Abstract
Prior studies have shown that birth complications interact with psychosocial risk factors in predisposing to increased externalizing behavior in childhood and criminal behavior in adulthood. However, little is known about the direct relationship between birth complications and externalizing behavior. Furthermore, the mechanism by which the birth complications predispose to externalizing behavior is not well explored. This study aims to assess whether birth complications predispose to early adolescent externalizing behavior and to test whether Intelligence Quotient (IQ) mediates relationships between predictor and outcome variables. We used data from a prospective, longitudinal birth cohort of 1,795 3-year-old boys and girls from Mauritius to test hypotheses. Birth complications were assessed from hospital record data, malnutrition from a pediatric exam at age 3 years, psychosocial adversity from parental interviews at age 3 years, and externalizing behavior problems from parental ratings at age 11 years. We found that babies with birth complications are more likely to develop externalizing behavior problems at age 11. Low IQ was associated with birth complications and was found to mediate the link between early predictors and later externalizing behavior. These prospective, longitudinal findings have potential clinical implications for the identification of early adolescent externalizing behavior and for public health attempts to prevent the occurrence of child externalizing behavior problems.
Childhood externalizing behavior problems are important predispositions to later violent offending (Hann, 2002), and violence prevention and protection from victimization have become two of the most pressing issues facing society today (Comerci, 1996). Although decades of research have emphasized social and biological risk factors for childhood externalizing behavior, surprisingly few studies have prospectively explored the role of early health risk factors. For example, compared with the area of psychosocial research, there has been relatively little research on prenatal and postnatal risk factors for childhood externalizing behavior (Raine, 2002).
To date several studies have found that birth complications are associated with increased externalizing behavior in childhood (Arsenault, Tremblay, Boulerice, & Saucier, 2002; Beck & Shaw, 2005) and criminal behavior in adulthood (Hodgins, Kratzer, & McNeil, 2001; Piquero & Tibbetts, 1999). For example, Raine, Brennan, and Mednick (1994) prospectively assessed birth complications and maternal rejection at age 1 year in 4,269 live male births in Copenhagen, Denmark. Birth complications significantly interacted with maternal rejection of the child in predicting violent offending at age 18 years. Only 4% of the sample had both birth complications and maternal rejection, but this small group accounted for 18% of all the violent crimes committed by the entire sample. More recently, Beck and Shaw (2005) replicated these finding by demonstrating that family adversity (including parental rejection) when combined with perinatal complications predicted youth antisocial behavior. Nevertheless, birth complications alone have rarely if ever been found to predispose to externalizing behavior and violence. Instead, externalizing behavior is thought to be especially likely to develop when birth complications combine with psychosocial risk factors, such as a disadvantaged family environment and poor parenting (Beck & Shaw, 2005; Hodgins et al., 2001; Piquero & Tibbetts, 1999). By utilizing longitudinal data from Mauritius, the main aim of this study is to investigate whether birth complications directly predispose to externalizing behavior. It is also hypothesized that any birth complication–aggression relationship is moderated by psychosocial adversity.
One important question concerns the mechanism by which these risk factors predispose to externalizing behavior. Prior studies have revealed that birth complications predispose to later cognitive deficits (e.g., Seidman, Goldstein, & Rieder, 2000). Several longitudinal studies have shown that low intelligence relatively early in childhood is associated with antisocial and aggressive behavior in later childhood and adolescence (e.g., Donnellan, Ge, & Wenk, 2000). We have previously demonstrated that a low Intelligence Quotient (IQ) mediates the relationship between early malnutrition and externalizing behavior (Liu, Raine, Venables, & Mednick, 2004). In this context, low IQ could be a potential candidate for mediating the relationship between birth complications and externalizing behavior if low IQ is also related to both of these factors. Consequently, we hypothesized that IQ will mediate the birth complication–behavior problem relationship on the grounds that cognitive impairment (as indicated by lower IQ) indirectly reflects brain dysfunction, which in turn is viewed to predispose to externalizing behavior problems (Liu et al., 2004).
Building on our previously published work on the influence of early malnutrition on later childhood externalizing behavior in this sample (Liu et al., 2004), the present study explores the influence of early health risk factors (birth complications, malnutrition, and psychosocial adversity) on childhood externalizing behavior, with an emphasis on birth complications. We hypothesized that birth complications predispose to higher externalizing behavior problems at age 11 years. We also hypothesized that poor cognitive ability at age 11 mediates this relationship.
METHOD
Participants
Participants consist of a birth cohort of 1,795 children from the island of Mauritius lying off the coast of Africa. Based on vaccination records, all children born in 1969–1970 in two main towns on the island were recruited into the study when aged 3 years between September 1972 and August 1973. The sample consisted of both boys (51.4%) and girls (48.6%). Ethnic distribution was as follows: Indian 68.7%, Creoles (African origin) 25.7%, and others (Chinese, English, and French) 5.6%. Details of sample selection can be found in our previous work on this population (Liu et al., 2004; Raine, Reynolds, Venables, Mednick, & Farrington, 1998; Raine, Yaralian, Reynolds, Venables, & Mednick, 2002). Verbal informed consent was obtained from the mothers of the participants in the early phases. Early research activities were conducted according to the principles outlined in the Declaration of Helsinki (World Medical Association, 1964), which prevailed in 1972 when the research was initiated, while research activities in later years were conducted using principles outlined in the Belmont Report (1979). Institutional Review Board approval for later research phases and retrospective data analyses was obtained from the University of Southern California and the University of California, Los Angeles.
Measures
Birth complications
Birth information was obtained from original medical records when the child was aged 3 years. The medical records of all subjects were stored in the Mauritius General Hospital. These records documented maternal signs and symptoms during pregnancy, labor/delivery, and also provided profiles on the newborn babies. Complete data are available on 1,079 of the subjects. Birth complication is a generic term which includes the following three indicators: (1) prenatal complications which consist of hypertension (measured by blood pressure above 140/90), low blood albumin level, bleeding, and other illness (diabetes, TB, pneumonia, asthma, and epilepsy); (2) perinatal complications which consist of difficult fetal presentations (e.g., breech birth); premature rupture of the membrane, instrument delivery (forceps and cesarean), and fetal distress (difficulty breathing); (3) postnatal complications as indicated by the following two signs: cyanosis and treatment with oxygen.
For each of the above three indicators, a weighted frequency scale of birth complications was computed following guidelines given in the McNeil–Sjostrom Scale for Obstetric Complications (McNeil & Sjostrom, 1998). Each birth complication was assigned a weight on a 6-point scale, with high scores indicating increased severity and reflecting the ordinal degree of inferred potential harm to the baby. Severity level 1 indicates not harmful or relevant (e.g., maternal heartburn); severity level 2: not likely harmful or relevant (e.g., maternal headache); severity level 3: potentially but not clearly harmful or relevant (e.g., hypertension without concurrent albuminuria/proteinuria); severity level 4: potentially clearly harmful or relevant (e.g., mild preeclampsia, breech delivery); severity level 5: potentially clearly greatly harmful/relevant (e.g., severe preeclampsia); severity level 6: very great harm to or deviation in offspring (e.g., severe neonatal distress). The scale has been viewed as being more sensitive to birth complications than other scales (McNeil et al., 1994). Rather than using the above three indicators to construct a latent variable, a single continuous dimensional scale of pre/peri/postnatal complications was formed by summation of the three separate scores. This approach was taken because preliminary analyses indicated that, due to the skewed distribution of each variable, the measures were largely uncorrelated. For example, those with maternal hypertension were no more likely to have maternal bleeding or forceps delivery than those without these complications.
Childhood nutritional deficits at age 3 years
At age 3 years, four early signs of malnutrition were assessed in a clinical examination of 1,559 of the children and a laboratory blood test. The four signs of malnutrition (see Liu, Raine, Venables, Dalais, & Mednick, 2003; Liu et al., 2004, for full details) were (1) angular stomatitis; (2) hair dyspigmentation; (3) sparse, thin hair; and (4) anemia. Participants were defined as suffering from nutritional deficits if at least one of the four above indicators was present (22.6%). Participants with no indicator present were defined as having relatively normative nutrition (77.4%). These four categorical measures of malnutrition were each entered as indicators of the latent construct “malnutrition” in the structural equation model.
Psychosocial adversity at age 3 years
The age 3 index of psychosocial adversity (Liu et al., 2004) was based on nine psychosocial variables collected by social workers who visited the homes of the children at age 3 years (see Raine, Venables, & Mednick, 1997, for full details). The index was created along lines similar to those described by Rutter (1978) and Moffitt (1990). To maintain consistency of measurement of psychosocial adversity with our previous publications (Liu et al., 2004; Raine et al., 1998), a total adversity score was created by adding one point for each of the nine variables (e.g., low parental education and occupation, single parent status). Data for this construct were available on 1,649 participants.
Intelligence at age 11 years
The mediator variable of total IQ was defined by two indicator variables that were used to measure and reflect the construct of intelligence and cognitive ability at age 11 years. This construct of intelligence was hypothesized to significantly mediate the relationship between the independent and dependent variables. Two estimates of verbal IQ (VIQ) and performance IQ were used to construct the latent variable of total IQ. These two estimates were assessed at age 11 years using seven subtests of the WISC (Wechsler, 1967). Details on this measures and the validity of the measures are given in Raine et al. (2002). Data were available on 1,385 subjects for the above two measures.
Externalizing behavior problems at age 11
Externalizing behavior was assessed from parental ratings using the three externalizing subscales (aggression, delinquency, hyperactivity) of the Child Behavior Checklist (Achenbach & Edelbrock, 1983), with item content common across boys and girls (Liu et al., 2004). The internal reliabilities (coefficient α) for the scales were as follows: aggression (.72), delinquency (.66), hyperactivity (.57), total externalizing problems (.84). Construct validity data are provided in Raine et al. (2002) and Liu et al. (2004). In this study, the latent construct of externalizing behavior problems was assessed by the above three indicators. Data were available on 1,206 participants.
Statistical Analyses
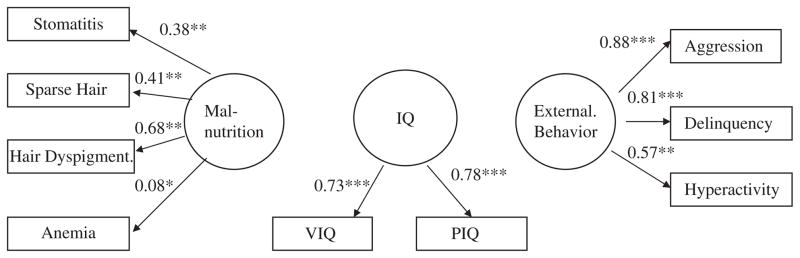
To address the research questions proposed in this study, we used structural equation modeling (SEM). We first built the confirmatory factor analysis (CFA) to test the construct validity of malnutrition at age 3 and IQ and externalizing behavior at age 11. Following an adequate fit to these data, we built the initial structural model by including two more measured variables (birth complications and psychosocial adversity) and by adding the directional paths. Consequently, the final structural model was derived by adding specific paths for model modification and by testing the hypothesized relations among the variables. Data were analyzed with the EQS program (Bentler 1995; Bentler & Wu, 2002) using maximum likelihood (ML) and robust estimation. Goodness-of-fit of the models was evaluated with the comparative fit index (CFI), the chi-square degree of freedom ratio, and the root mean squared error of approximation (RMSEA) index (Ullman, 2000). The hypothesized mediating effect of IQ was structured within the above whole SEM model (see Figure 2). In order to test whether IQ is a mediating construct, after the final structural model was established the path between IQ and externalizing behavior was removed from the model. The same procedures were employed using EQS to run the model. We compared the fit of these two models (with the path of IQ to behavior included vs. excluded) by evaluating whether the chi-square difference was significant with one degree of freedom and at a significance level of .01 (Steiger, Shapiro, & Browne, 1985; Ullman, 2000).
FIGURE 2.
Final structural equation model for early health/social risk factors and childhood externalized behavior, Circles =latent constructs, rectangle =measured variables. Parameter estimates are standardized, and significant levels were determined by critical ratios on unstandardized coefficients. *<.05. **<.01. ***<.001, External. behavior =externalizing behavior; PIQ =performance IQ; VIQ =verbal IQ.
Furthermore, the hypothesized interaction effects of birth complications and psychosocial adversity, and malnutrition and psychosocial adversity, were evaluated by using hierarchical multiple regression procedures (Aiken & West, 1991). Factor scores saved from the SEM model were used as data input. Separate regression equations were run for each of the two interaction effects. Taking as an example the interaction between birth complications and psychosocial adversity, on the first step, the birth complication measure was entered in the first step. On the second step, the psychosocial adversity measure was entered. On the third step, the product of birth complications and social adversity (the interaction) was entered. The main question to be answered concerns whether the interaction terms accounts for a significant increase in R2 after the main effects of birth complications and social adversity have both been taken into account. Similar hierarchical models were built to test the other hypothesized interaction between malnutrition and psychosocial adversity in relation to externalizing behavior. These procedures were conducted using SPSS (SPSS Inc., Chicago, IL).
Handling Missing and Nonnormal Data
Because variables used in this analysis were taken across 8 years (ages 3 and 11) and data are not complete for all subjects, and because preliminary analysis indicated that data were not normally distributed (Mardia’s normalized multivariate/univariate kurtosis for several variables was larger than 3), special attention was paid to handling these two issues while conducting the above SEM model using EQS. The Yuan–Bentler (Y–B) Robust correction statistic was chosen for the CFA and structural models as they help deal with both nonnormality and missing data (Yuan, Chan, & Bentler, 2000). ML estimators were used, which do not delete any cases and use all data optimally using a so-called EM algorithm to obtain the ML estimates. With this method, computation of standard errors can be made with two different approaches. The default uses the Fisher information matrix that is typically used with ML. The alternative is to use the observed information matrix, which involves second order derivatives and may possibly be better with small samples (Bentler & Wu, 2002). Because the analysis in this study involves a large sample, we used ML estimators with the Fisher information matrix to obtain the ML estimates for handling all the models when running the EQS model. For all the above analyses, post hoc modification was used by examining the Lagrange Multiplier Test (LM) (Byrne, 1994).
RESULTS
CFA Model for Reliability and Validity of Key Constructs
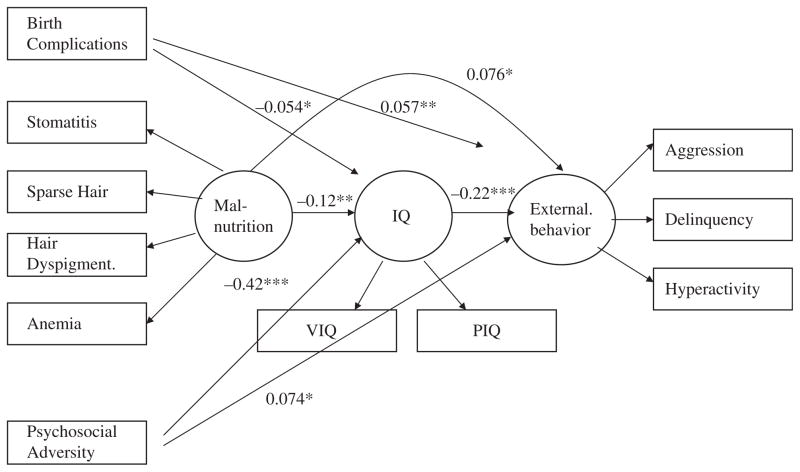
The CFA tested the hypothesized factor model. The data fit the CFA model adequately, Y–B χ2(20, N =1,795) =66.38, CFI =. 98, normed fit index (NFI) =. 98, nonnormed fit index (NNFI) =.98, and RMSEA =.036. Figure 1 presents the standardized factor loadings. It can be seen that the manifest variables all loaded significantly (p<.05) on their hypothesized latent factors. Furthermore, all factor loadings were in the expected direction, and most were substantial in magnitude. These analyses confirm that the indicators were reliable indicators of the latent constructs. They also provided important information regarding the degree of association among these constructs. Table 1 exhibits descriptive statistics of the measured variables and factor loadings of the latent variables.
FIGURE 1.
Confirmatory factor analysis model. Circles =latent constructs. Rectangles =measured variables. Factor loading are standardized, and significant levels were determined by critical ratios on unstandardized coefficients. *<.05. **<.01. ***<.001. External. Behavior =externalizing behavior; PIQ =performance IQ; VIQ =verbal IQ.
TABLE 1.
Sample Size, Score Ranges, Means, Standard Deviations, and Factor Loadings of the Measured Variables
| Latent/Measured Variables | Sample Size | Score Range | M (SD) | Factor Loadings |
|---|---|---|---|---|
| Malnutrition | 1,559 | |||
| Angular stomatitis | 0–1 | .07 (.25) | .38 | |
| Sparse, thin hair | 0–1 | .058 (.23) | .41 | |
| Kwashiorkor | 0–1 | .068 (.25) | .68 | |
| Anemia (low Hg) | 0–1 | .17 (.37) | .082a | |
| IQ | 1,388 | |||
| Verbal | 60–139 | 99.97 (15) | .74 | |
| Performance | 62–146 | 99.94 (14.97) | .79 | |
| Externalized behavior | 1,206 | |||
| Aggression | 0–18 | 4.6 (3.57) | .88 | |
| Delinquency | 0–18 | 4.73 (3.36) | .81 | |
| Hyperactivity | 0–15 | 3.59 (2.7) | .57 | |
| Other measured variables | ||||
| Birth complications | 1,079 | 0–6 | .64 (1.89) | |
| Psychosocial adversity | 1,649 | 0–9 | 1.88 (1.36) | |
Notes.
p<.05, all other loadings p<.001.
SEM Model for Main Effects, Mediating Effects, and Interaction Effects
The initial structural model
The CFA model described above was used as the foundation for developing the structural model outlined in Figure 2. The structural model retained the same latent variables and the same measurement parameters as those used in the CFA model. In addition, two measured variables (birth complications and psychosocial adversity) were added as predictors in the structural model.
In the initial structural model, other than the hypothesized path, there was no other path (e.g., correlations between residuals) estimated in this initial model, indicating that the initial model was the most parsimonious structural model. As anticipated, the initial model’s χ2(df =37, N =1,975) of 144.42 was statistically significant (p<.001), largely due to the large degrees of freedom. Some goodness-of-fit indices (e.g., RMSEA =.068, CFI =.91) indicated a good fit, while others (e.g., NFI =.884, NNFI =.866) indicated a less good fit, which suggested room for improvement in the overall fit (Bentler & Bonett, 1980; Bentler & Chou, 1987; Byrne, 1994). Therefore, post hoc model modification was attempted (Ullman, 2000).
Model modification and the final structural model
LM statistics were examined to assess which parameters contributed most to the model misfit (Bentler & Bonett, 1980; Bentler & Chou, 1987; Bentler & Wu 2002; Byrne, 1994). LM suggested that five paths, one between two predictor variables and four additional residual paths, would significantly improve the model fit. More specifically, a covariance path between psychosocial adversity and malnutrition was added. In addition, specific paths were added to reflect four sets of error covariance relationships between (1) aggression and delinquency, (2) aggression and hyperactivity, (3) angular stomatitis and delinquency, and (4) sparse, thin hair and hyperactivity.
The final model was tested with the integration of the above five parameters and with the implementation of the Y–B robust correction for both nonnormalized estimation and missing data. The results indicated excellent fit statistics, Y-B χ2(32, N =1,795) =40.15, RMSEA =.012, and other indices were all higher than .95. The results of path coefficients between predictors and outcome are shown in Figure 2. As indicated by the small but significant path coefficients between predictors and outcomes, all hypothesized links were supported.
Main effects
As predicted, externalizing behavior was directly predicted by early health risk factors and psychosocial adversity (see Figure 2). In addition, children whose mothers suffered pregnancy/birth complications were more likely to have higher scores on externalizing behavior at age 11 (p<.002). Similarly, children who experienced malnutrition at age 3 were more likely to score higher on externalizing behavior at age 11 (p<.02). Finally, children who came from psychosocially adverse family backgrounds at an early age were more likely to show externalizing behavior at age 11 (p<.02). The strongest path coefficient was for malnutrition (.076) and the weakest was for birth complications (.057). The effect for psychosocial adversity was slightly less than that of malnutrition (.074).
Mediating effects and interaction effect
The mediating effect of IQ was indicated in the SEM by the fact that the difference between the two chi-square values (IQ path included vs. excluded) was significant (p<.001). There were significant path coefficients between all three early biosocial risk factors (birth complications, malnutrition, and psychosocial adversity) and IQ at age 11. Specifically, the strongest path was for psychosocial adversity to IQ (path coefficient =.42), with a weaker path from malnutrition to IQ (.12). These findings indicate that IQ is a candidate as a mediator. The role of IQ as a mediator was confirmed by the significant path coefficient of .22 between IQ and externalizing behavior (see Figure 2). The direction of effects were such that higher psychosocial adversity, higher birth complications, and higher malnutrition were all associated with lower IQ, and lower IQ was linked to increased externalizing behavior. As regards interaction effects, the results from regression analyses are summarized in Table 2. Importantly, neither birth complications nor malnutrition interacted with psychosocial adversity in predicting childhood externalizing behavior.
TABLE 2.
Regression Analyses: Increments in Variance Explained (R2 Change) by Main Effects and Interactions in Predicting Childhood Externalized Behavior in Model A (Birth Complications and Psychosocial Adversity) and Model B (Malnutrition and Psychosocial Adversity)
| Predictive Variable | Outcome Variable: Externalized Behavior |
|---|---|
| Model A | |
| 1. Birth complications | .011*** |
| 2. Psychosocial adversity | .035*** |
| 3. BC × Psychosocial Adversity | .00 (NS) |
| Model B | |
| 1. Malnutrition | .005** |
| 2. Psychosocial Adversity | .032*** |
| 3. Malnutrition × Psychosocial Adversity | .00 (NS) |
Effects were entered in the 1, 2, 3 hierarchical order specified. If an effect was not significant, its increment in variance explained is not listed.
p<.01;
p<.001.
NS = nonsignifcant in hierarchical test.
DISCUSSION
Previous studies have shown that birth complications when combined with psychosocial factors increase the risk for externalizing behavior in children (e.g., Beck & Shaw, 2005), and criminal behavior in adults (e.g., Raine et al., 1994). Our findings have shown a direct effect of birth complications on child externalizing behavior at age 11 years and also the mediating effect of IQ on this relationship, indicating that birth complications results in brain dysfunction as reflected by low IQ which in turn predisposes to behavior problems. To the authors’ knowledge, this is the first large prospective longitudinal study showing a direct effect of birth complications on late-childhood externalizing behavior, and there is no prior research on the mediating effect of IQ on birth complication and externalizing behavior.
Main Effects of Risk Factors on Externalizing Behavior
Birth complications and externalizing behavior
We found that higher birth complication scores were associated with higher scores on externalizing behavior. In general, while this finding is broadly consistent with prior findings that obstetric factors are in some way associated antisocial behavior in both child and adult samples, most prior studies observe interaction effects but not main effects of obstetric factors (Arsenault et al., 2002; Beck & Shaw, 2005; Hodgins et al., 2001; Piquero & Tibbetts, 1999; Raine et al., 1994) or alternatively show only that low birth weight is associated with increased attention hyperactivity disorder (e.g., Mick, Biederman, Prince, Fischer, & Faraone, 2002).
It is not known exactly how birth complications play a role in the development of childhood externalizing behavior, but it has been suggested that birth complications might lead to externalizing behavior problems through damage/disruption to the prefrontal cortex, hippocampus, and dopamine system (Brennan, Mednick, & Raine, 1997; Cannon et al., 2002; Mednick & Kandel, 1988; Raine, 2002). More specifically, birth complications such as preeclampsia, maternal bleeding, or maternal infection can first cause an insufficiency in blood supply to the placenta. This in turn may lead to fetal hypoxia or anoxia (lack of oxygen), which further hampers fetal brain development, particularly the hippocampus (Cannon et al., 2002; Liu, 2004; Mednick & Kandel, 1988). Animal studies have shown that perinatal complications involving anoxia are associated with reductions in central dopamine transmission (Brake, Sullivan, & Gratton, 2000). Several lines of research suggest that dopaminergic neurotransmission is involved in the regulation of impulsive aggression and violence (Chen et al., 2005; Retz, Rosler, Supprian, Retz-Junginger, & Thome, 2003). In addition, perinatal complications impair neurotransmitter functioning in the left prefrontal cortex in animals (Brake et al., 2000), and reduced prefrontal functioning is one of the best-replicated findings from the brain imaging literature on violent offenders (Henry & Moffitt, 1997). These findings therefore suggest that birth complications may lead to externalizing behavior problems through the mechanism of damage/dysfunction to the prefrontal cortex, hippocampus, and the dopamine system.
Nutrition and externalizing behavior
We have recently reported that malnutrition at age 3 years is related to higher externalizing behavior at ages 8, 11, and 17 (see Liu et al., 2004, for a full discussion of these findings). Briefly, in interpreting the findings of this study, protein, iron, and zinc deficiency may contribute to some of the specific brain impairments that have been found in aggressive adult offenders and which in turn are thought to predispose to aggressive antisocial behavior (Moffitt, 1990; Raine, 1993; Volavka, 1987).
Psychosocial adversity and externalizing behavior
Psychosocial adversity was significantly related to externalizing behavior problems. This result is consistent with other studies which have examined biosocial risk factors on child behavior problems. For example, Laucht et al. (2000) in a prospective study found that although early birth complications and psychosocial adversity both affected later childhood development (motor, cognitive, and social-emotional functioning), the latter effect outweighed the former in terms of strength of relationship in all areas of functioning.
While the relationship between early psychosocial adversity and later externalizing behavior problems is significant, the question arises as to the mechanism by which they influence externalizing behavior. Unlike the above two biological risk factors which are hypothesized to mainly impact behavior through neurological processes, psychosocial adversity may influence the child’s behavior through poor parental supervision. That is, adversity may be a marker of poor supervision and poor parental supervision rather than general adversity that may predispose to externalizing behavior. This parenting construct has been found to be one of the strongest psychosocial correlates of delinquency (Loeber, 1990). It should be pointed out however that some of the indicators in psychosocial adversity index (e.g., parents’ education) may be in part genetically determined and reflect genetic influences on externalizing behavior. For example, IQ is in part heritable (Arthur & Thompson, 2005), and consequently educational level itself may be partly heritable.
Mediator Effect of IQ
While each of the above risk factors was shown to have its own pathways to childhood externalizing behavior, they all also had additional common negative relationships to IQ, with an additional path coefficient of .22 between IQ and externalizing behavior. These linkages suggest that cognitive processes mediate the relationships between the three main risk factors and later externalizing behavior. The finding that low IQ predisposes to externalizing behavior is consistent with a large body of prior work that has linked lower cognitive ability and lower IQ to externalizing behavior (Deitz, Lavigne, Atrend, & Rosenbaum, 1997; Moffitt, 1993; Wilson & Herrnstein, 1985).
An important question concerns why low intelligence should predispose to antisocial behavior in this sample. Some have argued that low IQ results in school failure, and it is the psychological and social consequences of school failure that drive antisocial behavior (e.g., Rutter, Giller, & Hagell, 1998). On the other hand, IQ–antisocial relationships have been found in some studies even after controlling for school achievement (Goodman, Simonoff, & Stevenson, 1995). Alternatively, low IQ may be a proxy for impairments to brain functioning, which in turn predispose to antisocial behavior (Henry & Moffitt, 1997; Raine et al., 2002). It has been hypothesized that low VIQ reflects poor left hemisphere functioning and that normally a well functioning left hemisphere contributes importantly to the brain’s normal control over impulsive behavior (Henry & Moffitt, 1997; Raine, 1993). Furthermore, it has been speculated that early spatial deficits are a marker for poor right hemisphere functioning, and such poor functioning negatively impacts early bonding which in the first 18 months heavily relies on good visuo-spatial communication between the infant and mother (Raine et al., 2002). Yet again, genetic factors (indirectly reflected by low parental education) may influence outcome for externalizing behavior.
No Interaction Between Birth Complications and Psychosocial Adversity
We did not find a significant interaction between birth complication and psychosocial adversity in this sample, whereas other prior studies have showed such effect exist (Arsenault et al., 2002; Hodgins et al., 2001; Raine et al., 1994). There are several possible reasons contributing to this fact. First, there is potential for type-II error in tests of interactions (Busemeyer & Jones, 1983; McClelland & Judd, 1993). Second, the psychosocial adversity measure used in this study did not include a direct measure of maternal rejection (Beck & Shaw, 2005; Raine et al., 1994) or parenting (Hodgins et al., 2001). Third, psychosocial adversity may conceivably have a different meaning in Mauritius than in the Western countries where interaction effects have been observed.
Clinical Implications
The identification of early risk factors for childhood externalizing behavior is a critically important step for developing successful prevention programs for adult violence. In addition to our prior findings showing malnutrition as a risk factor for later childhood externalizing behavior problems (Liu et al., 2004), we show here a main effect of birth complications. Consequently, ameliorating this risk factor in future prevention programs may help prevent the development of externalizing behavior in children.
Prenatal, perinatal, and postnatal health care interventions to reduce birth complications may also help reduce the likelihood of later behavior problems. Good prenatal care and early enrichments which improve cognitive ability may be effective in preventing antisocial behavior (Liu, 2004; Olds et al., 1998). Furthermore, micronutrient deficiency such as zinc deficiency in children continues to be a nutritional problem in both developing and developed countries (Penland, 2000). Because early health risk factors were found to contribute to low intelligence, it would also be expected that interventions to reduce early health risk factors such as birth complications would also be helpful in reducing outcome for low IQ, and hence outcome for externalizing behavior. Health care workers and social workers are in an ideal position to develop early prevention and intervention program to help reduce prenatal and perinatal complications. Consequently, such a multidisciplinary approach may potentially help reduce the likelihood of later externalizing behavior problems (Liu, 2004).
Limitations
First, the size of the path coefficients suggests that early biological and psychosocial factors do not explain much of the variance in the externalizing behavior, at least longitudinally. This perhaps is to be expected. Externalizing behavior is a complex construct, and it is likely that many different biological and psychosocial processes are involved, of which only a few were measured in this study. On the other hand, the path coefficient for the mediating effect of IQ was relatively more substantial at .22. This suggests that the biological and psychosocial risk factors each make separate contributions to low IQ and that these contributions combine together to make for a stronger link between low IQ and later externalizing behavior.
Second, because IQ and externalizing behavior are measured concurrently, it is conceivable that externalizing problems could also mediate the association between birth complications and low IQ. Third, there were limitations in the detail and quality of the birth complication data due to the fact that these data were collected from stored original hospital records 3 years after the birth. On the other hand, because the medical records were original, data on birth complications are prospective rather than retrospective. It was also necessary to combine across prenatal, perinatal, and postnatal processes to produce a single weighted frequency scale of “obstetric” factors. Further, a related issue concerns the relevance of the observed findings for Western countries and the generalizability of findings. Nevertheless, current findings from Mauritius may be a good model for externalizing problems in underserved subpopulations of American society, particularly since adolescent pregnancy is often associated with adverse pregnancy and birth complications and has been associated with poor behavioral functioning in low-income children in North American inner cities (Loto et al., 2004; Nagin, 1998).
CONCLUSIONS
Adolescent externalizing behaviors are being increasingly viewed as a public health problem (Hann, 2002), and reducing externalizing and violent behavior and violence prevention are increasingly receiving society and public attention. The key findings of this study suggest that birth complications are associated with increased externalizing behavior problems at age 11, and importantly that low IQ mediates the link between birth complications and later externalizing behavior. However, findings of this study are by no means definitive. Rather, they are best construed as initial results which, while providing potentially important pointers on the health basis of violence, also require both replication and extension.
Contributor Information
Jianghong Liu, University of Pennsylvania.
Adrian Raine, University of Pennsylvania.
Anne Wuerker, University of California, Los Angeles.
Peter H. Venables, University of York
Sarnoff Mednick, University of Southern California.
References
- Achenbach TM, Edelbrock CS. Manual for the child behavior checklist and revised child behavior profile. Burlington: Department of Psychiatry, University of Vermont; 1983. [Google Scholar]
- Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Newbury Park, CA: Sage; 1991. [Google Scholar]
- Arsenault L, Tremblay RE, Boulerice B, Saucier JF. Obstetrical complications and violent delinquency: Testing two developmental pathways. Child Development. 2002;73:496–508. doi: 10.1111/1467-8624.00420. [DOI] [PubMed] [Google Scholar]
- Arthur WT, Thompson PM. Genetics of brain structure and Intelligence annual. Review of Neuroscience. 2005;28:1–23. doi: 10.1146/annurev.neuro.28.061604.135655. [DOI] [PubMed] [Google Scholar]
- Beck J, Shaw D. The influence of perinatal complications and environmental adversity on boys’ antisocial behavior. Journal of Child Psychology and Psychiatry. 2005;46:35–46. doi: 10.1111/j.1469-7610.2004.00336.x. [DOI] [PubMed] [Google Scholar]
- Belmont Report. Ethical principles and guidelines for the protection of human subjects of biomedical and behavioral research: National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research. Washington, DC: DHHS; 1979. [PubMed] [Google Scholar]
- Bentler PM. EQS structural equations program mannual. Encino, CA: Multivariate Software; 1995. [Google Scholar]
- Bentler PM, Bonett DG. Significance tests and goodness of fit in the analysis of covariance structures. Psychological Bulletin. 1980;88:588–606. [Google Scholar]
- Bentler PM, Chou CP. Practical issues in structural modeling. Sociological Methods and Research. 1987;16:78–117. [Google Scholar]
- Bentler PM, Wu EJC. for Windows user’s guide. Encino, CA: Multivariate Software Inc; 2002. [Google Scholar]
- Brake WG, Sullivan RM, Gratton A. Perinatal distress leads to lateralized medial prefrontal cortical dopamine hypofunction in adult rats. Journal of Neuroscience. 2000;20:5538–5543. doi: 10.1523/JNEUROSCI.20-14-05538.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brennan PA, Mednick SA, Raine A. Biosocial interactions and violence: A focus on perinatal factors. In: Raine A, Brennan PA, et al., editors. Biosocial bases of violence. NATO ASI series: Series A: Life sciences. New York: Plenum Press; 1997. pp. 163–174. [Google Scholar]
- Busemeyer JR, Jones LE. Analysis of multiplicative combination rules when the causal variables are measured with error. Psychological Bulletin. 1983;93:549–562. [Google Scholar]
- Byrne BM. Structural equation modeling with EQS and EQS/Windows. Thousand Oaks, CA: Sage Publications; 1994. [Google Scholar]
- Cannon TD, van Erp TGM, Rosso IM, Huttunen M, Loenqvist J, Pirkola T, et al. Fetal hypoxia and structural brain abnormalities in schizophrenic patients, their siblings, and controls. Archives of General Psychiatry. 2002;59:35–41. doi: 10.1001/archpsyc.59.1.35. [DOI] [PubMed] [Google Scholar]
- Chen TJ, Blum K, Mathews D, Fisher L, Schnautz N, Braverman ER, et al. Are dopaminergic genes involved in a predisposition to pathological aggression? Hypothesizing the importance of “super normal controls” in psychiatric-genetic research of complex behavioral disorders. Medical Hypotheses. 2005;65:703–707. doi: 10.1016/j.mehy.2005.04.037. [DOI] [PubMed] [Google Scholar]
- Comerci GD. Efforts by the American Academy of Pediatrics to prevent and reduce violence and its effects on children and adolescents. Bulletin of the New York Academy of Medicine. 1996;73:398–410. [PMC free article] [PubMed] [Google Scholar]
- Deitz KR, Lavigne JV, Atrend R, Rosenbaum D. Relation between intelligence and psychopathology among preschoolers. Journal of Clinical Child Psychology. 1997;26:99–107. doi: 10.1207/s15374424jccp2601_10. [DOI] [PubMed] [Google Scholar]
- Donnellan MB, Ge X, Wenk E. Cognitive abilities in adolescent-limited and life-course-persistent criminal offenders. Journal of Abnormal Psychology. 2000;109:396–402. [PubMed] [Google Scholar]
- Goodman R, Simonoff E, Stevenson J. The impact of child IQ, parent IQ and sibling IQ on child behavioural deviance scores. Journal of Child Psychology and Psychiatry and Allied Disciplines. 1995;36:409–425. doi: 10.1111/j.1469-7610.1995.tb01299.x. [DOI] [PubMed] [Google Scholar]
- Hann DM. Taking stock of risk factors for child/youth externalizing behavior problems. Rockville, MD: National Institute of Mental Health; 2002. [Google Scholar]
- Henry B, Moffitt TE. Neuropsychological and neuroimaging studies of juvenile delinquency and adult criminal behavior. In: Stoff D, Breiling J, Maser J, editors. Handbook of antisocial behavior. New York: John Wiley & Sons Inc; 1997. pp. 2809–2888. [Google Scholar]
- Hodgins S, Kratzer L, McNeil TF. Obstetric complications, parenting, and risk of criminal behavior. Archives of General Psychiatry. 2001;58:746–752. doi: 10.1001/archpsyc.58.8.746. [DOI] [PubMed] [Google Scholar]
- Laucht M, Essser G, Baving L, Gerhold M, Hoesch I, Ihle W, et al. Behavioral sequelae of perinatal insults and early family adversity at 8 years of age. Journal of the American Academy of Child and Adolescent Psychiatry. 2000;39:1229–1237. doi: 10.1097/00004583-200010000-00009. [DOI] [PubMed] [Google Scholar]
- Liu J. Prenatal & perinatal complications as predispositions to externalizing behavior. Journal of Prenatal and Perinatal Psychology and Health. 2004;18:301–311. [Google Scholar]
- Liu J, Raine A, Venables P, Dalais C, Mednick SA. Malnutrition at age 3 years and lower cognitive ability at age 11 years: Independence from psychosocial adversity. Archives of Pediatrics and Adolescent Medicine. 2003;157:593–600. doi: 10.1001/archpedi.157.6.593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu J, Raine A, Venables P, Mednick SA. Malnutrition at age 3 years and externalizing behavior problems at ages 8, 11, and 17 years. American Journal of Psychiatry. 2004;260:2005–2013. doi: 10.1176/appi.ajp.161.11.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loeber R. Development and risk factors of juvenile antisocial behavior and deliquency. Clinical Psychology Review. 1990;10:1–41. [Google Scholar]
- Loto OM, Ezechi OC, Kalu BK, Loto A, Ezechi L, Ogunniyi SO. Poor obstetric performance of teenagers: Is it age- or quality of care-related? Journal of Obstetrics and Gynaecology. 2004;24:395–398. doi: 10.1080/01443610410001685529. [DOI] [PubMed] [Google Scholar]
- McClelland GH, Judd CM. Statistical difficulties of detecting interactions and moderator effects. Psychological Bulletin. 1993;114:376–390. doi: 10.1037/0033-2909.114.2.376. [DOI] [PubMed] [Google Scholar]
- McNeil TF, Cantor-Graae E, Torrey EF, Sjoestroem K, Bowler A, Taylor E, et al. Obstetric complications in histories of monozygotic twins discordant and concordant for schizophrenia. Acta Psychiatrica Scandinavica Munksgaard Scientific Journals. 1994;89:196–204. doi: 10.1111/j.1600-0447.1994.tb08092.x. [DOI] [PubMed] [Google Scholar]
- McNeil TF, Sjostrom K. McNeil-Sjostrom scale for obstetric complications manuel. Sweden: Lind University; 1998. [Google Scholar]
- Mednick SA, Kandel E. Genetic and perinatal factors in violence. In: Moffitt TE, Mednick SA, editors. Biological contributions to crime causation. Dordrecht, the Netherlands: Martinus Nijhoff Publishing; 1988. pp. 121–131. [Google Scholar]
- Mick E, Biederman J, Prince J, Fischer MJ, Faraone SV. Impact of low birth weight on attention-deficit hyperactivity disorder. Journal of Developmental and Behavioral Pediatrics. 2002;23:16–22. doi: 10.1097/00004703-200202000-00004. [DOI] [PubMed] [Google Scholar]
- Moffitt TE. The neuropsychological studies of juvenile delinquency: A critical review. In: Tonry MN, editor. Crime and justice: A review of the literature. Chicago: University of Chicago Press; 1990. [Google Scholar]
- Moffitt TE. The neuropsychology of conduct disorder. Development and Psychopathology. 1993;5:135–151. [Google Scholar]
- Nagin D. Criminal deference research: A review of the evidence and a research agenda for the outset of the 21st century. In: Tonry MH, editor. Crime and justice: A review of research. Vol. 23. Chicago: University of Chicago Press; 1998. pp. 1–42. [Google Scholar]
- Olds D, Henderson CJ, Cole R, Eckenrode J, Kitzman H, Luckey D, et al. Long-term effects of nurse home visitation on children’s criminal and antisocial behavior: 15-year follow-up of a randomized controlled trial [see comments] Journal of American Medical Association. 1998;280:1238–1244. doi: 10.1001/jama.280.14.1238. [DOI] [PubMed] [Google Scholar]
- Penland JG. Behavioral data and methodology issues in studies of zinc nutrition in humans. Journal of Nutrition. 2000;130(2S Suppl):361S–364S. doi: 10.1093/jn/130.2.361S. [DOI] [PubMed] [Google Scholar]
- Piquero A, Tibbetts S. The impact of pre/perinatal disturbances and disadvantaged familial environment in predicting criminal offending. Studies on Crime and Crime Prevention. 1999;8:52–70. [Google Scholar]
- Raine A. The psychopathology of crime: Criminal behavior as a clinical disorder. San Diego, CA: Academic Press; 1993. [Google Scholar]
- Raine A. Annotation: The role of prefrontal deficits, low autonomic arousal and early health factors in the development of antisocial and aggressive behavior in children. Journal of Child Psychology and Psychiatry and Allied Disciplines. 2002;43:417–434. doi: 10.1111/1469-7610.00034. [DOI] [PubMed] [Google Scholar]
- Raine A, Brennan P, Mednick SA. Birth complications combined with early maternal rejection at age 1 year predispose to violent crime at age 18 years. Archives of General Psychiatry. 1994;51:984–988. doi: 10.1001/archpsyc.1994.03950120056009. [DOI] [PubMed] [Google Scholar]
- Raine A, Reynolds C, Venables PH, Mednick SA, Farrington DP. Fearlessness, stimulation-seeking, and large body size at age 3 years as early predispositions to childhood aggression at age 11 years [see comments] Archives of General Psychiatry. 1998;55:745–751. doi: 10.1001/archpsyc.55.8.745. [DOI] [PubMed] [Google Scholar]
- Raine A, Venables PH, Mednick SA. Low resting heart rate at age 3 years predisposes to aggression at age 11 years: Evidence from the Mauritius Child Health Project. Journal of American Academy of Child Adolescent Psychiatry. 1997;36:1457–1464. doi: 10.1097/00004583-199710000-00029. [DOI] [PubMed] [Google Scholar]
- Raine A, Yaralian P, Reynolds C, Venables P, Mednick S. Spatial but not verbal cognitive deficits at age 3 years in persistently antisocial individuals. Development and Psychopathology. 2002;4:25–44. doi: 10.1017/s0954579402001025. [DOI] [PubMed] [Google Scholar]
- Retz W, Rosler M, Supprian T, Retz-Junginger P, Thome J. Dopamine D3 receptor gene polymorphism and violent behavior: Relation to impulsiveness and ADHD-related psychopathology. Journal of Neural Transmission. 2003;110:561–572. doi: 10.1007/s00702-002-0805-5. [DOI] [PubMed] [Google Scholar]
- Rutter M. Family, area, and school influences in the genesis of aggressions. In: Hersov LA, Schaffer D, editors. Aggression and anti-social behavior in childhood and adolescence. Oxford: Pergamon; 1978. pp. 95–113. [Google Scholar]
- Rutter M, Giller H, Hagell A. Antisocial behavior by young people. New York: Cambridge University Press; 1998. [Google Scholar]
- Seidman B, Goldstein H, Rieder T. The relationship of prenatal and perinatal complications to cognitive functioning at age 7 in the New England cohorts of the National Collaborative Perinatal Project. Schizophrenia Bulletin. 2000;2:309–321. doi: 10.1093/oxfordjournals.schbul.a033455. [DOI] [PubMed] [Google Scholar]
- Steiger JH, Shapiro A, Browne MW. On the asymptotic distribution of sequential chi-square statistics. Psychometrika. 1985;50:253–264. [Google Scholar]
- Ullman JB. Structural equation modeling. In: Tabachnick BG, Fidell LS, editors. Using multivariate statistics. Boston: Allyn and Bacon; 2000. pp. 653–771. [Google Scholar]
- Volavka J. Electrencephalogram among criminals. In: Mednick SA, Moffitt TE, Stack S, editors. The causes of crime: New biological approaches. Cambridge: Cambridge University Press; 1987. pp. 137–145. [Google Scholar]
- Wechsler D. Wechsler preschool and primary scale of intelligence. San Antonio, TX: The Psychological Corporation; 1967. [Google Scholar]
- Wilson JQ, Herrnstein RJ. Crime and human nature: The definitive study of the causes of crime. New York: Touchstone; 1985. [Google Scholar]
- World Medical Association. Declaration of Helsinki: Recommendations guiding doctors in clinical research adopted by the 18th World Medical Assembly. Helsinki: World Medical Association; 1964. [Google Scholar]
- Yuan KH, Chan W, Bentler PM. Robust transformation with applications to structural equation modelling. British Journal of Mathematical and Statistical Psychology. 2000;53(Pt 1):31–50. doi: 10.1348/000711000159169. [DOI] [PubMed] [Google Scholar]