Abstract
Purpose
The aim of this study was to evaluate the surgical outcomes of abdominal total gastrectomy, without mediastinal lymph node dissection for type II and III gastroesophageal junction (GEJ) cancers.
Materials and Methods
We retrospectively reviewed surgical outcomes in 67 consecutive patients with type II and III GEJ cancers that were treated by the surgical resection between 2004 and 2008.
Results
Thirty (45%) patients had type II and 37 (55%) had type III tumor. Among the 65 (97%) patients with curative surgery, 21 (31%) patients underwent the extended total gastrectomy with trans-hiatal distal esophageal resection, and in 44 (66%) patients, abdominal total gastrectomy alone was done. Palliative gastrectomy was performed in two patients due to the accompanying peritoneal metastasis. The postoperative morbidity and mortality rates were 21.4% and 1.5%, respectively. After a median follow up of 36 months, the overall 3-years was 68%, without any differences between the Siewert types or the operative approaches (transhiatal approach vs. abdominal approach alone). On the univariate analysis, the T stage, N stage and R0 resection were found to be associated with the survival, and multivariate analysis revealed that the N stage was a poor independent prognostic factor for survival.
Conclusions
Type II and III GEJ cancers may successfully be treated with the abdominal total gastrectomy, without mediastinal lymph node dissection in the Korean population.
Keywords: Surgery, Esophagogastric junction, Stomach neoplasms, Korea
Introduction
Despite the decreasing global incidence of gastric cancer, the gastroesophageal junction (GEJ) cancers have greatly increased in the Western countries.(1) However, distal gastric cancer is still a predominant type among gastric cancers in Korea and Japan(2,3) and patients are often diagnosed at an early stage with the use of endoscopy for mass screening.(4-6) Besides, the epidemiology of GEJ cancers is also quite different from that of the West, in which type I GEJ cancer is extremely rare, while type II and III account for the types of the GEJ cancers in Korea.
Although achieving complete tumor resection (R0 resection) is the mainstay of surgical treatment for GEJ cancers, the operative approaches, especially regarding the need for thoracotomy, still remain controversial.(7) Because of the frequent tumor infiltration, at least 6 cm of grossly normal esophageal resection has been advocated by several groups to achieve negative resection margins in the West.(8-10) Some investigators have even insisted that as long as 10 cm of esophageal resection is required to minimize the risk of positive proximal margins.(11,12) To secure these long proximal resection margins, thoracotomy often should be performed along with abdominal total gastrectomy. Possible metastasis to the mediastinal lymph nodes is another concern necessitating thoracotomy in GEJ cancer. However, the relationship between the operative approaches and survival still remains to be investigated.
Although GEJ cancer are surgically treated as another entity of esophageal cancer in the West, the surgical approach to GEJ cancers in Korea is just similar to that for gastric cancer, in which abdominal total gastrectomy without mediastinal lymph node dissection is commonly performed. To date, there were few case and study about the evaluation of the outcome of abdominal total gastrectomy in GEJ cancer in asia. In this study, we evaluated the surgical outcomes of abdominal total gastrectomy with the selective transhiatal approach that was perform for type II and III GEJ cancers to establish the optimal operative approach for these tumors and to define the prognostic factors. The aim of this study was to evaluate the short term and the long term results of the surgical procedure that was removal of complete tumor margin with the selective transhiatal approach or not.
Materials and Methods
1. Patients
From 2004 to 2008, 1775 patients underwent surgery for gastric carcinoma at our institution. By reviewing the operation record, pathological reports, and surgical specimen pictures, 67 (3.8%) patients with type II and III GEJ cancers and who were treated by surgical resection were included in this study. GEJ cancers were defined as tumors whose center was within 5 cm proximal and distal of the anatomical cardia, and were classified according to the Siewert's classification of GEJ cancer.(13)
All patients were preoperatively evaluated with endoscopy along with biopsy, abdominal computed tomography (CT) scanning, and a barium swallow study. Endoscopic ultrasound was performed in selected cases. None of the patients in this study received chemotherapy or radiation therapy before the operation. After operation, the patients were followed up every six months for the first three years, and then every 12 months after that. Disease recurrence was detected by physical examination, tumor markers, endoscopy and abdominal CT scanning.
The data regarding the patient demographics, the operative procedures, the pathologic results and the short-term surgical outcomes was obtained from a retrospective review of the medical records. The histologic differentiation and staging were principally based on the 6th edition of the International Union Against Cancer TNM classification for gastric carcinoma.(14) The information regarding disease recurrence and survival were obtained during outpatient clinical visits and by telephone interviews.
2. Operative procedures
The choice of surgical approach was based on the goal of achieving complete macroscopic and microscopic tumor resection. In general, abdominal total gastrectomy was performed with resection of the distal esophagus with at least 3 cm of a gross surgical margin from the tumor. The transhiatal approach was performed in selected cases where complete resection was less likely to be achieved with the abdominal approach alone, based on the preoperative examinations or the intraoperative findings. Intraoperative frozen section analysis was performed in every operation, and the adequacy of the extent of esophageal resection was confirmed. For most patients, D2 lymph node dissection was performed as a standard procedure as is outlined by the principles of the Japanese Classification of Gastric Carcinoma.(15) And mediastinal lymph node dissection was not undertaken in this study.
The mode of reconstruction was mechanical esophagojejunostomy or jejunal interposition, and the mode was selected according to the surgeon's preference.
3. Statistics
Statistical analysis was performed using the software SPSS version 12.0 statistical package for windows (SPSS Inc., Chicago, IL, USA). Chi-square tests or Fisher's exact tests and the student's t-test were used for comparisons as appropriate. Patient survival was calculated using the Kaplan-Meier method and the patient survival between groups was compared using the log rank test. Univariate and multivariate analysis were performed using the Cox regression models to identify the prognostic factors. A P-value <0.05 was considered statistically significant throughout the study.
Results
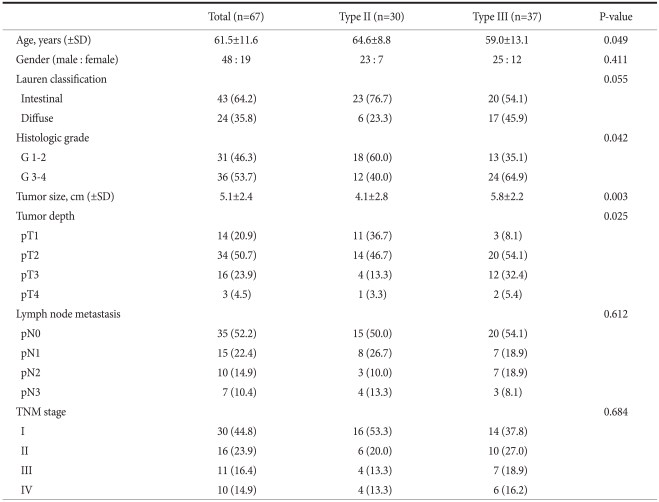
The patients consisted of 48 men and 19 women with a mean age of 61.5±11.6 years. The tumor location described in the final pathologic report was based on Siewert classification, and this revealed 30 type II and 37 type III tumors. No significant differences were observed between the type II and III tumors with respect to gender, Lauren's classification, the N stage, and the presence of Barrett's esophagus (Table 1). However, there were significant differences in age, the histologic grade, the tumor size, and the T stage between the two groups: an older age, more histologic grade G1/2 tumors, a smaller tumor size, and more pT1/2 stage tumors were the specific features of the type II tumors.
Table 1.
The clinicopathological features of the GEJ cancers
The numbers in parenthesis are percentages. TNM stage is based on the sixth edition of UICC/AJCC TNM classification. GEJ = gastroesophageal junction; SD = standard deviation; UICC = International Union Against Cancer; AJCC = American Joint Committee on Cancer.
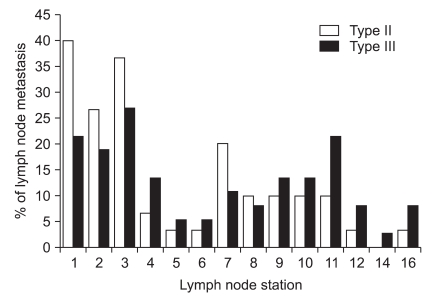
With respect to lymph node metastasis, both tumor types showed similar patterns of lymphatic spread. For both types of tumor, lymph nodes number 1, 2 and 3 were the most commonly involved lymph nodes, with spreading toward the celiac lymph nodes (Fig. 1).
Fig. 1.
Lymph node metastasis at each regional station in the patients with type II and III tumors. These two tumor types had similar patterns of lymphatic spread, with most commonly involving the lymph node station 1, 2, and 3 nodes and the spread was directed toward the celiac nodes.
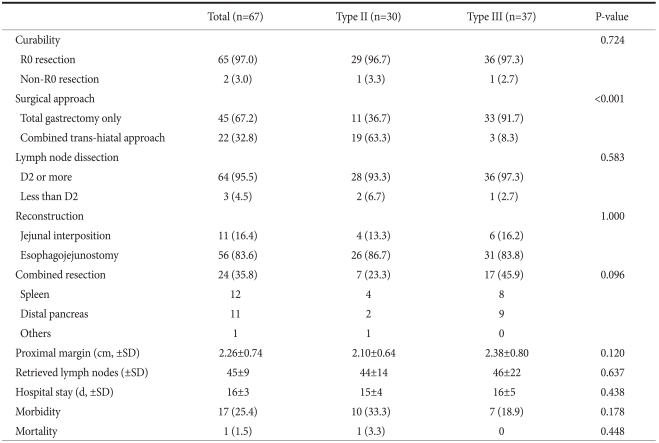
1. Surgical outcomes
Of the 67 patients, 65 (97.0%) patients underwent surgery with a curative intent, and two patients underwent palliative gastrectomy due to disseminated peritoneal metastasis. Twenty-two (33%) patients required the transhiatal approach for securing esophageal resection margin, while 45 (67%) patients required the abdominal approach only (Table 2). As a result, the transhiatal approach was performed for 19 (63%) of the 30 type II tumors and for 3 (8%) of the 37 type III tumors. The mean proximal margin length (cm) was 2.26±0.74 (range: 1.0~4.0 cm), and none of the patients revealed residual tumor cells at the esophageal resection margin. Combined spleen or pancreas resection was performed in 24 (35.8%) patients. Sixty-four (95.5%) patients underwent lymphadenectomy of more than D2, and the mean number of harvested lymph nodes was 45±9.
Table 2.
The surgical outcomes
The numbers in parenthesis are percentages. SD = standard deviation.
A total of 17 (25.4%) patients developed postoperative complications with one in-hospital death. The most common complication was pancreatic fistula (n=5) and this was followed by abdominal infection (n=4), and surgical wound infection (n=2). The mean hospital stay (in days) was 16±3.
2. Survival and the prognostic factors
With a median follow-up of 36 months (range: 13 to 58 months), the overall survival rate at 3 years was 68%: it was 70% for patients with type II tumors versus 67% for the patients with type III tumors (P=0.546), and 72% for the transhiatal approach vs. 66% for the abdominal approach alone (P=0.811). A total of 14 patients developed recurrence during the follow up: there were 11 cases of peritoneal seeding, 3 cases of distant lymph node metastases, 2 cases of hematogenous metastases and 4 cases of locoregional recurrences. No patients had recurrence at the mediastinal lymph nodes during the follow-up. Meanwhile, no significant difference of the recurrence pattern was observed according to the Siewert types or the surgical approaches.
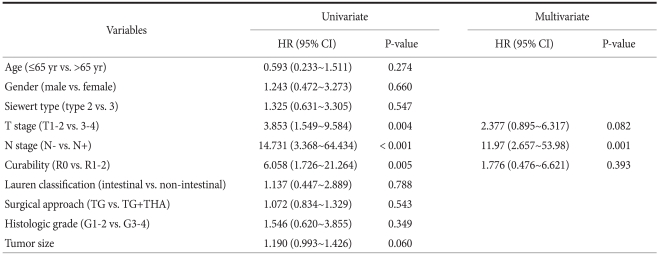
On the univariate analysis, the T stage (T1-2 vs. T3-4), N stage (N0 vs. N+) and R0 resection were significantly associated with survival, while the Siewert type or the transhiatal approach was not. Multivariate analysis of the significant variables on the univariate analysis showed that lymph node metastasis (hazard ratio=11.97, 95% confidence interval=2.657~63.98) was an independent factor for a poor prognosis (Table 3).
Table 3.
The prognostic factors on the univariate and multivariate analysis
HR = hazard ration; CI = confidence interval; TG = total gastrectomy; THA = transhiatal approach.
Discussion
Adenocarcinomas of the GEJ are biologically aggressive and they are typically diagnosed at an advanced stage of disease progression. As a result, they are difficult to treat and the patient prognosis is poor even after curative surgical resection. The five-year survival rate after surgical resection has been reported to range only 16% to 32.3%.(11,16,17) Although such reports are rare, the GEJ cancers in East Asia show significant differences of their clinicopathological features as compared with those observed in the West. First, its incidence is very low despite of the high prevalence of gastric cancer. Second, distal esophageal adenocarcinomas related to Barrett's mucosa (type I GEJ cancer) are rarely seen, and most GEJ cancers arise in the gastric cardia or subcardial region. Third, patients in these areas are often diagnosed at an early stage of disease because of the widespread use of endoscopy screening.(4-6) Thus, considering these distinctive features, abdominal total gastrectomy is frequently performed for GEJ cancers in Korea, rather than thoraco-abdominal approach in the West, but only a few studies have reported surgical outcomes of this procedure. This study shows that abdominal total gastrectomy with selective trans-hiatal approach is appropriate in terms of securing safe proximal resection margin and acceptable postoperative morbidity. Besides, long term outcomes were also similar to the historical controls.
Achieving complete tumor resection is the mainstay of the surgical treatment for GEJ cancers. The surgical approaches to achieve R0 resection for these tumors vary widely from esophagectomy through the transthoracic or transmediastinal approach to extended total gastrectomy with transhiatal resection.(18) Because of the frequent tumor infiltration at the esophageal resection margin, extended esophageal resection has been advocated by several research groups. Ito et al.(9) recommended that the surgical approach should be directed based on the goal of obtaining at least 6 cm of a gross proximal resection margin to avoid residual cancer cells at the resection margin, and this was generally consistent with that reported by Barbour et al.,(19) Bezzetti et al.,(8) and Mattioli et al.(10) However, most series have not demonstrated a survival benefit for one operative approach over another,(20,21) and proximal resection margin infiltration does not universally translate to poor survival when performing curative resection.(22)
In general, it has been well accepted that the selection of the surgical approach to GEJ cancers should be tailored based upon achieving macroscopic and microscopic tumor resection.(23) In this study, with performing grossly normal esophageal resection of only 3 cm, complete (R0) tumor resection was performed in as many as 97% of the patients. The rate of R0 resection of this study was considerably higher than those studies in the West that reported a 55% to 75% rate of complete resection.(9,19,24) Unlike the strong correlation of a positive resection margin with the extent of the surgical resection as observed by Mattioli et al.,(10) our study found no difference in R0 resection between the abdominal approach and the transhiatal approach. Complete tumor resection was accomplished via the abdominal approach alone in 43 (64%) patients, and the transhiatal approach was required only in 22 (33%) patients. Microscopic mural extension of cancer cells was very rare in our experience, as reflected by the fact that no positive resection margin was observed for all patients who underwent surgery with a curative intent. Therefore, our study suggests that the required extent of esophageal resection for GEJ cancers in Korea may differ from those insisted in the West, and the surgical approach could be tailored using a less extensive esophageal resection, such as the selective use of the transhiatal approach based on abdominal total gastrectomy.
The application of less extensive esophageal resection and the resulting high R0 resection rate in this study may be explained that the distinctive surgical epidemiology of GEJ cancers in Korea is different from those observed in the West. It is well known that the degree of mural extension is strongly correlated with the T stage.(12,25) In Western countries, most patients with GEJ cancers are typically diagnosed at an advanced stage as having T3 or T4 tumors, and lymph node metastasis.(18,19) On the contrary, our study found over 70% of the patients had tumors limited within the serosal layer (T1 or T2), and nearly 50% of the patients had no lymph node metastasis. Controversy continues concerning the optimal lymph node dissection when we perform GEJ cancer surgery. de Manzoni et al.(16)'s study suggested to perform total Gastrectomy with D2 lymphadenectomy with advanced cardia cancer type II or III. Pedrazzani et al.(26)'s study said that chest nodal involvement rate was 46.2% in type I, 29.5% in type II, 9.3% for type III. Siewert et al.(18)'s study suggested that lower mediastinal nodal involvement rate was 12% in type II, 5% in type III. So, our study performed D2 lymphadenectomy without mediastinal node dissection. Moreover, most GEJ cancers in our experience were limited in the cardia or subcardial region, which means that the vast majority of these tumors must be considered as gastric in origin and they should be treated as such. These characteristics of GEJ cancer observed in our study are consistent with those of other domestic reports from Korea.(4,6) However, further studies with a large number of patients are needed to ascertain the surgical epidemiology of GEJ cancers in Korea, and the optimal surgical approach should be determined based on these result.
In conclusion, our experience has shown that complete tumor resection can be achieved with less extensive esophageal resection as compared to those performed in the West. To achieve R0 resection, abdominal total gastrectomy with the selective use of the transhiatal approach was appropriate for treating GEJ cancer in Korea. This may be because the biologic and clinical features of GEJ cancer in Korea are different from those of the West, yet further studies with a large number of patients will be needed to establish the proper surgical approach to GEJ cancer in Korea.
References
- 1.Parkin DM, Bray F, Ferlay J, Pisani P. Global cancer statistics, 2002. CA Cancer J Clin. 2005;55:74–108. doi: 10.3322/canjclin.55.2.74. [DOI] [PubMed] [Google Scholar]
- 2.Blaser MJ, Saito D. Trends in reported adenocarcinomas of the oesophagus and gastric cardia in Japan. Eur J Gastroenterol Hepatol. 2002;14:107–113. doi: 10.1097/00042737-200202000-00003. [DOI] [PubMed] [Google Scholar]
- 3.Lee JY, Kim HY, Kim KH, Jang HJ, Kim JB, Lee JH, et al. No changing trends in incidence of gastric cardia cancer in Korea. J Korean Med Sci. 2003;18:53–57. doi: 10.3346/jkms.2003.18.1.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kim HJ, Kwon SJ. Analysis of clinocopathologic difference between type II and type III cancers in siewert classification for adenocarcinomas of the cardia. J Korean Gastric Cancer Assoc. 2004;4:143–148. [Google Scholar]
- 5.Kodera Y, Yamamura Y, Shimizu Y, Torii A, Hirai T, Yasui K, et al. Adenocarcinoma of the gastroesophageal junction in Japan: relevance of Siewert's classification applied to 177 cases resected at a single institution. J Am Coll Surg. 1999;189:594–601. doi: 10.1016/s1072-7515(99)00201-x. [DOI] [PubMed] [Google Scholar]
- 6.Park CH, Kang WK, Song KY, Bae JS, Kim JJ, Park SM, et al. Adenocarcinoma of the gastro-esophageal junction: Application of Siewert's classification to the Eastern experience. J Korean Gastric Cancer Assoc. 2004;4:36–43. [Google Scholar]
- 7.von Rahden BH, Stein HJ, Siewert JR. Surgical management of esophagogastric junction tumors. World J Gastroenterol. 2006;12:6608–6613. doi: 10.3748/wjg.v12.i41.6608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bozzetti F, Bonfanti G, Bufalino R, Menotti V, Persano S, Andreola S, et al. Adequacy of margins of resection in gastrectomy for cancer. Ann Surg. 1982;196:685–690. doi: 10.1097/00000658-198212001-00012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ito H, Clancy TE, Osteen RT, Swanson RS, Bueno R, Sugarbaker DJ, et al. Adenocarcinoma of the gastric cardia: what is the optimal surgical approach? J Am Coll Surg. 2004;199:880–886. doi: 10.1016/j.jamcollsurg.2004.08.015. [DOI] [PubMed] [Google Scholar]
- 10.Mattioli S, Di Simone MP, Ferruzzi L, D'Ovidio F, Pilotti V, Carella R, et al. Surgical therapy for adenocarcinoma of the cardia: modalities of recurrence and extension of resection. Dis Esophagus. 2001;14:104–109. doi: 10.1046/j.1442-2050.2001.00165.x. [DOI] [PubMed] [Google Scholar]
- 11.Mariette C, Castel B, Toursel H, Fabre S, Balon JM, Triboulet JP. Surgical management of and long-term survival after adenocarcinoma of the cardia. Br J Surg. 2002;89:1156–1163. doi: 10.1046/j.1365-2168.2002.02185.x. [DOI] [PubMed] [Google Scholar]
- 12.Tsujitani S, Okuyama T, Orita H, Kakeji Y, Maehara Y, Sugimachi K, et al. Margins of resection of the esophagus for gastric cancer with esophageal invasion. Hepatogastroenterology. 1995;42:873–877. [PubMed] [Google Scholar]
- 13.Siewert JR, Stein HJ. Classification of adenocarcinoma of the oesophagogastric junction. Br J Surg. 1998;85:1457–1459. doi: 10.1046/j.1365-2168.1998.00940.x. [DOI] [PubMed] [Google Scholar]
- 14.Sobin LH, Wittekind C, editors. International Union against Cancer, editors. TNM Classification of Malignant Tumours. 6th ed. New York: Willey-Liss; 2002. [Google Scholar]
- 15.Japanese Gastric Cancer Association. Japanese Classification of Gastric Carcinoma - 2nd English Edition - Gastric Cancer. 1998;1:10–24. doi: 10.1007/s101209800016. [DOI] [PubMed] [Google Scholar]
- 16.de Manzoni G, Pedrazzani C, Pasini F, Di Leo A, Durante E, Castaldini G, et al. Results of surgical treatment of adenocarcinoma of the gastric cardia. Ann Thorac Surg. 2002;73:1035–1040. doi: 10.1016/s0003-4975(01)03571-8. [DOI] [PubMed] [Google Scholar]
- 17.Rüdiger Siewert J, Feith M, Werner M, Stein HJ. Adenocarcinoma of the esophagogastric junction: results of surgical therapy based on anatomical/topographic classification in 1,002 consecutive patients. Ann Surg. 2000;232:353–361. doi: 10.1097/00000658-200009000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Siewert JR, Feith M, Stein HJ. Biologic and clinical variations of adenocarcinoma at the esophago-gastric junction: relevance of a topographic-anatomic subclassification. J Surg Oncol. 2005;90:139–146. doi: 10.1002/jso.20218. [DOI] [PubMed] [Google Scholar]
- 19.Barbour AP, Rizk NP, Gonen M, Tang L, Bains MS, Rusch VW, et al. Adenocarcinoma of the gastroesophageal junction: influence of esophageal resection margin and operative approach on outcome. Ann Surg. 2007;246:1–8. doi: 10.1097/01.sla.0000255563.65157.d2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hulscher JB, van Sandick JW, de Boer AG, Wijnhoven BP, Tijssen JG, Fockens P, et al. Extended transthoracic resection compared with limited transhiatal resection for adenocarcinoma of the esophagus. N Engl J Med. 2002;347:1662–1669. doi: 10.1056/NEJMoa022343. [DOI] [PubMed] [Google Scholar]
- 21.Sasako M, Sano T, Yamamoto S, Sairenji M, Arai K, Kinoshita T, et al. Japan Clinical Oncology Group (JCOG9502) Left thoracoabdominal approach versus abdominal-transhiatal approach for gastric cancer of the cardia or subcardia: a randomised controlled trial. Lancet Oncol. 2006;7:644–651. doi: 10.1016/S1470-2045(06)70766-5. [DOI] [PubMed] [Google Scholar]
- 22.Kim SH, Karpeh MS, Klimstra DS, Leung D, Brennan MF. Effect of microscopic resection line disease on gastric cancer survival. J Gastrointest Surg. 1999;3:24–33. doi: 10.1016/s1091-255x(99)80004-3. [DOI] [PubMed] [Google Scholar]
- 23.DeMeester SR. Adenocarcinoma of the esophagus and cardia: a review of the disease and its treatment. Ann Surg Oncol. 2006;13:12–30. doi: 10.1245/ASO.2005.12.025. [DOI] [PubMed] [Google Scholar]
- 24.Carboni F, Lorusso R, Santoro R, Lepiane P, Mancini P, Sperduti I, et al. Adenocarcinoma of the esophagogastric junction: the role of abdominal-transhiatal resection. Ann Surg Oncol. 2009;16:304–310. doi: 10.1245/s10434-008-0247-x. [DOI] [PubMed] [Google Scholar]
- 25.Casson AG, Darnton SJ, Subramanian S, Hiller L. What is the optimal distal resection margin for esophageal carcinoma? Ann Thorac Surg. 2000;69:205–209. doi: 10.1016/s0003-4975(99)01262-x. [DOI] [PubMed] [Google Scholar]
- 26.Pedrazzani C, de Manzoni G, Marrelli D, Giacopuzzi S, Corso G, Minicozzi AM, et al. Lymph node involvement in advanced gastroesophageal junction adenocarcinoma. J Thorac Cardiovasc Surg. 2007;134:378–385. doi: 10.1016/j.jtcvs.2007.03.034. [DOI] [PubMed] [Google Scholar]