Abstract
Background
Of all mastectomy patients, 90% will use an external prosthesis where the standard of care uses a stock prosthesis that is purchased “off the shelf.” Our objectives were to determine patient demand for and perceived value of a custom breast prosthesis. The information obtained will influence future research and program direction.
Methods
We asked 65 women who had undergone lumpectomy or mastectomy to participate before exploring rehabilitation options. The quantitative outcome measures were the European Organisation for Research and Treatment of Cancer qlq-C30 general and -BR23 breast cancer–specific quality of life questionnaires, and the Ambulatory Oncology Patients Satisfaction Tool. The qlq results were analyzed using the Mann–Whitney U-test. Results of the satisfaction tool were compared using the Fisher exact and chi-square tests. A descriptive qualitative approach—involving in-depth interviews exploring the experiences of the women—was used to establish the perceived value of the services to the patients. The analysis of the interview transcripts was conducted using a standardized content method to describe the experiences of the women.
Results
All the women had had previous experiences with a conventional prosthesis, and they reported that wearing a custom prosthesis was more satisfying for them. They reported comfort and ease in wearing it, coupled with a sense of feeling less like a victim. Comparison of the qlq and patient satisfaction scores showed no significant difference between the women wearing the conventional prosthesis and those wearing the custom prosthesis.
Conclusions
The qualitative data provide a strong case in support of the new device. Patient demand, perceived benefit, and experience wearing the prosthesis were documented. Suggestions for improvements in the device and in the program operations were gathered and will influence future development of this service.
Keywords: Mastectomy, custom breast prosthesis, mixed methodology, cancer rehabilitation, quality of life
1. INTRODUCTION
The incidence of breast cancer in Canada is continuing to rise. It was estimated that 23,600 new cases of breast cancer would be diagnosed in 2011 1. At the same time, it has been shown that, because of screening techniques, more women are surviving and living longer 2. In cancer rehabilitation, increased emphasis has therefore been placed on survivorship and on the treatment of the whole person, not just the disease 3.
In a study conducted to determine the treatment patterns for women diagnosed with invasive breast cancer in Ontario between April 1, 2003, and March 31, 2004, it was determined that, of the 7121 women diagnosed with breast cancer, 2479 (35%) had undergone complete mastectomy 4. Rates of breast reconstruction were not examined for the Ontario study, but it has been well established that, for a multitude of psychological reasons, not all women will choose to have breast reconstruction. Concern about further complications and the uncertainty about esthetic outcomes after surgery have been cited as reasons why women do not seek surgical rehabilitation 5. Demographic factors such as age, race, and education, together with preoperative counseling, have been shown to influence treatment choice 6. The alternative option is an external breast prosthesis.
It has been estimated that 90% of women undergoing mastectomy use a breast prosthesis either permanently or while awaiting reconstruction 7. The use of breast prostheses appears to help improve body image 8. That finding suggests that the physical characteristics of the prosthesis, among other issues, will influence a woman’s sense of her overall body image.
In the community, patients are potentially referred to two types of services. The first is commercial outlets that provide “off the shelf” external prostheses in standard sizes worn on the surface of the skin by mastectomy and lumpectomy patients, most often within a bra, but sometimes against the chest wall, fixed with self-adhering tapes 9. This option presents several challenges in finding an appropriately sized and comfortable prosthesis. Women are often dissatisfied with various aspects of conventional prostheses 10. They report dissatisfaction with incorrect fit, restrictive choice of clothing and difficulty dressing, discomfort, and prostheses weight and cost 5,9–13. The second kind of service is providers who make custom-fitted prostheses. These prostheses are individually designed to conform to the surface of the skin, based on a tissue record (impression) of the patient’s mastectomy site. They are held in place using various methods. A custom prosthesis offers the opportunity to simulate the missing tissue more realistically than a manufactured prosthesis can, and the custom prosthesis can be designed to address the aforementioned issues that cause dissatisfaction with stock prostheses. However, while a stock prosthesis may cost $200 to $400, a custom prosthesis may run as high as $4000–$5000 (rough cost estimates).
The present study was conducted to determine if patients perceive any value in the provision of custom breast prostheses as an additional option to traditional rehabilitation services for mastectomy and lumpectomy patients. The research objectives were to determine
patient demand for custom breast prostheses that would address the shortfalls of stock prostheses,
whether patients would perceive added value in a custom breast prosthesis over a stock prosthesis, and
whether patients were satisfied with the services received.
2. METHODS
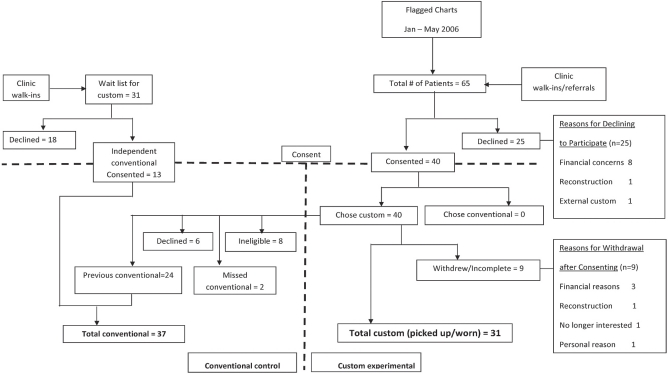
The study was intended to be conducted as a cohort trial, following patients who chose between an experimental custom external breast prosthesis and a conventional external breast prosthesis (Figure 1). However, given that all the consenting patients chose the custom prosthesis option, it became necessary to change the plan to a before-and-after design to take advantage of earlier experiences with conventional prostheses to create a control group. Other patients on the waitlist for a custom prosthesis, but who were willing to wear a conventional prosthesis on an interim basis, were also recruited so as to enlarge the control group, which increased the statistical power of the study.
FIGURE 1.
Pilot trial study design and number of patients flow chart.
2.1. Patients
Because this was a pilot study, an a priori sample size determination was not completed. Staff identified a convenience sample of patients by flagging the charts of those who were being followed in the Breast Site Group at a tertiary care cancer centre after active treatment for breast cancer. Additional recruitment was attained by posting a flyer in selected areas of the cancer centre and the patient support centre. Patients who had heard about the study from other participants also walked in with inquiries and wanted to enrol. Those patients were recruited to participate in the trial.
Because all 40 of the consenting patients chose the experimental custom prosthesis option, they were asked to complete a second set of surveys and were interviewed about their prior prostheses experiences, which served as their own historical control. Later, a further 31 patients on a waitlist for custom prostheses were recruited to enlarge the control group (13 consented). Those patients were not given the option of a custom prosthesis.
2.2. Procedures
In addition to the information about rehabilitation options that is normally given to Breast Site patients during follow-up visits, information sheets describing the study, with consent forms, were given to eligible patients. Follow-up with consenting patients in both the experimental and control groups was conducted by monthly telephone calls from the research assistant until after each individual’s prosthetic treatment was completed. Patients in the control group had their prostheses fitted by a provider in the community. The providers for the custom prostheses were male clinical anaplastologists, who were accompanied by a female attendant.
At the start of the study, a conventional breast prosthesis was partially funded by the provincial government to a maximum of $220. A custom breast prosthesis was also partially funded, leaving the patient responsible for 25% of the $831.30 total fee prescribed by the government. The cost to the patient for the custom prosthesis was $207.83. Vendors willing to provide custom prostheses at that fee could not be found in the community. After only 3 patients had been recruited to the study, the government announced a change in policy regarding the way it would provide support for all breast prostheses. For patients starting treatment after the new policy implementation date, funding would be limited to $195 for conventional or custom prostheses. For patients whose treatment started after the implementation date, that announcement effectively added more than $428 to the cost of the service, for a total of $635.83.
For patients accepted for custom prostheses, the routine used in the fabrication of facial prostheses was followed: making impressions, sculpting the fit, matching the colour, and having a final fitting.
After an initial consultation at the Craniofacial Prosthetic Unit, the first treatment visit involved making an impression of the affected area of the breast and the contralateral side, which was used to clinically determine the shape and volume for the prosthesis, which was sculpted at a subsequent appointment. That subsequent appointment was also used for formulating a custom silicone palette for matching the colour. The making of the mould and additional sculpting was done in the laboratory, where the patient’s presence was not required. The final appointment involved extrinsic painting of the prosthesis to more closely match the characterization of the surrounding tissues, delivery of the prosthesis to the patient, and education on its maintenance. At that appointment, patients were asked to call if they experienced any problems with the prosthesis. Otherwise, the experiences of the patients with the service were monitored through the research assistant’s follow-up calls.
2.3. Data Collection
To examine patient demand, descriptive information (including demographics) was gathered on the number of patients to whom the study information had been given, the number who sought a referral for a custom prosthesis and for outside conventional fitters, and the number in each cohort group who ultimately had a prosthesis made. Qualitative data were also collected on the perspectives of the women about decision-making regarding the prosthesis.
To assess perceived value added of the custom prosthesis, both quantitative and qualitative data were gathered. Patients were asked to complete validated satisfaction and quality-of life-tools. The tools were sent to each woman’s home 2 months after completion of their treatment. The tools used were these:
The Ambulatory Oncology Patients Satisfaction Tool 14 sections on “planning your treatment,” “symptom management,” “health care providers,” “overall impressions of your care,” and “your background.” This validated instrument is designed with Likert-type answer options to measure the patient’s views on the treatment process. Not all questions from this instrument, such as those on chemotherapy or nutritional needs, were analyzed because of the limited likelihood that they would be affected by any breast prosthesis service.
The European Organisation for Research and Treatment of Cancer (eortc) qlq-C30 15 and -BR23 16 general and breast-specific quality-of-life questionnaires. These validated measures are widely used to determine quality of life among cancer patients generally (-C30) and among breast cancer patients specifically (-BR23). Scores are reported on a 0–100 scale, with higher scores representing a higher level of functioning, more symptoms, or an increased number of side effects.
In addition, the research assistant interviewed patients over the telephone, using open-ended questions that focused on the women’s experiences in deciding about the prosthesis, receiving the prosthesis, and using the prosthesis. Questions were also posed about the quality of the prosthetic service and how it could be improved.
2.4. Analysis
Data on patient demand are reported using descriptive statistics and qualitative highlights describing decision-making about the prosthesis. Quantitative results for the standardized quality-of-life tools were analyzed using the Mann–Whitney U-test to determine differences between the women using a conventional prosthesis and those using the custom-designed prosthesis. Comparisons of the satisfaction analysis used the Fisher exact or chisquare test. Results were considered significant at p ≤ 0.05.
The qualitative data from the patient interviews were subjected to a standardized content analysis 17. Three team members read through the data from the interviews and created content category labels after discussions of their impressions of the information given in response to each question. One team member then coded all the data. Review of the coded data by three team members allowed for comparison across the participant experiences and identification of common perspectives from each content category. Those perspectives are reported in narrative terms, with selected items of note, including quotations where relevant.
The satisfaction, quality-of-life, and qualitative results from the patients with control conventional prostheses from the cohort portion of the trial (given the choice of prosthesis) were compared with the results from the patients who were recruited later for their use of conventional prostheses (without being given a choice for a custom prosthesis). Because no differences were found between the two control groups, they were combined for comparison with the experimental custom group. The satisfaction of the study patients with the services was also compared with the satisfaction expressed by the general population of patients at the cancer centre.
3. RESULTS
During the 5-month period of patient accrual, a total of 221 charts of women who could potentially be study candidates were flagged. The primary cancer care team, consisting of oncologists and oncology nurses, were responsible for sharing the information about the trial with the women during their follow-up clinic appointments. The women then made the decision to contact the research assistant about participating in the study.
3.1. Patient Demand
Of 65 women who discussed the trial with the research assistant (Figure 1), 25 did not participate. Of those 25, 11 did not return the research assistant’s calls, and 8 declined for financial reasons. The remaining 6 declined for a variety of other reasons.
Of the 40 consenting patients, 31 completed the process of being fitted for a custom prosthesis, and 9 withdrew for a variety of reasons (3 financial, 1 reconstruction, 1 not interested, 4 personal). When the same group was asked to serve as historical controls, 6 declined (not interested in participating in that arm of the study), 8 were ineligible (did not wear a conventional prosthesis), and 2 acted as their own control after being fitted for a custom prosthesis. Thus, 24 patients served as their own controls, supplemented by 13 patients from the waiting list who used conventional prostheses, for a total control group of 37 patients. Ultimately, 27 women in the control group completed surveys, and 24 were interviewed. In the custom arm of the project, of the 31 women who received and wore a custom prosthesis, 24 completed surveys, and 19 were interviewed.
3.2. Selected Sample Characteristics
The women who reported on their experiences with the custom prosthesis each had had previous experiences with a conventional approach. Results are presented separately for those groups, although both groups were equivalent in terms of age, marital status, and education level (Table i).
TABLE I.
Selected sample demographics
| Variable |
Prosthesis group |
|
|---|---|---|
| Conventional | Custom | |
| Completed surveys (n) | 27 | 24 |
| Age (years) | ||
| Mean ± sd | 51.7±13.0 | 51.1±12.5 |
| Range | 28–83 | 28–76 |
| Highest level of schooling (%) | ||
| High school | 7 | 13 |
| University/college | 37 | 33 |
| Postgraduate | 48 | 46 |
| Marital status (%) | ||
| Single | 22 | 21 |
| Married/common law | 50 | 57 |
| Separated/divorced/widowed | 28 | 22 |
sd = standard deviation.
3.3. Patient Perceived Added Value
The perceived added value of the new custom prosthesis over a conventional prosthesis was explored both quantitatively and qualitatively. Women completed standardized quality-of-life and service satisfaction scales and participated in semi-structured telephone interviews.
3.4. Quality of Life
Women completed the general eortc qlq-C30 (including breast cancer–specific items) and the eortc -BR23 (breast-cancer-specific module) to measure their quality of life. Table ii presents the overall quality-of-life and subscale scores for the qlq-C30. The values for all domains and for both groups are substantially higher than the mean reference values given by eortc for breast cancer patients at all stages 15. The highest mean total subscale scores were reported in physical functioning and role functioning for both groups. The lowest mean total subscale scores were for emotional functioning. However, no significant differences were observed between the groups for any of the functional subscales for global health scores.
TABLE II.
Scores on selected scales of the European Organisation for Research and Treatment of Cancer Quality of Life Questionnaire – C30
| Domain |
Total score for completed surveys by prosthesis group |
p Value | |||
|---|---|---|---|---|---|
|
Conventional (n=27) |
Custom (n=24) |
||||
| Mean±sd | Range | Mean±sd | Range | ||
| Physical functioning | 88.04±16.38 | 40–100 | 90.76±11.68 | 47–100 | 0.953 |
| Emotional functioning | 81.00±13.22 | 58.0–100 | 79.17±23.36 | 0.00–100 | 0.552 |
| Role functioning | 85.15±26.03 | 0.00–100 | 88.83±18.20 | 33.0–100 | 0.991 |
| Cognitive functioning | 84.44±16.63 | 33.0–100 | 82.63±21.70 | 33.0–100 | 0.936 |
| Social functioning | 83.30±25.32 | 17.0–100 | 85.52±22.67 | 33.0–100 | 0.729 |
| Global health | 76.22±19.68 | 33.0–100 | 77.38±21.28 | 33.0–100 | 0.773 |
sd = standard deviation.
Table iii highlights specific symptoms and psychosocial items from the general qlq-C30 that the research team thought would be relevant to women with a breast prosthesis. These items were ones that the team anticipated would be most likely to change once the women started wearing the new custom prostheses. Other items such as diarrhea and difficulty concentrating while reading a newspaper were not used. For all of the analyzed items, with the exception of sexual functioning, mean total scores were higher for the new custom prosthesis group than for the conventional prosthesis group. However, the differences were not statistically significant.
TABLE III.
Scores for selected items related to breast symptoms on the European Organisation for Research and Treatment of Cancer Quality of Life Questionnaire – C30
| Item |
Score for completed surveys by prosthesis group |
p Value | |||
|---|---|---|---|---|---|
|
Conventional (n=27) |
Custom (n=24) |
||||
| Mean±sd | Range | Mean±sd | Range | ||
| Breast symptom | 11.37±11.86 | 0.00–42.0 | 14.58±18.05 | 0.00–83 | 0.647 |
| Body image | 67.89±27.62 | 8.00–100 | 72.92±26.84 | 0.00–100 | 0.474 |
| Future perspective | 50.78±33.91 | 0.00–100 | 58.54±26.57 | 0.00–100 | 0.457 |
| Sexual functioning | 65.95±15.60 | 17.0–83 | 62.27±18.28 | 17.0–83.0 | 0.569 |
| plus nr | plus na | ||||
| Sexual enjoyment | 38.83±24.11 | 0.0–67.0 | 46.60±17.56 | 33.0–67.0 | 0.458 |
| plus na | plus na | ||||
| Arm symptom | 12.26±16.90 | 0.00–56.0 | 19.79±23.36 | 0.00–89.0 | 0.242 |
sd = standard deviation; nr = not reported; na = not available.
Table iv presents participant responses for selected items from the qlq-BR23 module. The research team selected items that they thought would be the ones most likely to change once the women started wearing the new custom prostheses. The most notable differences observed between the groups related to the items about “feeling less attractive” (41% in the conventional group and 21% in the custom group) and “feeling less feminine” (37% in the conventional group and 17% in the custom group) because of cancer and its treatment, and the extent of “[engagement] in sexual activity” (5% in the conventional group and 18% in the custom group). Another item of interest was “pain in your arm or shoulder” because of its relationship to the defect site (11% in the conventional group and 25% in the custom group). None of the foregoing observations was statistically significant.
TABLE IV.
Response to selected items on the European Organisation for Research and Treatment of Cancer Quality of Life Questionnaire breast-cancer–specific module – BR23
| Item |
Responses of “quite a bit” or “very much” by prosthesis group (%) |
p Value | |
|---|---|---|---|
| Conventional (n=27) | Custom (n=24) | ||
| In the past week | |||
| Felt physically less attractive as a result of your disease or treatment | 41 | 21 | 0.312 |
| Feeling less feminine as a result of your disease or treatment | 37 | 17 | 0.278 |
| Find it difficult to look at yourself naked | 7 | 8 | 0.550 |
| Been dissatisfied about your body | 22 | 21 | 0.936 |
| Were worried about your health in the future | 33 | 21 | 0.457 |
| In the past 4 weeks | |||
| Pain in your arm or shoulder | 11 | 25 | 0.615 |
| Have a swollen arm or hand | 11 | 13 | 0.292 |
| Difficult to raise your arm or to move it sideways | 0 | 4 | 0.052 |
| Pain in the area of your affected breast | 4 | 8 | 0.991 |
| Area of your affected breast swollen | 0 | 4 | 0.839 |
| Area of your affected breast oversensitive | 4 | 8 | 0.316 |
| Skin problems on or in the area of your affected breast | 4 | 4 | 0.950 |
| Extent your were interested in sex | 20 | 9 | 0.040 |
| Extent to which you were sexually active | 5 | 18 | 0.294 |
| If sexually active: Extent to which sex is enjoyable for you | 67 | 60 | 0.539 |
3.5. Ambulatory Patient Satisfaction Data
Women completed the patient satisfaction survey used at the cancer centre, which provided a comparison between the satisfaction of the women in the study and the satisfaction of the overall patient population. Four specific items were selected as ones that might be improved because of involvement with the custom prosthesis staff and participation in the breast prosthesis study. Table v presents those four items, together with data from the same time period for all the general clinic patients who responded to the overall survey. The percentage who were satisfied with the information received about possible changes in physical appearance and possible emotional changes was higher for study participants than for general responders to the survey. Similar differences were not observed based on information provided about changes in sexual activity or in the relationship with a spouse or partner. The participating women also provided an overall rating regarding their health. In contrast to the general survey responders, the women participating in this pilot study saw themselves as being in very good or excellent health (Table v). None of the observations was statistically significant.
TABLE V.
Results on the cancer centre’s Ambulatory Patient Satisfaction scale
| Item |
Respondents with positive results (%) |
p Value |
|||||
|---|---|---|---|---|---|---|---|
|
General clinic patients |
Prosthesis group |
C vs. D | D vs. B | ||||
| (A) 2007 (n=322,rr=55.0%) | (B) 2008 (n=265,rr=45.3%) | (C) Conventional (n=27) | (D) Custom (n=24) | ||||
| Did you get enough information about ... | |||||||
| 40. | ... possible changes in your physical appearance? | 59.8 | 51.9 | 76.9 | 72.7 | 0.572 | 0.078 |
| 41. | ... possible changes in your sexual activity? | 48.4 | 47.7 | 46.2 | 47.8 | 0.920 | 0.863 |
| 42. | ... possible changes in your emotions? | 42.2 | 33.7 | 57.7 | 47.8 | 0.488 | 0.227 |
| 44. | ... possible changes in your relationship with your spouse or partner? | 36.8 | 32.9 | 47.8 | 39.1 | 0.442 | 0.639 |
rr = response rate.
3.6. Patient Perspective and Experience Data
The telephone interviews with the women took an average of 30 minutes to complete. The data presented from the standardized content analysis focus on the perspectives of the interviewees about the value of their prosthesis and their satisfaction with the service delivery.
3.6.1. How Did They Hear About the Trial?
Most of the women heard about the opportunity to participate in the custom breast prostheses trial through their nurse (“the advance practitioner nurse told me”). A few women found the information on the posted flyer or received it from other patients who were enrolled in the study.
3.6.2. What Motivated Them to Inquire About It?
Most of the women who inquired about the custom breast prostheses project were motivated to do so because they believed that the new approach would be a good alternative to the conventional approach. The new prostheses sounded attractive and appealed to them. They wanted to have something that they could wear, and they were interested in pursuing an approach that could be more comfortable than the conventional approach that they were currently using (“I am not impressed with what is being offered as a replacement breast”).
3.6.3. How Did They Decide to Choose One Prosthesis Over the Other?
Most women who selected the new custom prosthesis over the conventional approach perceived that the option provided a strong alternative to reconstructive surgery. When they saw the quality of the prosthesis, they thought that it was attractive and appealing. Additionally, the reputation of the services provided at the hospital gave them a sense of comfort when thinking about trying a new approach (“I have already been through so much and didn’t want to go through another surgery so soon after the first”).
3.6.4. What Were Their Experiences with Each Type of Prosthesis?
The women who described their experiences with a conventional breast prosthesis spoke about difficulties with comfort (“it is so hot I can only keep it on for a few hours at a time”), the fit and shape (“it does not fit properly even though I got it fitted at the store.... I still have to stuff it and work with it.... and there are just not enough sizes”), and appearance (“I can’t wear a see-through bra because the prosthesis is not the right colour”; “it helps to create an illusion, but you need to have clothing on for it to work”). The participants identified a need for more choice in prostheses after a mastectomy and for more financially accessible options to be available. Many stated that they had received little information about breast prostheses, where to obtain them, or how to access funding or reimbursement.
Overall, the women who had experienced wearing the new custom breast prosthesis responded that many of the issues they had experienced while wearing a conventional prosthesis were markedly improved. They found the custom prosthesis fairly comfortable and light in weight (“I like the lightness of it; it feels like it’s me”), better fitting with clothing (“it fits so well that I can hardly believe I am wearing it”), and natural looking (“I do not have to think about how it looks. It is so realistic”). Women talked about the psychological benefit of the custom prosthesis: it helped them feel less like a “victim” and more “normal.” In being assessed and fitted for the new prosthesis, women found that they were well informed about the use of the prosthesis and its care. The main difficulties these women experienced were of a technical nature. The prosthesis could, on occasion, deflate and might lose its capacity to adhere after 10 days or 2 weeks. For some, the prosthesis did not move exactly like a normal breast, and they still experienced difficulties wearing normal bras or revealing clothing (“the custom prosthesis is not a breast, it doesn’t solve everything”).
3.6.5. What Were Their Suggestions for Improvement?
The primary areas in which the women suggested that improvement could be made were education and support (“there should be someone to talk to about this”). The women identified the need to receive clear and relevant information about prosthesis options early in the process of cancer diagnosis and treatment (“advertise in the surgeon’s office”). Access to a custom prosthesis was seen to have a psychological benefit to women if the prosthesis was affordable and if the practical issues related to durability were resolved (“most positive experience throughout my cancer journey”).
4. DISCUSSION
Given the number of women who have expressed concerns about conventional approaches regarding breast prostheses 5,9–13, there is a strong potential for a new approach that could provide a more comfortable fit and natural appearance without the need to undergo additional surgery. The advent of new materials and the availability of clinical anaplastologists who have developed new techniques make the actual production in a custom approach possible. However, there is a need to determine both patient demand and perceived value of the new prosthesis before recommending a full-service program.
Our study was limited by several factors related to methodologic design, all of which introduced bias into the results. Because the study took place in a tertiary health care setting, it has a highly self-selected sample of convenience. In addition, because this was a feasibility study, a priori sample size determination was not completed. The trial was intended to be conducted as a cohort trial that would follow patients who chose between an experimental custom external breast prosthesis and a conventional external breast prosthesis. However, because all the consenting patients chose the custom option, it became necessary to change the trial to a before-and-after design to take advantage of the earlier experiences of the women with conventional prostheses to create a control group. That type of design makes it difficult to determine whether an unknown factor is responsible for the result and also to account for other exposures that might have influenced the results. Seeing the actual prosthesis during the recruitment process may have influenced the decisions taken by the women. They found the look and feel of the prosthesis attractive and rather appealing when they first saw it. This prior exposure to the intervention may have given rise to the patients’ preferential search for the desired outcome and may have increased the attention the researchers gave to the experimental group. In addition, volunteers tend to have better outcomes than non-volunteers.
Despite the limitations of the study, the issue of patient demand was clarified. Accrual for this study was filled within 5 months after its announcement to the cancer centre’s patients. The women who consented went on to select the new custom prosthesis over the conventional approach. Of the 65 women who discussed the research project with the assistant, 54 were still “willing to pay” (wtp) out of pocket for a prosthesis, and an additional 31 patients were on a waitlist to get into the study. From an economic standpoint, the wtp approach is an indicator of the value of a commodity and gives rise to demand 18. Upon inspection of the demographics, it is not surprising then that wtp has been positively associated with education, income, beliefs, and the ideological acceptance of health care 19. When coupled with the fact that, during the qualitative interview process, women expressed the need for more options, wtp helps to clarify the demand for this type of service. Still, the major deterrent for declining participation in the study was the increase in cost because of lower government reimbursement (11 women). Most women spoke about the need to have more options available to them after a mastectomy and to have more financially accessible options for prosthetic services. Issues related to cost and access to care should be addressed because they relate both to conventional and to custom prosthetic care. It is often easier to have a breast implant procedure covered through a national health care program or private insurance than it is to have a breast prosthesis made. Women who elect—for either personal or health reasons—not to have additional surgery to restore their breast contour are therefore faced with the burden of having to pay for a prosthesis 20. It is evident that gaps exist in current breast prosthesis services for women when it comes to accessibility, equity, quality, and financial resources 21,22. Any future program would need to consider how best to assist women with the expense of this service.
Value added was addressed through both quantitative and qualitative measures, and showed mixed results. Patton postulated that a mixed-methods approach to research is a form of comparative analysis 23. Comparative research is an acknowledgement of the numerous problems of translation of evidence. Comparison can strengthen reliability, but there is often disagreement when the data do not come together as an integrated whole 24. Focusing on what is learned by the degree of convergence rather than forcing a dichotomous choice typically yields a more balanced result overall 23.
In using the quantitative measures, we narrowed our focus to questions that were thought most likely to be influenced by the wearing of the custom prosthesis. Women in the custom group felt more attractive and more feminine, and were more engaged in sexual activity, but they also experienced more pain in the arm or shoulder. Although we were able to establish some interesting observations related to body image, quantitative measures can be very broad in their scope, and it can be difficult to be certain that the outcome is a direct result of the treatment effect. For example, the source of the pain for the women was not identified specifically during this data collection, and so we are uncertain whether the pain was a result of wearing the prosthesis or whether the women in the custom group had a higher rate of morbidity or lymphedema, which would result in increased pain.
The lack of statistically significant findings in the quality-of-life measures was disappointing, but given the small sample size, that result should not be entirely surprising. A larger sample size is needed to determine if there are real differences from a quantitative perspective. Future research is needed to measure specific outcomes for women who choose to wear a custom prosthesis. Measurement tools that focus specifically on capturing the outcomes directly related to the new program’s interventions need to be used.
The qualitative data illustrate a perceived benefit of the new custom prostheses to the women who elected to wear them. In particular, their observations about feeling an increased degree of normalcy and feeling less like a victim are strong psychosocial benefits. Those data are encouraging. They support efforts to improve the custom prostheses service for future implementation and for further in-depth research to analyze the effects of using a prosthesis.
The quantitative and qualitative approaches showed mixed results with respect to patient satisfaction. In addition to looking for a difference between the custom and conventional groups, we hypothesized that a difference in patient satisfaction scores might be observable between the patients in the study and those in the general population of the cancer centre, given that the women in the study had more access to information. But the quantitative satisfaction scores failed to demonstrate any statistically significant findings, most likely for the same reasons that the quality-of-life scores were not significantly different.
The actual delivery of the service went relatively well from the perspective of the women, although there were several points of learning. An initial technical problem with the prosthesis itself was revealed through feedback from the women; that problem was corrected as the trial continued. The tendency for the prosthesis to deflate over time was reported and has led to the development of a new design for the custom prosthesis.
Feedback from the women supports the idea of sharing information in writing about prostheses and reconstructive surgery early in the process of telling patients about treatment options and effects. Although they may not read the information at the time of their diagnosis, they would have the information readily available for future reference. Study participants reported little consistency in what they were told about prosthesis services. However, once they were part of the trial, they reported that their access to prosthesis information was very satisfactory.
Although there were suggestions for improvement, the women were, in general, satisfied with the construction of the prostheses, and they agreed that the new approach addressed the shortfalls of conventional stock prostheses. They were also satisfied with the quality of the service they received. Most women felt that their prosthesis was comfortable, lightweight, and stable while in place, and that the staff was friendly and professional. A custom approach to prosthetic rehabilitation is the standard of care for most major categories of assistive devices—except for breast prostheses. It is this type of attention to care that makes it possible to address the needs of the patient and not the disease.
5. CONCLUSIONS
The willingness of women to pay for a prosthesis and the qualitative results from the present study demonstrate that there is demand for a custom approach to treatment. However, financial assistance would most likely be needed to make such a service universally accessible. If a mixed-methods approach had not been applied to this initial exploration of women’s experiences with custom breast prostheses, the essence of the perceived value of the custom prosthesis would have been lost. Quantitative measures suggest that there is no difference between custom and conventional breast prostheses, but the qualitative data captured in this study provide a sense of aspects of care that a standardized outcome measure cannot capture. Further research with a larger sample size is needed to determine if real differences from a quantitative perspective are possible.
6. ACKNOWLEDGMENTS
Thanks to Wendy Grennier and David Morrison for their participation in and contributions to the present study.
The details of the prosthesis fabrication procedures, a subsequent project exploring the materials aspects of the prostheses, and a full analysis of the women’s experiences wearing breast prostheses will be presented in a separate article.
Footnotes
7. CONFLICT OF INTEREST DISCLOSURES
The authors of the present work received reimbursement from the Assistive Devices Program in Ontario.
8. REFERENCES
- 1.Canadian Cancer Society and the National Cancer Institute of Canada. Canadian Cancer Statistics 2008. Toronto: Canadian Cancer Society; 2008. [Google Scholar]
- 2.Sun J, Chapman J, Gordon R, Sivaramakrishna R, Link M, Fish E. Survival from primary breast cancer after routine clinical use of mammography. Breast J. 2002;8:199–208. doi: 10.1046/j.1524-4741.2002.08403.x. [DOI] [PubMed] [Google Scholar]
- 3.Braude HD, Macdonald N, Chasen M. Healing and survivorship: what makes a difference? Curr Oncol. 2008;15:185–7. doi: 10.3747/co.v15i4.288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Quan ML, Hodgson N, Przybysz R, et al. Surgery for breast cancer. In: Urbach DR, Simunovic M, Schultz SE, editors. Cancer Surgery in Ontario: ICES Atlas. Toronto: Institute for Clinical Evaluative Sciences; 2008. pp. 7–28. [Google Scholar]
- 5.Handel N, Silverstein MJ, Waisman E, Waisman JR. Reasons why mastectomy patients do not have breast reconstruction. Plast Reconstr Surg. 1990;86:1118–22. doi: 10.1097/00006534-199012000-00012. [DOI] [PubMed] [Google Scholar]
- 6.Pusic A, Thompson TA, Kerrigan CL, et al. Surgical options for early-stage breast cancer: factors associated with patient choice and postoperative quality of life. Plast Reconstr Surg. 1999;104:1325–33. doi: 10.1097/00006534-199910000-00013. [DOI] [PubMed] [Google Scholar]
- 7.Rowland JH, Holland JC, Chaglassian T, Kinne D. Psychological response to breast reconstruction. Expectations for and impact on postmastectomy functioning. Psychosomatics. 1993;34:241–50. doi: 10.1016/S0033-3182(93)71886-1. [DOI] [PubMed] [Google Scholar]
- 8.Fallowfield LJ, Hall A, Maguire GP, Baum M. Psychological outcomes of different treatment policies in women with early breast cancer outside a clinical trial. BMJ. 1990;301:575–80. doi: 10.1136/bmj.301.6752.575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Thijs–Boer FM, Thijs JT, van de Wiel HB. Conventional or adhesive external breast prosthesis? A prospective study of the patients’ preference after mastectomy. Cancer Nurs. 2001;24:227–30. doi: 10.1097/00002820-200106000-00009. [DOI] [PubMed] [Google Scholar]
- 10.Hart S, Meyerowitz BE, Apolone G, Mosconi P, Liberati A. Quality of life among mastectomy patients using external breast prostheses. Tumori. 1997;83:581–6. doi: 10.1177/030089169708300221. [DOI] [PubMed] [Google Scholar]
- 11.Korvenoja ML, Smitten K, Asko–Seljavaara S. Problems in wearing external prosthesis after mastectomy and patient’s desire for breast reconstruction. Ann Chir Gynaecol. 1998;87:30–4. [PubMed] [Google Scholar]
- 12.Roberts S, Livingston P, White V, Gibbs A. External breast prosthesis use: experience and views of women with breast cancer, breast care nurses, and prosthesis fitters. Cancer Nurs. 2003;26:179–86. doi: 10.1097/00002820-200306000-00002. [DOI] [PubMed] [Google Scholar]
- 13.Lee J. Breast prostheses. BMJ. 1991;302:43–4. doi: 10.1136/bmj.302.6767.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fitch M, Green E. Measuring patient satisfaction across the cancer system. Support Care Cancer. 2005;13:472. [Google Scholar]
- 15.European Organisation for Research and Treatment of Cancer, eortc Group for Research into Quality of Life. eortc qlq-C30. Brussels. Belgium: eortc; 1994. [Available online at: http://groups.eortc.be/qol/questionnaires_qlqc30.htm; cited 2007] [Google Scholar]
- 16.European Organisation for Research and Treatment of Cancer, eortc Group for Research into Quality of Life. Specimen of eortc qlq-BR23. Brussels, Belgium: eortc; 1994. [Available online at: http://groups.eortc.be/qol/downloads/modules/specimen_20qlq_br23.pdf; cited 2007] [Google Scholar]
- 17.Denzin NK, Lincoln YS, editors. Handbook of Qualitative Research. Thousand Oaks, CA: Sage; 1994. [Google Scholar]
- 18.Gafni A. Willingness-to-pay as a measure of benefits. Relevant questions in the context of public decision-making about health care programs. Med Care. 1991;29:1246–52. doi: 10.1097/00005650-199112000-00007. [DOI] [PubMed] [Google Scholar]
- 19.Golan EH, Shechter M. Contingent valuation of supplemental health care in Israel. Med Decis Making. 1993;13:302–10. doi: 10.1177/0272989X9301300406. [DOI] [PubMed] [Google Scholar]
- 20.Moore KA. Breast cancer patients’ out-of-pocket expenses. Cancer Nurs. 1999;22:389–96. doi: 10.1097/00002820-199910000-00007. [DOI] [PubMed] [Google Scholar]
- 21.Livingston P, Roberts S, White V, Gibbs A, Bonnici D, Hill D. Do women have equitable access to quality breast prosthesis services? Aust N Z J Public Health. 2000;24:452–3. doi: 10.1111/j.1467-842X.2000.tb01612.x. [DOI] [PubMed] [Google Scholar]
- 22.Livingston PM, White V, Roberts S, Pritchard E, Gibbs A, Hill DJ. Access to breast prostheses via a government-funded service in Victoria, Australia. Experience of women and service providers. Eval Rev. 2003;27:563–8. doi: 10.1177/0193841X03256136. [DOI] [PubMed] [Google Scholar]
- 23.Patton MQ. Enhancing the quality and credibility of qualitative analysis. Health Serv Res. 1999;34:1189–208. [PMC free article] [PubMed] [Google Scholar]
- 24.Fielding NG, Fielding JL. Linking Data. Beverly Hills, CA: Sage Publications; 1986. Qualitative Research Methods Series 4. [Google Scholar]