Abstract
Objectives of the Study
To evaluate improvement in symptoms following arthrocentesis: Pain, Maximum Mouth Opening, Clicking/Crepitation.
Method
Eleven patients who reported to the department of Oral and Maxillofacial Surgery, M S Ramaiah Dental College, Bangalore clinically diagnosed to have Internal Derangement of the TMJ underwent Arthrocentesis. Patients were evaluated at the end of 1 week, 1 and 3 months and results tabulated.
Results
11 patients with clinically diagnosed Internal Derangement underwent Arthrocentesis and were followed up for 3 months. There was significant improvement in Pain, Maximum Mouth Opening and Clicking/Crepitation. All the results were statistically significant. There was no serious post operative complication.
Conclusion
Arthrocentesis can be recommended as a simple chair-side procedure for the treatment of TMJ Internal Derangement refractory to conservative management.
Keywords: TMJ, Arthrocentesis, Internal derangement
Introduction
TMJ disorders are an ever increasingly encountered clinical condition. Internal derangement, a type of disc interference disorder is cited as one of the most common [16]. Dolwick defined ‘Internal derangement is an abnormal relationship of the articular disc to the mandibular condyle, fossa and articular eminence’ [4, 5, 11].This disorder has clinical features such as pain, joint sounds, restriction of joint function during mandibular movements and irregular or deviating jaw function [7].
Arthrocentesis with joint lavage is the simplest form of surgical intervention and is suggested to be used as an initial procedure in the surgical algorithm [6, 17]. It is a minimally invasive procedure which reduces pain, joint sounds and improves mouth opening. It works on the principle that it could loosen adherent disc, remove inflammatory content and pain-mediators allowing nutrient perfusion and thereby free sliding movement of the disc [3, 10].
Arthrocentesis was useful for management of patients with continuing pain in TMJ unresponsive to conservative management, anterior disc displacement with and without reduction and associated osteoarthritis and rheumatoid arthritis [1, 5, 6, 8, 10, 12]. Although originally suggested for the treatment of painful limited mouth opening caused by TMJ derangement of acute onset, it is now widely used in the treatment of various ID as well as for diagnostic purpose [6, 15].
The purpose of this study was to evaluate the efficacy of arthrocentesis in clinically diagnosed TMJ internal derangement refractory to conservative treatment.
Methods
The study group consisted of 11 patients with 11 joints diagnosed to have ID clinically (5 male, 6 female) with a mean age of 27.08 (range, 16–64 years). Patients who reported to the out-patient department of Oral & Maxillofacial Surgery, M.S. Ramaiah dental college & Hospital with pain & dysfunction between Oct 2004 and Oct 2006 were evaluated. Clinical diagnosis of ID was made based on patients’ history and clinical signs and symptoms (limited mouth opening, TMJ pain and clicking).
Study group consisted of patients with ID with and without reduction and some of the patients were associated with either osteo arthritis (OA) and rheumatoid arthritis (RA). All patients were refractory to conservative treatment Fig. 1.
Fig. 1.
ID with closed lock
Patients were explained about the procedure, its possible immediate post operative sequelae like pain, swelling and potential complications. Patients’ written consent was obtained before the procedure.
The statistical analysis was done using paired t test for Pain and Maximum Mouth Opening (MMO) and χ2 test for clicking, crepitation. The data was computed in Microsoft excel worksheet and data was analyzed using SPSS (Version 10.0, Chicago). Patient details, findings of clinical examination were noted on a proforma. The following parameters were recorded. Pre-operative pain (analyzed using visual analog scale (0–10); Maximum inter incisal distance (measured using Vernier caliper); TMJ Clicking/Crepitation (present/absent, increase/decrease) evaluated based on patients own report. Arthrocentesis was then performed on the affected TMJ. Post-operatively these parameters were again assessed at 1 week, 1 month, 3 months and results tabulated.
Arthrocentesis of TMJ was performed according to the technique of Nitzan et al. The procedure was done under local anesthesia at chair–side. After betadine preparation of the target site, a reference line was drawn from the middle of the tragus marked to the outer canthus of the eye. The two points for needle insertion was then marked. The posterior entrance point was marked at a point 10 mm from the middle of the tragus and 2 mm below the canthotragal line; the anterior entrance point was placed 10 mm further forward along the line and 10 mm below it. Local Anesthetic (2% lidocaine) was injected subcutaneously above the articular fossa and eminence to block the auriculotemporal nerve. 1–2 ml of Bupivacaine 0.5% was than injected into the superior joint space. Eighteen gauge needles were inserted into the two points mentioned above and the upper joint compartment was irrigated with RL/NS (70–220 ml) through one needle ensuring a free flow of lavage through the other needle. On termination of the procedure, 1 ml of Hydrocortisone/sodium hyaluronate was injected into the joint Figs. 2 and 3.
Fig. 2.
Skin marking
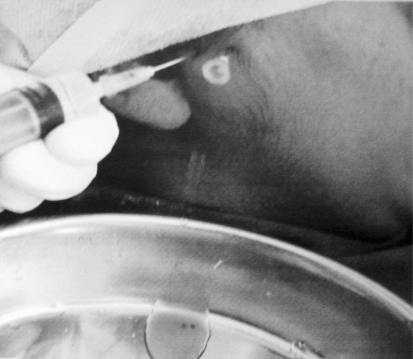
Fig. 3.
Lavage of the joint
After arthrocentesis, an NSAID (Diclofenac sodium) was advised for 3 days. Upper occlusal splint was given the next day to be worn round the clock for the first 10 postoperative days, there after, its use was restricted to during sleep for 3 months. Patients were taught certain simple exercises to be done four times a day; simple stretching; mouth opening against resistance of once own fist, side to side movement Fig. 4.
Fig. 4.
Increase in mouth opening
Results
Pre operative pain scores ranged from 4 to 8 (Mean 6.5). Post operative pain scores at 1 week, 1 month, and 3 months were compared with pre operative pain. There was significant decrease in pain scores at 1 week (P < 0.05), 1 month (P < 0.05), 3 months (P < 0.05).
The pre operative restriction in MMO ranged from 12 to 55 mm (Mean 31.18 mm) whereas post operative MMO at 1 week ranged from 15 to 43 mm (Mean 35.81 mm), at 1 month it ranged from 15 to 46 mm (Mean 36.54 mm), and at 3 months MMO ranged from 20 to 46 mm (Mean 37.27 mm). The results were statistically significant (P < 0.05).
At 1 week clicking decreased in 7 of 11 patients (63%), remaining 4 patients (36%) it was absent. At 1 month clicking decreased in 6 of 11 patients (54%), was absent in 3 (27%), increased in 1 (8.3%), and present in 1(8.3%). At 3 months clicking decreased in 4 of 11 patients (36%), absent in 3 (27%), increased in 2 (18%), and present in 2 (18%) Table 1.
Table 1.
Comparison of pain score and MMO at pre-op with different time interval
| Pre-op | 1 W | 1 M | 3 M | Statistical value | P-Value | |
|---|---|---|---|---|---|---|
| Pain score | 6.45 ± 1.29 | 3.18 ± 0.98 | 2.27 ± 1.27 | 2.09 ± 1.30 | 182.712 | <0.001* |
| MMO | 31.18 ± 10.52 | 35.81 ± 8.40 | 36.55 ± 8.29 | 36.82 ± 7.03 | 207.458 | <0.001* |
MMO Maximum mouth opening
* A very high significant difference
Preoperatively Crepitation was present in 2 of 11 patients (18%) and absent in remaining 9 patients (75%). At 1 week Crepitation decreased in 1 patients (9%), was absent in 10 patients (90%). At 1 month same results were observed. At 3 months Crepitation was absent in 10 patients (90%) and increased in 1 patient (9%).Overall, results were statistically significant (P < 0.05).
Discussion
TMD have always presented a therapeutic challenge. Arthrocentesis has been described as an effective modality in the treatment of patients demonstrating clinical findings consistent with the diagnosis of ID.
The landmarks for needle insertion were marked according to Nitzan technique (posterior entrance point for needle insertion was marked at a point 10 mm from the middle of the tragus and 2 mm below the canthotragal line, anterior needle was placed 10 mm farther forward along the line and 10 mm below it) [14]. In two of our cases, we got a free flow of lavage by putting the anterior needle 5 mm below the canthotragal line, instead of the usual 10 mm below. In one case, we had a sluggish outflow through the needle, so we used additional needle to enhance the transmission of the solution in accordance with Nitzan’s technique [14].
It has been estimated that 100 ml of fluid is necessary for a therapeutic lavage of the superior joint space [8, 13]. According to Keiseki Kaneyama et al. IL-6 and protein were effectively reduced by more that 200 ml of lavage [10]. In our study we used approximately 180–200 ml of RL for lavage depending upon swelling caused by effusion of fluid into adjacent tissue and patient’s pain tolerance. We did not perform any immunological study of the lavage and our aim was to determine clinical outcome of arthrocentesis and not immunological assay.
Intra-articular corticosteroid injection alone or after arthrocentesis provides long-term palliative effects on subjective symptoms and clinical signs of TMJ pain [12].In our last three cases we used Sodium hyaluronate injections in addition to Hydrocortisone since the clicking was sharper in accordance with Alpaslan et al [1, 2]. We could not appreciate much reduction in the clicking sound with or without Sodium hyaluronate.
Occlusal bite appliance helps preserve the results obtained by arthrocentesis and thus prevents the recurrence of inflammation and/or closed lock [10]. In our study, occlusal bite appliance was given in all cases
In our study 10 patients had clenching/bruxism and maxillary occlusal bite appliance was given to reduce post-operative pain and maintain the results obtained with arthrocentesis. In our study, the success rate of the treatment was Pain—91%, MMO—91%, clicking—66% crepitation—91%. The overall success rate with 3 months follow-up was 84.7%, which is in accordance with studies by Carvajal and Laskin (88%), but their study follow up was from 10 to 96 months [8]. Dorrit W Nitzan reported overall improvement of 95% and their follow up period was from 6 to 37 months [18]. Studies by Hosaka et al. showed their success rates increased with follow up.
Two cases of OA and one case of RA in association with ID had significant improvement in overall dysfunction as in accordance with Nitzan [9, 15].
Swelling of the neighbouring tissues due to perfusion of Ringer’s solution into the surrounding tissues may occur during arthrocentesis which is transient. In our study, immediate post operative swelling was encountered in majority of patients. But the swelling subsided overnight in all the cases. Otherwise there were no serious post operative complications.
Conclusion
Arthrocentesis can be recognized as a simple, economical and effective chair-side procedure in the treatment algorithm of TMJ ID as the overall treatment outcome of arthrocentesis was statistically significant in our study. With larger sample size and longer follow up our study can become more validated.
References
- 1.Alpaslan GH, Alpaslan C. Efficacy of temporomandibular joint arthrocentesis with and without injection of sodium hyaluronate in treatment of internal derangements. J Oral Maxillofac Surg. 2001;59:613–618. doi: 10.1053/joms.2001.23368. [DOI] [PubMed] [Google Scholar]
- 2.Alpaslan C, Dolwick MF, Heft MW. Five year retrospective evaluation of temporomandibular joint arthrocentesis. Int J Oral Maxillofac Surg. 2003;32:263–267. doi: 10.1054/ijom.2003.0371. [DOI] [PubMed] [Google Scholar]
- 3.Brennan PA, Ilankovan V. Arthrocentesis for temporomandibular joint pain dysfunction syndrome. J Oral Maxillofac Surg. 2006;64:949–951. doi: 10.1016/j.joms.2006.02.010. [DOI] [PubMed] [Google Scholar]
- 4.Christopher R, Katzberg RW, Espelandl MA. The clinical predictability of internal derangements of temporomandibular joint. Oral Surg Oral Med Oral Pathol. 1991;71:412–414. doi: 10.1016/0030-4220(91)90418-C. [DOI] [PubMed] [Google Scholar]
- 5.Emshoff R, Rudisch A. Are internal derangement and osteoarthritis linked to changes in clinical outcome measures of arthrocentesis of temporomandibular joint. J Oral Maxillofac Surg. 2003;61:1162–1167. doi: 10.1016/S0278-2391(03)00676-1. [DOI] [PubMed] [Google Scholar]
- 6.Emshoff R, Rudisch A. Prognostic indicators of the outcome of arthrocentesis: a short-term follow-up study. Oral Sur Oral Med Oral Pathol Oral Radiol Endod. 2003;96:12–18. doi: 10.1016/S1079-2104(03)00219-1. [DOI] [PubMed] [Google Scholar]
- 7.Emshoff R, Rudisch A, Gassner R. Effect of arthrocentesis and hydraulic distension on the temporomandibular joint disc position. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;89:271–277. doi: 10.1016/S1079-2104(00)70088-6. [DOI] [PubMed] [Google Scholar]
- 8.Frost DE, Kendell BD. The use of arthrocentesis for treatment of temporomandibular joint disorders. J Oral Maxillofac Surg. 1999;57:583–587. doi: 10.1016/S0278-2391(99)90080-0. [DOI] [PubMed] [Google Scholar]
- 9.Hosaka H, Murukami K, Goto K. Outcome of arthrocentesis for temporomandibular joint with closed lock at 3 years follow up. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1996;82:501–504. doi: 10.1016/S1079-2104(96)80193-4. [DOI] [PubMed] [Google Scholar]
- 10.Kaneyama K, Segami N, Nishmura M. The ideal lavage volume for removing bradykinin, interleukin-6, and protein from the temporomandibular joint by arthrocentesis. J Oral Maxillofac Surg. 2004;62:657–661. doi: 10.1016/j.joms.2003.08.031. [DOI] [PubMed] [Google Scholar]
- 11.Kaplan AS, Assael LA. Temporomandibular disorders: diagnosis and treatment. 1. Philadelphia: W B Saunder’s & Company; 1991. pp. 143–160. [Google Scholar]
- 12.Kurita K, Goss AN, Ogi N, Toyama M. Correlation between preoperative mouth opening and surgical outcome after arthroscopic lysis and lavage in patients with disc displacement without reduction. J Oral Maxillofac Surg. 1998;56:1394–1397. doi: 10.1016/S0278-2391(98)90401-3. [DOI] [PubMed] [Google Scholar]
- 13.Milam SB, Schmitz JP, Gustavo Z. Elution of proteins by continuous temporomandibular joint arthrocentesis. J Oral Maxillofac Surg. 1997;55:709–715. doi: 10.1016/S0278-2391(97)90583-8. [DOI] [PubMed] [Google Scholar]
- 14.Nitzan DW. Arthrocentesis for the management of severe closed lock of the temporomandibular joint. Oral Maxillofac Surg Clin North Am. 1994;6(2):245–257. [Google Scholar]
- 15.Nitzan DW, Price A. The use of arthrocentesis for the treatment of osteoarthritic temporomandibular joints. J Oral Maxillofac Surg. 2001;59:1154–1159. doi: 10.1053/joms.2001.26716. [DOI] [PubMed] [Google Scholar]
- 16.Rudiger E, Ansgar R. Determining predictor variables for treatment outcome of Arthrocentesis and hydraulic distension of TMJ. J Oral Maxillofac Surg. 2004;62:816–823. doi: 10.1016/j.joms.2003.12.020. [DOI] [PubMed] [Google Scholar]
- 17.Trieger N, Hoffman CH, Rodriguez E. The Effect of arthrocentesis of the temporomandibular joint in patients with rheumatoid arthritis. J Oral Maxillofac Surg. 1999;57:537–540. doi: 10.1016/S0278-2391(99)90070-8. [DOI] [PubMed] [Google Scholar]
- 18.Yoda T, Imai H. Effect of arthrocentesis on TMJ disturbance of mouth closure with loud clicking: a preliminary study. J Craniomand Pract. 2002;20(1):18–22. doi: 10.1080/08869634.2002.11746185. [DOI] [PubMed] [Google Scholar]