Summary
Granzyme B is a cytotoxic lymphocyte-derived protease that plays a central role in promoting apoptosis of virus-infected target cells, through direct proteolysis and activation of constituents of the cell death machinery. However, previous studies have also implicated granzymes A and B in the production of pro-inflammatory cytokines, via a mechanism that remains undefined. Here we show that IL-1α is a substrate for granzyme B and that proteolysis potently enhanced the biological activity of this cytokine in vitro as well as in vivo. Consistent with this, compared with full-length IL-1α, granzyme B-processed IL-1α exhibited more potent activity as an immunoadjuvant in vivo. Furthermore, proteolysis of IL-1α within the same region, by proteases such as calpain and elastase, was also found to enhance its biological potency. Thus, IL-1α processing by multiple immune-related proteases, including granzyme B, acts as a switch to enhance the pro-inflammatory properties of this cytokine.
Keywords: IL-1α, granzyme B, inflammation, proteolysis, cell death, apoptosis
Introduction
Granzyme (Gzm) B is a protease typically found in the cytotoxic granules of Natural Killer (NK) and cytotoxic T cells (CTLs) and, upon delivery into the cytoplasm of virus-infected target cells, promotes apoptosis to limit virus replication and dissemination (reviewed in Afonina et al., 2010). Gzm B promotes apoptosis through proteolysis of the BH3-only protein Bid, as well as via proteolytic processing and activation of caspase-3 (Afonina et al., 2010). However, accumulating evidence suggests that granzymes A and B may also influence the production of pro-inflammatory cytokines, although the molecular targets of these proteases in inflammatory contexts remain to be defined (Sower et al., 1996a,b; Metkar et al., 2008; Froelich et al., 2009). Interestingly, a number of non-cytotoxic cell types, such as mast cells and basophils, have also been found to secrete Gzm B upon activation (Tschopp et al., 2006; Strik et al., 2007). Furthermore, Gzm B is found at elevated levels in serum from Rheumatoid arthritis (RA) patients and in other inflammatory conditions associated with elevated levels of IL-1 (Lauw et al., 2000; Tak et al., 1999; Kim et al., 2007). For these reasons, we explored whether Gzm B may contribute to the processing and activation of IL-1.
IL-1 is a cytokine with diverse biological activities and is produced in the early stages of infection or sterile injury where it plays an important role in instigating immune responses (Dinarello, 1996; Kono et al., 2010). Although IL-1 is produced in two different forms (IL-1α and IL-1β), encoded by distinct genes, these cytokines bind to the same receptor and share similar biological activities (Dinarello, 1996). Despite their relatedness in structure and biological activity, IL-1α and IL-1β are post-translationally processed in a very different manner. IL-1α is expressed as a ~31 kDa polypeptide and in this form is capable of binding to the IL-1 receptor and is biologically active (Mosley et al., 1987a,b). IL-1β is also expressed as a ~31 kDa polypeptide, but in marked contrast to IL-1α, full length IL-1β is incapable of binding to the IL-1 receptor and consequently, exhibits little biological activity (Mosley et al., 1987a,b; Hazuda et al., 1990). IL-1β acquires biological activity upon limited internal processing by the aspartic acid-specific protease, caspase-1 (Thornberry et al, 1992). Caspase-1-dependent processing of IL-1β at Asp116 unlocks the biological activity of this cytokine. Gzm A has also been found to cleave IL-1β in vitro, however the functional consequences of this event remain unclear (Irmler et al., 1995).
IL-1α is typically released from cells as a result of injury or death and circulating IL-1α levels are persistently elevated in inflammatory conditions such as RA. Although full-length IL-1α displays biological activity, this cytokine is susceptible to proteolysis by certain intracellular proteases. For example, the calcium-activated protease, calpain-1, promotes restricted proteolysis of IL-1α to produce a ~17 kDa protein, although this reportedly has little effect on the biological activity of this cytokine (Kobayashi et al., 1990; Carruth et al., 1991). Therefore, it remains unclear what role calpain-mediated processing of IL-1α serves. As a full-length protein, IL-1α is typically cell-associated, and a portion of this cell-associated form may be present at the plasma membrane (Kurt-Jones et al., 1985). Proteolytic processing of IL-1α may remove a nuclear localization signal or permit shedding of membrane-associated IL-1α and increase the likelihood of secretion (Watanabe and Kobayashi, 1994; Matsuhima et al., 1986). Thus, proteolysis of IL-1α may convert this cytokine from a cell-associated form to a soluble molecule that could exert more systemic effects. An additional possibility is that proteolysis of IL-1α may modulate the biological potency of this cytokine, although this issue has not been explored in any detail.
Here we report that human IL-1α, but not IL-1β, is a substrate for the CTL/NK cell protease, Gzm B, and that processing of this cytokine by the latter protease enhanced its biological activity several-fold. A similar increase in IL-1α activity was also seen upon processing of IL-1α by other proteases, such as calpain-1, elastase and mast cell chymase. Thus, Gzm B and other proteases that are produced during inflammatory responses may promote inflammation, at least in part, through conversion of pro-IL-1α to its mature form.
Results
IL-1α is a substrate for granzyme B
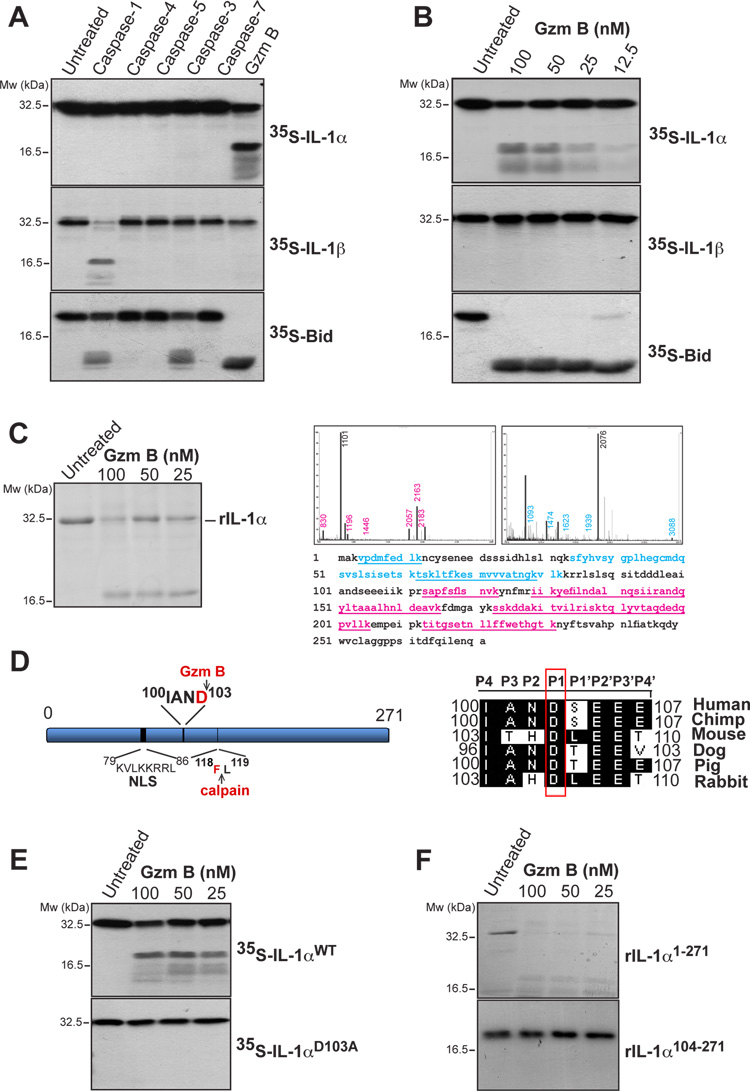
Because recent studies have suggested that CTL/NK granzymes may have extracellular pro-inflammatory roles, we set out to explore whether Gzm B was capable of processing any of the major pro-inflammatory cytokines. To address this issue, we screened a panel of in vitro transcribed and translated members of the interleukin family (IL-1 to IL-17) for susceptibility to proteolysis by Gzm B, as well as a range of other aspartic acid-specific proteases as controls (data not shown). All proteases were confirmed to be active by virtue of their ability to cleave synthetic tetrapeptide substrates (data not shown) or control proteins such as Bid (Figure 1A). The outcome of this screen identified full length IL-1α as a substrate for Gzm B but not for any of the other proteases tested. As Figure 1A shows, whereas caspases-1, -3, -4, -5, and – 7 failed to cleave IL-1α, Gzm B produced a major cleavage product at ~17 kDa. In contrast, Gzm B did not cleave IL-1β, whereas caspase-1 did so, as expected (Figure 1A). To confirm the specificity of IL-1α proteolysis by Gzm B, we titrated this protease over a range of concentrations from 12.5 to 100 nM. IL-1β failed to be cleaved by Gzm B at any of these concentrations, whereas proteolysis of IL-1α, as well as the known Gzm B substrate, Bid, was readily observed (Figure 1B). Importantly, because human and murine GzmB have been shown to have divergent substrate preferences (Cullen et al., 2007), we also tested whether murine IL-1α was a substrate for Gzm B and found that both human and mouse Gzm B cleaved murine IL-1α within the nanomolar range (Figure S1A and S1B).
Figure 1. IL-1α is a substrate for granzyme B.
(A) 35S-labeled IL-1α, IL-1β and Bid were incubated at 37°C for 2 h, either alone, or in the presence of recombinant caspase-1, -4, -5 (20 nM), caspase- 3, -7 or granzyme B (200 nM) followed by analysis by SDS-PAGE/fluorography.
(B) 35S-labeled IL-1α, IL-1β and Bid were incubated for 2 h at 37°C with the indicated concentrations of granzyme B and analysed as in (A).
(C) Recombinant purified full length IL-1α was incubated at 37°C for 2h with the indicated concentrations of granzyme B and analysed by SDS-PAGE with Coomassie staining. IL-1α cleavage fragments were excised from the gel and analysed by MALDI-TOF mass spectrometry. Mass spectra of cleavage fragments are indicated, with coverage of the two cleavage fragments underlined in blue and red, respectively.
(D) Schematic representation of IL-1α indicating nuclear localisation signal and granzyme B and calpain-1 cleavage sites. A sequence alignment of the putative granzyme B cleavage site in IL-1α from a number of mammals is shown to the right. The P1 Asp residue is indicated.
(E) 35S-labeled IL-1αWT and IL-1αD103A mutant were incubated at 37°C for 2h with the indicated concentrations of granzyme B followed by analysis by SDS-PAGE/fluorography.
(F) Recombinant IL-1αFL and IL-1α104-271 were incubated for 2 h at 37°C with the indicated concentrations of granzyme B, then analysed by SDS-PAGE and Coomassie staining. All data shown are representative of at least three independent experiments.
IL-1α is cleaved by granzyme B at Asp103
To map the Gzm B cleavage site within IL-1α, we expressed and purified the full-length cytokine from E. coli and incubated recombinant IL-1α with Gzm B to promote proteolysis. Cleavage products were then analysed by mass spectrometry, which suggested that proteolysis occurred between amino acids 80 and 112 (Figure 1C). Because Gzm B has an almost absolute preference for proteolysis after Asp residues and typically cleaves within IXXD/S motifs, this suggested that IL-1α was cleaved after Asp103, within the motif IAND103, which is conserved among mammals (Figure 1D). To confirm this as the site of proteolysis, we generated a point mutation Asp>Ala103 in IL-1α and tested the susceptibility of this mutant to proteolysis by Gzm B. As Figure 1E shows, this mutant fully resisted proteolysis, as did a deletion mutant of IL-1α lacking the N-terminal 103 amino acids (Figure 1F), confirming that Gzm B cleaves IL-1α at Asp103.
Granzyme B-mediated proteolysis of IL-1α potentiates biological activity
Previous studies have shown that calpain-1 can process IL-1α at Phe118 (Kobayashi et al., 1990), however the significance of this cleavage event for IL-1α bioactivity has not been determined. Indeed, it is widely assumed that proteolytic processing of IL-1α within its N-terminal region has little effect on the biological activity of this cytokine. For these reasons, we wondered whether Gzm B-mediated processing of IL-1α could impact upon its biological activity. To explore this issue, we measured the ability of IL-1α to stimulate production of IL-6 and IL-8 from HeLa cells and primary HUVECs, as both cell types are known to respond to this cytokine (Bertelsen and Sanfridson, 2007; Rhim et al., 2008).
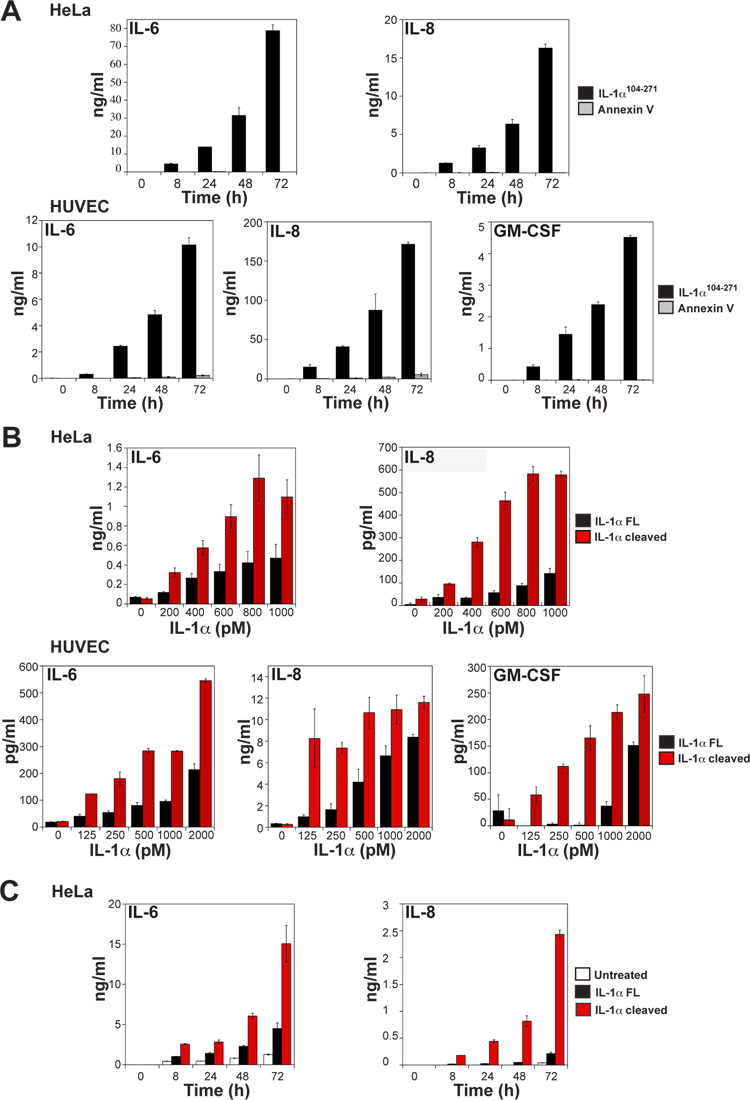
To mimic the Gzm B cleavage product of IL-1α, we generated a truncated form of this cytokine missing the N-terminal 103 amino acids (IL-1α104-271). Using this form of IL-1α we confirmed that both HeLa cells and primary HUVECs were highly responsive to this cytokine (Figure 2A), with both cell types producing IL-6 and IL-8 in response to IL-1α104-271. HUVECs also produced GM-CSF under the same conditions (Figure 2A). These observations confirmed that truncation of IL-1α after Asp103 produced a biologically active cytokine. However, this type of artificial truncation does not necessarily faithfully reproduce the natural cleaved form of full length IL-1α, as proteolysis of a protein does not necessarily disassociate the resulting cleavage products.
Figure 2. Granzyme B-dependent proteolysis of IL-1α enhances cytokine bioactivity.
(A) HeLa (top panels) or HUVEC cells (lower panels) were incubated with 1 nM of recombinant IL-1α104-271 or Annexin V as a control protein. Culture supernatants were collected at the indicated time-points, with IL-6, IL-8 and GM-CSF concentrations then determined by ELISA.
(B) HeLa or HUVEC cells were incubated with the indicated concentrations of full-length or granzyme B-cleaved IL-1α for 8h and concentrations of IL-6, IL-8 and GM-CSF in the supernatants were determined by ELISA.
(C) HeLa cells were left untreated or incubated with 2 nM of full-length or granzyme B-cleaved IL-1α. Culture supernatants were collected at the indicated time-points, with IL-6 and IL-8 concentrations subsequently determined by ELISA. All results are representative of at least three independent experiments. Error bars represent the mean ± the SEM of triplicate experiments.
To compare the effects of Gzm B-mediated proteolysis of IL-1α with the full-length cytokine, we incubated bacterially expressed IL-1α precursor in the presence or absence of Gzm B, followed by assessment of biological activity as above. Surprisingly, proteolytic processing of IL-1α by Gzm B increased the activity of this cytokine several-fold (Figure 2B). Similar observations were also made in time course experiments, once again indicating that Gzm B-mediated proteolysis dramatically increased the bioactivity of IL-1α (Figure 2C).
Importantly, we ruled out the possibility that co-purifying microbial contaminants in the Gzm B preparations contributed to the effects seen. First, we expressed and purified a catalytically inactive Gzm B mutant (Gzm BSA) in the same yeast system that was used to generate wild type Gzm B (Figure S2A-C). This mutant failed to cleave IL-1α and also failed to enhance the activity of IL-1α on HeLa or HUVECs (Figure S2C and S2D). Second, neither wild type nor mutant forms of Gzm B induced cytokines when added directly to HeLa cells in the absence of IL-1α (Figure S2E). Third, whereas HeLa cells are very responsive to IL-1α, these cells fail to produce IL-6 or IL-8 in response to a wide panel of microbial components (i.e. pathogen-associated molecular patterns) such as lipopolysaccharide that would represent possible contaminants (Figure S2F).
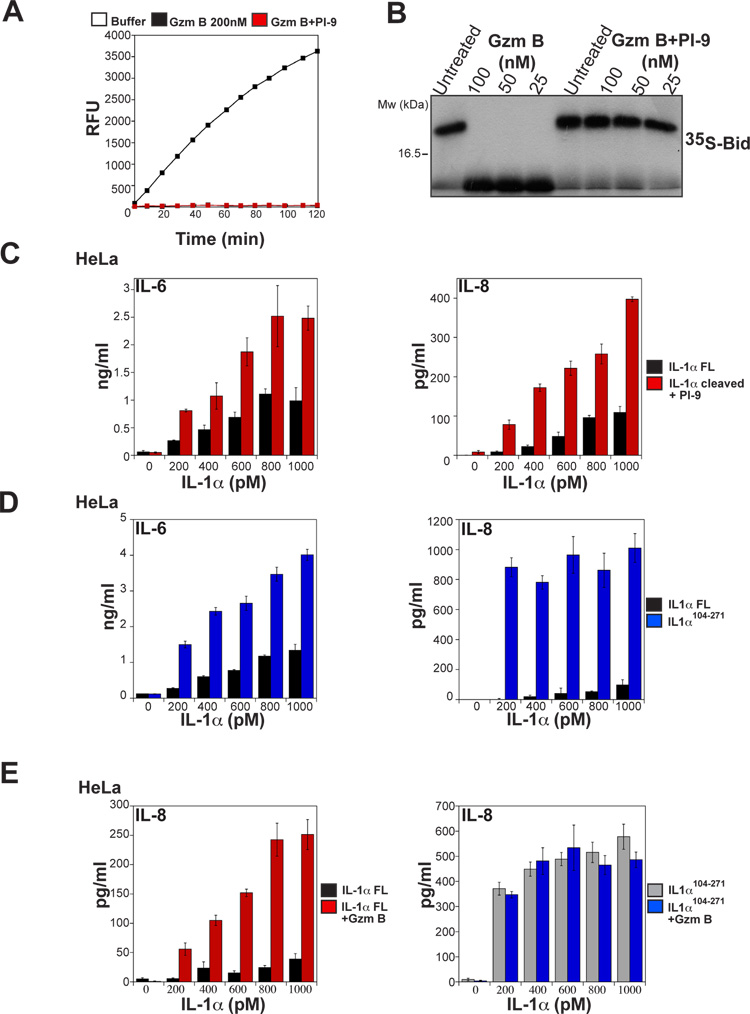
Granzyme B does not directly influence inflammatory cytokine production by HeLa or HUVECs
To further rule out the possibility that residual Gzm B activity within the cleaved IL-1α preparations was responsible for the increased pro-inflammatory effects seen, we neutralized this granzyme with the serpin protease inhibitor PI-9, confirming that no residual protease activity remained after the incubation period with IL-1α (Figure 3A and B). Addition of PI-9 after Gzm B-mediated proteolysis of IL-1α had no effect on the increased potency of the Gzm B-treated IL-1α preparations (Figure 3C), demonstrating that Gzm B was not directly acting upon the cells used to assay IL-1α activity. Similar observations were also made with HUVECs (data not shown).
Figure 3. Granzyme B activity does not directly promote inflammatory cytokine production.
(A) Recombinant IL-1α was incubated with granzyme B (200 nM) for 3 h at 37°C. Residual granzyme B activity was then measured after further incubation for 30 min either alone, or in the presence of the granzyme B inhibitor PI-9 (1 mM). Granzyme B activity was measured by monitoring hydrolysis of the synthetic granzyme B substrate IETD-AFC by fluorimetry.
(B) 35S-labeled Bid was incubated, either alone, or with the indicated concentrations of active or PI-9-treated granzyme B for 2 h at 37°C. Reactions were analysed by SDS-PAGE followed by fluorography.
(C) HeLa cells were incubated for 8 h with the indicated concentrations of full-length or granzyme B-cleaved IL-1α, where residual granzyme B activity after proteolysis of IL-1α was inhibited by addition of saturating amounts of PI-9. IL-6 and IL-8 levels in culture supernatants were determined by ELISA.
(D) HeLa cells were incubated for 8 h with the indicated concentrations of IL-1αFL or IL-1α104-271. IL-6 and IL-8 levels were determined by ELISA.
(E) HeLa cells were incubated for 8 h with the indicated concentrations of IL-1αFL, granzyme B-treated IL-1αFL, IL-1α104-271, or granzyme B-treated IL-1α104-271, as indicated. IL-6 and IL-8 levels were determined by ELISA.
Results are representative of at least three independent experiments. Error bars represent the mean ±SEM of determinations from three independent experiments.
We also directly compared the potency of full length IL-1α with the artificially-truncated IL-1α104-271 protein (which mimics the Gzm B-cleaved form of this cytokine) and once again observed considerable differences in activity between these forms of IL-1α (Figure 3D). Furthermore, incubation of truncated IL-1α104-271 with Gzm B did not have any effect on the activity of this cytokine, as expected (Figure 3E). Similarly, incubation of the Gzm B-non-cleavable form of IL-1α (IL-1αD103A) with this granzyme, also failed to enhance the activity of this protein (data not shown). Collectively, these data provide strong evidence that proteolysis of IL-1α by Gzm B enhances the biological activity of this protein up to 10-fold.
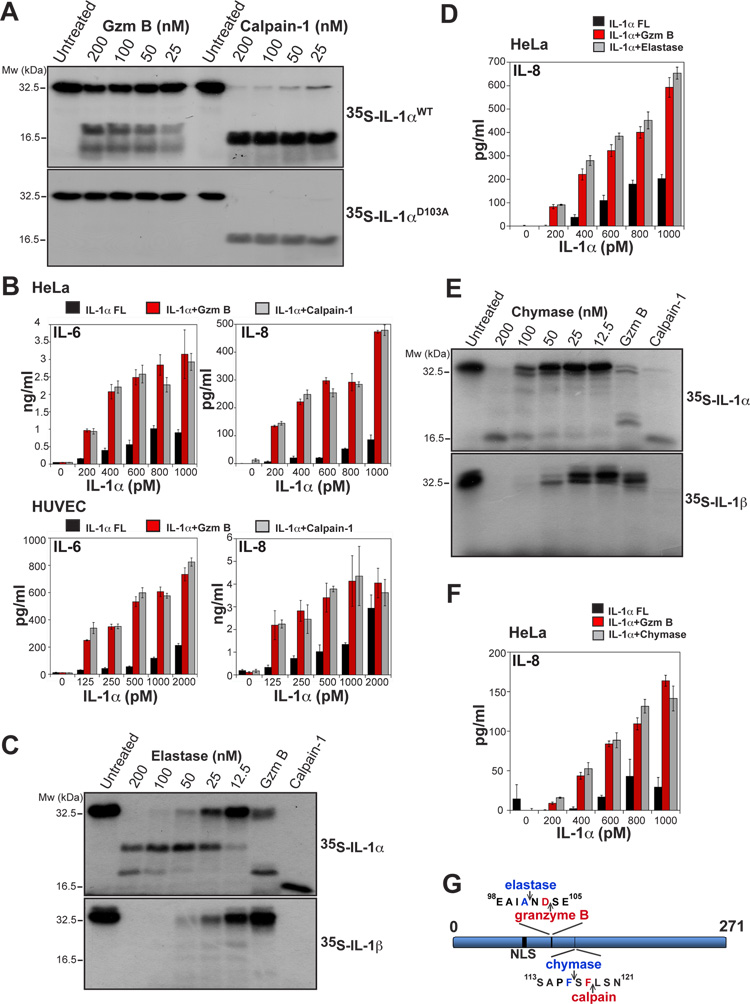
Proteolysis of IL-1α by calpain, as well as other proteases, enhances the bioactivity of this cytokine
As mentioned earlier, calpain-1 has been shown to cleave IL-1α at Phe118 (Kobayashi et al., 1990), close to the Gzm B cleavage site at Asp103 (Figure 1D). Therefore, we wondered whether calpain-mediated proteolysis of IL-1α also enhanced the activity of this cytokine, as previous studies have failed to address this issue. We first compared the relative efficiency of IL-1α processing by calpain-1 versus Gzm B. As Figure 4A illustrates, calpain cleaved IL-1α very efficiently at nanomolar concentrations, producing a cleavage pattern distinct from that of Gzm B. Furthermore, calpain-1 also cleaved the Gzm B-resistant IL-1αD103A mutant (Figure 4A), confirming that proteolysis by these proteases occurs at different sites within IL-1α.
Figure 4. Proteolysis of IL-1α by calpain and other proteases also enhances cytokine bioactivity.
(A) 35S-labeled IL-1αWT and IL-1αD103A were incubated for 2 h at 37°C with the indicated concentrations of granzyme B or calpain-1. Reactions were analysed by SDS-PAGE/fluorography.
(B) HeLa or HUVEC cells were incubated with the indicated concentrations of full-length IL-1α, or granzyme B- or calpain-1-cleaved IL-1α for 8 h. IL-6 and IL-8 levels were determined by ELISA.
(C) 35S-labeled in vitro transcribed/translated IL-1α and IL-1β were incubated for 2 h at 37°C with the indicated concentrations of elastase, or with granzyme B or calpain -1 (both at 200 nM) as controls. Reactions were then analysed as in (A).
(D) HeLa cells were incubated for 8 h with the indicated concentrations of full-length IL-1α, or IL-1α cleaved with either granzyme B, or elastase, as indicated. IL-6 and IL-8 levels were then determined by ELISA.
(E) 35S-labeled in vitro transcribed/translated IL-1α and IL-1β were incubated for 2 h at 37°C with the indicated concentrations of mast cell chymase, or with granzyme B or calpain-1 (both at 200 nM) as controls. Reactions were then analysed as in (A).
(F) HeLa cells were incubated for 8 h with the indicated concentrations of full-length IL-1α, or IL-1α cleaved with either granzyme B, or chymase, as indicated. IL-6 and IL-8 levels were then determined by ELISA.
All results are representative of at least three independent experiments. Error bars represent the mean ±SEM of determinations from three experiments.
(G) Schematic of IL-1α indicating sites of granzyme B- and calpain-mediated proteolysis and predicted sites of chymase- and elastase-mediated proteolysis.
We then explored the effects of calpain-1-mediated proteolysis on IL-1α activity using the HeLa and HUVEC assays as before. As Figure 4B illustrates, similar to our earlier observations with Gzm B, proteolysis of IL-1α by calpain-1 also enhanced the potency of this cytokine to a similar degree. Thus, proteolysis of IL-1α, by either Gzm B or calpain, greatly enhanced the biological activity of IL-1α, which suggests that restricted proteolysis of IL-1α within its N-terminus has a role in regulating the potency of this cytokine.
Elastase and mast cell chymase have been previously implicated as IL-1β-processing proteases (Black et al., 1988; Hazuda et al., 1990; Mizutani et al., 1991), but it is unclear whether IL-1α is also processed by these enzymes. Therefore, we explored the effects of elastase and mast cell chymase on IL-1α and found that both proteases did indeed cleave this cytokine, albeit producing different processing patterns (Figure 4C and E). Elastase generated an IL-1α cleavage product very similar in mobility to the Gzm B cleavage product of IL-1α (Figure 4C), consistent with proteolysis at a candidate site at Ala101 (Figure 4G). Mast cell chymase produced an IL-1α cleavage product running at an almost identical mobility to the product produced by calpain cleavage (Figure 4E), consistent with cleavage at a candidate site at Phe116 (Figure 4G). In agreement with this, both enzymes also enhanced the potency of IL-1α to an extent almost identical to Gzm B (Figure 4D and F). Thus, proteolysis of IL-1α within its N-terminus, which can be effected by multiple pro-inflammatory proteases, acts in a switch-like manner to potentiate the biological activity of this cytokine.
Intracellular and extracellular proteolysis of IL-1α during NK-mediated killing
Several non-cytotoxic cell types, such as plasmacytoid dendritic cells, mast cells, keratinocytes and basophils have been reported to express Gzm B, but not perforin, upon activation (Strik et al., 2007; Hernandez-Pigeon et al., 2007; Tschopp et al., 2006). This is puzzling, as gene knockout studies have shown that perforin is essential for the cytotoxic effects of granzymes (Kagi et al., 1994; Lowin et al., 1994). However, other studies have suggested that granzymes may have extracellular roles as pro-inflammatory molecules unrelated to their role in cell killing (Sower et al., 1996a,b; Metkar et al., 2008). Furthermore, several studies have also reported that Gzm B-expressing cells can actively secrete this protease into the extracellular space (Spaeny-Dekking et al., 1998; Prakash et al., 2009). This suggests that Gzm B might have extracellular functions, independent of its role as a pro-apoptotic protease, in certain settings.
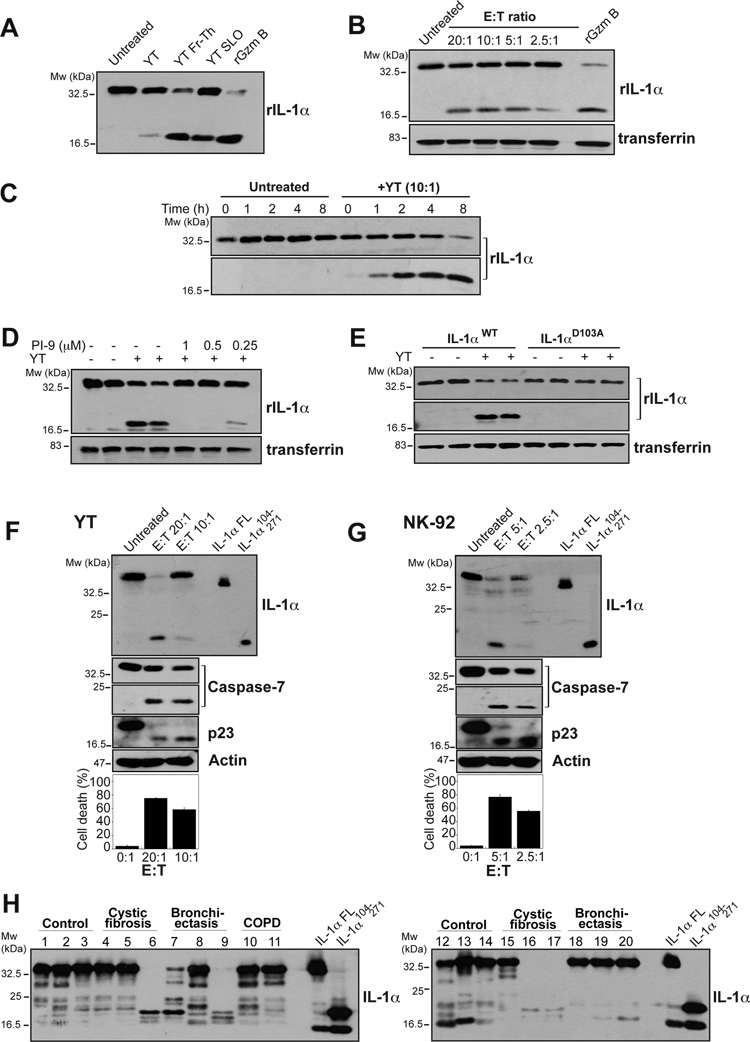
To explore this possibility, we investigated IL-1α processing as a consequence of Gzm B secretion into the extracellular space. First, we actively permeabilized the NK cell line, YT, using the pore-forming protein, streptolysin O, or through freeze thaw-induced cell lysis to promote granzyme release. This NK line does not express all of the granzymes but does express Gzm B, Gzm H and Gzm M in addition to perforin (Sedelies et al., 2004). As Figure 5A shows, active permeabilization of YT cells resulted in robust IL-1α proteolysis, with the resulting cleavage fragment running at an identical mobility to that produced through proteolysis of IL-1α by recombinant Gzm B. YT cells were also incubated in the presence or absence of HeLa target cells to induce secretion of granzymes, followed by assessment of the ability of culture supernatants derived from these assays to cleave full length IL-1α. As Figure 5B shows, proteolysis of IL-1α was readily detected using supernatants derived from NK cells over a range of effector to target cell ratios. A time course analysis revealed that proteolysis was already detectable within 1h of incubation of IL-1α with YT cell supernatants, whereas incubation with HeLa cell supernatants alone failed to cleave this cytokine (Figure 5C). Because it was formally possible that proteases other than Gzm B, released from YT cells, might be responsible for the proteolysis seen, we also explored whether the Gzm B-specific inhibitory serpin, PI-9, could inhibit IL-1α proteolysis within YT-derived cell supernatants. These experiments confirmed that proteolysis of IL-1α in the extracellular space was Gzm B-dependent as this could be completely inhibited through addition of PI-9 to the reactions (Figure 5D). Furthermore, the Gzm B non-cleavable IL-1αD103A point mutant was completely resistant to proteolysis by YT-derived cell supernatants, further confirming that the proteolysis seen was Gzm B-dependent (Figure 5E).
Figure 5. IL-1α is cleaved, either extracellularly or intracellularly, by endogenous granzyme B.
(A) YT cells were either left untreated or were permeabilized via 2 cycles of freeze-thaw (Fr-Th), or addition of 10 μg/ml of streptolysin O (SLO) for 90 min. Recombinant IL-1α was added to the supernatants which were further incubated for 2 h at 37°C and analysed for IL-1α processing by immunoblotting.
(B) YT cells were incubated for 18 h with HeLa target cells at the indicated effector:target ratios in the presence of recombinant IL-1α. Culture supernatants were analysed by immunoblot for IL-1α processing. Serum-derived transferrin served as a loading control.
(C) HeLa cells were incubated with recombinant extracellular IL-1α for the indicated times, in the presence or absence of YT cells, as indicated. Supernatants were then analysed for IL-1α processing by immunoblot.
(D) YT cells were incubated for 6 h with HeLa target cells at an E:T ratio of 10:1 in the presence of recombinant IL-1α and PI-9, as indicated. Supernatants were then analysed for IL-1α processing by immunoblot. Serum-derived transferrin served as a loading control.
(E) YT cells were incubated for 6 h with HeLa target cells at an E:T ratio of 10:1 in the presence of either recombinant IL-1αWT or IL-1αD103A mutant, as indicated. Supernatants were then analysed for IL-1α processing by immunoblot. Serum-derived transferrin served as a loading control.
(F, G) HeLa cells were transfected with IL-1α expression plasmid. 24h later cells were exposed to YT cells (F) or NK-92 cells (G) cells at an E:T ratio of 20:1 or 5:1, respectively. NK cells were removed 3-5 h later and HeLa cells were further incubated for the total of 24 h, after which cell lysates were generated and immunoblotted for the indicated proteins. Cell death was assessed by annexin V/propidium iodide binding, measured by flow cytometry. All data shown are representative of at least three independent experiments.
(H) Recombinant purified full length IL-1α was incubated at 37°C for 20 min with 10 μl of BALF samples from control patients or patients with cystic fibrosis, bronchiectasis or chronic obstructive pulmonary disease (COPD). IL-1α processing was analysed by immunoblot. As controls, full-length IL-1α and IL-1α104-271 were expressed in HEK293T cells and were included to facilitate size comparison of cleavage products.
We also explored the ability of YT cells to cleave cell-associated IL-1α during NK killing. As Figure 5F shows, intracellular IL-1α was also cleaved efficiently during target cell apoptosis. Similar results were also found using a different NK cell line, NK-92, as effectors in similar cell killing assays (Figure 5G). Collectively, these data demonstrate that endogenous Gzm B is capable of cleaving IL-1α, either intracellularly during NK-mediated killing, or as a consequence of release of both proteins into the extracellular space.
IL-1α cleaving activity in inflammatory patients
To explore whether IL-1α also underwent processing during inflammation, we obtained bronchoalveolar lavage fluids (BALF) from patients with persistent inflammatory lung conditions (cystic fibrosis, chronic obstructive pulmonary disease, bronchiectasis) as well as healthy donors. Previous studies have shown that such fluids contain high levels of inflammatory proteases, particularly elastase, due to invasion of the lungs by neutrophils and other cells of the innate immune system (McElvaney et al., 1991; Reeves et al., 2010). As Figure 5H illustrates, IL-1α underwent rapid proteolysis to fragments very similar to the Gzm B/elastase/calpain-cleaved forms of this cytokine in BALF from several cystic fibrosis and bronchiectasis patients, whereas little processing was seen in controls. Thus, proteases capable of processing IL-1α to its mature form are secreted into the extracellular space under inflammatory conditions in vivo.
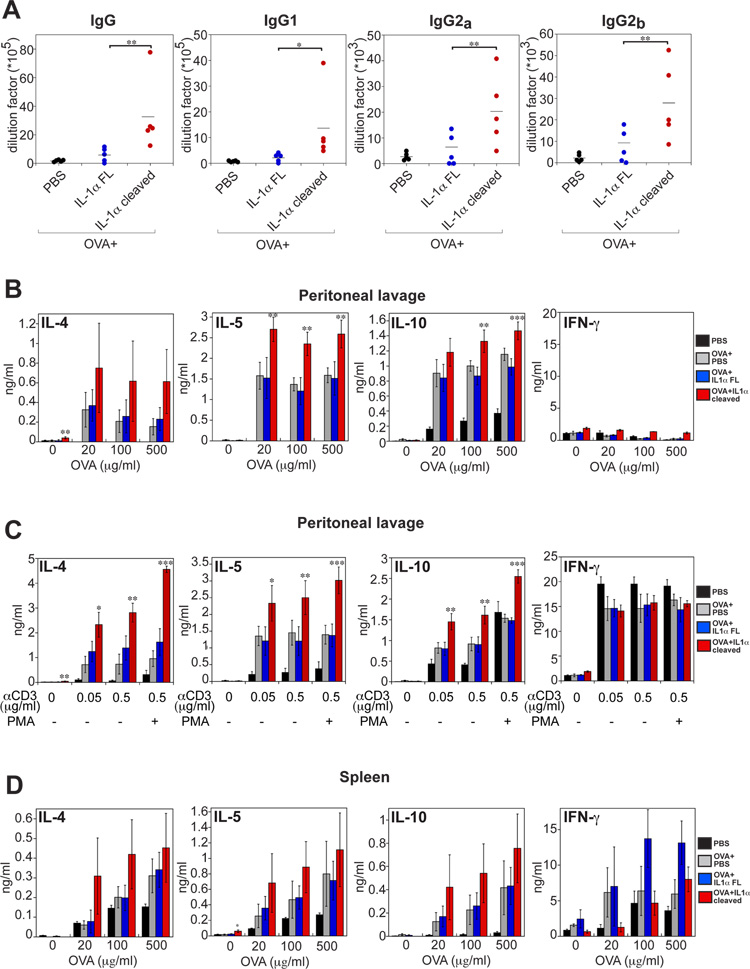
Granzyme B-cleaved IL-1α exhibits enhanced activity in vivo
We next explored whether the Gzm B-cleaved form of IL-1α also exhibited greater bioactivity in vivo. To address this question, we compared the adjuvant activity of full-length versus Gzm B-cleaved IL-1α in an antigen-driven model, using ovalbumin (OVA). Balb/c mice were immunized with OVA, either alone, or in combination with full-length or Gzm B-cleaved IL-1α, followed by boosting with the same combinations two weeks later. One week after boosting, OVA-specific antibodies were measured in the serum as well as OVA-specific T-cell responses in the peritoneal lavage and spleens of these mice. As Figure 6A and Figure S3 shows, both forms of IL-1α significantly boosted antibody responses to OVA, with the cleaved form of this cytokine exhibiting considerably greater potency in this regard. Furthermore, OVA-specific IL-4, IL-5, and IL-10 production from peritoneal lavage cell preparations was also significantly greater in mice that received the Gzm B-cleaved form of IL-1α (Figure 6B). Polyclonal stimulation with anti-CD3 also produced more robust cytokine responses from mice that had received cleaved IL-1α (Figure 6C). A similar trend towards more robust OVA-specific responses was also observed in splenocytes from the same mice, but this was less statistically significant than in peritoneal exudates (Figure 6D). Collectively, these data lend further support to our in vitro observations that Gzm B-dependent proteolysis of IL-1α acts to enhance the pro-inflammatory effects of this cytokine.
Figure 6. Granzyme B-cleaved IL-1α exhibits enhanced activity in vivo.
Balb/c mice (5 mice per group) were immunized either with ovalbumin (OVA) alone (200 μg), OVA in combination with full-length IL-1α (5 μg per mouse), or OVA in combination with granzyme B-cleaved IL-1α (5 μg per mouse). All mice were boosted with the same combinations on day 14. Peripheral blood, spleens and peritoneal lavages were collected on day 21.
(A) OVA-specific total IgG, IgG1, IgG2a and IgG2b in plasma samples were determined by ELISA. (B-D) Cells from peritoneal lavages (B, C) and spleens (D) were re-stimulated for 3 days with indicated concentrations of OVA, anti-CD3, or anti-CD3/PMA, as indicated. IL-4, IL-5, IL-10 and IFN-γ production was determined by ELISA.
All measurements were taken in triplicate. Error bars represent the mean ± SEM from each group of five mice. Significance levels, ***= p<.001, **= p<.05, *= p<.01, by students t-test.
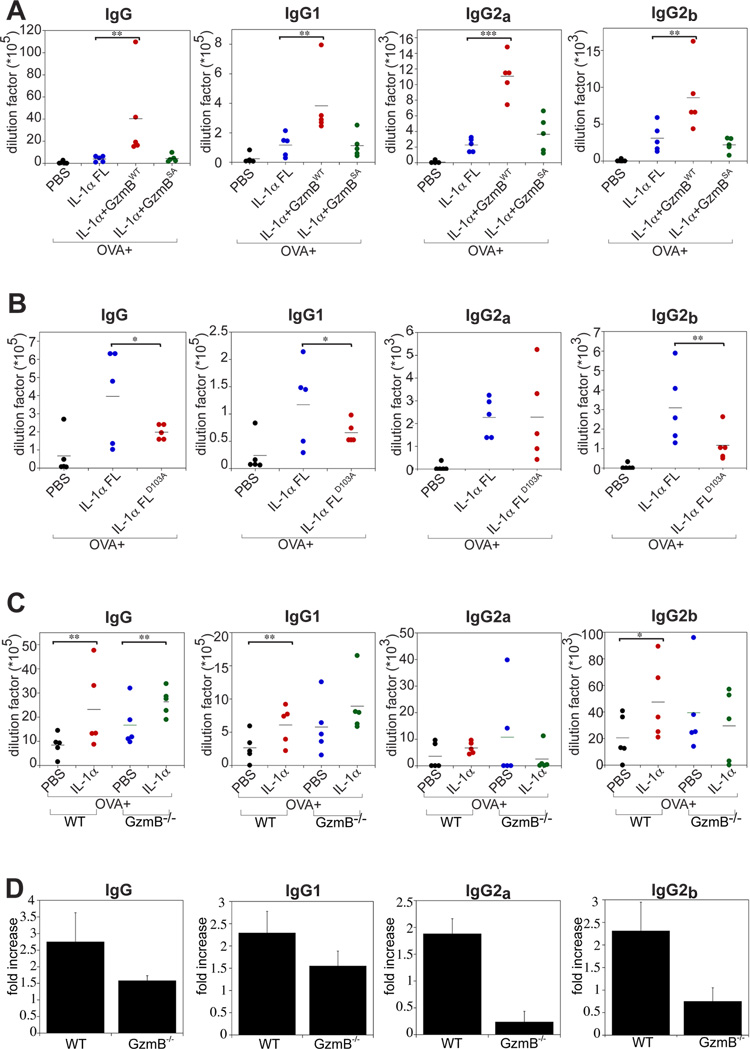
To again rule out the possibility that a contaminant within the Gzm B preparations could contribute to the enhanced IL-1α activity seen in vivo, we used the catalytically inactive mutant form of this protease (Gzm BSA; Figure S2A-C), to explore whether this mutant could enhance IL-1α activity in vivo. As Figure 7A shows, pre-incubation with Gzm BSA failed to potentiate IL-1α activity under conditions where incubation with wild type Gzm B clearly did so.
Figure 7. Granzyme B contributes to IL-1α processing in vivo.
(A and B) Balb/c mice (5 animals per group) were immunized either with ovalbumin (OVA) alone (200 μg), or OVA in combination with the full-length IL-1α, Gzm BWT-treated IL-1α, Gzm BSA-treated IL-1α, or non-cleavable mutant IL-1αD103A (5 μg per mouse). On day 21, peripheral bloods were collected and OVA-specific total IgG, IgG1, IgG2a and IgG2b antibodies in plasma samples were determined by ELISA.
(C) WT or Granzyme B-/- C57BL/6 mice (5 per group) were immunized either with OVA alone (200 μg), or with OVA in combination with full-length IL-1α (5 μg per mouse). On day 21, peripheral bloods were collected and OVA-specific total IgG, IgG1, IgG2a and IgG2b in plasma samples were determined by ELISA.
(D) Fold increase in antibody production in WT versus Granzyme B-/- mice treated with OVA plus IL-1α, compared with OVA alone. The analysis shown is based on the data presented in (C). Error bars represent the mean ± SEM from each group of five mice.
Significance levels, ***= p<.001, **= p<.05, *= p<.01, by students t-test.
We also asked whether the IL-1α mutant (D103A) incapable of undergoing processing by Gzm B (Figure 1E) possessed reduced activity in vivo, when compared to wild type IL-1α. As Figure 7B illustrates, IL-1α-dependent enhancement of OVA-specific antibody responses were consistently less pronounced with IL-1αD103A than with wild type IL-1α, suggesting that endogenous Gzm B contributes to the potency of IL-1α in vivo.
Finally, we also explored IL-1α-dependent enhancement of OVA-specific antibody responses in wild type versus gzmB-/- mice. Although it is important to note that several proteases can process IL-1α to a more active form, as we have shown here, we were nonetheless interested to explore whether the absence of Gzm B had a significant impact on IL-1α activity in vivo. As Figure 7C and 7D show, we found that IL-1α-dependent enhancement of OVA-specific antibodies was greater in wild type animals than that seen in gzmB-/- mice. Note however that baseline antibody responses to OVA alone were higher in gzmB-/- animals for reasons that are unclear. Nonetheless, the enhancement effect of IL-1α on OVA-specific responses was significantly higher in wild type animals than in knockouts, again suggesting that endogenous Gzm B contributes to IL-1α processing in vivo.
Collectively, these data reveal a hitherto unappreciated consequence of IL-1α processing to the mature ~17 kDa cytokine. The N-terminal IL-1α pro-peptide appears to function as a sensor for multiple pro-inflammatory proteases, proteolysis of which switches the activity of this cytokine from a basal to a hyperactive state.
DISCUSSION
Here we report that IL-1α is a substrate for the CTL/NK protease Gzm B and that proteolysis of this cytokine by the latter protease very significantly increased its biological potency. These data suggest that Gzm B may enhance inflammatory responses in certain situations through proteolytic processing of IL-1α. We have further shown that proteolysis of IL-1α by calpain-1, elastase and mast cell chymase, at sites close to but distinct from the Gzm B processing site, also potentiated the activity of this cytokine. This suggests that proteolysis of IL-1α within its N-terminus, irrespective of the protease involved, acts as a switch to increase the biological potency of this cytokine. Thus, contrary to current thinking, limited proteolysis of IL-1α increases biological activity and serves as a further level of regulation on this cytokine.
Proteolysis of IL-1α may induce a conformational change in this protein that increases its affinity for the IL-1 receptor complex, thereby increasing biological potency. Alternatively, the IL-1α N-terminus may partly occlude the receptor binding domain, removal of which now permits a more stable interaction with the IL-1R complex. This possibility is consistent with a previous study that utilized sensitivity to proteinase K-mediated proteolysis to explore whether IL-1α underwent a conformational change as a consequence of removal of its N-terminus (Hazuda et al., 1991). Although the latter study did not explore the functional effects of IL-1α proteolysis in any detail, it did suggest that proteolysis of this cytokine initiated a profound conformational change in the molecule from a proteinase K-sensitive to a proteinase K-insensitive state (Hazuda et al., 1991). This change is most likely reflected in an altered conformation that has increased IL-1 receptor affinity.
There are a number of scenarios where Gzm B may encounter IL-1α. First, in a classical CTL/NK killing reaction, where the target cell expresses IL-1α, this cytokine may become processed within the target cell and exacerbate pro-inflammatory responses if released from dying cells prior to clearance of the latter by phagocytes. In this context, it is relevant to note that Bid was substantially more sensitive to Gzm B-mediated proteolysis than IL-1α. Thus, although the concentration of Gzm B achieved in a CTL/NK killing reaction is unknown, at low nanomolar concentrations of Gzm B robust proteolysis of Bid and apoptosis might occur without significant proteolysis of IL-1α, with proteolysis of the latter becoming more significant upon exposure to higher granzyme concentrations.
Second, there are now a number of studies suggesting that NK cells and CTLs, as well as other cell types, may actively secrete granzymes into the extracellular space (Spaeny-Dekking et al., 1998; Prakash et al., 2009). In this scenario, where injury or infection has resulted in necrosis and release of IL-1α, Gzm B released from CTL/NK cells—or indeed one of the growing number of non-cytotoxic cell types that have been found to express this granzyme—could process this cytokine and enhance its potency. In this context it is noteworthy to mention that several studies have detected circulating Gzm B at elevated levels in rheumatoid arthritis patients and in patients with melioidosis (Spaeny-Dekking et al., 1998; Tak et al., 1999; Lauw et al., 2000). Furthermore, Gzm B expression and secretion has been repeatedly detected in non-cytotoxic, pro-inflammatory immune cells such as macrophages, plasmacytoid dendritic cells, activated mast cells, basophils, B lymphocytes, macrophages, keratinocytes, platelets, human articular chondrocytes, and breast carcinoma cells (reviewed in Afonina et al., 2010), further suggesting that this granzyme may have alternative, non-cytotoxic functions. Proteases such as elastase and mast cell chymase are abundantly released via degranulation of neutrophils and mast cells during inflammatory reactions, providing a ready means by which these proteases may encounter IL-1α released through cell damage. Indeed, several recent studies have shown that IL-1α is a major initiator of inflammatory responses to necrotic cells (Chen et al., 2007; Kono and Rock, 2008; Kono et al., 2010).
A recent study found that whereas IL-1α was readily released from cells undergoing necrosis, this cytokine was retained within the nucleus of cells undergoing apoptosis (Cohen et al., 2010). Retention of IL-1α within the nucleus appears to be facilitated by a nuclear localization signal within its N-terminus, the region that is separated from the molecule through Gzm B-dependent proteolysis. Thus, in addition to increasing biological potency through enhancing IL-1α binding to its receptor, proteolysis of IL-1α by proteases such as Gzm B may also facilitate its release by overriding the nuclear retention mechanisms that appear to operate during some forms of cell death.
In summary, in addition to acting as a direct instigator of cell death upon delivery into target cells, Gzm B may also serve in a hitherto unsuspected capacity as an amplifier of inflammatory responses through restricted proteolysis of IL-1α. We have also shown that proteolysis of IL-1α by several other proteases, each of which cleave this cytokine at distinct sites within its N-terminus, enhanced the biological potency of this cytokine. IL-1α processing to the mature ~ 17 kDa protein acts as a switch to enhance the pro-inflammatory properties of this cytokine, from a basal level of activity to a hyperactive one. Thus, in common with IL-1β, the biological activity of IL-1α is also regulated through restricted proteolysis.
MATERIALS AND METHODS
Reagents
Recombinant caspase-1, -3, -4, -5, -7 were expressed and purified from bacteria as described previously (Luthi et al., 2009). Recombinant poly-histidine-tagged human PI-9 was expressed and purified from bacteria according to standard procedures. Recombinant wild type Gzm B (both human and murine) and the catalytically inactive mutant, Gzm BSA, were expressed and purified from Pichia pastoris yeast as described previously (Cullen et al., 2007). cDNA clones encoding full-length human and murine IL-1α were obtained from Origene and subcloned into pET45b. Recombinant IL-1α and derivatives were expressed in E. coli and purified as described in supplemental experimental procedures. Human calpain-1 and human mast cell chymase were purchased from Calbiochem, human elastase was purchased from Serva. Polyclonal anti-IL-1α antibody was from AbD Serotec, goat anti-rabbit HRPO secondary antibody was from Jackson ImmunoResearch. Ac-IETD-AFC was purchased from Bachem (UK). Lipopolysaccharides (LPS), Mannan, Lipoteichoic acid (LTA), Muramyl dipeptide (MDP) were purchased from Sigma (Ireland) Ltd., Pam3CSK4, Flagellin, CpG were purchased from Invivogen (France). Unless otherwise stated, all other reagents were purchased from Sigma (Ireland) Ltd.
Cell culture
HeLa cells were cultured in RPMI media, supplemented with 5% fetal calf serum, YT cells in RPMI supplemented with 10% serum and HUVEC (PromoCell, Germany) in endothelial cell growth media with added growth supplement (PromoCell, Germany). Cells were cultured at 37°C in humidified atmosphere with 5% CO2.
Cell-killing assays
HeLa cells were transiently transfected with IL-1α expression plasmid using GeneJuice transfection reagent (Merck, Ireland). For NK-mediated killing, HeLa cells were incubated with YT or NK-92 cells at 20:1 and 10:1 effector to target ratios, respectively. NK cells were removed from the target cell monolayer after 3-5 h and HeLa cells were further incubated for total of 24 h. Cell lysates were generated at 2 × 107 cells/ml and analysed by western blotting.
Animals
Balb/c mice were purchased from Harlan (UK). Animal experiments were in accordance with the regulations of the Trinity College Dublin ethics committee and the Irish Department of Health. Granzyme B null mice, on the C57BL/6 background, were bred at Academic Medical Center (AMC), Amsterdam, The Netherlands.
Determination of cytokine and antibody concentrations
Cytokines were determined by ELISA as described previously (Luthi et al., 2009). Paired antibodies for mouse IL-4, IL-5, IL-10 and IFN-γ were purchased from BD PharMingen (UK), human IL-6, IL-8 and GM-CSF DuoSets were purchased from R&D Systems (UK). Serum immunoglobulin titres were determined as described previously (Lavelle et al., 2001).
IL-1α bioactivity assay
HeLa cells were plated at a density of 4 × 104 cells per well and primary HUVECs were plated at 2 × 104 cells per well on 24-well plates. 24 h later cells were incubated with the indicated concentrations of recombinant IL-1α, or recombinant annexin V (as a control protein), and culture supernatants were collected at the specified time-points for quantitative cytokine analysis by ELISA.
Bronchoalveolar lavage fluid analysis
Bronchoalveolar lavage fluid samples from control individuals or patients with cystic fibrosis (CF), chronic obstructive pulmonary disease (COPD) or bronchiectasis were collected as described previously (Reeves et al., 2010). Informed patient consent was obtained and ethical approval was granted by the Beaumont Hospital Institutional Review Board.
Supplementary Material
Acknowledgements
Work in the Martin laboratory is supported by SRC and PI grants from Science Foundation Ireland (07/SRC/B1144 and 08/IN.1/B2031) and The Wellcome Trust UK (082749). The Lavelle laboratory is supported by Science Foundation Ireland grant 07/SRC/B1144. I.S.A. was a Health Research Board of Ireland scholar. S.J.M is a Science Foundation Ireland Principal Investigator.
Footnotes
The authors have no conflicting financial interests to declare.
References
- Afonina I, Cullen SP, Martin SJ. Cytotoxic and non cytotoxic roles of the CTL/NK proteases granzyme B. Immunological Reviews. 2010;235:105–116. doi: 10.1111/j.0105-2896.2010.00908.x. [DOI] [PubMed] [Google Scholar]
- Bertelsen M, Sanfridson A. TAB1 modulates IL-1alpha mediated cytokine secretion but is dispensable for TAK1 activation. Cell Signal. 2007;19:646–57. doi: 10.1016/j.cellsig.2006.08.017. [DOI] [PubMed] [Google Scholar]
- Black RA, Kronheim SR, Cantrell M, Deeley MC, March CJ, Prickett KS, Wignall J, Conlon PJ, Cosman D, Hopp TP, et al. Generation of biologically active interleukin-1 beta by proteolytic cleavage of the inactive precursor. J. Biol. Chem. 1988;263:9437–42. [PubMed] [Google Scholar]
- Carruth LM, Demczuk S, Mizel SB. Involvement of a calpain-like protease in the processing of the murine interleukin 1 alpha precursor. J. Biol. Chem. 1991;266:12162–7. [PubMed] [Google Scholar]
- Chen CJ, Kono H, Golenbock D, Reed G, Akira S, Rock KL. Identification of a key pathway required for the sterile inflammatory response triggered by dying cells. Nat Med. 2007;13:851–6. doi: 10.1038/nm1603. [DOI] [PubMed] [Google Scholar]
- Choy JC, McDonald PC, Suarez AC, Hung VH, Wilson JE, McManus BM, Granville DJ. Granzyme B in atherosclerosis and transplant vascular disease: association with cell death and atherosclerotic disease severity. Mod Pathol. 2003;16:460–70. doi: 10.1097/01.MP.0000067424.12280.BC. [DOI] [PubMed] [Google Scholar]
- Cohen I, Rider P, Carmi Y, Braiman A, Dotan S, White MR, Voronov E, Martin MU, Dinarello CA, Apte RN. Differential release of chromatin-bound IL-1alpha discriminates between necrotic and apoptotic cell death by the ability to induce sterile inflammation. Proc Natl Acad Sci U S A. 2010;107:2574–9. doi: 10.1073/pnas.0915018107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conlon PJ, Grabstein KH, Alpert A, Prickett KS, Hopp TP, Gillis S. Localization of human mononuclear cell interleukin 1. J. Immunol. 1987;139:98–102. [PubMed] [Google Scholar]
- Cullen SP, Adrain C, Luthi AU, Duriez PJ, Martin SJ. Human and Murine Granzyme B Exhibit Divergent Substrate Preferences. The Journal of Cell Biology. 2007;176:435–444. doi: 10.1083/jcb.200612025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dinarello CA. Biologic basis for interleukin-1 in disease. Blood. 1996;87:2095–147. [PubMed] [Google Scholar]
- Eigenbrod T, Park JH, Harder J, Iwakura Y, Núñez G. Cutting edge: critical role for mesothelial cells in necrosis-induced inflammation through the recognition of IL-1 alpha released from dying cells. J. Immunol. 2008;181:8194–8. doi: 10.4049/jimmunol.181.12.8194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Froelich CJ, Pardo J, Simon MM. Granule-associated serine proteases: granzymes might not just be killer proteases. Trends Immunol. 2009;30:117–23. doi: 10.1016/j.it.2009.01.002. [DOI] [PubMed] [Google Scholar]
- Hazuda DJ, Strickler J, Simon P, Young PR. Structure-function mapping of interleukin 1 precursors. Cleavage leads to a conformational change in the mature protein. J. Biol. Chem. 1991;266:7081–6. [PubMed] [Google Scholar]
- Hernandez-Pigeon H, Jean C, Charruyer A, Haure MJ, Baudouin C, Charveron M, Quillet-Mary A, Laurent G. UVA induces granzyme B in human keratinocytes through MIF: implication in extracellular matrix remodeling. J Biol Chem. 2007;282:8157–64. doi: 10.1074/jbc.M607436200. [DOI] [PubMed] [Google Scholar]
- Irmler M, Hertig S, MacDonald HR, Sadoul R, Becherer JD, Proudfoot A, Solari R, Tschopp J. Granzyme A is an interleukin 1 beta-converting enzyme. J Exp Med. 1995;181:1917–22. doi: 10.1084/jem.181.5.1917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kagi D, Ledermann B, Burki K, Seiler P, Odermatt B, Olsen KJ, et al. Cytotoxicity mediated by T cells and natural killer cells is greatly impaired in perforin-deficient mice. Nature. 1994;369:31–37. doi: 10.1038/369031a0. [DOI] [PubMed] [Google Scholar]
- Kim WJ, Kim H, Suk K, Lee WH. Macrophages express granzyme B in the lesion areas of atherosclerosis and rheumatoid arthritis. Immunol. Lett. 2007;111:57–65. doi: 10.1016/j.imlet.2007.05.004. [DOI] [PubMed] [Google Scholar]
- Kobayashi Y, Yamamoto K, Saido T, Kawasaki H, Oppenheim JJ, Matsushima K. Identification of calcium-activated neutral protease as a processing enzyme of human interleukin 1 alpha. Proc Natl Acad Sci U S A. 1990;87:5548–52. doi: 10.1073/pnas.87.14.5548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kono H, Karmarkar D, Iwakura Y, Rock KL. Identification of the cellular sensor that stimulates the inflammatory response to sterile cell death. J Immunol. 2010;184:4470–8. doi: 10.4049/jimmunol.0902485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kono H, Rock KL. How dying cells alert the immune system to danger. Nat. Rev. Immunol. 2008;8:279–89. doi: 10.1038/nri2215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurt-Jones EA, Beller DI, Mizel SB, Unanue ER. Identification of a membrane-associated interleukin 1 in macrophages. Proc. Natl. Acad. Sci. U S A. 1985;82:1204–8. doi: 10.1073/pnas.82.4.1204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lauw FN, Simpson AJ, Hack CE, Prins JM, Wolbink AM, van Deventer SJ, Chaowagul W, White NJ, van Der Poll T. Soluble granzymes are released during human endotoxemia and in patients with severe infection due to gram-negative bacteria. J. Infect. Dis. 2000;182:206–13. doi: 10.1086/315642. [DOI] [PubMed] [Google Scholar]
- Lavelle EC, Grant G, Pusztai A, Pfüller U, O’Hagan DT. The identification of plant lectins with mucosal adjuvant activity. Immunology. 2001;102:77–86. doi: 10.1046/j.1365-2567.2001.01157.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lowin B, Beermann F, Schmidt A, Tschopp J. A null mutation in the perforin gene impairs cytolytic T lymphocyte- and natural killer cell-mediated cytotoxicity. Proc. Natl. Acad. Sci. USA. 1994;91:11571–11575. doi: 10.1073/pnas.91.24.11571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lüthi AU, Cullen SP, McNeela EA, Duriez PJ, Afonina IS, Sheridan C, Brumatti G, Taylor RC, Kersse K, Vandenabeele P, Lavelle EC, Martin SJ. Suppression of IL-33 Bioactivity through Proteolysis by Apoptotic Caspases. Immunity. 2009;31:84–98. doi: 10.1016/j.immuni.2009.05.007. [DOI] [PubMed] [Google Scholar]
- Matsushima K, Taguchi M, Kovacs EJ, Young HA, Oppenheim JJ. Intracellular localization of human monocyte associated interleukin 1 (IL-1) activity and release of biologically active IL-1 from monocytes by trypsin and plasmin. J Immunol. 1986;136:2883–91. [PubMed] [Google Scholar]
- McElvaney NG, Hubbard RC, Birrer P, Chernick MS, Caplan DB, Frank MM, Crystal RG. Aerosol alpha 1-antitrypsin treatment for cystic fibrosis. Lancet. 1991;337:392–394. doi: 10.1016/0140-6736(91)91167-s. [DOI] [PubMed] [Google Scholar]
- Metkar SS, Menaa C, Pardo J, Wang B, Wallich R, Freudenberg M, Kim S, Raja SM, Shi L, Simon MM, Froelich CJ. Human and mouse granzyme A induce a proinflammatory cytokine response. Immunity. 2008;29:720–33. doi: 10.1016/j.immuni.2008.08.014. [DOI] [PubMed] [Google Scholar]
- Mizutani H, Schechter N, Lazarus G, Black RA, Kupper TS. Rapid and specific conversion of precursor interleukin 1 beta (IL-1 beta) to an active IL-1 species by human mast cell chymase. J Exp Med. 1991;174:821–5. doi: 10.1084/jem.174.4.821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mosley B, Urdal DL, Prickett KS, Larsen A, Cosman D, Conlon PJ, Gillis S, Dower SK. The interleukin-1 receptor binds the human interleukin-1 alpha precursor but not the interleukin-1 beta precursor. J. Biol. Chem. 1987a;262:2941–4. [PubMed] [Google Scholar]
- Mosley B, Dower SK, Gillis S, Cosman D. Determination of the minimum polypeptide lengths of the functionally active sites of human interleukins 1 alpha and 1 beta. Proc. Natl. Acad. Sci. U S A. 1987b;84:4572–6. doi: 10.1073/pnas.84.13.4572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prakash MD, Bird CH, Bird PI. Active and zymogen forms of granzyme B are constitutively released from cytotoxic lymphocytes in the absence of target cell engagement. Immunol. Cell Biol. 2009;87:249–54. doi: 10.1038/icb.2008.98. [DOI] [PubMed] [Google Scholar]
- Reeves EP, Williamson M, Byrne B, Bergin DA, Smith SG, Greally P, O’Kennedy R, O’Neill SJ, McElvaney NG. IL-8 dictates glycosaminoglycan binding and stability of IL-18 in cystic fibrosis. J Immunol. 2010;184:1642–52. doi: 10.4049/jimmunol.0902605. [DOI] [PubMed] [Google Scholar]
- Rhim JH, Kim SA, Lee JE, Kim DJ, Chung HK, Shin KJ, Chung J. Cancer cell-derived IL-1alpha induces IL-8 release in endothelial cells. J. Cancer Res. Clin. Oncol. 2008;134:45–50. doi: 10.1007/s00432-007-0243-8. [DOI] [PubMed] [Google Scholar]
- Sedelies KA, Sayers TJ, Edwards KM, Chen W, Pellicci DG, Godfrey DI, Trapani JA. Discordant regulation of granzyme H and granzyme B expression in human lymphocytes. J Biol Chem. 2004;279:26581–26587. doi: 10.1074/jbc.M312481200. [DOI] [PubMed] [Google Scholar]
- Sower LE, Froelich CJ, Allegretto N, Rose PM, Hanna WD, Klimpel GR. Extracellular activities of human granzyme A. Monocyte activation by granzyme A versus alpha-thrombin. J Immunol. 1996a;156:2585–90. [PubMed] [Google Scholar]
- Sower LE, Klimpel GR, Hanna W, Froelich CJ. Extracellular activities of human granzymes. I. Granzyme A induces IL6 and IL8 production in fibroblast and epithelial cell lines. Cell Immunol. 1996b;10:159–63. doi: 10.1006/cimm.1996.0187. [DOI] [PubMed] [Google Scholar]
- Spaeny-Dekking EH, Hanna WL, Wolbink AM, Wever PC, Kummer JA, Swaak AJ, et al. Extracellular granzymes A and B in humans: detection of native species during CTL responses in vitro and in vivo. J. Immunol. 1998;160:3610–6. [PubMed] [Google Scholar]
- Strik MC, de Koning PJ, Kleijmeer MJ, Bladergroen BA, Wolbink AM, Griffith JM, Wouters D, Fukuoka Y, Schwartz LB, Hack CE, van Ham SM, Kummer JA. Human mast cells produce and release the cytotoxic lymphocyte associated protease granzyme B upon activation. Mol. Immunol. 2007;44:3462–72. doi: 10.1016/j.molimm.2007.03.024. [DOI] [PubMed] [Google Scholar]
- Tak PP, Spaeny-Dekking L, Kraan MC, Breedveld FC, Froelich CJ, Hack CE. The levels of soluble granzyme A and B are elevated in plasma and synovial fluid of patients with rheumatoid arthritis (RA) Clin. Exp. Immunol. 1999;116:366–70. doi: 10.1046/j.1365-2249.1999.00881.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thornberry NA, Bull HG, Calaycay JR, Chapman KT, Howard AD, Kostura MJ, Miller DK, Molineaux SM, Weidner JR, Aunins J, et al. A novel heterodimeric cysteine protease is required for interleukin-1 beta processing in monocytes. Nature. 1992;356:768–74. doi: 10.1038/356768a0. [DOI] [PubMed] [Google Scholar]
- Tschopp CM, Spiegl N, Didichenko S, Lutmann W, Julius P, Virchow JC, Hack CE, Dahinden CA. Granzyme B, a novel mediator of allergic inflammation: its induction and release in blood basophils and human asthma. Blood. 2006;108:2290–9. doi: 10.1182/blood-2006-03-010348. [DOI] [PubMed] [Google Scholar]
- Watanabe N, Kobayashi Y. Selective release of a processed form of interleukin 1 alpha. Cytokine. 1994;6:597–601. doi: 10.1016/1043-4666(94)90046-9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.