Abstract
Although persons with disabilities of all kinds have as wide a range of health conditions as the general population, they are profoundly underrepresented in mainstream health research. Such underrepresentation might contribute to the health disparities in this population. We propose the concept of Universal Design of Research (UDR), which would promote routine inclusion of persons with disabilities in mainstream biomedical studies, without the need for adaptation or specialized design. Elements of UDR include the use of multi-sensory formats for recruiting participants, presenting research instruments and interventions, and data gathering from participants, and should promote the inclusion of participants with a wide range of abilities, thus enhancing the generalizability of results.
INTRODUCTION
More than 20 years have passed since the Americans with Disabilities Act became law (1). Among the many benefits provided by this landmark legislation was the requirement for health professionals to make reasonable accommodations to provide health care to individuals with disabilities equivalent to that provided to those without disabilities. However, evidence exists that those with disabilities are often not served well by the U.S. health care system (2–5). One reason for this disparity is that persons with disabilities are grossly underrepresented in mainstream health research (research not focused on disability) (6). Although such individuals are a part of all geographic communities and have as wide a range of health conditions as the general population, several major publications addressing the state of health care for people with disabilities in the U.S. note that researchers often explicitly or implicitly exclude this group (3–7). Consequently, even though many persons with disabilities have conditions common in the general population, such as diabetes, cardiac disease, or cancer, most translational studies about such diseases do not include these people. As a result, we do not know to what extent study findings may generalize to those with disabilities. In this Commentary, we propose Universal Design of Research (UDR) as a new model for including persons with disabilities in mainstream research (Fig. 1).
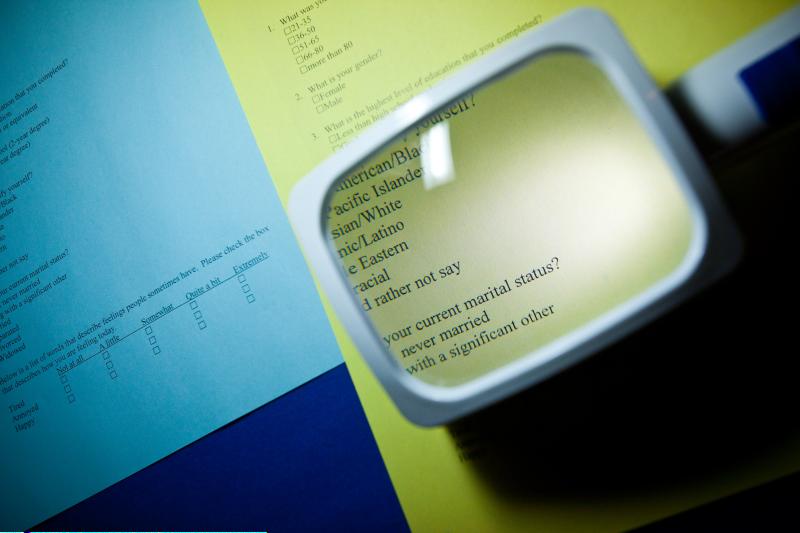
Fig. 1. Making biomedical studies more inclusive through UDR.
Providing a magnifier to allow persons with visual disabilities to read a questionnaire is an example of a simple adaption that can promote the participation of disabled individuals in mainstream research studies.
CREDIT: TKTK
BACKGROUND
Disabilities in the U.S. health care system
According to the U.S. Centers for Disease Control and Prevention, an estimated 47.5 million Americans, or 22% of the U.S. population, have a disability, defined as specific functional or sensory limitations (8). Among this group are 13.5 million people (6.2% of Americans) who have trouble with activities of daily living, 7.7 million (3.5% of Americans) who have trouble seeing words in regular print, and 7.7 million (3.6% of Americans) who have trouble hearing normal conversation. In some sub-populations (for example, people over the age of 65, or with diabetes or cardiac disease) the percentages of persons with disabilities are even higher.
Healthcare professionals often equate disability with poor health, even though many persons with disabilities live long, healthy, and active lives. However, persons with disabilities are at high risk for developing poor health for a variety of reasons, including (i) susceptibility to the same chronic health conditions that affect many Americans (for example, cardiac conditions, diabetes, overweight, cancer, and arthritis); (ii) sequelae of their disabling conditions; and (iii) the lack of equal care for people with disabilities in the American health care system, because of a lack of reasonable accommodations (2–6).
In spite of the fact that persons with disabilities use health care more frequently than the general population, they are profoundly underrepresented in mainstream health research (6). For example, 20% of individuals with diabetes describe difficulty seeing (9), and insulin pens have been widely used to inject insulin by visually impaired people since their introduction in the late 1980s. However, even though copious research exists on patient accuracy of dosing with insulin pens, such studies have routinely excluded people with visual disabilities (10).
Exclusion from health research might result from a misconception among health professionals that disabilities are of interest primarily as end points in studies, rather than as demographic characteristics of participants (2). In addition, many researchers are unfamiliar with the ways that persons with disabilities access information and perform activities of daily living. Lacking knowledge about how to design research studies in accessible formats, researchers may assume incorrectly that persons with visual impairment cannot fill out a questionnaire or those with hearing impairment cannot understand verbal instructions, and therefore must be excluded.
Without studies that include persons with disabilities, clinicians lack evidence for effective treatment of this large minority group. They do not know whether or how research conducted in non-disabled populations applies or does not apply to persons with disabilities. For example, the effects may or may not be different for each of the following disabled groups, as compared to non-disabled groups: physical activity to prevent cardiac disease in people who have mobility impairment; frequent self-monitoring and recording of blood glucose to help control diabetes in people who have severe visual impairment; or use of medications that were originally developed for postmenopausal women to prevent bone with young adult women who have spinal cord injuries.
Until people with disabilities are routinely included in research, we cannot know if differences may emerge for those with disabilities in general or with particular disabilities, just as differences have emerged for factors such as gender, race, and co-morbidities. This deficiency of evidence has been identified in several major U.S. publications on health care for people with disabilities as one cause contributing to the lack of structural support for reasonable accommodations within the American healthcare system (2–6).
Disability and universal design: Definitions and context
Historically, definitions of disability have focused on differences between “normal” persons and those who lack a usual range of abilities. After World War II, such concepts coalesced into a medical model of disability. In this model, disability is viewed as a problem caused by disease, trauma, or other health condition requiring medical care. The problem of disability belongs to the disabled individual, who has responsibility for complying with curative efforts, striving to overcome the disability, and adjusting to it (4).
During the disability rights movement of the 1970s and 1980s, persons with disabilities asserted that the major source of their functional limitations was not derived from themselves and their disabilities, but from the failure of physical and social environments to accept and accommodate them. They emphasized that they are persons first and individuals with disabilities second, they have many abilities, and they are more disabled by environments than by their sensory, physical, or cognitive limitations (4).
In 2001, the World Health Organization published the International Classification of Functioning, Disability and Health (ICF) (11). This model synthesizes the medical, social, and environmental perspectives into a biopsychosocial approach. Disability is defined functionally as an “umbrella term for impairments, activity limitations or participation restrictions.” The ICF explicitly acknowledges that disability involves “… a dynamic interaction between health conditions (diseases, disorders, injuries, traumas, etc.) and contextual factors,” particularly environmental factors that “interact with all the components of functioning and disability.” Rather than being seen as an all-or-nothing phenomenon, disability is seen as a continuum, and as an experience that all people may have at some time in their lives (4). The Committee on Disabiliy in America of the Institute of Medicine has recommended adoption of the ICF framework by governmental agencies involved in disability monitoring (12).
The concept of Universal Design (UD)—defined as “the design of products and environments to be usable by all people, to the greatest extent possible, without the need for adaptation or specialized design”—emerged during the 1990s and was originally developed for architecture (13). A classic example of UD is inclusion of a requirement for curb cuts in building codes. Before curb cuts were the norm, people in wheelchairs had little access to public spaces. Now, wheelchair access to such places as public buildings, recreational facilities, or parks is at least theoretically possible throughout the United States. Furthermore, curb cuts make travelling through traffic areas more convenient for many nondisabled persons, such as those riding bicycles, pushing strollers, or pulling wheeled luggage.
Concepts of UD are now used in a wide variety of contexts. When applied to education, UD for Learning provides for a flexible system through which a curriculum can be accessible and useful to a classroom with students of widely divergent abilities and backgrounds (14). In health care, UD has been applied to diverse topics, including general health care (15), medical devices (16), and diabetes self-management education (17).
UDR
We propose UDR—defined as the design of research so that all people can be included as potential participants, to the greatest extent possible, without the need for adaptation or specialized design—as a new model for research (18). UDR is a simple idea, with potentially system-wide, complex implications for researchers and health care providers.
A few simple rules for UDR
In the formative work, Crossing the Quality Chasm: A New Health System for the 21st Century, Plsek suggests “a few simple rules” to guide system change, including (i) setting the general direction or goals; (ii) defining boundaries, prohibitions, or limitations; and (iii) providing guidelines, resources, and support for implementation (19). In the spirit of Plsek’s suggestions, we offer the following “few simple rules” for UDR: (i) plan your research to include all potential participants who meet the inclusion criteria, regardless of their current abilities or disabilities; (ii) do not create exclusion criteria unless there is a compelling scientific rationale; (iii) provide multisensory, flexible options for recruitment, research instruments (such as questionnaires), measurements, and responses from participants, with reasonable accommodations that invite and facilitate participation by persons with disabilities; and (iv) when you do not know how to include someone with a disability, consult someone who does (the potential research participant, another person with that disability who is knowledgeable about the range of methods people use for living fully with it, or a professional who works with persons who have that disability).
Practical guidelines for implementing UDR
Many researchers are unfamiliar with the ways that persons with disabilities access information and perform activities of daily living. Therefore, we offer practical guidelines for implementing the simple rules: (i) plan multiple options for people to learn about, respond to, and arrive at opportunities to participate in research (Table 1); (ii) provide multiple means to communicate the information in research instruments and instructions for participants (Table 2); and (iii) provide multiple means of responding to research instruments and interventions (Table 3). These tables do not include an exhaustive set of possibilities. They are based on the authors’ experiences working mainly with persons who have hearing and visual disabilities. We invite comments from researchers with experience including people with other kinds of disabilities in research, and look forward to the development of comprehensive guidelines using multiple creative methods for inclusion of persons with disabilities in mainstream research.
Table 1.
Practical UDR guidelines for recruitment, accommodation, and site selection.
| Recruit through a variety of media. |
|---|
| • Make large print recruitment notices, using nationally recognized standards for large print (20). |
| • Use audible recruitment (for example, audible announcements on radio or television or in person at support groups). |
| • Recruit through local disability agencies and disability consumer organizations. |
| Plan multiple options for response to recruitment notices. |
| • Allow for response by telephone. |
| • Be prepared to receive responses by video relay service from Deaf participants (20–22). |
| • If you allow for Internet or Web-based responses to recruitment, provide a site accessible to screen readers and compliant with Section 508 Amendment of the 1973 Rehabilitation Act (24). |
|
Plan to accommodate special needs of participants during data gathering and other
research activities. |
| • Do not add disabilities to exclusion criteria unless they would substantively alter the scientific content of the research. |
| • Consult with disability experts about facilitating access for your particular project. |
| • In all recruitment materials, include contact information for requesting reasonable accommodations. |
| • For events lasting two or more hours, have planned breaks or rest periods. |
|
Plan for accessibility when choosing the location for research activities that involve
participants. |
| • Whenever feasible, plan for participation from a distance (for example, through online surveys or telephone interviews). |
| • When planning a location for face-to-face interaction, consider (i) the needs of non-drivers (such as a need for accessible and reliable public transportation, or inclusion of transportation for non-drivers in the research budget) and (ii) building accessibility standards, especially those pertaining to people in wheelchairs. |
| • Before research activities begin, provide an orientation to surroundings for people with visual impairment by (i) explaining the route or guiding each person from the front door to the correct room within a building and (ii) giving a brief orientation to the room layout, the location of a nearby bathroom, and, if meal times are included in research activities, a location for obtaining a meal. |
Table 2.
Practical UDR guidelines for communicating information in research instruments and interventions.
| Provide auditory, visual, tactile, and low literacy options for communicating all necessary information. |
|---|
| • Ensure that all materials needed by research participants are available in multiple formats (for example, the informed consent form, research instruments, and instructions for interventions). |
| • Ask each individual to choose his or her preferred format. |
| • Create print materials in a format readily transformed into accessible materials, according to the National Instructional Materials Accessibility Standard (23). The simplest way to do this for short documents is to use the “Styles” option in Word. |
| • Use plain language (24, 25). |
| • In visual formats, use pictures to illustrate major concepts. |
| • In audio formats, use conversations and sounds to illustrate major concepts. |
| • When creating study Web sites, make sure they are accessible to screen readers and compliant with Section 508 Amendment of the 1973 Rehabilitation Act (26). |
| • For surveys with numbered responses, consider using a telephone keypad survey, which is accessible to anyone who uses a telephone. |
| □ Options for communicating with persons with hearing impairment |
| • For communicating with persons who are hard of hearing, (i) speak in the middle of your voice range, (ii) pronounce words clearly, (iii) resist the urge to over-enunciate, which distorts pronunciation and lip movements, and (iv) consider purchasing and offering the use of a portable personal amplifier. |
| • Lip reading, although not sufficient for good communication alone, can provide useful information that helps make speech more understandable. Ask the person if he or she uses lip reading. For lip readers, position yourself with clear sight lines and good lighting on your face. Avoid sitting with a bright window behind you. |
| • For communicating with persons who use American Sign Language (ASL), hire an ASL interpreter (27). Because ASL has different grammar, syntax, and vocabulary from English, translation may not be exact (28). Like native speakers of other languages, people with ASL as their first language often have difficulty reading English fluently; they may need an ASL interpreter to understand documents in written English. Plain language in the original document can make accurate translation easier. |
| • Use a Video Relay Service to communicate with Deaf participants by telephone (20–22). (Telecommunication Device for the Deaf, an older technology, is being phased out.) |
| • When using audiovisual materials for interventions, ensure that all needed information is communicated visually (for example, though closed captioning). |
| □ Options for communicating with persons with visual impairment |
| • For participants with low vision, provide materials in large print (18 point, bold, sans-serif font) on non-glare paper; encourage the use of magnifiers and other assistive technology (29, 30). |
| • Provide materials in Braille for Braille readers (31). |
| • Provide text documents in digital format to participants who use computers with screen readers. |
| • Consider (i) providing audio recordings for people who cannot read large print or Braille and (ii) using digital media that allow for personalization (for example, changing the size and colors of fonts and controlling volume). |
| • When using audiovisual materials for interventions, ensure that all needed information is communicated audibly though a sound track that describes any necessary visual information or through audio description (32). |
Table 3.
Practical UDR guidelines for providing multiple means of responding to research instruments and interventions.
| Provide visual, voiced, and tactile means of response to questionnaires and other research instruments. |
|---|
| • For visual response, use both written and picture choices. |
| • Consider (i) using a Video Relay Service to communicate with Deaf participants, (ii) allowing Braille responses from Braille writers, (iii) providing an ASL interpreter for Deaf participants who use ASL, (iv) using touch screen questionnaires on tablet or pad computers, with visual, tactile, and audio cues, and (v) using telephone interviews, a standard technique that is already accessible to most people. |
| Provide accessible options for interventions. |
| • For self-management interventions using technology, ensure that options are available with visual, audible, and tactile output (for example, talking blood pressure and blood glucose meters with large print, insulin pumps with vibrating alarms, talking pedometers, and alarm clocks that talk or have flashing lights). |
| • For qualitative research that requires participants to keep journals, allow a recorded format for those who keep records as recordings. Consider providing a low-cost digital recorder that can be downloaded into a computer for easy transcription. |
Case Study: An Example of UDR
A researcher investigating cognitive impairment after adverse cardiac events became concerned about the validity of standard instruments for measuring cognitive impairment. In particular, one instrument requires reproducing a hand-drawn complex figure; another requires following verbal instructions. The population from which the research sample was drawn included many older adults. High rates of visual, hearing, and dexterity impairments led to a corresponding high potential for false positive measurements of cognitive impairment. Following simple rules 1 and 2, the researcher decided to include these persons with disabilities in the study.
The researcher believed she could provide options for persons with visual, hearing, and dexterity impairments to access and respond to the instruments used in the study (simple rule 3). However, she was not familiar with specific techniques, so she consulted someone who had worked with these populations (simple rule 4). The consultant offered procedural revisions: (i) The complex figure is now printed with thick lines on a large page of ivory-colored paper, making the figure more visible for persons with mild to moderate visual impairment and reducing background glare. (ii) A marker with a thick body and a pencil grip is provided for drawing the figure, allowing persons with dexterity impairment to hold the marker and persons with low vision to see what they draw. (iii) A video recording of the instructions is delivered on a computer screen, with noise-cancelling headphones plugged into the audio output. This accommodation allows persons with visual impairment to hear the instructions and those with hearing impairment to read lips and to adjust the volume to a comfortable level. As an unexpected benefit, it standardizes the instructions, ensuring that they are delivered as intended, unaffected by unusual pronunciations, variations in voice tones, or reading errors.
CONCLUSION
In summary, we propose a few simple rules and practical guidelines for UDR. We hope that UDR will promote inclusion of people with disabilities in health research, increase the generalizability of the results, and improve clinical applicability to entire populations. Furthermore, improved evidence about the health needs of persons with disabilities can be expected to produce improved care, and ultimately improved health, for this large minority population.
Acknowledgments
Funding: The work on this article was funded by a grant from the National Institutes of Nursing Research: 3P30NR010676-03S1 (S.M.M, principal investigator). Competing interests: A.S.W. has been paid as a consultant by Eli Lilly.
Footnotes
Simple changes in clinical study design allow individuals with disabilities to participate in and contribute to such research.
References and Notes
- 1.Americans with Disabilities Act of 1990. 1990.
- 2.U.S. Department of Health and Human Services [12/12/2010];Healthy People 2010: Disability and Secondary Conditions. 2000 Available from: http://www.healthypeople.gov/document/HTML/Volume1/06Disability.htm.
- 3.U.S. Department of Health and Human Services [12/12/2010];Healthy People 2020: Disability and Health. 2010 Available from: http://www.healthypeople.gov/2020/topicsobjectives2020/overview.aspx?topicid=9.
- 4.Iezzoni L. More than Ramps: A Guide to Improving Health Care Quality and Access for People with Disabilities. Oxford University Press; New York: 2006. [Google Scholar]
- 5.Leavitt MO. The Surgeon General’s Call to Action to Improve the Health and Wellness of Persons with Disabilities. U.S. Department of Health and Human Services; Washington, D.C.: [updated 1/4/2007]. 2005. Available from: http://www.surgeongeneral.gov/library/disabilities/calltoaction/index.html. [Google Scholar]
- 6.National Council on Disability . The Current State of Health Care for People with Disabilities. National Council on Disability; Washington, D.C.: 2009. [Google Scholar]
- 7.Agency for Healthcare Research and Quality [updated 9/20104/20/2010];Developing Quality of Care Measures for People with Disabilities. 2010 Available from: http://www.ahrq.gov/populations/devqmdis/index.html#contents.
- 8.Centers for Disease Control and Prevention (CDC) Prevalence and most common causes of disability among adults—United States, 2005. MMWR Morb. Mortal. Wkly. Rep. 2009;58:421–426. Medline. [PubMed] [Google Scholar]
- 9.Centers for Disease Control and Prevention . Diabetes data and trends:health status and disability. Centers for Disease Control and Prevention; Atlanta, GA: 2007. Available from: http://apps.nccd.cdc.gov/DDTSTRS/default.aspx. [Google Scholar]
- 10.Williams AS, Schnarrenberger PA. A comparison of dosing accuracy: visually impaired and sighted people using insulin pens. J. Diabetes Sci. Tech. 2010;4:514–521. doi: 10.1177/193229681000400303. Medline. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.World Health Organization . International Classification of Functioning, Disability and Health. World Health Organization; Geneva: 2001. [Google Scholar]
- 12.Institute of Medicine . The Future of Disability in America. National Academies Press; Washington, D.C.: 2007. [PubMed] [Google Scholar]
- 13.NC State University College of Design [2/8/2010];The Center for Universal Design. 2008 Available from: http://www.design.ncsu.edu/cud/
- 14.National Center on Universal Design for Learning . UDL Guidelines. Center for Applied Special Technology; Wakefield, MA: [updated 03/15/2010]. 2010. Available from: http://www.udlcenter.org/aboutudl/udlguidelines#top. [Google Scholar]
- 15.Mace R. Removing Barriers to Health Care: A Guide for Health Professionals. Center for Universal Design and The North Carolina Office on Disability and Health; ND: Available from: http://www.fpg.unc.edu/~ncodh/pdfs/rbhealthcare.pdf. [Google Scholar]
- 16.Wilcox S. [May 7, 2009];Applying Universal Design to Medical Devices. Design Science. 2003 Available from: http://www.dscience.com/articles/MDDIJanO3UnivDesign.pdf.
- 17.Williams AS. Universal design in diabetes care: an idea whose time has come. Diabetes Educ. 2009;35:45–57. doi: 10.1177/0145721708329700. doi:10.1177/0145721708329700 Medline. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Williams A. Universal design of research: an introduction. Frances Payne Bolton School of Nursing; Cleveland, Ohio: 2010. Available from: http://fpb.case.edu/FINDLab/udr.shtm. [Google Scholar]
- 19.Plsek P. Redesigning health care with insights from the science of complex adaptive systems. In: Medicine Io., editor. Crossing the Quality Chasm: A New Health System for the 21st Century. National Academy Press; Washington, D.C.: 2001. pp. 309–22. [Google Scholar]
- 20.National Association of the Deaf [12/10/2010];Telephone and Relay Services. n.d. Available from: http://www.nad.org/issues/technology/telephone-and-relay-services.
- 21.Federal Communications Commission [updated 5/6/201012/10/2010];Video Relay Services. 2010 Available from: http://www.fcc.gov/cgb/consumerfacts/videorelay.html.
- 22.Telecommunications for the Deaf Inc [12/10/2010];Fact Sheet: Video Relay Service Options. 2010 Available from: http://www.tdi-online.org/tdi/fs_videorelayservices.html.
- 23.Material NCoAI [updated 10/5/201012/10/2010];What is the National Instructional Materials Accessibility Standard (NIMAS)? 2010 Available from: http://aim.cast.org/learn/policy/federal/what_is_nimas.
- 24.Plain Language Action and Information Network [updated 12/201012/12/2010];Federal Plain Language Guidelines. 2010 Available from: www.plainlanguage.gov/howto/guidelines/bigdoc/index.cfm.
- 25.U.S. Department of Health and Human Services [12/12/2010];Plain language: a promising strategy for clearly communicating health information and improving health literacy. n.d. Available from: http://www.health.gov/communication/literacy/plainlanguage/PlainLanguage.htm.
- 26.United States Government [updated 6/201012/10/2010];Section 508.gov: Standards. 2010 Available from: http://www.section508.gov/index.cfm?fuseAction=stds.
- 27.Registry of Interpreters for the Deaf [12/10/2010];Find an interpreter/member. 2010 Available from: https://www.rid.org/acct-app/index.cfm?action=search.members.
- 28.National Institute on Deafness and Other Communication Disorders [12/10/2010];American Sign Language. 2010 Available from: http://www.nidcd.nih.gov/health/hearing/asl.html#d.
- 29.Kitchel JE. [updated 3/26/201012/12/2010];Large Print: Guidelines for Optimal Readability and APHontTM a font for low vision. American Printing House for the Blind. 2004 Available from: http://www.aph.org/edresearch/lpguide.htm.
- 30.American Foundation for the Blind [12/10/2010];Reading Tools and Techniques. 2010 Available from: http://www.afb.org/seniorsite.asp?SectionID=66&DocumentID=3254.
- 31.American Foundation for the Blind [12/12/2010];Braille/Electronic/Audio/Large Print Production - Find Services - Results. 2010 Available from: http://www.afb.org/Results.asp?CategoryID=13&SectionID=6&DocumentID=1356.
- 32.Coalition AD. [12/10/2010];About Audio Description. 2010 Available from: http://www.audiodescriptioncoalition.org/aboutad.htm.