Abstract
Background
Klebsiella pneumoniae is a Gram-negative, non-motile, facultative anaerobe belonging to the Enterobacteriaceae family of the γ-Proteobacteria class in the phylum Proteobacteria. Multidrug resistant K. pneumoniae have caused major therapeutic problems worldwide due to emergence of extended-spectrum β-lactamase producing strains. Two-component systems serve as a basic stimulus-response coupling mechanism to allow organisms to sense and respond to changes in many different environmental conditions including antibiotic stress.
Principal Findings
In the present study, we investigated the role of an uncharacterized cpxAR operon in bacterial physiology and antimicrobial resistance by generating isogenic mutant (ΔcpxAR) deficient in the CpxA/CpxR component derived from the hyper mucoidal K1 strain K. pneumoniae NTUH-K2044. The behaviour of ΔcpxAR was determined under hostile conditions, reproducing stresses encountered in the gastrointestinal environment and deletion resulted in higher sensitivity to bile, osmotic and acid stresses. The ΔcpxAR was more susceptible to β-lactams and chloramphenicol than the wild-type strain, and complementation restored the altered phenotypes. The relative change in expression of acrB, acrD, eefB efflux genes were decreased in cpxAR mutant as evidenced by qRT-PCR. Comparison of outer membrane protein profiles indicated a conspicuous difference in the knock out background. Gel shift assays demonstrated direct binding of CpxRKP to promoter region of ompC KP in a concentration dependent manner.
Conclusions and Significance
The Cpx envelope stress response system is known to be activated by alterations in pH, membrane composition and misfolded proteins, and this systematic investigation reveals its direct involvement in conferring antimicrobial resistance against clinically significant antibiotics for the very first time. Overall results displayed in this report reflect the pleiotropic role of the CpxAR signaling system and diversity of the antibiotic resistome in hyper virulent K1 serotype K. pneumoniae NTUH-K2044.
Introduction
Bacteria can encounter numerous environments in which chemical and physical factors such as osmotic pressure, temperature, pH and carbon source availability can change considerably and unpredictably [1]. To adapt to changing conditions, bacteria possess an array of mechanisms which sense external factors and respond accordingly, central to this are the two component systems (TCS) [2].
TCS are signal transduction devices found in all domains of life, and they are especially widespread in bacteria. These systems regulate diverse responses, including nutrient acquisition, energy metabolism, adapting to environmental cues, complex developmental pathways, and host-pathogen interactions. TCS are typically composed of a transmembrane sensor Histidine Kinase protein (HK) and a cytoplasmic transcriptional Response Regulator (RR) [3]. The transmembrane sensor component harbors at least two domains: an input domain that senses the environmental stimulus and a cytoplasmic transmitter with kinase activity that alters the external stimulus into an adaptive signal by autophosphorylation at a conserved histidine residue. The phosphorylated histidine is the resource for phosphorylation of a conserved aspartic acid residue in the receiver domain of the RR. The phosphorylated RR then mediates the cellular response, usually by differential expression of target genes. The target genes of a particular TCS are customized to the specific signal to which the particular TCS corresponds. This specificity is also reflected by the high specificity of HK and RR pairs [3].
The Cpx envelope stress response is controlled by the TCS consisting of membrane localized sensor kinase CpxA and the regulator CpxR. CpxA is induced by a variety of envelope stresses, all of which are predicted to result in protein misfolding. These include physical (osmolarity), chemical (ethanol, pH, indole), and biological (adhesion, lipids) stresses, misfolded proteins (adhesin subunits, β-barrel outer membrane proteins, and misfolded variants of the maltose-binding protein), copper, detergents, and EDTA.
Activation of CpxA involves relief of inhibition through proteolysis of the periplasmic protein CpxP, in addition to other events that require the periplasmic sensing domain of CpxA [4]. This leads to a cascade of phosphotransfer events that ultimately causes a build up of phosphorylated CpxR (CpxR∼P), which functions as a transcription factor to activate and, in a small number of cases, repress transcription of target genes. A set of the target genes encodes envelope protein folding and degrading factors, such as the periplasmic protease/chaperone DegP/HtrA, the major disulphide oxidase DsbA and two peptidyl-prolyl-isomerases PpiA and PpiD [5]. Accordingly, a major role of the Cpx response appears to be to maintain envelope protein folding status in the presence of adverse conditions. Molecular, biological and biochemical analysis of several Cpx signals supports the notion that most signals are specific. Therefore the Cpx system serves as an efficient model system to determine the mechanisms involved in signal transduction by a TCS, ranging from signal integration by the kinase CpxA to the output response by CpxR [6].
Studies have elucidated the different functions displayed by the Cpx system for example in envelope stress response system, pilus assembly, type III secretion, motility and chemotaxis, adherence, and biofilm development [6]. Furthermore, the Cpx system is required for invasion of host cells in diverse pathogenic bacteria, including Escherichia coli, Salmonella enterica serovar Typhimurium, Shigella sonnei, Yersinia enterocolitica, and Legionella pneumophila [6]–[7]. A recent study demonstrated that Xenorhabdus nematophilus requires the Cpx system both to colonize its nematode host (Steinernema carpocapsae) and to kill larvae of the tobacco hornworm (Manduca sexta) [8]. Overall, the Cpx system of bacteria is known to be involved in maintenance, adapt and protection of the bacterial envelope in response to a variety of stressors, one such environmental assail that pathogenic bacteria for example E. coli, Salmonella spp., Enterobacter spp., Campylobacter spp., Acinetobacter spp., Pseudomonas spp., including Klebsiella spp., get exposed to is the pressure of antibiotics. Though the Cpx system has been implicated in the multidrug resistance (MDR) of various human pathogens, however its direct involvement in regulating antimicrobial resistance has remained completely unexplored. Here, we initiated a systematic study to elucidate the direct role of Cpx TCS in conferring drug resistance by constructing a cpxAR deletion mutant in a notoriously drug resistant model organism; Klebsiella pneumoniae.
K. pneumoniae are opportunistic pathogens and can give rise to severe diseases such as septicemia, pneumonia, urinary tract infections, and soft tissue infection. The hospitalized, immune compromised patient with underlying diseases is the main target of these bacteria. Thus, Klebsiella infections may serve as a paradigm of hospital-acquired infections. Their incidence of 5 to 7% of all hospital-acquired infections ranks them among the most important nosocomial pathogens. Klebsiella infections are not only responsible for nosocomial infections but also for community acquired infections such as severe liver abscesses. The capsular polysaccharide on their surface is the prime factor of virulence and toxicity in causing pyogenic liver abscess, with a high 10–30% mortality rate globally [9]. The K. pneumoniae NTUH-K2044 strain encapsulated with K1 hyper virulent antigen is usually isolated from clinical liver abscess patients. Increasingly, Klebsiella bacteria have developed antibiotic resistance, most recently to the class of antibiotics known as carbapenems. The MisT2 database (http://mistdb.com/) has shown the presence of >466 signaling proteins in the 5,472,672 bp (GC content: 57.4%) genome sequence of the K1 serotype (Accession No: AP006725.1) [10]. Though the biological functions of few TCS have been demonstrated previously; however the role of Cpx system has never been examined. Due to their central role in bacterial virulence regulation and their absence in animals including humans, TCS have been suggested as targets for antimicrobials, thus it is prudent to investigate their role in bacterial physiology in general and drug resistance in particular.
In this report experimental evidence for the various physiological functions displayed by CpxAR system in K. pneumoniae NTUH-K2044 has been demonstrated for the very first time.
Results
Bioinformatic analysis of KP1_0078 (cpxA)/KP1_0079 (cpxR) TCS
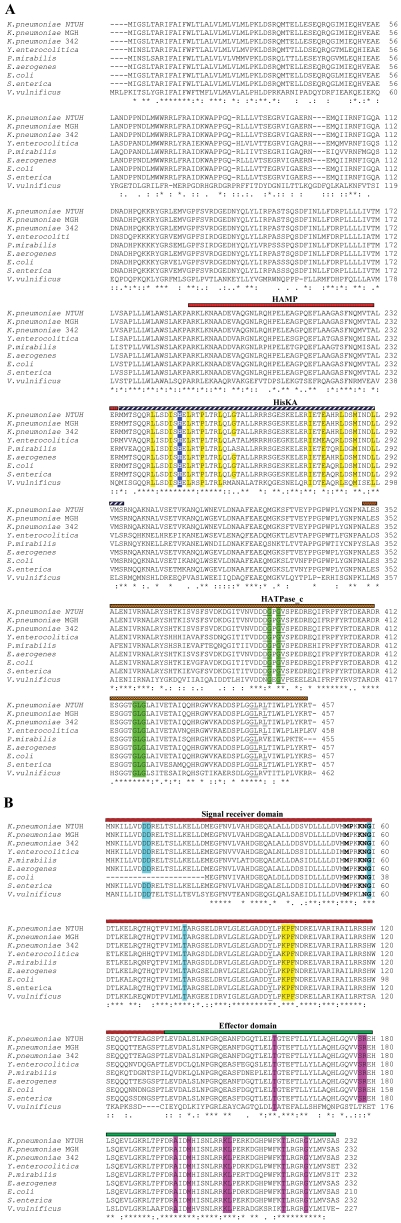
The K. pneumoniae gene KP1_0078 (1374 bp, 457aa) upon performing BLAST exhibits >75% identity (in brackets) with CpxA protein of other organisms with the closest homolog being CpxA of Enterobacter aerogenes (99%), S. Typhimurium (96%), E. coli (95%), Shigella flexneri (95%), Proteus mirabilis (86%), Yersinia pestis (88%) [4], [6]. Structural motifs present in K. pneumoniae CpxA mark it as the sensor/HK component of a TCS. Secondary-structure prediction and comparison to known HK structures indicates that this CpxA has a short, cytoplasmic part (amino acids 1 to 8), followed by a transmembrane helix (amino acids 9 to 27), residues 28 to 164 comprise the extracellular region with mixed secondary structures and probably which serve as the sensor, residues 165 to 182 forms the second transmembrane helix and amino acids from 183 to 457 comprises a large cytoplasmic region and other conserved residues/domains are present in its primary sequence (Figure 1A).
Figure 1. Multiple sequence alignment of KP1_0078 (CpxA homolog) and KP1_0079 (CpxR homolog) from other Gram negative bacteria.
A)Sequence alignment of KP1_0078 with CpxA from other bacteria. Sequence based multiple alignment of KP1_0078 with CpxA homologues. The accession numbers (given in brackets) of CpxR from different bacteria; K. pneumoniae NTUH-K2044 (BAH60994.1), K. pneumoniae MGH78578 (ABR79598.1), K. pneumoniae 342 (YP_002241207.1), Y. enterocolitica (YP_001004479.1), P. mirabilis (YP_002152884.1), E. aerogenes (YP_004591708.1), E. coli (YP_003231578.1), S. Typhimurium (NP_462939.1), V. vulnificus (NP_935907.1). Clustal W alignment (www.ebi.ac.uk/clustalw) of CpxA illustrates three conserved domains such as HAMP (amino acids 191–234), HisKA (amino acids 236–296) and HATPase_ c (amino acids 350–451). Probable phosphorylation site which are conserved are shown in blue shaded boxes with bold letters and dimer interface residues are yellow shaded. Residues that are conserved in ATP binding including the G-X-G motifs are highlighted in green and underlined. B) Sequence alignment of KP1_0079 with CpxR from other bacteria. Sequence based multiple alignment of KP1_0079 with CpxR homologues. The accession numbers (given in brackets) of CpxR from different bacteria; K. pneumoniae NTUH-K2044 (YP_002917062.1), MGH78578 (YP_001337866.1), K. pneumoniae 342 (YP_002241206.1), Y. enterocolitica (YP_001004480.1), P. mirabilis (YP_002152885.1), E. aerogenes (YP_004591709.1), E. coli (EFZ74944.1), S. Typhimurium (NP_462940.1), V. vulnificus (NP_760183.1). ClustalW alignment of CpxR revealed conserved two domains encompassing signal receiver (amino acids 5–115) and effector domain (amino acids 134–228). The conserved domain analyses (www.ncbi.nlm.nih.gov/Structure/cdd/cdd.shtml) were performed to identify the functionally important residues. Conserved residues contributing to the formation of active site are shown in light blue shade and probable intermolecular recognition sites which are close to active site are highlighted in bold. Probable DNA binding residues are highlighted in magenta. (*) represents identical residues, (:) and (.) indicates high and low similarity respectively.
The KP1_0079 (699 bp, 232aa) gene encodes a 23 kDa protein with homology to CpxR proteins which are the RRs in TCSs. KP1_0079 exhibits highest level of homology to CpxR of E. aerogenes (99%), S. Typhimurium (96%), E. coli (95%), S. flexneri (95%), P. mirabilis (79%), and Y. pestis (81%) [4], [6]. Comparing K. pneumoniae CpxR to other RRs indicates that this CpxR has two domains: an N-terminal signal receiver domain (amino acids 5 to 115) and a C-terminal effector domain (amino acids 134 to 228) (Figure 1B). In the receiver domain, the residue (D51) necessary for phosphoryl transfer from CpxA is conserved.
An analysis of the primary sequence and the secondary-structure prediction for K. pneumoniae aligned CpxR to the sequence of the receiver domain of the structurally characterized YycF from Bacillus subtilis (Protein Data Bank accession number 2ZWM) which indicates that this domain is 50% identical to that of K. pneumoniae CpxR, suggesting that the structures of the two proteins are likely to be very similar. The C-terminal domain of K. pneumoniae CpxR very likely binds to DNA, given its sequence homology to other effector domains that have this function. A multiple sequence alignment of the proteins clearly showed that they were highly conserved throughout bacterial kingdom. Overall, in silico analysis suggests that KP1_0078/KP1_0079 is indeed a CpxA/CpxR signaling system worthy to be characterized.
Construction and morphological analysis of cpxAR deletion mutant
The nucleotide sequence deduced from the 2073 bp DNA fragment obtained from K. pneumoniae NTUH-K2044 shared >75% identity with the CpxA/CpxR regulatory system of Gram negative pathogens. To determine the role of cpxAR, a cpxAR mutant was created by conjugation in the wild-type K. pneumoniae NTUH-K2044. This strain was selected due to its high virulence in a murine model of pneumonia [10]. We used insertion-duplication mutagenesis to interrupt cpxAR, required for the synthesis of a functional signaling system. PCR followed by DNA sequencing was done to confirm the disruption of the operon in K. pneumoniae. RT-PCR analysis confirmed that the mutations abolished the transcription of cpxA and cpxR (data not shown).
The cpxAR mutant appeared as smaller colonies (5.0–5.5 mm on average) compared to wild-type (6.0–6.5 mm on average), [wild type/ΔcpxAR mutant, P = 0.037669].
The average lengths of strings generated by NTUH-K2044 and NTUH-K2044ΔcpxAR mutant as per hypermucoviscosity string test were 5.12, 5.08 cm respectively.
The precipitation test was carried out on the 12 h grown culture in LB broth at 37°C. Both NTUH-K2044 and NTUH-K2044ΔcpxAR did not form a dense pellet after centrifuging at 10,000 g for 10 min.
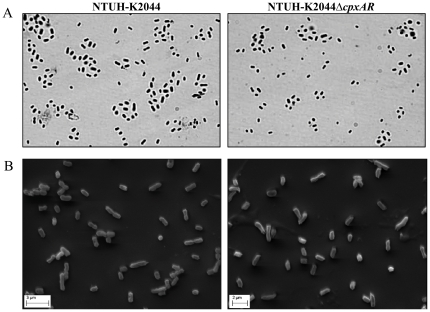
Visualization of cultures under microscope using 20% CuSO4 by Anthony's capsule staining methodology revealed no difference in the exopolysaccharide production around NTUH-K2044 and NTUH-K2044ΔcpxAR (Figure 2A). Quantification of glucuronic acid content reconfirmed the same observation (Table 1).
Figure 2. Characterization of ΔcpxAR mutant.
A) Anthony's capsule staining was performed to visualize wild type and mutant in Olympus microscope work station. No difference was observed between wild type and mutant. B) The morphology of NTUH-K2044 (panel A) and NTUH-K2044ΔcpxAR (panel B) was determined by scanning electron microscopy. No phenotypic alteration was observed.
Table 1. Determination of capsular polysaccharides.
| Strain | Glucuronic acid content (µg/109 CFU)a | Mucoviscosityb |
| NTUH-K2044 | 17.29±1.21 | Very strong |
| NTUH-K2044ΔcpxAR | 16.88±2.87 | Very strong |
| NTUH-K2044ΔcpxARΏcpxAR | 16.98±2.53 | Very strong |
Values are the averages of triplicate samples represented by mean ± standard deviation.
Confirmed by string test.
The effect of deleting cpxAR on the colony morphology of K. pneumoniae was evaluated by scanning electron microscopy. The results indicated no significant difference in cell size of NTUH-K2044 (1.163 µm±0.4) and NTUH-K2044ΔcpxAR (1.196 µm±0.32) (Figure 2B).
Role of cpxAR in bacterial growth
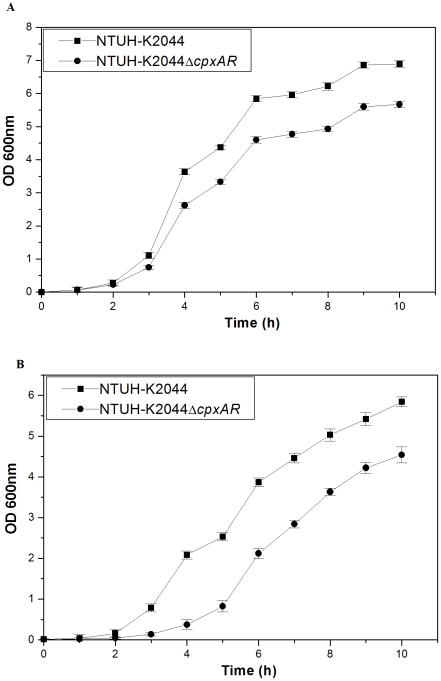
To decipher the involvement of Cpx signal transduction system in inducing a general or global response, the growth kinetics of ΔcpxAR strain was compared with that of the wild type strain. Experimentally the growth characteristics of NTUH-K2044 and NTUH-K2044ΔcpxAR were determined over a period of ∼10 h in LB medium with different pH and analysis revealed unique patterns. We tested the growth kinetics at pH 3.0, 6.0, 8.0 and 12.0 respectively. It was interesting to note that mutant exhibited 1.2–1.3 fold (±0.34) reduced growth compared to the wild type strain in LB at pH 6.0 (Figure 3A) [wild type/ΔcpxAR mutant, P = 0.000859].
Figure 3. Mutant strain displayed stunted growth in LB at varying pH.
Growth kinetics of NTUH-K2044, and NTUH-K2044ΔcpxAR was assessed in LB medium pH 6.0 (A) and pH 8.0 (B).
The NTUH-K2044ΔcpxAR exhibited 5.6 fold stunted growth compared to NTUH-K2044 after 4 h, and displayed a 1.2 fold difference thereafter in LB at pH 8.0 (Figure 3B) [wild type/ΔcpxAR mutant, P = 0.000672]. The differences observed in growth profiles at pH6.0 and pH8.0 were not statistically different.
The other tested pH 3.0 and 12.0 was toxic to both the cultures. The apparent density of the ΔcpxAR culture was 1.3 fold (±0.59) lower compared to wild-type parent strain after 8 h.
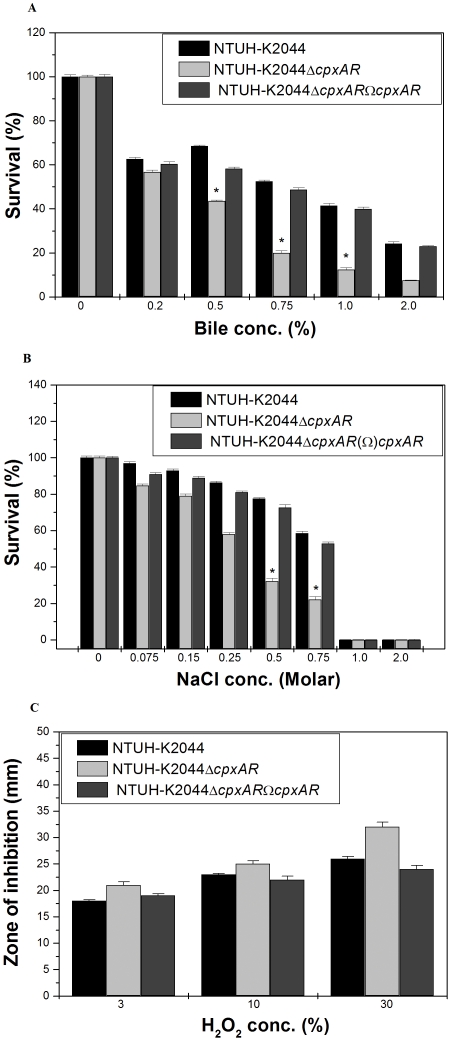
Role of cpxAR in bile and osmotic stress response
To determine the role of cpxAR in intestinal colonization, NTUH-K2044 and NTUH-K2044Δ cpxAR underwent specific gastrointestinal (GI) stress associated with bile and osmotic challenges. In the bile resistance assay, NTUH-K2044 and mutant were exposed to different concentrations (physiological concentration is 0.2% to 2%, [11]) of bile. The ability of NTUH-K2044 to grow in the presence of 0.75% bile was 2.6 fold (±0.089), 1% was 3.5 fold (±0.059) and 2% was 3.2 fold (±0.04) higher when compared to NTUH-K2044ΔcpxAR, while transcomplemented NTUH-K2044ΔcpxARΩcpxAR strain restored the ability to tolerate stress (Figure 4A) [wild type/ΔcpxAR mutant, P = 0.0191; wild type/transcomplememted, P = 0.087].
Figure 4. Survival of NTUH-K2044, NTUH-K2044ΔcpxARand NTUH-K2044ΔcpxARΩcpxAR under different concentration of bile, osmotic and oxidative stress challenge A) Stress sensitivity of the NTUH-K2044 wild-type strain, the cpxAR mutant.
The percentage of resistance to bile (0.2%, 0.5%, 0.75%, 1.0%, and 2.0%) was calculated by comparison to the numbers of viable cells in LB medium alone. B) The percentage of resistance to different concentration of osmotic stress (0.075 M, 0.15 M, 0.25 M, 0.5 M, 0.75 M, 1.0 M and 2.0 M) for NTUH-K2044, and NTUH-K2044ΔcpxAR was calculated by comparison to the numbers of viable cells in control. C) Oxidative stress response of ΔcpxAR mutant. The ability of NTUH-K2044, NTUH-K2044Δ cpxAR to combat different levels of hydrogen peroxide stress (3%, 10% and 30%) was measured by disc diffusion assay. The datas are the means of measurements made in triplicate and performed three times. *, Significant difference (P<0.05, Student t test).
The ability of NTUH-K2044 to grow in the presence of NaCl (physiological concentration being 150 mM, [12]) at 0.25 M was 1.5 fold (±0.024), 0.5 M was 2.5 fold (±0.033), and 0.75 M was 2.7 fold (±0.24), higher when compared to NTUH-K2044ΔcpxAR regardless of the inoculum size (Figure 4B) [wild type/ΔcpxAR mutant, P = 0.030051; wild type/transcomplememted, P = 0.012].
Involvement of cpxAR in oxidative stress tolerance
To deduce whether cpxAR is a peroxide sensor and transcription regulator, we performed the hydrogen peroxide challenge assay. Disc diffusion assay showed that the cpxAR mutant had 1.2 fold greater sensitivity to 30% H2O2 (inhibition zone = 32±1.0 mm) than the wild-type (inhibition zone = 24±0.0 mm) (Figure 4C) [wild type/ΔcpxAR mutant, P = 0.0927; wild type/transcomplememted, P = 0.528], thereby demonstrating that the response of K. pneumoniae cpxAR mutant is conserved in oxidative stress.
Association of cpxAR in antibiotic resistance in K. pneumoniae
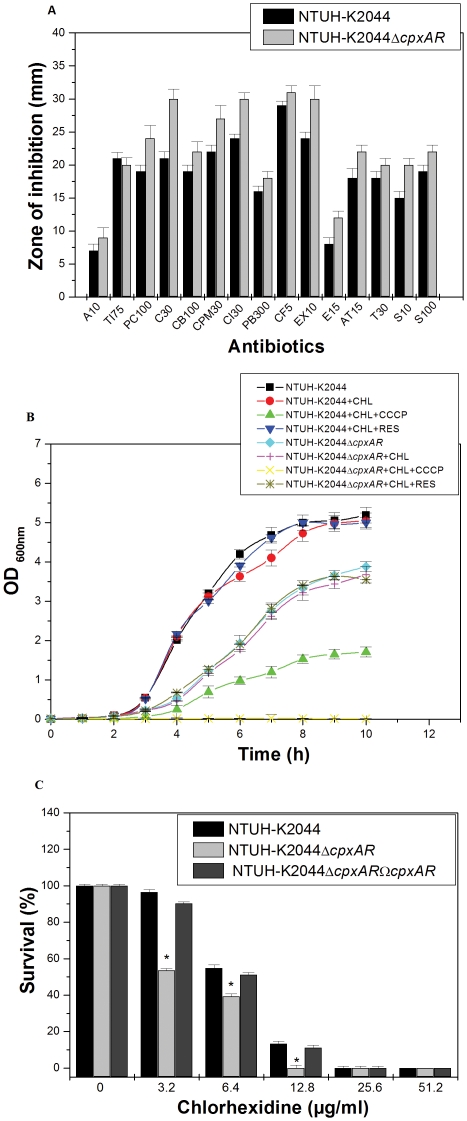
To evaluate the role of cpxAR, antibiotic susceptibilities of NTUH-K2044 and NTUH-K2044Δ cpxAR was monitored. The results of disc diffusion assay displayed that upon deleting the cell envelope response system the bacterial cells significantly displayed sensitivity to β-lactam group of antibiotics (imipenem, cefepime, ceftriaxone, ceftazidime, cefotaxime) and chloramphenicol (Figure 5A).
Figure 5. Antibiotic susceptibility testing, in vitro growth inactivation and chlorhexidine challenge assay with NTUH-K2044, NTUH-K2044ΔcpxARand NTUH-K2044ΔcpxARΩcpxAR.
A) The Kirby Bauer disc diffusion assay was performed with different antibiotics (A10, Ti75, PC100, C30, CB100, CPM30, CI30, PB300, CF5, EX10, E15, AT15, T30, S10 and S100) using commercial discs. Data for representative drugs from each class have been shown here. B) Growth inactivation assays using chloramphenicol (0.005 µg/ml). The efflux pump inhibitors CCCP and reserpine were used at a concentration of 10 µg/ml in the experiment. Abbreviations: CHL = chloramphenicol; RES = reserpine; CCCP = cyanide m-chloro phenyl hydrazone. C) Sensitivity towards disinfectant chlorhexidine was monitored by using the agar dilution assay for different concentrations (3.2 µg/ml, 6.4 µg/ml, 12.8 µg/ml, 25.6 µg/ml, 51.2 µg/ml) for the wild-type strain, and cpxAR mutant. The datas are the means of measurements made in triplicate and performed three times. *, Significant difference (P<0.05, Student t test).
The precise minimum inhibitory concentration (MIC) was further evaluated by following the guidelines of CLSI by E-test. The MIC for K. pneumoniae NTUH-K2044 for the different antibiotics was cefepime (2.048 µg/ml), ceftriaxone (0.016 µg/ml), ceftazidime (0.256 µg/ml), cefotaxime (0.256 µg/ml), and chloramphenicol (0.1 µg/ml) respectively.
The MIC for K. pneumoniae NTUH-K2044ΔcpxAR {fall in MIC fold in brackets} for the same line of drugs were cefepime (0.512 µg/ml, {4 fold}), ceftriaxone (0.016 µg/ml, {1 fold}), ceftazidime (0.128 µg/ml, {2 fold}), cefotaxime (0.064 µg/ml, {4 fold}), and chloramphenicol (0.01 µg/ml, {10 fold}) respectively (Table 2).
Table 2. Determination of MIC for wild type (NTUH-K2044), mutant (NTUH-K2044ΔcpxAR) and complemented (NTUH-K2044ΔcpxARΩcpxAR) strains.
| Antibiotics | NTUH-K2044 | NTUH-K2044ΔcpxAR | Fold changea | NTUH-K2044ΔcpxAR ΩcpxAR |
| Cefepime | 2.048 | 0.512 | 4 | >1.536 |
| Cefotaxime | 0.256 | 0.064 | 4 | 0.256 |
| Ceftazidime | 0.256 | 0.128 | 2 | 0.256 |
| Ceftriaxone | 0.016 | 0.016 | 1 | 0.016 |
| Chloramphenicol | 0.1 | 0.01 | 10 | 100 |
| Erythromycin | 0.01 | 0.01 | 1 | 0.01 |
| Nalidixic acid | 0.01 | 0.01 | 1 | 0.01 |
| Polymyxin | 0.1 | 0.1 | 1 | 0.1 |
| Streptomycin | 0.1 | 0.1 | 1 | 0.1 |
E-strips were used to determine the precise MIC for different group of antibiotics such as amikacin, ampicillin, cefepime, cefotaxime, ceftazidime, ceftriaxone, chloramphenicol, ciprofloxacin, erythromycin, kanamycin, nalidixic acid, ofloxacin, polymyxin, rifampicin, tetracycline, tobramycin, trimethoprim, and vancomycin following the CLSI guidelines.
Fold change is the ratio of MICs for NTUH-K2044 and NTUH-K2044Δ cpxA.
CpxAR influences drug efflux to confer antibiotic resistance
To decipher whether cpxAR confers antibiotic resistance by affecting drug efflux, screening for a potential efflux phenotype was accomplished by determining the growing ability of NTUH-K2044 and NTUH-K2044ΔcpxAR in the presence of chloramphenicol and CCCP or reserpine (10 µg/ml) as described in methods section [13]. The growth rate of NTUH-K2044ΔcpxAR in the presence of 0.005 µg/ml chloramphenicol (MIC being 0.01 µg/ml) was 2 fold lower than that of NTUH-K2044 [wild type/ΔcpxAR mutant, P = 0.00659].
Conversely, both wild type and ΔcpxAR mutant exhibited stunted growth in the presence of chloramphenicol and protonophore CCCP (Figure 5B). In independent experiments, growth remained unaltered on the addition of reserpine. Overall, preliminary findings clearly revealed that cpxAR utilises drug efflux as one of the mechanism to confer resistance against antimicrobial compounds such as chloramphenicol.
CpxAR confers cross resistance to disinfectants
K. pneumoniae is a nosocomial pathogen and has an ability to stay in abiotic surfaces for long [14]; therefore we tested the susceptibilities of NTUH-K2044 and NTUH-K2044ΔcpxAR towards different concentrations of popularly used disinfectant chlorhexidine (Figure 5C) and benzalkonium chloride (data not shown) in hospitals.
The percent survival of NTUH-K2044ΔcpxAR was reduced to 50% upon the lowest exposure of chlorhexidine [wild type/ΔcpxAR mutant, P = 0.014], indicating that cpxAR has a contributory role to mediate disinfectant resistance in this nosocomial pathogen.
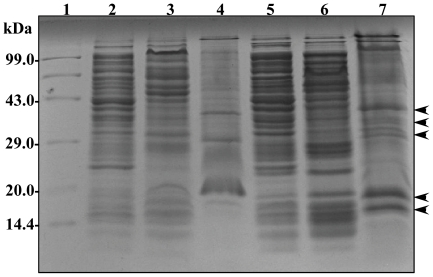
Outer membrane profile of cpxAR deletion mutant in K. pneumoniae
The cell envelope is the prime line for most outside stress conditions that may modify envelope components and thus bring an extra cytoplasmic stress response. In our present study, we found that CpxAR contribute to antibiotic resistance more precisely towards cefepime and chloramphenicol resistance. A reduction in the permeation of antibiotics is generally related to a decrease in porin expression or an alteration in the porin structure [15]. To get an insight, we evaluated the membrane profiles of cpxAR mutant and the wild type. Analysis revealed alterations in both inner and outer membrane fractions of wild type and mutant, however it was intriguing to note the presence of over expressed bands in the outer membrane fractions of cpxAR mutant in varying sizes ∼30 kDa, ∼22 kDa and ∼16 kDa respectively (Figure 6).
Figure 6. Comparison of membrane protein profiles of NTUH-K2044and NTUH-K2044ΔcpxAR.
Membrane protein profiles were compared between the wild-type strain, and cpxAR mutant. Total protein lysate of wild-type strain (lane 2), outer membrane fractions (lane 3), inner membrane fractions (lane 4), followed by total protein lysate of cpxAR mutant (lane 5), outer membrane fractions (lane 6), inner membrane fractions (lane 7). Equal protein concentrations were separated by SDS-PAGE with a 5% stacking gel and a 12% separating gel and stained with coomassie brilliant blue. Lane 1 has molecular weight standards. The over expressed bands in outer membrane fractions of cpxAR mutant are shown by arrow heads.
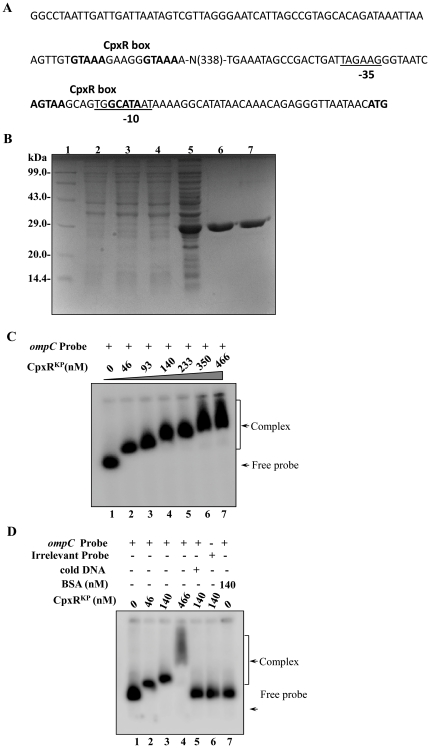
CpxR binds to the promoter region of OmpCKP in K. pneumoniae
The classical porins OmpF and OmpC are major constituents of the E. coli outer membrane and account for approximately 2% of the total protein content of the cell [5]. These proteins allow for the passive diffusion of solutes across the outer membrane. Many environmental factors have been identified that alter OmpF and OmpC expression, including osmolarity, temperature, pH, nutrient availability, and various toxins [5].
The binding site of the RR CpxR in the upstream regulatory region of its target genes has been identified before in E. coli and in S. sonnei [6]. According to these reports, CpxR has a conserved recognition site that contains the sequence GTAAA. A previous study indicated that strong CpxR regulation in E. coli can be correlated with the presence of this motif within 100 bp in the 5′ direction from the transcriptional start site [5], [6]. The DNA binding feature of CpxR prompted us to analyse the promoter regions of outer membrane proteins for the existence of putative CpxR binding sites. Interestingly analysis revealed the presence of a conserved putative CpxR binding site spanning region between 34 to 50 bp from the first methionine of OmpCKP (Figure 7A). The OmpCKP (homologue of E. coli OmpC) is found in the genome of K. pneumoniae KP1_3869, a 1098 bp gene that encodes a polypeptide of 365aa (40 kDa).
Figure 7. Cloning, expression and purification of CpxR and gel retardation assays using radio labeled ompC KP promoter.
A) Promoter region analysis of ompC KP. The numbers in brackets represent the distance from the transcription start site. The −35 and −10 region in the promoter is underlined. CpxR box has been shown in bold. B) SDS-PAGE profile of pET-CpxRKP. Lane 1: medium size marker, Lane 2: pET28C/BL21DE3 uninduced, Lane 3: pET28C/BL21DE3 induced, Lane 4: pET-CpxRKP/BL21DE3 uninduced, Lane 5: pET-CpxRKP/BL21DE3 induced, purified CpxRKP-fractions E1 and E2 (lanes 6–7) respectively. Protein samples after induction were subjected to SDS/PAGE (15% gel) followed by coomassie brilliant blue staining. C) Gel shift assays demonstrating the binding of CpxR to promoter of outer membrane protein OmpC in K. pneumoniae in a concentration dependent manner. Lane 1 (shows free probe), lanes 2–7 with increasing concentrations of CpxR protein (46 nM to 466 nM) respectively. Slower moving bound complexes and free probe has been indicated by arrows respectively. The gels are representative of at least three independent experiments. D) Gel shift assays demonstrating the sequence-specific binding of CpxR to ompC using different controls as in lane 1 (shows free probe), lanes 2–4 (labeled ompC promoter with increasing amount (46 nM, 140 nM and 466 nM) of CpxR), lane 5 (labeled ompC promoter and CpxR with specific competitive inhibitor: 10 fold excess of unlabeled ompC promoter), lane 6 (labeled non-specific DNA: promoter of gyrA and CpxR, 140 nM), lane 7 (labeled ompC promoter with non-specific protein: BSA, 140 nM) respectively. The gels are representative of at least three independent experiments.
To define the possible interaction of CpxRKP to the promoter of OmpCKP, we tested whether CpxRKP directly interacts with its promoter region. For that we first cloned and expressed the cpxR gene. The cpxR gene from K. pneumoniae was PCR amplified, cloned into pET-28c and after transformation in E. coli strain BL21(DE3), expression of the His-tagged protein (CpxRKP) was monitored following IPTG induction. Cell lysates following purification on a Ni-NTA column, where resolved by SDS/PAGE yielded an expected induced band of ∼24 kDa (Figure 7B).
Thereafter, gel shift assays were performed using the 32P-labeled ompC KP promoter fragment and CpxR. The protein-DNA complexes after incubation in reaction buffer were resolved on 5% PAGE gel and analysis revealed a clear retardation which was proportional to the protein concentration as shown in the Figure 7C. Use of various controls such as competitor inhibitor (specific and non-specific: poly (dI-dC)), irrelevant protein as shown Figure 7-D clearly demonstrated the specific DNA binding ability of CpxRKP to promoter region of outer membrane protein ompC KPin K. pneumoniae.
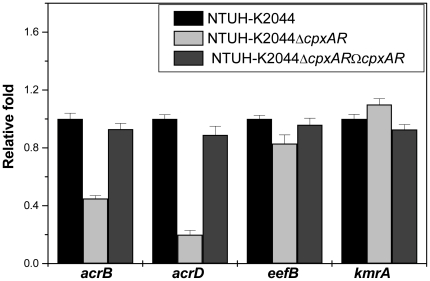
Expression analysis of the efflux genes in K.pneumoniae
Quantitative real-time RT-PCR (qRT-PCR) was used to examine expression of the efflux transporter genes in wild-type, cpxAR mutant, and cpxAR complemented strains. Compared to the wild-type strain, expression of resistance-nodulation-cell division (RND) efflux pump such as acrB, acrD and eefB genes were decreased by 3 fold, 5 fold and 2 fold respectively in the cpxAR mutant (For acrB, ΔcpxAR and wild type: P<0.0001, acrD, ΔcpxAR and wild type: P<0.0001, and eefB, ΔcpxAR and wild type: P<0.0001, Student's t test.), while there was a marginal increase in expression of major facilitator (MFS) type efflux pump kmrA compared to wild type (P values<0.0001) (Figure 8). Complementation of the cpxAR mutation almost restored expression of all the tested genes (P values<0.0001) (Figure 8). These results provide evidence for the additional regulatory role of Cpx system on MDR efflux pumps.
Figure 8. Quantification of the transcript levels of multidrug transporter genes that belong to RND-type and MFS-type efflux pumps.
Relative transcriptional levels of acrB, acrD, eefB, kmrA in NTUH-K2044ΔcpxAR and NTUH-K2044ΔcpxARΩcpxAR strains determined using real time RT-PCR is showed in comparison with wild type. The wild type expression level is represented as one fold. Each bar represents the average value of three independent experiments. Error bars are standard deviations.
Discussion
Bacteria have numerous different systems for sensing their environment and to respond with alterations in gene expression. Given the significance of the integrity of the cell envelope to bacterial survival, it is known that five different systems which respond to stresses in the cell envelope have been explored. Among these, the CpxAR TCS is conceivably the best characterized [2]. At least two important functions have been ascribed to the Cpx system in enteric bacteria; these include regulating factors that deal with misfolded proteins in the periplasmic space and affecting expression of surface components that mediate attachment to some surfaces. It has also been suggested that the Cpx signaling pathway may play a role in signaling E. coli cells present in biofilms to stop making biofilm-related adhesins [16]. The signals that activate the Cpx system in E. coli are diverse and include alkaline pH, overexpression of certain proteins, interaction with abiotic surfaces, and others. The Cpx regulon in E. coli has been described as involving 34 operons and at least 50 genes [17]. In this investigation the unprecedented area i.e. its direct involvement in drug resistance has been decoded in K. pneumoniae. The recently sequenced genomic data of K. pneumoniae NTUH-K2044, encoding 4,992 proteins reveals the presence of CpxAR operon in its genome [10]. The operon was disrupted and its effect on general physiology of the pleomorphic bacillus was studied.
The mucoid slimy nature of cells is indicative of an overproduction of a capsule like polysaccharide in K. pneumoniae, but in our study no significant difference in capsule synthesis between the K. pneumoniae wild-type strain and its cpxAR mutant was detected. It would be worthy to state here that other factors such as the production of exopolysaccharides, pilus synthesis, lipopolysaccharide composition, or the expression of auto transporter proteins, also are responsible for capsule synthesis [18], thus mere deletion of cpxAR might not be sufficient to see a loss in capsule production.
K. pneumoniae is an opportunistic pathogen responsible for many nosocomial infections. Multidrug resistant K. pneumoniae isolates are frequently isolated at an increased frequency, which therefore leads to a therapeutic impasse [19]. The reservoir for K. pneumoniae strain is the GI tract of patients, and GI colonization depends on the ability of the bacteria to adhere to mucosal surfaces, to form biofilm within the mucus layer, and to resist the specific stresses encountered in the GI tract [9]. Epidemiological studies have shown that, whatever the infection site, the first stage in nosocomial infections due to K. pneumoniae consists of the colonization in the patient's GI tract [20]. This pathogen therefore has to sense and respond to numerous different environments in order to survive and, consequently, to persist in the GI tract of the host. The first major barrier encountered following oral consumption is stomach acidity. The bacteria then enter the small intestine, where they encounter stresses associated with volatile fatty acids, variations in pH and osmolarity, and competition with endogenous flora [12].
The behaviour of the wild-type strain and the cpxAR deficient mutants was therefore investigated under some of these hostile conditions to further understand how cpxAR interacts in the GI tract. In the presence of osmotic and bile challenges, cpxAR mutant exhibited two to three fold lower survival capabilities than the wild type, and its level of growth in physiological pH was severely impaired. It is likely, therefore, that the cpxAR factor controls functions required for survival of bacteria in the upper parts of the GI, where they encounter both high osmolarity and bile salts in a microaerobic environment.
Reactive oxygen species, including hydrogen peroxide (H2O2), superoxide, and hydroxyl radical are toxic to cells due to their ability to damage DNA and especially proteins containing iron-sulfur clusters or sulfur atoms [21]. In bacteria, many transcription factors have been found to sense the presence of reactive oxygen species and induce antioxidant system. Evidence for the involvement of cpxAR system in oxidative stress tolerance has been demonstrated in this study.
Antimicrobial therapy for K. pneumoniae is often ineffective as members of the Klebsiella spp., are highly resistant to most clinically relevant antimicrobial agents including disinfectants. MDR in K. pneumoniae isolates is defined as resistance to all of the agents belonging to at least two of three classes of antibiotics, such as quinolones, aminoglycosides, and β-lactam agents. Yamaguchi et al, demonstrated the role of TCS to β-lactam resistance in E. coli. Thirteen RRs present in E. coli genome including cpxR when over reproduced in drug hypersensitive heterologous host, conferred increased β-lactam resistance [22]. In this study we studied the role of cpxAR in antibiotic and disinfectant resistance. Deletion of cpxAR made cells sensitive to β-lactam drugs such as cefepime, cefotaxime, ceftazidime and chloramphenicol which possibly are the preferred substrates of the resistance determinants for e.g. efflux pumps perhaps regulated by the Cpx regulon.
In spite of regular preventive surface disinfection in clinical settings, inanimate surfaces have often been described as the source for the persistence of multidrug resistant K. pneumoniae. This study provides primary evidence for the participation of cpxAR TCS in mediating disinfectant resistance.
Drug efflux represents an important protection mechanism in bacteria to withstand antibiotics and environmental toxic substances [13]. Efflux genes constitute 6–18% of all transporters in bacterial genomes [12]. Particularly interesting among mediators of MDR in K. pneumoniae are the efflux pumps belonging to MFS, RND, ATP binding cassette, small multidrug resistance, multidrug and toxic compound extrusion families [23]. In K. pneumoniae NTUH-K2044, deletion of cpxAR resulted in loss of drug efflux capacity. The cpxAR deletion reduced the expression levels of efflux genes such as acrB, acrD and eefB in mutant when compared to wild type which indicates that possibly CpxR has a role in modulating the expression of MDR efflux pumps.
Classical efflux pump comprises of an outer membrane protein that serves as a channel to regulate the exchange of extra and intra cellular substances which also includes antibiotics, detergents, dyes, organic solvents and bile acids [12]. It was interesting to observe that the outer membrane protein profile of NTUH-K2044ΔcpxAR had over expressed protein bands at ∼30 kDa, ∼22 kDa and ∼16 kDa.
Recently, it has been reported that double deletion of OmpK35 (homolog of OmpF in E. coli) and OmpK36 (homolog of OmpC in E. coli) altered the MIC's of β-lactams class of drugs in K. pneumoniae [7]. Previous study has shown that the expression levels of outer membrane proteins STM1530 and OmpD, were influenced by the cpxAR TCS and it played important roles in mediating ceftriaxone resistance of S. Typhimurium [24].
The notable differences in membrane profile prompted us to investigate the presence of CpxR binding sites in functionally characterized porins such as OmpC homolog (OmpK36) in K. pneumoniae. Evidence for the CpxR protein binding on the promoter fragments of OmpCKP has been shown for the first time which well corroborate with the reports documented previously in other Gram negative bacteria.
One striking feature of the predicted protein complement of K. pneumoniae is the presence of a disproportionately large number of regulatory proteins [10]. Besides the presence of TCS there exists the presence of eukaryotic-type Ser/Thr kinase known as one component system in bacterial genomes. Recently, our group has identified the presence of one component system homologue in K. pneumoniae (data to be communicated). Thus it is not only important to decode the regulatory cascade of the TCS but it is also imperative to understand the correlation between the one component system and TCS to get an overview of global signaling networks in clinically significant pathogens.
Thus, characterizing the functions of CpxAR operon marks just the beginning by in itself. In summary, this study provides preliminary experimental evidence for the participation of cell envelope stress response system CpxAR in mediating resistance against GI stresses, antibiotics and disinfectants in K. pneumoniae NTUH-K2044; hyper virulent K1 serotype for the very first time.
Materials and Methods
Bacterial strains, plasmids and media
K. pneumoniae NTUH-K2044 (a strain that resulted in pyogenic liver abscess in a 66 year old patient) was kindly provided by Dr. Jin Town Wang of the National Taiwan University Hospital, Taipei, Taiwan [25]. E. coli S17-1λ pir which carries the F plasmid and encodes π protein essential for replication of pUT-Km was used for cloning experiments. pUT-Km was used to create insertion-duplication mutations by homologous recombination. Bacteria cultures were grown in Luria-Bertani (LB) broth or on LB agar (Difco, Becton-Dickinson, Sparks, MD) at 37°C with constant shaking (220 rpm) and supplemented with Kanamycin (100 µg/ml) where required. The strains were harvested and stored at −80°C before use.
DNA methods
Restriction digestion, ligation, transformation, and agarose gel electrophoresis were done according to standard protocols. Plasmids were prepared from E. coli using a QIAprep Spin miniprep kit from Qiagen according to the manufacturer's protocol. Mobilization of plasmids into K. pneumoniae cells was performed as previously described [12]. Genomic DNA of K. pneumoniae was extracted using the Gene Aid DNA purification kit according to the manufacturer's instructions. DNA fragments used for cloning were extracted from agarose gels using a QIA quick gel extraction kit from Qiagen. PCR products were purified using a QIA quick PCR purification kit (Qiagen) and, when cloned, sequenced to confirm the correct sequences (Applied Biosystems). Primers used in the present study were custom-synthesized (Eurofins MWG operons, Germany).
Construction of the cpxAR deletion mutant in K. pneumoniae strain NTUH-K2044
The MisT2 database (http://mistdb.com) shows the presence of >466 signaling proteins in the 5,472,672 bp (GC content: 57.4%) genome sequence of the K1 serotype (Accession No: AP006725.1). The CpxAR operon is located starting from nucleotides 76799 bps to 78867 bps (cpxA: 1373 bp, 457aa and cpxR: 698 bp, 232aa) in the genome sequence of K. pneumoniae NTUH-K2044. To construct cpxAR knock out, a 700 bp internal fragment encompassing cpxA and cpxR of the operon was amplified by PCR using ΔcpxA/cpxR-F and ΔcpxA/cpxR-R primer from its genomic DNA (Table 3). The PCR product was ligated into an EcoRI digested plasmid pUT-Km which was blunted by klenow reaction (pUT-Km is a pUTKm1 derived plasmid, with miniTn5 excised by EcoRI, tnp excised by SalI, and bla removed by ApaLI, then with an insertion of kanamycin resistance cassette from pUC4K into PstI site) that contained the kanamycin resistance gene, transformed into E. coli S17-1λ pir and the resulting recombinant plasmid harbouring the internal fragment of cpxAR was designated as pUT-Km/GR. The plasmid pUT-Km/GR was mobilized into recipient K. pneumoniae NTUH-K2044 from donor E. coli S17-1λ pir.
Table 3. Primers used in this study.
| Primer name | Primer sequences (5′-3′) |
| ΔcpxA/cpxR-F | GGAACGAAGTGTTGGACAATGCGGCGTTTG |
| ΔcpxA/cpxR-R | TTATCGATGGCGCGAAACAAACGAC |
| Primer NT | GCGCATCACATACTCCCAAAACGTTTGTGT |
| Primer CT | CCCATATTAAGTATTCCCGGGGATGCTCC |
| cpxR-F | GCGTCATATGAATAAAATCCTGTTAGTTGATGATG |
| cpxR-R | CTCAGGATCCTCATGAAGCGGAAACCATCAGATAC |
| prom ompC-F | GGCCTAATTGATTGATTAATAGTCGTTAGGGAAT |
| prom ompC-R | GTTATTAACCCTCTGTTTGTTATATGCCTTTTAT |
| eefBnt | TTCTCGGTAACCATTATCTCGGCGATGATG |
| eefBct | TTATCTCCCCCTGGTCCTCCACCGG |
| acrBnt | AAGAGCACGCACCATTACACCGACAG |
| acrBct | TTCCTCACCCGGACGCTGGCTCCAGTC |
| acrDnt | GATCCTGCTGGTCTTCCTCGTGAT |
| acrDct | GCCCTGAATTTGTCCCATCGATTT |
| kmrAnt | TGCTGGAGCATTTCTACTGGGGGTCGGTGT |
| kmrAct | TGCAGCTCCTGGGCCATCAGTAGCTCAAAA |
| 16sF (rrsE) | CAGCCACACTGGAACTGAGA |
| 16sR (rrsE) | GTTAGCCGGTGCTTCTTCTG |
Briefly, K. pneumoniae was inoculated into 10 ml LB and was incubated for 2–3 h till OD600 nm reaches 0.2. For matings, recipient and donor culture were mixed in a ratio of 1∶2 respectively, pelleted and spotted onto the centre of an LB agar plate. After 3 h of growth at 37°C the cells were plated on Klebsiella selective agar (HiMedia HiCrome Klebsiella Selective Agar Base cat# M1573; Klebsiella Selective Supplement cat# FD225) containing Kanamycin 100 µg/ml and 5 µg/ml chlorhexidine to select for colonies. It is expected that colonies that appear on the selective plate would be transconjugants that resulted from one DNA exchange event in which the whole suicidal plasmid gets incorporated in the K. pneumoniae genome. The disruption at cpxAR operon was confirmed with selected transconjugant by PCR and DNA sequencing using gene specific and genome flanking primers and deleted mutant was denoted as NTUH-K2044ΔcpxAR.
Intact cpxAR genes were amplified along with its promoter using primer NT (binds −155 bases upstream of cpxR) and primer CT (binds +64 bases downstream of cpxA) and cloned into a pCRIITOPO-CAT plasmid (Table 3). The selected recombinant plasmid harbouring the intact cpxAR operon was transformed into the cpxAR isogenic mutant strain by electroporation. The complementation strains were selected on LB agar plates supplemented with 100 µg/mL kanamycin and 100 µg/mL chloramphenicol and transcomplemented strain was designated as NTUH-K2044ΔcpxARΩcpxAR.
String and Precipitation test for Hypermucoviscosity
The NTUH-K2044 and NTUH-K2044ΔcpxAR was streaked onto LB agar plates and incubated at 37°C overnight. A standard bacteriologic loop was used to stretch a mucoviscous string from the colony. Hypermucoviscosity was defined by the formation of viscous strings >5 mm in length when a loop was used to stretch the colony on agar plate which was considered the positive string test [19]. The strains to be tested were cultured overnight in LB broth at 37°C and subjected to centrifugation at 1,000×g for 5 min to check reduction in mucoidy.
For exopolysaccharide analysis [26], cells were grown to late log phase in shaking culture and stained with crystal violet followed by treatment with 20% copper sulphate solution (Anthony's capsule staining methodology). Samples were visualized using an Olympus microscope work station. Capsular polysaccharides were extracted from overnight bacterial suspensions adjusted to ∼108 cells per ml with Zwittergent 3–14 detergent. The amount of uronic acid was then measured according to the method described previously [27]. Each experiment was performed in triplicate.
Scanning electron microscopy
Overnight cultures were fixed after harvesting; cells were washed three times with ice-cold NaCl/Pi. The cells were then resuspended in NaCl/Pi, adhered to cover slips that had been coated with 0.1% poly (l-lysine). Adherent cells were washed with NaCl/Pi and then dehydrated using an ascending series of ethanol incubations. Finally, cells on covers lips were infiltrated with t-butyl alcohol and freeze-dried in a lyophilizer. Dried samples were sputter-coated with gold/palladium and then observed under a scanning electron microscope [28].
In vitro growth curves
To examine bacterial growth in vitro, overnight cultures were diluted 1∶100 and subcultured for 10 h. The growth kinetics was monitored with LB at different pH (3, 6, 8 and 12). The growth inhibition assay was performed as described previously [13]. The efflux pump inhibitors (10 µg/ml) used in this study was carbonyl cyanide 3-chlorophenylhydrazone (CCCP) and reserpine (Sigma, St. Louis, MO). CCCP is an extremely effective proton motive force inhibitor and used in this study as an active efflux pump blocker. Efflux pump inhibitors had no intrinsic antibacterial activity against wild type strain at the concentration used in the experiments.
Osmotic, bile, chlorhexidine challenge assays
Various stress assays were performed as described previously [12]. Briefly, K. pneumoniae NTUH-K2044 and NTUH-K2044ΔcpxAR were grown to mid-exponential phase, cultures were spread plated onto LB agar plates containing different concentrations of NaCl (0.075 M, 0.15 M, 0.25 M, 0.5 M, 0.75 M, 1.0 and 2.0 M), bile (0.2%, 0.5%, 0.75%, 1.0%, and 2.0%) and chlorhexidine (3.2 µg/ml, 6.4 µg/ml, 12.8 µg/ml, 25.6 µg/ml, 51.2 µg/ml) respectively. The results are expressed as the ratio of the number of colony forming units obtained from LB cultures containing different concentrations of NaCl, bile and chlorhexidine to the number of colony forming units obtained from control cultures (LB agar alone). These experiments were performed at least three times.
Oxidative stress sensitivity assay
In this susceptibility test, small Whatman 3 MM paper disks (6 mm) was impregnated with different amount of H2O2 (10 µl of 3%, 10% and 30%) and later air dried as reported before [27]. The K. pneumoniae NTUH-K2044 and NTUH-K2044ΔcpxAR were grown to the mid-log phase (OD600 nm 0.2) and was uniformly spread over an LB agar plate. Next, filter paper disks impregnated with specific concentrations of H2O2 was placed at the centre on to the agar surface. The culture was then incubated at 37°C for 12–24 hours. The diameter of a zone of inhibition was measured (in millimeters) which is a qualitative measure of the inhibitory activity of a compound. The data represents the distances from the edge of the disks to the end of the clear zone, where growth begins. Each experiment was repeated at least three times.
Antibiotic susceptibility testing
Strains in this study were examined for resistance to nalidixic acid: NA30 (30 µg/ml), colistin: CL30 (10 µg/ml), enrofloxacin: EX10 (10 µg/ml), polymyxin B: PB300 (300 µg/ml), ciprofloxacin: CF5 (5 µg/ml), azithromycin: AT15 (15 µg/ml), erythromycin: E15 (15 µg/ml), tetracycline: T30 (30 µg/ml), rifampicin: R5 (5 µg/ml), trimethoprim: TR5 (5 µg/ml), kanamycin: K30 (30 µg/ml), streptomycin: S10 (10 µg/ml), tobramycin: TB10 (10 µg/ml), clindamycin: CD2 (2 µg/ml), spectinomycin: S100 (100 µg/ml), imipenem: I10 (10 µg/ml), ampicillin: A10 (10 µg/ml), ertapenem: ETP10 (10 µg/ml), piperacillin: PC100 (100 µg/ml), ticarcillin: TI75 (75 µg/ml), ceftazidime: CA30 (30 µg/ml), chloramphenicol: C30 (30 µg/ml), ceftriaxone: CI30 (30 µg/ml), cefepime: CPM30 (30 µg/ml) and carbencillin: CB100 (100 µg/ml) by using commercial discs (Hi Media, Mumbai, India) as described previously according to the interpretation criteria recommended by Clinical and Laboratory Standards Institute CLSI [29].
MIC of antibiotics was tested using E-strips. Interpretation was done as per the criteria approved by CLSI [29]. E. coli ATCC 25922 was used as a reference strain (control) as recommended.
Outer membrane proteins preparation
Outer membrane proteins were purified by the method as described previously [30]. Cells were harvested by centrifugation (5,000× g for 15 min) and were suspended in 50 mM Tris-HCl buffer (pH 7.4) (Tris buffer) containing 5 mM phenylmethylsulfonyl fluoride and sonicated for 15 mins. The crushed material was treated with DNase and RNase (each at 100 µg/ml), and the unbroken cells were removed by centrifugation (10,000× g for 10 min). The crude envelope fraction was collected from the supernatant by centrifugation at 105,000× g for 1 h at 4°C. The pellet containing the crude envelope fraction was treated with 0.5% (wt/vol) Sarkosyl (Sigma) solution to selectively solubilise the inner membrane part. The insoluble outer membrane fraction was recovered as pellet by centrifugation at 105,000× g for 1 h at 4°C. The pellet was washed and stored at −20°C until used. Protein contents of membrane preparations were determined by the method of bicinchoninic acid (BCA) method (Pierce BCA protein assay kit, cat# 23225) with bovine serum albumin (BSA) (Sigma) as standard.
Gene cloning, expression, purification and electrophoretic mobility shift assays
The DNA-binding transcriptional regulator gene cpxR was amplified using gene specific primers, cpxR-F and cpxR-R has NdeI and BamHI site of the pET28C vector to generate an N-terminal His6-CpxR fusion protein. All clones were confirmed by sequencing and transformed into E. coli BL21 (DE3). After induction with 0.2 mM isopropyl 1-thio-β-d-galactopyranoside, CpxR protein was purified through Qiagen Ni2+nitrilotriacetic acid columns. The protein was dialysed using Tris buffer pH 8.0.
The ability of purified recombinant CpxR to bind ompC promoter was examined by using the electrophoretic mobility shift assay (EMSA). The ompC promoter region was amplified using prom ompC-F and prom ompC-R primers (Table 3) and subjected to EMSA with purified CpxR protein. Briefly, end-labelled (using [γ-32P] ATP) PCR products were incubated with increasing concentrations (in a range of 40 nM to 500 nM) of CpxR in binding buffer (10 mM Tris-HCl, pH 8.0, 2 mM EDTA, 0.5 mM DTT, 50 mM NaCl, 10% glycerol, and 1 µg of poly(dI·dC). The complexes were run on 5% native polyacrylamide gel electrophoresis (PAGE) gels for 2 h. The gel was then dried and exposed to the phosphor screen for image analysis. To confirm that the interaction between CpxR and the promoter region of ompC was specific, competition experiments with bovine serum albumin (BSA) as a negative control (non competitive) and with 10 fold excess of cold promoter (competitive) were also performed.
RNA isolation and real-time reverse transcription PCR (RT-PCR)
Total RNA was extracted from the log-phase cultures of K. pneumoniae NTUH-K2044 wild-type and cpxAR mutant using the RNeasy Mini Kit (Qiagen) according to the manufacturer's instructions. Total RNA was digested with DNase I to ensure the removal of contaminating genomic DNA prior to cDNA synthesis. Aliquots of 500 ng of DNase treated total RNA served as template for complementary DNA (cDNA) synthesis using SuperScript III Reverse Transcriptase (Invitrogen). The cDNA samples were diluted 1∶10 and 2 µL was used per 25 µL quantitative PCR reaction for different efflux genes such as acrD: (KP1_4054: aminoglycoside efflux system), kmrA (KP1_2943: smvA; energy-dependent efflux protein for methyl violgen), acrB (KP1_1319: acriflavine resistance protein B), eefB homolog (KP1_5407: acridine efflux pump) were performed using gene specific primers (Table 3).
Gene expression levels were monitored by real time RT-PCR using Maxima SYBR Green qPCR master mix (Fermentas) in an iCycler thermal cycler (Bio-Rad) and the melting curve analysis were carried out to confirm amplification of a single product. Total RNA was isolated from at least two separately grown replicate cultures. All real time RT-PCR experiments were performed in triplicate, with 16sRNA used as an internal control.
Bioinformatic analysis and Statistical analysis
The multiple sequence alignments were carried out using the Clustal program www.ebi.ac.uk Homology searches, similarities and identities analysis and conserved domain architecture analysis were performed using NCBI web server [31], Simple Modular Architecture Research Tool (SMART) www.smart.embl-heidelberg.de and NCBI conserved domain search. All data are presented as means ± the standard error of the mean. Plotting and calculation of the standard deviation was performed in Microsoft Excel. Statistical analysis was performed on crude data by using a paired Student t test. P values of <0.05 were considered significant.
Acknowledgments
We are highly thankful to our Director, CSIR-Institute of Microbial Technology (IMTECH), Chandigarh, for providing excellent facility to carry out this work. DNA sequencing and scanning electron microscopy service facilities provided in IMTECH is highly appreciated. We are also grateful to Dr Jin-Town Wang, National Taiwan University Hospital, for providing K. pneumoniae NTUH-K2044 and plasmids.
Footnotes
Competing Interests: The authors have declared that no competing interests exist.
Funding: VBS, VV, and AM are grateful to Department of Biotechnology (DBT), Innovative Young Biotechnologist Award, Government of India, University Grants Commission (UGC), and Council of Scientific and Industrial Research (CSIR), Diamond Jubilee scheme, Government of India, respectively, for their fellowships. The work was supported by CSIR-Institute of Microbial Technology, India; and a grant provided by Department of Biotechnology, Government of India. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.DiGiuseppe PA, Silhavy TJ. Signal detection and target gene induction by the CpxRA two-component system. J Bacteriol. 2003;185:2432–2440. doi: 10.1128/JB.185.8.2432-2440.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.MacRitchie DM, Buelow DR, Price NL, Raivio TL. Two-component signaling and gram negative envelope stress response systems. Adv Exp Med Biol. 2008;631:80–110. doi: 10.1007/978-0-387-78885-2_6. [DOI] [PubMed] [Google Scholar]
- 3.Stock AM, Robinson VL, Goudreau PN. Two component signal transduction. Annu Rev Biochem. 2000;69:183–215. doi: 10.1146/annurev.biochem.69.1.183. [DOI] [PubMed] [Google Scholar]
- 4.Raivio TL. Envelope stress responses and Gram-negative bacterial pathogenesis. Mol Microbiol. 2005;56:1119–1128. doi: 10.1111/j.1365-2958.2005.04625.x. [DOI] [PubMed] [Google Scholar]
- 5.Raffa RG, Raivio TL. A third envelope stress signal transduction pathway in Escherichia coli. Molecular Microbiology. 2002;45:1599–1611. doi: 10.1046/j.1365-2958.2002.03112.x. [DOI] [PubMed] [Google Scholar]
- 6.De Wulf P, Lin ECC. Cpx two-component signal transduction in Escherichia coli: excessive CpxR-P levels underlie CpxA phenotypes. J Bacteriol. 2000;182:1423–1426. doi: 10.1128/jb.182.5.1423-1426.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chen JH, Siu LK, Fung CP, Lin JC, Yeh KM, et al. Contribution of outer membrane protein K36 to antimicrobial resistance and virulence in Klebsiella pneumoniae. J Antimicrob Chemother. 2010;65:986–90. doi: 10.1093/jac/dkq056. [DOI] [PubMed] [Google Scholar]
- 8.Herbert Tran EE, Andersen AW, Goodrich-Blair H. CpxRA influences Xenorhabdus nematophila colonization initiation and outgrowth in Steinernema carpocapsae nematodes through regulation of the nil locus. Appl Environ Microbiol. 2009;75:4007–14. doi: 10.1128/AEM.02658-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Podschun R, Ullmann U. Klebsiella spp. as nosocomial pathogens: epidemiology, taxonomy, typing methods, and pathogenicity factors. Clin Microbiol Rev. 1998;11:589–603. doi: 10.1128/cmr.11.4.589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wu KM, Li LH, Yan JJ, Tsao N, Liao TL, et al. Genome sequencing and comparative analysis of Klebsiella pneumoniae NTUH-K2044, a strain causing liver abscess and meningitis. J Bacteriol. 2009;191:4492–501. doi: 10.1128/JB.00315-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gunn JS. Mechanisms of bacterial resistance and response to bile. Microbes Infect. 2000;2:907–913. doi: 10.1016/s1286-4579(00)00392-0. [DOI] [PubMed] [Google Scholar]
- 12.Coudeyras S, Nakusi L, Charbonnel N, Forestier C. A tripartite efflux pump involved in gastrointestinal colonization by Klebsiella pneumoniae confers a tolerance response to inorganic acid. Infect Immun. 2008;76:4633–41. doi: 10.1128/IAI.00356-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rajamohan G, Srinivasan VB, Gebreyes WA. Molecular and functional characterization of a novel efflux pump, AmvA, mediating antimicrobial and disinfectant resistance in Acinetobacter baumannii. 2010;65:1919–25. doi: 10.1093/jac/dkq195. [DOI] [PubMed] [Google Scholar]
- 14.Di Martino P, Cafferini N, Joly B, Darfeuille-Michaud A. Klebsiella pneumoniae type 3 pili facilitate adherence and biofilm formation on abiotic surfaces. Res Microbiol. 2003;154:9–16. doi: 10.1016/s0923-2508(02)00004-9. [DOI] [PubMed] [Google Scholar]
- 15.Pagès JM, James CE, Winterhalter M. The porin and the permeating antibiotic: a selective diffusion barrier in Gram-negative bacteria. Nat Rev Microbiol. 2008;12:893–903. doi: 10.1038/nrmicro1994. [DOI] [PubMed] [Google Scholar]
- 16.Dorel C, Lejeune P, Rodrigue A. The Cpx system of Escherichia coli, a strategic signaling pathway for confronting adverse conditions and for settling biofilm communities? Res Microbiol. 2006;157:306–14. doi: 10.1016/j.resmic.2005.12.003. [DOI] [PubMed] [Google Scholar]
- 17.Price NL, Raivio TL. Characterization of the Cpx regulon in Escherichia coli strain MC4100. J Bacteriol. 2009;191:1798–815. doi: 10.1128/JB.00798-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cheng HY, Chen YS, Wu CY, Chang HY, Lai YC, et al. RmpA regulation of capsular polysaccharide biosynthesis in Klebsiella pneumoniae CG43. J Bacteriol. 2010;12:3144–58. doi: 10.1128/JB.00031-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Arnold RS, Thom KA, Sharma S, Phillips M, Kristie Johnson J, et al. Emergence of Klebsiella pneumoniae carbapenemase-producing bacteria. South Med J. 2011;104:40–5. doi: 10.1097/SMJ.0b013e3181fd7d5a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Maroncle N, Balestrino D, Rich C, Forestier C. Identification of Klebsiella pneumoniae genes involved in intestinal colonization and adhesion using signature-tagged mutagenesis. Infect Immun. 2002;70:4729–34. doi: 10.1128/IAI.70.8.4729-4734.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Imlay JA. Pathways of oxidative damage. Annu Rev Microbiol. 2003;57:395–418. doi: 10.1146/annurev.micro.57.030502.090938. [DOI] [PubMed] [Google Scholar]
- 22.Hirakawa H, Nishino K, Hirata T, Yamaguchi A. Comprehensive studies of drug resistance mediated by overexpression of response regulators of two-component signal transduction systems in Escherichia coli. J Bacteriol. 2003;185:1851–6. doi: 10.1128/JB.185.6.1851-1856.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Piddock LJ. Clinically relevant chromosomally encoded multidrug resistance efflux pumps in bacteria. Clin Microbiol Rev. 2006;19:382–402. doi: 10.1128/CMR.19.2.382-402.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hu WS, Chen HW, Zhang RY, Huang CY, Shen CF. The expression levels of outer membrane proteins STM1530 and OmpD, which are influenced by the CpxAR and BaeSR two-component systems, play important roles in the ceftriaxone resistance of Salmonella enterica serovar Typhimurium. Antimicrob. Agents Chemother. 2011;55:3829–37. doi: 10.1128/AAC.00216-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fang CT, Chuang YP, Shun CT, Chang SC, Wang JT. A novel virulence gene in Klebsiella pneumoniae strains causing primary liver abscess and septic metastatic complications. J Exp Med. 2004;199:697–705. doi: 10.1084/jem.20030857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Shemesh M, Kolter R, Losick R. The biocide chlorine dioxide stimulates biofilm formation in Bacillus subtilis by activation of the histidine kinase KinC. J Bacteriol. 2010;192:6352–6. doi: 10.1128/JB.01025-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hennequin C, Forestier C. oxyR, a LysR-type regulator involved in Klebsiella pneumoniae mucosal and abiotic colonization. Infect Immun. 2009;77:5449–57. doi: 10.1128/IAI.00837-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chaba R, Raje M, Chakraborti PK. Evidence that a eukaryotic-type serine/threonine protein kinase from Mycobacterium tuberculosis regulates morphological changes associated with cell division. Eur J Biochem. 2002;269:1078–85. doi: 10.1046/j.1432-1033.2002.02778.x. [DOI] [PubMed] [Google Scholar]
- 29.Clinical and Laboratory Standards Institute. Performance standards for antimicrobial susceptibility testing. CLSI M100-S20U. 2010. Clinical and Laboratory Standards Institute. Wayne, PA.
- 30.Tsai YK, Fung CP, Lin JC, Chen JH, Chang FY, et al. Klebsiella pneumoniae outer membrane porins OmpK35 and OmpK36 play roles in both antimicrobial resistance and virulence. Antimicrob Agents Chemother. 2011;55:1485–93. doi: 10.1128/AAC.01275-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Altschul SF, Madden TL, Schäffer AA, Zhang J, Zhang Z, et al. Gapped BLAST and PSI-BLAST: a new generation of protein database search programs. Nucleic Acids Res. 1997;25:3389–402. doi: 10.1093/nar/25.17.3389. [DOI] [PMC free article] [PubMed] [Google Scholar]