Abstract
Objectives
To build upon state-of-the art theory and empirical data to estimate the strength of multiple mediators of the efficacious Keep Active Minnesota (KAM) physical activity (PA) maintenance intervention.
Methods
The total, direct, and indirect effects through which KAM helped randomized participants (KAM n=523; UC n=526) maintain moderate or vigorous PA (MVPA) for up to 2 years were estimated using structural equation modeling.
Results
Multiple mediators explained half (β=.052, P=.13) of the effect of KAM on MVPA (β=.105, P=.004). Self-efficacy was the upstream variable in 2 endogenously mediated effects, and the self-concept mediator emerged as the strongest predictor of MVPA.
Conclusions
KAM positively impacted self-efficacy, which was associated with PA enjoyment, integration into the self-concept, and PA maintenance. Successful long-term PA maintenance appears to be influenced by multiple small interrelated mediational pathways. Future research evaluating maintenance models should specify recursive relationships among mediators and outcomes.
Keywords: maintenance, physical activity, multiple mediation, behavioral intervention, structural equation modeling
INTRODUCTION
It is well established that regular physical activity (PA) of at least moderate intensity has positive effects on the health1–6 and well-being of mid-life and older adults.7–10 Yet, unless PA is maintained long-term, many of these benefits do not persist. Thus, attempts to increase population levels of PA face a 2-fold challenge: first, to encourage and facilitate the initiation of regular PA among the sedentary and, second, to assist individuals in developing and maintaining a habit of PA once they have begun.11
Interventions that are effective in helping people both initiate and maintain health-promoting levels of PA are needed to successfully increase population levels of PA. To maximize the health impact of such interventions, it is useful to know which work, but added value inheres in understanding why they work. A compelling argument has been made for the importance of adopting a mediating variable framework to systematically incorporate the role of theory in PA initiation interventions and for identifying the most efficacious intervention components, so that we can cost-effectively design and implement behavioral interventions.12–15 Also important is an understanding of the processes involved in maintaining PA so that there are effective interventions appropriate to individuals at differing points in their behavioral change process.16
In the spirit of identifying cost-effective interventions for PA adoption, a small but growing body of literature has used increasingly sophisticated methodological tools to better articulate some of the moderators or mediators of PA intervention efficacy.13,15,17–22 The predominant focus has been on the examination of mediators of PA initiation with less emphasis placed on the mediators of PA maintenance.16,23–27 In response to the increasing recognition of the importance of developing and understanding strategies to achieve long-term maintenance of behavior change, the present work attempts to build upon state-of-the art theory and empirical data regarding PA mediators23 to identify and estimate the strength of multiple mediational pathways of PA maintenance.
Examination of this literature suggests that psychosocial variables derived from social cognitive theory (eg, self-efficacy) and the transtheoretical model (eg, behavioral processes of change) are important mediators of physical activity. Previously identified mediators of the effects of PA interventions on PA outcomes include home access to PA equipment,16 self-efficacy,17,18,28,29 social support,18,30 enjoyment of PA,31 behavioral and cognitive processes of change,15,28,32 and decisional balance,32 with the most consistently observed mediator being self-efficacy.
The factors promoting behavior-change initiation may differ from those that promote their maintenance.23 For example, Rothman33 has suggested that decisions regarding behavioral initiation depend on favorable expectations regarding future outcomes, whereas decisions regarding behavioral maintenance depend on perceived satisfaction with received outcomes. Consistent with this argument, PA adherence has been found to be predicted by realization of psychological and fitness benefits.17,34
Based on the assertion that what predicts the adoption of PA may differ from what predicts PA maintenance, Nigg et al have recently proposed a theory of PA maintenance (PAM).23 The PAM posits that interventions aimed at long-term maintenance of PA would be expected to function largely through psychosocial variables grouped under the 3 headings of goal-setting, motivation, and self-efficacy. Moreover, these factors are theorized to be integral to PA maintenance, as well as being interrelated and having reciprocal effects. A recent empirical demonstration of such interrelatedness has been provided by Dishman et al, who documented an indirect effect of self-efficacy on PA adoption operating through self-management strategies.35 The PAM framework also recognizes that these interrelated psychosocial processes occur within the larger context of the PA environment on one hand (which may either facilitate or inhibit sustained PA) and ever-present life stressors on the other (which often negatively affect the setting and achievement of life goals, including sustained PA).
To date, theories regarding mediators of PA maintenance and potential differences between mediators of initiation and maintenance remain largely untested. It may not be feasible, for example, to incorporate a long-term maintenance component into initiation trials, given their focus and limited duration. Although formal mediational analyses of PA maintenance are not readily found in the literature, a number of studies have examined predictors of PA maintenance, typically following participation in a PA initiation program. Bock et al reported that baseline smoking status, perceived benefits of PA, and endorsement of processes of change were predictive of PA maintenance at 12 months.36 Additionally, use of behavioral and cognitive processes of change, more positive mood, higher self-efficacy, and lower perceived barriers to PA at the end of the 6-month initiation intervention were predictive of 12-month PA maintenance. In a recent home-based PA intervention among 205 sedentary adults, Williams et al explored differences in predictors of initiation and maintenance of PA, finding that although access to home-based PA equipment was predictive of PA adoption, maintenance of PA at 12 months was predicted only by self-efficacy and perceived satisfaction.16 In the study with the longest follow-up period, McAuley et al reported that older adults with higher self-efficacy following completion of a 6-month intervention were more likely to report higher levels of PA 18 months postintervention and that higher levels of PA, more positive affect, and higher self-efficacy at this interim time point were predictive of higher levels of PA at 5-year follow-up.24 These interventions, geared toward PA initiation, demonstrate that factors (eg, self-efficacy) supporting initiation may also be integral to PA maintenance and that extant theorizing on mediators of maintenance shows promise (eg, satisfaction, self-efficacy). The development and estimation of formal mediational models of PA maintenance can build upon the information regarding predictors of PA maintenance provided by these studies.
A direct approach for theory development with respect to PA maintenance is to examine mediational processes in the context of an intervention program that explicitly targets PA maintenance.23 Keep Active Minnesota (KAM) tested a PA maintenance intervention among active 50- to 70-year-old adults whose baseline level of activity represented an increase within the previous year.11,37–38 Participants randomized into the KAM intervention were offered an interactive telephone and mail-based PA support program. In addition to assessing PA level at 6, 12, and 24 months after randomization, we assessed multiple theoretically grounded mediators of PA maintenance at each time point. KAM was successful in helping adults maintain their PA level across the study period, providing the opportunity to explore potential pathways through which the intervention was effective.
Because this work represented an initial attempt to identify mediators of PA maintenance and quantify their relative importance, we measured constructs that had been shown previously to mediate behavior initiation or maintenance, that had been theorized to be relevant to PA maintenance, or that were explicitly emphasized in the content of the intervention. An inclusive approach made it possible to assess whether empirically demonstrated mediators of initiation also play a role in the context of maintenance. The mediators considered important to this work included self-efficacy for exercise,17,18,28,29 barriers to exercise,32 enjoyment of exercise,31 incorporation of PA into the self-concept,39–41 and social support received from family and from friends.18,30 Self-efficacy was included because there has been consistent empirical evidence that it is related to PA initiation17,18,28,29 and has been argued to be theoretically related to PA maintenance.23 Moreover, the KAM intervention focused on both increasing self-efficacy and identifying possible solutions to known barriers to PA, which itself has been considered a key potential factor for maintaining health-promoting behavior, particularly among older adults.17,42–45 Satisfaction with the outcomes of a behavior is thought to be integral to its maintenance.17,34 Enjoyment of PA was considered a potential mediator of maintenance because, like satisfaction, it taps into how much people positively evaluate PA that has been initiated.31,33 We speculated that there would be no single mediator uniquely associated with PA and, in fact, that a chain of mediational processes might best explain long-term maintenance. Assessing multiple mediators in a large sample enabled these goals to be met.
We propose that the mediators under study here are components of a process whereby over time, an individual’s self-concept is modified to incorporate the notion of being a physically active person. Specifically, we propose that through even modestly sustained physical activity and belief that one has the ability to continue engaging in physical activity (self-efficacy), being a physically active person becomes an important part of one’s self-concept. Activity becomes less about “what one does” and more about “who one is.”
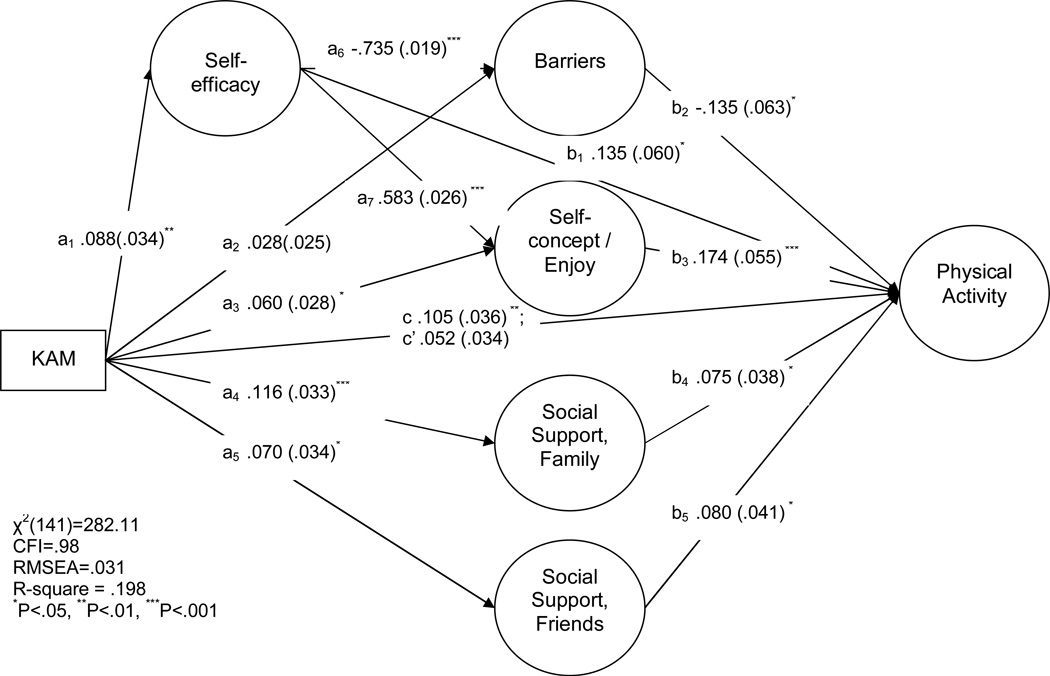
The goals of this exploratory process were to identify significant factors that mediated the efficacy of a phone-based intervention on PA and simultaneously estimate the relative strength of multiple indirect pathways through these constructs to increased PA. The KAM intervention focused on improving self-efficacy through cognitive, behavioral, and environmental strategies. As such, the most immediate effect of KAM should be on self-efficacy (path a1 in Figure 1). Heightened self-efficacy should reduce the extent to which participants allowed common barriers to prevent them from being physically active (a6) and promote the incorporation of activity into the self-concept (a7), in addition to the direct impact of KAM on these mediators (a2, a3). We also speculated that KAM participants would more frequently take advantage of social support from family (a4) and friends (a5) once such support was offered. Each of the mediators was expected to be predictive of MVPA (b1 through b5).
Figure 1.
Standardized Structural Path Coefficients and Standard Errors for the Mediators of KAM and Physical Activity
METHODS
Participant Eligibility and Recruitment
This study protocol was reviewed and approved by the HealthPartners Research Foundation Institutional Review Board; moreover, the study was conducted among 50-to 70-year-old members recruited from one large managed-care organization in the Minneapolis/St. Paul metropolitan area. Participants were recruited over 15 months beginning in September 2004 by means of direct mail to potentially eligible health plan members and supplemented with study advertisements in health plan communications.
We used health plan records and self-report to assess eligibility criteria. Participants were eligible if they were 50 to 70 years old, self-reported that they had increased their activity over the previous year and that they were accumulating an average of at least 30 minutes of moderate to vigorous PA at least 2 days per week over the previous 4 weeks, had no comorbidities that would preclude engaging in moderate to vigorous PA, and were enrolled in the health plan for 11 of the past 12 months to allow assessment of their health records to confirm the absence of significant comorbidities.
Eligible members who consented to participate in the study (N=1049) were randomly assigned to the KAM intervention or to a usual care group (UC). All participants self-reported their PA levels at baseline prior to being informed of their randomization assignment and again 6, 12, and 24 months postrandomization so that PA, expressed as weekly kcal expenditure, could be assessed over the 2 years following randomization. The targeted sample size of n=500 per arm was based on that needed to adequately power the primary efficacy analyses. A KAM-by-time interaction with between-groups differences of Cohen’s d=.00 at baseline and d=.25 at 24 months was predicted. Additional detail regarding the target population, eligibility assessment, recruitment, and study design may be found in previous publications.11,37
KAM Intervention
Participants randomized into KAM were offered an interactive telephone- and mail-based physical activity support program that was developed by this study team and based primarily on principles of Bandura’s social cognitive theory46,47 and relapse prevention theory.48 The core component of KAM included 7 phone-based sessions with an activity coach with background in exercise science and training in behavior-change theory. Coaching-session content focused on self-management, using cognitive, behavioral, and environmental strategies, with particular emphasis on enhancing self-efficacy through identification of PA barriers and problem solving to prevent and/or recover from relapse. These core sessions were followed by monthly check-in calls for the remainder of the first 12 months and bimonthly calls during the second year of study participation and supplemented with motivational challenges, 4 optional group sessions, and a physical activity resource lending library. Additional detail about the KAM intervention may be found in a previously published paper.38
Measures
Randomization to KAM (n=523) or UC (n=526) was the predictor in these analyses. Outcomes and mediators were measured during telephone interviews with participants prior to, and 6, 12, and 24 months after, randomization. The latent outcomes and mediators were constructed from the common variance across the 6-, 12-, and 24-month composites and scaled so that higher values represented more of the measured construct.
The intervention efficacy outcome measure was kilocalories expended per week on moderate and vigorous activities (MVPA) at 6, 12, and 24 months. MVPA was computed using the CHAMPS instrument, designed for use in adult populations such as this one to assess the self-reported frequency and duration of a range of common activities and convert these reports into weekly kcal expenditure.49
Six constructs hypothesized to function as mediators were each measured 6, 12, and 24 months postrandomization. The self-efficacy composite consisted of participant ratings of their confidence on a scale from 0 to 100% that they could continue being active even if each of 12 common barriers to physical activity (eg, bad weather, vacation, schedule conflict) was present.50 The mean of the 12 ratings was divided by a constant, 20, so that the 0–100 scale would more closely approximate the 5-point range of other mediators. The internal consistency of the self-efficacy measures ranged from α=.88 (6, 12m) to α=.90 (24m) in this sample.
To measure barriers to physical activity, participants rated how true it was (1=not at all true, 5= very true for me) that each of 21 barriers had made regular exercise more difficult in the previous 6 months (eg, I have difficulty exercising when I get busy; I have difficulty figuring out how to fit exercise into my daily life; I have difficulty exercising when I just want to relax and enjoy myself).51 In contrast to the perceived likelihood that they could be active in the future (self-efficacy), the barriers composite assessed how often situational adversity had in fact prevented participants from being active. A composite barriers score was calculated at each time point as the mean of the 21 ratings with internal consistencies ranging from α=.90 (6m, 12m) to α=.91 (24m).
Four items were included in each survey to assess how much enjoyment participants derived from being physically active.52 Each item (eg, I enjoy being physically active; being physically active is very pleasant) was rated on a 5-point scale (1=not at all true, 5= very true for me), and the mean of the ratings was taken at each time point. Internal consistencies ranged from α=.90 (12m) to α=.91 (6m, 24m).
Participants also reported on the extent to which being physically active was incorporated into the self-concept using an adaptation of the Athletic Identity Measurement Scale.53 Five (eg, Physical activity is an important part of my life; other people see me as a physically active person) of the original 10 items were rated on a 5-point scale (1=not at all true, 5= very true for me) and averaged into a single score at each time point. Internal consistencies ranged from α=.86 (6m) to α=.88 (24m).
Two scales were included to measure perceptions of how often in the past 6 months participants had received social support for being physically active from family or others living in the household or from friends or acquaintances.54 Each of the 10 supportive behaviors (eg, exercised with me, helped plan activities around my exercise) was rated on a 5-point scale (1=none, 2=rarely, 3=a few times, 4=often, 5=very often) twice, once in reference to family and once to friends. Responses to the family items were averaged into a measure of family support at each time point (α=.82 at 6m, 12m to α=.84 at 24m) whereas the friends items were averaged into a measure of friend support (α=.83)
Analysis Plan
A structural equation model was estimated using all available observations from all participants. Latent mediator and MVPA factors were estimated as the common variance in the 6-, 12-, and 24-month composites for each construct; and structural relationships between KAM participation, mediators, and MVPA were specified. Most pertinent to our conceptualization of the mechanisms by which KAM maintains MVPA were the multiply mediated indirect effects of KAM on MVPA. Standardized path coefficients were estimated using maximum likelihood estimation, and an excellent fit of the specified model to the raw covariance matrix would be obtained if the comparative fit index (CFI) > .95, root mean square error of approximation (RMSEA) < .05, and the model χ2/df < 2.55 All analyses were carried out using Mplus 5.0 software.56
The measurement model specified one manifest variable (KAM), 5 latent mediators, and one latent outcome (MVPA). KAM was a binary indicator measured without error of whether the participant was randomly assigned to KAM (KAM=1) or UC (KAM=0). Separate latent factors representing self-efficacy, barriers, family support, and friends support were each indicated by the composites measured for each construct at 6, 12, and 24 months For example, the self-efficacy factor was the shared variance of self-efficacy composites measured at 6, 12, and 24 months. Because the enjoyment and self-concept latent factors were correlated at .89, a single latent factor, self-concept/enjoyment, was the common variance in the 3 enjoyment and 3 self-concept composites. The MVPA latent factor was constructed from the 6-, 12-, and 24-month MVPA kcal expenditure composites. Correlations across the 5 latent mediators and between mediators measured at the same point in time (eg, barriers at 6m with enjoyment at 6m) were freely estimated to account for covariance in these measures arising from contemporaneous measurement that was independent of the structural relationships.
The structural model specified that paths be estimated from KAM to each of the 5 mediators (self-efficacy a1, barriers a2, self-concept/enjoyment a3, family support a4, friend support a5); from self-efficacy to barriers (a6) and to self-concept/enjoyment (a7); from each mediator to MVPA (self-efficacy b1, barriers b2, self-concept/enjoyment b3, family support b4, friend support b5); and from KAM to MVPA (c and c’). The a and c paths thus estimate between-groups differences in the latent mediator and outcome factors indicated by the 6-, 12-, and 24-month composites. The c path estimated the direct effect of KAM on MVPA whereas c’ estimated the residual direct effect once the hypothesized mediational effects were estimated. The mediation effects estimated by the a4-b4 and a5-b5 assessed whether KAM increased the extent to which participants relied on the social support offered by friends and family that helped them maintain PA. The endogenous mediation effects estimated by a1-a6-b2 and a1-a7-b3 assessed whether KAM increased perceptions of self-efficacy; which in turn was related to reducing perceived barriers to exercise or to incorporating activity and its enjoyment into the self-concept; and fewer barriers and activity being more central to the self-concept predictive of increased activity.
RESULTS
The participants were on average about 57 years old (M=57.1, SD=5.1) and tended to be female (72.4%), non-Hispanic white (93.0%), and overweight (MBMI = 27.6, SD=5.4). KAM participants relative to UC participants were less likely to be non- Hispanic white (91.0% vs 94.9%, P<.05), with no other significant between-groups differences in demographic characteristics. In general, there was excellent fidelity to the intervention as well as study retention. Eighty-two percent of the participants randomized to the KAM intervention completed the core components of the intervention, and 92–94% of the randomized participants completed follow-up surveys at 6, 12, or 24 months. A more detailed description of study participants and the KAM consort diagram are provided elsewhere.11,38
In the measurement model, the indicators for each construct loaded strongly on the intended latent factor, without any estimated cross-loadings, and were consistent over time. The median magnitude of correlations among the mediating latent factors was −.12 (barriers with social support from family) and ranged from .07 (self-efficacy with social support from family) to −.40 (barriers with self-concept/enjoyment). The means and standard deviations of the measured variables are shown in Table 1, and a table of correlations among the measured variables and factor loadings of each indicator is available from the first author.
Table 1.
Mean and Standard Deviations for Mediator and MVPA Composites at Baseline and 6, 12 and 24 Months Postrandomization
| B | 6 | 12 | 24 | |||
|---|---|---|---|---|---|---|
| Self-efficacy | KAM | Mean | 2.80 | 2.97 | 2.95 | 2.98 |
| SD | 0.87 | 0.88 | 0.86 | 0.89 | ||
| UC | Mean | 2.80 | 2.79** | 2.88 | 2.80** | |
| SD | 0.91 | 0.93 | 0.91 | 0.97 | ||
| Barriers to Exercise | KAM | Mean | 2.40 | 2.28 | 2.26 | 2.22 |
| SD | 0.69 | 0.69 | 0.68 | 0.66 | ||
| UC | Mean | 2.38 | 2.33 | 2.28 | 2.29 | |
| SD | 0.68 | 0.72 | 0.70 | 0.74 | ||
| Self-concept | KAM | Mean | 3.84 | 3.98 | 4.01 | 4.00 |
| SD | 0.78 | 0.76 | 0.73 | 0.79 | ||
| UC | Mean | 3.86 | 3.81** | 3.87** | 3.81*** | |
| SD | 0.84 | 0.84 | 0.86 | 0.91 | ||
| Exercise Enjoyment | KAM | Mean | 4.08 | 4.11 | 4.16 | 4.19 |
| SD | 0.81 | 0.77 | 0.73 | 0.75 | ||
| UC | Mean | 4.12 | 4.03 | 4.07 | 4.04** | |
| SD | 0.83 | 0.83 | 0.82 | 0.90 | ||
| Social Support, Family | KAM | Mean | 2.82 | 2.91 | 2.91 | 2.94 |
| SD | 0.71 | 0.77 | 0.78 | 0.77 | ||
| UC | Mean | 2.73* | 2.75*** | 2.78** | 2.77*** | |
| SD | 0.73 | 0.77 | 0.75 | 0.80 | ||
| Social Support, Friends | KAM | Mean | 2.65 | 2.72 | 2.70 | 2.76 |
| SD | 0.70 | 0.73 | 0.73 | 0.75 | ||
| UC | Mean | 2.60 | 2.61* | 2.67 | 2.64** | |
| SD | 0.70 | 0.72 | 0.73 | 0.72 | ||
| MVPA | KAM | Mean | 1946 | 2054 | 2183 | 2280 |
| SD | 1548 | 1766 | 1856 | 2093 | ||
| UC | Mean | 2157* | 1838 | 1934** | 1903** | |
| SD | 1848 | 2117 | 1615 | 1699 | ||
KAM vs UC comparison:
P<.05,
P<.01,
P<.001
Prior to estimating the mediated relationships between KAM and MVPA, there was a significant positive effect of KAM on MVPA, βc =.105, z=2.90, P=.004. On average, KAM participants expended about .10 SD, or about 190, more kcal per week on moderate and vigorous activities over the 2-year follow-up period than did UC participants. Once the indirect effects were added, the estimated structural model was an excellent representation of the covariances among the measured variables, χ2(141)=282.11, χ2/df=2.0, CFI=.98, RMSEA=.031, R-square = .198. The direct KAM-MVPA relationship was no longer significant, and the strength of the standardized path coefficient was reduced by about 50%, βc’ =.052, z=1.52, P =.13. This difference suggests that about half of the efficacy of KAM in helping participants maintain PA may be attributed to the mediated KAM-MVPA relationships.
Table 2 displays how the total indirect effect is partitioned into the specific indirect effects that were estimated in the structural model. The total indirect effect of KAM on MVPA by way of the mediators was significant, total β=.050, z=3.23, P <.001. The significance (ie, β/se ≥ 1.96) of all but one of the structural KAM-mediator (a*) paths, and all of the mediator-MVPA paths (b*), demonstrates that being a KAM participant positively impacted constructs that are predictive of physical activity (see Figure 1). However, none of the singly mediated indirect effects, and only one of the multiply mediated indirect effects, was significant once the combined effects of the a*and b* paths were considered. The one significant indirect effect, βa1- a7-b3 =.009, z=1.99, P<.05, showed that KAM significantly increased self-efficacy (βa1 =.088, z=2.57, P=.01), self-efficacy was positively related to physical activity enjoyment and self-concept (βa7=.583, z=22.80, P<.001), and a stronger self-concept as a physically active person predicted more physical activity (βb3 =.174, z=3.19, P=.001).
Table 2.
Partitioning the Total Effect of KAM on MVPA Into Direct, Indirect, and Singly and Multiply Mediated Indirect Effects
| β | se | z | p | |
|---|---|---|---|---|
| Total effect | .105 | .036 | 2.90 | .004 |
| Direct effect | .052 | .034 | 1.52 | .13 |
| Indirect effects | .050 | .016 | 3.23 | .001 |
| Singly and multiply mediated indirect effects | ||||
| KAM-Self-efficacy-MVPA (a1–b1) | .012 | .007 | 1.69 | .09 |
| KAM-Barriers-MVPA (a2–b2) | −.004 | .004 | −0.99 | .32 |
| KAM-Self-concept-MVPA (a3–b3) | .010 | .006 | 1.75 | .08 |
| KAM-Family-MVPA (a4–b4) | .009 | .005 | 1.71 | .09 |
| KAM-Friends-MVPA (a5–b5) | .006 | .004 | 1.42 | .16 |
| KAM-Self-efficacy-Barriers-MVPA (a1- a6-b2) | .009 | .005 | 1.65 | .10 |
| KAM-Self-efficacy-Self-concept-MVPA (a1- a7-b3) | .009 | .004 | 1.99 | .05 |
DISCUSSION
The goal of these analyses was to build upon state-of-the art theory and empirical data regarding physical activity maintenance by testing mediational models of physical activity maintenance using data from the KAM physical activity maintenance trial, one of the few trials to date specifically focused on maintenance. Self-efficacy and the enjoyment and incorporation of activity into the self-concept emerged as key mediators of KAM on PA maintenance. Self-efficacy was the upstream variable in 2 endogenously mediated effects, through perceived barriers to PA and incorporation of PA into the self-concept. The self-concept/enjoyment mediator emerged as the strongest predictor of PA and was thus figural in 2 indirect effects (ie, KAM – self-concept/enjoyment – MVPA; KAM – self-efficacy – self-concept/enjoyment – MVPA).
The role of self-efficacy in PA initiation is well documented, and it may have promoted PA maintenance in much the same manner as it promotes initiation. We assert that the KAM intervention enhanced self-efficacy by encouraging participants to identify ways to use multiple available resources, such as social support and their own problem-solving skills, to prevent relapse. Employing these strategies may have helped participants maintain short-term PA by successfully anticipating and preventing relapse, or by re-initiating activity after a brief relapse or reduction in activity.
We speculate that the enjoyment of activity and its integration into the self-concept may serve a function that is more specific to PA maintenance and has not, to date, received as much empirical attention in this literature. Several psychological processes could explain why engaging in PA could increase the likelihood that participants transitioned from thinking about PA as a behavior that they do – in which case the extrinsic costs, benefits, and barriers are more likely to exert influence on the likelihood of doing the behavior – to perceiving themselves as physically active people who enjoy being active. This transition may mean that the benefits of PA are more likely to be intrinsic23,33,41 and that engaging in PA says something about who they are. As an example, more frequent activity may have become a more salient piece of self-relevant information and included in the working self-concept; or the implications of repeated PA may have been internalized to bring about perceptions of consistency between behavior and the self-concept particularly if there is an interpersonal component of having engaged in the behavior, such as relying on a social network to support PA, having a workout buddy; or discussing plans for PA with an activity coach. Once incorporated, the self-concept may perpetuate long-term PA through well-documented processes such as dissonance or self-discrepancy reduction or self-verification. There is modest evidence that the relationship between intention to exercise and number of bouts of exercise is stronger among people for whom exercise is self-descriptive and important57 and that self-engagement predicts intentions to engage in healthful behaviors.58
These analyses highlight self-efficacy, self-concept integration, and enjoyment of PA as key candidates for further research on PA maintenance. Integration of PA into the self-concept and enjoyment of PA were not empirically distinct in these data, possibly due to the likelihood that people enjoy behaviors that reinforce a valued aspect of the self-concept. Future research would benefit from disentangling these empirically related but conceptually distinct factors. Perceived barriers to PA were not directly affected by the KAM intervention but, similar to previous work investigating the transition from PA initiation to maintenance, played an intervening role in predicting MVPA. Social support from family and social support from friends were not especially strong performers in these analyses although future research should confirm or refute their relative importance to PA maintenance. The relative importance of other constructs that have been studied in the PA initiation literature but were not included here (eg, satisfaction, psychological and fitness benefits, goal setting, motivation, self- management strategies) also warrant further attention.
The total indirect effect was statistically and practically significant. However, the facts that only one of the 7 estimated indirect effects was statistically significant and that all of the individual indirect effects were quite small demonstrate that appropriately incorporating the multitude and timing of mechanisms that work in concert to promote PA maintenance may require more complicated conceptual models than those that have been put forth to explain PA initiation. We assert that PA maintenance be conceptualized as a process that includes a multitude of small yet interrelated mediational pathways from behavior initiation to maintenance. Thus, we propose that no single mediator or indirect effect is at the heart of successful long-term maintenance and that effective maintenance models should capture recursive relationships among mediators and outcomes.
The theoretical frameworks from which the KAM intervention was developed and the literature that guided our selection of mediators explicitly address singly mediated pathways (ie, intervention – mediator – outcome). For the purposes of explaining long-term maintenance they can and should be expanded to accommodate multiple linkages between intervention and outcomes, including those in which mediators and outcomes predict each other over the course of time (eg, KAM intervention – t2 self-efficacy– t3 MVPA– t4 self-concept– t5 MVPA).59,60 Likewise, the interrelationships among mediators should not be overlooked as theories specific to activity maintenance are further developed and empirically tested.23
KAM focused on helping participants engage in cognitions and behaviors conducive to PA. If we consider that continued engagement in PA helps sustain the image of oneself as an active individual, it seems just as plausible to posit that continued participation in activities or perseveration on aspects of the self that are counterproductive or inconsistent with the development and sustenance of an “active” self-concept may pose a threat to PA maintenance. Thus, an alternative target for intervention might be to identify and address specific components of self-concept that inhibit individuals from integrating PA into the self-concept.
A limitation of the analytic approach lies in how repeated measures were incorporated into the structural model. Each latent factor was constructed as the common variance in a construct measured across 3 points in time, which effectively removed temporal order from the mediator to MVPA structural paths (b1 – b5). This measurement approach makes it impossible to assert temporality in the mediator-MVPA structural paths, only that the mediators and MVPA are related, because the mediator and outcome factors are aggregates of the 6-, 12-, and 24-month composites. At this relatively early stage of identifying mediators important to PA maintenance, and in the absence of time-specific a priori hypotheses to guide model specification, we determined that this limitation was acceptable.
We believe that these are some of the first empirical findings that bring integration of PA into the self-concept to light as an important determinant of long-term PA maintenance. These analyses provided empirical evidence to inform further development of conceptual frameworks to explain long-term behavioral maintenance that incorporate complex mediational paths between behavior initiation and long-term maintenance. Future empirical work would be well served by a priori hypotheses that guide when multiple mediators and outcomes are assessed, their placement relative to each other in a structural model, and the personal characteristics that could moderate the hypothesized processes.
ACKNOWLEDGMENTS
This study was supported by a grant from the National Institute on Aging (R01 AG023410). We would like to thank Marcia Hayes for her professionalism in managing this project, and Karen Speicher, Jessica Boerboom, Colleen Flattum, and Stephanie Williams for their invaluable contributions as KAM telephone coaches.
Contributor Information
A. Lauren Crain, Email: Lauren.A.Crain@HealthPartners.Com, 952-967-5354, HealthPartners Research Foundation, Mail Stop 21111R, PO Box 1524, Minneapolis, MN 55440-1524, fax: 952-967-5022.
Brian C. Martinson, Email: Brian.C.Martinson@HealthPartners.Com, 952-967-5021, HealthPartners Research Foundation, Mail Stop 21111R, PO Box 1524, Minneapolis, MN 55440-1524, fax: 952-967-5022.
Nancy E. Sherwood, Email: Nancy.E.Sherwood@HealthPartners.Com, 952-967-7303, HealthPartners Research Foundation, Mail Stop 21111R, PO Box 1524, Minneapolis, MN 55440-1524, fax: 952-967-5022.
Patrick J. O’Connor, Email: Patrick.J.Oconnor@HealthPartners.Com, 952-967-5034, HealthPartners Research Foundation, Mail Stop 21111R, PO Box 1524, Minneapolis, MN 55440-1524, fax: 952-967-5022.
REFERENCES
- 1.Physical Activity Guidelines Advisory Committee. Physical Activity Guidelines Advisory Committee Report. Washington, DC: U.S. Department of Health and Human Services; 2008. [DOI] [PubMed] [Google Scholar]
- 2.Angevaren M, Aufdemkampe G, Verhaar H, et al. Physical activity and enhanced fitness to improve cognitive function in older people without known cognitive impairment. Cochrane Database Syst Rev. 2008;(2) doi: 10.1002/14651858.CD005381.pub2. CD005381. [DOI] [PubMed] [Google Scholar]
- 3.Weuve J, Kang JH, Manson JE, et al. Physical activity, including walking, and cognitive function in older women. JAMA. 2004;292(12):1454–1461. doi: 10.1001/jama.292.12.1454. [DOI] [PubMed] [Google Scholar]
- 4.Liu-Ambrose T, Donaldson MG, Ahamed Y, et al. Otago Home-based strength and balance retraining improves executive functioning in older fallers: a randomized controlled trial. J Am Geriatr Soc. 2008;56(10):1821–1830. doi: 10.1111/j.1532-5415.2008.01931.x. [DOI] [PubMed] [Google Scholar]
- 5.Feskanich D, Willett W, Colditz G. Walking and leisure-time activity and risk of hip fracture in postmenopausal women. JAMA. 2002;288(18):2300–2306. doi: 10.1001/jama.288.18.2300. [DOI] [PubMed] [Google Scholar]
- 6.Hughes SL, Seymour RB, Campbell R, et al. Impact of the fit and strong intervention on older adults with osteoarthritis. Gerontologist. 2004;44(2):217–228. doi: 10.1093/geront/44.2.217. [DOI] [PubMed] [Google Scholar]
- 7.McAuley E, Konopack JF, Motl RW, et al. Physical activity and quality of life in older adults: influence of health status and self-efficacy. Ann Behav Med. 2006;31(1):99–103. doi: 10.1207/s15324796abm3101_14. [DOI] [PubMed] [Google Scholar]
- 8.Elavsky S, McAuley E, Motl RW, et al. Physical activity enhances long-term quality of life in older adults: efficacy, esteem, and affective influences. Ann Behav Med. 2005;30(2):138–145. doi: 10.1207/s15324796abm3002_6. [DOI] [PubMed] [Google Scholar]
- 9.King AC, Pruitt LA, Woo S, et al. Effects of moderate-intensity exercise on polysomnographic and subjective sleep quality in older adults with mild to moderate sleep complaints. J Gerontol A Biol Sci Med Sci. 2008;63(9):997–1004. doi: 10.1093/gerona/63.9.997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vallance JK, Courneya KS, Plotnikoff RC, et al. Randomized controlled trial of the effects of print materials and step pedometers on physical activity and quality of life in breast cancer survivors. J Clin Oncol. 2007;25(17):2352–2359. doi: 10.1200/JCO.2006.07.9988. [DOI] [PubMed] [Google Scholar]
- 11.Martinson BC, Crain AL, Sherwood NE, et al. Maintaining physical activity among older adults: six-month outcomes of the Keep Active Minnesota randomized controlled trial. Prev Med. 2008;46(2):111–119. doi: 10.1016/j.ypmed.2007.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Baranowski T, Anderson C, Carmack C. Mediating variable framework in physical activity interventions. How are we doing? How might we do better? Am J Prev Med. 1998;15(4):266–297. doi: 10.1016/s0749-3797(98)00080-4. [DOI] [PubMed] [Google Scholar]
- 13.Lewis BA, Marcus BH, Pate RR, et al. Psychosocial mediators of physical activity behavior among adults and children. Am J Prev Med. 2002;23 Suppl 2:S26–S35. doi: 10.1016/s0749-3797(02)00471-3. [DOI] [PubMed] [Google Scholar]
- 14.Williams DM, Papandonatos GD, Napolitano MA, et al. Perceived enjoyment moderates the efficacy of an individually tailored physical activity intervention. J Sport Exerc Psychol. 2006;28(3):300–309. [Google Scholar]
- 15.Napolitano MA, Papandonatos GD, Lewis BA, et al. Mediators of physical activity behavior change: a multivariate approach. Health Psychol. 2008;27(4):409–418. doi: 10.1037/0278-6133.27.4.409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Williams D, Lewis B, Dunsiger S, et al. Comparing psychosocial predictors of physical activity adoption and maintenance. Ann Behav Med. 2008;36(2):186–194. doi: 10.1007/s12160-008-9054-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Brassington GS, Atienza AA, Perczek RE, et al. Intervention-related cognitive versus social mediators of exercise adherence in the elderly. Am J Prev Med. 2002;23 Suppl 2:S80–S86. doi: 10.1016/s0749-3797(02)00477-4. [DOI] [PubMed] [Google Scholar]
- 18.Miller YD, Trost SG, Brown WJ. Mediators of physical activity behavior change among women with young children. Am J Prev Med. 2002;23(2) Supple 1:S98–S103. doi: 10.1016/s0749-3797(02)00484-1. [DOI] [PubMed] [Google Scholar]
- 19.Bauman AE, Sallis JF, Dzewaltowski DA, et al. Toward a better understanding of the influences on physical activity: the role of determinants, correlates, causal variables, mediators, moderators, and confounders. Am J Prev Med. 2002;23 Suppl 2:S5–S14. doi: 10.1016/s0749-3797(02)00469-5. [DOI] [PubMed] [Google Scholar]
- 20.King AC, Stokols D, Talen E, et al. Theoretical approaches to the promotion of physical activity: forging a transdisciplinary paradigm. Am J Prev Med. 2002;23 Suppl 1:S15–S25. doi: 10.1016/s0749-3797(02)00470-1. [DOI] [PubMed] [Google Scholar]
- 21.Heesch KC, Masse LC, Dunn AL. Using Rasch modeling to re-evaluate three scales related to physical activity: enjoyment, perceived benefits and perceived barriers. Health Educ Res. 2006 doi: 10.1093/her/cyl054. [DOI] [PubMed] [Google Scholar]
- 22.Cerin E, Vandelanotte C, Leslie E, et al. Recreational facilities and leisure-time physical activity: an analysis of moderators and self-efficacy as a mediator. Health Psychol. 2008;27(2) Suppl:S126–S135. doi: 10.1037/0278-6133.27.2(Suppl.).S126. [DOI] [PubMed] [Google Scholar]
- 23.Nigg CR, Borrelli B, Maddock J, et al. A theory of physical activity maintenance. Applied Psychology: An International Review. 2008;57(4):544–560. [Google Scholar]
- 24.McAuley E, Morris KS, Motl RW, et al. Long-term follow-up of physical activity behavior in older adults. Health Psychol. 2007;26(3):375–380. doi: 10.1037/0278-6133.26.3.375. [DOI] [PubMed] [Google Scholar]
- 25.Williams PT. Maintaining vigorous activity attenuates 7-yr weight gain in 8340 runners. Med Sci Sports Exerc. 2007;39(5):801–809. doi: 10.1249/mss.0b013e31803349b1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hughes SL, Seymour RB, Campbell RT, et al. Long-term impact of fit and strong! On older adults with osteoarthritis. Gerontologist. 2006;46(6):801–814. doi: 10.1093/geront/46.6.801. [DOI] [PubMed] [Google Scholar]
- 27.McAuley E, Jerome GJ, Elavsky S, et al. Predicting long-term maintenance of physical activity in older adults. Prev Med. 2003;37(2):110–118. doi: 10.1016/s0091-7435(03)00089-6. [DOI] [PubMed] [Google Scholar]
- 28.Lewis BA, Forsyth LH, Pinto BM, et al. Psychosocial mediators of physical activity in a randomized controlled intervention trial. J Sport Exerc Psychol. 2006;28(2):193–204. [Google Scholar]
- 29.Dishman RK, Motl RW, Saunders R, et al. Self-efficacy partially mediates the effect of a school-based physical-activity intervention among adolescent girls. Prev Med. 2004;38(5):628–636. doi: 10.1016/j.ypmed.2003.12.007. [DOI] [PubMed] [Google Scholar]
- 30.Cerin E, Taylor LM, Leslie E, et al. Small-scale randomized controlled trials need more powerful methods of mediational analysis than the Baron-Kenny method. J Clin Epidemiol. 2006;59(5):457–464. [Google Scholar]
- 31.Dishman RK, Motl RW, Saunders R, et al. Enjoyment mediates effects of a school-based physical-activity intervention. Med Sci Sports Exerc. 2005 March;37(3):478–487. doi: 10.1249/01.mss.0000155391.62733.a7. [DOI] [PubMed] [Google Scholar]
- 32.Pinto B, Lynn H, Marcus B, et al. Physician-based activity counseling: intervention effects on mediators of motivational readiness for physical activity. Ann Behav Med. 2001;23(1):2–10. doi: 10.1207/S15324796ABM2301_2. [DOI] [PubMed] [Google Scholar]
- 33.Rothman AJ. Toward a theory-based analysis of behavioral maintenance. Health Psychol. 2000;19 Suppl 1:S64–S69. doi: 10.1037/0278-6133.19.suppl1.64. [DOI] [PubMed] [Google Scholar]
- 34.Neff KL, King AC. Exercise program adherence in older adults: the importance of achieving one’s expected benefits. Med Exerc Nutr Health. 1995;4:355–362. [Google Scholar]
- 35.Dishman RK, Motl RW, Sallis JF, et al. Self-management strategies mediate self-efficacy and physical activity. Am J Prev Med. 2005;29(1):10. doi: 10.1016/j.amepre.2005.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bock BC, Marcus BH, Pinto BM, et al. Maintenance of physical activity following an individualized motivationally tailored intervention. Ann Behav Med. 2001;23(2):79–87. doi: 10.1207/S15324796ABM2302_2. [DOI] [PubMed] [Google Scholar]
- 37.Martinson BC, Crain AL, Sherwood NE, et al. Population reach and recruitment bias in a maintenance RCT in physically active older adults. J Phys Activ Health. 2010;7(1):127–135. doi: 10.1123/jpah.7.1.127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sherwood NE, Martinson BC, Crain AL, et al. A new approach to physical activity maintenance: rationale, design, and baseline data from the Keep Active Minnesota trial. BMC Geriatr. 2008 July 25;8:17. doi: 10.1186/1471-2318-8-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Dishman RK, Ickes W, Morgan WP. Self-motivation and adherence to habitual physical activity. J Appl Soc Psychol. 1980;10:115–132. [Google Scholar]
- 40.Motl RW, Dishman RK, Felton G, et al. Self-motivation and physical activity among black and white adolescent girls. Med. Sci. Sports Exerc. 2003;35(1):128–136. doi: 10.1097/00005768-200301000-00020. [DOI] [PubMed] [Google Scholar]
- 41.Chatzisarantis NLD, Hagger MS. The moral worth of sport reconsidered: contributions of recreational sport and competitive sport to life aspirations and psychological well-being. J Sports Sci. 2007;25(9):1047. doi: 10.1080/02640410600959954. [DOI] [PubMed] [Google Scholar]
- 42.King AC, Castro C, Wilcox S, et al. Personal and environmental factors associated with physical inactivity among different racial-ethnic groups of U.S. middle-aged and older-aged women. Health Psychol. 2000;19(4):354–364. doi: 10.1037//0278-6133.19.4.354. [DOI] [PubMed] [Google Scholar]
- 43.Sallis JF, Prochaska JJ, Taylor WC. A review of correlates of physical activity of children and adolescents. Med Sci Sports Exerc. 2000;32(5):963–975. doi: 10.1097/00005768-200005000-00014. [DOI] [PubMed] [Google Scholar]
- 44.Salmon J, Owen N, Crawford D, et al. Physical activity and sedentary behavior: A population-based study of barriers, enjoyment, and preference. Health Psychol. 2003;22(2):178–188. doi: 10.1037//0278-6133.22.2.178. [DOI] [PubMed] [Google Scholar]
- 45.Brawley LR, Rejeski WJ, King AC. Promoting physical activity for older adults: the challenges for changing behavior. Am J Prev Med. 2003;25(3) Suppl 2:S172–S183. doi: 10.1016/s0749-3797(03)00182-x. [DOI] [PubMed] [Google Scholar]
- 46.Bandura A. Social Foundations of Thought and Action: A social cognitive theory. Englewood Cliffs, NJ: Prentice Hall; 1986. [Google Scholar]
- 47.Bandura A. Health promotion by social cognitive means. Health Educ Behav. 2004;31(2):143–164. doi: 10.1177/1090198104263660. [DOI] [PubMed] [Google Scholar]
- 48.Marlatt GA, Gordon JR. Relapse prevention: maintenance strategies in the treatment of addictive behaviors. New York: Guilford Press; 1985. [Google Scholar]
- 49.Stewart AL, Mills KM, King AC, et al. CHAMPS physical activity questionnaire for older adults: outcomes for interventions. Med Sci Sports Exerc. 2001;33(7):1126–1141. doi: 10.1097/00005768-200107000-00010. [DOI] [PubMed] [Google Scholar]
- 50.McAuley E. Self-efficacy and the maintenance of exercise participation in older adults. J Behav Med. 1993;16:103–113. doi: 10.1007/BF00844757. [DOI] [PubMed] [Google Scholar]
- 51.Jeffery RW, Wing RR, Thorson C, et al. Use of personal trainers and financial incentives to increase exercise in a behavioral weight-loss program. J Consult Clin Psychol. 1998 October;66(5):777–783. doi: 10.1037//0022-006x.66.5.777. [DOI] [PubMed] [Google Scholar]
- 52.Robert WM, Rod KD, Ruth S, et al. Measuring enjoyment of physical activity in adolescent girls. Am J Prev Med. 2001;21(2):110–117. doi: 10.1016/s0749-3797(01)00326-9. [DOI] [PubMed] [Google Scholar]
- 53.Brewer BW, Van Raalte J, Linder DE. Athletic identity: Hercules’ muscle or Achilles heel? Int J Sport Psychol. 1993;24:237–254. [Google Scholar]
- 54.Sallis JF, Grossman RM, Pinski RB, et al. The development of scales to measure social support for diet and exercise behaviors. Prev Med. 1987;16:825–836. doi: 10.1016/0091-7435(87)90022-3. [DOI] [PubMed] [Google Scholar]
- 55.Hu L, Bentler PM. Cutoff criteria for fit indices in covariance structure analyses: conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal. 1999;6:1–55. [Google Scholar]
- 56.Muthén BO, Muthén L. Mplus User’s Guide. 5th ed. Los Angeles, CA: Author; 2007. [Google Scholar]
- 57.Sheeran P, Orbell S. Self-schemas and the theory of planned behaviour. Eur J Soc Psychol. 2000;30(4):533–550. [Google Scholar]
- 58.Pierro A, Mannetti L, Livi S. Self-identity and the theory of planned behavior in the prediction of health behavior and leisure activity. Self Ident. 2003;2(1):47–60. [Google Scholar]
- 59.Chanal JP, Marsh HW, Sarrazin PG, et al. The big-fish-little-pond effect on gymnastics self-concept: generalizability of social comparison effects to a physical setting. J Sport Exerc Psychol. 2005;27:53–70. [Google Scholar]
- 60.Marsh HW, Byrne BM, Yeung AS. Causal ordering of academic self-concept and achievement: reanalysis of a pioneering study and revised recommendations. Educ Psychol. 1999;34:155–167. [Google Scholar]