Abstract
This study was conducted to explore the effects of an event history calendar (EHC) approach on adolescent sexual risk communication and sexual activity. Adolescent school-linked health clinic patients (n = 30) who reported sexual activity self-administered the EHC that was used by nurse practitioners (NPs; n = 2) during a clinic visit. Immediately pre- and post-visit, and at 1 and 3 months, adolescents reported sexual risk behaviors and perceptions about EHC communication on questionnaires and by interview. NPs reported their perceptions of EHCs by questionnaire after the visit and poststudy interview. The EHC approach facilitated communication and adolescent awareness of their risk behaviors. Scores increased on Amount of Communication, t(29) = 8.174, p < .001; Satisfaction with Communication, t(29) = 3.112, p = .004; Client Involvement in Decision Making, t(29) = 3.901, p = .001, and Client Satisfaction with Interpersonal Style, t(29) = 3.763, p = .001. Adolescents reported decreased sexual intercourse at 1 month, p = .031. School nurses could use the EHC approach to facilitate adolescent communication and tailoring of interventions.
Keywords: adolescent, school-based clinics, screening/risk identification, sexual risk prevention
Despite declines in adolescent sexual activity and increases in contraceptive use (Santelli, Lindberg, Finer, & Singh, 2007), adolescents remain at high risk of pregnancy and at higher risk of acquiring sexually transmitted infections (STIs) than adults (Center for Disease Control and Prevention [CDC], 2010). The birth rate for U.S. teenagers (39.1 births per 1,000 teens ages 15 to 19) increased 5% between 2005 and 2007 (Moore, 2011), but fell 6% in 2009 (CDC, 2011). Adolescents’ sexually transmitted HIV rates are increasing; rates of gonorrhea and chlamydia are highest for adolescent females, and rates of syphilis are increasing among young adult males and females (CDC, 2010). Despite documented adolescent sexual risk behavior, nurses and other clinicians do not consistently talk with adolescents about their sexual risk histories (Adams, Husting,Zahnd, & Ozer, 2008; Klein & Wilson, 2002; Lemley, O'Grady, Rauckhorst, Russell, & Small, 1994). The Healthy Teen Network 2010 report, Healthy People 2020 and Adolescent Health, emphasized critical adolescent reproductive health objectives including, to “increase the proportion of adolescents (9th–12th grade students) who have never had sexual intercourse; if sexually experienced, are not currently sexually active; or if currently sexually active, used a condom the last time they had sexual intercourse” (p. 5). The Institute of Medicine's (IOM, 2008) report, Adolescent Health Services: Missing Opportunities, concluded that high-quality adolescent-centered health care effectively addresses adolescent behavior and contextual influences. IOM stated that in working with adolescents:
Context matters. Social context . . . can profoundly affect the health of adolescents and the health services they receive; Skill matters. Young people are best served by providers who understand the key developmental features, health issues, and overall social environment of adolescents; and Participation matters. Effective health services for young people invite adolescents and their families to engage with clinicians. (p. 2)
Event History Calendars
The Event history calendar (EHC) approach provides a means for nurses to obtain a history of adolescent sexual risk behavior in social context, understand what matters to the adolescents they work with, and engage adolescents in their care. This approach also addresses adolescent cognitive and brain development by providing adolescents with a means to concretely see his or her patterns of risk behaviors over time and discuss risks in context with nurses.
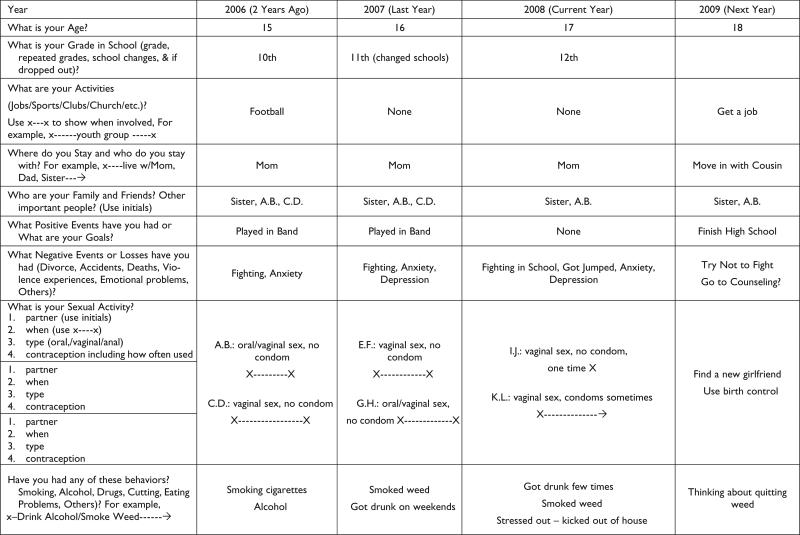
The EHC approach was developed to improve sexual risk assessment and communication (Martyn & Martin, 2003) and a clinical feasibility study indicated this method is time efficient and adolescent-friendly (Martyn, Reifsnider, & Murray, 2006). The EHC is an integrated method of sexual risk assessment designed to: (a) provide more complete risk history information for the nurse to use to tailor communication and treatment plans; and (b) increase adolescent's awareness of the interrelationship of risk behaviors and the effect of their choices on their health (Martyn, 2009). The EHC clearly and concisely shows integrated adolescent sexual risk behaviors using an approach visually similar to a family tree (see Figure 1). EHC integration of risk behaviors and social context is illustrated in a recent report on family/peer support of the adolescent females in this study that revealed those with positive support reported less risk behaviors (Saftner, Martyn, Lori, 2011).
Figure 1. Event history calendar sample.
Legend: X---------X = Duration, beginning and end points; X---------→ = Duration, beginning and continuing points
Adolescents self-administer the EHC by answering open-ended questions about their history (topics in far left column) on life events (i.e., social context) and sexual and other risk behaviors. They record their history for 3 years (the past 2 years and the current year). Then in the far right column, they fill in what they would like to see happen next year (e.g., their future goals). The EHC approach allows the adolescent to reflect on their time and context-linked sexual risk behaviors in a history graph and readies the adolescent to discuss his or her actual and potential risk behavior history with the nurse (Martyn et al., 2006). Prior to the visit with the adolescent, the nurse reviews the adolescent's completed EHC focusing on identification of risk behaviors and the interrelationship between risk behaviors and life events in the context of the timeline. Use of the EHC allows the nurse to identify potential risks and strengths (e.g., activities, relationships, and positive events) in context of the adolescent's life over time, including future goals. The nurse and adolescent then view and discuss the adolescent's sexual risk history together. They can use the EHC as a starting point to clarify the history, add further history details, discuss strengths and risks, and together identify health promoting strategies.
The combined nurse–adolescent use of the EHC provides a partnership approach to the visit facilitating the adolescent's identification of their own risks and strengths, and ways to reduce risk behaviors. The EHC enhances adolescent–nurse communication to reduce sexual risk behavior using key aspects of tailored health communication, including personalization (history that is meaningful to the adolescent is reported using open-ended questions), comparative feedback (the adolescent can see their own behavior over time and in context), and mutual identification of strategies (the adolescent views and discusses their EHC with the nurse; Hawkins, Kreuter, Resnicow, Fishbein, & Dijkstra, 2008).
Theoretical Framework
The EHC approach was developed using Cox's (1982, 2003) Interaction Model of Client Health Behavior (IMCHB), a clinical practice model that contends that client's health behavior is determined by the fit between their unique characteristics (e.g., adolescent sexual risk behavior in social context and awareness of risks and strengths) and the nurse–client interaction (e.g., nurse–adolescent risk behavior communication). The EHC approach encourages full development of the adolescent's awareness of risks and serves as a focused point of departure to facilitate tailored nurse–adolescent communication. This study was guided by the IMCHB to determine if the EHC approach improved nurse practitioner–adolescent risk behavior communication during a clinic visit and decreased adolescent sexual risk behavior at 1 and 3 months after the visit.
Method
This mixed methods study was conducted to explore clinical use of the EHC. Specific aims of this study were to explore the effect of the EHC approach on sexually active female and male adolescents’ perception of communication with nurse practitioners (NPs) and their sexual risk behavior at 1 and 3 months postintervention. The NPs’ perceptions of clinical use of EHCs with adolescents were also explored. The EHC intervention included: (a1) self-administration of the EHC by adolescent participants prior to a clinic visit with a NP and (b) the NP discussing the adolescent's EHC with them during a clinic visit to tailor sexual risk reduction communication. The study was approved by the Human Subjects Committees at the University of Michigan, Ann Arbor, and Oakwood Hospital and Medical Center, Dearborn, Michigan. Informed consent/assent was obtained from all the participants and confidentiality was maintained throughout the research project.
Sample
Thirty adolescents, aged 15–19 years, who were patients in a southeast Michigan school-linked clinic, and two NPs, participated in the study. The clinic provides primary care services to low-middle income adolescent patients who present to the clinic for preventative health services (including physical exam), common illness, STI treatment, and family planning services. The clinic has two NPs and a collaborating physician, all with experience in adolescent primary health care. The clinic schedules patients every 30 min and an average of 15–18 patients are seen by an NP in an 8-hr day. Each year, the clinic provides unduplicated care to approximately 2,000 adolescents. Adolescents who were referred by staff members or self-referred from the flyers were screened for eligibility and the study was explained by a trained research assistant. Eligibility criteria for adolescents included being 15–19 years old, sexually active (reported sex in last 3 months), and in the clinic for a primary health care visit. NP eligibility criteria required at least 1 year of adolescent health experience in the school-linked health clinic.
Procedures
Prior to starting the study in the clinic, the NPs completed a questionnaire on their demographics (e.g., education level, years of experience in adolescent health care) and usual communication with adolescents during primary health care clinic visits. Then the principal investigator (PI) and trained research assistant (RA) provided 60 min of training on the EHC approach, including an orientation to EHC procedures, EHC form and concepts, review of a sample EHC, and EHC approach guidelines. Specifically, the EHC approach guidelines included how to use the EHC, review and clarify the EHC data recorded by the adolescents, identify strengths and risks, and together identify health promotion and risk reduction strategies based on standards of care for adolescent health.
The RA conducted the study in the clinic with the NP and adolescent participants. She met potential adolescent participants who had a primary health care appointment in the clinic waiting room, determined eligibility, explained the study, and obtained consent/assent. Then she gave the adolescent a paper EHC to complete and asked them to answer the open-ended questions about their life events, and sexual and other risk behaviors for the current year, past 2 years, and the next (or future) year. Then the EHC was placed on the adolescent's chart and given to the NP. Prior to the visit with the adolescent, the NP reviewed the adolescent's EHC to identify risks and strengths, and the timeline and patterns of behaviors and events. Next, the NP and adolescent sat side-by-side to view and discuss the adolescent's EHC. The NP assisted the adolescent in clarifying his or her history during this process. Finally, the NP and adolescent together identified strengths and risks, and ways to promote health and reduce sexual risk behavior based on standards of care for adolescent health.
Data were collected from adolescents and NPs using questionnaires and interviews. Adolescents completed questionnaires pre- and postintervention, and at 1 and 3 months postintervention (retention was 95.5%). Demographic data on age, gender, occupation, marital status, social situation, residence, ethnicity, subsidized meals, and last visit for health care were collected. Questionnaires were adapted for the study based on established questionnaires on sexual risk behaviors (e.g., CDC Youth Risk Behavior Surveillance; CDC, 2009b) and adolescent–provider communication (e.g., APPIS; Woods, Klein, Wingood, Rose, & Wypij, 2006). Items in these measures used 4- or 5-point rating scales. Scores on the scales were calculated as the mean responses on the items. Adolescent–provider communication scale reliability coefficients αs ranged from .84 to .94. NPs completed pre- and postintervention questionnaires that were also adapted from existing communication tools (Woods et al.) and asked about usual communication with adolescents and communication using the EHC on a 5-point rating scales. Both the adolescents and NPs were interviewed postintervention about their perceptions of the clinical use of the EHC.
The RA conducted 15- to 20-min semistructured interviews with the adolescents immediately after the clinic visit and with the NPs after they completed all study clinic visits. During the interviews, both adolescents and NPs were asked similar questions about what they thought of using the EHC for sexual risk history and communication during clinic visits (i.e., did the EHC help and how?). Specifically, the interviews focused on adolescent and NP perceptions of how the EHC affected report of sexual risk histories, identification of risk behaviors, and communication with adolescents or NPs.
Data Analysis
Descriptive statistics using the Statistical Package for the Social Sciences (SPSS) were used to summarize questionnaire responses. Categorical data were summarized by percentages and frequency distributions and continuous measures by their means and standard deviations. For quantitative dependent variables that are approximately normally distributed (e.g., communication satisfaction), paired t tests comparing the means in the pretest with the posttest were the primary analysis. For dichotomous dependent variables (e.g., had sexual intercourse), the primary method of analysis was a variation of the chi-square test to determine whether the occurrence of the outcome is more or less likely in the posttest than in the 1- and 3-month follow-ups.
Power analysis for the effects of time (post vs. pre) on the continuous measures run with PASS software (Hintze, 2008) indicated that a sample size of 34 would be required to have 80% power to detect a medium sized difference between means (change divided by standard deviation of change = .5) with α of .05, two-tailed. Such an effect has been described by Cohen (1992) as visible to the naked eye, thus clearly important to be able to detect. With the sample of 30, power for this was 75% which is reasonably good. Power for detecting changes in rates of behavior over time is less both because the lower precision of estimates of percentages, lower correlation over time in those dichotomous measures, and because of loss of as many as three participants over time. Those analyses must be considered exploratory.
Qualitative analyses were performed by a team including the PI (an experienced qualitative researcher who guided analysis) and two RAs (one who conducted the interviews and a pediatric NP graduate student). The team used the constant comparative method to identify common themes related to clinical use of the EHC and communication from the perspectives of the adolescent and NP (Glaser, 1992). Then the PI made the final determination of common themes guided by the research question: “How does the EHC approach influence sexual risk communication from adolescent and NP perspectives?”
Results
The sample included thirty 15- to 19-year-old female and male patients (mean age = 17.3 for both groups) and two NPs (both master's-prepared with 6 and 12 years of adolescent health experience) from a school-linked health clinic in Southeast Michigan. Thirteen females and 6 males identified as European American, and 6 females and 5 males identified as African American. All participants were sexually active and 54% reported using a condom at last intercourse. The majority of adolescent participants were from low income (i.e., 53% of females and 64% of males reported eligibility for subsidized school meals) group. On average, the adolescents took 10–15 min to complete the EHC.
Perceptions of Adolescent–NP Communication
Adolescents’ and NPs’ qualitative interviews indicated that the EHC approach improved sexual risk communication, and adolescent awareness of their own risk behavior. The NPs reported that using the EHC allowed them to partner with the adolescent to: obtain a “richer amount of information;” “show [the adolescent] visually what their behavior was;” and “intervene on a different level” to promote sexual risk reduction. They also noted that this approach was easy to integrate into their clinic visit format and did not significantly increase the amount of time spent with the adolescent patient. On average, the clinic visits lasted 20–30 min. According to the NPs, using the EHC with adolescent patients did not add time to the usual clinic visit time or affect the number of patients seen during a clinic session.
Adolescents described four overall perceptions about sexual risk communication using the EHC with NPs. The themes and illustrative quotes indicated that the EHC approach:
1) Helped to get sexual risk communication started: “Instead of trying to pick it [sexual history] out of you, you've already written it down for [the NP];” 2) Increased awareness of sexual risks: “Sexual risk behavior was not seen as “a big deal until I had to write it down and see it for my own eyes;” “It brought back a lot of stuff that I didn't even remember . . . people that I've had sexual encounters with . . . made me think of a lot of stuff;” and “I think it helps you be aware of who you are sexually active with . . . if you would have an STD or something, you would know what partner it was;” 3) Encouraged discussion about sexual risks: “Just getting it all out there” . . . “helped me talk to [the NP] because it's not like I had to bring it up” and 4) Enhanced overall communication with the NPs: “We talked about the other things . . . not just my sexual history . . . like my life history and that made me feel more open and more able to talk to the practitioner.”
Ratings of Adolescent–NP Communication
Five scales were constructed to quantitatively assess the effects of the EHC approach on adolescent–NP communication from before to after the interaction with the NP. These measures are Amount of Communication (10 items, α of .93), Satisfaction with Communication (7 items, α of .94), Supportive Communication (10 items, α of .92), Client Involvement in Decision Making (4 items, α of .88), and Client Satisfaction with Interpersonal Style (13 items, α of .84). Examples of items for Amount of Communication included: In general, how much did you talk with the nurse practitioner or doctor; for Satisfaction with Communication: Overall, I am satisfied with communication with nurse practitioners and doctors during the clinic visits; for Supportive Communication: The nurse practitioner or doctor took my concerns seriously; for Client Involvement in Decision Making: The nurse practitioner or doctor tried to include me in decisions about my health care; and for Client Satisfaction with Interpersonal Style: The nurse practitioner or doctor were compassionate and caring.
Paired t tests were conducted comparing the posttest responses on these scales with the pretest responses on them (See Table 1). Statistically significant increases in posttest scores were noted on four of the five scales. Scores increased on: Amount of Communication from a mean of 2.65, corresponding to talking a little (2) or some (3), to a mean of 3.69, corresponding to some (3) or a lot (4); Satisfaction with Communication from a mean of 4.07, corresponding to agree (4), to 4.42, corresponding to agree (4) or agree strongly (5) with statements like “Overall, I am satisfied with communication with nurse practitioners and doctors during the clinic visits”; Client Involvement in Decision Making from a mean of 2.88, corresponding to some of the time (2) or most of the time (3), to a mean of 3.36, corresponding to most of the time (3) or all of the time (4) on items like “The nurse practitioner or doctor tried to include me in decisions about my health care,” and Client Satisfaction with Interpersonal Style from a mean of 3.13, corresponding to most of the time (3), to a mean of 3.40, corresponding to most of the time (3) or all of the time (4) with items like “The nurse practitioner or doctor were compassionate and caring.” However, scores did not change on the Supportive Communication scale, with a pretest mean of 3.27 and a posttest mean of 3.32, which are both in the range from most of the time (3) to all of the time (4) on items like “The nurse practitioner or doctor took my concerns seriously.”
Table 1.
Changes in Scale Scores From Before the EHC to Immediately After the Session With the Nurse Practitioner
| Measure | Pretest Mean (SD) | Posttest Mean (SD) | Mean Change (SD) | t-Test Result | Significance |
|---|---|---|---|---|---|
| Amount of communication | 2.65 (0.86) | 3.69 (0.75) | 1.04 (0.70) | t(29) = 8.174 | p < .001 |
| Satisfaction with communication | 4.07 (0.68) | 4.42 (0.52) | 0.36 (0.63) | t(29) = 3.112 | p = .004 |
| Supportive communication | 3.27 (0.66) | 3.32 (0.54) | 0.05 (0.47) | t(29) = 0.614 | p = .554 |
| Client involvement in decision making | 2.88 (0.86) | 3.36 (0.55) | 0.48 (0.67) | t(29) = 3.901 | p = .001 |
| Client satisfaction with interpersonal style | 3.13 (0.52) | 3.40 (0.31) | 0.27 (0.40) | t(29) = 3.763 | p = .001 |
Reports of Adolescent Sexual Risk Behavior
Reports of sexual behavior and condom use at various times indicated that the proportion of adolescent participants having sex dropped from a posttest report (100%; 95% CI [confidence interval]: [88.4%, 100%]) to 1-month follow-up (79%; 95% CI: [60%, 92%]) and 3-month follow-up (89%; 95% CI: [71%, 98%]). The drop from posttest to 1-month follow-up was significant (p = .031) but the change at 3 months was nonsignificant. The proportion who reported using a condom at last intercourse did not change notably (53%; 95% CI: [34%, 72%], 48%; 95% CI: [29%, 68%], and 59%; 95% CI: [39%, 78%] at post, 1 month, and 3 months, respectively). None of the changes over time in condom use were significant.
Discussion
Overall, the results of this mixed methods study support the use of the EHC approach to improve adolescent–NP communication about sexual risk behaviors. This is consistent with Cox's IMCHB (1982); the adolescent's EHC report of risk behavior and social context histories facilitated the fit between the adolescent's unique characteristics and the adolescent–nurse interaction and improved sexual risk communication. Adolescents’ and NPs’ perceptions of adolescent–NP communication using the EHC indicated improvement in relation to their overall communication; and their communication about sexual activity, risk behaviors, and patterns over time. Sexual risk communication with adolescents is recognized as an important part of quality adolescent health care; however, many clinicians have difficulty talking to adolescents about sex (Killebrew & Garofalo, 2002).
The adolescent and NP perspectives on the EHC approach were positive. The adolescents in this study described the EHC as providing an easy way to start the discussion about risks and to continue to address this often uncomfortable topic in greater depth. They also liked the fact that this approach allowed them to talk with NPs about other important things, like their life history and their goals. In addition, the EHC allowed them to better see their own risk behaviors in the context of the rest of their life. Rather than being told by a NP what their risk behaviors were, they could look at their calendar history and see their own behaviors and how they related to their life events. They could also focus on the changes they wanted to see happen in their lives in the future by discussing their goals. This creates more realistic interaction between adolescents and nurses or other clinicians and allows them to work together to help the adolescent identify what they can do to decrease their own risk behaviors. NPs thought the EHC approach enhanced tailoring of sexual risk reduction intervention.
The adolescent ratings on the Supportive Communication scale showed no change pre- and postintervention; however, this may be more a reflection of the supportive adolescent-centered philosophy of the school-linked health clinic than the EHC method. A larger study with nurses and other clinicians who work with a broader age range or a traditional clinical perspective could provide a better understanding of the influence of the EHC approach on this aspect of communication.
Adolescent report of sexual intercourse significantly decreased at 1 month; however, significant differences were not found in sexual intercourse at 3 months or condom use at 1 or 3 months. This may be related to a variety of reasons and since we did not have a control group in this study our interpretation of this finding is limited. Similar limited sustainability has been found in other sexual risk reduction brief interventions (Roye, Silverman, & Krauss, 2007). In addition, at 3 months, we had missing data because two participants were lost to follow-up.
Implications for Practice
The adolescent clinic visit is a critical event, often the only time adolescents can independently talk with nurses and other clinicians about sexual risk behaviors. The school setting, in particular school-based and school-linked health clinics, provide an excellent opportunity to reach and follow-up with adolescents about their risk behaviors and concerns. “School nurses and clinicians working in school settings could use the EHCs [event history calendars] to improve adolescent assessment and intervention” (p. 11, Saftner, Martyn, Lori, 2011). The EHC approach during clinic visits provides a unique opportunity to facilitate: adolescents’ awareness of sexual risks, adolescent–provider communication about sexual risks and future goals, and tailoring of sexual risk reduction intervention. Because the EHC method helps adolescents view their risk behavior in context of their life events over time, it is possible to increase adolescent awareness of their own behavior and interrelationships. This in turn, could improve adolescents’ decision making about their future behavior, positively influence health behavior, and ultimately reduce sexual risk behavior outcomes. The use of the EHC has been shown to improve nurses’ communication with adolescents around these issues. Development of a partnership between adolescents and nurses is a key component of effective interventions to reduce sexual risk behaviors. Successful adolescent–nurse interactions involve adolescents in their own care (Partners in Program Planning for Adolescent Health [PIPPAH], 2010); the EHC approach provides the opportunity to engage adolescents and facilitate sexual risk reduction interventions that are tailored to each adolescent's individual needs.
Limitations
This exploratory study was limited by a small sample of adolescents (n = 30) and NPs (n = 2); however, the mixed approach method approach provided rich in-depth data. In addition, a majority of the sample consisted of European American English speaking females from a school-linked health center. This limits generalizability, but does provide a foundation from which to build further research. Outcomes from this study were measured only at 1 and 3 months and no control group was included in this study. These limitations will be addressed in future studies. Our results suggest that, in this sample, the EHC was effective at increasing communication between adolescents and NPs regarding sexual risk behaviors.
Future Research
Given the significant findings from this study, we recommend further study of the EHC approach with adolescents and young adults focused on nurses and other clinicians’ communication and risk behavior reduction interventions, including a randomized control trial with longer follow-up in a variety of primary health care settings with nurses and other clinicians.
Conclusions
From the literature, we know that adolescent STIs and pregnancy rates continue to remain high and that nurses and other clinicians should communicate with adolescents about their sexual risk behavior histories, but do not do this consistently. The EHC is uniquely positioned to address communication issues around adolescent sexual risk behaviors in school-based, school-linked, and primary care clinic settings. We have shown in this study that the EHC can be used in one session in a school health setting to enhance adolescent–NP communication.
Acknowledgments
The authors gratefully acknowledge the contribution to this research project of Katherine Kristofik, MSN, RN, FNP-BC, Nurse Practitioner at Oakwood Taylor Teen Health Center, Southgate, MI, and Lissa Lee, MS, RN, CPNP-PC, former University of Michigan graduate student.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: National Institutes of Health and National Institute of Nursing Research, The Michigan Center for Health Intervention, P30 NR009000.
Biography
Kristy K. Martyn, PhD, RN, CPNP-PC, FNP-BC, is an associate professor and chair at the University of Michigan, School of Nursing, North Ingalls, Ann Arbor, MI, USA.
Cynthia Darling-Fisher, PhD, RN, FNP-BC, is a clinical assistant professor at the University of Michigan, School of Nursing, North Ingalls, Ann Arbor, MI, USA.
Michelle Pardee, DNP, RN, FNP-BC, is a clinical instructor at the University of Michigan, School of Nursing, North Ingalls, Ann Arbor, MI, USA.
David L. Ronis, PhD, is a research scientist and director of the Statistical Consulting Team at the University of Michigan School of Nursing and a Research Health Science Specialist at the VA Center for Clinical Management Research, Ann Arbor, MI, USA.
Irene L. Felicetti, MLS, is a Project Manager at the University of Michigan, School of Nursing, North Ingalls, Ann Arbor, MI, USA.
Melissa A. Saftner, PhD, RN, CNM is a recent graduate of the University of Michigan and is an assistant professor at The College of St. Scholastica, School of Nursing, Duluth, MN, USA.
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Adams SH, Husting S, Zahnd E, Ozer EM. Adolescent preventive services: Rates and disparities in preventive health topics covered during routine medical care in a California sample. Journal of Adolescent Health. 2008;44:536–545. doi: 10.1016/j.jadohealth.2008.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Center for Disease Control and Prevention STDs in adolescents and young adults. 2010 Retrieved from http://www.cdc.gov/std/stats09/adol.htm.
- Center for Disease Control and Prevention YRBSS: 2009 Questionnaires and item rationale. 2009. 2009 Retrieved from http://www.cdc.gov/HealthyYouth/yrbs/questionnaire_rationale.htm.
- Center for Disease Control and Prevention Teen birth rate declined again in 2009. 2011 Retrieved from http://www.cdc.gov/Features/dsTeenPregnancy/
- Cohen J. A power primer. Psychological Bulletin. 1992;112:155–159. doi: 10.1037//0033-2909.112.1.155. [DOI] [PubMed] [Google Scholar]
- Cox CL. An interaction model of client health behavior: Theoretical prescription for nursing. Advances in Nursing Science. 1982;5:41–56. doi: 10.1097/00012272-198210000-00007. [DOI] [PubMed] [Google Scholar]
- Cox CL. A model of health behavior to guide studies of childhood cancer survivors. Oncology Nursing Forum. 2003;30:E1–E8. doi: 10.1188/03.ONF.E92-E99. [DOI] [PubMed] [Google Scholar]
- Glaser BG. Basics of grounded theory analysis. Sociology Press; Mill Valley, CA: 1992. [Google Scholar]
- Hawkins RP, Kreuter M, Resnicow K, Fishbein M, Dijkstra A. Understanding tailoring in communicating about health. Health Education Research. 2008;23:454–466. doi: 10.1093/her/cyn004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Healthy Teen Network Healthy people 2020 and adolescent health: A primer. 2010 Retrieved from http://www.HealthyTeenNetwork.org.
- Hintze JL. PASS 2008 user's guide. Number Cruncher Statistical Software; Kaysville, UT: 2008. [Google Scholar]
- Institute of Medicine Adolescent health services: Missing opportunities. 2008 Retrieved from http://www.nap.edu/catalog/12063.html.
- Killebrew M, Garofalo R. Talking to teens about sex, sexuality, and sexually transmitted diseases. Pediatric Annals. 2002;31:566–572. doi: 10.3928/0090-4481-20020901-09. [DOI] [PubMed] [Google Scholar]
- Klein JD, Wilson KM. Delivering quality care: Adolescents’ discussion of health risks with their providers. Journal of Adolescent Health. 2002;30:190–195. doi: 10.1016/s1054-139x(01)00342-1. [DOI] [PubMed] [Google Scholar]
- Lemley KB, O'Grady ET, Rauckhorst L, Russell DD, Small N. Baseline delivery of clinical preventive services provided by nurse practitioners. Nurse Practitioner. 1994;5:57–63. [PubMed] [Google Scholar]
- Martyn KK. Adolescent health research and clinical assessment using self-administered event history calendars. In: Belli R, Stafford F, Alwin D, editors. Calendar and time diary methods in life course research. SAGE; Thousand Oaks, CA: 2009. pp. 69–86. [Google Scholar]
- Martyn KK, Martin R. Adolescent sexual risk assessment. Journal of Midwifery and Women's Health. 2003;8:213–219. doi: 10.1016/s1526-9523(03)00064-3. [DOI] [PubMed] [Google Scholar]
- Martyn KK, Reifsnider E, Murray A. Improving adolescent sexual risk assessment with event history calendars: A feasibility study. Journal of Pediatric Health Care. 2006;20:19–26. doi: 10.1016/j.pedhc.2005.07.013. [DOI] [PubMed] [Google Scholar]
- Moore KA. Teen birth rates: Examining the recent trends. 2011 Retrieved from http://www.thenationalcampaign.org/resources/birthdata/
- Partners in Program Planning for Adolescent Health (PIPPAH) Creating healthy opportunities: Conversations with adolescent health experts. 2010 Retrieved from www.ncsl.org/default.aspx?tabid=21298.
- Roye C, Silverman PP, Krauss B. A brief, low-cost, theory-based intervention to promote dual methods used by Black and Latina female adolescents: A randomized clinical trial. Health Education Behavior. 2007;34:608–621. doi: 10.1177/1090198105284840. [DOI] [PubMed] [Google Scholar]
- Santelli JS, Lindberg LD, Finer LB, Singh S. Explaining recent declines in adolescent pregnancy in the United States: The contribution of abstinence and improved contraceptive use. American Journal of Public Health. 2007;97:150–156. doi: 10.2105/AJPH.2006.089169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saftner MA, Martyn KK, Lori JR. Sexually active adolescent women: Assessing family and peer relationships using event history calendars. The Journal of School Nursing. 2011;27:225–236. doi: 10.1177/1059840510397549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woods ER, Klein JD, Wingood GM, Rose ES, Wypij D. Development of a new Adolescent Patient-Provider Interaction Scale (APPIS) for youth at risk for STDs/HIV. Journal of Adolescent Health. 2006;38:753e1–753e7. doi: 10.1016/j.jadohealth.2005.08.013. [DOI] [PubMed] [Google Scholar]