Abstract
Objective
Multiple studies from independent groups find evidence for Stat3 activation in nearly 50% of lung cancers suggesting a functional role for this target in subsets of lung cancer. Based on the existing evidence we hypothesized that bioavailable curcuminoid complex may modulate lung carcinogenesis, primarily by inhibiting Stat3 activation. With the safety of this botanical well established, the objective of these studies is to test our hypothesis in vitro and in vivo in an effort to inform the design of a phase II chemoprevention trial in former smokers.
Methods
We treated non-tumor derived, normal (but immortalized) human bronchial epithelial cells (AALE) and lung adenocarcinoma derived cells (H441) with bioactive Curcumin C3 Complex. Asynchronous cells in each case were treated with curcumin for 24 hrs, followed by immunoblotting for Stat3 and activated Stat3-P, prior signal of which was used for normalization. We also completed a preclinical trial in which 12 mice were randomly divided into three groups and subjected to 3 days or 9 days of curcumin i.p. injections, followed by analysis of lung tissues for Stat3-P changes and growth suppressive effects of the curcumin. The growth suppressive effects were measured using Cyclin D1 and the replicative helicase subunit, Mcm2, as surrogates for the proliferative capacity of the tissues.
Results
in vitro studies with curcuminoid complex demonstrated that the activity of Stat3 in both normal bronchoepithelial cells and lung cancer derived cells is sensitive to curcumin exposure. In a dose-dependent manner, curcumin treatment resulted in significant suppression of Stat3 phosphorylation and reduction in the proliferative capacity of both cell types. In the preclinical trial with rodent models, curcumin reduced Stat3-P and the proliferative markers CycD1 and Mcm2 in mice lung tissues in vivo.
Conclusion
These culture and preclinical studies indicate that the activity of the Stat3 pathway can be suppressed by curcumin treatment, concomitant with a reduction in cell proliferation, supporting our hypothesis that inhibition of the Stat3 pathway represents at least one important mechanism by which curcumin elicits its effects on the bronchoepithelium. These data provide a rationale for the use of curcumin as a promising chemopreventive agent in high risk populations such as former smokers.
Introduction
Lung cancer is the leading cause of cancer deaths worldwide and is responsible for 29% of cancer related deaths in the US 1-2. In addition to age and obstructive pulmonary disease, cigarette smoking is the major cause of lung cancer in the US and prevention of tobacco exposure has become critical in reducing lung cancer mortality 1-4. However, recent studies have demonstrated that over 50% of new lung cancers occur in former smokers, who are highly motivated and eagerly seeking strategies to reduce their risk 5. Although a number of previous studies to prevent lung cancer in smokers have failed, our understanding of novel compounds and their molecular targets relevant to pulmonary carcinogenesis, specific to current and former smokers has vastly expanded.1, 6-9 Other than smoking cessation as a prevention strategy, there is an urgent need to identify and test effectiveness and safety of promising, novel nutrient-derived substances as chemoprevention agents to modulate lung carcinogenesis.
Members of the signal transducer and activator of transcription (Stat) family of transcription factors are potential targets in lung cancer and other cancers.10 JAK/Stat signaling can be a common pathway activated by diverse upstream signaling proteins, including growth factor receptors, cytokines, and non-receptor tyrosine kinases such as Src and Abl. Stat proteins latent transcription factors that are activated by upstream tyrosine kinase signaling and control genes that regulate cancer hallmarks. Indirect or direct inhibition of Stat3 has been shown to affect tumor formation through inhibition of cell growth, induction of apoptosis, and/or inhibition of tumor angiogenesis.10 Stat proteins, in particular Stat3, are oncogenic in part by activating a gene transcription program that affects multiple cancer hallmarks. This includes cell proliferation (cyclin D, Myc), anti-apoptotic signaling (Mcl-1, Bcl-xL), angiogenesis (VEGF), and immune evasion.10 While non-tumor cells have robust systems to allow for only transient activation of this pathway, tumor cells acquire persistent pathway activation through various mechanisms. Targeting strategies such as small molecule inhibitors, natural products such as curcumin, RNA interference, and tyrosine kinase inhibitors are potential strategies to target Stat3 signaling in cancer.11 Multiple studies from independent groups find evidence for Stat3 activation in nearly 50% of lung cancers suggesting a functional role for this target in subsets of lung cancer.12-14 IL-6 and JAK signaling regulates Stat3 activity in lung cancer cells through an autocrine mechanism. 12 Our previous study found IL-6 to be a strong activator of Stat3 in lung cancer cells and along with its expression in lung cancer tumors suggests that this pathway could be responsible for constitutive Stat3 levels in lung cancer tumor cells.15-17 There is evidence in mouse models that tobacco smoke exposure leads to activation of the IL6/Stat3 pathway.18 Finally, overexpression of Stat3 in alveolar type II epithelial cells in mice leads to severe inflammation (associated with increased production of cytokines and chemokines) and spontaneous generation of adenocarcinomas.19 For these reasons, targeting Stat3 activation could be an important approach toward the prevention of lung cancers.
Curcumin (diferuloylmethane) is a natural compound derived from the rhizome of Curcuma Longa, an East Indian plant, commonly called turmeric. Historically, curcumin has been used to treat inflammatory disorders, including various respiratory conditions with no toxicity observed with use.20-2 The major curcuminoids present in turmeric are demethoxycurcumin, bisdemethoxycurcumin and cyclocurcumin, together termed the curcuminoid complex.23-24 Extensive research over the past two decades suggests that curcumin has multiple molecular targets and influences several biochemical and molecular cascades involved in cell cycle regulation, apoptosis, proliferation, survival, invasion, angiogenesis, metastasis and inflammation providing support for the chemoprevention potential of curcumin.25-36 In further support of this, studies with curcumin in lung carcinogenesis have demonstrated that it can induce apoptosis in human lung adenocarcinoma A549 and non-small cell lung cancer NCI-H460 cells, in a dose-dependant manner through mitochondria-dependent pathways. 35-36 Curcumin has also been shown to inhibit the migration and invasion of A549 lung cancer cells through the inhibition of matrix metalloproteinase-2 and -9 and Vascular Endothelial Growth Factor (VEGF), demonstrating its anti-metastatic potential.32
In preclinical trials with rodent models, studies have demonstrated curcumin’s chemopreventive potential in lung cancer. In a K-ras-induced mouse model, Moghaddan et al.,37 administered curcumin, 1% in diet before and during weekly NTHi exposure. This significantly reduced the number of visible lung tumors in the absence of NTHi exposure by 85% and in the presence of NTHi exposures by 53%. Mechanistically, curcumin markedly suppressed NTHi-induced increased levels of the neutrophil chemoattractant keratinocyte-derived chemokine by 80% and neutrophils by 87% in bronchoalveolar lavage fluid. In vitro studies of murine K-ras-induced lung adenocarcinoma cell lines (LKR-10 and LKR-13) indicated direct anti-tumoral effects of curcumin by reducing cell viability, colony formation and inducing apoptosis. The authors concluded that curcumin suppresses the progression of K-ras-induced lung cancer in mice by inhibiting intrinsic and extrinsic inflammation and by direct anti-tumoral effects. These findings suggest that curcumin could be used to protract the premalignant phase and inhibit lung cancer progression in high-risk COPD patients.37 It has also been shown that curcumin increases antioxidant defenses in lung, ameliorates radiation-induced pulmonary fibrosis, and improves survival in mice38 while not impairing tumor cell killing by radiation.
Based on the existing evidence we hypothesized that bioavailable curcuminoid complex may modulate lung carcinogenesis, primarily by inhibiting Stat3 activation. With the safety of curcumin well established due to the long use as a component of food in India, the objective of our studies is to test our hypothesis in vitro and in vivo, in an effort to inform the design of a phase II chemoprevention trial of curcumin in former smokers.
Materials and Methods
Curcuminoid compound
We selected Sabinsa’s Curcumin C3 Complex® which is composed of three main chemical compounds – Curcumin, Demethoxycurcumin and Bisdemethoxycurcumin – collectively known as Curcuminoids. C3 curcuminoid capsules, provided in a single batch by the Sabinsa Corporation (Piscataway, NJ) to be used in these studies. Sabinsa Corporation received Generally Recognized As Safe (GRAS) status for this branded and patented ingredient Curcumin C3 Complex® – curcuma longa (turmeric), after a comprehensive review of safety and toxicology data by an independent panel of scientists with international repute assembled by Soni & Associates, Inc. This formulation was selected on account of its reproducibility and bioavailability of curcuminoid content as demonstrated in previous trial in humans.
Cell culture
AALE normal human bronchoepithelial cells were provided by Melissa Hector (Dana-Farber Cancer Institute, Boston, MA), and H441 human lung adenocarcinoma cells were purchased from ATCC (Manassas, VA). AALE were cultured in BEBM medium with BEGM supplements (Lonza, Walkersville, MD), and H441 were cultured in RPMI with 10% FBS.
Antibodies and Immunoblotting
The anti-CycD1 and anti-phosphotyrosine-Stat3 (P-705) rabbit polyclonal antibodies were obtained from Cell Signaling (Danvers, MA) and total Stat3 rabbit polyclonal antibody was obtained from Santa Cruz Biotech (Santa Cruz, CA). Rabbit polyclonal anti-Mcm2 was generated by the Alexandrow lab and has been reported previously.39-40 Mouse monoclonal anti-Actin was obtained from Sigma-Aldrich (St. Louis, MO) and used at 1:10,000 for immunoblotting. All other primary antibodies were used at a dilution of 1:1000 for immunoblots. Immunoblotting experiments were performed using standard techniques and enhanced chemiluminescence (ECL).
Mouse experiments
CD-1 female nude mice were obtained from Charles River (Wilmington, MA). The mice were treated with Curcumin after 6-7 weeks, and weight of each mouse was ~22 g. Curcumin dissolution with dimethyl sulfoxide (DMSO) was given to mice at a dose of 50mg/2.5ml/kg by daily intraperitoneal (i.p.) injection. Equal amounts of DMSO diluted in water were administered to the control group. 12 mice were randomly divided into 3 groups of 4. Two groups of mice were given Curcumin for 3 days or 9 days. The control group was given DMSO for 9 days. The mice were sacrificed and whole lung tissue was removed for generating the protein extracts. 80μg of total protein extract was used for immunoblotting with indicated antibodies.
Results
Curcumin suppresses Stat3 activation and proliferation of lung cells in culture
We treated non-tumor derived, normal (but immortalized) human bronchial epithelial cells (Figure 1A, AALE cells) and human lung adenocarcinoma derived cells (Figure 1B, H441 cells) with bioactive Curcumin C3 Complex. Asynchronous cells in each case were treated with curcumin at the doses indicated for 24 hrs, followed by immunoblotting for Stat3-P and unphosphorylated Stat3 in total protein extracts. The Stat3 signal was used for normalization to determine changes in Stat3-P levels by densitometry. In both AALE and H441 cells, treatment with curcumin resulted in a dose-dependent reduction in the levels of activated Stat3, as measured by the levels of Stat3 phosphorylated on tyrosine-705 (Stat3-P). In addition, curcumin treatment resulted in reduced cell proliferation in a dose-dependent manner for both the AALE and H441 cells (Figure 2A&B). We conclude from these in vitro culture studies that the activity of the Stat3 pathway in normal and lung carcinoma cells can be suppressed by curcumin treatment, concomitant with a reduction in cell proliferation. Although we do not have access to true dysplastic cell lines in culture, we further conclude from these results using immortalized normal (and tumor-derived) lung cells as a surrogate that curcumin likely has the propensity to suppress non-neoplastic cells that will be present in dysplastic lesions. Importantly, such findings provide a rationale for performing a phase II chemopreventive curcumin trial in former smokers.
Figure 1. Curcumin Inhibits the Stat3 Pathway in Normal and Lung Cancer Derived Human Bronchoepithelial Cells.
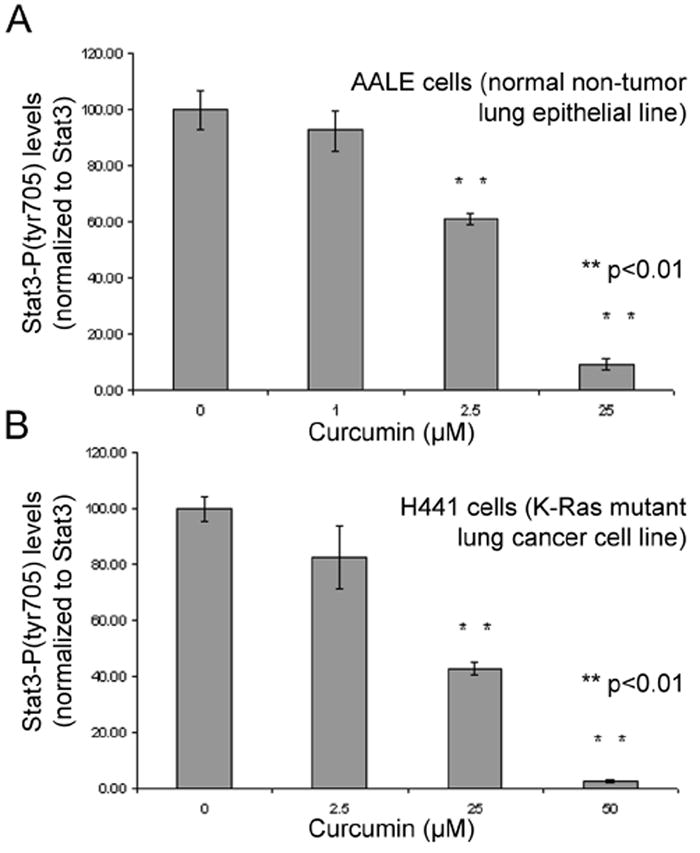
Asynchronous AALE (A) or H441 (B) cells were treated with curcumin at the doses indicated for 24 hrs, following which immunoblots were performed on total protein extracts for Ptyr705-Stat3 and total Stat3. Densitometric readings were used to normalize P-Stat3:Stat3, and resulting data are shown +/- 1 S.D. Untreated samples were arbitrarily set at 100% Stat3-P level (first column in each set). Statistically significant differences are indicated with P-values.
Figure 2. Curcumin Inhibits the Proliferation of Human Normal and Lung Cancer Cells.
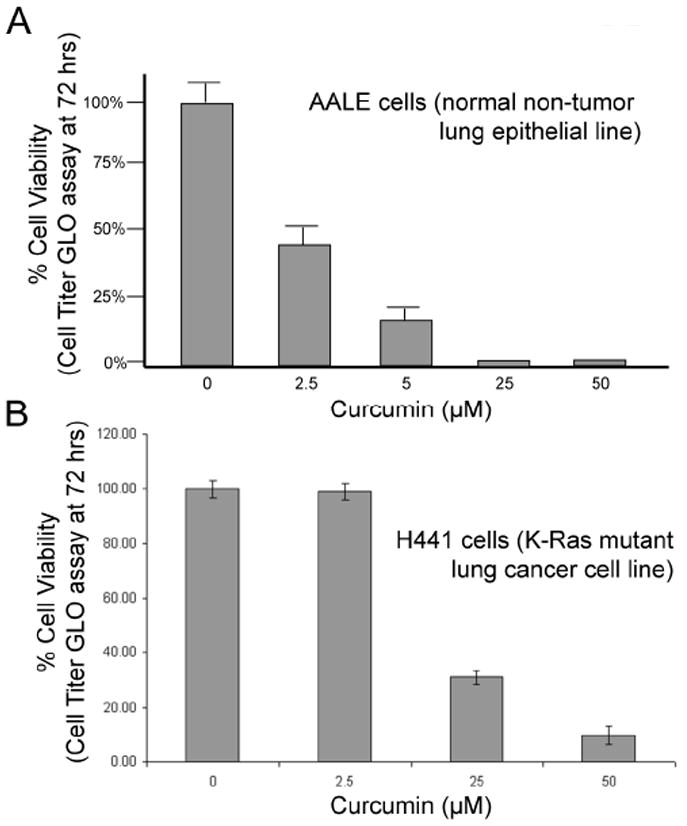
Asynchronous AALE (A) or H441 (B) cells were treated with curcumin at the doses indicated for 24 hrs, following which cell viability (GLO) assays were performed to determine growth suppressive effects of curcumin on each cell type. Triplicate samples were tested, and average results are shown +/- 1 S.D. Samples were normalized to untreated samples shown in first column in each graph, arbitrarily set to 100% viability.
Curcumin suppresses Stat3 activation and proliferation in lung tissue in vivo
We performed a preclinical trial in which 12 mice were randomly divided into three groups and subjected to 3 days or 9 days of curcumin intraperitoneal (i.p.) injections (or DMSO control), followed by analysis of lung tissues for Stat3-P changes and growth suppressive effects of the curcumin (Figure 3). The growth suppressive effects were measured using Cyclin D1 and Mcm2 as surrogates for the proliferative capacity of the tissues. Cyclin D1 is a well known cell cycle regulatory protein expressed in proliferating cells, and Mcm2 is a member of the DNA replicative helicase hexameric complex active and expressed in proliferating cells in culture and in animal tissues.39-41 Intriguingly, curcumin exposure dramatically suppressed Stat3-P (but not Stat3 total levels), and further suppressed Cyclin D1 and Mcm2 markers, the latter two indicative of a reduced proliferative capacity of the lung tissues in the presence of curcumin for 3 or 9 days. We conclude from this in vivo pre-clinical study that curcumin treatment indeed has the ability to suppress the proliferative capacity of lung tissues in animals, which is accompanied by a significant reduction in Stat3-P activation. This further supports our rationale for a chemopreventive curcumin trial for former smokers, and our hypothesis that Stat3-P suppression is an important mechanism by which curcumin reduces cell growth.
Figure 3. Curcumin Suppresses the Proliferative Capacity of Normal Lung Tissue in vivo in Mice.
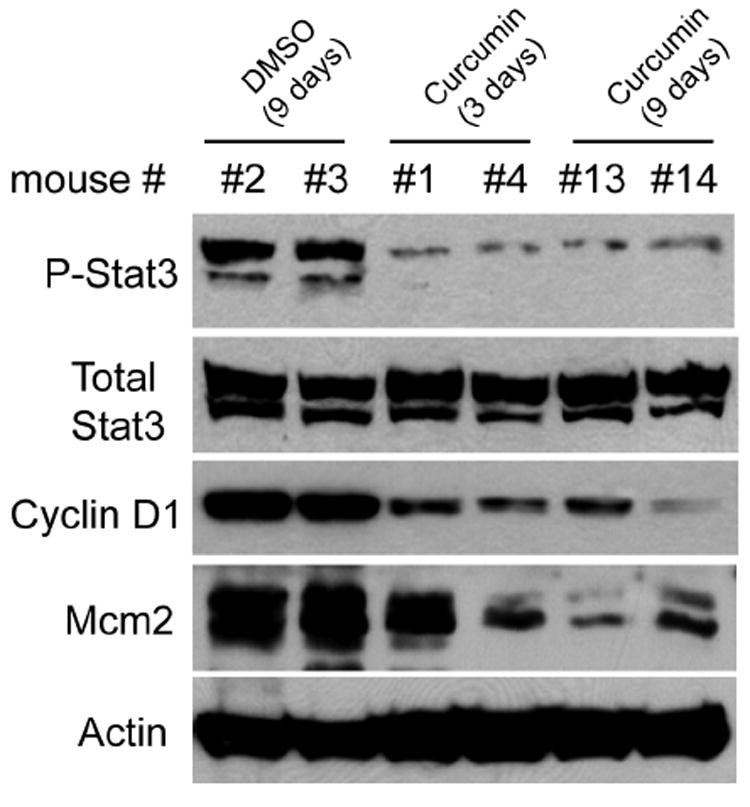
Curcumin (cur) in DMSO (or DMSO as a control) was given to mice at 50mg/2.5ml/kg daily by i.p. injection, for 3 or 9 days. 12 mice were randomly divided into 3 groups: (9d DMSO, 3d cur, 9d cur), and results from two mice for each condition are shown. Immunoblots were performed on total protein extracts using antibodies indicated, from mice sacrificed to obtain whole lung tissue for protein samples. Similar results were obtained in the remaining mice for each condition.
Discussion
These results show that the activity of the Stat3 pathway in both normal human bronchoepithelial cells and lung cancer derived cells is sensitive to curcumin exposure. In a dose-dependent manner, curcumin treatment results in significant suppression of Stat3 phosphorylation, indicative of Stat3 pathway suppression, and concomitantly reduces the proliferative capacity of both cell types. In agreement with this, preclinical trials using rodent models,37-38 and similar results herein, demonstrate that curcumin reduces Stat3-P and proliferation of murine lung tissue in vivo. Altogether, these findings support our hypothesis that inhibition of the Stat3 pathway represents at least one important mechanism by which curcumin elicits its growth-suppressive effects on the bronchoepithelium.
Future Directions
There is a pressing need to identify novel agents for lung cancer chemoprevention beyond smoking cessation. Several novel nutrient-derived substances such as black and green tea polyphenols, resveratrol, isoflavones, Indole-3-Carbinol and anthocyanins 42-46 have shown promise in preclinical and laboratory studies for lung cancer chemoprevention Among these naturally derived compounds, as demonstrated in our preclinical and invitro studies, curcumin appears most promising in modulating lung carcinogenesis. Several recently completed phase I-II clinical trials targeting gastrointestinal tract cancers have also reported curcuminoid formulations, especially with peperine to be bioavailable, with no dose-limiting toxicity at doses from 3.6 grams up to 12 g/day 47-53. These data provide a scientific rationale and support further evaluation of the safety and effectiveness of curcumin compounds in modulating lung carcinogenesis in well powered, phase II randomized chemoprevention trials, targeting populations at high risk for lung cancer such as former smokers and thus advancing our knowledge of the chemopreventive effects of curcumin. If the safety and efficacy of curcumin on valid intermediate endpoint biomarkers of lung cancer can be demonstrated in these clinical trials, this coupled with our provocative mechanistic rationale and consistent animal studies, can identify this agent as a potential chemopreventive agent that can be used in the form of oral supplements as well as well as in the daily diet in preventing lung cancer in healthy as well as high risk populations such as former smokers.
Acknowledgments
This research study was funded by an NCI Lung SPORE awarded to the Moffitt Cancer Center (1P50-CA119997) and 1R01 CA121182 (E.B.H). The Alexandrow Lab is supported by additional funds from the NCI (R01-CA130865 and R21-CA155393).
Footnotes
Publications/Presentations: To date, the results of this trial in part or as a whole have not been reported or presented elsewhere.
Disclaimers: None
Bibliography
- 1.Keith RL, Blatchford PJ, Kittelson J, Minna JD, Kelly K, Massion PP, Franklin WA, Mao J, Wilson DO, Merrick DT, Hirsch FR, Kennedy TC, Bunn PA, Jr, Geraci MW, Miller YE. Oral iloprost improves endobronchial dysplasia in former smokers. Cancer Prev Res (Phila) 2011 Jun;4(6):793–802. doi: 10.1158/1940-6207.CAPR-11-0057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jemal A, Siegel R, Ward E, Murray T, Xu J, Thun MJ. Cancer statistics, 2007. CA Cancer J Clin. 2007;57:43–66. doi: 10.3322/canjclin.57.1.43. [DOI] [PubMed] [Google Scholar]
- 3.Garfinkel L, Silverberg E. Lung cancer and smoking trends in the United States over the past 25 years. CA Cancer J Clin. 1991;41:137–45. doi: 10.3322/canjclin.41.3.137. [DOI] [PubMed] [Google Scholar]
- 4.Irvin JE, Brandon TH. The increasing recalcitrance of smokers in clinical trials. Nicotine Tob Res. 2000;2:79–84. doi: 10.1080/14622200050011330. [DOI] [PubMed] [Google Scholar]
- 5.Tong L, Spitz MR, Fueger JJ, Amos CA. Lung carcinoma in former smokers. Cancer. 1996;78:1004–1010. doi: 10.1002/(SICI)1097-0142(19960901)78:5<1004::AID-CNCR10>3.0.CO;2-6. [DOI] [PubMed] [Google Scholar]
- 6.Lynch TJ, Adjei AA, Bunn PA, Jr, Eisen TG, Engelman J, Goss GD, Haber DA, Heymach JV, Janne PA, Johnson BE, et al. Summary statement: novel agents in the treatment of lung cancer: advances in epidermal growth factor receptor-targeted agents. Clin Cancer Res. 2006;12:4365s–4371s. doi: 10.1158/1078-0432.CCR-06-1005. [DOI] [PubMed] [Google Scholar]
- 7.Kelly K, Kittelson J, Franklin WA, Kennedy TC, Klein CE, Keith RL, Dempsey EC, Lewis M, Jackson MK, Hirsch FR, Bunn PA, Miller YE. A randomized phase II chemoprevention trial of 13-CIS retinoic acid with or without alpha tocopherol or observation in subjects at high risk for lung cancer. Cancer Prev Res (Phila Pa) 2009;2(5):440–9. doi: 10.1158/1940-6207.CAPR-08-0136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nicholson AG, Perry LJ, Cury PM, Jackson P, McCormick CM, Corrin B, Wells AU. Reproducibility of the WHO/IASLC grading system for pre-invasive squamous lesions of the bronchus: a study of inter-observer and intra-observer variation. Histopathology. 2001;38:202–8. doi: 10.1046/j.1365-2559.2001.01078.x. [DOI] [PubMed] [Google Scholar]
- 9.O’Shaughnessy JA, Kelloff GJ, Gordon GB, Dannenberg AJ, Hong WK, Fabian CJ, Sigman CC, Bertagnolli MM, Stratton SP, Lam S, et al. Treatment and prevention of intraepithelial neoplasia: an important target for accelerated new agent development. Clin Cancer Res. 2002;8:314–46. [PubMed] [Google Scholar]
- 10.Yu H, Jove R. The STATs of cancer--new molecular targets come of age. Nat Rev Cancer. 2004;4:97–105. doi: 10.1038/nrc1275. [DOI] [PubMed] [Google Scholar]
- 11.Haura EB, Turkson J, Jove R. Mechanisms of disease: Insights into the emerging role of signal transducers and activators of transcription in cancer. Nat Clin Pract Oncol. 2005;2:315–24. doi: 10.1038/ncponc0195. [DOI] [PubMed] [Google Scholar]
- 12.Gao SP, Mark KG, Leslie K, et al. Mutations in the EGFR kinase domain mediate STAT3 activation via IL-6 production in human lung adenocarcinomas. J Clin Invest. 2007;117:3846–56. doi: 10.1172/JCI31871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Haura EB, Zheng Z, Song L, Cantor A, Bepler G. Activated Epidermal Growth Factor Receptor-Stat-3 Signaling Promotes Tumor Survival In vivo in Non-Small Cell Lung Cancer. Clin Cancer Res. 2005;11:8288–94. doi: 10.1158/1078-0432.CCR-05-0827. [DOI] [PubMed] [Google Scholar]
- 14.Cortas T, Eisenberg R, Fu P, Kern J, Patrick L, Dowlati A. Activation state EGFR and STAT-3 as prognostic markers in resected non-small cell lung cancer. Lung Cancer. 2007;55:349–55. doi: 10.1016/j.lungcan.2006.11.003. [DOI] [PubMed] [Google Scholar]
- 15.Haura EB, Livingston S, Coppola D. Autocrine interleukin-6/interleukin-6 receptor stimulation in non-small-cell lung cancer. Clin Lung Cancer. 2006;7:273–5. doi: 10.3816/CLC.2006.n.006. [DOI] [PubMed] [Google Scholar]
- 16.Song L, Turkson J, Karras JG, Jove R, Haura EB. Activation of Stat3 by receptor tyrosine kinases and cytokines regulates survival in human non-small cell carcinoma cells. Oncogene. 2003;22:4150–65. doi: 10.1038/sj.onc.1206479. [DOI] [PubMed] [Google Scholar]
- 17.Yeh HH, Lai WW, Chen HH, Liu HS, Su WC. Autocrine IL-6-induced Stat3 activation contributes to the pathogenesis of lung adenocarcinoma and malignant pleural effusion. Oncogene. 2006;25:4300–9. doi: 10.1038/sj.onc.1209464. [DOI] [PubMed] [Google Scholar]
- 18.Halappanavar S, Russell M, Stampfli MR, Williams A, Yauk CL. Induction of the interleukin 6/signal transducer and activator of transcription pathway in the lungs of mice sub-chronically exposed to mainstream tobacco smoke. BMC Med Genomics. 2009;2:56. doi: 10.1186/1755-8794-2-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Li Y, Du H, Qin Y, Roberts J, Cummings OW, Yan C. Activation of the signal transducers and activators of the transcription 3 pathway in alveolar epithelial cells induces inflammation and adenocarcinomas in mouse lung. Cancer Res. 2007;67:8494–503. doi: 10.1158/0008-5472.CAN-07-0647. [DOI] [PubMed] [Google Scholar]
- 20.Aggarwal BB, Sethi G, Ahn KS, Sandur SK, Pandey MK, Kunnumakkara AB, et al. Targeting signal-transducer-and-activator-of-transcription-3 for prevention and therapy of cancer: modern target but ancient solution. Ann N Y Acad Sci. 2006;1091:151–69. doi: 10.1196/annals.1378.063. [DOI] [PubMed] [Google Scholar]
- 21.Anand P, Sundaram C, Jhurani S, Kunnumakkara AB, Aggarwal BB. Curcumin and cancer: an “old-age” disease with an “age-old” solution. Cancer Lett. 2008;267(1):133–64. doi: 10.1016/j.canlet.2008.03.025. [DOI] [PubMed] [Google Scholar]
- 22.Lao CD, Ruffin MT, 4th, Normolle D, Heath DD, Murray SI, Bailey JM, Boggs ME, Crowell J, Rock CL, Brenner DE. Dose escalation of a curcuminoid formulation. BMC Complement Altern Med. 2006;17:6–10. doi: 10.1186/1472-6882-6-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kiuchi F, Goto Y, Sugimoto N, Akao N, Kondo K, Tsuda Y. Nematocidal activity of turmeric: synergistic action of curcuminoids. Chem Pharm Bull (Tokyo) 1993;41(9):1640–3. doi: 10.1248/cpb.41.1640. [DOI] [PubMed] [Google Scholar]
- 24.Bansal SS, Goel M, Aqil F, Vadhanam MV, Gupta RC. Advanced Drug-Relivery Systems of Curcumin for Cancer Chemoprevention. Cancer Prev Res (Phila) 2011 May 5; doi: 10.1158/1940-6207.CAPR-10-0006. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Goel A, Kunnumakkara AB, Aggarwal BB. Curcumin as “Curecumin”: from kitchen to clinic. Biochem Pharmacol. 2008;75(4):787–809. doi: 10.1016/j.bcp.2007.08.016. Review. [DOI] [PubMed] [Google Scholar]
- 26.Choudhuri T, Pal S, Das T, Sa G. Curcumin selectively induces apoptosis in deregulated cyclin D1-expressed cells at G2 phase of cell cycle in a p53-dependent manner. J Biol Chem. 2005;280(20):20059–68. doi: 10.1074/jbc.M410670200. [DOI] [PubMed] [Google Scholar]
- 27.Aggarwal BB, Harikumar KB. Potential therapeutic effects of curcumin, the anti-inflammatory agent, against neurodegenerative, cardiovascular, pulmonary, metabolic, autoimmune and neoplastic diseases. Int J Biochem Cell Biol. 2009;41(1):40–59. doi: 10.1016/j.biocel.2008.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chen Q, Wang Y, Xu K, Lu G, Ying Z, Wu L, et al. Curcumin induces apoptosis in human lung adenocarcinoma A549 cells through a reactive oxygen species-dependent mitochondrial signaling pathway. Oncol Rep. 23(2):397–403. YEAR IS MISSING. [PubMed] [Google Scholar]
- 29.Wu SH, Hang LW, Yang JS, Chen HY, Lin HY, Chiang JH, et al. Curcumin induces apoptosis in human non-small cell lung cancer NCI-H460 cells through ER stress and caspase cascade- and mitochondria-dependent pathways. Anticancer Res. 30(6):2125–33. YEAR IS MISSING. [PubMed] [Google Scholar]
- 30.Bill MA, Fuchs JR, Li C, Yui J, Bakan C, Benson DM, Jr, et al. The small molecule curcumin analog FLLL32 induces apoptosis in melanoma cells via STAT3 inhibition and retains the cellular response to cytokines with anti-tumor activity. Mol Cancer. 9:165. doi: 10.1186/1476-4598-9-165. YEAR IS MISSING. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kunnumakkara AB, Anand P, Aggarwal BB. Curcumin inhibits proliferation, invasion, angiogenesis and metastasis of different cancers through interaction with multiple cell signaling proteins. Cancer Lett. 2008;269(2):199–225. doi: 10.1016/j.canlet.2008.03.009. [DOI] [PubMed] [Google Scholar]
- 32.Lin SS, Lai KC, Hsu SC, Yang JS, Kuo CL, Lin JP, et al. Curcumin inhibits the migration and invasion of human A549 lung cancer cells through the inhibition of matrix metalloproteinase-2 and -9 and Vascular Endothelial Growth Factor (VEGF) Cancer Lett. 2009;285(2):127–33. doi: 10.1016/j.canlet.2009.04.037. [DOI] [PubMed] [Google Scholar]
- 33.Sameermahmood Z, Balasubramanyam M, Saravanan T, Rema M. Curcumin modulates SDF-1alpha/CXCR4-induced migration of human retinal endothelial cells (HRECs) Invest Ophthalmol Vis Sci. 2008;49(8):3305–11. doi: 10.1167/iovs.07-0456. [DOI] [PubMed] [Google Scholar]
- 34.Cho JW, Lee KS, Kim CW. Curcumin attenuates the expression of IL-1beta, IL-6, and TNF-alpha as well as cyclin E in TNF-alpha-treated HaCaT cells; NF-kappaB and MAPKs as potential upstream targets. Int J Mol Med. 2007;19(3):469–74. [PubMed] [Google Scholar]
- 35.Wu SH, Hang LW, Yang JS, Chen HY, Lin HY, Chiang JH, Lu CC, Yang JL, Lai TY, Ko YC, Chung JG. Curcumin induces apoptosis in human non-small cell lung cancer NCI-H460 cells through ER stress and caspase cascade- and mitochondria-dependent pathways. Anticancer Res. 2010;30(6):2125–33. [PubMed] [Google Scholar]
- 36.Chen QY, Lu GH, Wu YQ, Zheng Y, Xu K, Wu LJ, et al. Curcumin induces mitochondria pathway mediated cell apoptosis in A549 lung adenocarcinoma cells. Oncol Rep. 23(5):1285–92. doi: 10.3892/or_00000762. YEAR IS MISSING. [DOI] [PubMed] [Google Scholar]
- 37.Moghaddam SJ, Barta P, Mirabolfathinejad SG, Ammar-Aouchiche Z, Garza NT, Vo TT, et al. Curcumin inhibits COPD-like airway inflammation and lung cancer progression in mice. Carcinogenesis. 2009;30(11):1949–56. doi: 10.1093/carcin/bgp229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lee JC, Kinniry PA, Arguiri E, Serota M, Kanterakis S, Chatterjee S, et al. Dietary curcumin increases antioxidant defenses in lung, ameliorates radiation-induced pulmonary fibrosis, and improves survival in mice. Radiat Res. 173(5):590–601. doi: 10.1667/RR1522.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mukherjee P, Cao TV, Winter SL, Alexandrow MG. Mammalian MCM loading in late-G(1) coincides with Rb hyperphosphorylation and the transition to post-transcriptional control of progression into S-phase. PLoS ONE. 2009;4(5):e5462. doi: 10.1371/journal.pone.0005462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mukherjee P, Winter SL, Alexandrow MG. Cell cycle arrest by transforming growth factor beta1 near G1/S is mediated by acute abrogation of prereplication complex activation involving an Rb-MCM interaction. Mol Cell Biol. 2010;30(3):845–56. doi: 10.1128/MCB.01152-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bell SP, Dutta A. DNA replication in eukaryotic cells. Annu Rev Biochem. 2002;71:333–74. doi: 10.1146/annurev.biochem.71.110601.135425. [DOI] [PubMed] [Google Scholar]
- 42.Banerjee S, Manna S, Saha P, Panda CK, Das S. Black tea polyphenols suppress cell proliferation and induce apoptosis during benzo(a)pyrene-induced lung carcinogenesis. Eur J Cancer Prev. 2005 Jun;14(3):215–21. doi: 10.1097/00008469-200506000-00004. [DOI] [PubMed] [Google Scholar]
- 43.Riboli E. Nutrition and cancer of the respiratory and digestive tract: results from observational and chemoprevention studies. Eur J Cancer Prev. 1996 Dec;5(Suppl 2):9–17. doi: 10.1097/00008469-199612002-00002. [DOI] [PubMed] [Google Scholar]
- 44.Bianchini F, Vainio H. Wine and resveratrol: mechanisms of cancer prevention? Eur J Cancer Prev. 2003 Oct;12(5):417–25. doi: 10.1097/00008469-200310000-00011. [DOI] [PubMed] [Google Scholar]
- 45.Pastorino U. Lung cancer chemoprevention. Eur J Cancer Prev. 1994 Jul;3(4):371–3. doi: 10.1097/00008469-199407000-00014. Review. [DOI] [PubMed] [Google Scholar]
- 46.Yu R, Jiao JJ, Duh JL, Gudehithlu K, Tan TH, Kong AN. Activation of mitogen-activated protein kinases by green tea polyphenols: potential signaling pathways in the regulation of antioxidant-responsive element-mediated phase II enzyme gene expression. Carcinogenesis. 1997;18:451–456. doi: 10.1093/carcin/18.2.451. [DOI] [PubMed] [Google Scholar]
- 47.Sharma RA, Euden SA, Platton SL, Cooke DN, Shafayat A, Hewitt HR, Marczylo TH, Morgan B, Hemingway D, Plummer SM, Pirmohamed M, Gescher AJ, Steward WP. Phase I clinical trial of oral curcumin: biomarkers of systemic activity and compliance. Clin Cancer Res. 2004;10(20):6847–54. doi: 10.1158/1078-0432.CCR-04-0744. [DOI] [PubMed] [Google Scholar]
- 48.Cheng AL, Hsu CH, Lin JK, Hsu MM, Ho YF, Shen TS, Ko JY, Lin JT, Lin BR, Ming-Shiang W, Yu HS, Jee SH, Chen GS, Chen TM, Chen CA, Lai MK, Pu YS, Pan MH, Wang YJ, Tsai CC, Hsieh CY. Phase I clinical trial of curcumin, a chemopreventive agent, in patients with high-risk or pre-malignant lesions. Anticancer Res. 2001;21(4B):2895–900. [PubMed] [Google Scholar]
- 49.Bansal SS, Goel M, Aqil F, Vadhanam MV, Gupta RC. Advanced Drug-Relivery Systems of Curcumin for Cancer Chemoprevention. Cancer Prev Res (Phila) 2011 May 5; doi: 10.1158/1940-6207.CAPR-10-0006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Janakiram NB, Mohammed A, Zhang Y, Choi CI, Woodward C, Collin P, Steele VE, Rao CV. Chemopreventive effects of Frondanol A5, a Cucumaria frondosa extract, against rat colon carcinogenesis and inhibition of human colon cancer cell growth. Cancer Prev Res (Phila) 2010;3(1):82–91. doi: 10.1158/1940-6207.CAPR-09-0112. [DOI] [PubMed] [Google Scholar]
- 51.Suresh D, Srinivasan K. Tissue distribution & elimination of capsaicin, piperine & curcumin following oral intake in rats. Indian J Med Res. 2010;131:682–91. [PubMed] [Google Scholar]
- 52.Shoba G, Joy D, Joseph T, Majeed M, Rajendran R, Srinivas PS. Influence of piperine on the pharmacokinetics of curcumin in animals and human volunteers. Planta Med. 1998;64(4):353–6. doi: 10.1055/s-2006-957450. [DOI] [PubMed] [Google Scholar]
- 53.Carroll RE, Benya RV, Turgeon DK, Vareed S, Neuman M, Rodriguez L, Kararala M, Carpenter PM, McLaren C, Meyskens FL, Jr, Brenner DE. Phase IIa clinical trail of curcumin for the prevention of colorectal neoplasia. Cancer Prev Res (Phila) 2011;4(3):354–64. doi: 10.1158/1940-6207.CAPR-10-0098. [DOI] [PMC free article] [PubMed] [Google Scholar]


