Abstract
We report a case of retained wooden foreign body in the zygomatic region which posed a considerable diagnostic difficulty and was the source of persistent draining sinus and other distressing symptoms. The patient was not aware of the foreign body in the maxillofacial region. In such cases a thorough history of the patient is of utmost importance. The case has been described to highlight the problems associated in managing unlikely foreign bodies at unusual facial sites when there is a possibility that radiolucent material is embedded in the wound.
Keywords: Foreign body, Maxillofacial region, Trismus
Introduction
The presence of an embedded foreign body in the oral and maxillofacial region is not unusual [1]. Most of the impacted foreign bodies are inorganic in nature with amalgam tattoo as the most common [2, 3]. Usually impacted foreign bodies are small in size and relatively inert in nature, thus, eliciting a very limited or no inflammatory response [4]. Occasionally, foreign bodies may be retained for prolonged period causing persistent and distressing symptoms. Foreign bodies such as broken wooden pieces, lead pencil points, broken tooth fragments, betel nut, fish bone, fragments of a smoking pipe, metallic objects have been reported in the literature [5]. Foreign bodies may be accidental, iatrogenic, or in more bizarre cases it may be deliberate as well [6]. The purpose of this report is to highlight the significance of thorough history taking and keeping a high index of clinical suspicion for a probable foreign body when dealing with unusual abscesses in the head and neck.
Report of a Case
A 45-year-old male patient reported to the Department of Oral and Maxillofacial Surgery, Subharti Dental College, Meerut with chief complaint of an extra oral swelling with purulent discharge and inability to open the mouth.
The patient related a history of a road traffic accident 2 years ago following which he developed the above said symptoms. Primary management was done at a local medical centre which included primary closure of facial wounds immediately following the accident.
On thorough clinical examination a diffuse swelling with purulent discharge from the draining sinus was evident in the right zygomatic buttress region. Swelling was tender, hard in consistency, erythematous along with local rise in temperature.
There was no evidence of any occlusal derangement. Inter-incisal mouth opening had been reduced to 1 cm.
Osteomyelitis of the zygomatic bone or a parotid fistula was suspected clinically and methylene blue dye was injected into the parotid duct by inserting an 18 gauge cannula into the duct orifice to detect the same but there was no discharge of the dye from the draining sinus and hence parotid fistula secondary to trauma was ruled out.
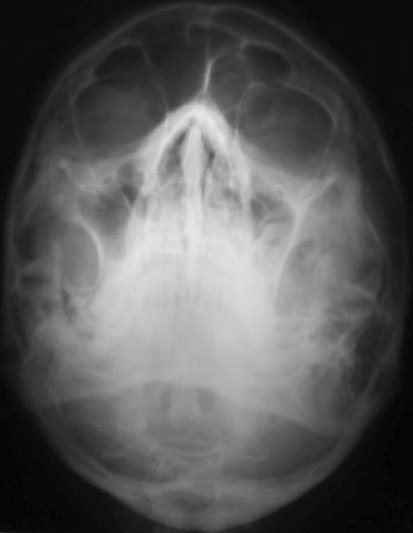
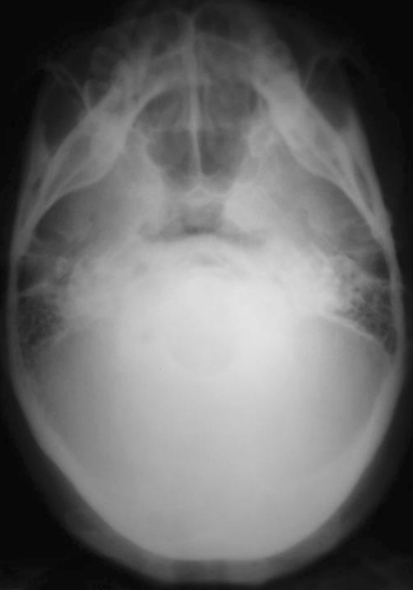
The patient was then subjected to a series of conventional radiographs comprising of OPG, Occipito—mental view, Submento—vertex view (Figs. 1, 2, 3) but no significant findings were noted and osteomyelitis was also ruled out.
Fig. 1.
Preoperative lateral view
Fig. 2.
Occipitomental view—no evidence of any foreign body
Fig. 3.
Submentovertex view—no evidence of any foreign body
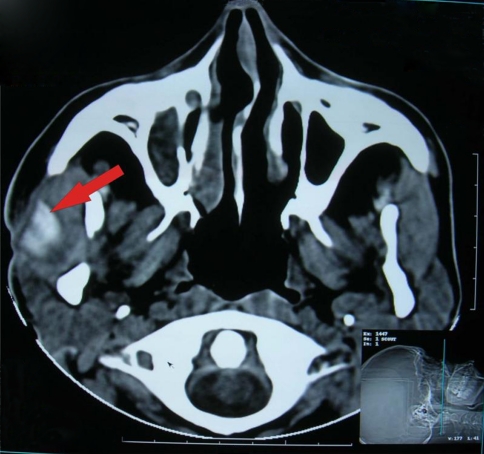
CT scan of the pre auricular region revealed a foreign body beneath the right zygomatic arch and in close proximity to the substance of the parotid gland (Fig. 4).
Fig. 4.
C.T. Scan axial view showing the presence of foreign body
Surgical exploration was done under local anaesthesia under antibiotic coverage. Functional testing of the facial nerve was performed prior to administration of local anesthetic solution. Blunt dissection was carried out with due care not to injure the facial nerve by following the sinus track under the external scar for about 2 cm beneath the skin layer. A wooden piece measuring approximately 3 × 1 cm enclosed in a fibrous capsule was encountered (Figs. 5, 6, 7).
Fig. 5.
Intra-operative dissection
Fig. 6.
Intra-operative view of wooden piece
Fig. 7.
Wooden piece retrieved
A cleavage plane was established and the wooden piece was carefully removed in toto by clamping it with a curved hemostat.
Transient facial nerve palsy was noted in the immediate post operative period. This traction paresis completely resolved by third post operative day. Thorough debridement of the operative site was carried out using Povidone iodine solution and primary closure of the wound achieved by suturing in two layers (Fig. 8).
Fig. 8.
Primary closure of the surgical site
The extra oral wound healed uneventfully and satisfactory mouth opening was achieved after post operative physiotherapy (Figs. 9, 10).
Fig. 9.
Post operative—after suture removal
Fig. 10.
Post operative—mouth opening on 10th day
Discussion
Foreign bodies are sometimes encountered in the maxillofacial region posing a great diagnostic dilemma. Despite a history of assault or trauma foreign bodies may not be suspected clinically leading to delay in diagnosis.
Occasionally, foreign bodies may be retained for prolonged period causing persistent and distressing symptoms.
Whilst some foreign bodies may be left in situ for good clinical reasons most are removed prior to the onset of complication, notably infection [7].
Wounds that have been contaminated with foreign materials, such as dirty gravel, wood, metal, tooth fragments, grass, and organic particles must be thoroughly searched for during the initial treatment phase and the material must be removed to prevent wound infections. Indications for the removal of foreign bodies from soft tissue are reactivity (thorns, spines, wood and other vegetative material), heavy contamination (soil, teeth), toxicity (heavy metals, spines with venom), impingement of vital structures (vessels, nerves, tendons), impairment of mechanical function (restricted joint mobility), intra-articular location, intravascular location, persistent pain, established infection, allergic reaction, cosmesis, psychological distress [8].
Accurate localization before removal is essential. Blind searching is time consuming and may produce further trauma or displacement of foreign body into the deeper fascial planes [7].
It may not be possible to remove all the fragments, but larger foreign bodies should be removed since they may cause pain, tenderness, or deformity. Some foreign bodies like wood may not be visible on radiographs but should be located and removed, as their presence will result in persistent infection.
Deep and large foreign bodies may not be found by following an epithelised or granulating track or draining sinus [9].
Radiographic examination in the various projections and computerized tomography will assist in the exclusion or location of foreign bodies and the precise determination of the nature of bony malposition.
Foreign body may not show up on conventional radiograph. Radiographs taken in several planes at right angles to one other are necessary to identify the exact position. In special circumstances, contrast media may be introduced to assist in the definition of the defects. Markers may be applied to the skin to help in the precise location of foreign bodies [8].
Every effort must be made to locate foreign bodies in all lacerations and penetrating injuries, suspected of harboring foreign bodies. Teeth and foreign bodies may be ingested or implanted into the soft tissues and may also impale the patient. Foreign bodies may implant anywhere and may be a great distance from mucosa or skin breach. A very high index of suspicion must be maintained, with any laceration in or around the eyes, including the lips, cheek, jaws and particularly in children who are often poor historians. Wooden objects are notorious for harboring organisms and producing abscesses and can be difficult to detect [10]. Thorough clinical examination along with diagnostic imaging is mandatory in the detection of foreign body. The purpose of imaging is two fold first to confirm the presence of foreign body and second to locate it. Methods used to confirm the presence of a foreign body, and demonstrate it’s approximate size include, plain radiograph, CT. MRI should not be used in any patient who may have a metallic fragment in the orbit as the magnetic field may displace the fragment and endanger sight, but it has an important place in detecting wood, if it has not been identified on C.T.
Worth recommended plain X-ray films, two views at right angles to each other, to locate the foreign object in three dimensions [11]. Other methods described to detect foreign bodies include use of metal detectors that sound an alarm in the proximity of a buried metal foreign body, use of intra-operative ultrasound for localization and retrieval of the foreign body in the head and neck region has been reported previously [12].
History and high degree of suspicion are most important in the diagnosis of a foreign body. Even if imaging is uneventful surgical exploration may be necessary. On the contrary exploration without adequate imaging is courting disaster, as additional foreign segments and sometimes even intracranial foreign body and damage may be missed [11].
Novel approaches to foreign body removal have been mentioned.
The fragment is rarely confined within the normally recognized planes of surgical dissection. The finger is the most sensitive probe and will readily palpate the buried foreign body. If a long curved hemostat is passed along the line of finger, the foreign body can be grasped and removed by an experienced surgeon through a relatively small wound.
In this case the history offered absolutely no suggestion of a foreign body and indeed clinically the patient appeared to have sustained a right zygomatic arch fracture which was not confirmed by conventional radiographs. So a C.T. scan was advised which showed foreign body impinging on the right zygomatic arch.
Trismus was due to foreign body embedded beneath the arch which prevented forward movement of the mandibular coronoid process during mouth opening. This was resolved following foreign body retrieval and postoperative physiotherapy. We therefore suggest whenever foreign body retention is suspected thorough surgical exploration of the wound is recommended particularly when the foreign material may be radiolucent or the object responsible for the injury is not adequately accounted for.
References
- 1.McKinney RV, Jr, Brady GL, Singh BB. Metallic foreign body embedded in the cheek for 20 years. JADA. 1981;102:331–332. doi: 10.14219/jada.archive.1981.0044. [DOI] [PubMed] [Google Scholar]
- 2.Cataldo E, Santis H. Response of the oral tissues to exogenous foreign materials. J Periodontol. 1974;45:93–106. doi: 10.1902/jop.1974.45.2.93. [DOI] [PubMed] [Google Scholar]
- 3.Weathers DR, Fine RM. Amalgam tattoo of oral mucosa. Arch Dermatol. 1974;110:727–728. doi: 10.1001/archderm.1974.01630110025004. [DOI] [PubMed] [Google Scholar]
- 4.Buchner A, Hansen LS. Amalgam pigmentation (amalgam tattoo) of the oral mucosa. Oral Surg Oral Med Oral Pathol. 1980;29:130–147. doi: 10.1016/0030-4220(80)90306-0. [DOI] [PubMed] [Google Scholar]
- 5.da Silva EJ, Deng Y, Tumushime-Buntro CG. An unusual foreign body in the tongue. Br J Oral Maxillofac Surg. 2000;38:241–242. doi: 10.1054/bjom.1998.0013. [DOI] [PubMed] [Google Scholar]
- 6.Din Quiamud. Foreign bodies in maxillofacial region. J Pak Dent Assoc. 2001;10(3):153–157. [Google Scholar]
- 7.Cameron M, Phillips B. Snookered! Facial infection secondary to occult foreign body. Int J Oral Maxillofac Surg. 2006;35:373–375. doi: 10.1016/j.ijom.2005.09.010. [DOI] [PubMed] [Google Scholar]
- 8.Fonseca RJ, Walker RV. Oral and maxillofacial trauma. 2. Philadelphia: W.B. Saunders Company; 1997. pp. 796–797. [Google Scholar]
- 9.Williams JLI. Rowe and Williams’ maxillofacial injuries. 1. London: Churchill Livingston; 1985. pp. 704–715. [Google Scholar]
- 10.Booth PW, Eppley BL, Schmelzeisen R. Maxillofacial trauma and esthetic facial reconstruction. 1. London: Churchill Livingstone; 2003. pp. 92–93. [Google Scholar]
- 11.Worth HM. Foreign bodies. In: Worth HM, editor. Principles and practice of oral radiologic interpretation. Chicago: Yearbook Medical Publishers; 1963. pp. 207–212. [Google Scholar]
- 12.Sharma PK, Songra AK, Ng SY. Intraoperative ultrasound-guided retrieval of an airgun pellet from the tongue: a case report. Br J Oral Maxillofac Surg. 2002;40:153–155. doi: 10.1054/bjom.2001.0733. [DOI] [PubMed] [Google Scholar]