318) | 100.0 | (71) | 100.0 | (115) | 95.2 | (40) | 89.2 | (92) | |
| Age, yr | .12 | ||||||||||
| Mean (SD) | 35.9 | (11.6) | 35.0 | (12.1) | 37.4 | (12.0) | 38.7 | (13.3) | 33.7 | (9.7) | |
| Months in unit | .01 | ||||||||||
| Mean (SD) | 37.2 | (45.6) | 52.7 | (68.5) | 45.2 | (51.7) | 33.1 | (36.3) | 23.0 | (17.2) | |
| Months at facility | <.00l | ||||||||||
| Mean (SD) | 56.2 | (68.9) | 63.5 | (79.7) | 77.7 | (87.3) | 45.7 | (35.2) | 30.3 | (22.6) | |
| Knowledge | .03 | ||||||||||
| Mean (SD) | 4.9 | (1.0) | 4.9 | (1.0) | 4.7 | (0.9) | 5.1 | (1.2) | 5.0 | (0.9) | |
| Range | (3-8) | (3-7) | (3-7) | (3-8) | (3-7) | ||||||
| Hand infection beliefs | .49 | ||||||||||
| Mean (SD) | 38.6 | (4.5) | 38.5 | (4.2) | 38.3 | (5.3) | 38.4 | (3.7) | 39.2 | (4.0) | |
| Range | (0-42) | (24-42) | (0-42) | (31-42) | (20-42) | ||||||
| Fingernail beliefs | .16 | ||||||||||
| Mean (SD) | 13.6 | (4.2) | 14.12 | (4.1) | 13.7 | (4.6) | 12.3 | (4.8) | 13.8 | (3.4) | |
| Range | (0-18) | (0-18) | (0-18) | (2-18) | (4-18) | ||||||
| Perceptions | .78 | ||||||||||
| Mean (SD) | 30.8 | (5.7) | 31.1 | (5.7) | 31.1 | (6.0) | 30.2 | (5.0) | 30.6 | (5.4) | |
| Range | (3-36) | (3-36) | (5-36) | (15-36) | (10-36) | ||||||
| Good glove use, % (n)† | 67.1 | (228) | 72.0 | (54) | 70.8 | (85) | 50.0 | (21) | 66.0 | (68) | .07 |
| Good fingernail traits, % (n)‡ | 68.7 | (233) | 75.7 | (56) | 66.9 | (81) | 60.5 | (26) | 69.3 | (70) | .35 |
| Handwashing frequency/shift hour | |||||||||||
| Mean (SD) | 4.67 | (3.1) | 4.8 | (1.5) | 4.4 | (1.6) | 5.3 | (1.7) | 4.6 | (5.2) | .52 |
NOTE. There were 13 missing values for occupation, 104 for age, 58 for months in facility, 152 for months in unit, 26 for knowledge, 2 for fingernail beliefs, 23 for perceptions, 3 on glove use, 4 on fingernail traits, and 26 on handwashing frequency.
P value compares characteristics across facilities using χ2 tests for categorical characteristics and analysis of variance for continuous characteristics.
Good glove use was defined as using gloves 100% of the time when anticipating contact with bodily fluids and changing gloves in all situations.
Good fingernail traits were defined as not wearing fingernails longer than the tip of the finger and not wearing artificial nails.
Fig 1.
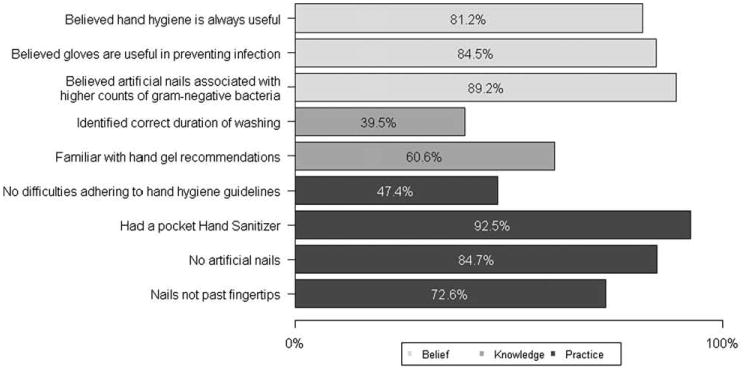
Response to beliefs, knowledge and reported practices. This Fig shows the percent of participants (N = 330) responding yes or no to questions regarding beliefs, knowledge, and practices related to hand hygiene and infection control.
CNAs reported washing their hands 1.5 times more on average than RN/NPs (P = .01). However, knowledge, beliefs, perception, and reported nail and gloving practices were not significantly different among RN/NP, LPN, or CNAs (all, P > .05). Participants with a better perception of hand hygiene were more likely to practice good glove use; the odds of reporting good glove use increased 1.09 times for a 1-unit increase in perception measure after adjusting for occupational title and number of patients per shift hour (95% confidence interval: 1.04-1.14). The odds of reporting good fingernail traits was positively associated with a stronger belief that fingernails played a role in infection transmission (odds ratio, 1.23; 95% confidence interval: 1.14-1.31). Knowledge and hand infection beliefs were not significantly associated with glove use and fingernail traits. Neither knowledge, beliefs, nor perceptions were related to handwashing frequency.
Discussion
Our study provides important insight regarding hand hygiene knowledge among nursing home HCW and uncovered some inconsistencies. A majority of HCW recognized hand hygiene as useful when providing patient care, believed that gloves are effective in preventing infection, and believed that artificial nails are associated with higher counts of gram-negative bacteria. This knowledge also translated into good hand hygiene practices such as avoiding artificial nails. In contrast, only 40% of HCWs identified the correct duration of washing, even though 60% professed familiarity with hand hygiene recommendations. This finding echoes results by Kennedy et al in neonatal intensive care units, where only 30% of HCWs were able to identify correct duration for hand hygiene.5 Knowledge was also lacking in staff's ability to identify appropriate recommendations regarding use of alcohol-based hand gels.
Our results indicate some differences in practices by occupational category. Nurses' aides washed their hands significantly more than RN/NP and LPN. In nursing homes, nurses' aides assume the role of frontline personnel with most contact with nursing home residents, including assistance with toileting, grooming, and assistance with meals, all of which require increased vigilance regarding hand hygiene.6
Although our survey is based on a validated scale, it was obtained by self-report, and we were unable to conduct observations of HCWs directly performing hand hygiene. In addition, home participation was voluntary, and, therefore, selection bias may have occurred. This bias could lead to greater self-selection of subjects who are more concerned with infection control procedures, and, therefore, we may have overestimated knowledge among nursing home staff. Notwithstanding, our excellent response rate from a diverse number of nursing homes enhances the generalizability of our results.
In conclusion, positive perceptions and beliefs regarding effectiveness of infection control in nursing homes was a determinant of reporting appropriate glove use and fingernail characteristics, respectively, among HCWs. We also identified the need to expand infection control training to incorporate specific recommendations and routine update of guidelines. Further research on hand hygiene intervention programs including specific targeted educational in-services should be conducted in the nursing home setting.
Acknowledgments
Supported by the University of Michigan-Medical School, Institute of Gerontology, Pepper Center Research Career Development Core (to A.E.A.), and by a National Institutes of Health NIA K23 AG028943, ASP/AGS T Franklin Williams Research Scholarship (to C.L.M.).
Footnotes
Conflicts of interest: The authors report no conflicts of interest.
References
- 1.Alvaran MS, Butz A, Larson E. Opinions, knowledge, and self-reported practices related to infection control among nursing personnel in long-term care settings. Am J Infect Control. 1994;22:367–70. doi: 10.1016/0196-6553(94)90036-1. [DOI] [PubMed] [Google Scholar]
- 2.Larson E, Bobo L, Bennett R, Murphy S, Seng ST, Choo JT, et al. Lack of caregiver hand contamination with endemic bacterial pathogens in a nursing home. Am J Infect Control. 1992;20:11–5. doi: 10.1016/s0196-6553(05)80118-x. [DOI] [PubMed] [Google Scholar]
- 3.Fendler EJ, Ali Y, Hammond BS, Lyons MK, Kelley MB, Vowell NA. The impact of alcohol hand sanitizer use on infection rates in an extended care facility. Am J Infect Control. 2002;30:226–33. doi: 10.1067/mic.2002.120129. [DOI] [PubMed] [Google Scholar]
- 4.Pittet D, Simon A, Hugonnet S, Pessoa-Silva CL, Sauvan V, Perneger TV. Hand hygiene among physicians: performance, beliefs, and perceptions. Ann Intern Med. 2004;141:1–8. doi: 10.7326/0003-4819-141-1-200407060-00008. [DOI] [PubMed] [Google Scholar]
- 5.Kennedy AM, Elward AM, Fraser VJ. Survey of knowledge, beliefs, and practices of neonatal intensive care unit healthcare workers regarding nosocomial infections, central venous catheter care, and hand hygiene. Infect Control Hosp Epidemiol. 2004;25:747–52. doi: 10.1086/502471. [DOI] [PubMed] [Google Scholar]
- 6.Eriksen W. Practice area and work demands in nurses' aides: a cross-sectional study. BMC Public Health. 2006;6:97. doi: 10.1186/1471-2458-6-97. [DOI] [PMC free article] [PubMed] [Google Scholar]


