Abstract
Diseases of the human brain are almost universally attributed to malfunction or loss of nerve cells. However, a considerable amount of work has, during the last decade, expanded our view on the role of astrocytes in CNS (central nervous system), and this analysis suggests that astrocytes contribute to both initiation and propagation of many (if not all) neurological diseases. Astrocytes provide metabolic and trophic support to neurons and oligodendrocytes. Here, we shall endeavour a broad overviewing of the progress in the field and forward the idea that loss of homoeostatic astroglial function leads to an acute loss of neurons in the setting of acute insults such as ischaemia, whereas more subtle dysfunction of astrocytes over periods of months to years contributes to epilepsy and to progressive loss of neurons in neurodegenerative diseases. The majority of therapeutic drugs currently in clinical use target neuronal receptors, channels or transporters. Future therapeutic efforts may benefit by a stronger focus on the supportive homoeostatic functions of astrocytes.
Keywords: aging, astrocyte, brain, calcium, disease, supportive cell, transmitter
Abbreviations: Aβ, amyloid β-peptide; AD, Alzheimer's disease; ALS, amyotrophic lateral sclerosis; AMPA, α-amino-3-hydroxy-5-methylisoxazole-4-propionic acid; CNS, central nervous system; EAAT1, excitatory amino acid transporter 1; EL, epileptic; EPO, erythropoietin; GABA, γ-aminobutyric acid; GAT-3, GABA transporter 3; GFAP, glial fibrillary acidic protein; mGluR, metabotropic glutamate receptor; OGD, oxygen glucose deprivation; TSP1/2, thrombospondins 1 and 2
INTRODUCTION
Astrocytes are specialized glial cells that are ubiquitously present in all regions of the CNS (central nervous system). Although astrocytes were first identified over 120 years ago and their responses to CNS injury have been recognized for over a century (Kettenmann and Verkhratsky, 2008), for much of this time they have been regarded largely as passive cells providing structural support for neuronal networks; and the notions that astrocytes might make important contributions to CNS function, or that dysfunctions of astrocytes might contribute to CNS pathological remodelling and disease, were generally not considered. In spite of this long ‘passive’ history, ideas about astrocytes are now changing radically. A steadily growing body of data has over the last 25 years established a variety of essential functions for astrocytes in the healthy nervous system and in the response to injury and disease. Moreover, mechanisms are being elucidated through which the loss or gain of astrocyte functions can contribute to dysfunction or degeneration as well as repair and post-disease remodelling of the CNS. Based on this information, the multiple roles of astroglia, which determine the progression and outcome of neurological diseases, are emerging, and it is becoming clear that astrocytes are involved in various aspects of disease initiation, progression and resolution. Knowledge emerging about many different aspects of neuropathologies clearly indicates that astrocytes contribute to many neurological diseases and in some cases, such as Alexander disease, is the direct cause of the neurodegeneration. As the astrocyte contribution to specific clinico-pathological entities is being defined, it is useful to compare the astroglial involvement across a number of diseases. We will here specifically review the role of astrocytes in epilepsy, stroke and neurodegenerative diseases. Alexander disease presents clinically as a classical early childhood leucodystrophy with seizure, myelin loss and neuronal degeneration, but is caused by mutation and accumulation of GFAP (glial fibrillary acidic protein). The fundamental fact that a defect in astrocytes underlies dysfunction and death of neurons and oligodendrocytes is discussed.
ASTROCYTES CONTROL CNS HOMOEOSTASIS
Astrocytes are the most numerous, morphologically heterogeneous and functionally diverse neuroglial cells. Indeed, even the definition of astrocyte does not really exist, as the ‘astroglia’ as a cell class covers all non-myelinating macroglial cells in the CNS, which along with classical protoplasmic and fibrous astrocytes includes, for example, such different cellular entities as retinal Muller radial glial cells, tanycytes in hypothalamus, pituicytes in the neuro-hypophysis, and ependymocytes, choroid plexus cells and retinal pigment epithelial cells that line the ventricles or the subretinal space (Reichenbach and Wolburg, 2005; Verkhratsky and Butt, 2007). All these cells have, however, one thing in common: their main function is in providing for CNS homoeostasis and therefore astrocytes can be broadly defined as ‘homoeostatic neuroglial cells’.
Astrocytes participate in controlling CNS homoeostasis at many levels. Astroglia is critical for maintaining molecular homoeostasis (astrocytes regulate concentrations of ions, neurotransmitters and neurohormones in the CNS (Newman, 1995; Danbolt, 2001); metabolic homoeostasis (astroglia accumulate energy substrates and supplies neurones with lactate; Magistretti, 2006), cellular homoeostasis (astrocytes are directly involved in neurogenesis; Alvarez-Buylla et al., 2001), morphological homoeostasis (astroglia define neural cell migration during development, control synaptogenesis/synaptic pruning and shape the micro-architecture of grey matter (Nedergaard et al., 2003; Pfrieger, 2009), and organ homoeostasis (astroglia control the formation and maintenance of the blood–brain barrier; Abbott, 2005). Furthermore, astrocytes appear to be critically important for brain chemosensing, being able to detect systemic fluctuations in CO2, pH and Na+ and initiate behavioural homoeostatic programmes (Shimizu et al., 2007; Gourine et al., 2010; Huckstepp et al., 2010; Gourine and Kasparov, 2011).
Astrocytes also act as integrators in the CNS. In the grey matter, astrocytes create relatively independent neuro-vascular units connected to the capillaries via astroglial perivascular processes. Recent findings show that astrocytes produce and release various molecular mediators, such as prostaglandin E, nitric oxide and arachidonic acid, which can increase or decrease CNS blood vessel diameter and blood flow in a co-ordinated manner (Gordon et al., 2007; Iadecola and Nedergaard, 2007). Furthermore, astrocytes appear to be primary mediators of changes in local CNS blood flow in response to changes in neuronal activity (Schummers et al., 2008; Wolf and Kirchhoff, 2008; Koehler et al., 2009). Astrocytes are fundamental for synaptic transmission and synaptic plasticity. Astrocyte processes that envelop or are in close proximity to synapses provide for spatial specificity of synaptic inputs through isolating individual synapses with astroglial ‘cradle’ and maintain the fluid, ion, pH and transmitter homoeostasis and provide local metabolic support that are critical for synaptic transmission (Bourne and Harris, 2008; Nedergaard and Verkhratsky, 2012). Astrocytes are endowed with multiple neurotransmitter receptors that allow them to monitor neuronal activity (Verkhratsky, 2010; Lalo et al., 2011a, 2011b) and, moreover, astrocytes secret multiple neurotransmitters and neurohormones (e.g. ATP/purines, glutamate, d-serine, etc.: Halassa et al., 2007a, 2007b; Shigetomi et al., 2008; Perea et al., 2009) that can regulate functional activity of many tens of thousands of synapses located within astroglial territorial domain by a paracrine route. As already mentioned above, astrocyte-derived molecules appear to play critical roles in the formation, maintenance and pruning of synapses (Christopherson et al., 2005; Stevens et al., 2007; Barres, 2008). In addition, polypeptide cytokines such as tumour necrosis factor-α produced by astrocytes as well as microglia can influence homoeostatic synaptic scaling by inducing the insertion of AMPA (α-amino-3-hydroxy-5-methylisoxazole-4-propionic acid) receptors at post-synaptic membranes (Stellwagen and Malenka, 2006). Astrocytes are also critical for maintaining glutamatergic transmission by recycling glutamate through the glutamate–glutamine shuttle for subsequent reconversion into active transmitter in the synaptic terminal (Danbolt, 2001; Sattler and Rothstein, 2006).
GENERAL PATHOPHYSIOLOGY OF ASTROGLIA: NEUROPATHOLOGY AS HOMOEOSTATIC FAILURE
Every disease of the CNS can be regarded as a homoeostatic failure either inherited (loss of homoeostatic function) or acute (trauma or stroke) or chronic (neurodegeneration). The initiation and progression of these diseases are determined by the degree of homoeostatic loss, which can be either general or function-specific. The general failure is characteristic for acute insults (trauma, stroke or toxic attack), which compromise brain homoeostasis on many levels from organ (disruption of blood–brain barrier) to metabolic (shutting down the brain energetics) and molecular (loss of neurotransmitter homoeostasis with subsequent excitotoxicity). The specific homoeostatic failures are operative in many forms of chronic pathology, when for example down-regulation of glutamate transporters induces neuronal death in Wernicke encephalopathy. In many pathologies, the homoeostatic failure progresses and broadens when for example initial disruptions of protein catabolism trigger inflammatory reactions, initiate cytotoxicity and compromise the blood–brain barrier (as happens in various neurodegenerative processes).
The systemic homoeostatic function of astroglia makes these cells the main targets for neuropathology (Giaume et al., 2007; Verkhratsky and Parpura, 2010). Astrocytes form the brain defence system by virtue of many homoeostatic molecules expressed in astroglia; using these molecules, astrocytes contain the damage and sustain neuronal survival through maintaining CNS homoeostasis. One of many examples is represented by maintaining brain metabolism following ischaemia/hypoglycaemia, when astrocyte glycogen breaks down to lactate that is transferred to adjacent neural elements where it is used aerobically as fuel (Brown and Ransom, 2007; Brown et al., 2007; Suh et al., 2007). When and if astroglial homoeostatic mechanisms are exhausted the nervous tissue dies.
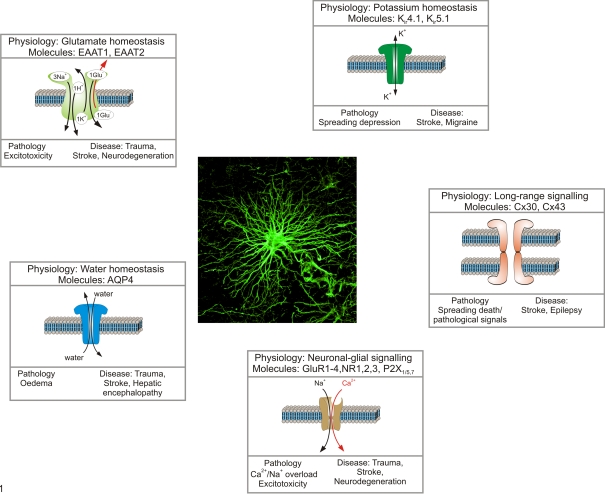
At the same time all glial homoeostatic mechanisms are endowed with an inherent dichotomy – being developed as survivalistic and protective they may turn to be deleterious and toxic. In conditions of severe insult astrocytes can assume damaging and toxic proportions (Figure 1). For example aquaporins expressed in astroglia are critical for water movements through brain tissue, but they can also be instrumental in mediating oedema in pathology (Zador et al., 2009). Similarly, K+ channels responsible for potassium buffering when under pathological stress can add to accumulation of extracellular K+ and mediate spreading depression (Nedergaard and Dirnagl, 2005). The connexins, which connect astrocytes into multicellular syncytia can become the passages for death signals underlying the spread of necrosis through ischaemic penumbra (Lin et al., 1998), whereas depolarization and Na+ accumulation in astroglia triggers reversal of glutamate transporters which increase glutamate excitotoxicity.
Figure 1. General pathophysiology of astroglia.
The homoeostatic cascades expressed in astrocytes control various aspects of CNS homoeostasis including extracellular ion homoeostasis (K+ buffering via Kir channels, Na/K pump and K transporters), regulate movements and distribution of water (via aquaporins and connexins), control extracellular concentration of neurotransmitters (by dedicated transporters) and provide the main reactive oxygen species scavenging system. In pathological conditions, the very same systems may contribute to brain damage. Failure in water transport triggers brain oedema, reversal of neurotransmitter transporters contributes to glutamate excitotoxicity, inadequate K+ buffering promotes further overexcitation of neural cells and spreading depression, and connexins become a conduit for death signals.
ASTROCYTE RESPONSES TO INJURY AND DISEASE: REACTIVE ASTROGLIOSIS AND SCAR FORMATION
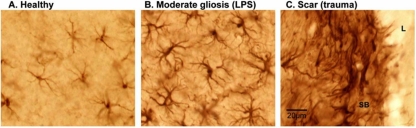
Astrocytes respond to all forms of CNS injury and disease through a process known as reactive astrogliosis. Substantial progress has been made recently in determining functions and mechanisms of reactive astrogliosis and in identifying roles of reactive astrocytes in CNS disorders and pathologies (Figure 2). For the sake of clarity, it is useful to begin with a working definition of the terms ‘reactive astrogliosis’ and ‘glial scar formation’ (Sofroniew, 2009; Sofroniew and Vinters, 2010). These terms are not synonymous. Contrary to commonly held beliefs, reactive astrogliosis is not a simple all-or-none stereotypic phenomenon. Instead, reactive astrogliosis is a finely gradated continuum of changes that occur in context-dependent manners regulated by specific molecular signalling events. These changes range from reversible alterations in gene expression and cell hypertrophy with preservation of cellular domains and tissue structure, to long lasting scar formation with rearrangement of tissue structure (Sofroniew, 2009; Sofroniew and Vinters, 2010). Based on a large body of observations in experimental animals and human pathological specimens, a definition of reactive astrogliosis has recently been proposed includes several grades of severity of reactive astrogliosis and glial scar formation that may be encountered in experimental and clinical histopathological examinations (Sofroniew, 2009; Sofroniew and Vinters, 2010). Although the increasing severities of reactive astrogliosis transition seamlessly along a continuum, it is convenient for purposes of description and classification to recognize several broad categories.
Figure 2. Appearance of astrocytes and different types of reactive astrocytes in mouse cerebral cortex.
Images show immunohistochemistry for the intermediate filament protein, GFAP, which visualizes the cell cytoskeleton. (A) In healthy cortex, some, but not all astrocytes express detectable levels of GFAP; cell bodies are small and the cytoskeleton is thin and restricted largely to the proximal portions of cell processes. (B) In response to the bacterial antigen, lipopolysaccharide (LPS) injected into the lateral cerebral ventricle, cortical astrocytes become moderately reactive, with up-regulation of GFAP expression such that it is now detectable in all astrocytes. In addition, there is substantial hypertrophy of the astrocyte cell bodies as well as hypertrophy of stem processes and associated cytoskeleton. However, there is no astrocyte proliferation and individual cells continue to respect their individual, non-overlapping domains. (C) In response to a severe traumatic injury that creates a lesion (L) with tissue necrosis and invasion of inflammatory cells, astrocytes not only become reactive but also proliferate in the immediate vicinity of the lesion and form a scar with a dense scar border (SB) that comprises many newly generated astrocytes that do not exhibit individual domains and instead have many overlapping and intermingling processes. All images are at the same magnification. Scale bar = 20 μm (Photos courtesy of the Sofroniew laboratory).
Mild to moderate reactive astrogliosis consists of changes (up- or down-regulation) in gene expression and hypertrophy of cell body and processes without substantive loss of individual astrocyte domains and little or no astrocyte proliferation; up-regulation of GFAP expression is prominent. This type of response is generally associated with mild non-penetrating and non-contusive trauma, diffuse innate immune activation (viral infections, system bacterial infections) and areas that are some distance to focal CNS lesions. Because there is little or no reorganization of tissue architecture, if the triggering mechanism is able to resolve, then mild or moderate reactive astrogliosis exhibits the potential for resolution in which the astrocytes return to an appearance similar to that in healthy tissue (Sofroniew, 2009; Sofroniew and Vinters, 2010).
Severe diffuse reactive astrogliosis also consists of changes (up- or down-regulation) in gene expression with pronounced up-regulation of GFAP expression and hypertrophy of cell body and processes, but in addition includes astrocyte proliferation and loss of individual astrocyte domains with substantive intermingling and overlapping of neighbouring astrocyte processes. These changes can result in long-lasting reorganization of tissue architecture that can extend diffusely over substantive areas. This type of response is generally found in areas surrounding severe focal lesions, infections or areas responding to chronic neurodegenerative triggers, and because there can be considerable tissue reorganization, the potential for resolution and return to normal structure is reduced (Sofroniew and Vinters, 2010).
Severe reactive astrogliosis with compact glial scar formation also includes changes in gene expression, cellular hypertrophy and astrocyte proliferation, with pronounced overlapping of processes to form compact borders around areas of severe tissue damage, necrosis, infection or autoimmune-triggered inflammatory infiltration (Bush et al., 1999; Faulkner et al., 2004; Drogemuller et al., 2008; Herrmann et al., 2008; Voskuhl et al., 2009). These glial scars include other cell types, in particular fibromeningeal and other glial cells (Bundesen et al., 2003; Herrmann et al., 2008; Sofroniew, 2009; Sofroniew and Vinters, 2010), and deposit collagenous extracellular matrix that contains many molecular cues that inhibit axonal and cellular migration (Silver and Miller, 2004). Triggering insults include penetrating trauma, severe contusive trauma, invasive infections or abscess formation, neoplasm, chronic neurodegeneration, or systemically triggered inflammatory challenges. It is noteworthy that the glial scar formation is associated with substantive tissue reorganization and structural changes that are long lasting and persist long after the triggering insult may have resolved.
The functional roles exerted by reactive astrocytes at different points along their continuum of potential responses to different kinds and severities of CNS insults are only beginning to be understood. Although astrogliosis and scar formation have often been viewed as maladaptive and purely detrimental responses, this is not the case. There are now many different kinds of evidence in vivo and in vitro that reactive astrocytes maintain their homoeostatic mechanisms and can protect CNS cells and tissue in various ways, including by (i) uptake of potentially excitotoxic glutamate (Rothstein et al., 1996; Bush et al., 1999; Swanson et al., 2004); (ii) protection from oxidative stress via glutathione production (Chen et al., 2001; Shih et al., 2003; Swanson et al., 2004; Vargas et al., 2008); (iii) protection via adenosine release that exerts systemic inhibitory and anti-inflammatory action (Lin et al., 2008); (iv) protection from NH4+ toxicity (Rao et al., 2005); (v) protection by degradation of Aβ (amyloid β-peptide; Koistinaho et al., 2004); (vi) facilitating blood–brain barrier repair (Bush et al., 1999); (vii) reducing vasogenic oedema after trauma, stroke or obstructive hydrocephalus (Bush et al., 1999; Zador et al. 2009); and (viii) stabilizing extracellular fluid and ion balance and reducing seizure threshold (Zador et al., 2009). Different types of transgenic models from different laboratories show that either ablation or attenuation of reactive astrogliosis causes increased lesion size, increased neuronal loss, demyelination and exacerbated loss of function after traumatic injury, stroke, autoimmune attack or infection (Bush et al., 1999; Faulkner et al. 2004; Myer et al., 2006; Okada et al., 2006; Drogemuller et al., 2008; Herrmann et al., 2008; Li et al., 2008; Voskuhl et al., 2009). Together, these findings indicate that reactive astrocytes exert essential neuroprotective functions. In addition, experimental evidence indicates that reactive astrocytes play important roles in regulating CNS inflammation, and that astrocyte scars act as essential functional barriers that restrict the migration of inflammatory cells and infectious agents and limit spread into adjacent healthy tissue (Sofroniew, 2005; Sofroniew, 2009; Sofroniew and Vinters, 2010).
THE GENETIC ASTROGLIOPATHOLOGY: ALEXANDER DISEASE
In considering how astrocyte dysfunction contributes to neurological disease, interpreting most models and natural diseases is complicated since there is presumed to be pre-existing injury to other cell types that then induces the changes in astrocytes. It is worth considering the simpler situation where astrocytes are clearly the primary instigator of disease – Alexander disease. This rare disorder arises from mutations in the major intermediate filament protein of astrocytes, GFAP (Brenner et al., 2001). Although GFAP is expressed at lower levels in a number of cell types throughout the body, many lines of evidence point to initial dysfunction of astrocytes as the key initiating event that then leads to a cascade of effects, ultimately affecting every other cell type in the CNS (Brenner et al., 2009).
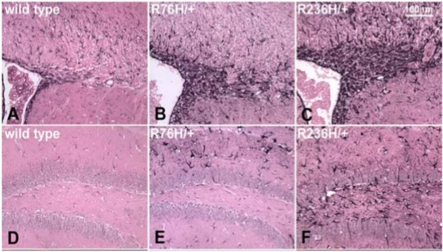
Alexander disease is generally classified among the leucodystrophies because the initial descriptions primarily focused on younger onset patients who had dramatic white matter deficits, especially involving the frontal lobes. From its initial description (Alexander, 1949), the disease was associated with distinctive pathology involving accumulations of cytoplasmic protein aggregates within the cell bodies and processes of astrocytes, known as Rosenthal fibres, which contain GFAP and other proteins (Figure 3). The most common classification is based on age of onset (early, juvenile and adult; Li et al., 2005). The younger patients typically have seizures or any of several psychomotor delays as their initial symptoms, with forebrain predominance to their lesions. In contrast, the older patients typically present with gait disturbances, bulbar signs, or autonomic dysfunction, and have a hindbrain predominance of their lesions, sometimes including atrophy of the medulla and cervical spinal cord. All forms are typically progressive, with median survivals reported as 3.6 years for the early onset group and 8 years for the juvenile group (and undefined for adult) (Li et al., 2005). A more recent classification recommends division into just two groups, Types 1 and 2, based on particular clustering of symptoms (Prust et al., 2011). In addition, survival may be longer for both groups than previously imagined.
Figure 3. Immunostaining for GFAP in brain tissue from mouse models of Alexander disease showing abundant Rosenthal fibres in the periventricular region.
GFAP immunohistochemistry in the periventricular white matter of (A) wild-type or (B, C) knock-in point mutants expressing either R76H or R236H mutant forms of GFAP (equivalent to the common R79H and R239H mutations in human GFAP). Abundant Rosenthal fibres with increased immunoreactivity for GFAP are particularly evident in periventricular and white matter astrocytes of adult mice (3 months old). Reproduced with permission from Figures 3(A)–3(C) of Hagemann et al. (2006) ©2006 Society for Neuroscience.
As noted above, all forms of Alexander disease are now associated with mutations in GFAP (Li et al., 2005). Most of these mutations are heterozygous single base pair changes within the coding region that predict single amino acid changes in the translated protein. A small number of mutations involve in frame deletions or insertions. All are heterozygous, genetically dominant, with nearly 100% penetrance. A very small number of patients with presumed Alexander disease have no identifiable coding region mutations, but in theory a similar disease could arise from other types of alterations at the GFAP locus such as promoter mutations or gene duplication. Most mutations occur de novo (as expected when survival is short), although later onset patients can survive to reproductive age and transmit the mutations to subsequent generations with typical autosomal dominant patterns of inheritance. A recent population-based survey in Japan reported a prevalence of 1 in 2.7 million, but this value may be low because the study excluded severely affected infants who died at very young ages and adult-onset patients are often missed (Yoshida et al., 2011).
How do GFAP mutations cause disease? There are no clear answers to this question yet, partly a reflection of how little we understand the normal functions of GFAP and other intermediate filaments. It is interesting that the known disease-causing mutations (now numbering 71 out of a total 432 amino acid sequence) are sprinkled throughout the rod and tail domains (Brenner et al., 2009; http://www.waisman.wisc.edu/alexander/mutations). The surprising fact is that all of these mutations essentially cause the same disease. Genotype–phenotype correlations are still only speculative, due in large part to the paucity of patients with any particular mutation. While the R239H mutations seem to consistently cause early onset disease, the R416W mutation has been found in all forms of the disease. Several examples exist of the same mutation causing different forms of the disease, even within the same family (Stumpf et al., 2003; Messing et al., 2011). It is possible that head domain mutations do occur, but are early lethal and so never reach the stage of diagnosis.
Unlike most of the other intermediate filament diseases, GFAP mutations appear to act in a gain-of-function fashion. In support of this hypothesis is the absence of truncation or null mutations among the human patients (Brenner et al., 2009), the dissimilarity in phenotype between mouse knockouts of GFAP and the human disease (Gomi et al., 1995; Pekny et al., 1995; McCall et al., 1996), and the finding that overexpression of wild-type protein alone to sufficient levels is lethal and replicates the key pathological feature of the disease, Rosenthal fibres (Messing et al., 1998). Using cell culture models, Tang and Goldman (2006) have found that forced overexpression of wild-type and mutant GFAP leads to pleiotropic effects, with activation of JNK (c-Jun N-terminal kinase) and p38 MLK (mixed-lineage kinase) stress pathways and impairment of the proteasome. One or more positive feedback loops then form to further enhance the toxic accumulation of GFAP. Paradoxically, there is also enhancement of autophagy, which occurs by both mTOR (mammalian target of rapamycin)-dependent and -independent mechanisms (Tang and Goldman, 2008). Mouse models show evidence of oxidative stress, particularly in white matter (Hagemann et al., 2006), and the cell culture models display increased sensitivity to camptothecin-induced apoptosis and H2O2-induced cell death (Tang and Goldman, 2006; Cho and Messing, 2009).
How GFAP mutations and/or excess activate these stress pathways and impact on the protein degradation machinery of the cell is not clear. Normally GFAP exists in an equilibrium between Triton-X soluble and insoluble pools, with the majority being insoluble. These two pools roughly correspond to the process by which monomers (which are soluble) gradually assemble into higher-ordered structures and finally mature intermediate filaments (which are insoluble). Expression of mutant GFAPs cause a distinct shift in this equilibrium towards the insoluble pool, perhaps reflecting the unknown proportion that accumulates in the Rosenthal fibres themselves (Hsiao et al., 2005). Interestingly, the shift towards insolubility is also displayed by the small stress protein αB-crystallin, which is a normal-binding partner of GFAP and accumulates in the Rosenthal fibres as well (Der Perng et al., 2006; Perng et al., 2008). Studies in mouse models have shown that αB-crystallin deficiency increases mortality (Hagemann et al., 2009). Perhaps αB-crystallin is sequestered to the point of deficiency? Hence, one hypothesis is that the Alexander phenotype reflects a combination of both gain of function (GFAP) and loss of function (αB-crystallin). One cannot blame the full Alexander phenotype on αB-crystallin deficiency alone; however, since mouse knockouts of αB-crystallin and humans with a nearly complete deletion at this locus have predominantly skeletal muscle phenotypes, with no evidence yet for neurological consequences (Brady et al., 2001; Del Bigio et al., 2011).
Are the astrocytes in Alexander disease simply extreme examples of reactive astrocytes? They do share some properties considered fundamental to the gliotic phenotype, such as increased expression of GFAP and the endothelin B receptor (Hagemann et al., 2006). Recent studies point towards impaired expression of the glutamate transporter Glt-1 (Hagemann et al., 2009; Tian et al., 2010), perhaps analogous to what occurs in other neurodegenerative diseases such as ALS (amyotrophic lateral sclerosis). However, as (probably) noted above, reactive astrocytes are highly diverse and likely differ considerably depending on the nature of insult, location in the nervous system, and stage of disease (Hamby and Sofroniew, 2010). In the case of Alexander disease, the initial insult is mutant GFAP, which may produce toxic forms that are unique to this condition and cause types of astrocyte dysfunction different from those in other types of reactive astrocytes. Interestingly, the Goldman laboratory has identified toxic oligomers in the soluble pool of GFAP that may be responsible for the impairment in proteasome function noted above, and also showed that this effect could be mitigated by co-expression of the small stress protein, αB-crystallin (Tang et al., 2010). That αB-crystallin may be a key modifier of astrocyte function, and potential therapeutic target, is also indicated by its ability to rescue mouse models of Alexander disease from an otherwise lethal phenotype induced by GFAP mutations and excess (Hagemann et al., 2009).
Despite the many gaps in our understanding of the mechanisms and impact of astrocyte dysfunction in Alexander disease, several strategies for therapy have been suggested (Messing et al., 2010). The most obvious approach is to reduce the expression or accumulation of GFAP, so as to avoid the initial insult that drives the entire process. One drug screen has already been completed using wild-type astrocytes in primary culture (Cho et al., 2010), and similar drug screens using astrocytes expressing mutant protein are underway. A second approach is to target downstream effects of GFAP toxicity, such as the proposed change in Glt-1 expression. Ceftriaxone, already in clinical trials for ALS, may be a good candidate for such an approach (Rothstein et al., 2005). Finally, manipulation of stress pathways such as those regulating αB-crystallin may prove effective. New Drosophila models of GFAP toxicity in glia have just been developed that will prove especially valuable for dissecting the pathways to dysfunction, and may even be suitable for drug screening (Wang et al., 2011a).
THE ACUTE ASTROGLIOPATHOLOGY: ISCHAEMIA AND STROKE
Stroke remains a major source of death and disability in the United States as a stroke-induced death occurs every 3 min. Over the past couple of decades, dozens of clinical trials tested neuroprotective agents in the treatment of stroke. These efforts largely targeted neuronal-specific cell death ignoring the roles of other cell types such as astrocytes, microglia and the vasculature. The failure of these trials has evoked a keen interest in elucidating the influence of non-neuronal cell types on brain survival and function during stroke. As discussed in detail at the beginning of this paper a large body of literature supports a pivotal influence of astrocytes on multiple processes within the brain, which impact the survival and function of neurons as well as the vasculature. Yet, astrocyte function may be both protective and harmful. Interestingly, the same molecule released by astrocytes may have opposing actions on brain tissue viability depending on their temporal expression following stroke. Determining the critical temporal windows and the molecular mechanisms by which astrocyte function either reduces or enhances injury is important to discern and will be a matter of the discussion to follow.
During the first few hours after the onset of ischaemia, the acute phase of stroke, several astrocyte functions may reduce ischaemic damage including the uptake of glutamate, scavenging of reactive oxygen species and uptake of K+ (Chen and Swanson, 2003). Yet many of these functions are likely compromised in the inhospitable environment of the ischaemic brain. In the stroke core, where glucose and oxygen supply are greatly reduced, the severe loss of energy substrates can lead to astrocyte membrane depolarization and death. If the membrane potential of astrocytes is compromised too severely, glutamate flux may reverse leading to release of glutamate by astrocytes and neuronal excitotoxicity. Although astrocytes in culture are more tolerant to OGD (oxygen glucose deprivation) compared with neurons, they are particularly susceptible to damage during acidosis and when ion concentrations of Na+ and Ca2+ are altered to model those found in the stroke core (Giffard et al., 1990, 2000; Chesler, 2005). In fact, some studies suggest that astrocytes may be more vulnerable to ischaemia than neurons (Garcia et al., 1993; Liu et al., 1999), although this point is debated (Gurer et al., 2009). Regardless, when astrocyte death occurs through necrosis, this unstructured loss of intracellular constituents into the extracellular space would be expected to enhance stroke damage by increasing inflammation and oedema.
Given that cell death in the stroke core occurs early and is overwhelming, research has focused on preventing delayed neuronal death in the stroke penumbra and reducing the growth of stroke volume in the hours and days after stroke onset. One clinical trial manipulated astrocyte function as a means to diminish the delayed growth of stroke volume. One of the mechanisms by which astrocytes likely enhance neuronal death following stroke is through the release of S100β (Matsui et al., 2002), which is toxic to neurons when present at high levels (Hu et al., 1997). AA (arundic acid; ONO-2506) was identified through a chemical screen as a compound that could diminish activation of astrocytes and S100β expression. In fact, AA reduced delayed growth of infarct volume and improved functional outcome in rodents (Tateishi et al., 2002). The protective effect of AA was greater if administered 24 h after stroke onset compared with its administration immediately after stroke onset, suggesting that its window of efficacy is very much extended compared with most neuroprotectants. A multiple-centre trial testing the efficacy of AA to reduce stroke-related disability was conducted. However, this trial was terminated early for lack of efficacy. Yet, clinical studies suggest that growth of stroke volume occurs in a subset of patients (Sorensen et al., 1996; Beaulieu et al., 1999; Barrett et al., 2009). As such, this delayed growth of stroke volume may be a worthy target for future work if this subset of patients can be reliably identified and targeted.
In the days and weeks after stroke onset, astrocytes release a number of neuroprotectants including EPO (erythropoietin), VEGF (vascular endothelial growth factor) and glial-derived neurotrophic factor, all of which may either reduce ischaemic neuronal damage or improve functional recovery following stroke (Kitagawa et al., 1999; Zhang et al., 2000; Hermann et al., 2001; Harvey et al., 2003; Jelkmann and Wagner, 2004; Chavez et al., 2006). In particular, the neuroprotective properties of EPO have been studied (Masuda et al., 1994; Marti et al., 1997; Ruscher et al., 2002; Prass et al., 2003). For example, EPO reduces neuronal death with OGD (Ruscher et al., 2002), glutamate toxicity (Morishita et al., 1997), and nitric oxide induced death (Sakanaka et al., 1998). Conditioned media taken from hypoxic astrocyte cultures is protective to neurons exposed to OGD through the actions of EPO, demonstrating the importance of astrocytes in mediating neuroprotection under these circumstances (Chavez et al., 2006). Similar to the in vitro experiments, protective effects have been described for EPO in vivo during stroke ( Bernaudin et al., 1999; Siren et al., 2001). Clinical trials were performed to establish the safety and efficacy of EPO in stroke treatment. An initial Phase II trial did not identify any safety concerns and suggested efficacy of EPO protection in acute stroke (Ehrenreich et al., 2002). A subsequent Phase III double-blinded, placebo-controlled trial enrolled 522 patients (Ehrenreich et al., 2009). Patients were treated with EPO within 6 h of the onset of their symptoms and clinical outcome was evaluated at 30 and 90 days after stroke (Ehrenreich et al., 2009). Unfortunately, EPO did not improve clinical outcome compared with the placebo. This negative result reminds us that all neuroprotective trials are hampered by the problem of delivery of a compound to a poorly perfused area of brain within a short time-frame after stroke onset. Yet, EPO could still be a potential agent to improve functional outcome after stroke. For example, EPO has multiple restorative functions, including promoting angiogenesis and neurogenesis (Shingo et al., 2001; Byts and Siren, 2009; Siren et al., 2009). To harness the restorative power of EPO in stroke, it is important to examine the mechanisms by which the temporal expression of endogenous EPO may be enhanced in astrocytes following stroke.
The transition from the acute stroke period to the sub-acute/chronic time frame after stroke can dramatically change the functional consequences of astrocyte-released proteins. Both VEGF and MMP-9 (matrix metalloproteinase-9) have dramatically different effects in the acute versus sub-acute time frames following onset of ischaemia. VEGF is expressed in astrocytes, as well as other cell types, during hypoxia and stroke (Sinor et al., 1998; Lee et al., 1999). While VEGF is neuroprotective in culture (Jin et al., 2000), administration of VEGF at the onset of stroke increases stroke volume (Jelkmann and Wagner, 2004). This pathological effect of VEGF is mediated by the ability of VEGF to enhance blood–brain barrier permeability, which leads to brain oedema. In contrast, when administered 2 days after stroke onset during the sub-acute stroke period, VEGF enhances angiogenesis and recovery from stroke (Jelkmann and Wagner, 2004). Thus, the protective or pathological actions of VEGF are determined by its temporal expression. Similarly, MMP-9 has pathological or adaptive functions depending on its temporal expression following stroke (Zhao et al., 2006). MMPs cleave extracellular matrix proteins, which are important in modulating cellular interactions during tissue remodelling in disease and trauma. It is well described that MMP-9 increases blood–brain barrier permeability and increases ischaemia-induced damage during acute stroke (Cunningham et al., 2005; Jian Liu and Rosenberg, 2005). In contrast, several days after stroke onset MMP-9 serves a neuroprotective role by cleaving and activating VEGF (Zhao et al., 2006). During this delayed time-frame, MMP is highly expressed on both astrocytes and neurons. In addition, VEGF localizes primarily to astrocytes, suggesting that astrocytes significantly contribute to this protective function of MMP-9. These temporally distinct and divergent actions of VEGF and MMP-9 demonstrate the important concept that astrocyte function may change from a pathological to adaptive depending on the temporal profile of expression following ischemia. As such, future therapeutics targeting these functions will need to carefully consider these critical time windows for intervention.
In the weeks to months following stroke onset, profound synaptic plasticity occurs in the peri-infarct cortex, which influences functional recovery (Carmichael, 2003; Nudo, 2007). Astrocytes have prominent roles in modifying synaptic plasticity and formation of new synapses (see above). Emerging evidence suggests that astrocytes release extracellular matrix proteins that encourage neurite outgrowth and plasticity and therefore may be a target for therapeutic intervention. For example, the TSP1/2 (thrombospondins 1 and 2), which are extracellular glycoproteins, are highly induced after stroke on astrocytes (Liauw et al., 2008). In cultures, the application of TSP1/2 enhances synaptogenesis several fold (Christopherson et al., 2005). Interestingly, in stroke models, synaptic number and axonal sprouting were reduced in transgenic knockout mice lacking TSP1/2 function (Liauw et al., 2008). Recovery of functional tests was also diminished in these TSP1/2 KO mice. Based on these results, designing treatments that increase TSP1/2 function or astrocyte release of TSP 1/2 may enhance stroke recovery.
Similar to the above discussions, the effect of reactive astrocytosis is also dependent on its time course after acute head trauma. The role of reactive astrocytes has traditionally been viewed as a process leading to glial scar formation, reducing the ability of the brain to form new synaptic connections and axon outgrowth. Yet, work over the last several years has illustrated that reactive astrocytosis contributes to tissue survival in several conditions, which is in part dictated by the time course after injury in which it occurs. One tool for examining reactive astrocytes is by utilizing transgenic mice with loss of GFAP and vimentin (Pekny and Nilsson, 2005). These mice have diminished reactive astrocytosis. Interestingly, the effect of reactive astrocytosis changes temporally after injury. For example, after neurotrauma, GFAP−/−:Vimentin−/− mice have increased loss of synapses during the acute phase of the injury, but synaptic number is enhanced in the weeks following acute injury (Wilhelmsson et al., 2004). In stroke, GFAP−/−:Vimentin−/− mice have increased stroke volume, suggesting a protective role under these conditions (Li et al., 2008). Similarly, ablation of proliferating reactive astrocytes enhanced spinal cord injury following spinal cord trauma (Faulkner et al., 2004) and traumatic brain injury (Myer et al., 2006), while it also enhanced neurite outgrowth (Bush et al., 1999).
THE CHRONIC ASTROGLIOPATHOLOGY: EPILEPSY
Epilepsy or the occurrence of recurrent seizures is a behavioural syndrome, that is, a component of several neurological conditions. Several brain foci associated with seizure generation are populated by increased numbers of astrocytes. Such foci include hippocampal seizure foci in temporal lobe epilepsy, several types of mass lesions in the brain (low-grade astrocytomas, oligodendrogliomas and arteriovenous malformations) and tuberous sclerosis. Gliotic scar formation is a prominent feature of human epilepsy (Foerster and Penfield, 1930; Penfield and Humphreys, 1940). What is the role of astrocytes in epileptogenesis in these neurological conditions?
Epileptogenesis literally means the beginning of epilepsy or spontaneous recurrent seizures. Do astrocytes play a role in the mechanisms necessary for spontaneous seizures to first appear or do astrocytes play a role in seizure maintenance in the chronic stages of epilepsy? There is some evidence to support a primary role of astrocytes in seizure generation, particularly in animal models. In the EL (epileptic) mouse the hippocampus is important for the generation of behavioural seizures. However, there is no neuronal injury or loss in this model but an increase in expression of astrocytes around the age when seizures appear (Drage et al., 2002), and these astrocytes have reduced glutamate transporters, suggesting a primary role for astrocytes, perhaps through defective glutamate clearance at the seizure focus (Ingram et al., 2001). More direct evidence is found mice in which there is astrocyte-specific inactivation of the Tsc1 gene (Tsc1 cKO mice). In these mice, there is an increase in proliferating GFAP-immunoreactive astrocytes throughout the brain (Uhlmann et al., 2002), with the most distinctive histological alterations seen in the hippocampus. What is significant is that these astrocyte-specific cKO mutant mice did not show cortical tubers or defects in neocortical lamination. These mice have electrographically confirmed seizures shortly after astrocyte proliferation has begun (Uhlmann et al., 2002). Further, the astrocytes in Tsc1 cKO exhibit decreased expression of the glutamate transporters GLT-1 and GLAST and a functional decrease in glutamate transport current in astrocytes in hippocampal slices and astrocyte cultures (Wong et al., 2003). Such changes in glutamate transporters may lead to the extracellular accumulation of glutamate, which could cause hyperexcitability of neurons and seizures. Cultured Tsc1-deficient astrocytes and hippocampal slices from cKO mice also exhibited reduced Kir currents and decreased expression of specific Kir channel protein subunits Kir2.1 and Kir6.1. Thus impaired extracellular K+ uptake by astrocytes may also contribute to neuronal hyperexcitability and epileptogenesis in this Tsc1 cKO mouse model (Jansen et al., 2005).
Much of our understanding of the role of glia in human epilepsy is obtained from the study of seizure foci surgically removed for the control of medically intractable seizures (de Lanerolle et al., 2010). The one limitation in studying human tissue that it is taken from patients is that they have had seizures for a considerable period (6–20 years) prior to surgery. Thus it is more difficult to draw conclusions from this patient group on the role of astrocytes in the early (acute) stages of epileptogenesis.
The seizure focus that has received the most study is the hippocampus from patients with medically intractable temporal lobe epilepsy. The examination of such hippocampi indicates that approximately 40–65% of these hippocampi have hippocampal sclerosis. Eighty percent of these sclerotic patients have an excellent surgical outcome. The sclerotic hippocampi have a very high density of astrocytes and these astrocytes have many distinctive properties compared with astrocytes from non-sclerotic hippocampi. Differences in these astrocytes are seen in their cell membrane properties – they show increased expression of the glutamate receptors mGluR2/3 (metabotropic glutamate receptor 2/3); mGluR4, mGluR8 and GluR1 receptors that have an elevated ratio of flip-to-flop mRNA splice variants (Seifert et al., 2002, 2004). The expression of membrane transporter molecules is also altered. Prominent among these are aquaporin 4 molecules, where their polarity of distribution on the astrocytes is altered with reduced expression on the perivascular end feet and unchanged on the membrane facing the neuropil. The GABA (γ-aminobutyric acid) transporter GAT-3 (GABA transporter 3) expression is increased on protoplasmic astrocytes in regions of relative neuronal sparing such as dentate gyrus and hilus. There is some disagreement in the literature as to whether the glutamate transporters EAAT1 (excitatory amino acid transporter 1) and EAAT2 are also reduced. The membrane Na+ channels and α1C subunit of the calcium ion channels are also up-regulated, suggesting that astrocytes in sclerotic hippocampi have a significant change in their membrane current characteristics. The inwardly rectifying potassium ion (Kir4.1) channels are also shown to be impaired, significantly impeding removal of K+ ions from the extracellular space (Bordey and Sontheimer, 1998; Hinterkeuser et al., 2000; Schroder et al., 2000). Among the astrocyte specific enzymes, glutamine synthetase activity is reduced (Eid et al., 2004), impeding glutamate clearance and thus leading to increases in extracellular glutamate levels (During and Spencer, 1993). There is also a reduced capacity for glutamine synthesis and ammonia detoxification. Levels of other astrocyte specific enzymes such as GDH (glutamate dehydrogenase), aspartate aminotransferase and lactate dehydrogenase (Malthankar-Phatak et al., 2006) are also altered in astrocytes in sclerotic hippocampi.
Gene expression studies in sclerotic hippocampi have also suggested changes in the expression of several genes associated with astrocytes. Among those up-regulated are those involved with immune and inflammatory functions, including several chemokines and cytokines, class II MHC antigen genes and interleukins and complement factors (Aronica et al., 2007; Lee et al., 2007). Several molecules associated with the astrocyte/microvascular interface are also altered, in particular increases in EPO-r (EPO receptor), the MDR1 (multidrug resistance gene-1) encoded P-glycoprotein (Tishler et al., 1995), CD44 and plectin 1 (Lee et al., 2007), among others (de Lanerolle et al., 2010).
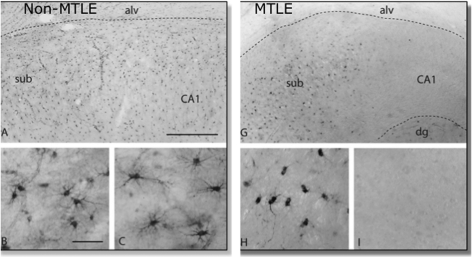
Associated with the above molecular anatomical changes in astrocytes in sclerotic hippocampi are also changes in their function. Some astrocytes in primary cultures derived from sclerotic hippocampi and in vitro hippocampal slices are capable of generating action potential-like responses in response to depolarizing currents (Bordey and Sontheimer, 1998; O'Connor et al., 1998). Astrocytes from sclerotic hippocampi respond to glutamate with elevated intracellular Ca2+ release and Ca2+ oscillations and waves (Lee et al., 1995). Additionally, several lines of evidence suggest that the altered properties of sclerotic astrocytes, particularly down-regulation of glutamine synthetase, also alter glutamine–glutamate cycling in hippocampal seizure foci resulting in increased extracellular glutamate levels before and during seizures (Figure 4).
Figure 4. Expression of glutamine synthetase immunoreactivity in a non-sclerotic and sclerotic hippocampus.
Glutamine synthetase immunoreactivty in the subiculum/CA1 region in a non-sclerotic [non-MTLE (mesial temporal lobe epilepsy)] (A) and sclerotic (MTLE) (G) hippocampus. Neurologically normal autopsy hippocampus shows a pattern of staining exactly similar to (A). (B, C) in higher magnification shows GS immunopositive astrocytes in both the subiculum and CA1 area of a normal or non-sclerotic hippocampus. The sclerotic hippocampus, in which the subiculum does not have neuronal loss shows GS immunoreactive astrocytes (H), whereas the neuron-depleted astrocyte-rich CA1 area (I) shows depletion of GS in astrocytes. (A and G) Scale bar = 0.5 mm. (B, C, H and I) Scale bar = 100 μm. Reprinted from The Lancet, 363, Eid T, Thomas MJ, Spencer DD, Runden-Pran E, Lai JC, Malthankar GV, Kim JH, Danbolt NC, Ottersren OP, de Lanerolle NC, Loss of glutamine synthetase in the human epileptogenic hippocampus: possible mechanism for raised extracellular glutamate in mesial temporal lobe epilepsy, 28-37, Copyright (2004), with permission from Elsevier.
More recent studies suggest the recognition of two functional classes of astrocytes. One type, sometimes referred to as GluR cells, is weakly positive for GFAP, expresses AMPA-type glutamate receptors and properties akin to NG2 cells. These cells are excitable (O'Connor et al., 1998). A second type of cell, the GluT cell, is more strongly GFAP positive, is more fibrous in appearance and expresses K+ channels, but lack glutamate receptors (Matthias et al., 2003). Cells similar to GluR and GluT cells have been recognized in the human hippocampus, and though both types are found in normal hippocampi, an almost complete loss GluT cells is reported in sclerotic hippocampi (Hinterkeuser et al., 2000). It is most likely that it is these cells that have impaired Kir channels. Further, the GluR cells in sclerotic hippocampus have increased levels of the Flip isoform of GluR1 receptor, suggesting an increased potential for excitability.
What role do astrocytes play in a mature hippocampal seizure focus? As the above review suggests, they may play several roles. (i) Astrocytes may contribute to the high glutamate levels at seizure foci through defective glutamate clearance, and additionally active release of glutamate from GluR (NG2)-like cells due to enhanced intracellular Ca2+ release or by astrocyte swelling due to reduced aquaporin 4 transporters on perivascular end feet (de Lanerolle et al., 2010). These elevated glutamate levels may activate neurons in surrounding or adjacent undamaged regions such as the subiculum to generate seizure activity. (ii) Defective astrocytes may contribute increased extracellular potassium in the seizure focus. Impaired inwardly rectifying K+ channels and decreased water flux due to reduced AQP transporters in astrocytic end feet may be contributory factors. (iii) The presence of excitable GluR or NG2-like cells with more glutamate-sensitive GluR1 receptors in the sclerotic seizure focus may directly contribute to an excitable focus. (iv) Astrocytes may also modulate the microvasculature, leading to vascular permeability and promoting entry of substances such as albumin or circulating leucocytes into the brain parenchyma with consequent seizure promoting effects (de Lanerolle et al., 2010). (v) The release of inflammatory and immune factors by astrocytes may also contribute to the development of the seizure focus in ways that are only just beginning to be understood.
Another interesting aspect of epilepsy is the destruction and loss of astrocytic domain organization (Figure 5). Several groups have shown that in the normal brain cortical and hippocampal astrocytes are organized in non-overlapping spatial domains with limited interdigitation of processes of adjacent cells (Bushong et al., 2002; Ogata and Kosaka, 2002; Halassa et al., 2007a, 2007b). Through a process termed ‘tiling,’ astrocytic processes grow within exclusive territories during development when neuronal and vascular territories are also being established. In the rodent brain, one astrocytic domain encompasses ∼100000 synapses, whereas this number rises to 2000000 synapses in the brain of homo sapiens (Bushong et al., 2002; Oberheim et al., 2006). Each domain represents an area of the neuropil that is under control of a single astrocyte, being also an entity of synaptic modulation that is independent of neural networking. All synapses within one territory will be contacted by processes from only one single astrocyte. Reactive astrocytes in three very different murine models of epilepsy (post-traumatic injury, genetic susceptibility and systemic kainate exposure) all were associated with a 10-15-fold increase in overlap of processes of neighbouring astrocytes (Oberheim et al., 2008). A similar loss of astrocytic domain organization was noted in tissue surgically resected from patients resilient to medical treatment. It is important to note that astroglial domain organization was preserved in APP transgenic mice expressing a mutant variant of human amyloid precursor protein despite a striking up-regulation in GFAP expression. Thus, while the functional consequences of loss of astrocytic territories have not been established, it appears to be specifically linked to epilepsy. It is tempting to speculate that synapses receiving input from more than one astrocyte may not function optimally.
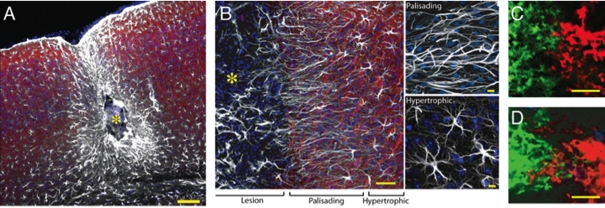
Figure 5. Organization of reactive astrocytes in a model of post-traumatic epilepsy induced by cortical injection of a ferrous chloride solution.
(A) Site of cortical injury 6 months after injury. The centre of the lesion (yellow asterisk) is surrounded by palisading astrocytes and, at a greater distance, by hypertrophic astrocytes. The mouse exhibited daily multiple generalized grand mall seizures. (B) Higher power image of a similar lesion displaying palisading and hyperthrophic astrocytes. White, GFAP; red, Map2; blue, Sytox. (C, D) Neighbouring astrocytes in control, non-EL brain exhibit little overlap of processes (C), whereas extensive overlap of processes between two adjacent astrocytes is evident in a mouse with epilepsy (D). Neighbouring astrocytes were duolistically labelled with DiL (green) or DiD (ref). Scale bar = 100 μm (A), 50 μm and 10 μm (B), 10 μm (C, D). See Oberheim et al. (2008) for details.
Are these changes in astrocytes in the hippocampal seizure focus secondary mechanisms in seizure development or are they causative? Comparison of these observations with animal studies discussed above, where astrocytes appear to have a more primary role in epilepsy, show that at least some of the astrocytic changes in the human focus may be causative, in particular impairment of Kir channels and decreased expression of astrocytic glutamate transporters.
THE CHRONIC ASTROGLIOPATHOLOGY: NEURODEGENERATIVE DISEASES
Neurocentric views dominate our current understanding of neurodegeneration, which is generally defined as a process of neuronal death that underlie specific neurological deficits. At the same time it becomes clear that idiosyncratic lesions associated with different forms of neurodegenerative diseases (such as for example senile plaques or Lewy bodies) appear at the late stages of neurodegenerative pathologies and massive neuronal demise signals terminal stages of the disease. Our knowledge about early stages of neurodegenerative processes (when arguably the disease can be either halted or slowed down) is remarkably limited, and yet data accumulate suggesting that neurodegeneration begins from failures in brain homoeostasis and alterations in connectivity of neural networks that signals early cognitive impairments (Terry, 2000; Kano and Hashimoto, 2009; Nedergaard et al., 2010; Heneka et al., 2010). The many levels of brain homoeostasis (cellular, micro-architectural, vascular, metabolic, neurotransmitter, ion, etc.) are controlled almost solely by neuroglia; and it is neuroglia that mount brain defence. With this in mind the progression of majority (if not all) of CNS disorders are determined by the ability of neuroglia to keep brain homoeostasis in stressed conditions, and the failure of glia to maintain homoeostatic balance signals irreparable damage and ultimate death of the neural tissue (Giaume et al., 2007). The pathological potential of astroglia in neurodegeneration is explored only superficially and yet (as we shall overview below) they seem to be involved in both early and late stages of many neurodegenerative diseases.
Astroglia in AD (Alzheimer's disease)
The pathological potential of neuroglia in dementia praecox was for the first time recognized by Alois Alzheimer, who found that glia populated senile plaques and closely contacted damaged neurones (Alzheimer, 1910). Conceptually there are two types of astroglial reactions observed in AD-affected brain tissues (Figure 6). Astroglial hypertrophy associated with increased GFAP and S100β levels, all indicative of generalized astrogliosis, are often observed in the post-mortem human tissues (Beach and McGeer, 1988; Griffin et al., 1989; Nagele et al., 2004; Mrak and Griffin, 2005), and similarly astrogliosis is detected in various AD animal models (Nagele et al., 2003; Rodriguez et al., 2009; Heneka et al., 2010). There is a degree of correlation between severity of astrogliosis and cognitive decline, although reactive astrocytes are not always associated with senile plaques (Simpson et al., 2010). The levels of GFAP alone cannot be predictable as little difference in GFAP expression was found in brains from non-demented and demented patients (Wharton et al., 2009). The second reaction of astroglia to AD progression was found recently in an animal model of familial AD, where reaction is manifest in the generalized decrease of morphological presence of astrocytes signalling astroglial atrophy/degeneration. The atrophic changes in astrocytes were detected in several brain regions, including hippocampus, pre-frontal and entorhinal cortex (Olabarria et al., 2010; Kulijewicz-Nawrot et al., 2011; Olabarria et al., 2011; Yeh et al., 2011). The astroglial atrophy preceded the appearance of senile plaques and appeared first (as early as 1-month-old animals) in the entorhinal cortex, the region earliest affected by the AD pathology. Atrophic changes in astroglia were also observed in the neocortices from the post-mortem demented human brains (Senitz et al., 1995).
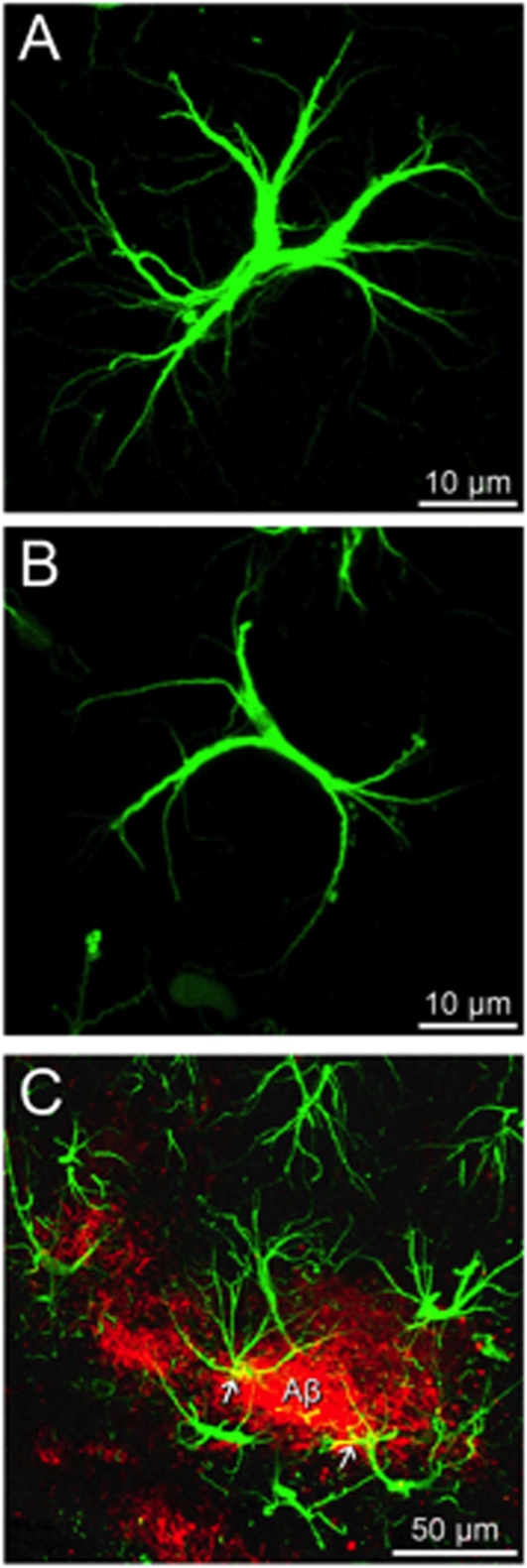
Figure 6. Astrocytes in neurodegeneration.
(A) Fluorescence micrographs illustrating a normal hippocampal astrocyte labelled with anti-GFAP antibody with elongated and multiple radial processes in an old (18 months) control animal. (B) In age-matched 3×TG-AD animals, astrocytes show a morphological atrophy with a significant reduction in cell soma volume and area as well as a reduction in the number and width of processes. (C) Confocal image showing hypertrophic astrocytes (green) concentrated around Aβ plaques (red); occasionally some of the astrocytes show intracellular Aβ accumulation (yellow). Scale bar (A and B): 10 μm; (C): 50 μm.
How do these two concomitant processes may affect homoeostatic/neuroprotective abilities of astrocytes? The answer to this question remains virtually unknown; for example several contradictory reports indicate that astrocytes in AD brain can participate in both clearance and degradation of Aβ (Guenette, 2003; Nicoll and Weller, 2003) as well as in the production of the latter (Heneka et al., 2005; Rossner et al., 2005). Astroglial accumulation and degradation of Aβ was shown in vitro (Wyss-Coray et al., 2003) and was observed in post-mortem entorhinal preparations (Nagele et al., 2003). Furthermore, it was found that reactive astrocytes from AD model mice (Tg2576) express the amyloid-degrading enzyme neprilysin (Apelt et al., 2003). Astroglial accumulation of Aβ, however, was very rarely found in 3×TG-AD mice (Rodriguez et al., 2009; Olabarria et al., 2010). At the same time astroglial production of Aβ was also reported: it appeared that, in conditions of chronic stress or amyloid load, reactive astrocytes begin to express γ-secretase (which normally is expressed only in neurons) and thus contribute to Aβ production (Hartlage-Rubsamen et al., 2003; Heneka et al., 2005; Rossner et al., 2005). The Aβ was additionally found to remodel astroglial metabolism, although the data remain similarly controversial: both increased (Allaman et al., 2010) and decreased (Soucek et al., 2003; Schubert et al., 2009) glucose utilization by Aβ-treated astrocytes were reported. This polymorphism of pathological astroglial phenotypes most likely results from multifaceted glial reaction to AD-like pathology which includes atrophic and astrogliotic changes.
Astrocytes in ALS
Clinical symptoms of ALS result from rapid progressive degeneration of motor neurons in the cortex, in the brain stem and in the spinal cord. Neuroglial reactions are prominent in ALS and most interestingly the early changes (observed in the human SOD1G93A transgenic mouse model) are represented by astroglial degeneration and atrophy which preceded both neuronal death and clinical manifestation (Rossi et al., 2008; Rossi and Volterra, 2009). Astrocytes selectively expressing hSOD1 demonstrated glutamate excitotoxicity, and inhibition of SOD1 expression selectively in astrocytes retarded the ALS progression in transgenic animals (Yamanaka et al., 2008). At the late disease stages, prominent astrogliosis is observed, although atrophic astrocytes still can be visualized (McGeer and McGeer, 2002; Rossi et al., 2008).
Astrocytes in Parkinson's disease
The pathological role of astrocytes in Parkinson's disease is unknown; the late stages of the disease are characterized by reactive astrogliosis (McGeer and McGeer, 2008; Mena and Garcia de Yebenes, 2008). The density of astrocytes in the substantia nigra, which is primarily affected by PD pathology, is the lowest in the brain (Mena and Garcia de Yebenes, 2008). This may explain specific vulnerability of substantia nigra neurons to stress factors; in addition, astroglial cells are known to protect dopaminergic neurones in vitro and are instrumental for neuronal utilization of L-DOPA (Mena et al., 1996, 1999; Mena and Garcia de Yebenes, 2008).
Astrocytes in Wernicke encephalopathy
Wernicke encephalopathy, most likely caused by thiamine deficiency which triggers thalamo-cortical lesions resulting in ataxia, ophthalmoplegia and mental changes, is an example of specific astrodegeneration. Indeed the leading mechanism for the cause of severe excitotoxicity and neuronal death in Wernicke encephalopathy is the dramatic (up to 70%) decrease in expression of astroglial glutamate transporters EAAT1 and EAAT2 that compromises glutamate uptake. The decrease in EAAT1/EAAT2 was detected in human post-mortem tissues and in the rat thiamine-deficiency model of the disease (Hazell, 2009; Hazell et al., 2009). The signs of astroglial atrophy observed in Wernicke encephalopathy also include significant decrease in expression of GFAP, of glutamine synthetase and astroglial GAT-3 (Hazell, 2009; Hazell et al., 2009).
Astrocytes in non-AD dementia
Astroglial degeneration is also observed in various forms of non-AD neurodegeneration/dementia. Significant astrodegeneration and astroglial apoptosis was observed in early stages of fronto-temporal dementia; the degree of astrodegeneration was reported to correlate with the severity of dementia (Broe et al., 2004). In addition to these atrophic changes, profound astrogliosis was detected in post-mortem tissues form patients with fronto-temporal dementia (Kersaitis et al., 2004). In thalamic dementia astrogliosis was suggested to lead to neuronal death (Potts and Leech, 2005). HIV-1-associated dementia is also characterized by astrogliosis and astrodegeneration; the degree of astroglial loss was reported to correlate with cognitive deficit (Thompson et al., 2001; Vanzani et al., 2006).
Astrodegeneration and astrogliosis drive neurodegeneration?
Analysis of the recent literature indicates the existence of multifaceted astroglial reactions in the progression of various neurodegenerative processes. Almost invariably these reactions are represented by astrodegeneration/astroglial atrophy and reactive astrogliosis. Balance between these two processes can determine the progression and outcome of the disease, thus placing astrocytes at the very core of neurodegenerative pathology (Rodriguez et al., 2009; Heneka et al., 2010; Verkhratsky et al., 2010; Rodriguez and Verkhratsky, 2011). Early astrodegeneration, for example, may be responsible for initial cognitive impairments that accompany early stages of neurodegenerative diseases. It is well demonstrated that the earliest morphological symptoms of AD are represented by synaptic loss and the extent of this loss correlates with the degree of dementia (DeKosky and Scheff, 1990; Terry et al., 1991; Samuel et al., 1994; Coleman et al., 2004). Astroglial atrophy may indeed be the mechanism of early synaptic failure in neurodegeneration: reduced astroglial coverage impacts upon synaptic metabolic support, synaptic maintenance and neurotransmitter homoeostasis and turnover. Furthermore, astroglial degeneration affects brain homoeostasis and favours excitotoxicity. At the more advanced stages of neurodegeneration appearance of specific lesions triggers reactive astrogliosis and microglial activation, which acting in concert mount neuroinflammatory responses that ultimately lead to neuronal death and brain atrophy. Would this hypothesis survive the scrutiny of experimental test? Only specifically designed research can provide an answer.
CONCLUSIONS: POTENTIAL PATHOLOGICAL CONSEQUENCES OF ASTROCYTE LOSS OR GAIN OF FUNCTIONS
Based on the many different essential roles played by astrocytes in the healthy CNS, it appears likely that the loss of normal functions or gain of abnormal effects by astrocytes has the potential to lead to neuronal dysfunction or degeneration. In this regard, the potential for genetic polymorphisms in different individuals to influence astrocyte functions and dysfunctions may be of clinical interest. Both experimental and clinical examples now exist of how loss of astrocyte functions can precipitate neuronal dysfunction or degeneration. Transgenic mouse models show that deletion of genes selectively from astrocytes can lead to non-cell-autonomous neuronal dysfunction and degeneration. For example, selective deletion from astrocytes of either the endoribonuclease, Dicer, or of the Wnt-signalling pathway gene, APC (adenomatous poliposis coli), in both cases leads to cell-non-autonomous neuronal degeneration of cerebellar Purkinje neurons and in the case of Dicer, also of cerebellar granule neurons (Tao et al., 2011; Wang et al., 2011a). Similarly, the loss of function associated with astroglial atrophy can assume pathological relevance in synaptic weakening and decreased neuronal support in various forms of neurodegenerative pathology as discussed above. In addition, gain-of-function transgenic models indicate that selective targeting to astrocytes of a mutant form of the SOD (superoxide dismutase) associated with ALS leads to neuronal degeneration (Lobsiger and Cleveland, 2007; Nagai et al., 2007; Yamanaka et al., 2008). As the first recognized clinical example of an astrocyte genetic disorder, mutations in the astrocyte protein, GFAP, have been identified as the cause of neuronal dysfunctions, including seizures, in the human clinical syndrome known as Alexander disease. The prominent association of reactive astrocytes with essentially all CNS insults has the potential for the functions or dysfunctions of these cells to influence CNS pathologies. Combination of mouse models of transgenic astrocyte manipulations with experimental models of CNS injury or disease show that genetic modulations of reactive astrogliosis and scar formation can markedly alter tissue repair, disease progression and functional outcome, such that ablation of astrocytes and attenuation of certain astrocyte functions exacerbates disease progression and tissue degeneration and worsens functional outcome (Bush et al., 1999; Faulkner et al., 2004; Myer et al., 2006; Drogemuller et al., 2008; Herrmann et al., 2008, Li et al., 2008; Voskuhl et al., 2009), whereas deletion of certain astrocyte genes appears to improve outcome in some situations (Brambilla et al., 2005, 2009; Okada et al., 2006). It is also important to acknowledge that human astrocytes are large, complex, and likely terminally differentiated cells. Astrocytes in rodent brains are several-fold smaller and maintain the potential for dividing. The much longer lifespan of humans combined with the more complex population of astrocytes, suggest that human astrocytes may participate to an even greater extent to disease progression than observations in rodent models suggest. Collectively, multiple findings point towards an enormous, yet incompletely understood, potential for astrocytes to contribute to, or play primary roles in, disease processes, tissue repair and functional outcome in a wide variety of clinical conditions (Sofroniew and Vinters, 2010), including stroke, epilepsy and neurodegenerative diseases.
Footnotes
Our own work was supported by the National Institutes of Health [grant number NS057624], National Multiple Sclerosis Society and Wings for Life, the Alzheimer's Research Trust Programme [grant number ART/PG2004A/1] to A.V. and J.J.R.; the Grant Agency of the Czech Republic [grant numbers GACR 309/09/1696 and GACR 304/11/0184] to J.J.R. and [grant numbers GACR 305/08/1381 and GACR 305/08/1384] to A.V.; by The Spanish Government, Plan Nacional de I+D+I 2008-2011 and ISCIII-Subdirección General de Evaluación y Fomento de la investigación [grant number PI10/02738] to J.J.R. and A.V. and the Government of the Basque Country [grant numbers AE-2010-1-28, AEGV10/16 to J.J.R., NS42803, HD03352 to A.M. and NS075177, NS078304 to M.N.].
REFERENCES
- Abbott NJ. Dynamics of CNS barriers: evolution, differentiation, and modulation. Cell Mol Neurobiol. 2005;25:5–23. doi: 10.1007/s10571-004-1374-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alexander WS. Progressive fibrinoid degeneration of fibrillary astrocytes associated with mental retardation in a hydrocephalic infant. Brain. 1949;72:373–381. doi: 10.1093/brain/72.3.373. [DOI] [PubMed] [Google Scholar]
- Allaman I, Gavillet M, Belanger M, Laroche T, Viertl D, Lashuel HA, Magistretti PJ. Amyloid-β aggregates cause alterations of astrocytic metabolic phenotype: impact on neuronal viability. J Neurosci. 2010;30:3326–3338. doi: 10.1523/JNEUROSCI.5098-09.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alvarez-Buylla A, Garcia-Verdugo JM, Tramontin AD. A unified hypothesis on the lineage of neural stem cells. Nat Rev Neurosci. 2001;2:287–293. doi: 10.1038/35067582. [DOI] [PubMed] [Google Scholar]
- Alzheimer A, Nissl F, Alzheimer A. Beiträge zur Kenntnis der pathologischen Neuroglia und ihrer Beziehungen zu den Abbauvorgängen im Nervengewebe. Histologische und Histopathologische Arbeiten über die Grosshirnrinde mit besonderer Berücksichtigung der pathologischen Anatomie der Geisteskrankheiten. Verlag von Gustav Fischer Jena. 1910:401–562. [Google Scholar]
- Apelt J, Ach K, Schliebs R. Aging-related down-regulation of neprilysin, a putative β-amyloid-degrading enzyme, in transgenic Tg2576 Alzheimer-like mouse brain is accompanied by an astroglial upregulation in the vicinity of beta-amyloid plaques. Neurosci Lett. 2003;339:183–186. doi: 10.1016/s0304-3940(03)00030-2. [DOI] [PubMed] [Google Scholar]
- Aronica E, Boer K, van Vliet EA, Redeker S, Baayen JC, Spliet WG, van Rijen PC, Troost D, da Silva FH, Wadman WJ, Gorter JA. Complement activation in experimental and human temporal lobe epilepsy. Neurobiol Dis. 2007;26:497–511. doi: 10.1016/j.nbd.2007.01.015. [DOI] [PubMed] [Google Scholar]
- Barres BA. The mystery and magic of glia: a perspective on their roles in health and disease. Neuron. 2008;60:430–440. doi: 10.1016/j.neuron.2008.10.013. [DOI] [PubMed] [Google Scholar]
- Barrett KM, Ding YH, Wagner DP, Kallmes DF, Johnston KC. Change in diffusion-weighted imaging infarct volume predicts neurologic outcome at 90 days: results of the acute stroke accurate prediction (ASAP) trial serial imaging substudy. Stroke. 2009;40:2422–2427. doi: 10.1161/STROKEAHA.109.548933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beach TG, McGeer EG. Lamina-specific arrangement of astrocytic gliosis and senile plaques in Alzheimer's disease visual cortex. Brain Res. 1988;463:357–361. doi: 10.1016/0006-8993(88)90410-6. [DOI] [PubMed] [Google Scholar]
- Beaulieu C, de Crespigny A, Tong DC, Moseley ME, Albers GW, Marks MP. Longitudinal magnetic resonance imaging study of perfusion and diffusion in stroke: evolution of lesion volume and correlation with clinical outcome. Ann Neurol. 1999;46:568–578. doi: 10.1002/1531-8249(199910)46:4<568::aid-ana4>3.0.co;2-r. [DOI] [PubMed] [Google Scholar]
- Bernaudin M, Marti HH, Roussel S, Divoux D, Nouvelot A, MacKenzie ET, Petit E. A potential role for erythropoietin in focal permanent cerebral ischemia in mice. J Cereb Blood Flow Metab. 1999;19:643–651. doi: 10.1097/00004647-199906000-00007. [DOI] [PubMed] [Google Scholar]
- Bordey A, Sontheimer H. Properties of human glial cells associated with epileptic seizure foci. Epilepsy Res. 1998;32:286–303. doi: 10.1016/s0920-1211(98)00059-x. [DOI] [PubMed] [Google Scholar]
- Bourne JN, Harris KM. Balancing structure and function at hippocampal dendritic spines. Annu Rev Neurosci. 2008;31:47–67. doi: 10.1146/annurev.neuro.31.060407.125646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brady JP, Garland DL, Green DE, Tamm ER, Giblin FJ, Wawrousek EF. αB-crystallin in lens development and muscle integrity: a gene knockout approach. Invest Ophthalmol Vis Sci. 2001;42:2924–2934. [PubMed] [Google Scholar]
- Brambilla R, Bracchi-Ricard V, Hu WH, Frydel B, Bramwell A, Karmally S, Green EJ, Bethea JR. Inhibition of astroglial nuclear factor κB reduces inflammation and improves functional recovery after spinal cord injury. J Exp Med. 2005;202:145–156. doi: 10.1084/jem.20041918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brambilla R, Persaud T, Hu X, Karmally S, Shestopalov VI, Dvoriantchikova G, Ivanov D, Nathanson L, Barnum SR, Bethea JR. Transgenic inhibition of astroglial NF-κB improves functional outcome in experimental autoimmune encephalomyelitis by suppressing chronic central nervous system inflammation. J Immunol. 2009;182:2628–2640. doi: 10.4049/jimmunol.0802954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brenner M, Johnson AB, Boespflug-Tanguy O, Rodriguez D, Goldman JE, Messing A. Mutations in GFAP, encoding glial fibrillary acidic protein, are associated with Alexander disease. Nat Genet. 2001;27:117–120. doi: 10.1038/83679. [DOI] [PubMed] [Google Scholar]
- Brenner M, Goldman JE, Quinlan RA, Messing A. Alexander disease: a genetic disorder of astrocytes. In Astrocytes in (Patho)Physiology of the Nervous System (Parpura V, Haydon PG eds), pp 591–648, Springer, New York. 2009 [Google Scholar]
- Broe M, Kril J, Halliday GM. Astrocytic degeneration relates to the severity of disease in frontotemporal dementia. Brain. 2004;127:2214–2220. doi: 10.1093/brain/awh250. [DOI] [PubMed] [Google Scholar]
- Brown AM, Ransom BR. Astrocyte glycogen and brain energy metabolism. Glia. 2007;55:1263–1271. doi: 10.1002/glia.20557. [DOI] [PubMed] [Google Scholar]
- Brown CE, Li P, Boyd JD, Delaney KR, Murphy TH. Extensive turnover of dendritic spines and vascular remodeling in cortical tissues recovering from stroke. J Neurosci. 2007;27:4101–4109. doi: 10.1523/JNEUROSCI.4295-06.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bundesen LQ, Scheel TA, Bregman BS, Kromer LF. Ephrin-B2 and EphB2 regulation of astrocyte-meningeal fibroblast interactions in response to spinal cord lesions in adult rats. J Neurosci. 2003;23:7789–7800. doi: 10.1523/JNEUROSCI.23-21-07789.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bush TG, Puvanachandra N, Horner CH, Polito A, Ostenfeld T, Svendsen CN, Mucke L, Johnson MH, Sofroniew MV. Leukocyte infiltration, neuronal degeneration, and neurite outgrowth after ablation of scar-forming, reactive astrocytes in adult transgenic mice. Neuron. 1999;23:297–308. doi: 10.1016/s0896-6273(00)80781-3. [DOI] [PubMed] [Google Scholar]
- Bushong EA, Martone ME, Jones YZ, Ellisman MH. Protoplasmic astrocytes in CA1 stratum radiatum occupy separate anatomical domains. J Neurosci. 2002;22:183–192. doi: 10.1523/JNEUROSCI.22-01-00183.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Byts N, Siren AL. Erythropoietin: a multimodal neuroprotective agent. Exp Transl Stroke Med. 2009;1:4. doi: 10.1186/2040-7378-1-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carmichael ST. Plasticity of cortical projections after stroke. Neuroscientist. 2003;9:64–75. doi: 10.1177/1073858402239592. [DOI] [PubMed] [Google Scholar]
- Chavez JC, Baranova O, Lin J, Pichiule P. The transcriptional activator hypoxia inducible factor 2 (HIF-2/EPAS-1) regulates the oxygen-dependent expression of erythropoietin in cortical astrocytes. J Neurosci. 2006;26:9471–9481. doi: 10.1523/JNEUROSCI.2838-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Y, Swanson RA. Astrocytes and brain injury. J Cereb Blood Flow Metab. 2003;23:137–149. doi: 10.1097/01.WCB.0000044631.80210.3C. [DOI] [PubMed] [Google Scholar]
- Chen Y, Vartiainen NE, Ying W, Chan PH, Koistinaho J, Swanson RA. Astrocytes protect neurons from nitric oxide toxicity by a glutathione-dependent mechanism. J Neurochem. 2001;77:1601–1610. doi: 10.1046/j.1471-4159.2001.00374.x. [DOI] [PubMed] [Google Scholar]
- Chesler M. Failure and function of intracellular pH regulation in acute hypoxic-ischemic injury of astrocytes. Glia. 2005;50:398–406. doi: 10.1002/glia.20141. [DOI] [PubMed] [Google Scholar]
- Cho W, Messing A. Properties of astrocytes cultured from GFAP over-expressing and GFAP mutant mice. Exp Cell Res. 2009;315:1260–1272. doi: 10.1016/j.yexcr.2008.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cho W, Brenner M, Peters N, Messing A. Drug screening to identify suppressors of GFAP expression. Hum Mol Genet. 2010;19:3169–3178. doi: 10.1093/hmg/ddq227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christopherson KS, Ullian EM, Stokes CC, Mullowney CE, Hell JW, Agah A, Lawler J, Mosher DF, Bornstein P, Barres BA. Thrombospondins are astrocyte-secreted proteins that promote CNS synaptogenesis. Cell. 2005;120:421–433. doi: 10.1016/j.cell.2004.12.020. [DOI] [PubMed] [Google Scholar]
- Coleman P, Federoff H, Kurlan R. A focus on the synapse for neuroprotection in Alzheimer disease and other dementias. Neurology. 2004;63:1155–1162. doi: 10.1212/01.wnl.0000140626.48118.0a. [DOI] [PubMed] [Google Scholar]
- Cunningham LA, Wetzel M, Rosenberg GA. Multiple roles for MMPs and TIMPs in cerebral ischemia. Glia. 2005;50:329–339. doi: 10.1002/glia.20169. [DOI] [PubMed] [Google Scholar]
- Danbolt NC. Glutamate uptake. Progr Neurobiol. 2001;65:1–105. doi: 10.1016/s0301-0082(00)00067-8. [DOI] [PubMed] [Google Scholar]
- de Lanerolle NC, Lee TS, Spencer DD. Astrocytes and epilepsy. Neurotherapeutics. 2010;7:424–438. doi: 10.1016/j.nurt.2010.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeKosky ST, Scheff SW. Synapse loss in frontal cortex biopsies in Alzheimer's disease: correlation with cognitive severity. Ann Neurol. 1990;27:457–464. doi: 10.1002/ana.410270502. [DOI] [PubMed] [Google Scholar]
- Del Bigio MR, Chudley AE, Sarnat HB, Campbell C, Goobie S, Chodirker BN, Selcen D. Infantile muscular dystrophy in Canadian aboriginals is an αB-crystallinopathy. Ann Neurol. 2011;69:866–871. doi: 10.1002/ana.22331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Der Perng M, Su M, Wen SF, Li R, Gibbon T, Prescott AR, Brenner M, Quinlan RA. The Alexander disease-causing glial fibrillary acidic protein mutant, R416W, accumulates into Rosenthal fibers by a pathway that involves filament aggregation and the association of αB-crystallin and HSP27. Am J Hum Genet. 2006;79:197–213. doi: 10.1086/504411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drage MG, Holmes GL, Seyfried TN. Hippocampal neurons and glia in epileptic EL mice. J Neurocytol. 2002;31:681–692. doi: 10.1023/a:1025747813463. [DOI] [PubMed] [Google Scholar]
- Drogemuller K, Helmuth U, Brunn A, Sakowicz-Burkiewicz M, Gutmann DH, Mueller W, Deckert M, Schluter D. Astrocyte gp130 expression is critical for the control of Toxoplasma encephalitis. J Immunol. 2008;181:2683–2693. doi: 10.4049/jimmunol.181.4.2683. [DOI] [PubMed] [Google Scholar]
- During MJ, Spencer DD. Extracellular hippocampal glutamate and spontaneous seizure in the conscious human brain. Lancet. 1993;341:1607–1610. doi: 10.1016/0140-6736(93)90754-5. [DOI] [PubMed] [Google Scholar]
- Ehrenreich H, Hasselblatt M, Dembowski C, Cepek L, Lewczuk P, Stiefel M, Rustenbeck HH, Breiter N, Jacob S, Knerlich F, Bohn M, Poser W, Ruther E, Kochen M, Gefeller O, Gleiter C, Wessel TC, De Ryck M, Itri L, Prange H, Cerami A, Brines M, Siren AL. Erythropoietin therapy for acute stroke is both safe and beneficial. Mol Med. 2002;8:495–505. [PMC free article] [PubMed] [Google Scholar]
- Ehrenreich H, Weissenborn K, Prange H, Schneider D, Weimar C, Wartenberg K, Schellinger PD, Bohn M, Becker H, Wegrzyn M, Jahnig P, Herrmann M, Knauth M, Bahr M, Heide W, Wagner A, Schwab S, Reichmann H, Schwendemann G, Dengler R, Kastrup A, Bartels C. Recombinant human erythropoietin in the treatment of acute ischemic stroke. Stroke. 2009;40:e647–e656. doi: 10.1161/STROKEAHA.109.564872. [DOI] [PubMed] [Google Scholar]
- Eid T, Thomas MJ, Spencer DD, Runden-Pran E, Lai JC, Malthankar GV, Kim JH, Danbolt NC, Ottersen OP, de Lanerolle NC. Loss of glutamine synthetase in the human epileptogenic hippocampus: possible mechanism for raised extracellular glutamate in mesial temporal lobe epilepsy. Lancet. 2004;363:28–37. doi: 10.1016/s0140-6736(03)15166-5. [DOI] [PubMed] [Google Scholar]
- Faulkner JR, Herrmann JE, Woo MJ, Tansey KE, Doan NB, Sofroniew MV. Reactive astrocytes protect tissue and preserve function after spinal cord injury. J Neurosci. 2004;24:2143–2155. doi: 10.1523/JNEUROSCI.3547-03.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foerster O, Penfield W. The structural basis of traumatic epilepsy and results of radical operations. Brain. 1930;53:99–119. [Google Scholar]
- Garcia JH, Yoshida Y, Chen H, Li Y, Zhang ZG, Lian J, Chen S, Chopp M. Progression from ischemic injury to infarct following middle cerebral artery occlusion in the rat. Am J Pathol. 1993;142:623–635. [PMC free article] [PubMed] [Google Scholar]
- Giaume C, Kirchhoff F, Matute C, Reichenbach A, Verkhratsky A. Glia: the fulcrum of brain diseases. Cell Death Differ. 2007;14:1324–1335. doi: 10.1038/sj.cdd.4402144. [DOI] [PubMed] [Google Scholar]
- Giffard RG, Monyer H, Choi DW. Selective vulnerability of cultured cortical glia to injury by extracellular acidosis. Brain Res. 1990;530:138–141. doi: 10.1016/0006-8993(90)90670-7. [DOI] [PubMed] [Google Scholar]
- Giffard RG, Papadopoulos MC, van Hooft JA, Xu L, Giuffrida R, Monyer H. The electrogenic sodium bicarbonate cotransporter: developmental expression in rat brain and possible role in acid vulnerability. J Neurosci. 2000;20:1001–1008. doi: 10.1523/JNEUROSCI.20-03-01001.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gomi H, Yokoyama T, Fujimoto K, Ikeda T, Katoh A, Itoh T, Itohara S. Mice devoid of the glial fibrillary acidic protein develop normally and are susceptible to scrapie prions. Neuron. 1995;14:29–41. doi: 10.1016/0896-6273(95)90238-4. [DOI] [PubMed] [Google Scholar]
- Gordon GR, Mulligan SJ, MacVicar BA. Astrocyte control of the cerebrovasculature. Glia. 2007;55:1214–1221. doi: 10.1002/glia.20543. [DOI] [PubMed] [Google Scholar]
- Gourine AV, Kasparov S. Astrocytes as brain interoceptors. Exp Physiol. 2011;96:411–416. doi: 10.1113/expphysiol.2010.053165. [DOI] [PubMed] [Google Scholar]
- Gourine AV, Kasymov V, Marina N, Tang F, Figueiredo MF, Lane S, Teschemacher AG, Spyer KM, Deisseroth K, Kasparov S. Astrocytes control breathing through pH-dependent release of ATP. Science. 2010;329:571–575. doi: 10.1126/science.1190721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffin WS, Stanley LC, Ling C, White L, MacLeod V, Perrot LJ, White CL, 3rd, Araoz C. Brain interleukin 1 and S-100 immunoreactivity are elevated in Down syndrome and Alzheimer disease. Proc Natl Acad Sci USA. 1989;86:7611–7615. doi: 10.1073/pnas.86.19.7611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guenette SY. Astrocytes: a cellular player in Aβ clearance and degradation. Trends Mol Med. 2003;9:279–280. doi: 10.1016/s1471-4914(03)00112-6. [DOI] [PubMed] [Google Scholar]
- Gurer G, Gursoy-Ozdemir Y, Erdemli E, Can A, Dalkara T. Astrocytes are more resistant to focal cerebral ischemia than neurons and die by a delayed necrosis. Brain Pathol. 2009;19:630–641. doi: 10.1111/j.1750-3639.2008.00226.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hagemann TL, Connor JX, Messing A. Alexander disease-associated glial fibrillary acidic protein mutations in mice induce Rosenthal fiber formation and a white matter stress response. J Neurosci. 2006;26:11162–11173. doi: 10.1523/JNEUROSCI.3260-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hagemann TL, Boelens WC, Wawrousek EF, Messing A. Suppression of GFAP toxicity by αB-crystallin in mouse models of Alexander disease. Hum Mol Genet. 2009;18:1190–1199. doi: 10.1093/hmg/ddp013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halassa MM, Fellin T, Haydon PG. The tripartite synapse: roles for gliotransmission in health and disease. Trends Mol Med. 2007a;13:54–63. doi: 10.1016/j.molmed.2006.12.005. [DOI] [PubMed] [Google Scholar]
- Halassa MM, Fellin T, Takano H, Dong JH, Haydon PG. Synaptic islands defined by the territory of a single astrocyte. J Neurosci. 2007b;27:6473–6477. doi: 10.1523/JNEUROSCI.1419-07.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamby ME, Sofroniew MV. Reactive astrocytes as therapeutic targets for CNS disorders. Neurotherapeutics. 2010;7:494–506. doi: 10.1016/j.nurt.2010.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartlage-Rubsamen M, Zeitschel U, Apelt J, Gartner U, Franke H, Stahl T, Gunther A, Schliebs R, Penkowa M, Bigl V, Rossner S. Astrocytic expression of the Alzheimer's disease β-secretase (BACE1) is stimulus-dependent. Glia. 2003;41:169–179. doi: 10.1002/glia.10178. [DOI] [PubMed] [Google Scholar]
- Harvey BK, Chang CF, Chiang YH, Bowers WJ, Morales M, Hoffer BJ, Wang Y, Federoff HJ. HSV amplicon delivery of glial cell line-derived neurotrophic factor is neuroprotective against ischemic injury. Exp Neurol. 2003;183:47–55. doi: 10.1016/s0014-4886(03)00080-3. [DOI] [PubMed] [Google Scholar]
- Hazell AS. Astrocytes are a major target in thiamine deficiency and Wernicke's encephalopathy. Neurochem Int. 2009;55:129–135. doi: 10.1016/j.neuint.2009.02.020. [DOI] [PubMed] [Google Scholar]
- Hazell AS, Sheedy D, Oanea R, Aghourian M, Sun S, Jung JY, Wang D, Wang C. Loss of astrocytic glutamate transporters in Wernicke encephalopathy. Glia. 2009;58:148–156. doi: 10.1002/glia.20908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heneka MT, Sastre M, Dumitrescu-Ozimek L, Dewachter I, Walter J, Klockgether T, Van Leuven F. Focal glial activation coincides with increased BACE1 activation and precedes amyloid plaque deposition in APP[V717I] transgenic mice. J Neuroinflam. 2005;2:22. doi: 10.1186/1742-2094-2-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heneka MT, Rodriguez JJ, Verkhratsky A. Neuroglia in neurodegeneration. Brain Res Rev. 2010;63:189–211. doi: 10.1016/j.brainresrev.2009.11.004. [DOI] [PubMed] [Google Scholar]
- Hermann DM, Kilic E, Kugler S, Isenmann S, Bahr M. Adenovirus-mediated GDNF and CNTF pretreatment protects against striatal injury following transient middle cerebral artery occlusion in mice. Neurobiol Dis. 2001;8:655–666. doi: 10.1006/nbdi.2001.0399. [DOI] [PubMed] [Google Scholar]
- Herrmann JE, Imura T, Song B, Qi J, Ao Y, Nguyen TK, Korsak RA, Takeda K, Akira S, Sofroniew MV. STAT3 is a critical regulator of astrogliosis and scar formation after spinal cord injury. J Neurosci. 2008;28:7231–7243. doi: 10.1523/JNEUROSCI.1709-08.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hinterkeuser S, Schroder W, Hager G, Seifert G, Blumcke I, Elger CE, Schramm J, Steinhauser C. Astrocytes in the hippocampus of patients with temporal lobe epilepsy display changes in potassium conductances. Eur J Neurosci. 2000;12:2087–2096. doi: 10.1046/j.1460-9568.2000.00104.x. [DOI] [PubMed] [Google Scholar]
- Hsiao VC, Tian R, Long H, Der Perng M, Brenner M, Quinlan RA, Goldman JE. Alexander-disease mutation of GFAP causes filament disorganization and decreased solubility of GFAP. J Cell Sci. 2005;118:2057–2065. doi: 10.1242/jcs.02339. [DOI] [PubMed] [Google Scholar]
- Hu J, Ferreira A, Van Eldik LJ. S100β induces neuronal cell death through nitric oxide release from astrocytes. J Neurochem. 1997;69:2294–2301. doi: 10.1046/j.1471-4159.1997.69062294.x. [DOI] [PubMed] [Google Scholar]
- Huckstepp RT, id Bihi R, Eason R, Spyer KM, Dicke N, Willecke K, Marina N, Gourine AV, Dale N. Connexin hemichannel-mediated CO2-dependent release of ATP in the medulla oblongata contributes to central respiratory chemosensitivity. J Physiol. 2010;588:3901–3920. doi: 10.1113/jphysiol.2010.192088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iadecola C, Nedergaard M. Glial regulation of the cerebral microvasculature. Nat Neurosci. 2007;10:1369–1376. doi: 10.1038/nn2003. [DOI] [PubMed] [Google Scholar]
- Ingram EM, Wiseman JW, Tessler S, Emson PC. Reduction of glial glutamate transporters in the parietal cortex and hippocampus of the EL mouse. J Neurochem. 2001;79:564–575. doi: 10.1046/j.1471-4159.2001.00612.x. [DOI] [PubMed] [Google Scholar]
- Jansen LA, Uhlmann EJ, Crino PB, Gutmann DH, Wong M. Epileptogenesis and reduced inward rectifier potassium current in tuberous sclerosis complex-1-deficient astrocytes. Epilepsia. 2005;46:1871–1880. doi: 10.1111/j.1528-1167.2005.00289.x. [DOI] [PubMed] [Google Scholar]
- Jelkmann W, Wagner K. Beneficial and ominous aspects of the pleiotropic action of erythropoietin. Ann Hematol. 2004;83:673–686. doi: 10.1007/s00277-004-0911-6. [DOI] [PubMed] [Google Scholar]
- Jian Liu K, Rosenberg GA. Matrix metalloproteinases and free radicals in cerebral ischemia. Free Radic Biol Med. 2005;39:71–80. doi: 10.1016/j.freeradbiomed.2005.03.033. [DOI] [PubMed] [Google Scholar]
- Jin KL, Mao XO, Greenberg DA. Vascular endothelial growth factor: direct neuroprotective effect in in vitro ischemia. Proc Natl Acad Sci USA. 2000;97:10242–10247. doi: 10.1073/pnas.97.18.10242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kano M, Hashimoto K. Synapse elimination in the central nervous system. Curr Opin Neurobiol. 2009;19:154–161. doi: 10.1016/j.conb.2009.05.002. [DOI] [PubMed] [Google Scholar]
- Kersaitis C, Halliday GM, Kril JJ. Regional and cellular pathology in frontotemporal dementia: relationship to stage of disease in cases with and without Pick bodies. Acta Neuropathol. 2004;108:515–523. doi: 10.1007/s00401-004-0917-0. [DOI] [PubMed] [Google Scholar]
- Kettenmann H, Verkhratsky A. Neuroglia: the 150 years after. Trends Neurosci. 2008;31:653–659. doi: 10.1016/j.tins.2008.09.003. [DOI] [PubMed] [Google Scholar]
- Kitagawa H, Sasaki C, Sakai K, Mori A, Mitsumoto Y, Mori T, Fukuchi Y, Setoguchi Y, Abe K. Adenovirus-mediated gene transfer of glial cell line-derived neurotrophic factor prevents ischemic brain injury after transient middle cerebral artery occlusion in rats. J Cereb Blood Flow Metab. 1999;19:1336–1344. doi: 10.1097/00004647-199912000-00007. [DOI] [PubMed] [Google Scholar]
- Koehler RC, Roman RJ, Harder DR. Astrocytes and the regulation of cerebral blood flow. Trends Neurosci. 2009;32:160–169. doi: 10.1016/j.tins.2008.11.005. [DOI] [PubMed] [Google Scholar]
- Koistinaho M, Lin S, Wu X, Esterman M, Koger D, Hanson J, Higgs R, Liu F, Malkani S, Bales KR, Paul SM. Apolipoprotein E promotes astrocyte colocalization and degradation of deposited amyloid-beta peptides. Nat Med. 2004;10:719–726. doi: 10.1038/nm1058. [DOI] [PubMed] [Google Scholar]
- Kulijewicz-Nawrot M, Verkhratsky A, Chvatal A, Syková E, Rodríguez JJ. Astrocytic morphological and functional alterations during the progression of Alzheimer's disease in the prefrontal cortex. Glia. 2011;59:S109. [Google Scholar]
- Lalo U, Pankratov Y, Parpura V, Verkhratsky A. Ionotropic receptors in neuronal-astroglial signalling: what is the role of ‘excitable’ molecules in non-excitable cells. Biochim Biophys Acta. 2011a;1813:992–1002. doi: 10.1016/j.bbamcr.2010.09.007. [DOI] [PubMed] [Google Scholar]
- Lalo U, Verkhratsky A, Pankratov Y. Ionotropic ATP receptors in neuronal-glial communication. Semin Cell Dev Biol. 2011b;22:220–228. doi: 10.1016/j.semcdb.2011.02.012. [DOI] [PubMed] [Google Scholar]
- Lee MY, Ju WK, Cha JH, Son BC, Chun MH, Kang JK, Park CK. Expression of vascular endothelial growth factor mRNA following transient forebrain ischemia in rats. Neurosci Lett. 1999;265:107–110. doi: 10.1016/s0304-3940(99)00219-0. [DOI] [PubMed] [Google Scholar]
- Lee SH, Magge S, Spencer DD, Sontheimer H, Cornell-Bell AH. Human epileptic astrocytes exhibit increased gap junction coupling. Glia. 1995;15:195–202. doi: 10.1002/glia.440150212. [DOI] [PubMed] [Google Scholar]
- Lee TS, Mane S, Eid T, Zhao H, Lin A, Guan Z, Kim JH, Schweitzer J, King-Stevens D, Weber P, Spencer SS, Spencer DD, de Lanerolle NC. Gene expression in temporal lobe epilepsy is consistent with increased release of glutamate by astrocytes. Mol Med. 2007;13:1–13. doi: 10.2119/2006-00079.Lee. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li L, Lundkvist A, Andersson D, Wilhelmsson U, Nagai N, Pardo AC, Nodin C, Stahlberg A, Aprico K, Larsson K, Yabe T, Moons L, Fotheringham A, Davies I, Carmeliet P, Schwartz JP, Pekna M, Kubista M, Blomstrand F, Maragakis N, Nilsson M, Pekny M. Protective role of reactive astrocytes in brain ischemia. J Cereb Blood Flow Metab. 2008;28:468–481. doi: 10.1038/sj.jcbfm.9600546. [DOI] [PubMed] [Google Scholar]
- Li R, Johnson AB, Salomons G, Goldman JE, Naidu S, Quinlan R, Cree B, Ruyle SZ, Banwell B, D'Hooghe M, Siebert JR, Rolf CM, Cox H, Reddy A, Gutierrez-Solana LG, Collins A, Weller RO, Messing A, van der Knaap MS, Brenner M. Glial fibrillary acidic protein mutations in infantile, juvenile, and adult forms of Alexander disease. Ann Neurol. 2005;57:310–326. doi: 10.1002/ana.20406. [DOI] [PubMed] [Google Scholar]
- Liauw J, Hoang S, Choi M, Eroglu C, Sun GH, Percy M, Wildman-Tobriner B, Bliss T, Guzman RG, Barres BA, Steinberg GK. Thrombospondins 1 and 2 are necessary for synaptic plasticity and functional recovery after stroke. J Cereb Blood Flow Metab. 2008;28:1722–1732. doi: 10.1038/jcbfm.2008.65. [DOI] [PubMed] [Google Scholar]
- Lin JH, Lou N, Kang N, Takano T, Hu F, Han X, Xu Q, Lovatt D, Torres A, Willecke K, Yang J, Kang J, Nedergaard M. A central role of connexin 43 in hypoxic preconditioning. J Neurosci. 2008;28:681–695. doi: 10.1523/JNEUROSCI.3827-07.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin JH, Weigel H, Cotrina ML, Liu S, Bueno E, Hansen AJ, Hansen TW, Goldman S, Nedergaard M. Gap-junction-mediated propagation and amplification of cell injury. Nat Neurosci. 1998;1:494–500. doi: 10.1038/2210. [DOI] [PubMed] [Google Scholar]
- Liu D, Smith CL, Barone FC, Ellison JA, Lysko PG, Li K, Simpson IA. Astrocytic demise precedes delayed neuronal death in focal ischemic rat brain. Brain Res Mol Brain Res. 1999;68:29–41. doi: 10.1016/s0169-328x(99)00063-7. [DOI] [PubMed] [Google Scholar]
- Lobsiger CS, Cleveland DW. Glial cells as intrinsic components of non-cell-autonomous neurodegenerative disease. Nat Neurosci. 2007;10:1355–1360. doi: 10.1038/nn1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magistretti PJ. Neuron-glia metabolic coupling and plasticity. J Exp Biol. 2006;209:2304–2311. doi: 10.1242/jeb.02208. [DOI] [PubMed] [Google Scholar]
- Malthankar-Phatak GH, de Lanerolle N, Eid T, Spencer DD, Behar KL, Spencer SS, Kim JH, Lai JC. Differential glutamate dehydrogenase (GDH) activity profile in patients with temporal lobe epilepsy. Epilepsia. 2006;47:1292–1299. doi: 10.1111/j.1528-1167.2006.00543.x. [DOI] [PubMed] [Google Scholar]
- Marti HH, Gassmann M, Wenger RH, Kvietikova I, Morganti-Kossmann MC, Kossmann T, Trentz O, Bauer C. Detection of erythropoietin in human liquor: intrinsic erythropoietin production in the brain. Kidney Int. 1997;51:416–418. doi: 10.1038/ki.1997.55. [DOI] [PubMed] [Google Scholar]
- Masuda S, Okano M, Yamagishi K, Nagao M, Ueda M, Sasaki R. A novel site of erythropoietin production. Oxygen-dependent production in cultured rat astrocytes. J Biol Chem. 1994;269:19488–19493. [PubMed] [Google Scholar]
- Matsui T, Mori T, Tateishi N, Kagamiishi Y, Satoh S, Katsube N, Morikawa E, Morimoto T, Ikuta F, Asano T. Astrocytic activation and delayed infarct expansion after permanent focal ischemia in rats. Part I: enhanced astrocytic synthesis of s-100β in the periinfarct area precedes delayed infarct expansion. J Cereb Blood Flow Metab. 2002;22:711–722. doi: 10.1097/00004647-200206000-00010. [DOI] [PubMed] [Google Scholar]
- Matthias K, Kirchhoff F, Seifert G, Huttmann K, Matyash M, Kettenmann H, Steinhauser C. Segregated expression of AMPA-type glutamate receptors and glutamate transporters defines distinct astrocyte populations in the mouse hippocampus. J Neurosci. 2003;23:1750–1758. doi: 10.1523/JNEUROSCI.23-05-01750.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCall MA, Gregg RG, Behringer RR, Brenner M, Delaney CL, Galbreath EJ, Zhang CL, Pearce RA, Chiu SY, Messing A. Targeted deletion in astrocyte intermediate filament (Gfap) alters neuronal physiology. Proc Natl Acad Sci USA. 1996;93:6361–6366. doi: 10.1073/pnas.93.13.6361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGeer PL, McGeer EG. Inflammatory processes in amyotrophic lateral sclerosis. Muscle Nerve. 2002;26:459–470. doi: 10.1002/mus.10191. [DOI] [PubMed] [Google Scholar]
- McGeer PL, McGeer EG. Glial reactions in Parkinson's disease. Mov Disord. 2008;23:474–483. doi: 10.1002/mds.21751. [DOI] [PubMed] [Google Scholar]
- Mena MA, Casarejos MJ, Carazo A, Paino CL, Garcia de Yebenes J. Glia conditioned medium protects fetal rat midbrain neurones in culture from L-DOPA toxicity. Neuroreport. 1996;7:441–445. doi: 10.1097/00001756-199601310-00016. [DOI] [PubMed] [Google Scholar]
- Mena MA, Casarejos MJ, Garcia de Yebenes J. The effect of glia-conditioned medium on dopamine neurons in culture. Modulation of apoptosis, tyrosine hydroxylase expression and 1-methyl-4-phenylpyridinium toxicity. J Neural Transm. 1999;106:1105–1123. doi: 10.1007/s007020050227. [DOI] [PubMed] [Google Scholar]
- Mena MA, Garcia de Yebenes J. Glial cells as players in Parkinsonism: the ‘good,’ the ‘bad,’ and the ‘mysterious’ glia. Neuroscientist. 2008;14:544–560. doi: 10.1177/1073858408322839. [DOI] [PubMed] [Google Scholar]
- Messing A, Daniels CM, Hagemann TL. Strategies for treatment in Alexander disease. Neurotherapeutics. 2010;7:507–515. doi: 10.1016/j.nurt.2010.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Messing A, Head MW, Galles K, Galbreath EJ, Goldman JE, Brenner M. Fatal encephalopathy with astrocyte inclusions in GFAP transgenic mice. Am J Pathol. 1998;152:391–398. [PMC free article] [PubMed] [Google Scholar]
- Messing A, Li R, Naidu S, Taylor JP, Silverman L, Flint D, van der Knaap MS, Brenner M. Archetypal and new families with Alexander disease and novel mutations in GFAP. Arch Neurol. 2011 doi: 10.1001/archneurol.2011.1181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morishita E, Masuda S, Nagao M, Yasuda Y, Sasaki R. Erythropoietin receptor is expressed in rat hippocampal and cerebral cortical neurons, and erythropoietin prevents in vitro glutamate-induced neuronal death. Neuroscience. 1997;76:105–116. doi: 10.1016/s0306-4522(96)00306-5. [DOI] [PubMed] [Google Scholar]
- Mrak RE, Griffin WS. Glia and their cytokines in progression of neurodegeneration. Neurobiol Aging. 2005;26:349–354. doi: 10.1016/j.neurobiolaging.2004.05.010. [DOI] [PubMed] [Google Scholar]
- Myer DJ, Gurkoff GG, Lee SM, Hovda DA, Sofroniew MV. Essential protective roles of reactive astrocytes in traumatic brain injury. Brain. 2006;129:2761–2772. doi: 10.1093/brain/awl165. [DOI] [PubMed] [Google Scholar]
- Nagai M, Re DB, Nagata T, Chalazonitis A, Jessell TM, Wichterle H, Przedborski S. Astrocytes expressing ALS-linked mutated SOD1 release factors selectively toxic to motor neurons. Nat Neurosci. 2007;10:615–622. doi: 10.1038/nn1876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagele RG, D'Andrea MR, Lee H, Venkataraman V, Wang HY. Astrocytes accumulate Aβ 42 and give rise to astrocytic amyloid plaques in Alzheimer disease brains. Brain Res. 2003;971:197–209. doi: 10.1016/s0006-8993(03)02361-8. [DOI] [PubMed] [Google Scholar]
- Nagele RG, Wegiel J, Venkataraman V, Imaki H, Wang KC. Contribution of glial cells to the development of amyloid plaques in Alzheimer's disease. Neurobiol Aging. 2004;25:663–674. doi: 10.1016/j.neurobiolaging.2004.01.007. [DOI] [PubMed] [Google Scholar]
- Nedergaard M, Dirnagl U. Role of glial cells in cerebral ischemia. Glia. 2005;50:281–286. doi: 10.1002/glia.20205. [DOI] [PubMed] [Google Scholar]
- Nedergaard M, Ransom B, Goldman SA. New roles for astrocytes: redefining the functional architecture of the brain. Trends Neurosci. 2003;26:523–530. doi: 10.1016/j.tins.2003.08.008. [DOI] [PubMed] [Google Scholar]
- Nedergaard M, Rodriguez JJ, Verkhratsky A. Glial calcium and diseases of the nervous system. Cell Calcium. 2010;47:140–149. doi: 10.1016/j.ceca.2009.11.010. [DOI] [PubMed] [Google Scholar]
- Nedergaard M, Verkhratsky A. Artifact versus reality–How astrocytes contribute to synaptic events? Glia. 2012 doi: 10.1002/glia.22288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newman EA. Glial cell regulation of extracellular potassium. In: Kettenmann H, Ransom B, editors. New York: Oxford University Press; 1995. pp. 717–731. [Google Scholar]
- Nicoll JA, Weller RO. A new role for astrocytes: β-amyloid homeostasis and degradation. Trends Mol Med. 2003;9:281–282. doi: 10.1016/s1471-4914(03)00109-6. [DOI] [PubMed] [Google Scholar]
- Nudo RJ. Postinfarct cortical plasticity and behavioral recovery. Stroke. 2007;38:840–845. doi: 10.1161/01.STR.0000247943.12887.d2. [DOI] [PubMed] [Google Scholar]
- O'Connor ER, Sontheimer H, Spencer DD, de Lanerolle NC. Astrocytes from human hippocampal epileptogenic foci exhibit action potential-like responses. Epilepsia. 1998;39:347–354. doi: 10.1111/j.1528-1157.1998.tb01386.x. [DOI] [PubMed] [Google Scholar]
- Oberheim NA, Tian GF, Han X, Peng W, Takano T, Ransom B, Nedergaard M. Loss of astrocytic domain organization in the epileptic brain. J Neurosci. 2008;28:3264–3276. doi: 10.1523/JNEUROSCI.4980-07.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oberheim NA, Wang X, Goldman S, Nedergaard M. Astrocytic complexity distinguishes the human brain. Trends Neurosci. 2006;29:547–553. doi: 10.1016/j.tins.2006.08.004. [DOI] [PubMed] [Google Scholar]
- Ogata K, Kosaka T. Structural and quantitative analysis of astrocytes in the mouse hippocampus. Neuroscience. 2002;113:221–233. doi: 10.1016/s0306-4522(02)00041-6. [DOI] [PubMed] [Google Scholar]
- Okada S, Nakamura M, Katoh H, Miyao T, Shimazaki T, Ishii K, Yamane J, Yoshimura A, Iwamoto Y, Toyama Y, Okano H. Conditional ablation of Stat3 or Socs3 discloses a dual role for reactive astrocytes after spinal cord injury. Nat Med. 2006;12:829–834. doi: 10.1038/nm1425. [DOI] [PubMed] [Google Scholar]
- Olabarria M, Noristani HN, Verkhratsky A, Rodriguez JJ. Concomitant astroglial atrophy and astrogliosis in a triple transgenic animal model of Alzheimer's disease. Glia. 2010;58:831–838. doi: 10.1002/glia.20967. [DOI] [PubMed] [Google Scholar]
- Olabarria M, Noristani HN, Verkhratsky A, Rodriguez JJ. Age-dependent decrease in glutamine synthetase expression in the hippocampal astroglia of the triple transgenic Alzheimer's disease mouse model: mechanism for deficient glutamatergic transmission? Mol Neurodegener. 2011;6:55. doi: 10.1186/1750-1326-6-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pekny M, Leveen P, Pekna M, Eliasson C, Berthold CH, Westermark B, Betsholtz C. Mice lacking glial fibrillary acidic protein display astrocytes devoid of intermediate filaments but develop and reproduce normally. EMBO J. 1995;14:1590–1598. doi: 10.1002/j.1460-2075.1995.tb07147.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pekny M, Nilsson M. Astrocyte activation and reactive gliosis. Glia. 2005;50:427–434. doi: 10.1002/glia.20207. [DOI] [PubMed] [Google Scholar]
- Penfield W, Humphreys S. Epileptogenic lesions of the brain. A histologic study. Arch Neurol Psychiatry. 1940;43:240–259. [Google Scholar]
- Perea G, Navarrete M, Araque A. Tripartite synapses: astrocytes process and control synaptic information. Trends Neurosci. 2009;32:421–431. doi: 10.1016/j.tins.2009.05.001. [DOI] [PubMed] [Google Scholar]
- Perng MD, Wen SF, Gibbon T, Middeldorp J, Sluijs J, Hol EM, Quinlan RA. Glial fibrillary acidic protein filaments can tolerate the incorporation of assembly-compromised GFAP-δ, but with consequences for filament organization and αB-crystallin association. Mol Biol Cell. 2008;19:4521–4533. doi: 10.1091/mbc.E08-03-0284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfrieger FW. Roles of glial cells in synapse development. Cell Mol Life Sci. 2009;66:2037–2047. doi: 10.1007/s00018-009-0005-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Potts R, Leech RW. Thalamic dementia: an example of primary astroglial dystrophy of Seitelberger. Clin Neuropathol. 2005;24:271–275. [PubMed] [Google Scholar]
- Prass K, Scharff A, Ruscher K, Lowl D, Muselmann C, Victorov I, Kapinya K, Dirnagl U, Meisel A. Hypoxia-induced stroke tolerance in the mouse is mediated by erythropoietin. Stroke. 2003;34:1981–1986. doi: 10.1161/01.STR.0000080381.76409.B2. [DOI] [PubMed] [Google Scholar]
- Prust M, Wang J, Morizono H, Messing A, Brenner M, Gordon E, Hartka T, Sokohl A, Schiffmann R, Gordish-Dressman H, Albin R, Amartino H, Brockman K, Dinopoulos A, Dotti MT, Fain D, Fernandez R, Ferreira J, Fleming J, Gill D, Griebel M, Heilstedt H, Kaplan P, Lewis D, Nakagawa M, Pedersen R, Reddy A, Sawaishi Y, Schneider M, Sherr E, Takiyama Y, Wakabayashi K, Gorospe JR, Vanderver A. GFAP mutations, age at onset, and clinical subtypes in Alexander disease. Neurology. 2011;77:1287–1294. doi: 10.1212/WNL.0b013e3182309f72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rao KV, Panickar KS, Jayakumar AR, Norenberg MD. Astrocytes protect neurons from ammonia toxicity. Neurochem Res. 2005;30:1311–1318. doi: 10.1007/s11064-005-8803-2. [DOI] [PubMed] [Google Scholar]
- Reichenbach A, Wolburg H. Astrocytes and ependymal glia. In: Kettenmann H, Ransom B R, editors. Oxford: Oxford University Press; 2005. pp. 19–35. [Google Scholar]
- Rodriguez JJ, Olabarria M, Chvatal A, Verkhratsky A. Astroglia in dementia and Alzheimer's disease. Cell Death Differ. 2009;16:378–385. doi: 10.1038/cdd.2008.172. [DOI] [PubMed] [Google Scholar]
- Rodriguez JJ, Verkhratsky A. Neuroglial roots of neurodegenerative diseases? Mol Neurobiol. 2011;43:87–96. doi: 10.1007/s12035-010-8157-x. [DOI] [PubMed] [Google Scholar]
- Rossi D, Brambilla L, Valori CF, Roncoroni C, Crugnola A, Yokota T, Bredesen DE, Volterra A. Focal degeneration of astrocytes in amyotrophic lateral sclerosis. Cell Death Differ. 2008;15:1691–1700. doi: 10.1038/cdd.2008.99. [DOI] [PubMed] [Google Scholar]
- Rossi D, Volterra A. Astrocytic dysfunction: Insights on the role in neurodegeneration. Brain Res Bull. 2009;80:224–232. doi: 10.1016/j.brainresbull.2009.07.012. [DOI] [PubMed] [Google Scholar]
- Rossner S, Lange-Dohna C, Zeitschel U, Perez-Polo JR. Alzheimer's disease beta-secretase BACE1 is not a neuron-specific enzyme. J Neurochem. 2005;92:226–234. doi: 10.1111/j.1471-4159.2004.02857.x. [DOI] [PubMed] [Google Scholar]
- Rothstein JD, Dykes-Hoberg M, Pardo CA, Bristol LA, Jin L, Kuncl RW, Kanai Y, Hediger MA, Wang Y, Schielke JP, Welty DF. Knockout of glutamate transporters reveals a major role for astroglial transport in excitotoxicity and clearance of glutamate. Neuron. 1996;16:675–686. doi: 10.1016/s0896-6273(00)80086-0. [DOI] [PubMed] [Google Scholar]
- Rothstein JD, Patel S, Regan MR, Haenggeli C, Huang YH, Bergles DE, Jin L, Dykes Hoberg M, Vidensky S, Chung DS, Toan SV, Bruijn LI, Su ZZ, Gupta P, Fisher PB. β-lactam antibiotics offer neuroprotection by increasing glutamate transporter expression. Nature. 2005;433:73–77. doi: 10.1038/nature03180. [DOI] [PubMed] [Google Scholar]
- Ruscher K, Freyer D, Karsch M, Isaev N, Megow D, Sawitzki B, Priller J, Dirnagl U, Meisel A. Erythropoietin is a paracrine mediator of ischemic tolerance in the brain: evidence from an in vitro model. J Neurosci. 2002;22:10291–10301. doi: 10.1523/JNEUROSCI.22-23-10291.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sakanaka M, Wen TC, Matsuda S, Masuda S, Morishita E, Nagao M, Sasaki R. In vivo evidence that erythropoietin protects neurons from ischemic damage. Proc Natl Acad Sci USA. 1998;95:4635–4640. doi: 10.1073/pnas.95.8.4635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Samuel W, Masliah E, Hill LR, Butters N, Terry R. Hippocampal connectivity and Alzheimer's dementia: effects of synapse loss and tangle frequency in a two-component model. Neurology. 1994;44:2081–2088. doi: 10.1212/wnl.44.11.2081. [DOI] [PubMed] [Google Scholar]
- Sattler R, Rothstein JD. Regulation and dysregulation of glutamate transporters. Handb Exp Pharmacol. 2006:277–303. doi: 10.1007/3-540-29784-7_14. [DOI] [PubMed] [Google Scholar]
- Schroder W, Hinterkeuser S, Seifert G, Schramm J, Jabs R, Wilkin GP, Steinhauser C. Functional and molecular properties of human astrocytes in acute hippocampal slices obtained from patients with temporal lobe epilepsy. Epilepsia. 2000;41(Suppl 6):S181–184. doi: 10.1111/j.1528-1157.2000.tb01578.x. [DOI] [PubMed] [Google Scholar]
- Schubert D, Soucek T, Blouw B. The induction of HIF-1 reduces astrocyte activation by amyloid β peptide. Eur J Neurosci. 2009;29:1323–1334. doi: 10.1111/j.1460-9568.2009.06712.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schummers J, Yu H, Sur M. Tuned responses of astrocytes and their influence on hemodynamic signals in the visual cortex. Science. 2008;320:1638–1643. doi: 10.1126/science.1156120. [DOI] [PubMed] [Google Scholar]
- Seifert G, Huttmann K, Schramm J, Steinhauser C. Enhanced relative expression of glutamate receptor 1 flip AMPA receptor subunits in hippocampal astrocytes of epilepsy patients with Ammon's horn sclerosis. J Neurosci. 2004;24:1996–2003. doi: 10.1523/JNEUROSCI.3904-03.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seifert G, Schroder W, Hinterkeuser S, Schumacher T, Schramm J, Steinhauser C. Changes in flip/flop splicing of astroglial AMPA receptors in human temporal lobe epilepsy. Epilepsia. 2002;43((Suppl. 5)):162–167. doi: 10.1046/j.1528-1157.43.s.5.10.x. [DOI] [PubMed] [Google Scholar]
- Senitz D, Reichenbach A, Smith TG Jr. Surface complexity of human neocortical astrocytic cells: changes with development, aging, and dementia. J Hirnforsch. 1995;36:531–537. [PubMed] [Google Scholar]
- Shigetomi E, Bowser DN, Sofroniew MV, Khakh BS. Two forms of astrocyte calcium excitability have distinct effects on NMDA receptor-mediated slow inward currents in pyramidal neurons. J Neurosci. 2008;28:6659–6663. doi: 10.1523/JNEUROSCI.1717-08.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shih AY, Johnson DA, Wong G, Kraft AD, Jiang L, Erb H, Johnson JA, Murphy TH. Coordinate regulation of glutathione biosynthesis and release by Nrf2-expressing glia potently protects neurons from oxidative stress. J Neurosci. 2003;23:3394–3406. doi: 10.1523/JNEUROSCI.23-08-03394.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shimizu H, Watanabe E, Hiyama TY, Nagakura A, Fujikawa A, Okado H, Yanagawa Y, Obata K, Noda M. Glial Nax channels control lactate signaling to neurons for brain [Na+] sensing. Neuron. 2007;54:59–72. doi: 10.1016/j.neuron.2007.03.014. [DOI] [PubMed] [Google Scholar]
- Shingo T, Sorokan ST, Shimazaki T, Weiss S. Erythropoietin regulates the in vitro and in vivo production of neuronal progenitors by mammalian forebrain neural stem cells. J Neurosci. 2001;21:9733–9743. doi: 10.1523/JNEUROSCI.21-24-09733.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silver J, Miller JH. Regeneration beyond the glial scar. Nat Rev Neurosci. 2004;5:146–156. doi: 10.1038/nrn1326. [DOI] [PubMed] [Google Scholar]
- Simpson JE, Ince PG, Lace G, Forster G, Shaw PJ, Matthews F, Savva G, Brayne C, Wharton SB. Astrocyte phenotype in relation to Alzheimer-type pathology in the ageing brain. Neurobiol Aging. 2010;31:578–590. doi: 10.1016/j.neurobiolaging.2008.05.015. [DOI] [PubMed] [Google Scholar]
- Sinor AD, Irvin SM, Cobbs CS, Chen J, Graham SH, Greenberg DA. Hypoxic induction of vascular endothelial growth factor (VEGF) protein in astroglial cultures. Brain Res. 1998;812:289–291. doi: 10.1016/s0006-8993(98)00976-7. [DOI] [PubMed] [Google Scholar]
- Siren AL, Fasshauer T, Bartels C, Ehrenreich H. Therapeutic potential of erythropoietin and its structural or functional variants in the nervous system. Neurotherapeutics. 2009;6:108–127. doi: 10.1016/j.nurt.2008.10.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siren AL, Fratelli M, Brines M, Goemans C, Casagrande S, Lewczuk P, Keenan S, Gleiter C, Pasquali C, Capobianco A, Mennini T, Heumann R, Cerami A, Ehrenreich H, Ghezzi P. Erythropoietin prevents neuronal apoptosis after cerebral ischemia and metabolic stress. Proc Natl Acad Sci USA. 2001;98:4044–4049. doi: 10.1073/pnas.051606598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sofroniew MV. Reactive astrocytes in neural repair and protection. Neuroscientist. 2005;11:400–407. doi: 10.1177/1073858405278321. [DOI] [PubMed] [Google Scholar]
- Sofroniew MV. Molecular dissection of reactive astrogliosis and glial scar formation. Trends Neurosci. 2009;32:638–647. doi: 10.1016/j.tins.2009.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sofroniew MV, Vinters HV. Astrocytes: biology and pathology. Acta Neuropathol. 2010;119:7–35. doi: 10.1007/s00401-009-0619-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sorensen AG, Buonanno FS, Gonzalez RG, Schwamm LH, Lev MH, Huang-Hellinger FR, Reese TG, Weisskoff RM, Davis TL, Suwanwela N, Can U, Moreira JA, Copen WA, Look RB, Finklestein SP, Rosen BR, Koroshetz WJ. Hyperacute stroke: evaluation with combined multisection diffusion-weighted and hemodynamically weighted echo-planar MR imaging. Radiology. 1996;199:391–401. doi: 10.1148/radiology.199.2.8668784. [DOI] [PubMed] [Google Scholar]
- Soucek T, Cumming R, Dargusch R, Maher P, Schubert D. The regulation of glucose metabolism by HIF-1 mediates a neuroprotective response to amyloid β peptide. Neuron. 2003;39:43–56. doi: 10.1016/s0896-6273(03)00367-2. [DOI] [PubMed] [Google Scholar]
- Stellwagen D, Malenka RC. Synaptic scaling mediated by glial TNF-α. Nature. 2006;440:1054–1059. doi: 10.1038/nature04671. [DOI] [PubMed] [Google Scholar]
- Stevens B, Allen NJ, Vazquez LE, Howell GR, Christopherson KS, Nouri N, Micheva KD, Mehalow AK, Huberman AD, Stafford B, Sher A, Litke AM, Lambris JD, Smith SJ, John SW, Barres BA. The classical complement cascade mediates CNS synapse elimination. Cell. 2007;131:1164–1178. doi: 10.1016/j.cell.2007.10.036. [DOI] [PubMed] [Google Scholar]
- Stumpf E, Masson H, Duquette A, Berthelet F, McNabb J, Lortie A, Lesage J, Montplaisir J, Brais B, Cossette P. Adult Alexander disease with autosomal dominant transmission: a distinct entity caused by mutation in the glial fibrillary acid protein gene. Arch Neurol. 2003;60:1307–1312. doi: 10.1001/archneur.60.9.1307. [DOI] [PubMed] [Google Scholar]
- Suh SW, Bergher JP, Anderson CM, Treadway JL, Fosgerau K, Swanson RA. Astrocyte glycogen sustains neuronal activity during hypoglycemia: studies with the glycogen phosphorylase inhibitor CP-316,819 ([R-R*,S*]-5-chloro-N-[2-hydroxy-3-(methoxymethylamino)-3-oxo-1-(phenylmet hyl)propyl]-1H-indole-2-carboxamide). J Pharmacol Exp Ther. 2007;321:45–50. doi: 10.1124/jpet.106.115550. [DOI] [PubMed] [Google Scholar]
- Swanson RA, Ying W, Kauppinen TM. Astrocyte influences on ischemic neuronal death. Curr Mol Med. 2004;4:193–205. doi: 10.2174/1566524043479185. [DOI] [PubMed] [Google Scholar]
- Tang G, Perng MD, Wilk S, Quinlan R, Goldman JE. Oligomers of mutant glial fibrillary acidic protein (GFAP) Inhibit the proteasome system in alexander disease astrocytes, and the small heat shock protein αB-crystallin reverses the inhibition. J Biol Chem. 2010;285:10527–10537. doi: 10.1074/jbc.M109.067975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang G, Xu Z, Goldman JE. Synergistic effects of the SAPK/JNK and the proteasome pathway on glial fibrillary acidic protein (GFAP) accumulation in Alexander disease. J Biol Chem. 2006;281:38634–38643. doi: 10.1074/jbc.M604942200. [DOI] [PubMed] [Google Scholar]
- Tang G, Yue Z, Talloczy Z, Hagemann T, Cho W, Messing A, Sulzer DL, Goldman JE. Autophagy induced by Alexander disease-mutant GFAP accumulation is regulated by p38/MAPK and mTOR signaling pathways. Hum Mol Genet. 2008;17:1540–1555. doi: 10.1093/hmg/ddn042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tao J, Wu H, Lin Q, Wei W, Lu XH, Cantle JP, Ao Y, Olsen RW, Yang XW, Mody I, Sofroniew MV, Sun YE. Deletion of astroglial Dicer causes non-cell-autonomous neuronal dysfunction and degeneration. J Neurosci. 2011;31:8306–8319. doi: 10.1523/JNEUROSCI.0567-11.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tateishi N, Mori T, Kagamiishi Y, Satoh S, Katsube N, Morikawa E, Morimoto T, Matsui T, Asano T. Astrocytic activation and delayed infarct expansion after permanent focal ischemia in rats. Part II: suppression of astrocytic activation by a novel agent (R)-(−)-2-propyloctanoic acid (ONO-2506) leads to mitigation of delayed infarct expansion and early improvement of neurologic deficits. J Cereb Blood Flow Metab. 2002;22:723–734. doi: 10.1097/00004647-200206000-00011. [DOI] [PubMed] [Google Scholar]
- Terry RD. Cell death or synaptic loss in Alzheimer disease. J Neuropathol Exp Neurol. 2000;59:1118–1119. doi: 10.1093/jnen/59.12.1118. [DOI] [PubMed] [Google Scholar]
- Terry RD, Masliah E, Salmon DP, Butters N, DeTeresa R, Hill R, Hansen LA, Katzman R. Physical basis of cognitive alterations in Alzheimer's disease: synapse loss is the major correlate of cognitive impairment. Ann Neurol. 1991;30:572–580. doi: 10.1002/ana.410300410. [DOI] [PubMed] [Google Scholar]
- Thompson KA, McArthur JC, Wesselingh SL. Correlation between neurological progression and astrocyte apoptosis in HIV-associated dementia. Ann Neurol. 2001;49:745–752. doi: 10.1002/ana.1011. [DOI] [PubMed] [Google Scholar]
- Tian R, Wu X, Hagemann TL, Sosunov AA, Messing A, McKhann GM, Goldman JE. Alexander disease mutant glial fibrillary acidic protein compromises glutamate transport in astrocytes. J Neuropathol Exp Neurol. 2010;69:335–345. doi: 10.1097/NEN.0b013e3181d3cb52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tishler DM, Weinberg KI, Hinton DR, Barbaro N, Annett GM, Raffel C. MDR1 gene expression in brain of patients with medically intractable epilepsy. Epilepsia. 1995;36:1–6. doi: 10.1111/j.1528-1157.1995.tb01657.x. [DOI] [PubMed] [Google Scholar]
- Uhlmann EJ, Wong M, Baldwin RL, Bajenaru ML, Onda H, Kwiatkowski DJ, Yamada K, Gutmann DH. Astrocyte-specific TSC1 conditional knockout mice exhibit abnormal neuronal organization and seizures. Ann Neurol. 2002;52:285–296. doi: 10.1002/ana.10283. [DOI] [PubMed] [Google Scholar]
- Vanzani MC, Iacono RF, Caccuri RL, Troncoso AR, Berria MI. Regional differences in astrocyte activation in HIV-associated dementia. Medicina (Buenos Aires) 2006;66:108–112. [PubMed] [Google Scholar]
- Vargas MR, Johnson DA, Sirkis DW, Messing A, Johnson JA. Nrf2 activation in astrocytes protects against neurodegeneration in mouse models of familial amyotrophic lateral sclerosis. J Neurosci. 2008;28:13574–13581. doi: 10.1523/JNEUROSCI.4099-08.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verkhratsky A. Physiology of neuronal-glial networking. Neurochem Int. 2010;57:332–343. doi: 10.1016/j.neuint.2010.02.002. [DOI] [PubMed] [Google Scholar]
- Verkhratsky A, Butt A. Chichester: A Textbook, John Wiley & Sons; 2007. Glial Neurobiology. [Google Scholar]
- Verkhratsky A, Olabarria M, Noristani HN, Yeh CY, Rodriguez JJ. Astrocytes in Alzheimer's disease. Neurotherapeutics. 2010;7:399–412. doi: 10.1016/j.nurt.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verkhratsky A, Parpura V. Recent advances in (patho)physiology of astroglia. Acta Pharmacol Sin. 2010;31:1044–1054. doi: 10.1038/aps.2010.108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Voskuhl RR, Peterson RS, Song B, Ao Y, Morales LB, Tiwari-Woodruff S, Sofroniew MV. Reactive astrocytes form scar-like perivascular barriers to leukocytes during adaptive immune inflammation of the CNS. J Neurosci. 2009;29:11511–11522. doi: 10.1523/JNEUROSCI.1514-09.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang L, Colodner KJ, Feany MB. Protein misfolding and oxidative stress promote glial-mediated neurodegeneration in an Alexander disease model. J Neurosci. 2011a;31:2868–2877. doi: 10.1523/JNEUROSCI.3410-10.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang X, Imura T, Sofroniew MV, Fushiki S. Loss of adenomatous polyposis coli in Bergmann glia disrupts their unique architecture and leads to cell nonautonomous neurodegeneration of cerebellar Purkinje neurons. Glia. 2011b;59:857–868. doi: 10.1002/glia.21154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wharton SB, O'Callaghan JP, Savva GM, Nicoll JA, Matthews F, Simpson JE, Forster G, Shaw PJ, Brayne C, Ince PG. Population variation in glial fibrillary acidic protein levels in brain ageing: relationship to Alzheimer-type pathology and dementia. Dement Geriatr Cogn Disord. 2009;27:465–473. doi: 10.1159/000217729. [DOI] [PubMed] [Google Scholar]
- Wilhelmsson U, Li L, Pekna M, Berthold CH, Blom S, Eliasson C, Renner O, Bushong E, Ellisman M, Morgan TE, Pekny M. Absence of glial fibrillary acidic protein and vimentin prevents hypertrophy of astrocytic processes and improves post-traumatic regeneration. J Neurosci. 2004;24:5016–5021. doi: 10.1523/JNEUROSCI.0820-04.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolf F, Kirchhoff F. Neuroscience. Imaging astrocyte activity. Science. 2008;320:1597–1599. doi: 10.1126/science.1160122. [DOI] [PubMed] [Google Scholar]
- Wong M, Ess KC, Uhlmann EJ, Jansen LA, Li W, Crino PB, Mennerick S, Yamada KA, Gutmann DH. Impaired glial glutamate transport in a mouse tuberous sclerosis epilepsy model. Ann Neurol. 2003;54:251–256. doi: 10.1002/ana.10648. [DOI] [PubMed] [Google Scholar]
- Wyss-Coray T, Loike JD, Brionne TC, Lu E, Anankov R, Yan F, Silverstein SC, Husemann J. Adult mouse astrocytes degrade amyloid-β in vitro and in situ. Nat Med. 2003;9:453–457. doi: 10.1038/nm838. [DOI] [PubMed] [Google Scholar]
- Yamanaka K, Chun SJ, Boillee S, Fujimori-Tonou N, Yamashita H, Gutmann DH, Takahashi R, Misawa H, Cleveland DW. Astrocytes as determinants of disease progression in inherited amyotrophic lateral sclerosis. Nat Neurosci. 2008;11:251–253. doi: 10.1038/nn2047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeh C-Y, Verkhratsky A, Rodríguez JJ. Early astrocytic atrophy in the entorhinal cortex of a triple transgenic animal model of Alzheimer's disease. ASN Neuro. 2011;3:e00071. doi: 10.1042/AN20110025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoshida T, Sasaki M, Yoshida M, Namekawa M, Okamoto Y, Tsujino S, Sasayama H, Mizuta I, Nakagawa M. Nationwide survey of Alexander disease in Japan and proposed new guidelines for diagnosis. J Neurol. 2011;258:1998–2008. doi: 10.1007/s00415-011-6056-3. [DOI] [PubMed] [Google Scholar]
- Zador Z, Stiver S, Wang V, Manley GT. Role of aquaporin-4 in cerebral edema and stroke. Handb Exp Pharmacol. 2009:159–170. doi: 10.1007/978-3-540-79885-9_7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang ZG, Zhang L, Jiang Q, Zhang R, Davies K, Powers C, Bruggen N, Chopp M. VEGF enhances angiogenesis and promotes blood-brain barrier leakage in the ischemic brain. J Clin Invest. 2000;106:829–838. doi: 10.1172/JCI9369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao BQ, Wang S, Kim HY, Storrie H, Rosen BR, Mooney DJ, Wang X, Lo EH. Role of matrix metalloproteinases in delayed cortical responses after stroke. Nat Med. 2006;12:441–445. doi: 10.1038/nm1387. [DOI] [PubMed] [Google Scholar]